Abstract
Iron poisoning is a well-respected historically significant toxicologic problem. In the pediatric population, iron has been regarded as the most fatal of all toxic exposures [1]. Fortunately because of regulations on packaging in the USA and other countries, serious poisonings have declined [2]. Visible warning labels and dispensing of tablets and capsules in blister packages have limited the dose a child might consume. For example, iron poisoning fatalities in children less than 6 years of age in the USA decreased from 29 in 10 years before the packaging regulation to one death in the 5 years after [3]. Total reported exposures in children younger than 6 years old have declined from 3026 in 1995 to 2139 in 2013 in the USA [4, 5]. The other patient population at risk is suicidal patients, most notably women of childbearing age with access to iron products. In 2013, 28% of iron exposures in the USA occurred in patients who were teenagers or older [5]. Despite the significant toxic potential of iron, death and serious sequelae are uncommon because most exposures are unintentional and involve negligible amounts.
Access provided by CONRICYT-eBooks. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Iron
- Iron poisoning
- Hemoglobin
- Ferritin
- Transferrin
- Ferrous gluconate
- Ferrous sulfate
- Ferrous fumarate
- Haber–Weiss reaction
- Free radicals
- Lipid peroxidation
- Coagulopathy
- Metabolic acidosis
- Hepatotoxicity
- Gastric outlet obstruction
- Serum iron concentration
- Gastrointestinal hemorrhage
- Deferoxamine
- Whole-bowel irrigation
- Ferrioxamine
Iron poisoning is a well-respected historically significant toxicologic problem. In the pediatric population, iron has been regarded as the most fatal of all toxic exposures [1]. Fortunately because of regulations on packaging in the USA and other countries, serious poisonings have declined [2]. Visible warning labels and dispensing of tablets and capsules in blister packages have limited the dose a child might consume. For example, iron poisoning fatalities in children less than 6 years of age in the USA decreased from 29 in 10 years before the packaging regulation to one death in the 5 years after [3]. Total reported exposures in children younger than 6 years old have declined from 3026 in 1995 to 2139 in 2013 in the USA [4, 5]. The other patient population at risk is suicidal patients, most notably women of childbearing age with access to iron products. In 2013, 28% of iron exposures in the USA occurred in patients who were teenagers or older [5]. Despite the significant toxic potential of iron, death and serious sequelae are uncommon because most exposures are unintentional and involve negligible amounts.
Biochemistry and Pharmacokinetics of Iron
The primary functions of iron include participation in oxygen delivery as a constituent of hemoglobin and myoglobin and production of adenosine triphosphate via oxidative phosphorylation. It is a highly reactive ion and functions in many enzymatic biochemical processes. Iron is a transition metal (number 26 on the periodic table) with an atomic weight of 55.8. It is the second most prevalent metal and the fourth most abundant element in the Earth’s crust.
Iron has interesting and unique properties related to its absorption, distribution, and elimination. Intestinal iron absorption is a complex and active process that occurs mostly in the proximal small intestine [6]. Most dietary inorganic iron is in the ferric (Fe3+) form. Iron in the gut lumen may form complexes with other constituents, forming insoluble nonbioavailable products. Mucin, at the cell surface of the enterocyte, binds iron, preparing it for integrin-mediated systemic absorption. Mobilferrin binds the iron within the enterocyte cytoplasm. Iron eventually is transferred to paraferritin and ferritin before entering the bloodstream complexed to transferrin. Because the proportion of iron absorbed decreases with increasing dose [7], an overdosed patient absorbs disproportionately less of the dose ingested than the amount absorbed when iron is given therapeutically. In healthy adults, 2–10% of dietary iron eventually is absorbed. A canine model showed that only 14% of a fatal oral dose of ferrous sulfate was absorbed [8]. In contrast, people with iron deficiency may absorb 80–90% of an oral dose [9].
After oral ingestion, iron either remains in the gut mucosa and eventually is excreted in the stool or is transported in the blood by transferrin primarily to the bone marrow for hemoglobin synthesis. The liver differs from the rest of the body, including the placenta, in that its capacity for iron uptake is unlimited [10, 11]. This first-pass effect is chiefly responsible for the decrease in plasma iron concentration after ingestion. These concepts support early iron concentration determination – 4–6 h after ingestion – as being useful after overdose, followed by the use of clinical parameters to predict prognosis after 8–12 h.
Pharmacokinetics of Iron
Volume of distribution: preparation dependent
Protein binding: 99%
Mechanisms of clearance: renal, fecal, skin desquamation
Active metabolites: none
Method to enhance clearance: deferoxamine
Total iron body stores are approximately 3–4 g in adults, with 70% distributed in hemoglobin in the ferrous (Fe2+) state. It is also present in ferritin and hemosiderin, which are stored in the liver, spleen, and bone marrow. About 1–2 mg of iron is eliminated daily through urinary and fecal excretion and skin desquamation. The usually recommended daily allowance of iron is 10 mg in men, 18 mg in women, and 30–60 mg in women during pregnancy and lactation.
The amount of elemental iron ingested is the key factor in predicting the severity of toxicity. Common preparations contain various percentages of elemental iron (Table 1). Although 20 mg/kg of elemental iron or less may result in gastric upset, potentially severe toxicity may follow ingestions of 40–60 mg/kg, and potentially lethal doses range from 200–250 mg/kg [12]. In toddlers, doses of 1.0 g of elemental iron have been reported to be fatal [13, 14].
