Abstract
Malnutrition and dysphagia are common after stroke and frequently occur together. Failure to recognise their presence and manage them effectively will result in increased morbidity and mortality. Infection risk may be raised, recovery and rehabilitation will be slowed, and people will be more likely to end up in long-term care. Treatment of malnutrition and swallowing difficulties requires early recognition, e.g. through routine screening procedures, and their management requires input from the multi-disciplinary team.
Monitoring of nutrition and swallowing status needs to be regular and consistent and may need to continue beyond hospital discharge into the care home environment and in those living at home. Consequently, issues around the detection and management of malnutrition and dysphagia need to be raised with all care staff and professionals.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Key Messages-
Dysphagia and nutritional problems are common after stroke.
-
Poor nutritional status may predate the stroke, as may dysphagia.
-
People may not eat due to post-stroke co-morbidities, depression, infection, and psychological and social issues.
-
Poor nutrition and dysphagia are markers of poor outcome and increased mortality.
-
The management of both dysphagia and malnutrition requires multi-disciplinary input.
-
Ongoing nutritional care needs (including swallowing problems) should be considered during discharge planning.
-
Patients with long-term care needs should be reviewed regularly post-discharge.
Introduction
Dysphagia after stroke is common as is under-nutrition. Both are indicators of a poorer prognosis and an increase in dependency. It is therefore essential that they are recognised and managed appropriately at the earliest opportunity.
Definitions
Malnutrition
No universally accepted definition of malnutrition exists; however, one that is commonly cited in the UK literature is as follows:
A state of nutrition in which a deficiency or excess (or imbalance) of energy, protein, and other nutrients causes measurable adverse effects on tissue/body form (body shape, size and composition) and function, and clinical outcome. [1]
This definition encompasses both over- and under-nutrition and emphasises the impact of malnutrition on functional and clinical outcomes in individuals. Recently, an International Guideline Consensus Committee [2] categorised malnutrition, i.e. under-nutrition, in the following three ways:
-
1.
Starvation-related malnutrition where chronic starvation occurs in the absence of inflammation such as might result from a range of social and/or psychological issues.
-
2.
Chronic disease-related malnutrition where there is chronic, mild to moderate inflammation such as might be associated with chronic diseases such as COPD, cancer, or chronic renal failure.
-
3.
Acute disease or injury-related malnutrition where there is acute, severe inflammation and the patient is usually hospitalised.
While this provides a useful aetiological classification of under-nutrition, and recognises the effects of illness and other factors on nutritional status, there remain no clear criteria for how each category might be identified in clinical practice. Taken together however, these two definitions [1, 2] encapsulate both the potential causes and adverse impacts of malnutrition.
Overweight and Obesity
Overweight and obesity are defined as “abnormal or excessive fat accumulation that may impair health” [3]. In this chapter, the term malnutrition will be taken to mean under-nutrition and the terms overweight and obesity will be used to describe over-nutrition.
Dysphagia
Dysphagia is defined in the Oxford English Dictionary as “A condition in which swallowing is either difficult or painful. It may be caused by diseases of the mouth, pharynx, or larynx, neuromuscular disturbances, or obstruction of the oesophagus”. Aphagia is just an extreme form of dysphagia.
Other relevant definitions in this context are eating, i.e. “The transfer of food/drink to the mouth” and swallowing, i.e. “The transfer of food from the mouth to the stomach”.
Malnutrition
Epidemiology
Malnutrition has widespread adverse effects on physical, social, and psychological function including decreased muscle strength, low mood, decreased ability to perform everyday tasks [4], and poorer quality of life [5]. In the presence of illness, malnutrition results in delayed recovery, increased complications, and increased mortality [6] and is associated therefore with increased hospitalisation and use of health and social care resources [7]. As a result, malnourished individuals cost twice as much to manage as the well-nourished [8], and in the UK the cost of managing malnourished individuals has been estimated to be up to £13 billion per year [9]. Furthermore, caring for nutritionally vulnerable family members or friends imposes a significant burden on carers, with around 60 % of carers worrying about the nutrition of the person they care for, and one-quarter looking after someone who is underweight [10]. In the UK, national surveys using a validated nutrition screening tool [11] suggest that, at any time, around three million individuals are at risk of malnutrition or are malnourished, i.e. nutritionally vulnerable, with more than one million being elderly [12]. Until recently the focus of detecting and managing malnutrition has been in hospitals [7]; however, it is evident that the vast majority of nutritionally vulnerable individuals (90 %) live in their own homes in the community with only 5 % being in sheltered housing, 3 % in care homes, and 2 % in hospital [13].
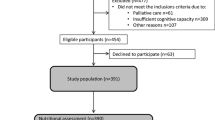
In stroke populations, reported prevalence rates of malnutrition vary widely from 6 % up to 62 % [14]. While this variation may in part depend on the care setting, type, and severity of stroke or time since initial insult [15–21], there is also considerable variability in the methods and thresholds used to define malnutrition [14]. For example, of the 18 studies included in the review by Foley et al., only three used structured nutritional assessment methods that had been validated previously [17, 19, 20], i.e. the Mini Nutritional Assessment [22] and the Subjective Global Assessment [23], and one large, multi-centre study [24] used a variety of methods in the different recruitment sites (n = 25 hospitals) including a previously validated “informal assessment” [25]. In a recent study in two stroke units in south London, the use of a validated nutrition screening tool, i.e. the Malnutrition Universal Screening Tool (MUST), suggested around 30 % patients are at medium or high risk of malnutrition on admission to hospital following an acute stroke [26].
Similar to other malnourished populations, malnourished stroke patients are more likely to develop complications in hospital such as gastrointestinal bleeds, pneumonia, and other infections [20, 21, 24] and as a result they stay in hospital longer [16, 20, 27], suffer poorer functional outcomes [21], are less likely to be discharged home [28], and have higher hospitalisation costs [27]. They are also more likely to die in hospital or soon after discharge [16, 17, 21]. Indeed, being malnourished has been shown to be an independent predictor of poor outcome in patients who have had a stroke [18, 26].
Following a stroke, those patients who survive frequently develop swallowing and other feeding difficulties secondary to their stroke and often become more malnourished during their hospital stay [29]. Furthermore, in a significant proportion of patients, malnutrition continues beyond hospital discharge and can last for many months after the initial insult. For example, in a study of 206 stroke survivors more than 65 % reported some eating difficulties at 6 months post-stroke, with eating disabilities having a significant adverse effect on quality of life [30], and in a study of 305 stroke survivors weight loss persisted for up to 12 months post-stroke in one-quarter of patients [31]. Patients discharged to nursing homes appear to be at particular risk of eating difficulties, with one study reporting that more than 80 % of stroke patients in nursing homes were assessed as having some sort of dependence in eating [32]. These studies suggest that stroke patients who are malnourished at hospital discharge are likely to require longer term nutritional support and regular monitoring in care homes and/or the community to avoid the negative outcomes associated with malnutrition, e.g. hospital readmissions, decline in functional status, and poor quality of life.
Aetiology
Following a stroke, the most obvious cause of malnutrition is dysphagia. However, there are a whole host of other potential causes that could either exacerbate pre-existing malnutrition or precipitate it in the nutritionally vulnerable (Table 7.1). While in hospital, the reasons for poor dietary intake and subsequent weight loss are most likely to be illness related and may include disease- or drug-induced anorexia, periods of temporary starvation (nil by mouth) for dysphagia or medical procedures, feeding difficulties secondary to impaired mobility and/or perception issues, pain, anxiety, or depression [33]. In both hospitals and care homes however, organisational issues might further limit individuals’ choice, availability, and access to food. Furthermore, a lack of attention to nutritional care might also have an adverse impact on an individual’s intake. For example, provision of unfamiliar or inappropriate foods, inadequate supervision or support during mealtimes, patients being in an uncomfortable position to eat, food placed out of reach, utensils or packaging presenting difficulties for eating, and environmental factors such as staff interrupting meal times or long gaps between evening meal and breakfast have all been shown to have a negative impact on dietary intake in hospitalised or institutionalised individuals [34–37]. Following hospital discharge, in addition to the continuing effects of the stroke and its management, sub-optimal nutritional status may be further compounded by previously existing, or a new range of, psychological and social issues (Table 7.1). While many individuals function alone very effectively when healthy, this often changes during and following illness. Even the most independent individual may require practical help after a stroke, and it is therefore important to identify patients with minimal social support, e.g. the recently bereaved, homeless, or recent immigrants, while they are in hospital in order to start addressing their likely nutritional, and other, care needs on discharge. The effort involved in shopping, preparing, or cooking a meal can seem insurmountable during or after illness, and many patients may need some assistance with this in the early stages of recovery. If these social and psychological issues are not recognised prior to, or soon after discharge, this can result in a vicious, self-perpetuating cycle of inadequate intake, associated complications, repeated hospital admissions, and poor outcomes [7].
Detection
Malnourished individuals, or those who have been identified as at medium or high risk of malnutrition, are more likely to benefit from nutritional intervention than those who are adequately nourished or at low risk of malnutrition [6]. On admission to hospital following a stroke, the focus should be on identifying those who are nutritionally vulnerable, i.e. malnourished or at medium/high risk of malnutrition. In clinical practice this can be accomplished by the routine use of nutrition screening tools. Nutrition screening using a validated tool has been recommended by a number of professional organisations in the USA and Europe, among them the American Society for Parenteral and Enteral Nutrition [38], the British Dietetic Association [39], the European Society for Parenteral and Enteral Nutrition [40], the British Association for Parenteral and Enteral Nutrition (BAPEN) [11], and the National Institute for Health and Clinical Excellence [7].
The role of a nutrition screening tool (NST) is to aid the identification of patients who are nutritionally vulnerable, i.e. currently malnourished or at risk of becoming malnourished, in order that they might be referred for further assessment and nutritional intervention if required [1]. NSTs are not designed to assess the nutritional status of patients, establish the severity of malnutrition, or identify the reasons for poor status; they simply indicate that a patient has actual or potential nutritional problems and requires further investigation. While providing a useful, structured aide memoire, NSTs support, but do not replace, clinical judgement. NSTs are usually completed by nursing staff or health-care assistants who are not nutrition specialists, and thus people identified as at medium or high risk of malnutrition during a screening procedure should be referred for a full nutritional assessment by a nutrition specialist such as a dietician. Similar to all screening tools, NSTs should be valid and reliable, and since they should be completed on all patients in a particular setting, they should be quick to administer, easy to use and to interpret, and acceptable to both patients and health-care professionals [41]. Examples of validated nutrition screening tools used in the UK and Europe include the Malnutrition Universal Screening Tool (MUST) [11], the Nutrition Risk Score-2002 (NRS-2002) [42], the Short Nutritional Assessment Questionnaire (SNAQ) [43], and the short-form Mini Nutritional Assessment (Short-form MNA) [44]. The majority of these screening tools require the measurement of height and weight to determine body mass index (BMI) and also require a record of recent weight change and/or change in dietary intake. People who eat almost nothing for 5 days lose about 5 % of their body weight, even in the absence of disease. Furthermore, minimal dietary intake for a few days in the presence of disease results in poor muscle function, increased risk of infection, and delayed wound healing, even in the absence of recorded weight loss [6]. Therefore, patients who are nil by mouth (or have minimal intake) for more than 5 days, e.g. due to dysphagia following a stroke, should be considered to be at nutritional risk, even if their nutritional status was adequate when they were admitted to hospital.
Recently, it was shown that a validated NST is a good predictor of poor outcome in patients who have had a stroke. In a study of 537 patients screened using MUST within 72 h of hospital admission for acute stroke, there was a strong positive correlation between risk of malnutrition and mortality rate which remained significant after adjustment for possible confounders [26]. At 6 months those patients who were at high risk of malnutrition on admission to hospital were twice as likely to die than those at low risk. Furthermore, for patients who survived there was a strong positive correlation between the risk of malnutrition and both length of hospital stay and hospitalisation costs, which again remained significant after adjustment for possible confounders [26]. Patients at high risk of malnutrition were likely to stay in hospital three times longer than those at low risk and cost nearly twice as much [26].
It is perhaps not surprising, therefore, that to aid the identification of at-risk and malnourished patients, the National Institute for Health and Clinical Excellence recommends that all patients should be screened routinely on admission to hospital and care homes, at regular intervals throughout their stay, during outpatient and GP visits, and on first contact with community care teams [7]. In England and in other countries, similar recommendations around the use of validated nutrition screening tools have been incorporated into recent guidelines for the management of acute stroke [45–47].
Assessment
Following nutrition screening, patients identified as malnourished or at medium/high risk of malnutrition should undergo a full nutritional assessment conducted by a health-care professional with specialist nutrition knowledge, usually a dietician [7]. Nutritional assessment establishes the nutritional status of an individual and explores the causes and duration of nutritional problems. The assessment forms the basis for determining treatment goals and the nature, mode, and duration of nutritional intervention.
A full nutritional assessment usually comprises five major components: anthropometry, i.e. measurements of weight, height, and body composition; a review of laboratory data; an assessment of clinical status; an assessment of dietary intake; and consideration of environmental factors. There are a number of validated nutrition assessment tools available, e.g. the Mini Nutritional Assessment (MNA) tool [22], Subjective Global Assessment (SGA) tool [23], and Patient-Generated SGA [48], all of which include at least some of the following components.
Anthropometry
Body weight is usually recorded routinely as part of the nutrition screening process and provides valuable information on both current and past nutritional status. While most clinicians will readily identify someone who is thin as either malnourished or at risk of malnutrition, individuals who are not thin may also be at risk of malnutrition, even if they look (or are) overweight or obese. Whereas low body mass index (BMI) reflects chronic malnutrition, recent weight loss reflects acute changes in nutritional status and suggests underlying physical or psychological illness or social issues. Regardless of BMI, unintentional weight loss greater than 10 % over 3–6 months, or more than 5 % in 1–3 months, is generally considered to be clinically significant because it is associated with loss of body function and poor clinical and functional outcomes [11].
In a recent study of 543 acute stroke patients, 109 (20 %) participants had unintentionally lost weight prior to hospital admission for a variety of reasons unrelated to their stroke, including gastrointestinal symptoms, excess alcohol intake, previous surgery, taste changes, loss of interest in food, and bereavement [49]. In this study those who had experienced pre-admission weight loss had a significantly higher risk of mortality and a significantly longer hospital stay at 6 months post-stroke, and cost significantly more (£8,416 versus £5,506 per patient) than those who had been weight stable prior to the stroke. Furthermore, those who had lost the most weight were at greatest risk of poor outcomes. A history of unintentional weight loss before admission should therefore send warning bells to any clinician who might be considering the nutritional needs of their patient, particularly if the patient has had a severe stroke and/or has dysphagia, and oral intake is likely to be compromised for more than a couple of days [7].
Since BMI provides useful information regarding nutritional status in both the malnourished and obese, the accurate measurement of height is an important component of a full nutritional assessment. Both in the outpatient and inpatient setting, health-care professionals have a role in ensuring that, wherever possible, all patients have their height measured and documented at least once in adulthood [7]. In those patients where height is not known, and where it cannot be measured safely due to mobility issues, surrogate measures for height such as ulna length [50], demi-span [51], or knee-height [52] can be used. All three of these techniques provide a reliable estimate of height, suitable for determining BMI, if undertaken by a trained practitioner.
During the first few days following a stroke, a small proportion of patients will be unsafe or unable to mobilise and it may not be possible to weigh them, either to obtain information for a weight history or to calculate BMI (although hoist scales should be available on most stroke units). In this case a measurement of mid-arm circumference (MAC) by a skilled practitioner may be used in the absence of weight to estimate BMI. Data collected from 1,561 hospitalised patients included in a nutrition intervention trial [53] suggest that those with a MAC less than 25.0 cm are likely to have a BMI less than 20 kg/m2 and those with a MAC less than 23.5 cm are likely to have a BMI less than 18.5 kg/m2 [53, 54].
Biochemistry
During a full nutritional assessment, laboratory data will be reviewed to help determine the patient’s hydration status, clinical condition, e.g. raised CRP, and low serum albumin levels indicating metabolic stress, and nutritional markers such as vitamin and trace element status. Some patients could be at risk of re-feeding syndrome [55, 56] if dietary intake has been poor for a prolonged period prior to (or during) hospital admission and phosphate, potassium, calcium, and magnesium levels should be reviewed prior to implementation of nutritional support in all patients with known re-feeding risk factors [7]. There are several published regimens for managing patients at risk of re-feeding syndrome. The lack of randomised controlled trials in this area, however, means that management is based on consensus and expert opinion rather than evidence [56]. Irrespective of which regimen is employed, the common principles are to prevent re-feeding syndrome by cautious re-introduction of energy and correction of biochemical abnormalities [7, 55]. It is likely that the problems associated with re-feeding are less likely to arise with oral nutritional support since illness is usually accompanied by a loss of appetite; however, care should be taken in the prescription of oral nutritional supplements in those at high risk of re-feeding syndrome [7].
Clinical
Quite apart from the direct impacts of a stroke, e.g. dysphagia, hemianopia, arm weakness, or neglect, patients who have had a stroke often present with a number of nutritionally relevant co-morbidities such as diabetes, hypertension, hyperlipidaemia, gastro-oesophageal reflux, or depression. All of these conditions will need to be taken into account when devising a nutrition action plan whether the patient is capable of consuming an oral diet or requires tube feeding.
Dietary
The onset of malnutrition is usually insidious, although in conditions of acute metabolic stress such as critical illness, nutritional depletion and weight loss can be very rapid and severe [6]. While there tends to be a focus on inadequate energy and protein intakes, it should be recognised that in people with a poor dietary intake, micronutrient intakes are also likely to be deficient [7]. It is also important to recognise that micronutrient intakes may be sub-optimal even in the presence of adequate macro-nutrient intakes, particularly if individuals follow a restricted diet or a diet of limited variety or poor quality [57].
