Abstract
Acute obstruction of a coronary artery is the most common cause of ST-segment elevation myocardial infarction (STEMI). The most common clinical presentation of myocardial infarction is acute chest pain. It is essential that initial assessment and management be rapid but methodical and evidence based focusing on distinguishing between chest pain secondary to acute coronary syndrome and that caused by nonischemic etiologies. Early revascularization is the mainstay of improving outcomes. Primary percutaneous coronary intervention (PCI) supported by appropriate antithrombotic therapy is the preferred approach when rapidly available. Guideline-directed medical therapy, secondary prevention, and lifestyle modification complement successful long-term management. In this chapter, we will discuss the management of acute STEMI, highlighting some important key elements in the pathophysiology of and mechanisms by which STEMI can develop.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Myocardial infarction
- Plaque rupture
- Fibrinolytics
- Primary percutaneous coronary intervention
- STEMI
- Statins
- Thrombin inhibitors
- Nitrates
- Glycoprotein IIb/IIIa inhibitors
1 Introduction
The understanding of the sequence of biological events involved in the pathophysiology and mechanism by which myocardial infarction (MI) occurs has witnessed a significant change over the past decades. The early theory of progressive worsening of severe coronary lesions leading to coronary lumen compromise along with successive vascular spasm and intracoronary thrombosis was heavily supported as the key mechanism by which acute coronary syndromes (ACS) including unstable angina and MI occur. However, extensive angiographic studies following fibrinolysis revealed that the majority of plaques leading to ACS were not sufficiently angiographically severe to fully explain the underlying pathology.
Further detailed vascular biology studies have led to the conclusion that ACS occurs because of acute rupture or disruption of a plaque, known as the thin-capped fibroatheroma, which is different in composition and character from the stable benign plaque (Chap. 19).
In this chapter, we will discuss further the mechanism and pathophysiology by which acute myocardial infarction occurs. We will also highlight the management and pharmacotherapy of treating ST-segment elevation myocardial infarction (STEMI). The management of the remainder of the ACS spectrum (unstable angina and non-ST-segment elevation myocardial infarction) is discussed in Chap. 23.
2 Pathophysiology of Myocardial Infarction
2.1 Myocardial Injury and Myocardial Cell Death
The constantly pumping heart muscle needs a steady supply of oxygen and fuel to contract. Balance between myocardial oxygen supply and demand is the prime determinant of normal cardiac function. Energy demand is determined by the cardiac workload, which primarily depends on wall stress, heart rate, and inotropic state. Supply is provided by regulation of coronary blood flow through epicardial coronary arteries, resistance arteries, precapillary arterioles, and capillaries. If myocardial oxygen demand exceeds its supply, ischemia-induced contractile dysfunction leads to hypotension and further myocardial ischemia. Under normal physiological conditions, the myocardium gets its supply from aerobic metabolism of glucose, lactate, and free fatty acids via the Krebs citrate cycle into the production of adenosine triphosphate (ATP). In acute myocardial infarction, a sudden cessation of blood supply to a region of the myocardium results in decreased oxidative ATP synthesis, eventually leading to stimulation of anaerobic glycolysis and glycogen breakdown, and inhibition of Na+/K+ ATPase resulting in cell swelling. Low cytosolic ATP concentration reduces the contractile ability of the myocardium and, when coupled with increased cytosolic Ca2+ from disrupted transport systems in the sarcolemma and sarcoplasmic reticulum, promotes alteration in contractile proteins.
After a variable duration of ischemia, irreversible myocardial injury ensues. Phospholipase activation promotes accumulation of lysophospholipids and free fatty acids within the cell, and development of free radicals and toxic reactive oxygen species (ROS) occurs via different mechanisms including xanthine oxidase, activated neutrophils, electron leakage from ischemic mitochondria, and catecholamine oxidation, in addition to cyclooxygenase and lipoxygenase enzymes. The end result is breaking of cytoskeletal anchoring proteins and progressive membrane permeability of the sarcolemma, resulting in physical and structural disruption, impairment of contractile function, and cardiomyocyte cell death [1–3].
