Abstract
Octreotide (Sandostatin) is a synthetic analogue of somatostatin that has similar, if not identical, pharmacologic activity to this endogenous hormone but is longer acting and more potent [1–11]. Somatostatin was first isolated from the hypothalamus and characterized as an inhibitor of pituitary growth hormone secretion in 1973 [12]. It is synthesized and widely distributed throughout the body (particularly in neurons, pancreas, and gastrointestinal tract but also in immune and inflammatory cells), modulates neurotransmission (primarily in the central nervous system), and has generalized inhibitory effects on paracrine function. With respect to the last-mentioned, somatostatin inhibits the release of the following:
This is an update of the chapter written by Christopher H. Linden for the first edition of this text.
Access provided by CONRICYT-eBooks. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Octreotide
- Somatostatin
- Lanreotide
- Pasireitude
- Pancreatic alpha cells
- Sulfonylurea drugs
- Pancreatic islet beta cells
- Somatostatin membrane receptors
- Sulfonylurea poisoning
- Glucagon
Octreotide (Sandostatin) is a synthetic analogue of somatostatin that has similar, if not identical, pharmacologic activity to this endogenous hormone but is longer acting and more potent [1–11]. Somatostatin was first isolated from the hypothalamus and characterized as an inhibitor of pituitary growth hormone secretion in 1973 [12]. It is synthesized and widely distributed throughout the body (particularly in neurons, pancreas, and gastrointestinal tract but also in immune and inflammatory cells), modulates neurotransmission (primarily in the central nervous system), and has generalized inhibitory effects on paracrine function. With respect to the last-mentioned, somatostatin inhibits the release of the following:
-
Thyrotropin
-
Prolactin
-
Gastrin
-
Motilin
-
Vasoactive intestinal peptide
-
Pancreatic polypeptide
-
Glicentin
-
Glucagon
-
Insulin
-
Insulin-like growth factors (somatomedins)
-
Parathyroid hormone
-
Luteinizing hormone
-
Calcitonin
-
Renin
-
Adrenocorticotropic hormone
-
Growth hormone
Somatostatin is involved in the regulation of many physiologic processes and also inhibits exocrine secretions from the pancreas, gut, gallbladder, and salivary glands. It consists of two main peptides, SST-14 and SST-28, which bind to and activate five related G-protein coupled receptors [1–5]. Octreotide , lanreotide, and pasireotide are the only three somatostatin analogs currently in widespread clinical use and approved for use in the USA. Octreotide and lanerotide are cyclic octapeptides, while pasireotide is a cyclohexapeptide. They display the greatest affinity for somatostatin type 2 and type 5 receptors found in the pituitary gland and the pancreas [6–12].
Indications for the use of octreotide currently approved by the US Food and Drug Administration are limited to the treatment of acromegaly, carcinoid tumors, and vasoactive intestinal peptide tumors [11]. Clinical experience also supports its use in the treatment of nonsecretory, corticotropin-secreting, and thyrotropin-secreting pituitary adenomas; pancreatic islet cell tumors; congenital and acquired hyperinsulinism; nesidioblastosis; acute pancreatitis; pancreatic fistulas and pseudocysts; bleeding from esophageal varices and peptic ulcers; and diarrhea associated with ileostomies, short bowel syndrome, intestinal graft-versus-host disease, radiation colitis, intestinal fistulas, and acquired immunodeficiency syndrome [6–10, 13, 14]. Its effects on other endocrine disorders, nonendocrine tumors, hematologic function, immunologic function, neurologic function, vascular disease, and a host of other processes, including aging, are under investigation. Lanreotide is a longer-acting depot preparation used for acromegaly and gastroenteropancreatic neuroendocrine tumors. Pasireotide is used to treat acromegaly and Cushing’s syndrome.
The ability of octreotide to inhibit the secretion of insulin, glucagon , and other insulin counterregulatory hormones makes it a rational choice for the treatment of poisoning due to sulfonylureas and other drugs causing hyperinsulinemia (see Chap. 70, “Antidiabetic Agents”). With proven efficacy, low cost, ease of administration, and a highly favorable safety profile, it has virtually all the properties characterizing an ideal antidote. Although much more is known about the pharmacology of octreotide (and somatostatin), the remainder of this chapter focuses only on the actions relevant to the understanding and treatment of drug-induced hyperinsulinemic hypoglycemia.