Dietary assessment should take account not only current (i.e. inpatient) nutritional intake but also previous (prior to stroke) and likely future intakes (post-discharge). Dietary intake may be assessed in a number of different ways (and for varying lengths of time) depending on the nutrient or food of interest, the care setting, and the patient’s ability to provide valid and accurate information [58]. In the acute setting, dietary intake is usually estimated from data recorded by nursing staff on food record charts. Since food record charts are rarely fully or accurately completed [59], a dietician may also ask the patient (and/or their carer or nurse) to describe everything they have eaten and drunk in the previous 24 h (24-h recall method) [58]. In order to obtain information on a patient’s habitual intake, e.g. pre-admission, a diet history may be taken [58].
In patients who have had a stroke, dietary assessment aims to determine the patient’s actual and potential ability to meet their nutritional needs by normal texture diet via the oral route. In a significant proportion of patients, this will be unlikely (or unsafe) and alternative routes and methods of feeding will need to be considered. While it might be expected that patients who have had a stroke would have a poor dietary intake in hospital, very few studies exist that describe the nutritional intakes of hospitalised stroke patients. One study suggests that the energy intake of hospitalised stroke patients with adequate swallow is similar to that of other hospitalised patient groups, i.e. an average of 75 % of predicted energy requirements over 2 weeks [60]. One other study which examined energy and protein intakes following stroke reported that, on average, regardless of diet type (oral or non-oral) and texture (regular diet or texture modified because of swallowing impairment), hospitalised patients consumed an average of 85 % of their energy requirements, and 86 % of protein requirements, during the first 21 days following stroke [61]. While these deficits might appear relatively small, over time they are sufficient to result in weight loss and may have an adverse effect on outcome in malnourished or medium/high-risk patients. If not treated, this could have a profound impact on rehabilitation, functional recovery, and outcome, even in previously adequately nourished patients [6].
Environmental
This final part of the assessment aims to establish how well the patient functioned in their home environment with regard to food purchase, preparation, and cooking prior to admission. For example, was the patient coping alone, did they require practical help and support from family and friends, or were they in receipt of a package of care which included help with these activities? Since a stroke is likely to have an adverse impact on several aspects of a person’s physical, social, or psychological function, the dietician will need to assess whether or not the patient is going to be capable of undertaking these activities on discharge (or soon afterwards) and start to make appropriate arrangements prior to discharge. Together with the multi-disciplinary team, the dietician will assess the patient’s need for post-discharge support including intermediate care, sheltered housing, care home admission, home meal delivery, shopping, or befriending services.
Management
Observational studies have shown an association of reduced mortality after stroke with nutritional assessment [62] and adequate nutrition and hydration (with antiplatelet therapy if required) [63]; however, a recent systematic review seeking to evaluate the impact of nutritional supplementation versus no supplementation in non-dysphagic stroke patients showed little benefit from supplementation [64]. This review should, however, be interpreted with caution since, although eight RCTs were included (4,391 participants), all included studies except the FOOD trial [24] were small and of relatively short duration. The inclusion criteria for the review failed to examine both nutritional risk status at baseline and compliance with intervention, and included studies conducted in patients recruited at any time up to 6 months post-stroke. Furthermore, the included studies described a variety of different nutritional interventions (including one assessing antioxidant and ω-3 fatty acids and one that included some tube-fed patients) in a variety of stroke populations. It is impossible therefore to determine if the observed lack of effect was due to heterogeneity in the interventions and populations, the result of inadequate intake due to poor compliance, or to failure of the intervention per se.
The underlying causes of inadequate intake in patients who have had a stroke are multi-factorial and multi-disciplinary and may originate in any part of a health-care organisation from the strategic policy level down to the individual feeding of a patient. Therefore, in the management of malnutrition in the acute setting, it is necessary to take into account not only the patient-specific issues that might impact on nutritional status, e.g. nutrition risk status on admission, severity of stroke, or ability to swallow but also to consider the systems for food and drink provision as well as the ward environment and nutritional care procedures. As a result, some interventions may be targeted and tailored for individuals while others may be non-targeted and implemented at ward or unit level. The need for these latter interventions assumes that a significant proportion of the stroke unit population are nutritionally vulnerable, and prevention of nutritional deterioration is the key aim. Examples of such interventions include protected mealtimes, red trays, feeding assistance, food fortification, or altering the mealtime environment to encourage food and drink consumption [65].
Goals of Treatment
In patients who have had a stroke, the goals of nutritional treatment are likely to include one or more of the following:
-
Meeting all nutritional requirements (macro- and micronutrients and fluid) in patients who are nil by mouth
-
Meeting nutritional needs while minimising the risk of aspiration by provision of a texture-modified diet for patients with dysphagia
-
Nutritional support (supplementation) for patients who are not meeting their full nutritional requirements (for whatever reason)
Nutritional Requirements
One of the aims of devising a nutritional prescription is to provide a patient with their complete requirements either via a single route or any combination of oral, enteral, or parenteral nutrition, while avoiding the known complications associated with both under- and over-feeding [7]. The nutritional requirements of an individual following a stroke will depend on their nutritional status, clinical condition, physical activity level, nutritional goals, and likely duration of nutritional support [7]; however, the nutritional requirements of patients who have had a stroke have yet to be fully characterised. While evidence suggests there is a small, temporary increase (7–14 % above predicted resting energy expenditure) in metabolic rate post-ischaemic stroke [66, 67], there is conflicting evidence around the impact of haemorrhagic stroke on metabolic rate [68–70].
A recent review of the evidence around energy requirements in healthy and sick populations by the Scientific Advisory Committee in Nutrition [71] concluded that while acute illness may result in a temporary increase in basal metabolic rate, this is usually accompanied by a significant reduction in physical activity such that total energy expenditure is usually around the same, or a little less than, healthy populations of the same age and gender. In the absence of stroke-specific studies, an energy prescription of 20–30 kcal/kg body weight/day is likely to be adequate for the majority of patients, although those who are severely malnourished (at risk of re-feeding syndrome), or are acutely unwell, might need to commence feeding at lower levels, and specialist advice should be sought [7].
Together with the assessment of dietary intake (see above), estimated nutritional requirements will indicate if there are any nutritional deficits, e.g. low energy intake, sub-optimal micronutrient intake, inadequate fluid intake, that need to be taken into account when devising the nutritional prescription.
Feeding Route
Wherever possible, nutritional and fluid requirements should be met via the oral route [72, 73]. In those who are unable to meet all their nutritional needs via the oral route, tube feeding should be considered [7]. Parenteral nutrition to meet all, or a proportion, of nutritional needs in those patients with a non-functioning gastrointestinal tract who are unable or unsafe to meet their needs by any other route is very rarely used in patients who have had a stroke [7].
Nutritional Interventions
In the management of malnutrition, interventions targeted at individuals may comprise one, or any combination, of the following strategies:
-
1.
Dietary counselling where the patient and/or their carers are counselled to increase the frequency of food and/or fluid consumption and thus maximise energy and protein intake. Advice is tailored to a patient’s preferences and lifestyle, taking into account any clinical conditions such as diabetes, hyperlipidaemia, or renal insufficiency.
-
2.
Food fortification to increase the macro- and micronutrient density of food and/or drink, using energy and protein-rich ingredients such as milk powder, butter, and milk, or commercially available, prescribable powders and liquids, e.g. Pro-cal (Vitaflo, Liverpool, UK) or Duocal (Scientific Hospital Supplies, Liverpool, UK).
-
3.
The provision of prescribable oral nutritional supplements (ONS) (often known as sip feeds), e.g. Ensure (Abbott, Maidenhead, UK), Fortisip (Nutricia, Trowbridge, UK), or Resource (Novartis, Camberley, UK).
-
4.
Texture-modified diets to meet the nutritional needs of those patients who are unsafe to swallow food and drink of normal texture.
-
5.
Tube feeding to meet all, or a proportion, of nutritional needs in those patients with a functioning gastrointestinal tract who are unable or unsafe to meet their needs orally.
Dietary Counselling
The aim of dietary counselling is to improve the macro- and micronutrient intakes of individuals by providing patients and/or their carers with tailored advice and support, often accompanied by written information including suggested daily menus and recipe sheets. By tailoring advice to an individual’s nutritional requirements, preferences, symptoms, and lifestyle it may be possible to achieve good compliance. Furthermore, on cessation of intervention, dietary habits may have changed sufficiently to ensure maintenance of any weight gain and/or functional benefits. Advice may be provided on a variety of topics including food choice and preparation, altered meal patterns, snacks, and nourishing drinks and may include advice on how to manage specific symptoms (e.g. dry mouth, taste changes) or how to overcome anorexia or specific eating difficulties. The effectiveness of dietary counselling will depend on many factors, and in patients who have had a stroke, confusion, altered consciousness, or limited comprehension may make it difficult for some patients to comply with dietary advice in the acute setting. On discharge, people recovering from a stroke may have some difficulties with shopping and food preparation, and multi-disciplinary team input may be required to address these issues in discharge planning. To date there are no studies evaluating the impact of dietary counselling in patients who have had a stroke [73].
Food Fortification
The aim of food fortification is to increase the nutrient density of food and drink without increasing portion sizes. Thus, this strategy might be particularly useful in individuals with a poor appetite or early satiety, symptoms that frequently accompany acute illness. Food fortification advice can be provided for individuals and/or their carers but can also be implemented at ward or unit level for vulnerable populations. Studies that have measured the impact of providing energy-dense meals and snacks to hospitalised patients have reported increased energy and protein intakes [74–76], a significant increase in body weight [77], and a significantly shorter length of hospital stay in a subgroup of the intervention patients [78]. To date there are no studies that have investigated the impact of food fortification on other clinical outcomes or cost.
Oral Nutritional Supplements (ONS)
While the FOOD trial suggests there are no benefits in routine supplementation of stroke patients using ONS [24], there is evidence that ONS can be beneficial in terms of energy intake, weight gain, and functional status in other patient groups, in particular the elderly [78], if they are provided to those who are nutritionally at risk or malnourished [79]. Typically, ONS contain a mix of macro- and micronutrients and most provide around 300 kcal, 12 g protein, and a full range of vitamins and minerals per serving, although there is a wide range available. ONS are usually present in liquid form, but puddings and powders are also available. Like tube feeds, ONS are foods for special medical purposes (FSMPs), and as such their composition and labelling are regulated under the European Commission Directive 1999/21/EC. ONS can be prescribed in the community for the management of disease-related malnutrition (and a number of other indications) in accordance with the Advisory Committee on Borderline Substances (ACBS) guidelines. The cost of ONS in the community is, however, often a consideration, and recently there has been considerable emphasis on the use of care pathways to ensure their appropriate use, including the need for regular monitoring and follow-up [80].
Texture-Modified Diets
In patients with dysphagia, a texture-modified diet may be prescribed after a full swallow assessment, usually by a speech and language therapist. Several studies have reported that patients requiring thickened fluids are less likely to meet fluid requirements [81, 82] and that texture-modified diets are often nutritionally inadequate [83, 84]. Since people who are nil by mouth (or have minimal intake) for more than 5 days are considered nutritionally at risk, patients may require oral nutritional supplements and/or supplementary tube feeding in order to meet their nutritional requirements [7].
The aims of dysphagia management are as follows [81, 85]:
-
Minimise risk of malnutrition
-
Minimise risk of dehydration
-
Minimise risk of aspiration pneumonia
-
Maintain oral intake
It is considered good clinical practice to maximise the nutritional intake of patients on texture-modified diets, but currently there is a lack of evidence around how best to achieve this [7]. In clinical practice it appears difficult to achieve consistent supplementation of texture-modified food and drinks, in part due to organisational constraints, but also due to issues around achieving the correct texture when adding thickeners at ward level, and the observation that people on these diets tend not to consume very much and frequently fail to meet their nutritional and fluid requirements [81–84]. Currently, it is not possible to discriminate between the impact of the food’s unappetising appearance, diluted flavour, and altered texture; patient-specific factors such as poor appetite, impaired mobility, or depression; and organisational issues such as limitations on the provision of a choice of attractive meals of the correct texture.
Tube Feeding
In those with a functioning gastrointestinal tract, tube feeding should be considered not only for those who are nil by mouth due to unsafe swallow, but also for those who are unable to meet their nutritional needs by the oral route alone, especially if they are already malnourished [7]. It should be noted that even in stroke populations, dysphagia is not the only reason that people fail to meet their nutritional requirements by the oral route alone. In general, people should be fed via a tube into the stomach unless there is upper gastrointestinal dysfunction. Where there is evidence of upper gastrointestinal dysfunction, or an inaccessible upper gastrointestinal tract, post-pyloric (duodenal or jejunal) feeding should be considered. For people being fed into the stomach, bolus or continuous methods should be considered, taking into account patient preference, convenience, and drug administration [7]. Those requiring post-pyloric feeding should, however, receive continuous rather than bolus feeding [7]. People who are unable to swallow safely or take sufficient nutrition orally should have an initial 2- to 4-week trial of tube feeding, and those who require longer term support should be considered for gastrostomy feeding [7, 47].
For a full discussion of the role of tube feeding in the management of stroke please see below.
Mealtime Improvements and Optimising Nutritional Care
At any time on a stroke unit there is likely to be a high proportion of patients experiencing significant feeding difficulties, either as a result of their stroke or due to pre-existing malnutrition. In recognition of this, it would appear to be good clinical practice to ensure ward-based systems and procedures are implemented that maximise the dietary intake of all patients, rather than targeting only those who are already malnourished. A number of strategies have been recommended as good clinical practice (Table 7.2) by national and international organisations including BAPEN and the European Commission, and professional bodies including the Royal College of Nursing and the Royal College of Physicians, although currently there is a lack of good-quality evidence to support their use [65]. At ward level the provision of food and drink is considered a nursing responsibility; however, it could be argued that strategies that aim to improve the mealtime environment and the patient meal experience require support from clinicians and other health-care professionals at all levels if they are to be effective.
Monitoring and Evaluation
The main objective of monitoring is to ensure nutritional support is provided safely and effectively. Monitoring also permits clinicians to assess the extent to which nutritional goals have been met and to detect and treat clinical complications as early and effectively as possible. Should any complications occur, or nutritional goals not be met, monitoring and evaluation will allow clinicians to alter the type of nutrition support, or amend the regimen, to improve its effectiveness or to minimise or prevent complications. To achieve these objectives, monitoring protocols should include a variety of observations and measurements (Table 7.3) [7].
The type and frequency of monitoring will depend on the extent and severity of the stroke, the presence of any co-morbidities that might complicate nutritional management, e.g. diabetes, in patients receiving enteral tube feeding, whether previous results were abnormal, the type of nutrition support used, the setting of the nutritional care, and the expected duration of nutrition support.
While not currently recommended for use in routine clinical practice in hospitalised patients who have had a stroke, serial triceps skinfold thickness (TSF) measurements can be a useful way to measure changes in fat mass over time (weeks or months) in patients who are likely to be followed up in the long term, e.g. in outpatient clinic. Together with MAC (see previously), TSF measurements can be used to determine mid-arm muscle circumference (which provides an estimate of lean body mass), and thus regular measurements of both TSF and MAC over time can indicate changes in body composition, i.e. lean body mass and fat mass. In clinical practice, this can be useful if the aim is to measure the impact of nutritional intervention either alone or together with physical and/or other therapies, such as might occur during rehabilitation after stroke. Since both the measurements of MAC and TSF are prone to large inter- and intra-observer error, all such anthropometric measurements should be undertaken by the same skilled practitioner on each occasion [93]. Similarly, hand-grip strength can be used to measure the impact of nutritional interventions over time on skeletal muscle function [94].
Observational studies show that documentation regarding nutritional status, body weight, appetite, and food intake is generally poor [95–98], yet nutritional intervention cannot be managed safely or effectively without adequate standards of both monitoring and documentation [7]. This would seem particularly pertinent with the decreases in length of hospital stay observed in recent years. With average hospital stays as short as 4 or 5 days, it is perhaps unrealistic to expect that the full nutritional treatment plan will be implemented in time for the patient to be discharged. While it should be possible to ensure the patient undergoes nutrition screening and assessment while in hospital, the full treatment plan may not be fully implemented prior to discharge. In such cases, post-discharge monitoring and follow-up arrangements to ensure the patient’s nutritional status are evaluated effectively, and to measure the impact of nutritional intervention, are particularly necessary. However, evidence suggests that discharge documentation to GPs relating to nutrition is poor and that, as a result, only a small proportion of malnourished patients are followed up by a dietician [99]. The doctor’s role in communicating relevant nutritional information between hospital and community health-care professionals is pivotal in ensuring effective discharge planning and safe transfer of care with respect to nutrition. This will be accomplished usually in collaboration with a dietician and other members of the multi-disciplinary team such as speech and language therapists and physiotherapists.
Since eating and drinking can remain problematic for many months post-stroke, and stroke may result in changes in social and/or psychological status that might impact on dietary intake and/or nutritional status, patients should be screened for nutritional risk status whenever they attend outpatient clinics, including at 6- and 12-month reviews in stroke clinic, or when they come into contact with community-based health-care professionals [7]. All those identified as malnourished or at risk of malnutrition in the community should be referred for a full nutritional assessment and intervention if required [7, 80].
Overweight and Obesity
Epidemiology
Obesity, i.e. excess body weight, in particular excess fat mass, is associated with an increased risk of several conditions that may lead to stroke, including hypertension, hyperlipidaemia, and diabetes mellitus.
Since 1980 the prevalence of obesity has nearly doubled worldwide. In 2008, more than 1.4 billion adults (35 %) aged 20 years and older were overweight, and of these, over 500 million (11 %) were obese [3]. Overweight and obesity are the fifth leading risk for global deaths, and at least 2.8 million adults die each year as a result of being overweight or obese. In addition, 44 % of the diabetes burden, 23 % of the ischaemic heart disease burden, and between 7 and 41 % of certain cancer burdens are attributable to overweight and obesity [3]. By 2050 obesity is predicted to affect 60 % of adult men and 50 % of adult women in the UK, and the NHS costs attributable to overweight and obesity are projected to reach £9.7 billion, with wider costs to society estimated to reach £49.9 billion per year [100]. These factors combine to make the prevention of obesity a major public health challenge.