Pathophysiology
Iron , an essential element for bodily functions, must come from exogenous sources. It functions as a catalyst for the Haber–Weiss reaction resulting in the generation of a highly reactive hydroxyl radical:
Iron-induced lipid peroxidation , resulting from the production of these free radicals , is the primary mechanism of iron poisoning [15, 16]. These free radicals induce local injury, most notably in locations of high iron concentrations, such as the intestine and liver. The primary intracellular target of toxicity is the mitochondria, resulting in destruction of cristae and loss of respiratory enzyme activity in a manner that is consistent with suppression of cellular respiration, without uncoupling oxidative phosphorylation [17, 18]. Iron primarily affects the gastrointestinal (GI) tract, liver, cardiovascular system, and acid–base status of the poisoned patient. Because of the high metabolic activity of the heart, the myocardial mitochondria are particularly vulnerable to the toxic effects of iron poisoning.
Gastrointestinal
The initial GI symptoms after iron overdose are due to a direct local irritant effect. With large ingestions, free radical-induced lipid peroxidation causes secondary injury to the GI tract. There is a significant risk of hemorrhage and ulcerative damage from segmental gut infarction in children and adults [19]. Because of this damage, there is a concern for emerging GI bleeding during the first 48–72 h after ingestion. Delayed effects, classically stricture formation, may occur weeks after exposure. Gastric outlet obstruction occurring 2–4 weeks post exposure is a consequence of healing and scarring of the gut. A high index of suspicion for gastric outlet obstruction exists in patients who have continual vomiting 2–3 weeks after the exposure incident or an onset of emesis after a symptom-free period [20]. Although pyloric injury is most common, lesions may occur at any location in the gut [19].
Hepatic
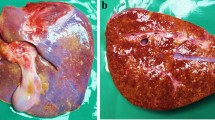
Characteristic hemorrhagic hepatic periportal necrosis has been described in autopsy reports of patients who died from iron poisoning and in experimental animal models [21]. Other reports indicate similar damage in patients and animal models [22]. After absorption, iron is transported to the liver via the portal vein, where carrier-mediated uptake into zone 1 acinar cells eventually becomes overwhelmed. Microscopic observations indicate that hepatic mitochondrial injury within zone 1 is the primary location and mechanism of toxicity [23]. Because liver cell regeneration is a zone 1 function, injury to this region is of particular significance. After this injury, acute hepatic failure with elevated hepatic transaminases and serum ammonia concentrations, jaundice, steatosis, and hepatic coma may occur [24].
Coagulopathy
Coagulopathy resulting from severe iron poisoning is characteristically biphasic [25]. A dose-related reversible coagulopathy has been demonstrated in a canine model and in humans [25]. This condition results from a transient, early, dose-dependent depression of coagulation factors V, VII, IX, and X, causing a prolongation of the partial thromboplastin time [25]. An in vitro study revealed that free iron may inhibit the formation of thrombin and subsequently thrombin’s ability to form fibrin from fibrinogen [26]. This early coagulopathy may subside as iron levels decrease; however, severe poisoning may result in a second phase (2–7 days postingestion) of progressive dysfunction of coagulation secondary to hepatotoxicity.
Cardiovascular
Circulatory shock is the most common cause of death after severe iron poisoning . In addition to hypovolemia resulting from GI volume loss and hemorrhage, an early distributive shock has been shown in animal models [27, 28]. The myocardium has high metabolic activity, and acute iron-induced cardiotoxicity may be mediated by free radical generation [29]. In addition to interference with mitochondrial adenosine triphosphate production, membrane lipid peroxidation may interfere directly with slow-channel calcium exchange or the activity of the sarcoplasmic reticulum [30]. Diminished myocardial contractility is an important component of the pathogenesis of iron-induced shock [31]. Cardiac failure may occur 1 to several days after a major iron overdose [32]. The pathophysiology of shock resulting from iron overdose is therefore multifactorial.
Metabolic
Metabolic acidosis is a prominent feature of iron poisoning . As discussed earlier, circulatory shock is one pathophysiologic mechanism responsible for this metabolic acidosis. Acidosis also may occur, however, in the absence of cardiovascular instability [33]. As described previously, iron poisoning suppresses cellular respiration. A principal mechanism by which iron causes a metabolic acidosis occurs, however, after absorption of a quantity of iron that exceeds the binding capacity of transferrin . When unbound iron is present, its hydrolysis liberates three unbuffered protons from each ferric ion [34]:
Other Pathophysiologic Effects
Altered mental status may occur after large ingestions and is presumably multifactorial and related to the factors described earlier. Although no major direct toxicity is clinically apparent and relevant to the central nervous system, kidney, lung, and spleen, autopsy studies have revealed elevated iron concentrations in these organ systems and in the stomach, liver, and small intestine [35].
Clinical Presentation and Life-Threatening Complications
Classically, iron poisoning is described as occurring in five clinical stages (Table 2). Not all patients manifest this “textbook” presentation after overdose, however, and there is the potential for considerable temporal variability and overlap among these stages. The severity and stage of a particular patient’s poisoning should be determined by his or her individual clinical evaluation, not simply by the number of hours postingestion.
Stage I (the GI stage) of poisoning is encountered almost universally in all patients after significant iron ingestion. Epigastric pain, nausea, vomiting, and diarrhea typically occur immediately after ingestion in cases of overdose [36]. Hypotension, pallor, and lethargy often occur, resulting from vasodilation, intravascular volume loss, gastroenteritis, hematemesis, melena, or hematochezia secondary to the local effects of iron on the gut mucosa. Metabolic acidosis may occur at this stage. If acidosis is significant, blood volume loss occurs, resulting in circulatory shock, and the patient may progress directly into stage III.
Stage II is the time period associated with iron poisoning that is described as the latent or quiescent phase. During this interval, which may begin several hours postingestion, the patient is in transition between the resolution of direct GI signs and symptoms and the appearance of overt systemic toxicity. This often-described quiescent phase may reflect failure to recognize ongoing clinical toxicity. The patient may have fewer overt GI manifestations during this time, lulling the clinician into an underestimation of the true seriousness of the ingestion [12]. During this apparently clinically benign period, however, patients may have a worsening metabolic acidosis if volume resuscitation is not sufficient to restore adequate tissue perfusion. Patients who progress through stage I with resolution of clinical manifestations and without development of a metabolic acidosis are unlikely to develop more serious systemic iron toxicity.
