Abstract
A portion of patients with chronic rhinosinusitis will present with disease which does not respond to either maximal medical or surgical therapy. Otherwise known as recalcitrant chronic rhinosinusitis, this presents a particularly frustrating and difficult challenge to physicians and patients alike. When faced with recalcitrant disease, it is important to take a multifaceted approach. In patients who have had previous surgery, evaluation of the sinonasal cavities for certain anatomic factors which contribute to management failure is necessary. Previously undiagnosed medical conditions complicating the disease process must also be considered. Finally, the type and delivery of topical therapies must be reviewed with all available options considered. The following is a review of recalcitrant chronic rhinosinusitis with a focus on further workup and management of these patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Chronic rhinosinusitis
- Recalcitrant chronic rhinosinusitis
- Endoscopic sinus surgery
- Topical treatment
- Revision sinus surgery
-
Some patients with chronic rhinosinusitis will fail standard medical and surgical therapy. This disease process is known as recalcitrant chronic rhinosinusitis.
-
Anatomy, certain concurrent disease processes, and failure of the delivery of topical therapies can all contribute to unsuccessful management of recalcitrant sinusitis.
-
The differential diagnosis for recalcitrant CRS includes underlying allergic rhinitis, aspirin-exacerbated respiratory disease (AERD), gastroesophageal reflux disease (GERD), mucociliary dysfunction, biofilms, autoimmune disease, and immunodeficiency.
-
Some of the most common anatomic factors leading to revision surgery include lateralization of the middle turbinate, incomplete ethmoidectomy, scarring of the frontal recess, and middle meatal antrostomy stenosis.
-
Multiple topical therapies and delivery mechanisms exist without clear evidence that one drug or one method of delivery is more effective than the others.
Introduction
Chronic rhinosinusitis (CRS) is defined as a group of disorders characterized by inflammation of the mucosa of the nose and paranasal sinuses of at least 12 consecutive weeks’ duration [1]. Further, CRS is often subdivided into chronic rhinosinusitis with nasal polyposis (CRSwNP) and chronic rhinosinusitis without polyposis (CRSsNP). The pathogenesis of CRS is multifactorial; thus the treatment can be challenging. The primary management of CRS includes systemic medical and topical therapies. When these fail, surgical management is considered in appropriate cases.
Recalcitrant CRS occurs when the disease process does not respond to maximal medical and surgical therapy. In this setting, it is important to reevaluate the patient, repeat computed tomography (CT) imaging, and obtain endoscopic cultures. Recalcitrant disease can occur if the primary surgical approach was insufficient, in the setting of certain systemic diseases (immunodeficiency or cystic fibrosis), or both as medical treatments can be refractory if there are predisposing anatomic factors. Obtaining more information will help guide further management decisions. Both revision surgery and optimization of systemic and topical medical therapies can be utilized to improve the patient’s disease burden.
When endoscopic sinus surgery (ESS) results in an unsatisfactory outcome, the presence of an underlying disease process which may have been previously undiagnosed should definitely be considered. The differential diagnosis for recalcitrant CRS includes underlying allergic rhinitis, aspirin-exacerbated respiratory disease (AERD), gastroesophageal reflux disease (GERD), mucociliary dysfunction, biofilms, autoimmune disease, and immunodeficiency, to mention a few. A thorough history and physical exam, including rigorous evaluation with angled endoscopes, will help the clinician assess previous surgical completeness as well as guide further medical workup for the aforementioned disease processes.
Allergic Rhinitis/Inhalant Allergy
The relationship between allergic rhinitis and CRS is controversial. The association of allergy and CRS has been reported from 25 to 50 %, which is greater than the prevalence in the general population [1]. Batra et al. found an overall prevalence of inhalant allergy in 38.7 % of the patients undergoing revision ESS for refractory CRS [2]. Both allergic rhinitis and CRS with nasal polyposis have been shown to have a similar underlying pathophysiology driven by a shift in the immune system with a skewed T-helper 2 cell cytokine profile. Allergy could potentially lead to or exacerbate CRS by causing generalized inflammation of the mucosa and obstruction of the sinus ostia. It therefore stands to reason that targeting the allergies and improving any component of inflammation for which allergies may be responsible for could help in the overall management of CRS. Of note, there is large overlap in the symptoms of allergic rhinitis and CRS; this can complicate the assessment of patients for subjective improvement following treatment of sinus disease.