While it is recognised that overweight and obesity are associated with the incidence of first-ever stroke, it is still debatable whether or not this is an association with obesity alone or a reflection of the fact that overweight and obese individuals are more likely to have other conditions such as hypertension, diabetes, and hyperlipidaemias, that in themselves increase the risk of stroke and cardiovascular diseases. Most studies seem to show that obesity is a modifiable risk factor for ischaemic stroke, but that it is highly mediated through other risk factors, i.e. diabetes, hypertension, and hyperlipidaemia [101].
Aetiology
The fundamental cause of obesity and overweight is an imbalance between energy (calories) consumed and energy expended, i.e. more energy is consumed than the body burns. The excess energy is stored as adipose tissue.
The exact cause of obesity is not clear, and in any individual likely arises from a complex combination of factors. The Obesity Systems Map [102] was developed to provide an insight into the multiple factors contributing to the high prevalence of obesity in the UK. It shows a complex web of often reinforcing causal factors that range from genetic predisposition and individual psychology and physiology, through the culture and economics of food production, food consumption, and the built environment; to education on food and nutrition, and attitudes towards physical activity and lifestyle. It is not within the scope of this chapter to consider all of these factors, but it is worth noting that eating habits, physical activity, and psychological issues are considered modifiable, and therefore are most often targeted in weight-loss interventions.
Detection
Body mass index (BMI) is a simple index of weight for height that is commonly used to classify overweight and obesity in adults. It is defined as a person’s weight in kilograms divided by the square of their height in metres (kg/m2). BMI provides the most useful population-level measure of overweight and obesity, as it is the same for both sexes and for all ages of adults. It should be considered a rough guide however, since the same BMI may not correspond to the same degree of fatness or associated health risk in different individuals and populations. Acknowledging this, the World Health Organisation continues to recommend that using a standard definition allows for meaningful comparisons between individuals and populations and provides a firm basis for evaluating interventions [103].
Health-care professionals need to be aware, and inform their patients, that members of black, Asian, and other ethnic groups face an increased risk of chronic health conditions at a lower BMI than the white population (below BMI 25 kg/m2) [104]. This has been demonstrated mainly in relation to risk of type 2 diabetes, and more research is needed to find out if the increased risk at lower BMI in different ethnic groups holds for first-ever stroke and/or stroke recurrence. Table 7.4 shows the BMI thresholds for white European and other populations recommended by the World Health Organisation (WHO 2004) [104].
More recently, it has become evident that the distribution of fat around the body is associated with different health risks. Abdominal obesity (also known as central adiposity) is associated with an increased risk of metabolic and cardiovascular diseases than an even or peripheral distribution of fat around the body [103]. Abdominal fat can vary dramatically within a narrow range of total body fat and BMI, which suggests the need for additional measures to assess the health risks associated with overweight and obesity [103]. Indeed, abdominal obesity has been shown to be a stronger risk factor for stroke than BMI [105, 106].
To detect central adiposity, it is possible to measure waist circumference [107], although there is considerable debate around the potential impact of measurement site on risk categorisation [108]. Waist circumference (WC), measured at the midpoint between the lower border of the rib cage and the iliac crest, is a convenient and simple method considered a good surrogate of visceral adiposity across a wide age range. It provides a measure of fat distribution that cannot be obtained by measuring BMI alone. Waist circumference is not recommended as a routine measure but may be used to give additional information on the risk of developing other long-term health problems [109]. It should be noted that the waist circumference cut-offs are different for the sexes and for different ethnic groups (Table 7.5) [110]. Since metabolic and cardiovascular risk plateaus at higher BMIs, there is no benefit to measuring waist circumference in those with a BMI greater than 35 kg/m2 [102].
To date there is a lack of evidence that weight reduction in overweight or obese individuals has an impact on the primary or secondary prevention of stroke [111]. However, being overweight or obese is associated with conditions that increase the risk of first-ever stroke, e.g. hypertension, diabetes, and hyperlipidaemia, and current guidelines therefore recommend that people who have had a stroke should be encouraged and supported to lose weight, at the same time as addressing other risk factors such as smoking, hypertension, diabetes, or physical inactivity [46, 47].
Assessment
Assessment should be focused on determining the degree of obesity, identification of risk factors for developing complications of obesity (cardiovascular disease and/or stroke), dietary intake, and contributing causes [109]. The degree of obesity can be established through measurements of weight and height to determine BMI, and the presence and extent of any central obesity may be established by a waist circumference measurement. Identification of other cardiovascular risk factors may be determined by blood pressure measurements [112] and through the biochemical assessment of blood glucose and a lipid profile. Other tests may be considered if appropriate, e.g. liver function tests or thyroid function tests.
Any medical conditions and co-morbidities that could increase the risk of developing complications of obesity should be discussed, e.g. family history of stroke and vascular disease, medical problems, medication, as should any psychological factors that might impact on, or be impacted by, obesity. An assessment of current dietary and alcohol intake should be made and should include an exploration of the patient’s knowledge about diet, and any previous dietary changes they have made in an attempt to lose weight or decrease alcohol intake. The assessment should also include identification of any environmental factors, e.g. social issues, smoking, physical activity, and exercise, that might impact on the risk of developing complications of obesity [109].
Management
The level of intervention should be determined based on the degree of obesity, waist circumference, and the presence of relevant co-morbidities and risk factors [109, 113]. Interventions should be escalated from general advice on healthy weight and lifestyle, through diet and physical activity tailored to the individual (often in combination with psychological interventions), to consideration of drug therapy or surgery [109].
In the face of many misleading articles in the lay media, it is important to set realistic targets for weight loss at the outset and to manage expectations. People should be made aware of national sources of accurate information and advice, such as NHS Choices and Change4life, and should be advised to lose a maximum of 0.5–1.0 kg per week [109]. Guidelines [109, 113] recommend that people should be advised to avoid “yo-yo” dieting (otherwise known as weight cycling), in which weight is repeatedly lost and regained over weeks, months, or years, since in some studies this has been shown to increase a person’s likelihood of developing fatal health problems more than if the weight had been lost gradually or not lost at all. More recent evidence however, suggests the impact of “yo-yo” dieting on morbidity and mortality is not consistent [114].
People should be made aware that the more weight they lose, the greater the health benefits, particularly if they lose more than 5 % of their body weight and maintain this for life [109, 113]. Furthermore, people should be reassured that even preventing future weight gain can lead to health benefits [109, 113]. Clinicians should acknowledge the effort required to lose weight, prevent weight regain, or avoid any further weight gain, and to maximise the chance of achieving weight loss, should take into account the person’s feelings about being overweight or obese, and their willingness and motivation to try to lose weight [109, 113].
Lifestyle Modification Programmes
Multi-component interventions are the treatment of choice [109], since dietary interventions are more likely to be successful in terms of reducing morbidity if they form one component of a lifestyle modification programme [109, 113].
Lifestyle modification programmes usually address dietary intake, physical activity, and behaviour change, and include input from a dietician, a physiotherapist, or qualified physical activity instructor and a psychologist. The focus of such programmes is on life-long lifestyle change and the prevention of future weight gain. Such programmes usually last at least 3 months, and sessions are offered at least weekly or fortnightly and include a “weigh-in” at each session. People attending lifestyle weight management programmes lose on average around 3 % of their body weight, but this varies considerably [109].
Dietary Intake
To date there appears to be no evidence to suggest that advice on losing weight while still in hospital following an acute stroke confers any benefits on overweight or obese individuals. The need to lose weight, however, is frequently addressed in outpatient clinics soon after hospital discharge following acute stroke.
The main requirement of a dietary approach to weight loss is that total energy intake should be less than energy expenditure. Dietary changes should be individualised, tailored to food preferences and lifestyle, and should allow for flexible approaches to reducing energy intake [109]. Diets that contain 600 kcal less per day than the person needs to stay the same weight are recommended for sustainable weight loss [115]. While low-calorie diets (1,000–1,600 kcal/day) may also be considered, they are less likely to be nutritionally complete [116]. Very low-calorie diets (less than 1,000 kcal/day) may be considered for a maximum of 12 weeks continuously, or intermittently with a low-calorie diet (for example for 2–4 days a week), by people who are obese and have reached a plateau in weight loss [109]. Guidelines recommend that diets of less than 600 kcal/day should be used only under clinical supervision when there is an urgent need for weight loss [109, 113].
People are more likely to maintain a healthy weight if they reduce their consumption of energy-dense diets containing fatty and/or sugary food and drinks and follow a lower energy, high-fibre diet; consuming fewer take-away meals; eating more fruit, vegetables, and whole grains; minimising alcohol intake; and consuming less confectionery and fewer sugary drinks [117]. While there is considerable debate around which macronutrients (fat or carbohydrate) are most likely to result in excess weight gain, a recent large RCT with follow-up to 2 years concluded that reduced energy diets result in clinically meaningful weight loss regardless of which macronutrients they emphasise [118].
People should be advised to avoid concentrating on reducing the intake of one or two foods, or one particular food group, e.g. fat or sugar, since this strategy is less likely to be successful in the long term than aiming to eat a well-balanced, varied diet including all food groups in the correct proportions [109, 113].
Different types of diets have been attempted in the prevention of cardiovascular disease and, to a lesser extent, stroke, e.g. Mediterranean diet, lipid-lowering diets, low-salt diets for hypertension. These diets were designed to alter macro- and micronutrient profiles to reduce risk factors and were not necessarily designed for weight loss. However, in controlling the intake of macronutrients, weight loss often accompanies any changes in risk factors such as reduced blood pressure and altered blood lipid profile [119].
Some people may prefer a commercial weight-loss programme such as Weight Watchers, although the effectiveness of these programmes is difficult to assess, since they vary widely in content, presentation, timing, and venues. Furthermore, drop-out rates can be very high [120]. However, programmes that emphasise realistic goals, gradual progress, sensible eating, and exercise can be very effective for some people [109, 113].
Physical Activity
There is consistent evidence that interventions combining diet and physical activity are more effective for weight loss than diet alone [109, 113]. People who have had a stroke should be encouraged to increase their physical activity as much as is safely possible, even if they do not lose weight as a result, because of the other health benefits physical activity can bring, such as reduced risk of type 2 diabetes and cardiovascular disease.
Recent guidelines [121] recommend that adults should be encouraged to do at least 30 min of moderate-intensity physical activity on 5 or more days a week. The activity can be in one session or several lasting 10 min or more. Moderate-intensity activity usually increases a person’s breathing rate and heart rate and makes them feel warm, and includes activities such as brisk walking, cycling, gardening, house cleaning, golf, and racquet sports.
To prevent obesity, most people should be advised they may need to do 45–60 min of moderate-intensity activity a day, particularly if they do not reduce their energy intake [121]. People who have been obese and have lost weight should be advised they may need to do 60–90 min of physical activity a day to avoid regaining weight [121].
Adults should be encouraged to build up to the recommended levels of physical activity for weight maintenance, using a managed approach with agreed goals. Any activity should take into account the person’s current physical fitness and ability. While guidelines recommend that people should be encouraged to reduce the amount of time they spend in sedentary activities such as watching television or using a computer [109, 113], and should be supported and encouraged to try other activities that may be locally available, e.g. community walking groups, gardening schemes, or dog walking, there is currently a lack of evidence to support this strategy.
Behavioural Interventions
Evidence suggests the combination of behavioural interventions with diet and exercise results in an even greater weight reduction than either intervention alone, and thus weight management programmes should include behaviour change strategies to increase people’s physical activity levels or decrease inactivity and improve eating behaviour with regard to the quality of the person’s diet and energy intake [109].
Behaviour therapy usually focuses on what and how much a person eats and may involve asking the patient to keep a food diary to help them better understand the nutritional content of foods. It may also involve changing grocery-shopping habits, timing of meals, or advising the person to slow down the rate at which they eat. The behaviour programme may also explore how a person responds to food, in an attempt to understand what psychological issues may underlie a person’s eating habits. For example, one person may binge eat when under stress, while another may use food as a reward. In recognising these psychological triggers, an individual can develop alternative coping mechanisms that do not focus on food. Involving family members (usually spouse/partner) in behavioural treatment programmes is generally more effective for weight loss than targeting the overweight individual alone [109].
Pharmacological Interventions
Drug treatment should be considered only after dietary, exercise, and behavioural approaches have been attempted and have failed to achieve the desired weight loss, or for those people who have reached a plateau on these interventions [109]. Currently, only one drug is specifically licensed for use in the treatment of obesity in the UK (Orlistat, Roche, Switzerland). A meta-analysis of 15 RCTs found that this drug, in combination with a weight-reducing diet, was more effective for weight loss maintenance than placebo and diet at 12 months. At the same time, use of Orlistat was associated with small decreases in total cholesterol, %Hb1Ac and both systolic and diastolic blood pressure [109]. Since Orlistat reduces the absorption of energy-dense fat by inhibiting pancreatic and gastric lipases, it is associated with increased rates of gastrointestinal symptoms that are usually mild and transient.
When drug treatment is prescribed, arrangements should be made for appropriate health-care professionals to offer information, support, and counselling on additional diet, physical activity, and behavioural strategies, and information on patient support programmes should also be provided [109]. Regular review is recommended to monitor the effect of drug treatment and to reinforce lifestyle advice and adherence.
If there is concern about the adequacy of micronutrient intake, a supplement providing the reference nutrient intake for all vitamins and minerals should be considered, particularly for vulnerable groups such as older people (who may be at risk of malnutrition) [109].
Surgical Interventions
Overall mortality is 29–40 % lower in the 7–10 years after surgery in patients receiving bariatric surgery compared with BMI-matched subjects not receiving surgery [122]. Bariatric surgery is therefore recommended as a treatment option for people with obesity if all of the following criteria are fulfilled [109]:
-
BMI ≥40 kg/m2, or 35–40 kg/m2 in the presence of other significant disease that have the potential to be improved by weight loss, e.g. type 2 diabetes or high blood pressure.
-
All appropriate non-surgical measures have been tried but have failed to achieve or maintain adequate, clinically beneficial weight loss for at least 6 months.
-
The person has been receiving or will receive intensive management in a specialist obesity service and the person recognises the need for long-term follow-up.
-
The person is generally fit for anaesthesia and surgery.
Regular, specialist postoperative dietetic monitoring is recommended [109], and should include information on the appropriate diet for the bariatric procedure; monitoring of the person’s micronutrient status; and individualised nutritional supplementation, support, and guidance to achieve long-term weight loss and weight maintenance. Patients may also benefit from information on national or local patient support groups.
Monitoring and Evaluation
Weight loss is very difficult to achieve in the long term, therefore most patients will require medium- to long-term monitoring, encouragement, and support [123, 124]. Monitoring should include records of weight change and changes in waist circumference [109, 113] and may include measurements of changes in body composition, e.g. fat mass and lean body mass, although current national guidelines do not recommend routine use of bioelectrical impedance analysis to achieve this [109]. An increase in physical activity level together with changes in diet will make it easier for people to alter their body composition in a positive way, i.e. increase lean body mass and decrease fat mass.
Perhaps more importantly, clinicians should monitor the impact of multi-component interventions on changes in risk factors such as hypertension (may respond to dietary salt reduction), blood lipid profile (may respond to changes in diet although people are more likely to receive statins), and blood glucose (will respond to changes in diet).
Changes in dietary intake can be assessed using a variety of methods, including 24-h dietary recall, 5-day dietary diary, or weighed food intakes [58], although it should be recognised that each method has its strengths and weaknesses and requires specialist training in order to obtain an accurate assessment of intake. Clinicians should also remember that people who are overweight or obese are those who are most likely to under-report dietary intake, particularly the energy and fat components of the diet, as well as other nutrients they perceive to be “bad” [125].
The Obesity “Paradox”
In stroke populations it has been shown that those with low BMI (<20 kg/m2) are more likely to suffer poor outcomes than those with a higher BMI, and indeed those who are overweight or obese have even better outcomes than those in the desirable range for BMI [126–129]. This paradoxical association between BMI and mortality after stroke is most effectively demonstrated in a large cohort study in Denmark using data collected as part of a national stroke registry [126]. In this study of 13,242 individuals, mortality was higher in underweight patients (i.e. BMI <20 kg/m2) compared with those who were in the healthy range BMI (i.e. 20–25 kg/m2), overweight (BMI 25–30 kg/m2), obese (BMI 30–35 kg/m2), or severely obese (BMI >35 kg/m2) [126]. More recently, a prospective study of 543 patients designed to examine the impact of BMI on outcomes post-stroke showed that those with BMI less than 18.5 kg/m2 (underweight) were more than twice as likely to die at 6 months than those who were overweight or obese [129]. In this study it was also shown that there were no significant differences in stroke recurrence rates between BMI categories at 6 months post-stroke (BMI <18.5 kg/m2 = 3.7 %; healthy BMI = 3.8 %; overweight = 4.5 %; obese = 2.8 %; p = 0.91).
This better survival of overweight and/or obese patients (and increased mortality of underweight patients), observed in both ischaemic and haemorrhagic strokes, suggests that weight management strategies targeting the optimal BMI range used for the healthy population may require further evaluation and individualisation in the secondary prevention of strokes. In the future, it would be important to evaluate other indicators of nutritional status and distribution of body fat, such as waist circumference, in order to explore this paradox and its effect on stroke recurrence and mortality.
Dysphagia
Swallowing
The process of swallowing has been described as the most complex of “all or non-reflex” [130, 131]; however, although the pharyngeal swallow is a basic reflex, feedback regarding bolus size and viscosity emanating from afferents in the mouth and pharynx [132] regarding bolus size and viscosity via the cortex will modify timings of various components of the swallow.