Stage III, the shock stage of iron toxicity, is defined by evidence of insufficient tissue perfusion and shock and typically becomes manifest at least several hours after ingestion. Most deaths due to iron poisoning occur in this stage. Multiple organ dysfunction as a result of cellular toxicity and inadequate perfusion may result in hypotension, tachycardia, altered mental status, seizures, coma, worsening metabolic acidosis, renal failure, hepatic dysfunction, coagulopathy, myocardial depression, pulmonary edema, and mesenteric ischemia [37]. Hepatotoxicity often is evident during stage III; however, this may also occur without concomitant shock.
Stage IV (hepatotoxicity) is not a universal finding in iron-poisoned patients [38]. The onset of this stage typically occurs 12–24 h postingestion but may occur 2–3 days after overdose [24]. Hepatic dysfunction is a poor prognostic sign when present [25], with hemorrhage secondary to coagulopathy often contributing to patient demise [25].
The hallmark of stage V is gastric outlet obstruction; however, fortunately this stage rarely occurs [12]. Local mucosal injury may lead to development of stricture formation several weeks postingestion [19]. Although the classic site of obstruction is the pylorus, segmental injury may occur along the length of the gut [19]. The diagnosis of gastric outlet obstruction should be considered in patients with persistent vomiting, achlorhydria, abdominal pain, and distention more than 1 week postingestion.
Iron poisoning may present in any of the abovementioned discrete stages, may skip specific stages, or may reflect overlap between or among different stages. The stages of toxicity are used as a guide to the conceptualization of the natural course of iron poisoning rather than as a consistently predictable sequence of events.
Diagnosis
The diagnosis of iron toxicity may be evident based on a history of ingestion and corresponding signs of iron toxicity. Any pediatric ingestion over 40 mg/kg (or 6.5 ml syrup/kg) should be assessed for iron toxicity. GI symptoms are present within 1 hr of ingestion in virtually all patients with significant iron ingestions [39]. Tachycardia may also be an early sign of iron toxicity. If no history of iron ingestion is offered, however, the differential diagnosis includes other medical and surgical reasons for the varied manifestations of iron poisoning. Other poisonings to consider include those involving mercuric chloride, salicylates, pesticides, arsenic, and colchicine.
All patients with known or suspected iron overdose should receive an X-ray of the abdomen to evaluate for radiopaque tablets [40, 41]. Large overdoses of tablets can be visualized in the GI tract, helping to verify historical features and guide management with GI decontamination. If the patient ingested a liquid preparation, the abdominal film typically is unrevealing [41]. Pediatric multivitamins containing iron have such a low iron content that X-rays after ingestion of these also typically are negative [42]. Clinically significant poisoning after ingestion of iron-containing multivitamins is virtually nonexistent [43]. Negative abdominal plain films after iron ingestion also may be explained by dissolution of an ingested solid formulation; this is especially true in patients who present late after ingestion.
We recommend that a serum iron concentration be obtained on presentation and then every 1–2 h to monitor the symptomatic patient further. When a clear downward trend of serum iron concentrations is established, it is no longer necessary to follow this parameter. Iron concentrations less than 500 μg/dL (<90 μmol/L) at 4–6 h postingestion typically are not associated with significant systemic toxicity [44, 45]. Systemic toxicity often is seen with iron concentrations of 500–1000 μg/dL (90–180 μmol/L), with levels greater than 1000 μg/dL (>180 μmol/L) being associated with severe life-threatening illness.
A high anion gap metabolic acidosis accompanying an elevated lactate concentration should be assumed to be an indication of serious toxicity from iron ingestion [37] and the need for chelation therapy. Because of the possibility of hemorrhage and multiple-organ toxicity, a complete blood count, hepatic and renal function tests, electrolytes, and coagulation profile should be obtained. The presence of hemorrhage or anemia should prompt preparation for possible blood product replacement.
Historically, other laboratory findings, such as leukocytosis (white blood cell count >15,000/mm3) and hyperglycemia (serum glucose >150 mg/dL [8.25 mmol/L]), were used as indices of severity of iron poisoning [46]. These parameters have not been shown to be sensitive predictors of toxicity, however [44, 47]. Likewise, a serum iron concentration greater than the total iron-binding capacity, previously considered an indication for chelation therapy, has not been found to be a reliable index of toxicity and no longer is recommended [44, 48, 49].
Treatment
Patients with significant iron ingestions or severe systemic toxicity warrant monitoring in the intensive care unit. Secure intravenous access, fluid volume replacement, oxygen supplementation, cardiac monitoring, and airway and ventilatory support are essential to the initial management of the critically iron-poisoned patient. Bedside ultrasound of the heart and inferior vena cava or even a Swan–Ganz catheter may be indicated for monitoring of hemodynamic parameters during treatment and to differentiate between cardiogenic and distributive shock.
Limiting the absorption of ingested iron should be considered during initial management. Gastric lavage is an alternative form of gastric emptying. This procedure also has serious risks, has not proved to change outcome after iron ingestion, and should be considered only in life-threatening ingestions presenting within 1 h [50, 52]. Even in these circumstances, the efficacy of gastric lavage is questionable. Activated charcoal has not been shown to be effective in adsorbing iron [53]. Consideration of activated charcoal is appropriate when coingestion of noniron products has occurred. However, activated charcoal has not been shown to alter the outcome in poisoned patients. It may decrease drug absorption if given within 1 hr of ingestion.
