Abstract
Endothelium is formed by a contiguous network of cells that separate the circulation from the underlying tissue. Cells within the endothelial network collaborate to relay chemical and mechanical signals between blood and tissue. Each of these cells is highly specialized. Such specialization is seen in endothelial cell growth, where some cells are highly proliferative, others less so, and some display no growth potential at all. The highly replication competent cells fulfill the criteria of a “progenitor.” Progenitor cells have important implications for vascular maintenance and for vascular repair following injury. This chapter examines the current state of knowledge regarding endothelial cell progenitor cells found within lung capillaries and identifies knowledge gaps within the field that are ongoing areas of research.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
The pulmonary circulation is a unique vascular bed; it receives 100 % of the cardiac output from the right ventricle while maintaining low vascular pressures. Even with intense exercise, when cardiac output increases 5–8-fold, pulmonary artery pressure increases only modestly. The ability to maintain low pressures even in the face of high cardiac outputs is partly attributable to the vast surface area of the lung capillaries, their ability to distend, and the ability to recruit blood into capillaries that are not otherwise continuously perfused. Indeed, blood flow through individual capillaries is intermittent and subject to active regulation in order to match ventilation with perfusion to optimize gas exchange. Such specialization of the lung’s capillaries has fascinated investigators since their original discovery in 1661 by Marcello Malpighi (West 2013).
We now know that endothelium contributes to the alveolar-capillary membrane, where capillary endothelial cells and type I pneumocytes border one another through a fused basement membrane. However, this association was impossible to fully appreciate until development of the electron microscope allowed for high-resolution analysis of intact anatomy. Cell biology and physiology studies of lung capillary endothelium have only recently been advanced. This ongoing work indicates that the lung capillary endothelium represents a highly specialized, differentiated cell phenotype (Stevens 2005; Gebb and Stevens 2004). One of the unique features of this cell is its high replication competence and the ability to self-renew (Alvarez et al. 2008). Highly replication competent cells that self-renew are features of progenitor cells, meaning that lung capillary endothelium constitutes an important progenitor cell niche. Here, we highlight evidence that lung capillary endothelium represents a progenitor cell niche, and we discuss the physiological demands for rapid neoangiogenesis in the alveolar-capillary compartment.
2 Stem Cells
Genetic evidence for the existence of stem cells arose from studies examining hematopoietic cells (Becker et al. 1963; Till 1961; Wu et al. 1968a, b). During these experiments, investigators discovered colonies of progenitor cells, each derived from a single clonogenic precursor, in the spleens of conditioned hosts. The colonies were composed not only of differentiated cells, but also cells that could be used to reconstitute all blood cell lineages. From these initial studies, numerous investigations ensued revealing that stem cells are very unique cells that have the potential to self-renew, that is, to divide and create additional stem cells or to differentiate into mature cells of any particular cell lineage. Stem cells will either go through symmetric cell division giving rise to two daughter cells that remain undifferentiated or perform asymmetric cell division to become differentiated. This unique characteristic of stem cells is vital in the generation of specialized cells forming different types of tissues, in addition to continually renewing normal tissue and repairing injured tissue (Reya et al. 2001).
There are two major types of stem cells. The first type is an embryonic stem cell, which is found in the inner cell mass of the mammalian blastocyst. Embryonic stem cells are able to differentiate into the three types of germ layers which are the ectoderm (gives rise to the skin and neural lineages), mesoderm (generates blood, bone, muscle, cartilage, and fat), and endoderm (contribute to tissues of the respiratory and digestive tracts) along with having the capability to infinitely grow (Wagers and Weissman 2004). Specific signaling mechanisms between stem cells, their progeny, and the surrounding tissues guarantee that the correct amount of new cells will be formed within the proper locations. This is especially important during development when the embryonic stem cells are induced down a specific cell lineage pathway as opposed to all the other lineage pathways through intercellular cross-talk (Fuchs and Segre 2000).
Stem cell hierarchy determines the potential of the stem cell to differentiate into varying cell types. The earliest stem cells in the hierarchy are totipotent stem cells, which are capable of differentiating into all embryonic and extra-embryonic cell types. Totipotent stem cells give rise to pluripotent stem cells that are able to give rise to all cell types of the embryo proper. Pluripotent stem cells generate multipotent stem cells, which are progenitor cells within the same embryonic layer. Multipotent stem cells further differentiate into stem cells that are incapable of self-renewal, called oligolineage progenitors. Oligolineage progenitors only have the capacity to divide into one particular cell lineage and give rise to progeny that are more restricted in their differentiating potential. A hallmark of both stem and progenitor cells is their ability to proliferate and give rise to functional progeny; however, progenitor cells are unable to infinitely divide like stem cells (Weissman 2000). Finally, unipotent cells are produced that are only able to contribute one mature cell type.
In contrast to embryonic stem cells, the second type of stem cell, the adult stem cell, resides within an adult organ or tissue and is only able to select a differentiation program from a few possible pathways (Fuchs and Segre 2000). Adult stem cells include the somatic stem cell and the germ stem cell (Takahashi and Yamanaka 2006). Although the majority of the diversification of various cell types is carried out at or shortly after birth, adult tissues must still be regenerated during adult life from stem cell to progenitor cell to functional progeny. Therefore, populations of stem cells must be present to undergo self-renewal as well as select for a particular differentiation program to replenish dying cells and regenerate damaged tissues (Fuchs and Segre 2000; Takahashi and Yamanaka 2006; Weissman et al. 2001). For this reason, adult stem cells are frequently localized to specific microenvironments called stem cell niches. External and intrinsic cues within these niches act on the adult stem cells to alter gene expression and induce self-renewal or terminal differentiation (Fuchs and Segre 2000).
Pioneering studies performed by Yamanaka and Takahashi (2006) have shown that differentiated somatic cells can be reprogrammed to an undifferentiated state leading to the formation of pluripotent stem cells. Pluripotent stem cells are able to differentiate into any of the three types of embryonic layers. Through the introduction of Oct3/4, Sox2, c-Myc, and Klf4 under embryonic stem cell conditions, pluripotent stem cells can be induced, which exhibit normal embryonic stem cell morphology. They proliferate indefinitely in culture, as well as express genes characteristic of embryonic stem cells. Because of these qualities, inducible pluripotent cells are useful in disease models along with drug development and transplantation medicine (Yamanaka and Takahashi 2006).