A normal swallow is difficult to define, but essentially it is a series of sequential coordinated events that ensures a safe passage of food or liquid from the mouth to the stomach [133]. As food is brought from the plate or cup towards the mouth, preparation to swallow begins.
There are essentially three functions to the oro-pharyngeal swallow. These are bolus preparation, airway protection (trachea and nasal), and bolus passage through the pharynx to the oesophagus; and three swallowing phases: oral, pharyngeal, and oesophageal (relaxation of the upper oesophageal sphincter). The relationship between these phases of timing and duration is dependent to some degree on bolus characteristics.
Bolus Preparation/Oral Phase
The oral phase of swallowing is under volitional control, in that it is personal choice how long food is chewed before the bolus is gathered together and transferred to the back of the mouth; this will be influenced by bolus viscosity, texture, volume, and personal preference [134, 135].
As the bolus approaches the lips, the hyoid bone moves forward and up pulling the larynx up against the base of the tongue [136, 137]. Once the bolus has been placed in the oral cavity, lips are closed; the bolus is prepared for swallowing, by chewing and mixing with saliva in the case of a solid bolus (e.g. meat). When ready, the bolus is collected on the tongue and trapped between the tongue and the hard palate, such that in the antero-posterior view it is said to resemble a Viking long boat. The bolus is then propelled backwards to the pharynx by a rippling movement of the tongue from anterior to posterior.
Passage Through the Pharynx
Passage of the bolus through the pharynx is not straightforward. Once the bolus has left the back of the tongue, it moves momentarily into the valleculae, before passing over or around the epiglottis [138, 139]. The bolus then divides and passes through the lateral food channels (pyriform sinus), before reforming to pass through the upper oesophageal sphincter (cricopharyngeus), which is relaxed and opened.
The movement of the bolus is not a passive phenomenon, but an active process commencing with a push from the posterior tongue, and continued with a rippling of the lateral [140] and posterior pharyngeal wall (the pharyngeal stripping wave) [141].
Airway Protection
The pharynx is an anatomical structure/“tube” that is shared by both respiration and swallowing. To swallow safely, there needs to be an interruption to the respiratory cycle [142, 143]. As a consequence, during swallowing there is a period of apnoea, followed by expiration, but this is not invariable and certainly after sequential swallowing, inhalation may occur [139]. Where apnoea is not possible, e.g. lung fibrosis, COPD, or heart failure, swallowing may be a problem, resulting in dysphagia.
Protection of the airway commences at the beginning of the swallow, with upward and forward laryngeal movement. Concurrently the false vocal cords begin to come together, followed closely by the true vocal cords and then the epiglottis. The real protection of the airway is not the epiglottis but the vocal cords. It is possible to swallow without the presence of an epiglottis [144] and in sequential swallows the epiglottis is frequently upright [139].
As the bolus moves to the back of the oral cavity, the soft palate elevates to close off the nasal passages, aided by the forward movement of the posterior pharyngeal wall (Passavant’s cushion) [133].
Commencement of the Pharyngeal Swallow
Original research had suggested that the pharyngeal swallow would commence once a bolus passed the base of the anterior faucial arches. Subsequent research has found that this is true in some cases, but for many others the swallow does not trigger until the bolus is in the pharynx itself [145, 146].
Neural Control of Swallowing
The pharyngeal swallow is triggered by the presence of the bolus in the pharynx. The exact point at which the swallow triggers is different in each person. Information regarding the bolus presence is referred to as the brainstem and cortex [147, 148] and a swallow is triggered. However, there is not one interneuron but a system of connections within the reticular formation of the medulla, near the inferior olive, which has an important role to play. At the same time, information regarding the bolus characteristics are conveyed via afferents (within cranial nerves V, VII, IX, X–XII) to the cortex, which then modulates the swallow to regulate how long the upper oesophageal sphincter remains open, the dimensions of the pharynx, and the control of respiration and airway closure [148].
Cortical control is complex and is detailed elsewhere [149], suffice to say that there is no single cortical or subcortical region that has ultimate control. The swallow is bilaterally, but asymmetrically, represented [150] within the cortex (motor cortex, supplementary motor cortex, amygdala, frontal cortex, and cerebellum). Two areas that appear to be critical for the coordination of swallowing are the nigrostriatal pathway and the anterior insula cortex. Within these areas are numerous neuro-transmitters including substance P, dopamine, and noradrenalin (see Fig. 7.1) [151, 152].
Swallowing Following Stroke
As a consequence of stroke, dysphagia will occur if the cortical pathways related to swallowing are interrupted anywhere along their path. Also, a lesion within the medulla or pons could similarly affect the ability to swallow [153, 154].
Lesion Site
Dysphagia may follow a stroke in any area/lobe of the brain, as the pathways are complex and interdependent. The occurrence and recovery of dysphagia will frequently depend on the relative dominance between the affected and unaffected hemisphere for swallowing. There has been much research investigating the lesion location, but there has been no conclusive single cortical location identified as the most relevant. Stroke within the subcortical structures, cerebellum, and brainstem may be more likely to result in dysphagia, particularly because of the close proximity of many important pathways [152].
From a cortical perspective, the occurrence of dysphagia will depend on the side of the brain affected, i.e. if the hemisphere affected by stroke is the dominant hemisphere for swallowing, then dysphagia will occur. The particular problem that occurs will depend on which area of the brain is affected. The issue may be motor, sensory, or sensorimotor. There may be a problem of coordination (stages of swallow or with respiration) or dyspraxia.
Epidemiology
Abnormalities within the swallowing system are common following stroke, and some authors have suggested that the occurrence may be as high as 100 %; however, clinically relevant problems with swallowing or dysphagia are present in 28–65 % of people during the acute phase of stroke.
Globally, 15 million people suffer a stroke annually [154], of these up to 9,750,000 (65 %) will have dysphagia. Of these, about half (4,875,000) will be aspirating, and half of these (2,437,500) silently.
The number with dysphagia reduces significantly during the early days of stroke, such that by 14 days after the stroke 90 % of people will be swallowing safely [155–157]. However, a small proportion of people will have ongoing problems for some time [152]. Some of those who appear to have returned to a safe swallow after 3 months are found to have difficulties at 6 months [154–156]. If the swallow does not show any signs of recovery in the first 10 days, it is probable that the return of a safe swallow may take between 2 and 3 months.
Swallowing recovery is dependent on neural plasticity [158–160], with either the non-affected hemisphere enlarging [43], or other cortical areas taking over, or both. Failure of the non-affected hemisphere to enlarge will result in dysphagia persisting. Hamdy and colleagues have undertaken many eloquent studies to show this, using both fMRI and transcranial magnetic stimulation [153, 162].
Aetiology of Dysphagia Following Stroke
The ability to swallow safely may have many different aetiologies/co-morbidities (many predating the stroke) that interplay; compounded by the fact that some older people will have presbyphagia, and a new physiological insult has led to a decompensation of their swallow. Frequently, medications will also have a negative impact on swallowing (Table 7.6) [163].
With increasing age, there are subtle but definite changes in swallowing, which frequently go unnoticed because of the slow onset and the gradual compensation strategies employed, i.e. smaller portions, softer consistency, or skipping courses. These changes are termed presbyphagia [164].
Many people may wear dentures or have a reduced number of teeth. Reduced numbers of teeth reduce chewing capacity, resulting in larger portions of food being swallowed [165], consequently when the swallow is compromised after stroke, this may lead to a high risk of aspiration.
For dentures to work, there needs to be good bone structure, muscle strength, and healthy gums. Many people do not wear theirs due to pain, either because the dentures do not fit (as a result of bone resorption or poor fitting), or because of infection in the gums. Following a stroke, with facial nerve palsy the muscle tone in the cheek is reduced, resulting in a failure to keep dentures in place, making hard food impossible to eat.
Many medications prescribed prior to or after stroke, such as antihypertensive medications or statins, have an anticholinergic effect [166–168]; these may result in a dry mouth, poor vision, or confusion. This may decompensate the swallow in those people whose physiological reserve is already limited. Other medications such as antidepressants, medication for incontinence (urologicals), and anti-psychotic medication have strong recognised anticholinergic effects, resulting in much the same outcome, but also causing drowsiness. Drowsiness is the commonest cause of dysphagia. Any reduction of conscious level, including sleep, results in a reduction in the frequency of swallowing and on occasion the swallow reflex stops [166, 167].
Infections such as gum disease, abscess, salivary gland infections, or candidiasis in the mouth and possibly the oesophagus may make swallowing painful and difficult. This may manifest itself as food refusal rather than any particular aspect of swallowing itself, particularly in those people with communication difficulties.
Concomitant lung disease or cardiac diseases may be associated with dysphagia, particularly in those people where breath holding is not possible, such as stage III/IV cardiac failure or end-stage lung disease [169].
Detection
Initially there is a need to determine whether someone has dysphagia or not. A screening assessment is often undertaken by nursing and medical staff. The majority of these assessments are based on that initially described by Smithard et al. [151, 156, 170].
The assessment includes a series of questions followed by a simple swallow assessment using teaspoons of water, followed by a larger volume of water (50–90 ml). The sensitivities and specificities of all swallowing screens are similar. The main purpose of these screens is to permit those people to eat and drink who are considered to be safe. The majority of screens are able to rule out aspiration risk (NPV 90 %) [171] rather than rule it in. Therefore, a safe swallow on a screen probably is.
Ramsey et al. [171] investigated the addition of a chest radiograph to the standard bedside screen/assessment. The study did not provide any conclusive results, as not enough strokes with relevant pathology could be recruited.
If the swallow screen flags up a problem with the swallow, a referral should be made to a speech and language therapist for a formal assessment, or the swallow rescreened if it is at a time when speech and language therapists are unavailable.
Assessment
The assessment of dysphagia (as opposed to the screening assessment performed at the time of stroke) is a mixture of a clinical bedside assessment by a speech and language therapist or someone trained in dysphagia management (the actual professional may depend on the country), followed, where appropriate, by instrumental investigation [46, 172]. The most frequently used investigations are video fluoroscopy [173] and fibre-optic endoscopic evaluation of swallowing (or FEES) [174].
Video fluoroscopy provides the ability to see anatomy and physiology at the same time. It is generally widely available in most hospitals but does require the use of a radiology screening suit and a radiographer. Patients are exposed to radiation, equivalent to that of a chest radiograph. FEES, on the other hand, can be done at the bedside. It requires access to a nasal endoscope and training in its use. The advantage is that it can be performed at the bedside and does not expose the patient to radiation. The main disadvantage is that the passage of the bolus cannot be followed clearly, aspiration is only seem after the event, and the oesophagus is not seen at all.
Other assessments have been used including ultrasound [174], manometry [175], and scintigraphy [176]. Frequently more than one procedure will be used, usually in combination with a workstation that permits the “swallowologist” to review all the information together.
The major concern of dysphagia is the development of aspiration, and as a consequence a chest infection (see section “Complications of aspiration” below). The risk of aspiration increases with the increasing dependency of the patient. Those who are bed-bound and require feeding by others are more likely to develop pneumonia. The major reason for aspiration pneumonia is not food or liquid directly, instead it is frequently entry of oral pathogens into the airway, either with food or saliva or both [177–179].
Complications of Aspiration
-
No obvious ill effects
-
Recurrent cough
-
Grumbling pyrexia
-
Chest infection
-
Asthma/COPD
-
Food avoidance
-
Weight loss
-
Dehydration
-
Cyanosis/hypoxia
-
Hypoxic fit
-
Airway obstruction
-
Death
There is a debate in the dysphagia world as to whether detection of aspiration is important. Undoubtedly aspiration is important, but if someone has a clinically unsafe swallow, is it important to document aspiration? Bear in mind the long-term outcome in people with clinically documented dysphagia is similar to those with aspiration.
It has been suggested that the use of technology to investigate the swallow slows down the return to oral feeding. Clinicians can be too quick to refuse people food when previously they have been managing quite successfully.
Management
The management of dysphagia post-stroke has one aim only and that is to provide a method of safely providing adequate nutrition to the patient. Where possible, the oral route is used to provide nutrition, and if this is not possible, enteral feeding is used. On occasions both will be used together.
The ability to swallow will improve over time, with the swallow returning to many people within the first 2–10 days [155, 157]. Generally there is no need to consider any intervention over the first 24–48 h (except with intravenous fluids). If the swallow has not improved by that time, and it is not possible to resume oral feeding, a nasogastric tube should be passed, with all the usual caveats regarding nasogastric feeding. On occasion there may be a clinical need for an oral route for medication, and where oral feeding is not possible, and an alternative method of delivery (transcutaneous, buccal, rectal) is not available, then a nasogastric tube may be used.
Oral Nutrition
If oral feeding is considered appropriate, then there are essentially two ways of managing a poor swallow. The first is to alter what is eaten, by changing the texture, viscosity, taste, and size of the bolus. The second is to change the anatomy/physiology by monitoring breathing, turning the head, or tucking down the chin [180, 181]. Changing the viscosity/texture of the bolus is the commonest approach to managing the swallow. This is despite some counselling against the use of thickeners [182].
The role of the speech and language therapists (pathologist) is to reduce the risk of aspiration and improve swallowing function to allow a safe ingestion of food and liquid [183]. This is achieved by using posture changes (chin tuck, head turning) or swallow manoeuvres (breath holding, effortful swallow) to alter the physiology of swallowing.
Carnaby et al. compared usual care with three times weekly and daily swallowing therapy for 1 month [181]. Those with daily therapy were more likely to regain their swallow (p = 0.02) and be eating a normal diet (p = 0.04). The incidence of chest infection was reduced.
The literature supports the use of swallowing manoeuvres and postural movements for some patients [184, 185]. Head turning or chin tuck has shown benefit in 67 % and 77 %, respectively, reducing aspiration with some bolus consistencies [186] and increased the size of the bolus that could be swallowed [185]. Manometric studies have not been able to support the clinical findings [187]. McCullough and Kim, studying the Mendelsohn manoeuvre, noted some clinical benefit, but found that in stroke patients fatigue was a problem, particularly with older patients [187]. However, the evidence is limited due to the size of the studies, and that often studies are of mixed aetiologies [188, 189]. Similarly requesting change in eating or drinking speed may prove a problem, particularly in older patients, due to changes in oral sensorimotor function and in the ability to fully monitor the bolus characteristics [190].
Bolus Modification
The mouth and pharynx are full of sensory receptors that provide input into the cortex to modify the pharyngeal swallow. Bolus temperature, viscosity, volume, and taste can modulate the swallow [191], and hence can be used in the management of dysphagia.
Taste
Chee et al., studying healthy adults, suggested that the swallow is highly influenced by chemical-sensorial stimuli, with sweet and sour eliciting the shortest oral preparatory phase [191]. Sour taste may elicit a strong submental muscle contraction which could be beneficial with rehabilitation. Similarly bitter tastes produce a longer oral preparatory phase, which may provide longer for pharyngeal protection and should be explored in the realms of rehabilitation [191]. A study by Cola et al. has suggested that the use of (cold) sour tasting foods can shorten the duration of pharyngeal transit, though further work is still required in this area [192].
Rheology
Rheology is often interpreted as referring to the viscosity of a liquid; however, it is a term to describe the mechanical properties of liquid in its totality [193, 194]. Bolus size and consistency, with a normal swallow, is a major determinant on the duration of the swallow. Sensory feedback to the cortex via the mouth and pharynx regarding bolus characteristics will determine how long the larynx is elevated and the relaxation of the upper oesophageal sphincter [195, 196].
Oral/tongue deficits require, in many cases, a thicker bolus to promote bolus cohesiveness, whereas pharyngeal paresis/slow transit and pooling may require a thinner consistency. Clavé et al. found that increasing bolus consistency in those oral preparatory problems reduced the risk of laryngeal penetration and aspiration (39.5 % vs 26.3 %) [195]. Hamdy et al. examined the effect of bolus pH and temperature on the swallow [193]. Cold water with citric acid added slowed the swallow significantly. Although the texture and size of a bolus are frequently changed to support oral feeding in the clinical setting, little work has been done in anything other than water [197, 198].
Although increasing the viscosity of liquids with thickening agents (based on starch or guar gum) may reduce aspiration risk, due to their consistency and palatability, patients requiring thickened fluids are less likely to meet fluid requirements [82].
Modified-Texture Diets
As the rheology of liquid can affect the swallow, so can the consistency of food. The speech and language therapist may recommend following an assessment of the swallow, a change in the consistency of food and the rate that it is delivered to the patient.
Once the consistency of a food has to be changed, the palatability of the food may be reduced [199], and the nutritional content may be poor [83, 84, 199, 200]. It is not unknown for relatives/carers to provide people with pre-prepared baby food with all the nutritional risks that this entails. Modern techniques involved with preparing food for people with dysphagia should bypass many of these problems and may markedly increase intake and hence nutritional status.
Tube Feeding
Enteral feeding, either by the nasogastric route or the gastrostomy route, does not prevent aspiration pneumonia occurring, as the most common reason is the aspiration of oro-pharyngeal secretions. As a consequence, good mouth care in the presence of enteral feeding is essential. Those fed via gastrostomy may suffer with reflux; this can be treated with either proton pump inhibitors and or pro-kinetic agents.
Nasogastric tubes are usually the primary route for enteric feeding used for short-term feeding (usually less than 4 weeks) in those who are either nil by mouth due to unsafe swallow, or who require supplementary feeding due to inadequate oral intake. Gastrostomy feeding is commonly used for long-term feeding following a stroke. A recent review by Gomes et al. for the Cochrane Library has suggested that percutaneous endoscopic gastrostomy (PEG) feeding is probably safer and more effective than nasogastric tube feeding in the longer term [198].
Nasogastric Tube
For a long time the consensus view has been that the presence of a nasogastric (or orogastric) tube inhibits a normal swallow [200–202]. This no longer holds true, and the use of such tubes may assist in rehabilitation due to the provision of nutrition [203].