Indications for ICU Admission in Iron Poisoning
Significant acidemia (arterial pH < 7.3)
Shock/neurodynamic compromise
Altered mental status
Gastrointestinal hemorrhage
Serum iron concentration >500 μg/dL (90 μmol/L)
Radiologic evidence of a significant gastrointestinal burden of iron (>50 mg of elemental iron/kg)
Deferoxamine administration
Significant hepatic dysfunction
The mainstay of GI decontamination for iron poisoning generally is considered to be whole-bowel irrigation [54, 55] (Grade III evidence). This procedure has not been shown, however, to alter the clinical course or outcome of iron-poisoned patients [54]. Whole-bowel irrigation theoretically is important only in patients with abdominal radiographs revealing substantial numbers of radiopaque iron tablets. Whole-bowel irrigation is reviewed in Chap. 3, “Therapeutic Approach to the Critically Poisoned Patient.” Although whole-bowel irrigation usually is limited to several hours of administration, one case report of multiple iron tablet persistence in the gut described a 5-day course of whole-bowel irrigation [56]. This case also may be taken as evidence, however, of the lack of efficacy of this technique. Subsequent abdominal X-rays can help guide the clearance of iron from the gut.
Gastroenterologic or surgical consultation may be warrented if a concretion or bezoar is shown or suspected; this is unusual, however. Concretions may be present when iron levels continue to rise. Usually there is a downward trend toward clearing by 6–24 h postingestion. Several authors reported successful gastrotomy and removal of massive amounts of iron tablets not amenable to removal by less invasive measures [57–61]. Clinical evidence of bowel obstruction may indicate intestinal necrosis. Lifesaving small-bowel resection was performed 24 h after presentation in a patient with a distended abdomen and signs of peritonitis [62].
Other attempts at reducing iron absorption from the gut have been undertaken without success. Oral bicarbonate, phosphate, and magnesium hydroxide have been used with the idea that if they formed insoluble complexes with iron, this would decrease absorption. Except for one canine study, data from in vitro and in vivo studies do not support bicarbonate or phosphate use, and these treatments may result in severe electrolyte imbalances [63–66]. Animal and human volunteer studies revealed a reduction in iron absorption after the administration of magnesium hydroxide; however, it does not affect absorption in humans after large overdoses of iron [67–69]. At present, there are insufficient data to support routine use of these modalities in human iron poisoning. Oral deferoxamine was shown in one prospective human study to reduce GI absorption of ferrous sulfate when mixed as a slurry with activated charcoal. Ferrioxamine , the deferoxamine–iron complex, has been shown to be lethal in animals after it is absorbed, but ferrioxamine absorption is reduced when activated charcoal is coadministered with deferoxamine [70, 71]. Because of the concerns about the toxicity of ferrioxamine, oral deferoxamine is not recommended.
Iron-induced hepatotoxicity should be regarded as a marker of severe toxicity. Because the periportal area is most affected, iron-induced hepatotoxicity portends a much poorer overall prognosis than similar insults caused by other toxicants [22]. In light of this, hepatic monitoring and treatment of organ failure or coagulopathy are indicated. Profound liver dysfunction warrants surgical consultation for possible transplantation. Correction of electrolyte and glucose abnormalities also may be crucial to patient outcome.
Hemodialysis should be used on a supportive basis for acute renal failure, usually developing in response to circulatory shock. Iron is not amenable to hemodialysis, even though the iron–deferoxamine complex can be cleared in this manner [72, 73].
Deferoxamine , derived from Streptomyces pilosus, is the specific chelator of choice for iron poisoning . After complexing with free iron (iron not found in hemoglobin, myoglobin, ferritin, or transferrin), it forms ferrioxamine, which is excreted in the urine [3]. Deferoxamine also has been shown to promote clearance of intracellular iron effectively. Ferrioxamine produces a reddish-brown or “vin rose” appearance to the urine [74]. Deferoxamine challenge tests have been used in the past as a marker of iron excretion, as indicated by this urine color change. This test no longer is recommended; however, it is one may observe a urine sample before treatment and follow the course of color change during chelation. A total of 100 mg of deferoxamine mesylate chelates only approximately 8.5 mg of ferric iron. Although the use of deferoxamine in severe iron poisoning is considered the standard of care, there are no published controlled studies that show a change in outcome with this treatment [75, 76] (Grade III evidence).
Deferoxamine treatment should be administered as early as possible after poisoning. Although not formally validated, the data reviewed earlier in this chapter that suggest logical indications for deferoxamine treatment are indications of moderate-to-severe systemic toxicity, such as shock, GI bleeding, lethargy, and central nervous system depression. Metabolic acidosis is a reliable marker of cellular iron toxicity [37] and therefore should be considered to be an indication for initiating treatment. There is no rationale for withholding chelation while waiting for a serum iron concentration in significantly poisoned patients. An iron level 4–6 h postingestion of equal to or greater than 500 μg/dL (≥90 μmol/L) also is considered to be an indication for treatment [44, 45] (Grade III recommendation). After 12 h, the serum iron concentration is of no practical significance because the systemic burden has been distributed from the vascular compartment into tissues.
