Abstract
Wide-field imaging is important in the field of ocular oncology. This technology allows a panretinal image that includes tumor margins and relationships to surrounding structures with imaging of associated features and, most importantly, allows for accurate planning of tumor therapy. Several tumors in the eye arise from the retina, retinal pigment epithelium (RPE), choroid, and optic disc. Some of these tumors are benign and others are malignant. Wide-field imaging, in conjunction with other diagnostic testing, has improved our understanding of ocular tumors and provided better documentation of tumor appearance and effects. In this chapter, we provide images of intraocular tumors with various wide-field cameras.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Eye
- Tumor
- Iris
- Choroid
- Retina
- Retinal pigment epithelium
- Nevus
- Melanoma
- Metastasis
- Hemangioma
- Retinoblastoma
- Astrocytic hamartoma
- Congenital hypertrophy
Wide-field imaging is important in the field of ocular oncology. This technology allows a panretinal image that includes tumor margins and relationships to surrounding structures with imaging of associated features and, most importantly, allows for accurate planning of tumor therapy. Several tumors in the eye arise from the retina, retinal pigment epithelium (RPE), choroid, and optic disc. Some of these tumors are benign and others are malignant. Wide-field imaging, in conjunction with other diagnostic testing, has improved our understanding of ocular tumors and provided better documentation of tumor appearance and effects. In this chapter, we provide images of intraocular tumors with various wide-field cameras.
Tumors of the Retina
The neurosensory retina is composed of neural, glial, and vascular tissue, each of which can produce specific retinal tumors. Most retinal tumors are congenital or develop in childhood. Some are benign; others are malignant. These tumors include retinoblastoma, retinal astrocytic hamartoma, retinal vascular tumors (hemangioblastoma, cavernous hemangioma, racemose hemangioma, and vasoproliferative tumor), and lymphoid/leukemic infiltrations.
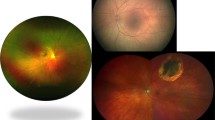
Retinoblastoma
Retinoblastoma is a highly malignant intraocular tumor of childhood [1–4]. Retinoblastoma accounts for approximately 11 % of cancers in children during the first year of life, and most cases are detected before 5 years old. Worldwide, it is estimated that there are approximately 7,000–8,000 new cases per year. The diagnosis of retinoblastoma is established by recognition of classic clinical and imaging features without the need for biopsy. Retinoblastoma can appear endophytic with tumor invasion into the vitreous or exophytic with tumor invasion under the retina. Management of retinoblastoma includes methods of chemotherapy, radiotherapy, laser photocoagulation, thermotherapy, cryotherapy, and enucleation (Figs. 1, 2 and 3).
Retinal Astrocytic Hamartoma
Retinal astrocytic hamartoma is a benign and classically stable retinal tumor found in patients with tuberous sclerosis complex or as a sporadic condition [5]. This retinal lesion is classified into three morphological groups: types 1, 2, and 3. Type 1 occurs in about 50 % of cases and is characterized by a circular or oval flat semitransparent solitary lesion in the retinal nerve fiber layer with an average size of 0.5 disc diameter [5]. Type 2 shows multiple calcified nodular areas of variable size with a mulberry-like appearance. Type 3 shows features of both type 1 and type 2 with a whitish-gray glistening central calcification and a peripheral semitranslucent, irregular rim. Occasionally, depigmented RPE “punched-out” lesions can be seen with this tumor as part of tuberous sclerosis complex (Fig. 4) [6].
Retinal Hemangioblastoma
Retinal hemangioblastoma is a vascular hamartoma with a circumscribed orange-colored mass with dilated feeding vessels, often producing subretinal fluid and exudation (Fig. 5). This tumor can be a feature of von Hippel–Lindau syndrome [7]. Management includes laser photocoagulation, photodynamic therapy, cryotherapy, plaque radiotherapy, external beam radiotherapy, surgical resection, or anti–vascular endothelial growth factor (anti-VEGF) medications.
Retinal Cavernous Hemangioma
Retinal cavernous hemangioma is a vascular hamartoma with little potential for growth, but it can produce vitreous hemorrhage (Fig. 6). This can be a feature of a syndrome of cavernous hemangioma of the brain, skin, and eye. Management is typically observation.
Retinal Racemose Hemangioma
Retinal racemose hemangioma is vascular malformation in which there is a dilated single or multiple retinal vessels without intervening capillary system, producing a vermiform vascular anomaly (Fig. 7). Occasionally, a vascular obstruction is noted. This lesion can be a feature of the Wyburn-Mason syndrome. Management is observation.