Nasogastric tubes are frequently not tolerated [204] for a variety of reasons (see section “Complications of nasogastric tube placement” below). Where a nasogastric tube needs to be repeatedly replaced, a method of restraint may need to be considered, the most common of which is the nasal loop in the UK [205]. The use of constraints carries moral and ethical connotations which are discussed later.
Nasogastric tube placement is not a begin procedure, and the risk of complications has to be considered. The misplacement of a nasogastric tube is considered a never event by the Patient Safety Agency and as such, care has to always be exercised in its placement, as food in the wrong place could be fatal.
Complications of Nasogastric Tube Placement
-
Recurrent placement
-
Nasal ulceration
-
Poor tube placement/wrong placement
-
Food sticking to the nasogastric tube
-
Increased pharyngeal secretions
-
Feed failure
-
Oesophageal reflux
-
Placement in the lung
-
Oesophageal perforation
-
Aspiration
-
Poor body image
Percutaneous Endoscopic Gastrostomy (PEG)
Over the last few years, PEG feeding has become the enteral feeding route of choice for long-term feeding, as there is more certainty over feed success and compliance with feeding regimens [206–208]. What is not certain is whether the use of PEGs improves the swallow, or that the swallow improves as part of the general improvement seen after their placement due to nutritional benefit [209, 210].
Gastrostomy tubes pass through the abdominal wall directly into the stomach. They are usually used for patients who require medium- to long-term feeding, or where passing and or retaining a nasogastric tube is difficult. The most common route for the placement of gastrostomy tubes is endoscopically (PEG) but they can also be placed radiologically or as a last resort, surgically. Many percutaneous jejunostomy tubes are placed endoscopically or radiologically via gastric puncture with an extension through the pylorus into the duodenum or jejunum (PEG-Jejunostomy).
Timing of Placement
The paper by Hussein suggests that if the swallow has not returned or is not returning within 10 days, it may take 70 days or longer for the swallow to return for oral feeding. As a consequence, a gastrostomy should be sited somewhere between 2 and 4 weeks post-stroke [46, 47, 208]. Gastrostomy placement is an operation that requires consent, and as such, the risks and complications have to be explained. Major complications are not common but can be serious and rarely fatal (Table 7.7).
Behavioural Techniques
Behavioural techniques often utilise biofeedback as part of the treatment package. Biofeedback may take many forms, but essentially they provide the patient and therapist with cotemporaneous information of their performance of the intervention task.
Biofeedback is used in conjunction with other methods of swallowing therapy. Logemann et al. reported a case study using indirect biofeedback with pharyngeal swallowing manoeuvres [211]. Over the years, different researchers have experimented with the use of biofeedback in conjunction with surface EMG [212, 213] and video endoscopy [214], accelerometry [215], and neck transducers [216].
Tongue Exercises
To move the swallow from the front of the mouth to the back relies on the movement of the tongue in relation to the palate and the pressures exerted during this procedure. Steele et al. have noticed that this is different between different viscosities and textures [217, 218]. With age, skeletal muscle quality may change and there may be a consequent reduction in isometric and swallowing tongue strength [219, 220].
Robbins et al. studied tongue strength in older people and found that an 8-week progressive resistance regimen improved swallowing pressures and increased muscle volume by 5 % [219]. Similarly, Lazarus et al. found that by using the IOWA Oral Performance Instrument there was a significant increase in tongue strength [220]. Clark et al. in a slightly larger cohort (39 adults) found similar results after 9 weeks directional training [221]. Robbins et al. found improvement in tongue strength and improved swallowing (timings and residue remaining) [222] and less aspiration in a small cohort (Martin-Harris et al.) of stroke patients with dysphagia.
Shaker Exercises
The Shaker exercise programme consists of a series of head-raising exercises whilst lying flat on the bed or floor. Three head raises are sustained and followed by a series of 30 repetitive head raises. The exercise strengthens the suprahyoid muscles, resulting in improved upper oesophageal opening, laryngeal anterior excursion, and a reduction in post-swallow aspiration. In a small study of 27 people in 2002, Shaker and colleagues demonstrated that those in the treatment arm were able to resume swallowing; videofluoroscopy was the gold standard assessment [223]. Logemann et al., in a small multi-centre study (19 patients) that was beset with problems, noted that the Shaker and traditional therapy produced similar results but by different mechanisms [224]. They concluded that the traditional exercises (Mendelssohn Manoeuvre) should be used where there are neck problems. A further small study [225] of 11 patients showed that the Shaker exercise resulted in an increase of thyro-hyoid shortening after 6 weeks compared to traditional exercises involving tongue exercises and swallow manoeuvres. Where it is not possible to perform the Shaker exercise, Yoon et al. have suggested that chin tuck against resistance offers the same benefits [226].
McNeill Dysphagia Training Program (MDTP)
The MDTP uses the act of swallowing as an exercise incorporating a hard swallow [183, 227]. The main thrust of the programme is to rebuild functional patterns of swallowing. During the programme, a patient is moved up or down the ladder of treatment of increasing resistive forces and alterations in movement velocities, timings, and movement specificity of the swallowing activity. Small case series have suggested that the MDTP is superior to standard therapy with sEMG. However, the studies are all a mixed case series and are not stroke specific [228, 229].
Surface Electromyography (sEMG)
sEMG is the recording of electrical activity within muscles. It has been advocated as an adjunct to swallowing therapy. Crary et al. reviewed the charts of 25 stroke patients who had dysphagia for a mean of 24.8 months and found that after a period of therapy that there was a 92 % increase in oral intake with a mean improvement of 2.96 on the Functional Oral Intake scale [228]. Bogaardt et al. found improvement in all 11 subjects to varying degrees [229]. Apart from a standard use of sEMG for varying periods of time (mean seven sessions), different swallowing therapy was used (Mendelsohn, Shaker exercises).
Faucial Stimulation
Lazzara et al. studied a mixed group of neurologically impaired individuals [230]. Results suggested that there was a decrease in the oral and pharyngeal transit times. Power et al., studying stroke patients only, were unable to replicate these findings, and instead noted that stimulation of the faucial arches at a frequency of 5 Hz increased the swallowing response time by 114 %, whereas 10 Hz inhibited the swallow [231, 232]. This suggests that the relationship is far more complex than initially realised, which is borne out by the variability of the triggering of the swallow between individuals.
Neuromuscular Electrical Stimulation (NMES)
Neuromuscular electrical stimulation (NMES), usually trans-cutaneously, is of interest as it is potentially a non-invasive way of retraining the swallow. The whole basis of the treatment is to stimulate innervated healthy muscle recruiting fibres to cause a contraction. If the stimulation is used to augment a functional activity, then it is referred to as Functional Electrical stimulation. NMES in the case of swallowing involves the placing of electrodes on the skin over the larynx, and during the swallow and using the muscle stimulation of the hyoid muscles, to cause the larynx to elevate. There are many individual muscles in this area; intramuscular stimulation has noted that the thyro-hyoid is more closely related time wise to the laryngeal elevation than the myelo-hyoid [213, 233, 234].
Transcutaneous stimulation is unable to attain this degree of accuracy. In a meta-analysis of seven studies, Carnaby-Mann et al. found a small but positive effect for this intervention [213]. In 2009 Clark et al. recommended that further studies were required as no high-quality randomised trials existed [234]. Studies by Shaw and Bülow have noted positive effects with NMES [235, 236]. Permsirivanich et al., in a single-blind randomised study, compared rehabilitation swallowing therapy (diet modification, oral motor exercises, thermal stimulation, and swallowing manoeuvres) to NMES therapy (diet modification, oral motor exercises, and NMES) [237]. Both groups showed an improvement in swallowing using the Function Oral Intake score, by three to four levels; however, there was an absolute benefit in the NMES arm by 10 % (81 % vs. 91 %). The difference in mean change was significant at the p < 0.001.
There is increasing evidence that NMES does have a place in swallowing treatment, but as Ludlow et al. noted in their review, it is beneficial for a small group of mild to moderate dysphagia rather than severe dysphagia [238].
Pharyngeal Stimulation
Swallowing, although reflexic, is highly dependent on sensory feedback [237, 239]. This feedback provides information regarding bolus characteristics. Fraser et al. and Hamdy et al. have shown that stimulation of the pharynx will produce changes in the cortex lasting up to 30 min [240]. However, the peak excitation of pharyngeal swallow is later than that usually produced by a volitional swallow, suggesting that the maximal benefit of pharyngeal stimulation would be achieved in conjunction with volitional swallowing exercises. Jayasekeran and colleagues further investigated this effect in people with acute stroke [241]. One treatment each day produced improved airway protection compared with controls (P = 0.038). Active PES also reduced aspiration, improved feeding status [237, 239], and resulted in a shorter time to hospital discharge [242].
Pharmacological Interventions
Swallowing is complex, with several sites of intervention, including the cerebral hemispheres/lobes, brainstem, and topically. A topical theory is that depletion of substance P in the pharyngeal plexus as well as centrally results in a disordered pharyngeal swallow. Several papers [242, 243] have suggested that ACE inhibitors can reduce aspiration and the incidence of aspiration pneumonia. Capsaicin will act topically on the pharynx. Recent work by Rofes et al. has shown an increase in the vertical movement of the larynx with capsaicinoids by way of the TRPV1 receptor, reducing laryngeal penetration by 50 % (p < 0.05) and pharyngeal residue by 50 % (p < 0.05), and shortened the time of laryngeal vestibule closure (p < 0.001), upper oesophageal sphincter opening (p < 0.05), and maximal hyoid and laryngeal displacement [244]. Rofes et al., using Piperine acting via the TRPV1/A1 receptor in the pharynx, noted a 35 % (150 μM) to 57 % (1 mM) reduction in unsafe swallows (reduced time to laryngeal closure) and a consequent reduction in the severity score of the penetration-aspiration scale [245].
Perez et al. found improvements in pharyngeal transit times (a mean reduction of 1.34 s, 95 % CI −2.56, −0.11) and a reduction in swallow delay of 1.91 s (95 % CI −3.58, −0.24) using Nifedipine controlled release in a crossover design study [245–246].
These studies would suggest that the pharynx hosts an array of receptors, which can be utilised to assist in the recovery of the swallow. It is possible that all medications are acting via a final common pathway, which may be substance P, or calcium channels, or both.
Acupuncture
Li et al. and Zou et al. suggest that acupuncture following stroke may be beneficial in swallowing recovery [247, 248]. In the 2008 Cochrane review, Xie and colleagues concluded that there was not enough evidence to support the use of acupuncture for the treatment of dysphagia in acute stroke [249]. Long and Wu, undertaking a meta-analysis of 72 RCTs enrolling a total of 6,134 patients, report that the treatment with acupuncture with usual treatment was more effective than usual treatment (OR 5.17, 95 % CI 4.18–6.38) [250]. They do acknowledge that in the majority of the trials there were questions regarding methodology and randomisation, but conclude further studies are needed.
Orthoses
Selley and colleagues reported the use of a palatal training device, essentially a wire loop attached to the plate of a full denture, that supports the soft palate. In 37 stroke patients, of the 23 that survived, 22 were taking adequate oral diets [251].
Surgery
Surgical techniques for the management of aspiration are not new, with publications being prevalent in the 1970s. Brooks and McKelvie published a case review of a patient who underwent an epiglottoplexy for intractable aspiration [252]. This involves subtotal closure of the larynx by fixation of the epiglottis. The report suggests that the airway is maintained, speech preserved, and aspiration abolished. Cricopharyngeal myotomy has been suggested by some authors, where there is a lack of relaxation of the cricopharyngeus or upper oesophageal sphincter resulting in pooling. The results are mixed, though some have found good results [253].
Other surgical techniques such as laryngeal suspension, laryngeal closure, or diversions have been employed in the field of head and neck cancer. Total laryngectomy and tracheostomy have both been used in the past, and have limited or no role in the management of dysphagia following stroke, though may retain some use in neuromuscular disorders such as motor neuron disease.
Outcome Measures
The question that needs to be asked regarding swallowing studies: Are the right questions being asked, and are the right things being measured? It is always useful to know what the physiology is and whether an intervention improves this. But the end result is an improvement in swallowing, and hence quality of life. Changes to physiology do not matter if there is no change clinically.
The Dysphagia Outcome Severity Scale [254], SWALQOL [255], and Functional Oral Intake Scale [256] are useful measures in the clinical situation, as they permit the clinicians to speak a common language. All studies using patients should use these scales or a common scale so that results can be pooled. Researchers in the dysphagia field need to think about a common minimum data set, and there needs to be a push towards randomised trials. A common minimum data set would permit the combining of the results of similar studies to provide a more powerful answer than a single study alone.
Long-Term Outcome
Dysphagia is an independent predictor of outcome [157], including mortality, length of hospital stay after the acute event, and admission to long-term care. Smithard et al. found using the South London Stroke Register the largest effect exerted is in the first year, but that there is an increase in admissions to care homes at approximately 4–5 years [257]. Further work is needed to investigate the factors underlying this.
Ethical Issues
There are many difficult and contentious issues around the provision of nutrition. The main question is “whether to provide nutrition is appropriate or not”? Generally enteral nutrition is seen as a medical treatment. Consequently, it can be stopped and started along the lines of any medical treatment [258]. If there is doubt, a 2-week trial of enteral feeding should be attempted with outcomes monitored.
The question that needs to be asked: Is this long enough, and what improvements are expected in this time? What is clear is that no food equates, eventually, to no life. The decision to provide nutrition or not must not be taken lightly and must be done on an individual case-by-case basis after full discussion with all parties involved, including the patient if they are competent.
There are two further issues that frequently tax clinicians; first is that of the person who wants to eat and drink, but whose swallow is unsafe, putting them at high risk of aspiration. The compliance with instructions/advice may depend on the food consistency, with less compliance being demonstrated with thickened fluids [259]. Providing the patient is cognitively intact and is deemed to have mental capacity, and after explaining all the risks that eating and drinking entails, they should be allowed to eat and drink. If capacity is an issue, a similar discussion should be had with their representative/advocate.
The second scenario is of someone who is capable of swallowing and is able to meet their own needs but refuses to swallow. This case scenario is difficult and very burdensome on all formal and informal carers. Restraint and forced provision of nutrition will only work whilst it is being administered, with the original position rapidly returning. In a patient with mental capacity, this is not an option in some countries [260].
The use of restraints is not encouraged, as frequently they do not influence the long-term outcome or prognosis of the patient. Where restraint is being used, it should be used for the minimum period of time after seeking legal advice. Where possible, the person with swallowing difficulties should make the decision regarding swallowing and compliance, as part of the informed consent process, and capacity is autonomy. In short a competent patient has the right of self-determination, so long as no one else is harmed [261].
Who makes the decision and the appropriateness of a decision is always difficult. Although a proxy may have been appointed to make a medical decision, research has shown that their decision and that of the person they are acting for are, in the majority of cases, not congruent [262].
Whatever decisions are taken, it is essential that communication is paramount, to ensure that all carers (formal and informal) are aware of the plan of care; a framework may need to be implemented when the person and professionals do not agree on the best treatment.
Conclusion
Malnutrition and swallowing problems are common after stroke and frequently occur together. Failure to recognise their presence will result in increased morbidity and mortality. Patients admitted to hospital following a stroke may already be malnourished or at risk of malnutrition, and people often become more malnourished while they are in hospital. Recovery and rehabilitation will be slowed, infection risk may be elevated, and people will be more likely to end up in long-term care.
Since malnutrition and swallowing are associated with poor outcomes and can persist for many months post-stroke, monitoring of nutrition and swallowing status needs to be regular and consistent, and may need to continue into the care home environment and in those living at home. Consequently, the issues need to be raised with all care staff/professionals, and treatment of malnutrition and swallowing difficulties requires input from the MDT.
Patient Questions
-
Q. During admission to hospital with a stroke, weight loss may occur. What are the reasons behind this and what can be done to ameliorate any malnutrition?
-
A. Weight loss may be due to many reasons. An acute illness is often associated with an increase in metabolic rate and protein metabolism, but is also accompanied by a decrease in physical activity such that total energy expenditure is not usually elevated above that expected for a healthy person of the same age and gender. Malnutrition (accompanied by weight loss) can occur gradually over time, e.g. due to social reasons such as isolation, poverty, lack of support, or psychological reasons such as depression. Malnutrition can be caused, or exacerbated, by stroke, e.g. due to altered consciousness, anorexia (common in acute illness), oral pain due to infection, psychosis and mistrust, bland taste (food or medication), or the presence of swallowing problems. Malnutrition following illness can take many months to correct, especially if there are also social or psychological reasons why intake may be compromised.
The correct management is to identify the underlying problem and correct it. A dietician referral should be made whenever nutrition is poor, swallowing is a problem, or there is weight loss. A dietician can advise on the provision of the correct amount of nutrients (not just energy) using snacks, food fortification, oral nutritional supplements (also known as sip feeds), or supportive enteral feeding. If the underlying problem is dysphagia, this needs to be identified. A referral to the speech and language therapist needs to happen to determine the correct method of feeding and food consistency.
-
Q. What are the dangers associated with poor nutrition?
-
A. For any biological system to function, energy and other nutrients such as protein, vitamins, and minerals are required. The lack of adequate nutrition will eventually result in organ and system shutdown and failure. Lack of nutrition will result in muscle and protein loss, increased risk of infection, increased risk of pressure ulcers, weight loss, and eventually death. Re-feeding after a period of poor nutrition is associated with ion shifts, in particular potassium, calcium, and magnesium. These can result in cardiac arrhythmias and the risk of gastrointestinal dysfunction and epileptic fits. The key to avoiding re-feeding syndrome is prevention by ensuring nutrition is introduced slowly, together with daily monitoring of calcium, electrolytes, glucose, and magnesium.