Recommendations for deferoxamine dosing are based primarily on case reports and have been established arbitrarily [76]. The intravenous route of administration is preferred. Intramuscular administration was used previously for less severe poisoning, but it is not reliable. Titration of the intravenous infusion up to a rate of 15 mg/kg/h should be initiated while the patient is carefully monitored for adverse effects, including rate-related hypotension [77, 78]. Histamine release may underlie the hypotension and the flushing and urticaria that may be observed during deferoxamine infusion [78]. Administration of deferoxamine at even higher rates has been shown to be safe in ill patients and in patients on long-term hemodialysis [79]. There have been recommendations to administer less than 6–8 g/day even though 16 g/day has been given without concomitant side effects [80]. It is vital to maintain adequate intravenous fluid volume replacement during deferoxamine therapy to protect against the development of acute renal failure [81]. Finally, continuous infusions for greater than 24 h have been reported to be associated with adult respiratory distress syndrome; however, this interpretation is confounded by the presence of adult respiratory distress syndrome in severe iron poisoning, even in untreated cases [82–84]. A reasonable end point of therapy is cessation of anion gap metabolic acidosis and resolution of systemic toxicity. Because the deferoxamine–iron complex acts as a siderophore for the growth of Yersinia enterocolitica, sepsis after chelation therapy is a risk, and appropriate antimicrobial therapy should be initiated if high-grade fever, diarrhea, or signs of peritonitis develop. Appropriate antibiotics include aminoglycosides, trimethoprim–sulfamethoxazole, third-generation cephalosporins, doxycycline, or fluoroquinolones. If abscesses occur, they will require surgical drainage. Chelation therapy should not be suspended during antibiotic therapy [85–87]. It is important to determine serum iron concentrations by atomic absorption spectroscopy in deferoxamine-treated patients because deferoxamine interferes with most other routine assays.
Criteria for ICU Discharge in Iron Poisoning
Absence of acidemia or other systemic disorders (e.g., coagulopathy)
Hemodynamic stability
Clear sensorium
Declining serum iron concentrations
Special Populations
Pregnant Patients
Iron overdose has occurred with relative frequency in pregnant patients [88]. There is no proven teratogenic risk of deferoxamine therapy during pregnancy, and fetal loss may occur as a result of severe maternal iron toxicity. Similar to trauma and many other diseases of pregnant women, the goals are to stabilize and treat the mother, which stabilizes and treats the fetus. The approach to a pregnant patient is no different from that for any other patient; other than that if the fetus is potentially viable, it should be monitored for distress. Although spontaneous abortion, preterm delivery, and malformations are potential sequelae of treatment in severe iron poisoning, several cases reported successful use of deferoxamine in pregnancy [89–92]. Whole-bowel irrigation has been used successfully in the first trimester to treat an iron overdose [93]. One report described a postnatal fatality in a 30-year-old woman who was treated with deferoxamine 1 day after ingestion and successfully delivered a healthy infant 2 weeks before experiencing lethal multiple organ dysfunction [94]. The placenta serves as the fetus’s barrier to systemic iron overload and associated toxicity. This concept is supported in an ovine model [11]. Deferoxamine may cross the placenta when the mother is treated for toxicity [89]. Harm to the fetus from deferoxamine use in pregnancy is referenced [11, 91] yet not supported by the actual evidence. Cases describe first-trimester use of deferoxamine in women with chronic overload without subsequent fetal abnormalities [95, 96]. Based on this deferoxamine therapy should not be withheld out of concern for the fetus. Appropriately treating the mother is tantamount to treating the fetus.
Parenteral Iron Infusions
Intravenous iron therapy is indicated in patients who (1) are hemodialysis dependent with iron deficiency anemia, (2) have gastrointestinal maladies such as Crohn’s disease or a history of gastric resection or bypass, or (3) are losing iron from blood sources at higher rates than oral iron can be tolerated. While isolated parenteral iron toxicity requiring deferoxamine therapy is not reported, iron infusions can result in infusion reactions. Infusion reactions are considered hypersensitivity reactions and patients at risk include previous reactions, rapid infusion rates, multiple drug reactions, severe atopy, and possibly severe inflammatory diseases [97]. There exists controversy whether or not these reactions are always true IgE mediated in all cases. Iron dextran has historically thought to be linked to anaphylactoid reactions compared to iron gluconate and sucrose [98]. Complement activation-related pseudo-allergy triggered by iron nanoparticles is probably a more frequent pathogenetic mechanism in acute reactions to current formulations of intravenous iron than is an immunological IgE-mediated response [97].
Management of these reactions is therefore recognition and discontinuation of the infusion. Current consensus would still recommend intravenous fluids and corticosteroids for moderate reactions and potentially supplemental oxygen, epinephrine, and a nebulized beta-2 agonist for more severe reactions [99].
Common Errors in Iron Poisoning
Withholding deferoxamine in an ill patient while waiting for a serum iron concentration
Withholding deferoxamine in a pregnant patient who meets criteria for treatment
Assessing a patient in stage II of toxicity as improved or fully recovered
Relying on leukocytosis and hyperglycemia to predict prognosis or guide therapy
Using total iron-binding capacity or a chelation challenge test to indicate need for deferoxamine
Administering deferoxamine to patients who exhibit only direct gastrointestinal toxicity
Key Points in Iron Poisoning
-
1.
Estimate total iron ingested based on the elemental dose and not the weight of the salt.
-
2.
Serum iron concentrations beyond 12 h after ingestion are of no benefit.
-
3.
The end point of deferoxamine therapy is guided best by clinical stability of the patient and cessation of acidemia.
-
4.
Fluid hydration is crucial during deferoxamine administration to help prevent acute renal failure.
-
5.
Pregnant patients are approached in the same way and aggressively as nonpregnant patients.
References
Litovitz T, Manoguerra A. Comparison of pediatric poisoning hazards: an analysis of 3.8 million exposure incidents. Pediatrics. 1992;89:999–1006.
Nightingale SL. From the Food and Drug Administration. JAMA. 1997;277:1343.
Chang TP, Rangen C. Iron poisoning: a literature-based review of epidemiology, diagnosis, and management. Pediatr Emerg Care. 2011;27:978–85.
Litovitz TL, Felberg L, White S, Klein-Schwartz W. 1995 Annual report of the American Association of Poison Control Centers Toxic Exposure Surveillance System. Am J Emerg Med. 1996;14:487–537.