3 Endothelial Progenitor Cells
A landmark study was performed in 1997 by Asahara et al. (1997) examining adult human peripheral blood for a circulating progenitor cell capable of differentiating into endothelial cells. Asahara et al. (1997) documented a particular group of human-circulating cells that had become endothelial cell-like in culture and were able to engraft into injured vessels. These particular cells were then termed “endothelial progenitor cells.” Therefore, the authors concluded that some circulating cells in peripheral blood have the potential to serve as progenitors of the endothelial lineage. This paper defined endothelial progenitor cells as cells having key criteria, such as displaying CD34, Tie-2, CD31, UEA-1, ac-LDL, and expressing CD45 in certain instances (Asahara et al. 1997).
For nearly two decades, the term “endothelial progenitor cell” was used to broadly describe a heterogeneous group of circulating cells that putatively give rise to endothelial cells in vitro or in vivo. Studies have shown over the years that there are two main categories of endothelial progenitor cells. The first category is a heterogeneous population of hematopoietic cells that display crucial paracrine angiogenic activity called pro-angiogenic hematopoietic progenitor cells (Chao and Hirschi 2010; Duong et al. 2011; Richardson and Yoder 2011). The second category is endothelial colony-forming cells, which are capable of generating blood vessels de novo.
Recent evidence has revealed that the original endothelial progenitor cells identified by Asahara et al. (1997) were most likely circulating pro-angiogenic hematopoietic progenitor cells (Medina et al. 2010). These cells have been shown to correlate with the degree of diseases such as cardiovascular disease and pulmonary hypertension (Asosingh et al. 2008; Hill et al. 2003; Kissel et al. 2007). Studies have also demonstrated that pro-angiogenic hematopoietic progenitor cells originate from the bone marrow, circulate within the peripheral blood, and temporarily engraft themselves into injured host vessels (Asahara et al. 1997; Hristov and Weber 2004; Lin et al. 2000). Although pro-angiogenic hematopoietic cells exhibit some properties of endothelial cells, they are not capable of vessel formation (Yoder et al. 2007).
Numerous methods have been developed to properly identify endothelial progenitor cells, including various combinations of cell surface markers, functional assays, and colony-forming assays; however, there is not a uniform definition of an endothelial progenitor cell (Hirschi et al. 2008). In 2004, Ingram et al. (2004) described a novel approach that identified endothelial progenitor cells based on their clonogenic and proliferative capacities rather than on the expression of cell surface antigens. After single-cell in vitro clonogenic assays were performed on both adult peripheral blood and umbilical cord blood, a hierarchy was discovered in both blood samples (Ingram et al. 2004). This growth hierarchy was similar to hematopoietic stem cells, and a second category of endothelial progenitor cells was discovered—cells which proliferate to form new blood vessels, called endothelial colony-forming cells (Chao and Hirschi 2010; Duong et al. 2011; Richardson and Yoder 2011).
Endothelial colony-forming cells possess true endothelial progenitor cell characteristics because they are highly proliferative, form blood vessels de novo, and contribute to endothelialization and angiogenesis (Basile and Yoder 2014). The endothelial colony-forming cells found in the umbilical cord blood were capable of achieving at least 100 population doublings, form re-platable secondary and tertiary colonies, and retain high levels of telomerase activity. Overall, the endothelial colony-forming cells found within umbilical cord blood have a significantly higher proliferative potential compared to those isolated from the adult peripheral blood (Ingram et al. 2004; Yoder 2012).
Currently, it is unknown whether endothelial colony-forming cells are unipotent, multipotent, or a fully differentiated endothelial cell possessing a high proliferative potential (Duong et al. 2011). Similar to pro-angiogenic hematopoietic progenitor cells, endothelial colony-forming cells cannot be identified through specific cell markers, but they have been shown to express CD34, CD146, CD31, Flk-1, and CD105. Importantly, endothelial colony-forming cells do not express CD133 or CD45, which indicates that they are not hematopoietic cells (Ingram et al. 2004).
Along with peripheral and umbilical cord blood, endothelial colony-forming cells have been found within the endothelium of the umbilical vein, human aorta, and the pulmonary microvasculature (Alvarez et al. 2008; Ingram et al. 2005). In 2008, Alvarez et al. (2008) found that the pulmonary microvasculature is enriched with endothelial colony-forming cells that have a high proliferative potential, are able to reconstitute the entire hierarchy of growth potentials, and perform postnatal vasculogenesis while retaining their endothelial microvascular phenotype (Alvarez et al. 2008) (see Sect. 11.6). These findings suggest a progenitor cell niche within the pulmonary microvasculature that regenerates and repairs the pulmonary endothelium in order to maintain vascular homeostasis.
Recently, Prasain et al. (2014) derived cells possessing endothelial colony-forming cell-like properties from human iPS cells and human embryonic stem cells. These cells were NRP-1+CD31+ and displayed high clonal proliferative potential, angiogenic capacity, and significantly contributed to vascular repair of ischemic tissue. Additionally, Yoon et al. (2005) revealed that pro-angiogenic cells and endothelial colony-forming cells synergistically interact to perform vascular repair and neovascularization. Individually, both types of endothelial progenitor cells enhance angiogenesis; however, a combination of both cells has been found to yield the largest angiogenic response in both the mouse hind limb ischemia model and the Matrigel plug model (Yoon et al. 2005). Due to pro-angiogenic hematopoietic cells expressing greater amounts of pro-angiogenic cytokines, it has been suggested that these cells exert their pro-angiogenic effects via paracrine mechanisms interacting with endothelial colony-forming cells distributed throughout the tissue. In turn, endothelial colony-forming cells are activated by the pro-angiogenic chemokines to fulfill the reparative needs of the endothelium (Fig. 11.1) (Asosingh et al. 2008; Basile and Yoder 2014).