In a case of recalcitrant CRS where the history suggests a possible allergic component, allergy testing is recommended. Allergy should be considered when patients have seasonal symptoms, itching of the nose and eyes, conjunctivitis, nasal congestion, sneezing, or established environmental triggers. Allergy testing can be conducted by skin testing (intradermal, skin prick, or scratch) or by in vitro serologic testing such as modified radioallergosorbent (mRAST). In appropriate cases, immunotherapy (IT) should be initiated by an otolaryngologist or allergist. IT has been shown to improve both clinical measures (radiographic and endoscopic scores, fewer revision surgeries, fewer office visits) and symptoms of CRS when used in addition to traditional therapies [3]. The evidence-based literature up to this point is weak, however, and more data in the form of randomized controlled trials is required.
Aspirin-Exacerbated Respiratory Disease (AERD)
AERD is a disease process with a constellation of clinical symptoms including aspirin (ASA) sensitivity, nasal polyposis, and asthma, also known as “Samter’s triad.” Patients with AERD have abnormal arachidonic acid metabolism resulting in an overproduction of proinflammatory leukotrienes through the 5-lipoxygenase pathway [4, 5]. Aspirin inhibits cyclooxygenase, thereby decreasing prostaglandin-E2, which normally inhibits leukotriene production and also prevents mast cell degranulation [4, 5]. The inhibition of cyclooxygenase by aspirin thus triggers exacerbations.
In general, the CRSwNP component of AERD (Fig. 8.1) is treated with topical and systemic steroids with a large portion of patients failing purely medical therapy and requiring ESS. Surgery is rarely curative as this disease process represents one of the most recalcitrant forms of CRS with 37 % of the patients requiring revision surgery at 5 years and 89 % at 10 years [6]. This is compared to CRSwNP without ASA triad or asthma in which 10 % of the patients required revision surgery at 5 years and 17 % at 10 years [6].
Postoperative care for this subset of patients is a controversial topic. Many otolaryngologists utilize high-dose topical steroid irrigations in controlling the recurrence of this disease. However, one study has demonstrated that budesonide nasal irrigations have not been shown to alter postoperative recurrence of the disease at 1 year [7]. More research is needed to establish what effect, if any, high-dose nasal steroid irrigations have on disease progression and the need for revision surgery.
More recently, ASA desensitization has shown promise for patients with CRS and AERD. Aspirin desensitization and daily aspirin maintenance have been established as beneficial in the management of CRSwNP in patients with AERD [5, 8]. ASA desensitization has been shown to have a positive impact on endoscopic polyp scores and is associated with both a decreased frequency of sinus surgeries and sinus infections [5]. The process of ASA desensitization is conducted as an inpatient, medical day unit or outpatient setting. Patients undergo a pretreatment regimen including optimization of pulmonary status, daily montelukast, and treatment of other concomitant conditions. ESS if needed should be timed 4–6 weeks prior to desensitization, as the therapy is more effective at preventing the regrowth of polyps than at reducing polyp size. A challenge is given by increasing doses of ASA until a target dose (usually 325 mg) is reached. The patient is then maintained on a maintenance dose (650 mg twice a day) indefinitely or risk re-sensitization. This dose can then often be weaned after a month if there is adequate symptom response, and systemic corticosteroids are reduced or eliminated [8].
Overall, ASA desensitization and ongoing maintenance therapy is tolerated in the majority of patients with only 8–23 % of the patients experiencing mild adverse events. Side effects including gastritis, dyspepsia, or epistaxis can be barriers to success. ASA desensitization has also shown a significant reduction of oral corticosteroid use by AERD patients and a significant improvement in subjective symptoms; however, double-blind randomized placebo-controlled studies are still necessary to prove causation [5].
Postoperative management in AERD and CRS should include twice-daily nasal saline irrigations with the addition of high-dose topical steroids at the discretion of the clinician. ASA desensitization should be considered in all AERD patients with severe or intractable symptoms or aggressive nasal polyp formation.
Gastroesophageal Reflux (GERD)
GERD has not been shown to cause or at least contribute to CRS. It is known to coexist in nearly half of the patients with postnasal drainage as a complaint, which can be misinterpreted by both patients and general practitioners as ongoing sinus disease [9]. However, GERD has been shown to be more prevalent in patients with refractive CRS than in patients with treatment responsive CRS and in healthy controls [10]. In addition, a few small studies have shown modest improvement of CRS symptoms in patients on once- or twice-daily proton pump inhibitor (PPI) therapy [10]. This suggests a possible causative effect that many feel represents contribution of reflux to underlying inflammation in the sinonasal tract. As such, in the setting of known GERD, symptoms suggestive of GERD, and/or findings on physical exam suggestive of GERD (flexible laryngoscopy findings), a referral for pH probe testing or initiation of PPI therapy should be considered.