Mowry JB, Spyker DA, Cantilena Jr LR, et al. 2013 annual report of the American Association of Poison Control Centers National Poison Data System (NPDS): 31st annual report. Clin Toxicol. 2014;52:1032–283.
Umbreit JN, Conrad ME, Moore EG, Latour LF. Iron absorption and cellular transport: the mobilferrin/paraferritin paradigm. Semin Hematol. 1998;35:13–26.
Smith MD, Pannacciulli IM. Absorption of inorganic iron from gradient doses: its significance in relation to iron absorption tests and the mucosal block theory. Br J Haematol. 1958;4:428–34.
Reissman KR, Coleman TJ, Budai BS, Moriarty LR. Acute intestinal iron intoxication: iron absorption, serum iron and autopsy findings. Blood. 1955;10:35–45.
Harju E. Clinical pharmacokinetics of iron preparations. Clin Pharmacokinet. 1989;17:69–89.
Zimelman AP, Zimmerman HJ, McLean R, Weintraub LR. Effects of iron saturation of transferrin on hepatic iron uptake: an in vitro study. Gastroenterology. 1977;72:129–31.
Curry SC, Bond GR, Raschke R, et al. An ovine model of maternal iron poisoning in pregnancy. Ann Emerg Med. 1990;19:632–8.
Banner Jr W, Tong TG. Iron poisoning. Pediatr Clin North Am. 1986;33:393–409.
Spencer IOB. Ferrous sulphate poisoning in children. BMJ. 1951;2:1112–7.
Thomson J. Two cases of ferrous sulfate poisoning. BMJ. 1947;1:640–1.
Halliwell B, Gutteridge JMC. Oxygen free radicals and iron in relation to biology and medicine: some problems and concepts. Arch Biochem Biophys. 1986;246:501–14.
Bacon BR, Britton RS. The pathophysiology of hepatic iron overload: a free radical-mediated process? Hepatology. 1990;11:127–37.
Link G, Saada A, Pinson A, et al. Mitochondrial respiratory enzymes are a major target of iron toxicity in rat heart cells. J Lab Clin Med. 1998;131:466–74.
Witzleben CL. An electron microscopic study of ferrous sulfate induced liver damage. Am J Pathol. 1966;49:1053–8.
Tenenbein M, Littman C, Stimpson RE. Gastrointestinal pathology in adult iron overdose. J Toxicol Clin Toxicol. 1990;28:311–20.
Gandhi RK, Robarts FH. Hour-glass stricture of the stomach and pyloric stenosis due to ferrous sulphate poisoning. Br J Surg. 1962;49:613–7.
Luongo MA, Bjornson SS. The liver in ferrous sulfate poisoning. N Engl J Med. 1954;251:995–9.
Tenenbein M. Hepatotoxicity in acute iron poisoning. J Toxicol Clin Toxicol. 2001;39:721–6.
Ganote CE, Nahara G. Acute ferrous sulfate hepatotoxicity in rats: an electron microscopic and biochemical study. Lab Invest. 1973;28:426–36.
Gleason WA, deMello DE, deCastro FJ, Conners JJ. Acute hepatic failure in severe iron poisoning. J Pediatr. 1979;95:138–40.
Tenenbein M, Israels SJ. Early coagulopathy in severe iron poisoning. J Pediatr. 1988;113:695–7.
Rosenmund A, Haeberli A, Straub PW. Blood coagulation and acute iron toxicity. J Lab Clin Med. 1984;103:524–33.
Whitten CF, Chen YC, Gibson GW. Studies in acute iron poisoning: III. The hemodynamic alterations in acute experimental iron poisoning. Pediatr Res. 1968;2:479–85.
Vernon DD, Banner W, Dean JM. Hemodynamic effects of experimental iron poisoning. Ann Emerg Med. 1989;18:863–6.
Artman M, Olsen RD, Boucek RJ, Boerth RC. Depression of contractility in isolated rabbit myocardium following exposure to iron: role of free radicals. Toxicol Appl Pharmacol. 1984;72:324–32.
Pinson GL, Hershko C. Heart cells in culture: a model of myocardial iron overload and chelation. J Lab Clin Med. 1985;106:147–53.
Artman M, Olson RD, Boerth RC. Depression of myocardial contractility in acute iron toxicity in rabbits. Toxicol Appl Pharmacol. 1982;66:329–37.
Tenenbein M, Kopelow ML, deSa DJ. Myocardial failure and shock in iron poisoning. Hum Toxicol. 1988;7:281–4.
Tenenbein M. Toxicokinetics and toxicodynamics of iron poisoning. Toxicol Lett. 1998;102–103:653–6.
Reissman KR, Coleman TJ. Acute intestinal iron intoxication: II. Metabolic, respiratory, and circulatory effects of absorbed iron salts. Blood. 1955;10:46–51.
Pestaner JP, Ishak KG, Mullick FG, Centeno JA. Ferrous sulfate toxicity: a review of autopsy findings. Biol Trace Elem Res. 1999;69:191–8.
Robotham JL, Lietman PS. Acute iron poisoning: a review. Am J Dis Child. 1980;134:875–9.
Mills KC, Curry SC. Acute iron poisoning. Emerg Med Clin North Am. 1994;12:397–413.
Henretig FM, Karl SR, Weintraub WH. Severe iron poisoning treated with enteral and intravenous deferoxamine. Ann Emerg Med. 1983;12:306–9.
Knasel AL, Collins-Barrow MD. Applicability of early indicators of iron toxicity. J Natl Med Assoc. 1986;78:1037–40.
Ng RC, Perry K, Martin DJ. Iron poisoning: assessment of radiography in diagnosis and management. Clin Pediatr. 1979;18:614–6.