Proangiogenic hematopoietic cells may interact with resident endothelial progenitor cells to promote neoangiogenesis. Circulating hematopoietic (bone marrow-derived) cells are proposed to provide paracrine signals that stimulate resident endothelial cell colony-forming cells to undergo neoangiogenesis. Schematic adapted from Basile and Yoder (2014)
Questions remain as to the location (niche) of resident endothelial colony-forming cells within the vessel wall, and how these cells interpret tissue-specific cues to control development, neo-angiogenesis, and the response to injury. These issues are highly relevant to the pulmonary circulation, which possesses the largest vascular surface area and the highest number of endothelial cells among all internal organs. Even within the lung, endothelium changes structurally and functionally along the arterial-capillary-venous axis. The richest abundance of endothelial progenitors cells is found within the lung’s capillary segment.
4 Endothelial Heterogeneity in the Pulmonary Circulation
Although anatomical differences in endothelium lining pulmonary arteries, capillaries, and veins were widely acknowledged in the twentieth century (Crapo et al. 1982; Haies et al. 1981; Weibel 1973), in general, lung endothelium was considered to be a functionally inert, homogeneous layer functioning primarily as a semi-permeable barrier separating blood from the underlying tissue (Gebb and Stevens 2004). Evidence that the endothelium contributes to vasoregulation and metabolism, such as the conversion of angiotensin I to angiotensin II, directed a research focus on the “non-respiratory” functions of the lung (Pfannkuch and Blumcke 1985). These studies contributed to our understanding of functional heterogeneity among lung vascular compartments; for example, lung capillaries possess extensive angiotensin converting enzyme activity (Ryan et al. 1975, 1976; Ryan and Ryan 1984a). Recognition that certain lectins discriminate between pulmonary artery and microvascular endothelial cells provided a way to test whether these cells were phenotypically different in vivo, and ultimately led to a way to purify cell phenotypes in vitro (Gebb and Stevens 2004). Lectins are plant and animal proteins that recognize sugar moieties with nominal specificity, and therefore, differential lectin binding is indicative of distinctive cell surface molecular signatures. Simultaneous infusion of labeled Griffonia simplicifolia and Helix pomatia lectins revealed a distinctive border between endothelial cell phenotypes, where pulmonary artery endothelial cells preferentially interacted with Helix pomatia and capillary endothelial cells preferentially interacted with Griffonia simplicifolia. No apparent overlap in lectin binding was noted. Recent studies seeking to resolve the transition zone found that all endothelial cells in blood vessels less than 38 μm in diameter interacted with Griffonia lectin, whereas half of the endothelial cells in blood vessels 38–60 μm in diameter interacted with Griffonia lectin, and none of the endothelial cells in blood vessels >60 μm in diameter interacted with Griffonia simplicifolia (Wu et al. 2014). These data illustrated a stark transition zone between 38 and 60 μm diameter pulmonary arterioles where a shift in endothelial cell phenotype is observed (Fig. 11.2). This transition zone resides immediately before arterioles enter the capillary plexus.
Lung capillary endothelium is discriminated by Griffonia lectin, whereas precapillary endothelium possesses Weibel–Palade bodies. (a) The lung’s circulation was gelatin-filled and the airways were agarose-filled, thick sections were cut, and the lung slices were incubated with Griffonia lectin. Whereas endothelium lining extra-alveolar blood vessels does not interact with the lectin, capillary endothelium uniformly interacts with Griffonia simplicifolia. (b) Griffonia lectin reveals a zone, in blood vessels ranging from 38 to 60 μm, where the macrovascular endothelial cell phenotype transitions to a microvascular endothelial cell phenotype. Endothelium lining blood vessels smaller than 38 μm in diameter are uniformly Griffonia-positive, and endothelium in blood vessels greater than 60 μm in diameter is Griffonia-negative. (c) Weibel–Palade bodies are seen in precapillary endothelial cells, but are not seen in capillary endothelial cells. Adapted from Wu et al. (2014)
Weibel–Palade bodies are endothelial-specific organelles that contain many proteins important to the stimulated immune response, including P-selectin and von Willebrand factor (vWf). Interestingly, not all endothelial cells possess Weibel–Palade bodies. Fuchs and Weibel first recognized that lung capillary endothelial cells do not possess Weibel–Palade bodies, and more specifically, they found that the transition zone was in blood vessels with an approximately 20 μm internal diameter (Fuchs and Weibel 1966; Weibel 2012). The relationship between Weibel–Palade bodies and interaction with Griffonia lectin was recently compared in lung endothelium (Wu et al. 2014). In agreement with the results of Fuchs and Weibel (Fuchs and Weibel 1966; Weibel 2012), Weibel–Palade bodies were present in endothelium in small precapillary vessels, with internal diameters of approximately 18 μm. All of the endothelial cells in these blood vessels interacted with Griffonia lectin (Fig. 11.2). Thus, it appears that a macroheterogeneity among lung endothelial cell phenotypes is defined by recognition of the Griffonia lectin, although this molecular pattern does not designate the formation of Weibel–Palade bodies. These findings also resolve an important precapillary niche in lung endothelium, where a transition in phenotype occurs.
Recognition that changes in the structure of pulmonary artery and capillary endothelial cells are paralleled by distinct molecular signatures gave rise to the idea that not all endothelial cells within the pulmonary circulation are homogeneous in their function. The study of highly purified macro- and microvascular endothelial cell populations in culture has supported this view and provides insight into the rich source of endothelial progenitor cells seeded within lung capillaries.
5 Endothelial Heterogeneity: Insights Gained by the Study of Lung Endothelium in Culture
Mammalian cell isolation and culture has represented a breakthrough technology that is fundamental to identifying the molecular basis of cell physiology and pathophysiology. Endothelial cell cultures were not developed until the 1970s (Nachman and Jaffe 2004). Early endothelial cultures were generated from conduit-derived vessels, mostly from larger animals, because larger vessel segments were more easily accessible. What is considered normal endothelial cell identity in culture primarily arose from studies using aortic, pulmonary artery, and umbilical vein endothelial cells. In these primary cell lines, endothelial cells were shown to take up low-density lipoprotein (LDL) and to express proteins such as vWf, factor VIII, and platelet-endothelial cell adhesion molecule-1 (PECAM-1). More recently, expressions of the endothelial cell nitric oxide synthase (eNOS) and vascular endothelial cell cadherin (VE-cadherin) have been found useful in resolving endothelial identity.