For the individual there are adverse impacts on mobility, mood, quality of life, function, and activities of daily living. For health and social care providers, there is the added cost of managing malnourished individuals who are more likely to need to visit their GP, be hospitalised, and need care home placement or a package of care on hospital discharge.
-
Q. How do you assess whether someone is malnourished, and its causes after stroke?
-
A. A significant proportion of people admitted with stroke will be already malnourished. The aetiology of this may be as simple as someone on a diet, but may be associated with an underlying malignancy, pre-existing dysphagia, lack of teeth, medication causing a dry mouth, or sore mouth due to oral candidiasis.
Everyone admitted with stroke needs to be screened for nutritional risk using a validated nutrition screening tool. Anyone identified as at risk or malnourished should be referred for a full nutritional assessment by a nutrition specialist such as a dietician. The assessment will include the following components: body mass index, history of weight change, review of laboratory data, review of clinical condition (including ability to swallow safely), dietary assessment, and consideration of relevant environmental factors (whether in hospital, care home, or at home). Enquire about change of appetite, fatigue, and medication that may cause a dry mouth or change taste perception. Dysphagia may be assessed by using a bedside water screen or just observing someone eat and drink. Remember that a low conscious level is the commonest cause of dysphagia.
References
Elia M. Guidelines for detection and management of malnutrition: a report by the Malnutrition Advisory Group of the British Association for Parenteral and Enteral Nutrition (BAPEN). Maidenhead: BAPEN; 2000.
Jensen GL, Mirtallo J, Compher C, International Consensus Guideline Committee, et al. Adult starvation and disease-related malnutrition: a proposal for etiology-based diagnosis in the clinical practice setting from the International Consensus Guideline Committee. J Parenter Enteral Nutr. 2010;34(2):156–9.
World Health Organisation, Obesity and overweight. Fact sheet N°311. Updated Aug 2014.
Keys A, Brozek J, Henschel A, et al. The biology of human starvation. Minneapolis: University of Minnesota Press; 1950.
Hickson M, Frost GS. An investigation into the relationships between quality of life, nutritional status and physical function. Proc Nutr Soc. 2004;63:30A.
Stratton RJ, Green CJ, Elia M. Disease-related malnutrition: an evidence-based approach to treatment CAB International. Wallingford: Oxon; 2003. OX10 8DE UK.
National Collaborating Centre for Acute Care. Nutrition support in adults oral nutrition support, enteral tube feeding and parenteral nutrition. London: National Collaborating Centre for Acute Care; 2006. Available from www.nice.org.uk/guidance/cg32.
Guest JF, Panca M, Baeyens JP, et al. Health economic impact of managing patients following a community-based diagnosis of malnutrition in the UK. Clin Nutr. 2011;30(4):422–9.
Elia M, Stratton RJ. Calculating the cost of disease-related malnutrition in the UK in 2007. In: Elia M, Russell CA, editors. Combating malnutrition: recommendations for action. A report from the Advisory Group on Malnutrition led by BAPEN. Redditch: BAPEN; 2009.
Carers UK. Malnutrition and caring. The hidden cost for families. 2012. Available from: http://www.shapingourlives.org.uk/documents/UK4049Malnutritionandcaring.pdf.
Elia M. The “MUST” report. Nutritional screening of adults: a multidisciplinary responsibility. Redditch: The Malnutrition Advisory Group of the British Association for Parenteral and Enteral Nutrition; 2003.
Russell CA, Elia M. Symposium 2: the skeleton in the closet: malnutrition in the community. Malnutrition in the UK: where does it begin? Proc Nutr Soc. 2010;69:465–9.
Russell CA, Elia M, on behalf of BAPEN and collaborators. Nutrition screening survey in the UK and Republic of Ireland in 2010. A Report by the British Association for Parenteral and Enteral Nutrition (BAPEN). Hospitals, care homes and mental health units. Redditch: BAPEN; 2010. http://www.bapen.org.uk/pdfs/nsw/nsw10/nsw10-report.pdf.
Foley NC, Salter KL, Robertson J, et al. Which reported estimate of the prevalence of malnutrition after stroke is valid? Stroke. 2009;40:e66–74.
Finestone HM, Greene-Finestone LS, Wilson ES, et al. Malnutrition in stroke patients on the rehabilitation service and at follow-up: prevalence and predictors. Arch Phys Med Rehabil. 1995;764:310–6.
Dávalos A, Ricart W, Gonzalez-Huix F, Soler S, Marrugat J, Molins A, Suñer R, Genís D. Effect of malnutrition after acute stroke on clinical outcome. Stroke. 1996;27(6):1028–32.
Davis JP, Wong AA, Schluter PJ, Henderson RD, O’Sullivan JD, Read SJ. Impact of premorbid undernutrition on outcome in stroke patients. Stroke. 2004;35(8):1930–4.
Dennis MS, Lewis SC, Warlow C. FOOD Trial Collaboration. Routine oral nutritional supplementation for stroke patients in hospital (FOOD): a multicentre randomised controlled trial. Lancet. 2005;365(9461):755–63.
Crary MA, Carnaby-Mann GD, Miller L, Antonios N, Silliman S. Dysphagia and nutritional status at the time of hospital admission for ischemic stroke. J Stroke Cerebrovasc Dis. 2006;15(4):164–71.
Martineau J, Bauer JD, Isenring E, Cohen S. Malnutrition determined by the patient-generated subjective global assessment is associated with poor outcomes in acute stroke patients. Clin Nutr. 2005;24(6):1073–7.
Yoo SH, Kim JS, Kwon SU, Yun SC, Koh JY, Kang DW. Undernutrition as a predictor of poor clinical outcomes in acute ischemic stroke patients. Arch Neurol. 2008;65(1):39–43. doi:10.1001/archneurol.2007.12.
Guigoz Y, Vellas B, Garry PJ. Assessing the nutritional status of the elderly: the mini nutritional assessment as part of the geriatric evaluation. Nutr Rev. 1996;54(1 Pt 2):S59–65.
Baker JP, Detsky AS, Whitwell J, Langer B, Jeejeebhoy KN. A comparison of the predictive value of nutritional assessment techniques. Hum Nutr Clin Nutr. 1982;36(3):233–41.
The FOOD Trial Collaboration. Routine oral nutritional supplementation for stroke patients in hospital (FOOD): a multicentre randomized controlled trial. Lancet. 2005;365:755–63.
Mead GE, Donaldson L, North P, Dennis MS. An informal assessment of nutritional status in acute stroke for use in an international multicentre trial of feeding regimens. Int J Clin Pract. 1998;52(5):316–8.
Gomes F, Emery P, Weekes CE. Risk of Malnutrition on admission predicts mortality, length of stay and hospitalisation costs. Stroke. 2014;45:ATP142.
Gomes F, Emery PW, Weekes CE. Risk of malnutrition, body mass index and waist circumference as predictors of mortality after stroke. Cerebrovasc Dis. 2013;35 Suppl 3:312.
Axelsson K, Asplund K, Norberg A, Alafuzoff I. Nutritional status in patients with acute stroke. Acta Med Scand. 1988;224:217–24.
Mosselman MJ, Kruitwagen CL, Schuurmans MJ, Hafsteinsdóttir TB. Malnutrition and risk of malnutrition in patients with stroke: prevalence during hospital stay. J Neurosci Nurs. 2013;45(4):194–204.
Perry L, McLaren S. Coping and adaptation at six months after stroke: experiences with eating disabilities. Int J Nurs Stud. 2003;40(2):185–95.
Jönsson AC, Lindgren I, Norrving B, Lindgren A. Weight loss after stroke: a population-based study from the Lund Stroke Register. Stroke. 2008;39(3):918–23. doi:10.1161/STROKEAHA.107.497602. Epub 2008 Jan 31.
Kumlien S, Axelsson K. Stroke patients in nursing homes: eating, feeding, nutrition and related care. J Clin Nurs. 2002;11(4):498–509.
Kelly IE, Tessier S, Cahill A, Morris SE, Crumley A, McLaughlin D, McKee RF, Lean ME. Still hungry in hospital: identifying malnutrition in acute hospital admissions. QJM. 2000;93(2):93–8.
Sullivan DH, Sun S, Walls RC. Protein-energy undernutrition among elderly hospitalized patients: a prospective study. JAMA. 1999;281(21):2013–9.
Horan D, Coad J. Can nurses improve patient feeding? Nurs Times. 2000;96:33–4.
Dupertius YM, Kossovsky MP, Kyle UG, Raguso CA, Genton L, Pichard C. Food intake in 1707 hospitalised patients: a prospective comprehensive hospital survey. Clin Nutr. 2003;22:115–23.
Naithani S, Whelan K, Thomas J, Gulliford MC, Morgan M. Hospital inpatients’ experiences of access to food: a qualitative interview and observational study. Health Expect. 2008;11(3):294–303.
The American Society for Parenteral and Enteral Nutrition. ASPEN standards for nutrition support: hospitalized patients. Nutr Clin Pract. 1995;10(6):208–19.
Mackintosh M, Williams A, Goudge D, Bryan F, McAtear CA, Ogilvie M, Murray A. Nutrition screening tools. Birmingham: British Dietetic Association; 1999.
Kondrup J, Allison SP, Elia M, Vellas B, Plauth M, Educational and Clinical Practice Committee, European Society of Parenteral and Enteral Nutrition (ESPEN). ESPEN guidelines for nutrition screening 2002. Clin Nutr. 2003;22(4):415–21.
Anthony PS. Nutrition screening tools for hospitalized patients. Nutr Clin Pract. 2008;23(4):373–82.
Kondrup J, Rasmussen HH, Hamberg O, Stanga Z, Ad Hoc ESPEN Working Group. Nutritional risk screening (NRS 2002): a new method based on an analysis of controlled clinical trials. Clin Nutr. 2003;22(3):321–36.
Kruizenga HM, Seidell JC, de Vet HC, Wierdsma NJ, van Bokhorst-de van der Schueren MA. Development and validation of a hospital screening tool for malnutrition: the short nutritional assessment questionnaire (SNAQ). Clin Nutr. 2005;24(1):75–82.
Kaiser MJ, Bauer JM, Ramsch C, Uter W, Guigoz Y, Cederholm T, Thomas DR, Anthony P, Charlton KE, Maggio M, Tsai AC, Grathwohl D, Vellas B, Sieber CC, MNA-International Group. Validation of the Mini Nutritional Assessment short-form (MNA-SF): a practical tool for identification of nutritional status. J Nutr Health Aging. 2009;13(9):782–8.
Lindsay MP, Gubitz G, Bayley M, Phillips S (Editors) on Behalf of the Canadian Stroke Best Practices and Standards Working Group. Canadian best practice recommendations for acute stoke care. Update 2012–2013. P19 http://best.isunderconstruction.com/wp-content/uploads/2010/10/Ch4_SBP2013_Acute-Inpatient-Care_22MAY13_EN_FINAL4.pdf.
Scottish Intercollegiate Guidelines Network: Management of patients with stroke or TIA: assessment, investigation, immediate management and secondary prevention. National clinical Guideline 108. Dec 2008.
Intercollegiate Stroke Working Party. National clinical guideline for stroke. 4th ed. London: Royal College of Physicians; 2012.
Ottery FD. Definition of standardized nutritional assessment and interventional pathways in oncology. Nutrition. 1996;12(1 Suppl):S15–9.
Gomes F, Emery PW, Weekes CE. Weight loss prior to stroke is associated with increased mortality and length of hospital stay at 6 months post-stroke. Int J Stroke. 2013;8 Suppl 3:39.
Mitchell CO, Lipschitz DA. Arm length measurement as an alternative to height in nutritional assessment of the elderly. JPEN J Parenter Enteral Nutr. 1982;6(3):226–9.
Bassey EJ. Demi-span as a measure of skeletal size. Ann Hum Biol. 1986;13(5):499–502.
Chumlea WC, Roche AF, Steinbaugh ML. Estimating stature from knee height for persons 60 to 90 years of age. J Am Geriatr Soc. 1985;33(2):116–20.
Vlaming S, Biehler A, Hennessey EM, Jamieson CP, Chattophadhyay S, Obeid OA, Archer C, Farrell A, Durman K, Warrington S, Powell-Tuck J. Should the food intake of patients admitted to acute hospital services be routinely supplemented? A randomized placebo controlled trial. Clin Nutr. 2001;20(6):517–26.
Powell-Tuck J, Hennessy EM. A comparison of mid upper arm circumference, body mass index and weight loss as indices of undernutrition in acutely hospitalized patients. Clin Nutr. 2003;22(3):307–12.
Crook MA, Hally V, Panteli JV. The importance of the refeeding syndrome. Nutrition. 2001;17(7–8):632–7.
Khan LU, Ahmed J, Khan S, Macfie J. Refeeding syndrome: a literature review. Gastroenterol Res Pract. 2011. doi:10.1155/2011/410971. pii: 410971, Epub 2010.
Shenkin A. Micronutrients in health and disease. Postgrad Med J. 2006;82(971):559–67.
Bingham SA. The dietary assessment of individuals: methods, accuracy, new techniques and recommendations. Nutr Abstr Rev. 1987;57:705–42.
Palmer M, Miller K, Noble S. The accuracy of food intake charts completed by nursing staff as part of usual care when no additional training in completing intake tools is provided. Clin Nutr. 2014. pii: S0261-5614(14). (In press).
Gariballa SE. Malnutrition in hospitalized elderly patients: when does it matter? Clin Nutr. 2001;20(6):487–91.
Foley N, Finestone H, Woodbury MG, Teasell R, Greene Finestone L. Energy and protein intakes of acute stroke patients. J Nutr Health Aging. 2006;10(3):171–5.
Ingeman A, Pedersen L, Hundborg HH, Petersen P, Zielke S, Mainz J, Bartels P, Johnsen SP. Quality of care and mortality among patients with stroke: a nationwide follow-up study. Med Care. 2008;46(1):63–9.
Bray BD, Ayis S, Campbell J, Hoffman A, Roughton M, Tyrrell PJ, Wolfe CD, Rudd AG. Associations between the organisation of stroke services, process of care, and mortality in England: prospective cohort study. BMJ. 2013;346:f2827.
Geeganage C, Beavan J, Ellender S, Bath PM. Interventions for dysphagia and nutritional support in acute and subacute stroke. Cochrane Database Syst Rev. 2012;10:CD000323. doi:10.1002/14651858.CD000323.pub2.
Weekes CE, Spiro A, Baldwin C, Whelan K, Thomas JE, Parkin D, Emery PW. A review of the evidence for the impact of improving nutritional care on nutritional and clinical outcomes and cost. J Hum Nutr Diet. 2009;22(4):324–35.
Weekes E, Elia M. Resting energy expenditure and body composition following cerebro-vascular accident. Clin Nutr. 1992;11(1):18–22.
Finestone HM, Greene-Finestone LS, Foley NC, Woodbury MG. Measuring longitudinally the metabolic demands of stroke patients: resting energy expenditure is not elevated. Stroke. 2003;34(2):502–7.
Bardutzky J, Georgiadis D, Kollmar R, Schwarz S, Schwab S. Energy demand in patients with stroke who are sedated and receiving mechanical ventilation. J Neurosurg. 2004;100(2):266–71.
Esper DH, Coplin WM, Carhuapoma JR. Energy expenditure in patients with nontraumatic intracranial hemorrhage. JPEN J Parenter Enteral Nutr. 2006;30(2):71–5.
Frankenfield DC, Ashcraft CM. Description and prediction of resting metabolic rate after stroke and traumatic brain injury. Nutrition. 2012;28(9):906–11.
Scientific Advisory Committee on Nutrition. Dietary reference values for energy. 2012. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/339317/SACN_Dietary_Reference_Values_for_Energy.pdf.
NICE guideline 174. Intravenous fluid therapy in adults in hospital. Dec 2013. www.guidance.nice.org.uk/cg174.
Baldwin C, Weekes CE. Dietary advice with or without oral nutritional supplements for disease-related malnutrition in adults. Cochrane Database Syst Rev. 2011;(9):CD002008.
Gall MJ, Grimble GK, Reeve NJ, Thomas SJ. Effect of providing fortified meals and between-meal snacks on energy and protein intake of hospital patients. Clin Nutr. 1998;17(6):259–64.
Barton AD, Beigg CL, Macdonald IA, Allison SP. A recipe for improving food intakes in elderly hospitalized patients. Clin Nutr. 2000;19(6):451–4.
Odlund-Olin A, Osterberg P, Hadell K, Armyr I, Jerstrom S, Ljungqvist O. Energy-enriched hospital food to improve energy intake in elderly patients. J Parenter Enter Nutr. 1996;20:93–7.
Johansen N, Kondrup J, Plum LM, Bak L, Nørregaard P, Bunch E, Baernthsen H, Andersen JR, Larsen IH, Martinsen A. Effect of nutritional support on clinical outcome in patients at nutritional risk. Clin Nutr. 2004;23(4):539–50.
Milne AC, Potter J, Vivanti A, Avenell A. Protein and energy supplementation in elderly people at risk from malnutrition. Cochrane Database Syst Rev. 2009;(2):CD003288
Stratton RJ, Elia M. A review of reviews: a new look at the evidence for oral nutritional supplements in clinical practice. Clin Nutr Suppl. 2007;2:5–23.
Managing adult malnutrition in the community. Produced by a multi-profession consensus panel. May 2012. Available from: http://www.malnutritionpathway.co.uk/.
Finestone HM, Foley NC, Woodbury MG, Greene-Finestone L. Quantifying fluid intake in dysphagic stroke patients: a preliminary comparison of oral and nonoral strategies. Arch Phys Med Rehabil. 2001;82(12):1744–6.
Vivanti AP, Campbell KL, Suter MS, Hannan-Jones MT, Hulcombe JA. Contribution of thickened drinks, food and enteral and parenteral fluids to fluid intake in hospitalized patients with dysphagia. J Hum Nutr Diet. 2009;22:148–55.