2.2 Evolution of Myocardial Infarction
The initial ischemic cellular changes in the myocardium begin almost immediately at the onset of ischemia. Severe loss of myocardial contractility occurs within 60 s. Depending on metabolic state and collateral blood flow, total cessation of blood supply can cause irreversible injury and loss of cellular viability within 20–40 min and up to several hours. At autopsy, hearts with acute myocardial infarction show two zones of myocardial damage: a zone with no flow or very low flow, a central zone, surrounded by a marginal zone with supply from collateral vessels. One important determinant of infarct size is the extent of collateral coronary circulation that sustains survival of the marginal zone. The presence of collaterals is therefore critically related to survival and development of future congestive heart failure [4]. Irreversible cell death occurs first in the subendocardial zone of the myocardium and then extends as a wave front toward the subepicardium; by 6–24 h, necrosis becomes transmural [5]. Other factors that influence infarct size are ischemic preconditioning and reperfusion.
2.3 Ischemic Pre- and Postconditioning
Brief repetitive episodes of transient ischemia separated by periods of reperfusion appear to protect the myocardium against subsequent prolonged ischemia; this has been termed ischemic preconditioning. Two phases of preconditioning have been described: the initial phase, known as the classical or early preconditioning operative for up to 3 h before sustained coronary occlusion, and the delayed phase, operative 24 h after the precondition, known as the second window of protection (SWOP) [6].
The exact mechanism by which ischemic preconditioning-mediated cardioprotection occurs is not fully understood; however, the classical or early phase has been associated with the activation of adenosine (A1/A3) receptors, activation of protein kinase C (PKC) coupled to G proteins, opening of ATP-sensitive potassium (KATP) channels, and closure of mitochondrial permeability transition pore (MPTP). The mechanism of how SWOP occurs remains even less clear but is believed to be triggered by a spectrum of chemical stimuli including adenosine receptor agonists, cyclooxygenase-2 (COX-2), bradykinin, opioid-κ receptor agonists, nitric oxide donors, cytokines, ROS, and endotoxin derivatives (e.g., monophosphoryl lipid A); these trigger complex signal transduction pathways via kinase cascades, including mitogen-activated protein kinases, tyrosine protein kinases, and nuclear factor kappa B (NFκB). Furthermore, it has been proposed that some nonchemical triggers of SWOP are ischemia, heat stress, rapid ventricular pacing, and exercise [7, 8].
Data from animal models have suggested that ischemic postconditioning can reduce reperfusion-induced myocardial injury by brief repetitive episodes of reperfusion and reocclusion in the affected coronary artery applied at the beginning of reperfusion therapy. It appears that this strategy has similar benefits as ischemic preconditioning and invokes similar protein kinase pathways in animal models [9]. Particularly, the activation of the reperfusion injury salvage kinase (RISK) pathway including prosurvival kinases, such as PI3K-Akt, eNOS, and p70S6K, appears to play a prominent role in protecting the myocardium [10]. However, a clinical trial in STEMI patients did not show ischemic postconditioning to be effective [11].
2.4 Ischemia Reperfusion Injury
If ischemic myocardium is reperfused early, there is the potential for nearly complete recovery of the ischemic territory. Frequently, however, the myocardium remains dysfunctional despite successful reperfusion. Sometimes ischemic cellular damage even appears exaggerated and accelerated after successful restoration of blood flow. This paradoxical reperfusion injury occurs after sudden reperfusion of severely ischemic myocardium and has been linked to damage from free radicals and calcium. This manifests as reduction in myocardial contractility and systolic function, lowering of the threshold for fatal arrhythmias, conversion of reversible to irreversible myocyte injury, and microvascular dysfunction. Reperfusion thus may have a paradoxical effect on the myocardium, reducing its beneficial actions [12]. Reactive oxygen species (ROS), sudden increases in intracellular Ca2+, rapid restoration of physiologic pH, and inflammation are mediators of this process. The release of ROS leads to reduction in the bioavailability of nitric oxide. Nitric oxide (endothelium-derived relaxing factor), a cardioprotective vasodilatory molecule, inactivates superoxide radicals and improves coronary flow.