Pioneering work by Ryan and colleagues paved the way for isolating capillary endothelial cells from the lungs of small animals (Habliston et al. 1979; Ryan and Ryan 1977, 1984b; Ryan et al. 1982). Using a peripheral lung cut technique and a bead retro-perfusion approach, Ryan’s group was able to obtain lung microvascular endothelial cells suitable for study in vitro. They tested the metabolic activity of these cells, including their ability to generate angiotensin II, since angiotensin-converting enzyme is largely expressed in lung capillary endothelium. These approaches have been widely adapted by investigators over the past four decades.
Comparison of lung “microvascular” (i.e., PMVECs) and “macrovascular” (PAECs) endothelial cells led to new insight in vascular biology (Stevens 2005; Gebb and Stevens 2004; King et al. 2004; Ochoa et al. 2010). Key to this insight, however, was rigorous characterization of the cell phenotype. Both PMVECs and PAECs display cobblestone morphology at confluence. Both cell types express markers characteristic of endothelium, including vWf, eNOS, VE-cadherin, and PECAM-1. However, PMVECs differ from PAECs with respect to their lectin-binding characteristics. PMVECs preferentially interact with Griffonia simplicifolia and Glycine max, whereas PAECs preferentially interact with Helix pomatia. Retention of these discriminating features is critical to the study of endothelial cell heterogeneity. It is noteworthy that most commercially available pulmonary microvascular endothelial cell lines do not report interaction with Griffonia simplicifolia in cell characterization. However, this feature of cell phenotyping is critical to resolving PMVEC behavior in culture that is reflective of its in vivo behavior. Thus, lectin-binding criteria is a critical component of endothelial cell phenotyping, especially when considering the heterogeneity of cell phenotypes.
Study of PMVECs and PAECs characterized using the aforementioned approaches has revealed that these cells differ with regard to many physiological properties, including their semi-permeable barrier function, mechanotransduction, migration, proliferation, and angiogenic capacity [reviewed in (Stevens 2005; Gebb and Stevens 2004; Ochoa and Stevens 2012; King et al. 2004; Ochoa et al. 2010)]. Rapid migration, proliferation, and angiogenic capacity is consistent with the presence of progenitor cells. Rapid PMVEC migration was noted in studies designed to evaluate mechanisms by which thrombin induces gap formation (Cioffi et al. 2002). Thrombin stimulated PMVEC gap formation within minutes of its application. However, even large micron-sized gaps were resealed within 2 h. In contrast, gap formation was slow and progressive in PAECs, and gap size was at its greatest 2 h post-thrombin challenge. Time-lapse movies revealed rapid PMVEC movement with extensive lamellipodia as cells resealed the barrier. Subsequent scratch wound assays substantiated these initial observations. From this work, it was surmised that PMVECs rapidly migrate, perhaps to sustain alveolar-capillary integrity especially following injury.
If PMVECs migrate rapidly as a cellular feature designed to protect the alveolar-capillary membrane, then they may also proliferate rapidly to repair the post-natal lung following injury. Consistent with this idea, serum-stimulated growth is greater in PMVECs than it is in PAECs, and accordingly, population doubling time during log phase growth is much shorter in the microvascular cells (King et al. 2004). In contrast to PAECs, PMVEC growth, while slowed, is not abolished in low serum conditions (0.1 %) (Solodushko and Fouty 2007). The microvascular cells do not undergo G0/G1 arrest and progress through S phase. They possess increased cdk4 and cdk2 kinase activity along with hyperphosphorylated and inactive retinoblastoma and increased cyclin D1 protein. Despite maintaining growth in low serum conditions, the establishment of a monolayer—confluence—causes G0/G1 arrest, with concomitant retinoblastoma hypophosphorylation and p27Kip1 upregulation. Thus, PMVECs possess an intrinsic growth advantage, but their growth advantage remains regulated by cell adhesion, e.g., formation of a monolayer.
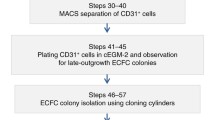
6 Endothelial Microheterogeneity: Progenitor Cells Within a Population
The studies of Solodushko and Fouty (2007) provided mechanistic insight into what controls PMVEC progression through the cell cycle. However, their work focused on the growth characteristics of cell populations and did not seek ways to evaluate the presence, or function, of endothelial cell progenitor cells within the population. As discussed above (see Sect. 11.3), Ingram and colleagues (2004) utilized single cell cloning approaches to establish growth hierarchies within endothelial cell populations, and thereby developed functional assays to identify endothelial progenitors. Alvarez and colleagues (2008) adapted this approach for evaluation of PMVEC and PAEC progenitor growth characteristics.
Using PMVEC and PAEC populations, characterized as described (see Sect. 11.5), Alvarez and colleagues (2008) subjected cells to the clonogenic assay and established a hierarchy of growth potentials among single cells. Whereas the hierarchy of PAEC growth potentials was similar to previous descriptions in HUVECs, with <10 % of cells displaying a high proliferative potential, nearly 50 % of single PMVECs were highly replication competent (Fig. 11.3). Similar results were obtained in endothelial cells isolated from mice (Schniedermann et al. 2010). These data suggest that endothelial cells isolated from lung capillaries possess an intrinsically high proliferative potential with the capacity to self-renew, distinguishing characteristics of progenitor cells.