Pharmacodynamics
Physiologically, somatostatin acts as a gastrointestinal and pancreatic counter-regulatory hormone [1, 3, 15]. It is secreted from pancreatic islets of Langerhans delta cells in response to increases in blood glucose, amino acids, fatty acids, and gastrointestinal hormones that occur after the ingestion of food. Systemic effects include decreased gastrointestinal and gallbladder motility and secretory activity with consequent slowing of the digestion and absorption of food. Locally, somatostatin inhibits the pancreatic secretion of insulin from islet beta cells and of glucagon from islet alpha and intestinal alpha-like or L cells, decreasing the uptake and use of absorbed nutrients. Although pancreatic alpha cells are about 50 times more sensitive to somatostatin than beta cells, their effect on insulin secretion is more prolonged than that on glucagon secretion. Teleologically, by preventing the rapid assimilation and consequent exhaustion of ingested food, somatostatin lessens inequalities between the intermittent supply and continuous demand for nutrients, increasing the overall efficiency of food processing.
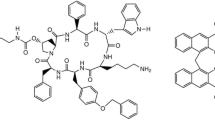
Sulfonylurea drugs counteract hyperglycemia by enhancing the release of insulin from pancreatic islet beta cells in response to glucose, the principal stimulus and an essential permissive factor for insulin secretion [3, 16, 17]. Their mechanism of action is similar to that of high plasma glucose concentrations: inhibition of the pancreatic islet beta cell membrane adenosine triphosphate (ATP)–sensitive potassium (K+) channels leading to membrane depolarization with consequent calcium (Ca2+) influx through voltage-sensitive Ca2+ channels, mobilization of Ca2+ from the endoplasmic reticulum, increased intracellular Ca2+, and insulin secretion. Sulfonylureas bind to specific receptors associated with K+ channels on the beta cell membrane, whereas glucose generates ATP through its oxidative metabolism within beta cells. Intracellular Ca2+ is the ultimate insulin secretagogue, with increases in intracellular calcium promoting the synthesis and release of insulin (Fig. 1).
Schematic diagram of a pancreatic beta cell showing the regulation of insulin secretion. Glucose is transported into the beta cell by a glucose-transporter protein (GLUT-2). The enzyme glucokinase (GK) initiates glycolysis by catalyzing the transfer of phosphate from adenosine triphosphate (ATP) to glucose, resulting in the formation of glucose-6-phosphate (G-6-P). ATP generated by subsequent steps in the glycolytic pathway and by the Krebs (citric or tricarboxylic acid) cycle leads to closure of ATP-sensitive potassium channels (K+ ATP) and membrane depolarization. Membrane depolarization results in opening of voltage-dependent calcium channels (Ca+ VD), influx of extracellular calcium, and subsequent release of calcium from intracellular (endoplasmic reticulum) stores. Increased intracellular calcium promotes the exocytosis of insulin granules (Golgi vesicles) with release of insulin into extracellular fluid and the systemic circulation. Although the phosphorylation of glucose is a rate-limiting step, beta cell GK has a high Michaelis constant (KM, the substrate concentration at which the reaction rate is half of the maximal value) for glucose. Glucose metabolism and ATP production, potassium and calcium channel activity, intracellular calcium concentration, and insulin release are controlled primarily by the intracellular glucose concentration. Sulfonylureas (SU) inhibit potassium efflux by binding to specific receptors (SUR) associated with K+ ATP channels and enhance the release of insulin. Somatostatin (SST) and its analogues, such as octreotide, inhibit calcium influx by binding to receptors (SSTR) associated with Ca+ VD channels, inhibiting the release of insulin
The action of octreotide (and of somatostatin and other analogues) on beta cell Ca2+ disposition is diametrically opposite to that of the sulfonylureas, and the mechanism is slightly different [3, 18, 19]. Octreotide binds to specific somatostatin membrane receptors (SST receptors or SSTRs) associated with Ca2+ channels, resulting in decreased calcium conductance, decreased intracellular Ca2+, and inhibition of insulin secretion. Opening of potassium channels with subsequent membrane hyperpolarization also may be involved. Somatostatin receptors are coupled to G proteins. To date, five SSTR subtypes have been identified. Receptor affinity and selectivity differ from one somatostatin analogue to another. Subtypes 2 and 5 mediate insulin secretion. Octreotide’s action does not seem to be mediated by increased potassium efflux through K+ channels [20]. Suppression of insulin secretion by octreotide has been documented in experimental [21–24] and, human sulfonylurea poisoning [25, 26] (see Fig. 1).