Retinal Vasoproliferative Tumor
Retinal vasoproliferative tumor is an acquired, benign retinal mass, typically located in the inferotemporal periphery and with surrounding exudation and subretinal fluid (Fig. 8) [8–10]. This tumor is classified into primary or secondary lesions. Secondary lesions are found in eyes with retinitis pigmentosa, pars planitis, Coats disease, or other retinal scarring conditions. Management includes observation, laser photocoagulation, photodynamic therapy, cryotherapy, plaque radiotherapy, or anti-VEGF medications.
Retinal Lymphoma/Leukemia
Retinal involvement with lymphoma or leukemia can appear as a white infiltration, occasionally with surrounding hemorrhage [11]. Vitreoretinal lymphoma classically shows sub-RPE tumor and vitreous cells and can have central nervous system lymphoma. Retinal leukemia usually is a late finding with systemic leukemia. Management with systemic chemotherapy is indicated (Figs. 9 and 10).
Same patient as in Fig. 9 with vitreoretinal lymphoma and sub-RPE lymphoma deposits in the left eye
Tumors of the RPE
The RPE is a single-layer epithelium and can spawn several tumors including congenital hypertrophy of the RPE (CHRPE), congenital RPE markers of familial adenomatous polyposis (FAP), congenital simple hamartoma of the RPE, combined hamartoma of the retina and RPE, and adenoma/adenocarcinoma of the RPE.
Congenital Hypertrophy of the RPE
CHRPE is a flat, heavily pigmented benign lesion that classically occurs in the peripheral fundus [12]. The diameter of CHRPE varies from a tiny flat spot to large flat lesion of up to 13 mm with geographic margins and central hypopigmented lacunae [12]. This lesion classically displays sharp margins and can be associated with a surrounding nonpigmented and a complementary pigmented halo [12]. Multifocal CHRPE is known as “bear tracks.” Optical coherence tomography (OCT) of CHRPE shows complete lack of photoreceptors over the lesion, and autofluorescence shows complete lack of lipofuscin (Figs. 11 and 12) [13–15].
Congenital RPE Markers of FAP
Congenital RPE lesions that show pisciform (fishlike) configuration, depigmented tail, or even focal RPE dot can serve as a marker of FAP, especially if the patient has four or more lesions in both eyes (Fig. 13) [16]. These lesions remain stable and require no ophthalmic intervention.
Congenital Simple Hamartoma of the RPE
Congenital simple hamartoma of the RPE is a dark black, round mass located in the parafoveal region (Fig. 14) [17]. In most cases, visual acuity is normal. This lesion rarely enlarges and requires no intervention.
Combined Hamartoma of the Retina and RPE
Combined hamartoma of the retina and RPE is a benign, presumed congenital condition that can manifest in the papillomacular region or more peripheral near the equator of the eye [18, 19]. This mass displays a mossy green color with retinal traction and tortuosity as well as vitreoretinal traction. Association with neurofibromatosis type 2 and brachial cleft syndrome is occasionally noted (Fig. 15).
Adenoma/Adenocarcinoma of the RPE
The RPE can proliferate into a nodular mass composed of benign (adenoma) or malignant (adenocarcinoma) epithelial cells. Occasionally, surrounding exudation and vitreous hemorrhage is found (Fig. 16).
Tumors of the Ciliary Body Epithelium
The ciliary body epithelium can produce benign or malignant medulloepithelioma of childhood or adenoma/adenocarcinoma of adulthood.
Medulloepithelioma
Medulloepithelioma is a benign or malignant proliferation of the nonpigmented ciliary epithelium that is believed to be a congenital tumor that continues to proliferate after birth. Lens coloboma and neovascular glaucoma are also found in some cases (Fig. 17). Management includes plaque radiotherapy or enucleation.
Adenoma/Adenocarcinoma of the Ciliary Body Pigmented or Nonpigmented Epithelium
Adenoma or adenocarcinoma of the ciliary body epithelium typically arises in midadult or older adults as a pigmented or nonpigmented mass located immediately behind the lens. Surgical resection is the treatment of choice.
Tumors of the Choroid
The choroid is composed of melanocytes, vascular elements, and neural tissue, each of which can produce tumors. The most common tumors of the choroid include nevus, metastasis, and melanoma. These lesions can be differentiated based on clinical and imaging evaluations. Occasionally, fine-needle aspiration biopsy is necessary to establish the diagnosis.