The sudden and rapid release of intracellular Ca2+ induces cell death by stimulating myofibril contraction, leading to opening of the MPTP and uncoupled oxidative phosphorylation, rapid ATP depletion, and cell death. Reperfusion injury can be reduced by hypothermia when initiated late during ischemia in animal models, but this has been difficult to demonstrate in clinical trials [13]. Despite improved understanding of the underlying pathways mediating reperfusion injury, there are currently no specific therapies to prevent it.
2.5 Microembolization
Embolization of small fragments of fibrin-platelet thrombus and necrotic core can occur with acute coronary thrombosis. This phenomenon may play a role in some complications of acute myocardial infarction, such as arrhythmias, contractile dysfunction, microinfarcts, and reduced coronary reserve [14]. Other proposed mechanisms of microembolization include primary percutaneous coronary intervention (PCI), PCI of saphenous vein grafts, and coronary thrombolysis.
2.6 Stunned and Hibernating Myocardium
Abnormal regional left ventricular wall motion due to total or subtotal coronary occlusion for a brief period of time (5–15 min) results in a condition termed – myocardial stunning. Typically, in myocardial stunning, despite reestablishment of coronary blood flow, left ventricular dysfunction may persist for hours or days following reperfusion. Another possible cause for episodes of stunned myocardium is a sudden increase in oxygen demand in the setting of a fixed coronary stenosis, for instance, in patients with stable coronary disease.
If the myocardium is exposed to prolonged ischemia, its contractile function is persistently impaired but may partially or completely recover by improvement of blood flow or reduced oxygen demand; the myocardium is termed to be in a state of – myocardial hibernation. The chronicity of underperfusion determines the rate of functional recovery after restoration of normal flow. Acutely hibernating myocardial segments typically recover rapidly while chronically hibernating myocardium has very slow recovery rates after restoration of coronary blood flow, usually weeks to months. Myocardial hibernation can occur in patients with chronic stable angina, unstable angina, or acute myocardial infarction. Revascularization of viable myocardium may improve ventricular dysfunction, inhibit the progression of congestive heart failure, and improve survival [15].
While hibernation describes contractile dysfunction during ischemia, stunning describes abnormal myocardium after ischemia. Moreover, despite these differences, both stunned and hibernating myocardium can be differentiated from irreversibly injured tissue by imaging techniques, such as response to inotropic agents (demonstrated by dobutamine stress echocardiography), improvement of wall motion abnormality after restoration of flow, and shifting metabolism from utilization of free fatty acids to glucose as a source of energy (utilization of radionuclide myocardial perfusion imaging).
2.7 Ventricular Remodeling
During the postinfarction period, healing of transmural infarcts takes weeks and months after the initial event, involving an early inflammatory response, myocardial hypertrophy in the infarct border zone, and eventual scar formation. These mechanisms promote architectural changes of the left ventricle such as ventricular dilatation and a change to a more spherical shape of the ventricle, a process known as ventricular remodeling [16]. The extent of transmural necrosis is perhaps the major determinant of remodeling; islands of viable myocardium in the subepicardial necrotic regions are associated with decreased remodeling. Furthermore, microvascular integrity and baseline ventricular compliance also play a major role in reduction of remodeling. The more viable zones of myocardium there are after successful reperfusion in myocardial infarction, the less the degree of remodeling [17].
2.8 Coronary Anatomy and Location of Infarction
STEMI with transmural necrosis typically occurs distal to an acutely occluded coronary artery, with thrombus superimposed on a ruptured plaque. However, a coronary occlusion that has developed slowly over time may be silent clinically and evident only on electrocardiogram.