Pulmonary microvascular endothelial cell populations contain a high percentage of progenitor cells that contribute to their rapid proliferation. (a) PMVEC populations proliferate rapidly when compared to PAEC populations. Cells were seeded at 105 cells in 35 mm dishes, and serum (10 %)-stimulated growth evaluated over 6 days. (b) Single cell clonogenic assay reveals a high percentage of replication competent PMVECs; as many at 50 % of PMVECs display a high proliferative capacity. Adapted from Alvarez et al. (2008)
PMVECs display a restrictive barrier property, limiting trans-endothelial water, solute and protein flux. However, it is generally believed that cell adhesion limits cell proliferation. High proliferative potential cells isolated from PMVECs were tested to determine whether they establish a restrictive barrier (Alvarez et al. 2008). Similar to the parent cell population, high proliferative potential cells generated a restrictive barrier. These cells also retained expression of usual endothelial “marker” proteins, such as VE-cadherin, vWf, PECAM-1, eNOS, and N-cadherin. They retained an ability to interact with Griffonia simplicifolia and did not readily interact with Helix pomatia, similar to the parent cells. High proliferative potential cells expressed proteins characteristic of circulating endothelial progenitor cells, including vascular endothelial cell growth factor receptor-2 and CD105, but they did not express CD133 or CD45. Thus, high proliferative potential cells were selected from a population of lung microvascular endothelial cells, PMVECs, and while these individual cells grew rapidly and fulfilled the criterion of progenitor cells, they maintained their “microvascular” identity.
High proliferative potential endothelial cells were tested to determine whether they displayed evidence of replicative senescence (Alvarez et al. 2008). Short telomeres are associated with replicative senescence. Telomeres were fluorescently labeled, and their length evaluated against control cell populations. PAECs displayed the shortest telomere lengths and high proliferative potential PMVECs possessed the longest telomere lengths, consistent with their rapid proliferative capacity. Growth in soft agar matrix was measured to evaluate possible cell transformation. Whereas breast cancer cells grew into large, anchorage-independent clumps, growth was suppressed in PAECs, PMVECs, and high proliferative potential PMVECs, suggesting high proliferative potential cells displayed regulated cell cycle progression. Consistent with this idea, as high proliferative potential PMVECs grew to confluence in a serum (10 %)-stimulated growth curve, the percentage of S phase cells decreased substantially (e.g., cells came out of the cell cycle), similar to both PAECs and PMVECs. Both PMVECs and high proliferative potential PMVECs were rapidly neo-angiogenic as well, when compared to PAECs. However, selection of high proliferative potential cells did not enrich for a cell population with even greater angiogenic benefit, as both the parent PMVEC population and the high proliferative potential PMVECs generated similar numbers of blood vessels.
Studies seeking to resolve a molecular basis for rapid endothelial growth identified increased expression of nucleosome assembly protein 1 in PMVECs and in high proliferative potential PMVECs (Clark et al. 2008). Nucleosome assembly protein 1 is an epigenetic, pro-proliferative factor that is conserved from yeast to mammals. This protein was detected in a comparative mRNA profiling transcript analysis in PAECs and PMVECs. In the initial screen, nucleosome assembly protein 1 was highly expressed in PMVECs, even at confluence. Nucleosome assembly protein 1 downregulation decreased the proliferative and neo-angiogenic capacity of PMVECs, and its overexpression increased the proliferative and neo-angiogenic capacity of PAECs. In both experimental cases, however, changing nucleosome assembly protein 1 expression did not impact the expression of endothelial cell markers, including PECAM-1, VE-cadherin, and vWf. It also had no effect on lectin-binding criteria; PAECs recognized Helix pomatia even following nucleosome assembly protein 1 overexpression, and PMVECs recognized Griffonia simplicifolia even following nucleosome assembly protein 1 silencing. These findings implicate nucleosome assembly protein 1 as an epigenetic determinant of endothelial growth, but not in either endothelial or “microvascular” versus “macrovascular” phenotype specifications. Studies have not yet been completed to evaluate how nucleosome assembly protein 1 impacts the clonogenic potential, or the hierarchy of growth potentials, among single endothelial cells.
Endothelial cells that display rapid growth characteristics, such as PMVECs, can easily be identified in culture systems by the color of their medium at post-confluence. Mammalian cell culture medium contains phenol red, which is red at normal pH, light red-to-pink with alkalotic pH, and yellow with acidotic pH. The medium of post-confluent PMVECs becomes increasingly yellow, suggesting development of a lactic acidosis. This observation prompted investigation into the means by which PMVECs sustain bioenergetic demands during rapid growth (Parra-Bonilla et al. 2010, 2013). Microarray, RT-PCR, and western blot analysis revealed increased expression of glycolytic enzymes in PMVECs when compared with PAECs. Moreover, as cells grew to confluence in a standard serum-stimulated growth curve, PMVECs consumed glucose from the medium, generated lactate, and produced acidosis. Oxygen consumption was lower in PMVECs than it was in PAECs, and yet total ATP concentrations were higher in the microvascular cells. These data suggest that PMVECs, and likely high proliferative potential PMVECs, rely on glucose fermentation to sustain their rapid proliferation.
To test this idea more directly, glucose was restricted from the PMVEC medium during growth (Fig. 11.4). Glucose restriction produced a dose-dependent decrease in cell growth and attenuated the lactate accumulation and acidosis. Moreover, galactose substitution for glucose abolished the lactic acidosis and greatly reduced cell proliferation, while reducing PMVEC ATP concentrations. Interestingly, supplying extracellular lactate to the galactose-treated PMVECs rescued ATP concentrations. Glucose consumption and the reliance on glycolysis to sustain ATP concentrations and cell proliferation are consistent with the use of aerobic glycolysis to sustain the bioenergetic demands of PMVEC growth.
Pulmonary microvascular endothelial cells utilize aerobic glycolysis to sustain their bioenergetic demands during proliferation. As PMVECs undergo rapid proliferation (a), they consume glucose from the media (b), produce an acidosis (c), and generate lactate (d). These features, including glucose consumption and production of lactic acidosis in the presence of sufficient oxygen, are characteristic of aerobic glycolysis. Adapted from Parra-Bonilla and coworkers (2010)
Lactate dehydrogenase is the enzyme responsible for converting pyruvate to lactate in a reaction that oxidizes NADH to NAD+ and H+. The functional lactate dehydrogenase enzyme is a tetramer comprised of different combinations of “A” (or M, predominates in muscle and liver) and “B” (or H, predominates in heart) proteins (Jungmann et al. 1998; Zhong and Howard 1990). The different combinations of A and B subunits produce five separate enzymes, lactate dehydrogenase 1–5. Lactate dehydrogenase 5 is comprised of four A subunits. Lactate dehydrogenase A activity had been linked to cell proliferation and neoangiogenesis, prompting investigation into the function of this protein in maintaining PMVEC rapid growth (Parra-Bonilla et al. 2010, 2013). Pharmacological inhibition, and genetic disruption, of lactate dehydrogenase A reversibly impaired aerobic glycolysis, decreased proliferation, and decreased neo-angiogenesis. Thus, PMVECs utilize aerobic glycolysis to meet the bioenergetic demands of rapid angiogenesis.