Nowson C, Sherwin AJ, McPhee JG, Wark JD, Flicker L. Energy, protein, calcium, vitamin D and fibre intakes from meals in residential care establishments in Australia. Asia Pac J Clin Nutr. 2003;12(2):172–7.
Wright L, Cotter D, Hickson M, Frost G. Comparison of energy and protein intakes of older people consuming a textured modified diet with a normal hospital diet. J Hum Nutr Diet. 2005;18:213–9.
Perry L, Love CP. Screening for dysphagia and aspiration in acute stroke: a systematic review. Dysphagia. 2001;16(1):7–18. Winter.
Hickson M, Connolly A, Whelan K. Impact of protected mealtimes on ward mealtime environment, patient experience and nutrient intake in hospitalised patients. J Hum Nutr Diet. 2011;24(4):370–4.
Huxtable S, Palmer M. The efficacy of protected mealtimes in reducing mealtime interruptions and improving mealtime assistance in adult inpatients in an Australian hospital. Eur J Clin Nutr. 2013;67(9):904–10.
Bradley L, Rees C. Reducing nutritional risk in hospital: the red tray. Nurs Stand. 2003;17(26):33–7.
Hickson M, Bulpitt C, Nunes M, Peters R, Cooke J, Nicholl C, Frost GS. Does additional feeding support provided by health care assistants improve nutritional status and outcome in acutely ill older patients? – a randomised control trial. Clin Nutr. 2004;23:69–77.
Duncan DG, Beck SJ, Hood K, Johansen A. Using dietetic assistants to improve the outcome of hip fracture: a randomised controlled trial of nutritional support in an acute trauma ward. Age Ageing. 2006;35(2):148–53.
Nijs KA, de Graaf C, Siebelink E, Blauw YH, Vanneste V, Kok FJ, van Staveren WA. Effect of family-style meals on energy intake and risk of malnutrition in Dutch nursing home residents: a randomized controlled trial. J Gerontol A Biol Sci Med Sci. 2006;61(9):935–42.
Wright L, Hickson M, Frost G. Eating together is important: using a dining room in an acute elderly medical ward increases energy intake. J Hum Nutr Diet. 2006;19(1):23–6.
Heymsfield SB, Casper K. Anthropometric assessment of the adult hospitalized patient. JPEN J Parenter Enteral Nutr. 1987;11(5 Suppl):36S–41.
Flood A, Chung A, Parker H, Kearns V, O’Sullivan TA. The use of hand grip strength as a predictor of nutrition status in hospital patients. Clin Nutr. 2014;33(1):106–14.
McWhirter JP, Pennington CR. Incidence and recognition of malnutrition in hospital. BMJ. 1994;308(6934):945–8.
Almdal T, Viggers L, Beck AM, Jensen K. Food production and wastage in relation to nutritional intake in a general district hospital–wastage is not reduced by training the staff. Clin Nutr. 2003;22(1):47–51.
Porbén SS. The state of the provision of nutritional care to hospitalized patients–results from The Elan-Cuba Study. Clin Nutr. 2006;25(6):1015–29.
Visvanathan R, Macintosh C, Callary M, Penhall R, Horowitz M, Chapman I. The nutritional status of 250 older Australian recipients of domiciliary care services and its association with outcomes at 12 months. J Am Geriatr Soc. 2003;51(7):1007–11.
van Bokhorst-de van der Schueren MA, Klinkenberg M, Thijs A. Profile of the malnourished patient. Eur J Clin Nutr. 2005;59(10):1129–35.
McPherson K, Marsh T, Brown M. Foresight Report. Tackling obesities: future choices – modelling future trends in obesity & their impact on health. 2007 Available from: http://veilleagri.hautetfort.com/media/02/00/2025691480.pdf.
Kurth T, Gaziano JM, Rexrode KM, Kase CS, Cook NR, Manson JE, Buring JE. Prospective study of body mass index and risk of stroke in apparently healthy women. Circulation. 2005;111(15):1992–8.
Vandenbroeck P, Goossens J, Clemens M. Foresight Report. Tackling obesities: future choices – obesity systems map. 2007 Available from: http://www.shiftn.com/obesity/Full-Map.html.
World Health Organisation. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i–xii. 1–253.
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–63. Review. Erratum in: Lancet. 2004 Mar 13;363(9412):902.
Suk SH, Sacco RL, Boden-Albala B, Cheun JF, Pittman JG, Elkind MS, Paik MC, Northern Manhattan Stroke Study. Abdominal obesity and risk of ischemic stroke: the Northern Manhattan Stroke Study. Stroke. 2003;34(7):1586–92. Epub 2003 May 29.
Winter Y, Rohrmann S, Linseisen J, Lanczik O, Ringleb PA, Hebebrand J, Back T. Contribution of obesity and abdominal fat mass to risk of stroke and transient ischemic attacks. Stroke. 2008;39(12):3145–51.
Lean ME, Han TS, Morrison CE. Waist circumference as a measure for indicating need for weight management. BMJ. 1995;311:158–61.
Ross R, Berentzen T, Bradshaw AJ, et al. Does the relationship between waist circumference, morbidity and mortality depend on measurement protocol for waist circumference? Obes Rev. 2007;9:312–25.
NICE Guidance on the prevention, identification, assessment and management of overweight and obesity in adults and children. Clin Guide 43. 2006 (Updated 2013). Available from: http://www.nice.org.uk/guidance/cg43/resources/guidance-obesity-pdf.
Alberti KG, Zimmet P, Shaw J. International diabetes federation: a consensus on type 2 diabetes prevention. Diabet Med. 2007;24(5):451–63.
Curioni C, André C, Veras R. Weight reduction for primary prevention of stroke in adults with overweight or obesity. Cochrane Database Syst Rev. 2006;(4):CD006062.
NICE Guidance on Hypertension. Clinical management of primary hypertension in adults 2011. Available from: www.guidance.nice.org.uk/cg127.
Scottish Intercollegiate Guidelines Network. Management of obesity. A national clinical guideline 115. 2010. Available from: http://www.sign.ac.uk/pdf/sign115.pdf.
Mehta T, Smith Jr DL, Muhammad J, Casazza K. Impact of weight cycling on risk of morbidity and mortality. Obes Rev. 2014;15:870–81.
Avenell A, Broom J, Brown TJ, Poobalan A, Aucott L, Stearns SC, et al. Systematic review of the long-term effects and economic consequences of treatments for obesity and implications for health improvement. Health Technology Assess 2004;8(21). http://www.hta.ac.uk/fullmono/mon821.pdf.
Antje Damms-Machado A, Gesine Weser G, Bischoff SC. Micronutrient deficiency in obese subjects undergoing low calorie diet. Nutr J. 2012;11:34. Published online 2012 June 1.
Rosenheck R. Fast food consumption and increased caloric intake: a systematic review of a trajectory towards weight gain and obesity risk. Obes Rev. 2008;9(6):535–47.
Sacks FM, Bray GA, Carey VJ, Smith SR, Ryan DH, Anton SD, et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med. 2009;360(9):859–73.
Rees K, Dyakova M, Wilson N, Ward K, Thorogood M, Brunner E. Dietary advice for reducing cardiovascular risk. Cochrane Database Syst Rev. 2013;12:CD002128.
Ahern AL, Olson AD, Aston LM, Jebb SA. Weight watchers on prescription: an observational study of weight change among adults referred to weight watchers by the NHS. BMC Public Health. 2011;11:434.
Department of Health, Physical Activity, Health Improvement and Protection. Start active, Stay active: a report on physical activity from the four home countries’ Chief Medical Officers. July 2011. Available from: www.gov.uk/government/uploads/system/uploads/attachment_data/file/216370/dh_128210.pdf.
Adams TD, Davidson LE, Litwin SE, Kolotkin RL, LaMonte MJ, Pendleton RC, Strong MB, Vinik R, Wanner NA, Hopkins PN, Gress RE, Walker JM, Cloward TV, Nuttall RT, Hammoud A, Greenwood JL, Crosby RD, McKinlay R, Simper SC, Smith SC, Hunt SC. Health benefits of gastric bypass surgery after 6 years. JAMA. 2012;308(11):1122–31.
Perri MG, Sears Jr SF, Clark JE. Strategies for improving maintenance of weight loss. Toward a continuous care model of obesity management. Diabetes Care. 1993;16(1):200–9.
Skender ML, Goodrick GK, Del Junco DJ, Reeves RS, Darnell L, Gotto AM, Foreyt JP. Comparison of 2-year weight loss trends in behavioral treatments of obesity: diet, exercise, and combination interventions. J Am Diet Assoc. 1996;96(4):342–6.
Macdiarmid J, Blundell J. Assessing dietary intake: who, what and why of under-reporting. Nutr Res Rev. 1998;11(2):231–53.
Olsen TS, Dehlendorff C, Petersen HG, Andersen KK. Body mass index and poststroke mortality. Neuroepidemiology 2008;30(2):93–100. doi:10.1159/000118945. Towfighi A, Ovbiagele B. The impact of body mass index on mortality after stroke. Stroke 2009;40(8):2704–8. doi:10.1161/STROKEAHA.109.550228. Epub 2009 Jun 18.
Vemmos K, Ntaios G, Spengos K, Savvari P, Vemmou A, Pappa T, Manios E, Georgiopoulos G, Alevizaki M. Association between obesity and mortality after acute first-ever stroke: the obesity-stroke paradox. Stroke. 2011;42(1):30–6.
Kim Y, Kim CK, Jung S, Yoon BW, Lee SH. Obesity-stroke paradox and initial neurological severity. J Neurol Neurosurg Psychiatry. 2014. doi:10.1136/jnnp-2014-308664. pii: jnnp-2014-308664.
Gomes F, Emery PW, Weekes CE. Mortality and stroke recurrence in obese stroke patients: the obesity paradox in a London-based population. International Journal of Stroke. 2013;8 Suppl 3:39.
Miller AJ. Characteristics of the swallowing reflex induced by peripheral nerve and brainstem stimulation. Exp Neurol. 1972;34:210–22.
Doty RW. Neural organization of deglutition. In: Code CF, editor. Handbook of physiology, vol. 4. Washington, DC: American Physiological Society; 1968. p. 1861–18902.
Smithard DG. Swallowing and stroke. Cerebrovasc Dis. 2002;14:1–8.
Palmer JB, Rudin NJ, Lara G, Crompton AW. Coordination of mastication and swallowing. Dysphagia 1992;7187–200.
Dantas RO, Kern MK, Massey BT, Dodds WJ, Kahrilas PJ, Brasseur JG, Cook IJ, Lang IM. Effects of swallowed bolus variables on oral and pharyngeal phases of swallowing. Am J Physiol Gastrointest Liver Physiol. 1990;258:G675–81.
Curtis DJ, Curesss DF. Videofluoroscopic identification of two types of swallowing. Radiology. 1984;152(2):305–8.
Borgström P, Ekberg O. Speed of peristalsis in pharyngeal constrictor muscles: correlation to age. Dysphagia. 1988;2:140–4.
Martin-Harris B, Brodsky MB, Price CC, Michel Y, Walters B. Temporal coordination of pharyngeal and laryngeal dynamics with breathing during swallowing: single liquid swallows. J Appl Physiol. 2003;94:1735–43.
Dozier TS, Brodsky MB, Michel Y, Walters B, Martin-Harris B. Coordination of swallowing and respiration in normal sequential cup swallows. Laryngoscope. 2006;116:1489–93.
Miller JL, Watkin KL. Lateral pharyngeal wall motion during swallowing using real time ultrasound. Dysphagia. 1997;12:125–32.
Logemann JA. Swallowing physiology and pathophysiology. Otolaryngol Clin N Am. 1983;21:613–23.
Hiss SG, Treole K, Stuart A. Effects of age, gender, bolus volume, and trial on swallowing apnea duration and swallow/ respiratory phase relationships of normal adults. Dysphagia. 2001;16:128–35.
Reginelli A, Pezzullo MG, Scaglione M, Scialpi M, Brunese L, Grassi R. Gastrointestinal disorders in elderly patients. Radiol Clin of N Am. 2008;46:755–71.
Ardran GM, Kemp FH. The protection of the laryngeal airway during swallowing. Br J Radiol. 1952;25:406–16.
Dua KS, Ren J, Barden E, Shaker R. Coordination of deglutitive glottal function and pharyngeal transit during normal eating. Gastroenterology. 1997;112:75–83.
Matsuo K, Hiiemae KM, Gonzalez-Fernandez M, Palmer JB. Respiration during feeding on solid food: alterations in breathing during mastication, pharyngeal bolus aggregation, and swallowing. J Appl Physiol. 2008;104:674–81.
Hamdy S, Aziz Q, Rothwell JC, Hobson A, Barlow J. Thompson DG Cranial nerve modulation of human cortical swallowing motor pathways. Am J Physiol Gastrointest Liver Physiol. 1997;272:G802–8.
Bastian RW, Riggs LC. Role of sensation in swallowing function. Laryngoscope. 1999;109:1974–7.
Kern MK, Jaradeh S, Armdorfer RC, Shaker R. Cerebral cortical representation of reflexic and volitional swallow in humans. Am J Physiol. 2001;280:G354–60.
Hamdy S, Aziz Q, Rothwell JC, Singh KD, Barlow J, Hughes DG, Tallis RC, Thompson DG. The cortical topography of swallowing musculature in health and disease. Nat Med. 1996;2:1217–24.
Martin R, Goodyear BG, Gati JS, et al. Cerebral cortical representation of automatic and volitional swallowing in humans. J Neurophysiol. 2000;85:938–50.
Smithard DG. Substance P and swallowing after stroke. Therapy. 2006;3:291–8.
Hamdy S, Mikulis DJ, Crawley A, Xue S, Lau H, Henry S, Diamant NE. Cortical activation during human volitional swallowing; an event related fMRI study. Am J Physiol Gastrointest Liver Physiol. 1999;277:G219–25.
The atlas of heart disease and stroke. WHO http://www.who.int/cardiovascular_diseases/resources/atlas/en/.
Gordon C, Hewer RL, Wade DT. Dysphagia in acute stroke. BMJ. 1987;295:411–4.
Martino R, Foley N, Bhogel S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke. Incidence, diagnosis and pulmonary complications. Stroke. 2005;36:2756–63.
Smithard DG, O’Neill PA, England RE, Park CL, Wyatt R, Martin DF, Morris J. The natural history of dysphagia following stroke. Dysphagia. 1997;12:188–93.
Mann G, Hankey GJ, Cameron D. Swallowing function after stroke: prognosis and prognostic factors at six months. Stroke. 1999;30:744–48.
Hamdy S. The organization and re-organisation of human swallowing motor cortex. Suppl Clin Neurophysiol. 2003;56:204–10.
Martin RE. Neuroplasticity and swallowing. Dysphagia. 2009;24:218–29.
Barritt AW, Smithard DG. Role of cerebral cortex plasticity in the recovery of swallowing function following dysphagic stroke. Dysphagia. 2009;24:83–90.
Fraser C, Power M, Hamdy S, Rothwell J, Hobday D, Hollander I, Tyrell P, Hobson A, Williams S, Thompson D. Driving plasticity in human adult motor cortex is associated with improved motor function after brain injury. Neuron. 2002;34:831–40.
Smithard DG. The aetiology of oropharyngeal dysphagia and its effects in stroke. J Gastroenterol Hepatol Res. 2014;3(10):1252–64.
Leslie P, Drinnan MJ, Ford GA, Wilson JA. Swallow respiratory patterns and aging: presbyphagia or dysphagia. J Gerontol A Biol Sci Med Sci. 2005;60:391–5.
Walls AW. Oral health and nutrition. Age Ageing. 1999;28:419–20.
Fox C, Richardson K, Maidment ID, Savva GM, Matthews FE, Smithard D, Coulton S, Katona C, Boustania MA, Brayne C. Anticholinergic medication use and cognitive impairment in the older population: the Medical Research Council Cognitive Function and Ageing Study. J Am Geriatr Soc. 2011;59:1477–83.
Fox C, Livingstone G, Maidment ID, Coulton S, Smithard D, Boustani MA, Katona C. The impact of anticholinergic burden in Alzheimer’s dementia – the laser AD study. Age Ageing. 2011;40:730–5.
Smithard DG, Fox C, Maidment ID, Katona C, Boustani M. Do anticholinergic drugs contribute to functional and cognitive decline. Aging Health. 2012;8:57–60.
Sjogren P, Nilsson E, Forsell M, Johansson O, Hoogstraate J. A systematic review of the preventive effect of oral hygiene on respiratory tract infection in hospitals and nursing homes: effect estimates and methodological quality of randomized controlled trials. JAGS. 2008;56:2124–30.
European Society for Swallowing Disorders Position Statements. Dysphagia. 2013;28:280–2.
Ramsey DJC, Smithard DG, Kalra L. Silent aspiration: what do we know? Dysphagia. 2005;20:218–25.
Ramsey DJC, Smithard DG, Kalra L. Can pulse oximetry or a bedside swallowing assessment be used to detect aspiration after stroke? Stroke. 2006;37:2984–8.
Splaingard ML, Hutchins B, Sulton LD, Chaudhuri G. Aspiration in rehabilitation patients: videofluoroscopy vs bedside clinical assessment. Arch Phys Med Rehabil. 1988;69:637–40.
Kelly AM, Drinan MJ, Lelsie P. Assessing penetration and aspiration: how do videofluoroscopy and fibre optic endoscopic evaluation of swallowing compare? Laryngoscope. 2007;117:1723–7.
Watkin KL. Ultrasound and swallowing. Folia Phoniatr Logop. 1999;51:199–212.
Cappabianca S, Reginelli A, Monaco L, Del Vexxhio L, Di Martino N, Grassi R. Combined videofluoroscopy and manaometry in the diagnosis of oropharyngeal dysphagia: examination technique and preliminary experience. Radiol Med. 2008;113:923–40.