The antidotal effects of octreotide in sulfonylurea poisoning also may be due to its antagonism of glucagon and possibly other counterregulatory hormones. Octreotide not only inhibits the secretion of glucagon in response to hypoglycemia but also inhibits the actions of glucagon [1, 3]. Glucagon activates adenylyl cyclase, which catalyzes the synthesis of cyclic adenosine monophosphate (AMP), whereas octreotide inhibits this enzyme. In the absence of octreotide, this action of glucagon increases cyclic AMP levels, and this stimulates glycogen phosphorylase (the rate-limiting enzyme in glycogenolysis), inhibits glycogen synthase, and increases intracellular Ca2+, effects that may lead to hyperglycemia, rebound hyperinsulinemia, and recurrent hypoglycemia after glucose administration (see Fig. 1 and see Chap. 70, “Antidiabetic Agents”). As with insulin, SSTR subtypes 2 and 5 mediate glucagon secretion [18, 19]. Octreotide has been shown to decrease epinephrine, norepinephrine, and glucagon levels in experimental models of glipizide overdose [21].
Octreotide also is likely to be effective in treating hyperinsulinemic hypoglycemia due to other drugs, including insulin itself (see Chap. 70, “Antidiabetic Agents”). One report described improvement in glucose concentrations after octreotide was administered to a 56-year-old male who overdosed on insulin glargine [27]. The meglitinides (repaglinide and nateglinide) act similarly to sulfonylureas to increase insulin secretion by blocking ATP-dependent potassium channels. This leads to depolarization of the membrane and facilitates calcium entry through calcium channels, thereby stimulating insulin release from the pancreatic beta cells. At least one report described successful treatment of repaglinide-induced hypoglycemia with octreotide [28]. Its use has also been reported in a case of quinine-induced hypoglcyemia [29]. Octreotide is relatively inexpensive, costing less than $10 US for a 100-μg dose.
Pharmacokinetics
Octreotide is well-absorbed after subcutaneous administration, with peak plasma concentrations averaging 5.2 ng/mL 0.4 h after a 100-μg dose in healthy volunteers [11]. It is about 65% bound to plasma lipoproteins, has a small volume of distribution (approximately 0.2 L/kg), and a half-life of about 1.7 h, which is much longer than that of somatostatin (1–3 min). About one third of the dose is excreted unchanged in the urine, and the half-life is doubled in renal dialysis patients and the elderly. The metabolic fate of the remaining fraction has not been determined.
Octreotide is also absorbed after oral administration, though bioavailability is low. A 2-mg oral dose results in peak plasma drug levels similar to a 50-μg subcutaneous dose, with the time to peak level delayed about 1.5 h.
Contraindications and Adverse Effects
Except for hypersensitivity, there are no contraindications to octreotide use [1, 3, 5–11]. Overall, octreotide is well tolerated. As with most subcutaneously administered medications, burning pain at the injection site can occur. In the three largest studies and case series evaluating octreotide for sulfonylurea poisoning in adults, no adverse effects were reported among almost 40 patients [30–32]. Similarly, a larger retrospective study in pediatric patients reported no adverse effects in 121 patients [33]. There are a few scattered reports of adverse effects temporally related to octreotide administration for sulfonylurea poisoning, but a cause-and-effect association is unclear. A pediatric patient developed hypertension and apnea 30 min after administration of octreotide; the dose was not reported [34]. Hyperkalemia and worsening heart failure have each been reported once, both in adult patients [35, 36]. When used for congenital diseases such as acromegaly and hyperinsulinism, octreotide has been associated with cases of drug-induced hepatitis [37–40]. However, there may have been other contributing factors and the hepatitis occurred after prolonged use in each case. Hepatitis has not been reported with the short-term therapeutic use of octreotide for sulfonylurea overdose.