7 Lung Capillaries: A Progenitor Endothelial Cell Niche?
Considerable work in the past decade has validated the anatomical, biochemical, and physiological heterogeneity of lung macrovascular and microvascular endothelium. A specialized transition zone has been identified in small precapillary blood vessels, where the phenotype switches from one characteristic of a “macrovascular” to a “microvascular” cell type (Wu et al. 2014). It is interesting to note that cell–cell junctions between these PAECs and PMVECs is quite distinct (Ofori-Acquah et al. 2008), leading to the hypothesis that this vascular site—where phenotypically different cell types border one another—might contribute to pulmonary vasculopathy (Stevens 2005). Indeed, this transition zone is recognized as the site where complex, lumen-occluding lesions form in pulmonary arterial hypertension. These lesions are at least partly due to the exuberant overgrowth of endothelial cells that lose the “law of the monolayer,” perhaps beginning with the overgrowth of apoptosis-resistant cells (Tuder et al. 2001). Preliminary results suggest that cells in the occlusive lesion interact with Griffonia simplicifolia and overexpress both nucleosome assembly protein 1 and lactate dehydrogenase A (Stevens 2005). It will be important to better resolve whether the apoptosis-resistant, lumen-occluding cells represent endothelial progenitor cells, and whether they have a “macrovascular” or “microvascular” specification.
Evidence supporting the idea that lung capillary endothelial cells represent a progenitor cell niche comes from the study of highly characterized cells in culture. PMVECs grow rapidly in cell population studies. An abundance of individual PMVECs display high proliferative potential, and these cells reconstitute the entire growth hierarchy of growth potentials. These cells express circulating endothelial cell progenitor cell markers CD34 and VEGFR2, but not CD113, and they express a high level of nucleosome assembly protein 1 and glycolytic enzymes, including lactate dehydrogenase A. They require aerobic glycolysis to sustain rapid proliferation and neo-angiogenesis. All of these cellular characteristics support the notion that lung capillaries are enriched with resident progenitor cells.
However, resident endothelial progenitor cells have not been specifically distinguished in the intact capillary. Currently, there is not a universally accepted approach to visualize progenitor cells within the vessel wall and discriminate their location and function among neighboring cells. Clear evidence for endothelial microheterogeneity—a heterogeneity between adjacent cells within any specific vascular segment—has been seen in intact vessels (Majno and Palade 1961; Majno et al. 1961; Aird 2005). Perhaps this concept is best known from dynamic measurements of cytosolic calcium, where endothelial cells display dynamic transitions in cytosolic calcium even at rest. Here, the vessel-averaged endothelial cell cytosolic calcium signals are not synonymous with individual cell cytosolic calcium signals. How these different calcium signals translate into cellular physiology, within the consortium of cells comprising the vessel wall, remains unclear. Decoding complex cytosolic calcium signatures may be useful in identifying endothelial progenitor cells within a vessel wall, to match the signature with an important cellular physiology. Such functional assays may complement ongoing efforts to identify protein matrices that define cellular function (Li et al. 2011; Nolan et al. 2013). While we recognize that no single protein marker is sufficient to define endothelial cell progenitor cells, in time, a protein matrix can aid the search for their location within the vascular wall.
Recognition that endothelial populations possess cells with a hierarchy of growth potentials, including highly replication competent cells that fulfill the definition of progenitor cells, represents a major advance in vascular biology. As the field moves forward, it will be essential to identify the in vivo location of these progenitor cells in the post-natal lung with precision, to understand their role in vascular maintenance and to appreciate how they contribute to vascular repair following injury. Advancing our fundamental knowledge of resident endothelial progenitor cells may reveal their therapeutic potential.
References
Aird WC (2005) Spatial and temporal dynamics of the endothelium. J Thromb Haemost 3(7):1392–1406
Alvarez DF, Huang L, King JA, ElZarrad MK, Yoder MC, Stevens T (2008) Lung microvascular endothelium is enriched with progenitor cells that exhibit vasculogenic capacity. Am J Physiol Lung Cell Mol Physiol 294(3):L419–L430
Asahara T, Murohara T, Sullivan A, Silver M, van der Zee R, Li T, Witzenbichler B, Schatteman G, Isner JM (1997) Isolation of putative progenitor endothelial cells for angiogenesis. Science 275(5302):964–967
Asosingh K, Aldred MA, Vasanji A, Drazba J, Sharp J, Farver C, Comhair SA, Xu W, Licina L, Huang L, Anand-Apte B, Yoder MC, Tuder RM, Erzurum SC (2008) Circulating angiogenic precursors in idiopathic pulmonary arterial hypertension. Am J Pathol 172(3):615–627
Basile DP, Yoder MC (2014) Circulating and tissue resident endothelial progenitor cells. J Cell Physiol 229(1):10–16
Becker AJ, Mc CE, Till JE (1963) Cytological demonstration of the clonal nature of spleen colonies derived from transplanted mouse marrow cells. Nature 197:452–454