Right ventricular infarction. Approximately 50 % of patients with inferior infarction have some involvement of the right ventricle. Transmural infarction involving the inferoposterior wall and posterior portion of the septum is seen. Isolated infarction of the right ventricle (RV) is seen in 3–5 % of autopsies with MI. The right ventricle can sustain long periods of ischemia but demonstrate excellent recovery of contractile function after reperfusion. The RV is thin walled and receives significant blood supply from endocardial perfusion; therefore, ischemia is less likely to induce RV dysfunction.
Atrial infarction. This occurs in up to 10 % of patients with STEMI, usually in conjunction with ventricular infraction, and can result in rupture of the atrial wall. Rarely isolated atrial infarction has been reported in 3.5 % of autopsies of patients with STEMI. The right atrium is more commonly involved than the left, and infarction is more frequent in the atrial appendage than the lateral or posterior atrial walls. Atrial infarction is frequently associated with atrial arrhythmias [18, 19].
2.9 Non-atherosclerotic Causes of Acute Myocardial Infarction
Only a small number of patients with STEMI have normal coronary arteries. In these patients, a lysed embolus, a transiently occlusive platelet aggregate, or a prolonged episode of severe coronary spasm may have been the underlying cause of the infarct. Numerous pathologic processes other than atherosclerosis can lead to sudden occlusion of a coronary artery and result in STEMI (see Table 20.1).
3 Plaque Morphology
Acute myocardial infarction in the majority of cases is believed to result from disruption of the endothelium covering an atherosclerotic plaque – type 1 myocardial infarction; this occurs with plaque rupture or erosion, allowing blood to come in contact with the highly thrombogenic contents of the necrotic core of the plaque, leading to luminal thrombosis. Another mechanism for acute myocardial infarctions is supply-demand mismatch – type 2 myocardial infarction [20].
3.1 Composition of Plaques
Acute myocardial infarction related to atherosclerosis is a dynamic process with multiple stages: intimal thickening, fibrous cap atheroma (fibroatheroma) formation, thin-cap fibroatheroma (vulnerable plaque) formation, and plaque rupture.
Intimal thickening can be observed soon after birth. While some plaques may begin as fatty streaks, intimal thickening may be the precursor to symptomatic atherosclerotic disease since these lesions occur in children at similar locations as advanced plaques occur in adults. Histologically, intimal thickening consists mainly of smooth muscle cells and proteoglycan-collagen matrix with little or no infiltrating inflammatory cells [21].
Fibrous cap atheroma is characterized by a lipid-rich necrotic core encapsulated by fibrous tissue and is considered the earliest stage of advanced coronary disease. Early progression of the fibrous cap atheroma involves necrosis with macrophage infiltration of the lipid pool. Later, localized areas of cellular debris, increased free cholesterol, and near-complete depletion of extracellular matrix are seen. Eventually, a lesion develops with significant luminal narrowing after episodes of hemorrhage with or without calcium deposition and surface disruption [22].
Thin-cap fibroatheroma (vulnerable plaque) has a large necrotic core comprising approximately 25 % of plaque area, separated from the lumen by a thin fibrous cap, less than 65 μm in thickness. The fibrous cap is heavily infiltrated by macrophages and T lymphocytes and typically is devoid of smooth muscle cells, enabling it to be more vulnerable to rupture.