Octreotide has been used in all age groups, including neonates and pregnant women. Although no adverse effects on fertility or fetal development have been noted in experimental animals, because octreotide has not been studied extensively in pregnant women, it has a Food and Drug Administration category B use-in-pregnancy rating (no evidence of risk in humans; the chance of fetal harm is remote but remains a possibility).
Treatment
There have been numerous case reports, case series, retrospective studies, and even randomized controlled trials examining octreotide for sulfonylurea poisoning . Both pediatric and adult populations have been studied. One of the earliest studies demonstrated that a continuous octreotide infusion (30 ng/kg/min or 126 μg/h for a 70-kg person) was effective in lessening the severity of hypoglycemia in nondiabetic human volunteers (n = 8) who ingested a large dose of glipizide (1.45 mg/kg) [21]. This therapy reduced the need for exogenous glucose in all subjects and entirely eliminated it in half. It was also found that without octreotide, some patients experienced recurrent hypoglycemia up to 30 h following glipizide ingestion.
Pediatric Patients
There are at least 10 published reports of octreotide use in pediatric patients [33, 34, 43–50]. Fifteen children are discussed in nine small studies [34, 43–50]. Ages ranged from 1 to 17 years with most under age 6 years. Fourteen of the 15 children ingested second-generation sulfonylureas (eight glipizide and six glyburide or glibenclamide); the drug was not reported in the remaining case. Octreotide was generally administered after intravenous (IV) 10–50% dextrose boluses and infusions failed to correct hypoglycemia or maintain euglycemia. The dose range of octreotide was 0.51–2.5 μg/kg IV or SC; most patients received octreotide 1–1.5 μg/kg IV. Octreotide resulted in correction of the serum glucose concentration in all 15 patients and recurrent hypoglycemia was observed in eight. Seven patients received additional octreotide doses as IV boluses or infusion. Time to recurrent hypoglycemia after octreotide administration ranged from 6 to 17 h.
One group retrospectively examined 9 years of the American Association of Poison Control Centers’ National Poison Data System to evaluate octreotide as an antidote for sulfonylurea overdose in children younger than 6 years of age [33]. One hundred twenty one cases were identified in which a child ingested a sulfonylurea and experienced at least one episode of hypoglycemia (median age 22 months). Prior to octreotide administration, the median glucose concentration was 44 mg/dL (range 2–62 mg/dL). Glipizide was the most frequently ingested sulfonylurea accounting for 70% of cases. Though octreotide doses were not recorded, the number of hypoglycemic episodes before octreotide (median, 2) was significantly higher than after octreotide (median, 0; P < 0.0001). After octreotide, 99 of 121 had no further hypoglycemic episodes. Twenty-two children experienced a hypoglycemic episode after the first dose of octreotide, occurring at a median time of 5 h (range, 1–25 h) after administration. Further details about these cases were not reported.
Adult Patients
At least 16 published reports describe octreotide use for sulfonylurea poisoning in adults [25, 30–32, 35, 36, 41, 42, 51–58]. Thirteen case reports (16 patients) described exposures to first and second generation sulfonylureas, with 10 identified as glyburide/glibenclamide or glipizide [25, 35, 36, 41, 42, 51–58]. The most common dose of octreotide was 50 μg subcutaneously, followed by 50 μg subcutaneously every 6–12 h for 2–3 doses. A 100 μg subcutaneous dose was also used in a few cases, followed by 50–100 μg subsequent doses. Two patients were treated with octreotide by continuous IV infusion (30 ng/kg/min for 13 h, and 50 μg/h). Five patients developed recurrent hypoglycemia 2–9 h after octreotide was administered. Six patients had serum insulin or C-peptide levels measured during hypoglycemia; all were elevated. Three of the six had repeat levels drawn after octreotide administration; all had decreased.