Balan KK, Vinjamin S, Maltby P, Bennett J, Woods S, Playfer JR, Critchley M. Gastroesophageal reflex inpatients fed by percutaneous endoscopic gastrostomy (PEG): detection by a simple scinitigraphic method. Am J Gastroenterol. 1998;93:946.
Millins B, Gosney M, Jack CIA, Martin MV, Wright AE. Acute stroke predisposes to oral gram negative bacilli- a cause of aspiration pneumonia. Gerontology. 2003;49:17.
Gosney M, Martin MV, Wright AE. The role of selective decontamination of the digestive tract in acute stroke. Age Ageing. 2006;35:42–7.
Nilsson H, Ekberg O, Bülow M, Hindfelt B. Assessment of respiration during videoflurosocpy of dysphagic patients. Acad Radiol. 1997;4:503–7.
Hoffman MR, Mielens JD, Ciucci MR. High-resolution manometry of pharyngeal swallow pressure events associated with effortful swallow and the Mendelsohn manoeuvre. Dysphagia. 2012;27:418–26.
Hori K, Tamine K, Barbezat C, Maeda Y, Yamori M, Muller F, Ono T. Influence of Chin-down posture on tongue pressure during dry swallow and bolus swallows in healthy subjects. Dysphagia. 2011;26:2238–45.
Chichero JAY. Thickening agents used for dysphagia management: effect on bioavailability of water, medication and feelings of satiety. Nutr J. 2013;12(1):54.
Carnaby-Mann GD, Crary MA. McNeill dysphagia therapy programme: a case controlled study. Arch Phys Med Rehabil. 2010;91:743–9.
Ertekin C, Keskin A, Kiylioglu N, et al. The effect of head and neck positions on oropharyngeal swallowing: a clinical and electrophysiologic study. Arch Phys Med Rehabil. 2001;82:1255–60.
Rasley A, Logemann JA, Kahrilas PJ. Prevention of barium aspiration during videofluoroscopic swallowing studies: value of change in posture. AJR. 1993;160:1005–9.
Bülow M, Olsson R, Ekberg O. Supraglottic swallow, effortful swallow, and chin tuck did not alter hypopharyngeal intrabolus pressure in patients with pharyngeal dysfunction. Dysphagia. 2002;17:197–201.
McCullough GH, Kim Y. Effects of the Mendelsohn maneuver on extent of hyoid movement and UES opening post-stroke. Dysphagia. 2013;28:511–9.
Speyer R, Baijens, Heijnen M, Zwijnenberg I. Effects of therapy in oro-pharyngeal dysphagia by speech and language therapists: a systematic review. Dysphagia. 2010;25:40–65.
Yang Y, Leow LP, Yoon WL, et al. Relationship between age and drinking instructions on the modification of drinking behaviour. Dysphagia. 2012;27:210–5.
Clavé P, Arreola V, Romea M, Medina L, Palomera E, Serra-Prat M. curacy of the volume-viscosity swallow test for clinical screening of oro-pharyngeal dysphagia and aspiration. Clin Nutr. 2008;27:806–15.
Chee C, Arshad S, Singh S, Mistry S, Hamdy S. The influence of chemical and gustatory stimuli and oral anaesthesia on healthy human pharyngeal swallowing. Chem Senses. 2005;30:393–400.
Cola PC, Gatto AR, da Silva RG, Spadotto AA, Schelp AC, Aparecida M, de A Henry C. The influence of sour taste and cold temperature in pharyngeal transit duration in patients with stroke. Aq de Gastroenterologia. 2010;47:18–21.
Hansen B, O’Leary MT, Smith CH. The effect of saliva on the viscosity of thickened fluids. Dysphagia. 2012;27:10–9.
Clavé P, De Kraa M, Areola V, Girvent M, Farré R, et al. The effect of bolus viscosity on swallowing function in neurogenic dysphagia. Aliment Pharmacol Ther. 2006;24:1385–94.
Hamdy S, Jilani S, Price V, et al. Modualtion of human swallowing behavior by thermal and chemical stimulation in health after brain injury. Neurogastroenterol Motil. 2003;15:69–77.
Fraser C, Rothwell J, Power M, Hobson A, Thompson D, Hamdy S. Differential changes in human pharyngoesophageal motor excitability induced by swallowing, pharyngeal stimulation, and anesthesia. Am J Physiol Gastrointest Liver Physiol. 2003;285(1):G137–44. doi:10.1152/ajpgi.00399.2002. Published 1 July.
Carlaw C, Finlayson H. Outcomes of a pilot water protocol project in a rehabilitation setting. Dysphagia. 2012;27:297–306.
Hotaling DL. Nutritional considerations for the pureed diet texture in dysphagic elderly. Dysphagia. 1992;7:81–5.
Keller H, Chambers L, Niezgoda H, Duizer L. Issues associated with use of textured foods. J Nutr Health Aging. 2012;16:195–200.
Gomes CAR, Lustosa SAS, Matos D, et al. Percutaneous endoscopic gastrostomy versus nasogastric tube feeding for adults with swallowing disturbances (Review). The Cochrane Library 2012 http://www.thecochranelibrary.com. Wiley.
Dziewas R, Warnecke T, Hamacher C, Oelenberg S, Teismann I, Kraemer C, Ritter M, Ringelstein EB, Schaebitz. Do nasogastric tubes worsen dysphagia in patients with acute stroke? BMC Neurol. 2008;8:28. doi:10.1186/1471-2377-8-28.
Wang TG, Wu MC, Chang YC, Hsiao TY, Lien IN. The effect of nasogastric tubes on swallowing function in persons with dysphagia following stroke. Arch Phys Med Rehabil. 2006;87:1270–3.
Rabadi MH, Coar PL, Lukin M, Lesser M, Blass JP. Intensive nutritional supplements can improve outcomes in stroke rehabilitation. Neurology. 2008;71:1856–61.
Langdon PC, Lee AH, Binns CW. High incidence of respiratory infections in “nil by mouth” tube-fed acute ischaemic stroke patients. Neuroepidemiology. 2009;32:107–13.
Bevan J, Conroy SP, Harwood R, Gladman JRF, Leonardi-Bee J, Sach T, Bowling T, Sunman W, Gaynor C. Does looped nasogastric tube feed improve nutritional delivery for patients with dysphagia after acute stroke? A randomised controlled trial. Age Ageing. 2010;39:624–30.
Ha L, Hauge T. Percutaneous endoscopic gastrostomy (PEG) for enteral nutrition in patients with stroke. Scand J Gastroenterol. 2003;38:962–6.
Laasch H-U, Wilbraham L, Bullen K, Marriott A, Lawrance JAL, Johnson RJ, Lee SH, England RE, Gamble RE, Martin DF. Gastrostomy insertion: comparing the options—PEG, RIG or PIG? Clin Radiol. 2003;58:398–405.
Klor BM, Milianti FJ. Rehabilitation of neurogenic dysphagia with percutaneous endoscopic gastrostomy. Dysphagia. 1999;14:162–4.
Allinson MC, Morris AJ, Park RHR, Mills PR. Percutaneous endoscopic gastrostomy tube feeding may improve outcome of late rehabilitation following stroke. J R Soc Med. 1992;85:147–9.
The FOOD Trial Collaboration. Effect of timing and method of enteral tube feeding for dysphagic stroke patients (FOOD): a multicentre randomised controlled trial. Lancet. 2005;365:764–72.
Logemann JA, Kahrilas PJ. Relearning to swallow after stroke – application of maneuvers and indirect biofeedback. Neurology. 1990;40:11.
ML H, Steele CM. An analysis of lingual contribution to submental surface electromyographic measures and pharyngeal pressure during effortful swallow. Arch Phys Med Rehabil. 2006;87:1067–72.
Carnaby-Mann GD, Crary MA. Examining the evidence on neuromuscular electrical stimulation for swallowing. Arch Otolaryngol Head Neck Surg. 2007;133:564–71.
Denk DM, Kaider A. Videoendoscopic biofeedback: a simple method to improve the efficacy of swallowing rehabilitation after head and neck surgery. ORL. 1997;59:100–5.
Reddy NP, Katakam A, Gupta V, et al. Measurements of acceleration during videofluorographic evaluation of dysphagic patients. Med Eng Phys. 2000;22:405–12.
Coulas VL, Smith RC, Qadri SS, Martiin E. Differentiating effortful and non effortful swallow with a neck force transducre: implications for the development of a clinical feedback system. Dysphagia. 2009;24:7–12.
Steele CM, Bailey GL, Molfenter SM. Tongue pressure modulation during swallowing: water versus nectar-thick liquids. J Speech Lang Hear Res. 2010;53:273–83.
Butler SG, Stuart A, Leng X, et al. The relationship of aspiration status with tongue and handgrip strength in healthy older adults. J Gerentol A Biol Sci Med Sci. 2011;66A:452–258.
Robbins JA, Theis SM, Kays SA. The effects of lingual exercise on swallowing in older adults. J Am Ger Soc. 2005;53:1483–9.
Lazarus C, Logemann JA, Huang CF, Rademaker AW. Effects of two types of tongue strengthening exercises in young normal. Folia Phoniatr Logop. 2003;55:199–205.
Clark HM, O’Brien K, Calleja A, Corrie SN. Effects of directional exercise on lingual strength. J Speech Lang Hear Res. 2009;52:1034–47.
Robbins JA, Kays SA, Gangnon RE, et al. The effects of lingual exercise in stroke patients with dysphagia. Arch Phys Med Rehabil. 2007;88:150–8.
Shaker R, Easterling C, Kerin M, et al. Rehabilitation of swallowing by exercise in tube-fed patients with pharyngeal dysphagia secondary to abnormal UES opening. Gastroeneterology. 2002;122:1314–21.
Logemann JA, Rademaker A, Pauloski BR, et al. A randomized study comparing the Shaker exercise with traditional therapy: a preliminary study. Dysphagia. 2009;24:403–11.
Mepani R, Antonik S, Massey B, et al. Augmentation of deglutitive thyrohyoid muscle shortening by the Shaker exercise. Dysphagia. 2009;24:26–31.
Yoon WL, Khoo JKP, Liow SJR. Chin tuck against resistance (CTAR): new method for enhancing suprahyoid muscle activity using a Shaker-type exercise. Dysphagia. 2014;29:243–8.
Lan Y, Ohkubo M, Berretin-Felix G, Sia I, et al. Normalization of temporal aspects of swallowing physiology after the McNeill Dysphagia Therapy program. Ann Otol Rhinol Laryngol. 2012;121:525–32.
Crary MA, Carnaby GD, Groher M, Helseth E. Functional benefits of dysphagia therapy using adjunctive sEMG biofeedback. Dysphagia. 2004;19:160–4.
Bogaardt HCA, Grolman W, Fokkens WJ. The use of biofeedback in the treatment of chronic dysphagia in stroke patients. Folia Phoniatr Logop. 2009;61:200–5.
de L Lazzara G, Lazarus CL, Logemann JA. Impact of thermal stimulation on the triggering of the swallow reflex. Dysphagia. 1986;1:73–7.
Power M, Fraser CH, Hobson A, Singh S, Tyrrell P, Nicholson DA, Turnbull I, Thompson DG, Hamdy S. Evaluating oral stimulation as a treatment for dysphagia after stroke. Dysphagia. 2006;1:45–55.
Power M, Fraser C, Hobson A, et al. Changes in pharyngeal corticobulbar excitability and swallowing behavior after oral stimulation. Am J Physiol Gastrointest Liver Physiol. 2004;286:G45–50.
Burnett TA, Mann EA, Stoklosa JB, Ludlow CL. Self-triggered functional electrical stimulation during swallowing. J Neurophysiol. 2005;94:4011–8.
Clark H, Lazarus C, Arvedson J, et al. Evidence based systematic review. Effects of neuromuscular electrical stimulation on swallowing and neural activation. Am J Speech Lang Pathol. 2009;18:361–75.
Shaw GY, Sechtem PR, Searl J, et al. Transcutaneous neuromuscular stimulation (VitalStim) curative therapy for severe dysphagia: myth or reality. Ann Otol Rhinol Laryngol. 2007;116:36–44.
Bülow M, Speyer R, Baijens L, et al. Neuromuscular electrical stimulation (NMES) in stroke patients with oral and pharyngeal dysfunction. Dysphagia. 2008;23:302–9.
Permsirivanich W, Tipchatyotin S, Leelamanit V, et al. Comapring the effects of rehabilitation swallowing therapy vs Neuromuscular electrical stimulation therapy among stroke patients with persistent pharyngeal dysphagia: a randomized controlled study. J Med Assoc Thai. 2009;92:259–65.
Ludlow CL, Humbert I, Saxon K, Poletto, Sonies B, Crujido L. Effects of surface electrical stimulation both at rest and during swallowing in chronic pharyngeal dysphagia. Dysphagia. 2007;22:1–10.
Car A, Jean A, Roman C. A pontine relay for ascending projections of the superior laryngeal nerve. Exp Brain Res. 1975;22:197–210.
Hamdy S, Rothwell JC, Brooks DJ, Baily D, Aziz Q, Thompson DG. Identification of the cerebral loci processing human swallowing with H2 15O PET activation. J Neurophysiol. 1999;81:1917–26.
Jayasekeran V, Singh S, Tyrell P, Michou E, Jefferson S, Mistry S, Gamble E, Rothwell J, Thomson D, Hamdy S. Adjunctive functional pharyngeal electrical stimulation reverses swallowing disability after brain lesions. Gastroenterology. 2010;138:1737.
Sekizawa K, Matsui T, Nakagawa T, et al. ACE Inhibitors and pneumonia. Lancet. 1998;352:1069.
Shibuya S, Murahashi M, Inoue M, et al. ACE inhibitors and its usefulness in the prevention of aspiration pneumonia in chronic cerebrovascular disease patients with asymptomatic swallowing dysfunction. Rinsho Shinkeigaku. 2002;42:240–2.
Rofes L, Arreola, Martin A, Clavé P. Natural Capsaicinoids improve swallow response in older patients with oropharyngeal dysphagia. Gut gutjnl-2011-300753v1 62/9/1280.
Rofes L, Arreola V, Martin A, Clavé P. Effect of oral Piperine on the swallow response of patients with oropharyngeal dysphagia. J Gastroenterol. 2013. doi:10.007/s005335-01300920-0.
Perez I, Smithard DG, Davies H, et al. Pharmacological treatment of dysphagia in stroke. Dysphagia. 1998;13(12):691–8.
Li H, Wang YL, Zou BH, Long JJ. The effects of swallow training and acupuncture treatment on the swallowing function of patients with dysphagia following acute cerebral ischaemia. Hainan Med J 2008–2009. http://en.cnki.com.cn/Article_en/CJFDTotal-HAIN200809017.htm. Accessed 20 Feb 2014.
Zhou RX, Zhang CH. Clinical progress of acupuncture treatment for dysphagia after stroke. J Clin Acupunct Moxibust 2011;11. http://en.cnki.com.cn/Article_en/CJFDTOTAL-ZJLC201111036.htm. Accessed 20 Feb 2014.
Xie Y, Wang L, He J, Wu T. Acupuncture for dysphagia in acute stroke (Review). 2008;3 Chochrane Library 2008. Wiley. http://www.thecochranelibrary.com.
Long YB, Wu XP. A meta-analysis of the efficacy of acupuncture in treating dysphagia in patients with a stroke. Acupunct Med. 2012;30:291–7.
Selley WG, Roche MT, Pearce VR. Dysphagia following strokes: clinical observations of swallowing rehabilitation employing palatal training appliances. Dysphagia. 1995;10:32–5.
Brookes GB, McKelvie P. Epiglottoplexy: a new surgical technique to prevent intractable aspiration. Ann R Coll Surg Engl. 1983;65:293–6.
Cook IJ, Kahrilas PJ. AGA technical review on management of oropharyngeal dysphagia. Gastroenterology. 1999;116:455–78.
O’Neil KH, Purdy M, Falk J, Gallo L. The dysphagia outcome severity scale. Dysphagia. 1999;14:139–45.
McHorney CA, Robbins JA, Lomax K. The SWAL-QOL and SWAL-CARE outcomes tool for oro-pharyngeal dysphagia I adults: III. Documentation of reliability and validity. Dysphagia. 2002;17:97–114.
Crary MA, Carnaby Mann GD, Groher ME. Initial psychometric assessment of functional oral intake scale for Dysphagia in stroke patients. Arch Phys Med Rehabil. 2005;86:1516–20.
Smithard DG, Smeeton NC, Wolfe CD. Long-term outcome after stroke: does dysphagia matter? Age Ageing. 2007;36(1):90–4.
Raffin A. Ethics and withdrawal of life support. In: Murray JF, Nadel JA, editors. Philidelphia: WB Saunders Co. Caring for patients with dysphagia.
Kaizer F, Spiridigliozzi AM, Hunt MR. Promoting shared decision-making in rehabilitation: development of a framework when patients with dysphagia refuse diet modification recommended by the treatment team. Dysphagia. 2012;27:81–7.
Mental Capacity Act 2005. HMSO London. http://www.legislation.gov.uk/ukpga/2005/9/pdfs/ukpga_20050009_en.pdf.
Badger J, Ladd RE, Adler P. Respecting patient autonomy versus protecting the patient’s health: a dilemma for healthcare providors. JONA’s Healthcare Law Ethics Regul. 2009;11:120–4.
Wagner LCB. Exploring complications of advance directives and the obligations of a rehabilitation team. Top Stroke Rehabil. 2001;8:56–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Smithard, D., Weekes, C.E. (2015). Swallowing and Nutritional Complications. In: Bhalla, A., Birns, J. (eds) Management of Post-Stroke Complications. Springer, Cham. https://doi.org/10.1007/978-3-319-17855-4_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-17855-4_7
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-17854-7
Online ISBN: 978-3-319-17855-4
eBook Packages: MedicineMedicine (R0)