Mucociliary Dysfunction
Most inherited forms of ciliary dysfunction, including Kartagener syndrome and cystic fibrosis (CF), are typically diagnosed in childhood. A detailed history and physical exam including past medical history and family history may heighten suspicion for these syndromes in patients with recalcitrant CRS. In the event of elevated suspicion, further testing for evaluation of Kartagener syndrome or CF should be considered. A referral to genetics for further genetic testing and counseling is necessary for any positive or equivocal test results.
Kartagener syndrome is a primary form of ciliary dyskinesia due to an abnormality in the dynein arm and is diagnosed by the saccharine mucociliary transport test or nasal biopsy with electron microscopy. It is associated with recurrent lung, ear, and sinonasal infections in children as well as hyposmia, infertility, and the findings of situs inversus and dextrocardia.
CF, an autosomal recessively inherited disease, results in secondary ciliary dysmotility by altering the viscosity of mucous through the disruption of transmembrane transport of chloride ions. The body’s mucociliary transport mechanisms are not efficient with this more viscous form of mucous. Recurrent Pseudomonas aeruginosa and Staphylococcus aureus colonization and infections are common. CF is typically diagnosed in childhood in the setting of bronchiectasis, recurrent pulmonary infections, CRS, malabsorption, and stunted growth. CF should be ruled out in any child that presents with nasal polyps. Diagnosis is made through newborn screening, sweat testing, and/or genetic testing. CT imaging in CF will often reveal hypoplastic sinus cavities with mucosal thickening and sclerosis and thickening of the adjacent bony framework (Fig. 8.2). Some less severe phenotypes of CF may not be diagnosed until adulthood and should be in the differential diagnosis in refractory CRS.
The management of CF is difficult and requires a multidisciplinary approach. As the pathophysiology of this disease results in a chronic process, the management of CRS is primarily medical. However, many patients fail medical management and require a surgical approach. In general, the indications for ESS are sinus disease that is contributing to pulmonary exacerbations and declining pulmonary function, medically refractory polyposis with nasal obstruction, and lung transplant candidacy [11, 12]. As the survival of cystic fibrosis patients continues to increase, this number will likely increase. Larger surgical openings are generally advocated for the refractory CF patient with significant CRS.
Biofilms
Certain common bacterial species including Staphylococcus aureus and Pseudomonas aeruginosa are capable of forming biofilms. Bacterial biofilms are defined as an assemblage of microbial cells enclosed in a self-produced polymeric matrix that is irreversibly associated with an inert or living surface [13]. The organized communities of bacteria attached to the sinonasal mucosa can then release planktonic bacteria that create acute exacerbations. The adherent and organized nature of the biofilm imparts a resistance to standard oral antibiotics.
The confirmation of the presence of biofilms depends on identification by scanning electron microscopy, confocal laser microscopy, or transmission electron microscopy, which are not accessible in the clinical setting. As such, the diagnosis is more often made with positive cultures for typical biofilm forming species in the setting of recalcitrant disease. CRS patients with biofilms have been shown to have more severe disease both preoperatively and postoperatively suggesting a role in recalcitrant disease [14].
Studies looking at topical antibiotic therapies have shown mixed results in patients with CRS. Various surfactants including 1 % baby shampoo in normal saline and manuka honey have shown some promising results in overall symptom control and antibiofilm activity; however, more research is necessary to establish evidence-based recommendations [15].
Immunodeficiency
Patients with immunodeficiency have recalcitrant disease because of their underlying immune disorder. Recurrent sinopulmonary infections are the most prevalent infections among primary immunodeficiency patients. CRS can be seen in common variable immunodeficiency (CVID), selective IgA deficiency, IgG subclass deficiency, and specific polysaccharide antibody deficiency [16]. CVID is the most common symptomatic primary immunodeficiency in adults and has been observed in up to 10 % of patients with refractory CRS [16, 17]. Further, more than 20 % of patients with CRS have lower than normal levels of one or more immunoglobulins [18].