Staple TW, McAlister WH. Roentgenographic visualization of iron preparations in the gastrointestinal tract. Radiology. 1964;83:1051–6.
Everson GW, Oudjhane K, Young LW, Krenzelok EP. Effectiveness of abdominal radiographs in visualizing chewable iron supplements following overdose. Am J Emerg Med. 1989;7:459–63.
Linakis JG, Lacouture PG, Woolf A. Iron absorption from chewable vitamins with iron versus iron tablets: implications for toxicity. Pediatr Emerg Care. 1992;8:321–4.
Chyka PA, Bradyr AY. Assessment of acute iron poisoning by laboratory and clinical observations. Am J Emerg Med. 1993;11:99–103.
Bosse GM. Conservative management of patients with moderately elevated serum iron levels. J Toxicol Clin Toxicol. 1995;33:135–40.
Lacouture PG, Wason S, Temple AR, et al. Emergency assessment of severity in iron overdose by clinical and laboratory methods. J Pediatr. 1981;99:89–91.
Palatnick W, Tenenbein M. Leukocytosis, hyperglycemia, vomiting, and positive x-rays are not indicators of severity of iron overdose in adults. Am J Emerg Med. 1996;14:454–5.
Siff JE, Meldon SW, Tomassoni AJ. Usefulness of total iron binding capacity in the evaluation and treatment of acute iron overdose. Ann Emerg Med. 1999;33:73–6.
Tenenbein M, Yatscoff RW. The total iron-binding capacity in iron poisoning: is it useful? Am J Dis Child. 1991;145:437–9.
Tenenbein M. Inefficacy of gastric emptying procedures. J Emerg Med. 1985;3:133–6.
American Association of Clinical Toxicology, European Association of Poisons Centres and Clinical Toxicologists. Position statement: ipecac syrup. J Toxicol Clin Toxicol. 1997;35:699–709.
American Association of Clinical Toxicology, European Association of Poisons Centres and Clinical Toxicologists. Position statement: gastric lavage. J Toxicol Clin Toxicol. 1997;35:711–9.
Decker WJ, Combs HF, Corby DG. Adsorption of drugs and poisons by activated charcoal. Toxicol Appl Pharmacol. 1968;13:454–60.
Tenenbein M. Whole bowel irrigation in iron poisoning. J Pediatr. 1987;111:142–5.
American Association of Clinical Toxicology, European Association of Poisons Centres and Clinical Toxicologists. Position statement: whole bowel irrigation. J Toxicol Clin Toxicol. 1997;35:753–62
Kaczorowski JM, Wax PM. Five days of whole-bowel irrigation in a case of pediatric iron ingestion. Ann Emerg Med. 1996;27:258–63.
Peterson CD, Fifield GC. Emergency gastrotomy for acute iron poisoning. Ann Emerg Med. 1980;9:262–4.
Venturelli J, Kwee Y, Morris N, Cameron G. Gastrotomy in the management of acute iron poisoning. J Pediatr. 1982;100:768–9.
Foxford R, Goldfrank L. Gastrotomy – a surgical approach to iron overdose. Ann Emerg Med. 1985;14:1223–6.
Landsman I, Bricker JT, Reid BS, Bloss RS. Emergency gastrotomy: treatment of choice for iron bezoar. J Pediatr Surg. 1987;22:184–5.
Tenenbein M, Wiseman N, Yatscoff RW. Gastrotomy and whole bowel irrigation in iron poisoning. Pediatr Emerg Care. 1991;7:286–8.
Roberts RJ, Nayfield S, Soper R, Kent TH. Acute iron intoxication with intestinal infarction managed in part by small bowel resection. Clin Toxicol. 1975;8:3–12.
Czajka PA, Konrad JD, Duffy JP. Iron poisoning: an in vitro comparison of bicarbonate and phosphate lavage solutions. J Pediatr. 1981;98:491–4.
Dean BS, Krenzelok EP. In vivo effectiveness of oral complexation agents in the management of iron poisoning. Clin Toxicol. 1987;25:221–30.
Bachrach L, Correa A, Levin R, Grossman M. Iron poisoning: complications of hypertonic phosphate lavage therapy. J Pediatr. 1979;94:147–9.
Geffner ME, Opas LM. Phosphate poisoning complicating treatment for iron ingestion. Am J Dis Child. 1980;134:509–10.
Wallace KL, Curry SC, LoVecchio F, Raschke RA. Effect of magnesium hydroxide on iron absorption following simulated mild iron overdose in human subjects. Acad Emerg Med. 1998;5:961–5.
Corby DG, McCullen AH, Chadwick EW, Decker WJ. Effect of orally administered magnesium hydroxide in experimental iron intoxication. J Toxicol Clin Toxicol. 1985–1986;23:489–99.
Snyder BK, Clark RF. Effect of magnesium hydroxide administration on iron absorption after a supratherapeutic dose of ferrous sulfate in human volunteers: a randomized controlled trial. Ann Emerg Med. 1999;33:400–5.
Gomez HF, McClafferty HH, Flory D, et al. Prevention of gastrointestinal iron absorption by chelation from an orally administered premixed deferoxamine/charcoal slurry. Ann Emerg Med. 1997;30:587–92.
Whitten CF, Chen Y, Gibson GW. Studies in acute iron poisoning: II. Further observation on desferrioxamine in the treatment of acute experimental iron poisoning. Pediatrics. 1966;38:102–10.
Richardson JR, Sugerman DL, Hulet WH. Extraction of iron by chelation and desferrioxamine and hemodialysis. Clin Res. 1967;15:368.
Gumber MR, Kute VB, Shah PR, et al. Successful treatment of severe iron intoxication with gastrointestinal decontamination, deferoxamine, and hemodialysis. Ren Fail. 2013;35:729–31.