Choroidal Nevus
Choroidal nevus is a benign tumor found in approximately 7 % of the Caucasian population [20, 21]. In a population-based study, the mean diameter of choroidal nevus was 1.5 mm [20]. In an ocular oncology clinic-based study, the mean diameter was 5 mm [22]. Choroidal nevus is brown-pigmented in 80 %, and yellow-nonpigmented in 20 % [22]. Overlying drusen (40 %), RPE atrophy (13 %), RPE hyperplasia (9 %), orange pigment (10 %), and choroidal neovascularization (<1 %) can be seen [15]. Transformation into melanoma occurs 1 in 8,845 cases, often identified by risk factors including tumor thickness greater than 2 mm; overlying orange pigment; associated subretinal fluid; symptoms of flashes, floaters, or blurred vision; location of the mass within 3 mm of the optic disc; ultrasound evidence of tumor hollowness, and absence of halo or drusen [23, 24] (Figs. 18, 19, 20, 21, 22 and 23).
Choroidal Melanoma
Choroidal melanoma is a serious, life-threatening intraocular malignancy that appears with a dome or mushroom configuration, often with surrounding subretinal fluid and occasional subretinal or vitreous hemorrhage [25]. Approximately six individuals per million population annually develop this malignancy, with roughly 2,000 new cases in the United States each year. Prognosis of melanoma depends on tumor thickness, with each increasing millimeter imparting 5 % increased risk for metastasis [26, 27]. Treatment includes enucleation, surgical resection, proton radiotherapy, plaque radiotherapy, or thermotherapy (Figs. 24, 25, 26, 27, 28, 29, 30, 31 and 32).
Choroidal Metastasis
Choroidal metastases appear as a yellow mass, often with subretinal fluid. This malignancy originates from primary breast cancer in 53 %, lung cancer in 20 %, and others [28]. Bilateral metastases are most often secondary to breast carcinoma (70 %) (Figs. 33, 34, 35 and 36) [28].
Choroidal Hemangioma
Choroidal hemangioma can appear as a circumscribed or diffuse vascular mass. The circumscribed lesion appears as a circumscribed, round, slightly elevated orange mass of mean diameter 6 mm and thickness of 3 mm [29]. This tumor classically occurs in the postequatorial region and exhibits slow enlargement with progressive subretinal fluid or macular edema. The diffuse hemangioma occurs in patients with Sturge-Weber syndrome and can produce total retinal detachment. Management includes photodynamic therapy or radiotherapy (Figs. 37, 38, 39, 40 and 41) [30, 31].
Choroidal Osteoma
Choroidal osteoma is a benign intraocular tumor composed of mature bone [32, 33]. This tumor classically manifests as an orange-yellow plaque deep to the retina in the juxtapapillary or macular region of young women. This tumor can be unilateral (80 %) or bilateral (20 %). The cause and pathogenesis of this tumor are unknown. Ten-year probability for tumor growth is 51 %, tumor decalcification is 46 %, related choroidal neovascularization is 31 %, visual acuity loss of 3 or more Snellen lines is 45 % (Figs. 42, 43, 44 and 45) [33].
Choroidal osteoma in the left macula of the patient in Fig. 44
Choroidal Leiomyoma
Ciliary body/choroidal leiomyoma is a benign tumor arising in the suprauveal space [34]. This tumor appears nonpigmented and most often is managed with surgical resection (Fig. 46).
Choroidal Lymphoma
Intraocular lymphoma can be divided into uveal and vitreoretinal forms [35]. In the uveal form, the tumor is typically low grade and appears as a placoid thickening of the choroid with occasional overlying subretinal fluid. In the vitreoretinal form, the tumor is high-grade large cell lymphoma and can manifest with vitreous tumor, sub-RPE infiltration, and retinal infiltration. Definitive diagnosis is made through fine-needle aspiration biopsy (Figs. 47 and 48).
Tumors of the Disc
Optic Disc Melanocytoma
Optic disc melanocytoma is a darkly pigmented nevus obscuring the disc details and occasionally causing compression with visual acuity or visual field loss. This benign lesion can slowly grow in 14 % of cases and can rarely transform into melanoma [36]. Management is observation (Figs. 49 and 50).
Optic Disc Hemangioblastoma
Optic disc hemangioblastoma is a benign reddish mass of the disc, often with indiscrete margins that can produce subretinal fluid and exudation. Evaluation for von Hippel–Lindau disease is warranted. Management is challenging and includes laser photocoagulation, photodynamic therapy, plaque radiotherapy, external beam radiotherapy, or anti-VEGF medications (Fig. 51).