Six adult patients were reported in a case series, all of which experienced hypoglycemia after therapeutic doses of sulfonylureas (4 glimepiride, 1 glyburide, and 1 glipizide) [32]. Intermittent IV administration of 50% dextrose did not result in a sustained and adequate blood glucose response. The patients were treated with octreotide 50 μg subcutaneously every 8 h, receiving 2–4 doses. Half experienced recurrent hypoglycemia after initial octreotide administration. Three patients had serum insulin and C-peptide levels measured during hypoglycemia; all were elevated and decreased after octreotide. Nine adult patients were retrospectively reviewed after ingestion of a sulfonylurea (6 glyburide and 3 glipizide) [30]. The initial octreotide dose was 40–100 μg subcutaneously, followed by 40–100 μg subcutaneously every 6–12 h, 2–3 doses in six patients and 125 μg/h IV for 9 h in one patient. There were 3.2 hypoglycemic events per patient recorded before octreotide compared to 0.2 per patient after octreotide (p = 0.008). There were 72.5 g of 50% dextrose administered before octreotide compared to 5 g after octreotide (p = 0.004). Two patients had recurrent hypoglycemia, one 14 h after octreotide and the other 36 h after octreotide. In the first patient, hypoglycemia occurred more than 30 h after the ingestion of glyburide. The second patient experienced recurrent hypoglycemia 40 h after ingestion of extended-release glipizide. Both were beyond the duration of effect of octreotide.
One randomized, double-blind, placebo controlled trial exists evaluating the efficacy of octreotide in sulfonylurea poisoning [31]. In addition to standard dextrose therapy, 22 patients received octreotide 75 μg subcutaneously after sulfonylurea-induced hypoglycemia. Eighteen patients served as controls and received placebo in addition to standard dextrose therapy. The mean glucose values for octreotide patients compared with placebo were consistently higher during the first 8 h but showed no difference in subsequent hours. The mean glucose difference in the octreotide group versus placebo was 56 mg/dL in hours 1–3 after administration and 127 mg/dL in hours 408. Ten octreotide-treated patients experienced recurrent hypoglycemia compared with six patients in the control group. Only one dose of octreotide was administered. All patients were admitted to the hospital and monitored for recurrent hypoglycemia for at least 24 h.
Indications for octreotide treatment are not well defined. Although it is generally agreed that octreotide is indicated for recurrent hypoglycemia due to sulfonylurea poisoning, whether it should be given after the first episode of hypoglycemia is unclear. Doing so is reasonable in patients who are likely to develop further episodes (e.g., patients with large or intentional overdoses or children with an unsupervised ingestion of an unknown amount), but it may prolong unnecessarily the period of observation for patients who are not (e.g., patients with therapeutic misadventures). As always, the reliability of the history must be assessed when making such decisions. Given that the overdose history is often inaccurate, incomplete, or unobtainable, we prefer to reserve treatment for patients with a documented second episode of hypoglycemia (Grade III recommendation). Treatment recommendations for these patients are discussed in detail in Chap. 70, “Antidiabetic Agents.”
Administration
Based on clinical experience and the available data, a subcutaneous dose of 1–2 μg/kg (50–100 μg in adults) every 6–8 h can be expected to be effective for the treatment of sulfonylurea-induced hypoglycemia (Grade II-2 recommendation). A continuous IV infusion of the same dose on an hourly basis also is likely to be effective. IV administration is more expensive and more difficult to prepare and administer (and more susceptible to dosing errors). Because there is no evidence that this route and method of dosing are superior or necessary, we recommend intermittent subcutaneous dosing as the preferred treatment regimen. For adult patients, we recommend 100 μg subcutaneously every 6 h (GRADE I recommendation). For pediatric patients, we recommend 1.5 μg/kg subcutaneously every 6 h (Level of Evidence II-3) (Table 1).