Evaluation for immunodeficiency should be considered in patients with frequently recurrent, persistent, and/or severe infections or recalcitrant rhinosinusitis with rare organisms. These patients may also have associated atopy, autoimmune disease, or gastrointestinal disease. The importance of identifying an underlying immunodeficiency cannot be stressed enough as the management changes drastically. More judicious use of antibiotics, both prophylactic and culture directed, should be used, and IVIG may be indicated in certain situations. Once identified, these patients should be monitored in coordination with an immunologist.
Revision Surgery
As mentioned, sometimes more surgery can offer an advantage in the management of the refractory CRS patient who is not doing well after a prior surgical intervention. Both the endoscopic exam and repeat CT imaging will characterize when the etiology for failure is anatomic. The decision to proceed with revision surgery should be made on an individual basis depending on the underlying contributing factors. Symptomatic patients with obstruction on imaging or symptomatic patients with a significant disease burden are likely to be good candidates. The role of revision surgery in CRS is to improve medical management by reducing disease load and improving access for irrigations and topical therapies.
It has been estimated that 8–20 % of patients undergoing ESS will require revision surgery [19, 20]. Multiple studies have reviewed the common anatomic reasons for revision surgery. Musy reported the most common anatomic factors leading to revision surgery were lateralization of the middle turbinate (78 %), incomplete anterior ethmoidectomy (64 %), scarred frontal recess (50 %), incomplete posterior ethmoidectomy (41 %), and middle meatal antrostomy stenosis (39 %) [21]. Gore et al. noted residual anterior and posterior ethmoid cells or septations (75 %), a residual uncinate process (64 %), residual agger nasi cells (64 %), unopened sphenoid sinuses (53 %), and frontal cells (45 %) on preoperative imaging of patients undergoing revision surgery [22]. Bassiouni identified the most common location for polyp recurrence to be in the frontal sinus or frontal recess (55 %) followed by the ethmoid cavity (38 %) [23].
Revision surgery of the maxillary sinus is most often required when there is a residual uncinate process or a surgically created opening into the sinus not confluent with the natural ostium. The latter predisposes to recirculation of mucus from the natural opening back into the sinus via the “false” surgical opening, predisposing the patient to recurrent infections. A remnant uncinate can result in a bridge of tissue between the natural os and the surgical antrostomy causing recirculation (Fig. 8.3). Recirculation can also occur secondary to scarring or incomplete initial antrostomy. Another cause of maxillary sinus obstruction is persistent infraorbital ethmoid cells (Haller cells). These cells can be overlooked due to a more anterior position than expected. A 30° scope can be utilized to both ensure the natural os is included in the antrostomy and that there is not a residual Haller cell.
Although total ethmoidectomy is not indicated in all patients undergoing primary endoscopic sinus surgery, most will undergo uncinectomy, anterior ethmoidectomy, and maxillary antrostomy if they have severe enough disease to necessitate surgery. In revision ethmoid surgery, the entire ethmoid labyrinth should be opened in a posterior to anterior fashion. Surgical navigation can be helpful to identify unopened cells and the location of the skull base and lamina papyracea. The strut of the horizontal segment of the basal lamella should remain intact to prevent lateralization of the middle turbinate. A curette should be used to ensure the medial bulla has been removed, and all of the bony partitions along the lamina should be removed to reduce the mucosal surface area for recurrent polyp growth. Mucosal preservation will reduce scarring and antrostomy stenosis; therefore, sharp dissection should be used to prevent mucosal stripping.
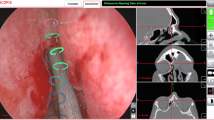
Patients with chronic frontal sinusitis should at minimum undergo resection of the agger nasi cell and complete excision of the superior uncinate process. Preoperative analysis of the frontal recess anatomy on imaging (especially using sagittal CT reconstructions) is particularly important to identify the drainage pathway and to identify reasons for failure. If the frontal recess is not obvious intraoperatively, an image-guided probe can be invaluable. Once identified, synechiae and bone fragments can be cut and removed. Curettes can be used to take down the beak anteriorly. A lateralized middle turbinate (Fig. 8.4) can often be an iatrogenic cause for frontal sinusitis; this can be addressed by medialization with a stitch (pexy), spacer, or middle turbinate resection. The frontal sinus rescue procedure has also been described as a method to prevent recurrent stenosis [24]. More recently, aggressive management of the frontal recess by Draf 3/modified Lothrop/frontal drillout procedure has been shown to reduce long-term (>12 months) polyp recurrence, especially in more complicated patients with asthma and AERD [23].