Optic Disc Metastasis
Optic disc metastasis appear as a yellow, pallid swelling of the disc with intrinsic vascularity, often in a patient with known cancer [37]. Typically, there are surrounding choroidal metastases. Management generally involves chemotherapy or ocular radiotherapy.
References
Wong JR, Tucker MA, Kleinerman RA, Sevesa SS. Retinoblastoma incidence patterns in the US Surveillance, Epidemiology, and End Results program. JAMA Ophthalmol. 2014;132:478–83.
Kivelä T. The epidemiological challenge of the most frequent eye cancer: retinoblastoma, an issue of birth and death. Br J Ophthalmol. 2009;93:1129–31.
Shields CL, Kaliki S, Rojanaporn D, Al-Dahmash S, Bianciotto CG, Shields JA. Intravenous and intra-arterial chemotherapy for retinoblastoma: what have we learned? Curr Opin Ophthalmol. 2012;23:202–9.
Shields CL, Fulco EM, Arias JD, Alarcon C, Pelligrini M, Rishi P, et al. Retinoblastoma frontiers with intravenous, intra-arterial, periocular and intravitreal chemotherapy. Eye. 2013;27:253–64.
Mennel S, Meyer CH, Eggarter F, Peter S. Autofluorescence and angiographic findings of retinal astrocytic hamartomas in tuberous sclerosis. Ophthalmologica. 2005;219:350–6.
Shields CL, Reichstein DA, Bianciotto CG, Shields JA. Retinal pigment epithelial depigmented lesions associated with tuberous sclerosis complex. Arch Ophthalmol. 2012;130:387–90.
Singh AD, Shields CL, Shields JA. Major review: von Hippel-Lindau disease. Surv Ophthalmol. 2001;46:117–42.
Shields JA, Decker WL, Sanborn GE, Ausberger JJ, Goldberg RE. Presumed acquired retinal hemangiomas. Ophthalmology. 1983;90:1292–309.
Shields CL, Shields JA, Barrett J, De Potter P. Vasoproliferative tumors of the ocular fundus. Classification and clinical manifestations in 103 patients. Arch Ophthalmol. 1995;113:615–23.
Shields CL, Kaliki S, Al-Dahmash S, Rajanaporn D, Shukla S, Reilly B, et al. Retinal vasoproliferative tumors: comparative clinical features of primary versus secondary tumors in 334 cases. JAMA Ophthalmol. 2013;131:328–34.
Guyer DR, Schachat AP, Vitale S, Markowitz JA, Braine H, Burke PJ, et al. Leukemic retinopathy. Relationship between fundus lesions and hematologic parameters at diagnosis. Ophthalmology. 1989;96:860–4.
Shields CL, Mashayekhi A, Ho T, Cater J, Shields JA. Solitary congenital hypertrophy of the retinal pigment epithelium: clinical features and frequency of enlargement in 330 patients. Ophthalmology. 2003;110:1968–76.
Shields CL, Materin MA, Walker C, Marr BP, Shields JA. Photoreceptor loss overlying congenital hypertrophy of the retinal pigment epithelium by optical coherence tomography. Ophthalmology. 2006;113:661–5.
Fung AT, Pellegrini M, Shields CL. Congenital hypertrophy of the retinal pigment epithelium: enhanced depth imaging optical coherence tomography in 18 cases. Ophthalmology. 2014;121:251–6.
Shields CL, Pirondini C, Bianciotto C, Harmon SA, Shields JA. Autofluorescence of congenital hypertrophy of the retinal pigment epithelium. Retina. 2007;27:1097–100.
Traboulsi EI, Apostolides J, Giardiello FM, Krush AJ, Booker SV, Hamilton SR, et al. Pigment ocular fundus lesions and APC mutations in familial adenomatous polyposis. Ophthalmol Genet. 1996;17:167–74.
Shields CL, Shields JA, Marr BP, Sperber DE, Gass JD. Congenital simple hamartoma of the retinal pigment epithelium: a study of five cases. Ophthalmology. 2003;110:1005–11.
Schachat AP, Shields JA, Fine SL, Sanborn GE, Weingeist TA, Valenzuela RE, et al. Combined hamartomas of the retina and retinal pigment epithelium. Ophthalmology. 1984;91:1609–15.