Octreotide is administered parenterally for the treatment of hyperinsulinemic hypoglycemia due to drug overdose. Solutions containing 50 μg/mL, 100 μg/mL, 200 μg/mL, 500 μg/mL, or 1000 μg/mL are available for subcutaneous injection or intravenous infusion. Long-acting, sustained-release preparations containing 10 mg/2 mL, 20 mg/2 mL, or 30 mg/2 mL for intramuscular (intragluteal) injection at monthly intervals (e.g., Sandostatin LAR Depot) are used for the treatment of chronic conditions. No oral formulations of octreotide are commercially available. Similar doses to the above are likely effective for the treatment of other drug-induced states of hyperinsulinism (see Chap. 70, “Antidiabetic Agents”), but there is little experience with its use in this setting.
References
Reichlin S. Somatostatin. N Engl J Med. 1983;309:1495–501, 1556–63.
Parker KL, Schimmer BP. Chapter 38. Introduction to endocrinology: the hypothalamic-pituitary axis. In: Brunton LL, Chabner BA, Knollmann BC, editors. Goodman & Gilman’s the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill; 2011.
Powers AC, D’Alessio D. Chapter 43. Endocrine pancreas and pharmacotherapy of diabetes mellitus and hypoglycemia. In: Brunton LL, Chabner BA, Knollmann BC, editors. Goodman & Gilman’s the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill; 2011.
Underwood LE. Growth hormone and insulin-like growth factors. In: Munson PL, Mueller RA, Breese GR, editors. Principles of pharmacology: basic concepts and clinical applications. New York: Chapman & Hall; 1996. p. 904.
McEvoy GK, editor in chief. American hospital formulary service drug information. Bethesda: American Society of Health-System Pharmacists; 2015.
Rosenberg JM. Octreotide: a synthetic analog of somatostatin. Drug Intell Clin Pharm. 1988;22:748–54.
Battershill PE, Clissold SP. Octreotide: a review of its pharmacodynamic and pharmacokinetic properties, and therapeutic potential in conditions associated with excessive peptide secretion. Drugs. 1989;38:658–702.
Chanson P, Timsit J, Harris AG. Clinical pharmacokinetics of octreotide: therapeutic applications in patients with pituitary tumours. Clin Pharmacokinet. 1993;25:375–91.
Proceedings: Sandostatin, “State of the Art”. Metabolism. 1992;41 Suppl 2:1–122.
Lamberts SWJ, van der Lely AJ, de Herder WW, et al. Octreotide. N Engl J Med. 1996;334:246–53.
Sandostatin® prescribing information (package insert). East Hanover: Novartis Pharmaceuticals Corporation, Novartis Pharma Stein AG; 2012.
Brazeau P, Vale WW, Burgess R, et al. Hypothalamic polypeptide that inhibits the secretion of immunoreactive pituitary growth hormone. Science. 1973;179:77–9.
Barrons RW. Octreotide in hyperinsulinism. Ann Pharmacother. 1997;31:239–41.
Stanley CA. Hyperinsulinism in infants and children. Pediatr Clin North Am. 1997;44:363–74.
Guyton AC, Hall JE. Textbook of medical physiology. 10th ed. Philadelphia: WB Saunders; 2000. p. 893.
Gerich JE. Oral hypoglycemic agents. N Engl J Med. 1989;321:1231–45.
Panten U, Schwantecher M, Schwantecher C. Pancreatic and extrapancreatic sulfonylurea receptors. Horm Metab Res. 1992;24:549–54.
Patel YC, Srikant CB. Subtype selectivity of peptide analogs for all five cloned human somatostatin receptors (hsstr 1–5). Endocrinology. 1994;135:2814–7.
Benali N, Ferjoux G, Puente E, et al. Somatostatin receptors. Digestion. 2000;62 Suppl 1:27–32.
Doyle ME, Egan JM. Pharmacological agents that directly modulate insulin secretion. Pharmacol Rev. 2003;55:105–31.
Boyle PJ, Justice K, Krentz AJ, et al. Octreotide reverses hyperinsulinemia and prevents hypoglycemia induced by sulfonylurea overdoses. J Clin Endocrinol Metab. 1993;76:752–6.
Bauer W, Briner U, Doepfner W, et al. SMS 201–995: a very potent and selective octapeptide analogue of somatostatin with prolonged action. Life Sci. 1982;31:1133–40.