(a) Lateralized middle turbinate remnant (arrows) obstructing the frontal recess bilaterally in the setting of AERD with recurrent polyps. (b) Lateralized middle turbinate remnant (m) obstructing the right frontal sinus. Posterior septal defect (s) and synechiae (arrow) secondary to previous surgery. (c) Right frontal recess (f) after medialization of the middle turbinate (m) and balloon dilation
The sphenoid sinus may be obstructed from stenosis and scarring. The location of the natural os can be identified medial to the superior turbinate or turbinate remnant. Image guidance may be helpful. A large sphenoidotomy should be created in revision surgery to reduce the risk of restenosis and to allow for adequate topical drug delivery. This should be accomplished in a medial and inferior direction using through-cutting instruments and good visualization to avoid vascular injury and to cut through the thick sphenoid bone.
Overall, the goals of revision surgery are to widely open obstructed sinus cavities, decrease disease burden by removing bulky polypoid tissue, remove residual cells and partitions that are acting as a nidus for infection or polyposis, and improve access for irrigations and topical therapies.
Topical Drug Delivery
Arguably, medical therapies for CRS are the strongest weapons in the veritable armamentarium of each physician and represent the true “workhorse” in the management of this chronic disease. Irrigations act by removing antigens, mucus, bacteria, and pollutants from the sinonasal mucosa. Topical therapies allow for direct application of medication to the diseased tissue at an increased concentration with decreased systemic absorption and associated side effects than systemic therapies. Topical therapy does however have limitations including variable penetration into the sinuses, adverse effects such as discomfort and epistaxis, and a need for education on the appropriate technique for mixing and using each therapy. All of which can limit compliance.
Delivery of irrigant into unoperated paranasal sinuses has been shown to be quite limited; the frontal and sphenoid sinuses are essentially not accessible, and high-flow devices provide some infiltration to the maxillary and ethmoid sinuses [25]. ESS allows for improvement in access for topical drug delivery, though the degree depends on the extent of surgery. Multiple types of therapies have been proposed as means to topically treat CRS including corticosteroids, antibiotics, and antifungals. The more commonly used medications and doses are listed in Table 8.1. Multiple delivery devices exist as well and are described below.
Nasal Saline
Nasal saline irrigations both preoperatively and postoperatively have become a standard of care. Evidence has established that irrigating with saline can improve symptoms and quality of life both before and after surgery [15]. High-volume (≥200 mL) low-pressure irrigations have been shown to be more effective than low-volume low-pressure delivery systems. Hypertonic and isotonic solutions have been shown to be fairly equivocal in regard to symptom management [30]. It is important to note that nasal saline irrigations are often used as an adjuvant to other medical therapies for CRS and not in isolation. Fortunately, nasal saline is well tolerated with few side effects and is inexpensive.
Intranasal Steroids
Numerous metered-dose topical steroid sprays exist and include triamcinolone acetonide, fluticasone propionate, mometasone furoate, fluticasone furoate budesonide, and beclomethasone dipropionate monohydrate. In both CRSsNP and CRSwNP, metered-dose nasal steroid sprays improve both subjective and objective outcomes in patients including better endoscopy scores and significant decrease in polyp size [15]. Further, patients with sinus surgery had significantly greater reduction in polyp size while on nasal steroid sprays than did patients without sinus surgery [31]. Overall, metered-dose nasal steroid sprays are well tolerated; however, they have been associated with epistaxis and headache which may limit their use. The well-established benefit from this medical therapy, which is relatively safe (limited systemic absorption) and inexpensive, has made it another standard in the management in CRSwNP.
In an attempt to increase both the volume and concentration of steroid delivered topically to the mucosa, some physicians advocate irrigation with steroids such as budesonide mixed with saline, particularly in the setting of more recalcitrant forms of CRS. Not as much evidence exists for steroid irrigations as does for metered-dose nasal sprays, but at least one large case series has shown that postoperative use of budesonide or betamethasone in high-volume irrigation provides improvement in quality of life, symptoms, and endoscopy scores [32]. Another retrospective review showed that patients experienced worsening symptoms and endoscopy findings when not using budesonide irrigations despite the use of metered-dose nasal steroid sprays [33]. Studies have shown that twice-daily budesonide irrigations do not cause an appreciable change in serum or urine cortisol or significantly suppress adrenal function [15]. As these therapies are “off label” and not approved by the FDA, they can be prohibitively expensive which is a major disadvantage.