Chao H, Hirschi KK (2010) Hemato-vascular origins of endothelial progenitor cells? Microvasc Res 79(3):169–173
Cioffi DL, Moore TM, Schaack J, Creighton JR, Cooper DM, Stevens T (2002) Dominant regulation of interendothelial cell gap formation by calcium-inhibited type 6 adenylyl cyclase. J Cell Biol 157(7):1267–1278
Clark J, Alvarez DF, Alexeyev M, King JA, Huang L, Yoder MC, Stevens T (2008) Regulatory role for nucleosome assembly protein-1 in the proliferative and vasculogenic phenotype of pulmonary endothelium. Am J Physiol Lung Cell Mol Physiol 294(3):L431–L439
Crapo JD, Barry BE, Gehr P, Bachofen M, Weibel ER (1982) Cell number and cell characteristics of the normal human lung. Am Rev Respir Dis 125(6):740–745
Duong HT, Erzurum SC, Asosingh K (2011) Pro-angiogenic hematopoietic progenitor cells and endothelial colony-forming cells in pathological angiogenesis of bronchial and pulmonary circulation. Angiogenesis 14(4):411–422
Fuchs E, Segre JA (2000) Stem cells: a new lease on life. Cell 100(1):143–155
Fuchs A, Weibel ER (1966) Morphometric study of the distribution of a specific cytoplasmatic organoid in the rat's endothelial cells. Z Zellforsch Mikrosk Anat 73:1–9
Gebb S, Stevens T (2004) On lung endothelial cell heterogeneity. Microvasc Res 68(1):1–12
Habliston DL, Whitaker C, Hart MA, Ryan US, Ryan JW (1979) Isolation and culture of endothelial cells from the lungs of small animals. Am Rev Respir Dis 119(6):853–868
Haies DM, Gil J, Weibel ER (1981) Morphometric study of rat lung cells. I. Numerical and dimensional characteristics of parenchymal cell population. Am Rev Respir Dis 123(5):533–541
Hill JM, Zalos G, Halcox JP, Schenke WH, Waclawiw MA, Quyyumi AA, Finkel T (2003) Circulating endothelial progenitor cells, vascular function, and cardiovascular risk. N Engl J Med 348(7):593–600
Hirschi KK, Ingram DA, Yoder MC (2008) Assessing identity, phenotype, and fate of endothelial progenitor cells. Arterioscler Thromb Vasc Biol 28(9):1584–1595
Hristov M, Weber C (2004) Endothelial progenitor cells: characterization, pathophysiology, and possible clinical relevance. J Cell Mol Med 8(4):498–508
Ingram DA, Mead LE, Tanaka H, Meade V, Fenoglio A, Mortell K, Pollok K, Ferkowicz MJ, Gilley D, Yoder MC (2004) Identification of a novel hierarchy of endothelial progenitor cells using human peripheral and umbilical cord blood. Blood 104(9):2752–2760
Ingram DA, Mead LE, Moore DB, Woodard W, Fenoglio A, Yoder MC (2005) Vessel wall-derived endothelial cells rapidly proliferate because they contain a complete hierarchy of endothelial progenitor cells. Blood 105(7):2783–2786
Jungmann RA, Huang D, Tian D (1998) Regulation of LDH-A gene expression by transcriptional and posttranscriptional signal transduction mechanisms. J Exp Zool 282(1–2):188–195
King J, Hamil T, Creighton J, Wu S, Bhat P, McDonald F, Stevens T (2004) Structural and functional characteristics of lung macro- and microvascular endothelial cell phenotypes. Microvasc Res 67(2):139–151
Kissel CK, Lehmann R, Assmus B, Aicher A, Honold J, Fischer-Rasokat U, Heeschen C, Spyridopoulos I, Dimmeler S, Zeiher AM (2007) Selective functional exhaustion of hematopoietic progenitor cells in the bone marrow of patients with postinfarction heart failure. J Am Coll Cardiol 49(24):2341–2349
Li Y, Massey K, Witkiewicz H, Schnitzer JE (2011) Systems analysis of endothelial cell plasma membrane proteome of rat lung microvasculature. Proteome Sci 9(1):15
Lin Y, Weisdorf DJ, Solovey A, Hebbel RP (2000) Origins of circulating endothelial cells and endothelial outgrowth from blood. J Clin Invest 105(1):71–77
Majno G, Palade GE (1961) Studies on inflammation. 1. The effect of histamine and serotonin on vascular permeability: an electron microscopic study. J Biophys Biochem Cytol 11:571–605
Majno G, Palade GE, Schoefl GI (1961) Studies on inflammation. II. The site of action of histamine and serotonin along the vascular tree: a topographic study. J Biophys Biochem Cytol 11:607–626
Medina RJ, O'Neill CL, Sweeney M, Guduric-Fuchs J, Gardiner TA, Simpson DA, Stitt AW (2010) Molecular analysis of endothelial progenitor cell (EPC) subtypes reveals two distinct cell populations with different identities. BMC Med Genomics 3:18
Nachman RL, Jaffe EA (2004) Endothelial cell culture: beginnings of modern vascular biology. J Clin Invest 114(8):1037–1040
Nolan DJ, Ginsberg M, Israely E, Palikuqi B, Poulos MG, James D, Ding BS, Schachterle W, Liu Y, Rosenwaks Z, Butler JM, Xiang J, Rafii A, Shido K, Rabbany SY, Elemento O, Rafii S (2013) Molecular signatures of tissue-specific microvascular endothelial cell heterogeneity in organ maintenance and regeneration. Dev Cell 26(2):204–219
Ochoa CD, Stevens T (2012) Studies on the cell biology of interendothelial cell gaps. Am J Physiol Lung Cell Mol Physiol 302(3):L275–L286
Ochoa CD, Wu S, Stevens T (2010) New developments in lung endothelial heterogeneity: von Willebrand factor, P-selectin, and the Weibel-Palade body. Semin Thromb Hemost 36(3):301–308
Ofori-Acquah SF, King J, Voelkel N, Schaphorst KL, Stevens T (2008) Heterogeneity of barrier function in the lung reflects diversity in endothelial cell junctions. Microvasc Res 75(3):391–402
Parra-Bonilla G, Alvarez DF, Al-Mehdi AB, Alexeyev M, Stevens T (2010) Critical role for lactate dehydrogenase A in aerobic glycolysis that sustains pulmonary microvascular endothelial cell proliferation. Am J Physiol Lung Cell Mol Physiol 299(4):L513–L522