Overkamp D, Volk A, Maerker E, et al. Acute effect of glimepiride on insulin-stimulated glucose metabolism in glucose-tolerant insulin-resistant offspring of patients with type 2 diabetes. Diabetes Care. 2002;25:2065–73.
Lee PE, Meneilly GS. The effect of octreotide on glucose and insulin levels in a patient with type 2 diabetes on glibenclamide. Diabetes Metab. 1999;25:347–9.
Graudins A, Linden CH, Ferm RP. Diagnosis and treatment of sulfonylurea-induced hyperinsulinemic hypoglycemia. Am J Emerg Med. 1997;15:95–6.
Mordel A, Sivilotti MLA, Old AC, Ferm RP. Octreotide for pediatric sulfonylurea poisoning. Clin Toxicol. 1998;36:437.
Groth CM, Banzon ER. Octreotide for the treatment of hypoglycemia after insulin glargine overdose. J Emerg Med. 2013;45(2):194–8.
Fasano CJ, Rowden AK. Successful treatment of repaglinide-induced hypoglycemia with octreotide. Am J Emerg Med. 2009;27(6):e3–4.
Phillips RE, Looaresuwan S, Bloom SR, et al. Effectiveness of SMS 201–995, a synthetic, long-acting somatostatin analogue, in treatment of quinine-induced hyperinsulinemia. Lancet. 1986;1:713–6.
McLaughlin SA, Crandall CS, McKinney PE. Octreotide: an antidote for sulfonylurea-induced hypoglycemia. Ann Emerg Med. 2000;36:133–8.
Fasano CJ, O’ Malley G, Dominici P, et al. Comparison of octreotide and standard therapy versus standard therapy alone for the treatment of sulfonylurea-induced hypoglycemia. Ann Emerg Med. 2008;51:400–6.
Fleseriu M, Skugor M, Chinnappa P, et al. Successful treatment of sulfonylurea-induced prolonged hypoglycemia with use of octreotide. Endocr Pract. 2006;12:635–40.
Dougherty PP, Lee SC, Lung D, et al. Evaluation of the use and safety of octreotide as antidotal therapy for sulfonylurea overdose in children. Pediatr Emerg Care. 2013;29:292–5.
Calello DP, Osterhoudt KC, Henretig FM, et al. Octreotide for pediatric sulfonylurea overdose: review of 5 cases. Clin Toxicol. 2005;43:671 (abstract).
Adabala M, Jhaveri KD, Gitman M. Severe hyperkalaemia resulting from octreotide use in a haemodialysis patient. Nephrol Dial Transplant. 2010;25:3439–42.
Vallurupalli S. Safety of subcutaneous octreotide in patients with sulfonylurea-induced hypoglycemia and congestive heart failure. Ann Pharmacother. 2010;44:387–90.
Koren I, Riskin A, Barthlen W, et al. Hepatitis in an infant treated with octreotide for congenital hyperinsulinism. J Pediatr Endocrinol Metab. 2013;26:183–5.
Ben-Ari J, Greenberg M, Nemet D, et al. Octreotide-induced hepatitis in a child with persistent hyperinsulinemia hypoglycemia of infancy. J Pediatr Endocrinol Metab. 2013;26:179–82.
Avatapalle B, Padidela R, Randell T, et al. Drug-induced hepatitis following use of octreotide for long-term treatment of congenital hyperinsulinism. BMJ Case Rep. 2012. https://www.ncbi.nlm.nih.gov/pubmed/22850563
Feenstra J, van Aken MO, de Herder WW, et al. Drug-induced hepatitis in an acromegalic patient during combined treatment with pegvisomant and octreotide long-acting repeatable attributed to the use of pegvisomant. Eur J Endocrinol. 2006;154:805–6.
Bui L, Adler D, Keller KH. Prolonged octreotide infusion to treat glyburide-induced hypoglycemia. Clin Toxicol. 2000;38:576 (abstract).
Hung O, Eng J, Ho J, et al. Octreotide as an antidote for refractory sulfonylurea hypoglycemia. Clin Toxicol. 1997;35:540 (abstract).
Glatstein M, Garcia-Bournissen F, Scolnik D, et al. Sulfonylurea intoxication at a tertiary care paediatric hospital. Can J Clin Pharmacol. 2010;17:e51–6.