Antibiotics
Systemic antibiotics are a mainstay of treatment for acute exacerbations of CRS. The idea of topical delivery of antibiotics for chronically infected sinuses is appealing as the systemic side effect of antibiotics can be avoided. The literature is fairly mixed however, on the efficacy and role of topical antibiotic therapies. In their systematic review, Rudmik et al. identified three randomized controlled trials which were heterogenous in the antibiotics used and the methods of delivery; all of the studies failed to show any benefit of a topical antibiotic over placebo [15]. Other studies have shown that irrigation with topical antibiotics is effective in CRS [34–36].
Certain patient populations appear to derive a clearer benefit from topical antibiotics. One such population is patients with CF and pseudomonal infections. These patients have improved outcome scores and a decreased need for revision surgery while on tobramycin irrigations [28, 35]. Another population is those with chronic Staphylococcus aureus infection in the setting of CRS. Irrigation with 0.05 % mupirocin mixed in saline has been shown to decrease biofilm burden and improve endoscopic and symptoms scores [37, 38]. Despite these promising results, reinfection rates remain high in this subgroup [27].
Antifungals
It has been hypothesized that fungal elements contribute to mucosal inflammation in a subset of patients with CRS. Certainly, fungus plays a role in allergic fungal sinusitis, but a contribution to other types of chronic sinus disease has not been established and largely fallen out of favor.
While one study has shown improvement in endoscopy scores and CT scores in patients irrigating with amphotericin B versus placebo, four separate randomized controlled trials and two meta-analyses have shown no statistically significant difference between topical amphotericin B over placebo in regard to clinical outcomes [15]. Further, a Cochrane Review failed to show any benefit with either topical or systemic antifungals in CRS [39]. Topically delivered antifungals can cause adverse events such as nasal burning, epistaxis, and even exacerbation of CRS; therefore, the use of this therapy is not recommended as the risks appear to outweigh any benefits.
Delivery Devices
As stated above, ESS is a necessary prerequisite to allow for delivery of topical substances into the sinuses. Multiple delivery devices exist and can be classified by low-volume and high-volume delivery.
Low-Volume Devices and Properties
Low-volume delivery devices include metered-dose/nasal pump sprays and nebulizers. Each delivers a small volume of substance to the nasal cavities in either a spray or mist form. Numerous factors influence the delivery of particles to the paranasal sinuses and include a smaller particle size between 3 and 10 μm, higher flow rates, and ostial size (greater than 3.95 mm is necessary for maxillary penetration) [26]. Nasal sprays typically produce droplets 50–100 μm in size, and therefore, the vast majority of these particles are deposited in the anterior nasal cavity [26]. Nebulizers can produce particles of various sizes, and studies have shown improved particle deposition in the posterior nasal cavity and at the ostiomeatal complex when compared to metered-dose/nasal pump sprays [26].
High-Volume Devices and Properties
High-volume delivery devices include the squeeze bottle and the neti pot. The major difference between the two is that the volume is delivered by high pressure versus low pressure, respectively. In several studies, high-volume delivery devices have outperformed low-volume delivery devices in penetration into postoperative sinus cavities [26]. However, when comparing the neti pot to the squeeze bottle, or the low-pressure system to the high-pressure system, outcomes have been mixed with one outperforming the other in one study and in another study showing the reverse [40].
Other Delivery Devices
Topical drug delivery is an evolving field with many new up and coming products. These include drug-eluding stents (Fig. 8.5), dissolvable drug-saturated packing, and dissolvable drug-concentrated foam to name a few. As these products are fairly recent innovations, ultimately more study is required to determine their efficacy in CRS.
A key point that should be underscored on the use of topical therapy is that up until now, investigations in this field have revolved around delivery into the sinus cavities. Little study has been done on the delivery of the active agent into the diseased tissues themselves (mucosa, polyps, etc.). As some recent studies have highlighted, any irrigant which enters into a sinus cavity stays for a very brief period of time before most of the solution flows out. A solution simply entering the sinus cavity is therefore likely a poor proxy for mucosal drug delivery [25]. Simply put, how much active drug is getting into the diseased tissue in the setting of polyposis, infection, etc. is the central question. A more sophisticated approach to study and practice of topical sinus drug delivery is desperately needed.