Frenandez S, Castro P, Nogue S, Nicolas JM. Acute iron intoxication: change in urine color during chelation therapy with deferoxamine. Intensive Care Med. 2014;40:104.
Sankar J, Shukla A, Khurana R, Dubey N. Near fatal iron intoxication managed conservatively. BMJ Case Rep. 2013. doi:10.1136/bcr-2012-007670.
Westlin WF. Deferoxamine in the treatment of acute iron poisoning: clinical experiences with 172 children. Clin Pediatr. 1966;5:531–5.
Leikin S, Vossough P, Mochis-Fatemi F. Chelation therapy in acute iron poisoning. J Pediatr. 1967;71:425–30.
Whitten CF, Gibson GW, Good MH, et al. Studies in acute iron poisoning: desferrioxamine in the treatment of iron poisoning: clinical observations, experimental studies and theoretical considerations. Pediatrics. 1965;36:322–5.
Berland Y, Carhon SA, Olmer M, Meunier PJ. Predictive value of desferrioxamine infusion test for bone aluminum deposit in hemodialyzed patients. Nephron. 1985;40:433–5.
Leikin JB, Paloucek FB, editors. Poisoning and toxicology handbook. 4th ed. Boca Raton: CRC Press; 2008.
Koren G, Bentur Y, Strong D, et al. Acute changes in renal function associated with deferoxamine therapy. Am J Dis Child. 1989;143:1077–80.
Tenenbein M, Kowalski S, Sienko A, et al. Pulmonary toxic effects of continuous desferrioxamine administration in acute iron poisoning. Lancet. 1992;339:699–701.
Anderson KJ, Rivers RPA. Desferrioxamine in acute iron poisoning. Lancet. 1992;339:1602.
Ioannides AS, Panisello JM. Acute respiratory distress syndrome in children with acute iron poisoning: the role of intravenous desferrioxamine. Eur J Pediatr. 2000;159:158–9.
Melby K, Skordahl S, Guttebert TJ, Nordbo SA. Septicaemia due to Yersinia enterocolitica after oral overdose of iron. BMJ. 1982;285:467–8.
Mofenson HC, Caraccio TR, Sharieff N. Iron sepsis: Yersinia enterocolitica septicemia possibly caused by an overdose of iron. N Engl J Med. 1987;316:1092–3.
Milteer RM, Sarpong S, Poydras U. Yersinia enterocolitica septicemia after accidental oral iron overdose. Pediatr Infect Dis J. 1989;8:537–8.
Tran T, Wax JR, Philput C, et al. Intentional iron overdose in pregnancy – management and outcome. J Emerg Med. 2000;18:225–8.
Rayburn WF, Donn SM, Wulf ME. Iron overdose during pregnancy: successful therapy with deferoxamine. Am J Obstet Gynecol. 1983;14:717–8.
Lacoste H, Goyert GL, Goldman LS, et al. Acute iron intoxication in pregnancy: case report and review of the literature. Obstet Gynecol. 1992;80:500–1.
McElhatton PR, Roberts JC, Sullivan FM. The consequences of iron overdose and its treatment with desferrioxamine in pregnancy. Hum Exp Toxicol. 1991;10:251–9.
Turk J, Aks S, Ampuero F, Hryhorczuk DO. Successful therapy of iron intoxication in pregnancy with intravenous deferoxamine and whole bowel irrigation. Vet Hum Toxicol. 1993;35:441–4.
Van Ameyde KJ, Tenebein M. Whole bowel irrigation during pregnancy. Am J Obstet Gynecol. 1989;160:646–7.
Olenmark M, Biber B, Dottori O, Rybo G. Fatal iron intoxication in late pregnancy. Clin Toxicol. 1987;25:347–59.
Thomas RM, Skalicka AE. Successful pregnancy in transfusion-dependent thalassaemia. Arch Dis Child. 1980;55:572–4.
Martin K. Successful pregnancy in β-thalassaemia major. Aust Paediatr J. 1983;19:182–3.
Rampton D, Folkerson J, Fishbane S, et al. Hypersensitivity reactions to intravenous iron: guidance for risk minimization and management. Haematologica. 2014;19:1671–6.
Bishu K, Agarwal R. Acute Injury with intravenous iron and concerns regarding long-term safety. Clin J Am Soc Nephrol. 2006;1:S19–23.
Szebeni J, Fishbane S, Hedenus M, et al. Hypersensitivity to intravenous iron: classification, terminology, mechanisms, and management. Br J Pharmacol. 2015;172:5025–36.
Author information
Authors and Affiliations
Corresponding authors
Editor information
Editors and Affiliations
Grading System for Levels of Evidence Supporting Recommendations in Critical Care Toxicology, 2nd Edition
-
I
Evidence obtained from at least one properly randomized controlled trial.
-
II-1
Evidence obtained from well-designed controlled trials without randomization.
-
II-2
Evidence obtained from well-designed cohort or case-control analytic studies, preferably from more than one center or research group.
-
II-3
Evidence obtained from multiple time series with or without the intervention. Dramatic results in uncontrolled experiments (such as the results of the introduction of penicillin treatment in the 1940s) could also be regarded as this type of evidence.
-
III
Opinions of respected authorities, based on clinical experience, descriptive studies and case reports, or reports of expert committees.
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this entry
Cite this entry
Bryant, S.M., Leikin, J.B. (2017). Iron. In: Brent, J., et al. Critical Care Toxicology. Springer, Cham. https://doi.org/10.1007/978-3-319-17900-1_26
Download citation
DOI: https://doi.org/10.1007/978-3-319-17900-1_26
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-17899-8
Online ISBN: 978-3-319-17900-1
eBook Packages: Biomedical and Life SciencesReference Module Biomedical and Life Sciences