Rath S, Naor B-Z, Anderson K, Fahy R, Robeby R. Octreotide in children with hypoglycemia due to sulfonylurea ingestion. J Paediatr Child Health. 2008;44:383–4.
Kent DA, Main BA, Friesen MS. Use of octreotide in sulfonylurea poisoning in a child. J Toxicol Clin Toxicol. 2003;41:669 (abstract).
Mordel A, Sivilotti MLA, Old AC, et al. Octreotide for pediatric sulphonylurea poisoning. J Toxicol Clin Toxicol. 1998;36:437 (abstract).
Pelavin PI, Abramson E, Pon S, et al. Extended-release glipizide overdose presenting with delayed hypoglycemia and treated with subcutaneous octreotide. J Pediatr Endocrinol Metab. 2009;22:171–5.
Calello DP, Kelly A, Osterhoudt KC. Case files of the Medical Toxicology Fellowship Training Program at the Children’s Hospital of Philadelphia: a pediatric exploratory sulfonylurea ingestion. J Med Toxicol. 2006;2:19–24.
Soderstrom J, Murray L, Daly FFS, et al. Toxicology case of the month: oral hypoglycaemic overdose. Emerg Med J. 2006;23:565–7.
Llamdo R, Czaja A, Stence N, et al. Continuous octreotide infusion for sulfonylurea-induced hypoglycemia in a toddler. J Emerg Med. 2013;45(6):e209–13.
Green RS, Palatnick W. Effectiveness of octreotide in a case of refractory sulfonylurea-induced hypoglycemia. J Emerg Med. 2003;25(3):283–7.
Braatvedt GD. Octreotide for the treatment of sulphonylurea induced hypoglycaemia in type 2 diabetes. N Z Med J. 1997;110:189–90.
Carr R, Zed PJ. Octreotide for sulfonylurea-induced hypoglycemia following overdose. Ann Pharmacother. 2002;36:1727–32.
Crawford BAL, Perera C. Octreotide treatment for sulfonylurea-induced hypoglycemia. Med J Aust. 2004;180(10):540–1.
Krentz AJ, Boyle PJ, Justice KM, et al. Successful treatment of severe refractory sulfonylurea-induced hypoglycemia with octreotide. Diabetes Care. 1993;16:184–6.
Nzerue CM, Thomas J, Volcy J, Edeki T. Use of octreotide to treat prolonged sulfonylurea-induced hypoglycemia in a patient with chronic renal failure. Int J Artif Organs. 2003;26(1):86–9.
Gonzalez RR, Zweig S, Rao J, et al. Octreotide therapy for recurrent refractory hypoglycemia due to sulfonylurea in diabetes-related kidney failure. Endocr Pract. 2007;13:417–23.
Hanchard B, Boulouffe C, Vanpee D. Sulfonylurea-induced hypoglycaemia: use of octreotide. Acta Clin Belg. 2009;64:56–8.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Grading System for Levels of Evidence Supporting Recommendations in Critical Care Toxicology, 2nd Edition
-
I
Evidence obtained from at least one properly randomized controlled trial.
-
II-1
Evidence obtained from well-designed controlled trials without randomization.
-
II-2
Evidence obtained from well-designed cohort or case-control analytic studies, preferably from more than one center or research group.
-
II-3
Evidence obtained from multiple time series with or without the intervention. Dramatic results in uncontrolled experiments (such as the results of the introduction of penicillin treatment in the 1940s) could also be regarded as this type of evidence.
-
III
Opinions of respected authorities, based on clinical experience, descriptive studies and case reports, or reports of expert committees.
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this entry
Cite this entry
Hayes, B.D. (2017). Octreotide. In: Brent, J., et al. Critical Care Toxicology. Springer, Cham. https://doi.org/10.1007/978-3-319-17900-1_164
Download citation
DOI: https://doi.org/10.1007/978-3-319-17900-1_164
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-17899-8
Online ISBN: 978-3-319-17900-1
eBook Packages: Biomedical and Life SciencesReference Module Biomedical and Life Sciences