Conclusion
When faced with a patient who is not responding to maximal medical and surgical therapy, it is important to take a step back and approach them with a number of considerations. If the patient had surgery, it is essential to closely examine the sinonasal cavity for anatomic factors contributing to failure. The value of a thorough past medical history, family history, and review of systems with the goal of identifying underlying undiagnosed medical comorbidities cannot be overstated. Finally, consideration of the different topical therapies and an understanding of how various delivery mechanisms can impact sinus drug distribution are essential in these patients. Exploring factors related to therapeutic reasons for failure provides a deeper understanding of the patient’s condition and can uncover opportunities to more effectively manage recalcitrant disease.
References
Benninger MS, Ferguson BJ, Hadley JA, et al. Adult chronic rhinosinusitis: definitions, diagnosis, epidemiology, and pathophysiology. Otolaryngol Head Neck Surg. 2003;129:S1–32.
Batra PS, Tong L, Citardi JL. Analysis of comorbidities and objective parameters in refractory chronic rhinosinusitis. Laryngoscope. 2013;123:S1–11.
DeYoung K, Wentzel JL, Schlosser RJ, Nguyen SA, et al. Systematic review of immunotherapy for chronic rhinosinusitis. Am J Rhino Allergy. 2014;28:145–50.
White AA, Stevenson DD. Aspirin-exacerbated respiratory disease: update on pathogenesis and desensitization. Semin Respir Crit Care Med. 2012;33:588–94.
Xu JJ, Sowerby L, Rotenberg BW. Aspirin desensitization for aspirin-exacerbated respiratory disease (Samter’s Triad): a systematic review of the literature. Int Forum All Rhinol. 2013;3:915–20.
Mendelsohn D, Jeremic G, Wright ED, Rotenberg BW. Revision rates after endoscopic sinus surgery: a recurrence analysis. Ann Otol Rhinol Laryngol. 2011;120:162–6.
Rotenberg BW, Zhang I, Arra I, Payton KB. Postoperative care for Samter’s triad patients undergoing endoscopic sinus surgery: a double-blinded, randomized controlled trial. Laryngoscope. 2011;121:2702–5.
Williams AN, Woessner KM. The clinical effectiveness of aspirin desensitization in chronic rhinosinusitis. Curr Allergy Asthma Rep. 2008;8:245–52.
Pawar S, Lim HJ, Gill M, et al. Treatment of postnasal drip with proton pump inhibitors: a prospective, randomized, placebo-controlled study. Am J Rhinol. 2007;21:695–701.
Lupa M, DelGaudio JM. Evidence-based practice: reflux in sinusitis. Otolaryngol Clin North Am. 2012;45:983–92.
Nishioka GJ, Cook PR. Paranasal sinus disease in patients with cystic fibrosis. Otolaryngol Clin North Am. 1996;29:193–205.
Shatz A. Management of recurrent sinus disease in children with cystic fibrosis: a combined approach. Otolaryngol Head Neck Surg. 2006;135:248–52.
Sanclement JA, Webster P, Thomas J, et al. Bacterial biofilms in surgical specimens of patients with chronic rhinosinusitis. Laryngoscope. 2005;115:578–82.
Singhal D, Psaltis AJ, Foreman A, Wormald PJ. The impact of biofilms on outcomes after endoscopic sinus surgery. Am J Rhinol All. 2010;24:169–74.
Rudmik L, Hoy M, Schlosser RJ, et al. Topical therapies in the management of chronic rhinosinusitis: an evidence-based review with recommendations. Int Forum Allergy Rhinol. 2013;3:281–98.
Ocampo CJ, Peters AT. Antibody deficiency in chronic rhinosinusitis: epidemiology and burden of illness. Am J Rhinol Allergy. 2013;27:34–8.
Chee L, Graham SM, Carothers DG, et al. Immune dysfunction in refractory sinusitis in a tertiary care setting. Laryngoscope. 2001;111:233–5.
Vanlerberghe L, Joniau S, Jorissen M. The prevalence of humoral immunodeficiency in refractory rhinosinusitis: a retrospective analysis. B-ENT. 2006;2:161–6.
Marchioni D, Alicandri-Ciufelli M, Mattioli F, et al. Middle turbinate preservation versus middle turbinate resection in endoscopic surgical treatment of nasal polyposis. Acta Otolaryngol. 2008;128:1019–26.
McMains KC, Kountakis SE. Revision functional endoscopic sinus surgery: objective and subjective surgical outcomes. Am J Rhinol. 2005;19:344–7.
Musy PY, Kountakis SE. Anatomic findings in patients undergoing revision endoscopic sinus surgery. Am J Otolaryngol. 2004;25(6):418–22.