Parra-Bonilla G, Alvarez DF, Alexeyev M, Vasauskas A, Stevens T (2013) Lactate dehydrogenase a expression is necessary to sustain rapid angiogenesis of pulmonary microvascular endothelium. PLoS One 8(9):e75984
Pfannkuch F, Blumcke S (1985) What's new in lung physiology? Pulmonary vessel regulation/non-respiratory metabolic lung functions. Pathol Res Pract 180(6):718–720
Prasain N, Lee MR, Vemula S, Meador JL, Yoshimoto M, Ferkowicz MJ, Fett A, Gupta M, Rapp BM, Saadatzadeh MR, Ginsberg M, Elemento O, Lee Y, Voytik-Harbin SL, Chung HM, Hong KS, Reid E, O'Neill CL, Medina RJ, Stitt AW, Murphy MP, Rafii S, Broxmeyer HE, Yoder MC (2014) Differentiation of human pluripotent stem cells to cells similar to cord-blood endothelial colony-forming cells. Nat Biotechnol 32(11):1151–1157
Reya T, Morrison SJ, Clarke MF, Weissman IL (2001) Stem cells, cancer, and cancer stem cells. Nature 414(6859):105–111
Richardson MR, Yoder MC (2011) Endothelial progenitor cells: quo vadis? J Mol Cell Cardiol 50(2):266–272
Ryan JW, Ryan US (1977) Pulmonary endothelial cells. Fed Proc 36(13):2683–2691
Ryan US, Ryan JW (1984a) The ultrastructural basis of endothelial cell surface functions. Biorheology 21(1–2):155–170
Ryan US, Ryan JW (1984b) Cell biology of pulmonary endothelium. Circulation 70(5 Pt 2):III46–III62
Ryan JW, Ryan US, Schultz DR, Whitaker C, Chung A (1975) Subcellular localization of pulmonary antiotensin-converting enzyme (kininase II). Biochem J 146(2):497–499
Ryan US, Ryan JW, Whitaker C, Chiu A (1976) Localization of angiotensin converting enzyme (kininase II). II. Immunocytochemistry and immunofluorescence. Tissue Cell 8(1):125–145
Ryan US, White LA, Lopez M, Ryan JW (1982) Use of microcarriers to isolate and culture pulmonary microvascular endothelium. Tissue Cell 14(3):597–606
Schniedermann J, Rennecke M, Buttler K, Richter G, Stadtler AM, Norgall S, Badar M, Barleon B, May T, Wilting J, Weich HA (2010) Mouse lung contains endothelial progenitors with high capacity to form blood and lymphatic vessels. BMC Cell Biol 11:50
Solodushko V, Fouty B (2007) Proproliferative phenotype of pulmonary microvascular endothelial cells. Am J Physiol Lung Cell Mol Physiol 292(3):L671–L677
Stevens T (2005) Molecular and cellular determinants of lung endothelial cell heterogeneity. Chest 128(6 Suppl):558S–564S
Takahashi K, Yamanaka S (2006) Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 126(4):663–676
Till JE (1961) Radiation effects on the division cycle of mammalian cells in vitro. Ann N Y Acad Sci 95:911–919
Tuder RM, Cool CD, Yeager M, Taraseviciene-Stewart L, Bull TM, Voelkel NF (2001) The pathobiology of pulmonary hypertension. Endothelium. Clin Chest Med 22(3):405–418
Wagers AJ, Weissman IL (2004) Plasticity of adult stem cells. Cell 116(5):639–648
Weibel ER (1973) Morphological basis of alveolar-capillary gas exchange. Physiol Rev 53(2):419–495
Weibel ER (2012) Fifty years of Weibel-Palade bodies: the discovery and early history of an enigmatic organelle of endothelial cells. J Thromb Haemost 10(6):979–984
Weissman IL (2000) Stem cells: units of development, units of regeneration, and units in evolution. Cell 100(1):157–168
Weissman IL, Anderson DJ, Gage F (2001) Stem and progenitor cells: origins, phenotypes, lineage commitments, and transdifferentiations. Annu Rev Cell Dev Biol 17:387–403
West JB (2013) Marcello Malpighi and the discovery of the pulmonary capillaries and alveoli. Am J Physiol Lung Cell Mol Physiol 304(6):L383–L390
Wu AM, Siminovitch L, Till JE, McCulloch EA (1968a) Evidence for a relationship between mouse hemopoietic stem cells and cells forming colonies in culture. Proc Natl Acad Sci U S A 59(4):1209–1215
Wu AM, Till JE, Siminovitch L, McCulloch EA (1968b) Cytological evidence for a relationship between normal hematopoietic colony-forming cells and cells of the lymphoid system. J Exp Med 127(3):455–464
Wu S, Zhou C, King JA, Stevens T (2014) A unique pulmonary microvascular endothelial cell niche revealed by Weibel-Palade bodies and Griffonia simplicifolia. Pulm Circ 4(1):110–115
Yamanaka S, Takahashi K (2006) Induction of pluripotent stem cells from mouse fibroblast cultures. Tanpakushitsu Kakusan Koso 51(15):2346–2351
Yoder MC (2012) Human endothelial progenitor cells. Cold Spring Harb Perspect Med 2(7):a006692
Yoder MC, Mead LE, Prater D, Krier TR, Mroueh KN, Li F, Krasich R, Temm CJ, Prchal JT, Ingram DA (2007) Redefining endothelial progenitor cells via clonal analysis and hematopoietic stem/progenitor cell principals. Blood 109(5):1801–1809
Yoon CH, Hur J, Park KW, Kim JH, Lee CS, Oh IY, Kim TY, Cho HJ, Kang HJ, Chae IH, Yang HK, Oh BH, Park YB, Kim HS (2005) Synergistic neovascularization by mixed transplantation of early endothelial progenitor cells and late outgrowth endothelial cells: the role of angiogenic cytokines and matrix metalloproteinases. Circulation 112(11):1618–1627
Zhong XH, Howard BD (1990) Phosphotyrosine-containing lactate dehydrogenase is restricted to the nuclei of PC12 pheochromocytoma cells. Mol Cell Biol 10(2):770–776
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Hartman, L., Stevens, T. (2015). Lung Microvascular Endothelium as a Putative Progenitor Cell Niche. In: Firth, A., Yuan, JJ. (eds) Lung Stem Cells in the Epithelium and Vasculature. Stem Cell Biology and Regenerative Medicine. Springer, Cham. https://doi.org/10.1007/978-3-319-16232-4_11
Download citation
DOI: https://doi.org/10.1007/978-3-319-16232-4_11
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-16231-7
Online ISBN: 978-3-319-16232-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)