Shields CL, Thangappan A, Hartzell K, Valente P, Pirondini C, Shields JA. Combined hamartoma of the retina and retinal pigment epithelium in 77 consecutive patients. Visual outcome based on macular versus extramacular tumor location. Ophthalmology. 2008;115:2246–52.
Sumich P, Mitchell P, Wang JJ. Choroidal nevi in a white population: the Blue Mountains Eye Study. Retina. 1998;116:645–50.
Greenstein MB, Myers CE, Meuer SM, Klein BE, Cotch MF, Wong TY, et al. Prevalence and characteristics of choroidal nevi: the multi-ethnic study of atherosclerosis. Ophthalmology. 2011;118:2468–73.
Shields CL, Furuta M, Mashayekhi A, Berman EL, Zahler JD, Hoberman DM, et al. Clinical spectrum of choroidal nevi based on age at presentation in 3422 consecutive eyes. Ophthalmology. 2008;115:546–52.
Singh AD, Kalyani P, Topham A. Estimating the risk of malignant transformation of a choroidal nevus. Ophthalmology. 2005;112:1784–9.
Shields CL, Furuta M, Berman EL, Zahler JD, Hoberman DM, Dinh DM, et al. Choroidal nevus transformation into melanoma: analysis of 2514 consecutive cases. Arch Ophthalmol. 2009;127:981–7.
Shields CL, Kaliki S, Furuta M, Mashayekhi A, Shields JA. Clinical spectrum and prognosis of uveal melanoma based on age at presentation in 8033 cases. Retina. 2012;32:1363–72.
Shields CL, Furuta M, Thangappan A, Nagori S, Mashayekhi A, Lally DR, et al. Metastasis of uveal melanoma millimeter-by-millimeter in 8033 consecutive eyes. Arch Ophthalmol. 2009;127:989–98.
Margo CE. The Collaborative Ocular Melanoma Study: an overview. Cancer Control. 2004;11:304–9.
Shields CL, Shields JA, Gross NE, Schwartz GP, Lally SE. Survey of 520 eyes with uveal metastases. Ophthalmology. 1997;104:1265–76.
Shields CL, Honavar SG, Shields JA, Cater J, Demirci H. Circumscribed choroidal hemangioma: clinical manifestations and factors predictive of visual outcome in 200 consecutive cases. Ophthalmology. 2001;108:2237–48.
Blasi MA, Tiberti AC, Scupola A, Balestrazzi A, Colangelo E, Valente P, et al. Photodynamic therapy with verteporfin for symptomatic circumscribed choroidal hemangioma: five-year outcomes. Ophthalmology. 2010;117:1630–7.
Arepalli S, Shields CL, Kaliki S, Komarnicky L, Shields JA. Diffuse choroidal hemangioma management with plaque radiotherapy in 5 cases. Ophthalmology. 2013;120:2358–9.
Shields CL, Shields JA, Augsburger JJ. Choroidal osteoma. Surv Ophthalmol. 1988;33:17–27.
Shields CL, Sun H, Demirci H, Shields JA. Choroidal osteoma: factors predictive of tumor growth, tumor decalcification, choroidal neovascularization, and visual outcome in 74 eyes. Arch Ophthalmol. 2005;123:1658–66.
Shields JA, Shields CL, Eagle Jr RC, De Potter P. Observations on seven cases of intraocular leiomyoma. The 1993 Byron Demorest Lecture. Arch Ophthalmol. 1994;112:521–8.
Mashayekhi A, Shukla SY, Shields JA, Shields CL. Choroidal lymphoma: clinical features and association with systemic lymphoma. Ophthalmology. 2014;121:342–51.
Shields JA, Demirci H, Mashayekhi A, Shields CL. Melanocytoma of the optic disc in 115 cases. The 2004 Samuel Johnson Memorial Lecture. Ophthalmology. 2004;111:1739–46.
Shields JA, Shields CL, Singh AD. Metastatic neoplasms in the optic disc. The 1999 Bjerrum Lecture. Part 2. Arch Ophthalmol. 2000;118:217–24.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Shields, C.L., Shields, J.A. (2016). Wide-Field Retinal Imaging of Retinal and Choroidal Tumors. In: Kozak, I., Arevalo, J. (eds) Atlas of Wide-Field Retinal Angiography and Imaging. Springer, Cham. https://doi.org/10.1007/978-3-319-17864-6_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-17864-6_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-17863-9
Online ISBN: 978-3-319-17864-6
eBook Packages: MedicineMedicine (R0)