Gore MR, Ebert Jr CS, Zanation AM, Senior BA. Beyond the “central sinus”: radiographic findings in patients undergoing revision functional endoscopic sinus surgery. Int Forum Allergy Rhinol. 2013;3(2):139–46.
Bassiouni A, Wormald PJ. Role of frontal sinus surgery in nasal polyp recurrence. Laryngoscope. 2013;123(1):36–41.
Citardi MJ, Javer AF, Kuhn FA. Revision frontal sinusotomy with mucoperiosteal flap advancement: the frontal sinus rescue procedure. Otolaryngol Clin North Am. 2001;34(1):123–32.
Harvey RJ, Goddard JC, Wise SK, Schlosser RJ. Effects of endoscopic sinus surgery and delivery device on cadaver sinus irrigation. Otolaryngol Head Neck Surg. 2008;139:137–42.
Liang L, Lane AP. Topical drug delivery for chronic rhinosinusitis. Curr Otorhinolaryngol Rep. 2013;1:51–60.
Jervis-Bardy J, Wormald PJ. Microbiological outcomes following mupirocin nasal washes for symptomatic, Staphylococcus aureus with mupirocin irrigations. Int Forum Allergy Rhinol. 2012;2:111–5.
Desrosiers MY, Salas-Prato M. Treatment of chronic rhinosinusitis refractory to other treatments with topical antibiotic therapy delivered by means of a large-particle nebulizer: results of a controlled trial. Otolaryngol Head Neck Surg. 2001;125(3):265–9.
Sacks 4th PL, Harvey RJ, Rimmer J, Gallagher RM, et al. Antifungal therapy in the treatment of chronic rhinosinusitis: a meta-analysis. Am J Rhinol Allergy. 2012;26(2):141–7.
Pynnonen MA, Mukerji SS, Kim HM, et al. Nasal saline for chronic sinonasal symptoms: a randomized controlled trial. Arch Otolaryngol Head Neck Surg. 2007;133:1115–20.
Snidvongs K, Kalish L, Sacks R, et al. Topical steroid for chronic rhinosinusitis without polyps. Cochrane Database Sys Rev. 2011;10(8):CD009274.
Snidvongs K, Pratt E, Chin D, et al. Corticosteroid nasal irrigations after endoscopic sinus surgery in the management of chronic rhinosinusitis. Int Forum Allergy Rhinol. 2012;2:415–21.
Jang DW, Lachanas VA, Segel J, Kountakis SE. Budesonide nasal irrigations in the postoperative management of chronic rhinosinusitis. Int Forum Allergy Rhinol. 2013;3:708–11.
Lim M, Citardi MJ, Leong JL. Topical antimicrobials in the management of chronic rhinosinusitis: a systematic review. Am J Rhinol. 2008;22(4):381–9.
Moss RB, King VV. Management of sinusitis in cystic fibrosis by endoscopic surgery and serial antimicrobial lavage. Reduction in recurrence requiring surgery. Arch Otolaryngol Head Neck Surg. 1995;121(5):566–72.
Vaughan WC, Carvalho G. Use of nebulized antibiotics for acute infections in chronic sinusitis. Otolaryngol Head Neck Surg. 2002;127(6):558–68.
Le T, Psaltis A, Tan LW, Wormald PJ. The efficacy of topical antibiofilm agents in a sheep model of rhinosinusitis. Am J Rhinol. 2008;22:560–7.
Uren B, Psaltis A, Wormald PJ. Nasal lavage with mupirocin for the treatment of surgically recalcitrant chronic rhinosinusitis. Laryngoscope. 2008;118:1677–80.
Sacks PL, Harvey RJ, Rimmer J, Gallagher RM, Sacks R. Topical and systemic antifungal therapy for the symptomatic treatment of chronic rhinosinusitis. Cochrane Database Syst Rev. 2011;(8):CD008263.
Abadie WM, McMains KC, Weitzel EK. Irrigation penetration of nasal delivery systems: a cadaver study. Int Forum Allergy Rhinol. 2011;1:46–9.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Halderman, A.A., Stokken, J., Sindwani, R. (2015). Management of Functional Endoscopic Sinus Surgery (FESS) Failures. In: Batra, P., Han, J. (eds) Practical Medical and Surgical Management of Chronic Rhinosinusitis. Springer, Cham. https://doi.org/10.1007/978-3-319-16724-4_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-16724-4_8
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-16723-7
Online ISBN: 978-3-319-16724-4
eBook Packages: MedicineMedicine (R0)