3.2 Plaque Rupture
Although the precise mechanism of plaque rupture is poorly understood, the disruption is believed to occur at the site of the fibrous cap which is heavily infiltrated by macrophages and T lymphocytes where the underlying necrotic core is typically large. Fibrillar collagens, especially type I collagen, provide most of the tensile strength to the fibrous cap. Collagen synthesis is inhibited by interferon gamma secreted by activated T-cells with the expression of CD40 ligands (CD40L/CD154), which bind to CD40 receptors on the macrophages, B lymphocytes, and other cells including endothelial and smooth muscle cells. This promotes tissue proteolysis through the release of matrix metalloproteinases (MMPs) leading to fibrous cap thinning. Plaque rupture sites typically are deficient in smooth muscle cells, which play an essential role in maintaining the fibrous cap. In vitro studies have shown that smooth muscle apoptosis is promoted and mediated by secretion of interferon gamma, Fas ligand, tumor necrosis factor-α (TNF-α), interleukin-1 (IL-1), and reactive oxygen species by macrophages and T lymphocytes, as well as oxidized LDL. This may be responsible for the decrease in smooth muscle cells in thin-cap fibroatheroma and ruptured plaques [23].
Blood flow-induced shear stress may also influence processes that lead to plaque rupture, where increased peak circumferential stress is greater in thinner fibrous caps. Regions with high shear stress typically exhibit high strain; these combined mechanical stressors, when applied to the weakened fibrous cap, may precipitate rupture, particularly in the presence of microcalcification [24].
3.3 Plaque Erosion
Plaque erosion represents the second most common lesion in acute coronary thrombosis. Erosions differ from rupture lesions, as there is absence of fibrous cap disruption. The characteristics of plaque erosion, unlike plaque rupture, include an abundance of smooth muscle cells and proteoglycan matrix and absence of surface endothelium, without a prominent lipid core. There is no communication between the necrotic core and the lumen. Either no or few macrophages and T lymphocytes are close to the lumen. The luminal surface of erosion is separated from flowing blood by a platelet-rich thrombus adherent to the proteoglycan-rich intima. The absence of endothelium, secondary to apoptotic loss of endothelial cells, allows flowing blood to come in contact with collagen and induces thrombus formation [25].
4 Management of ST-Segment Elevation Myocardial Infarction
Prompt recognition is the first step in management of patients with ST-segment elevation myocardial infarction (STEMI) and is a complex, multidisciplinary, and staged process. Typical ST-segment elevations on ECG in a patient with angina-type chest pain most commonly reflect the acute occlusion of an epicardial coronary artery. Cardiomyocytes quickly die if exposed to hypoxia and do not regenerate. Therefore, the most important goal in the care of a patient with STEMI is to reopen promptly the affected coronary artery. Currently, the most reliable method is PCI. This section deals with prehospital care, management in the emergency department, hospital management, and complications.
4.1 Prehospital and Initial Management
Once STEMI is suspected, a key element is early initiation of care prior to presenting to the hospital, which raises the likelihood of survival. Most STEMI deaths occur within the first hour of onset, with ventricular fibrillation as the most common cause of mortality. Thus, an approach that enables definitive resuscitative efforts and transport to a hospital is pivotal. Major components of the delay from the onset of symptoms to reperfusion include (1) the time for the patient to recognize the seriousness of the problem and seek medical attention; (2) the time for prehospital evaluation, treatment, and transportation; (3) the time for diagnostic measures and initiation of treatment in the hospital (e.g., door-to-needle time for patients receiving a fibrinolytic agent and door-to-balloon time for patients undergoing a catheter-based reperfusion strategy); and (4) the time from initiation of treatment to restoration of coronary blood flow [26].
Because the vast majority of STEMIs occur outside the hospital, it is essential to implement systems to minimize delay in presenting to a health-care facility equipped to manage STEMI. Some patient-related factors associated with longer time to present to a hospital or seek medical attention include older age, female gender, ethnic and racial minorities, low socioeconomic and literacy status, history of diabetes, and consulting a family relative or a physician [27, 28]. Health-care professionals and especially primary care providers must emphasize and reinforce with patients and families the necessity of urgent medical care for symptoms of an acute coronary syndrome including chest discomfort, extreme fatigue, and dyspnea, especially if accompanied by diaphoresis, lightheadedness, palpitations, or a sense of impending doom. Counseling on timely activation of emergency services for ischemic-type chest pain is key for prompt access to a health-care facility for proper diagnosis and initiation of management.
Communities should maintain regional systems for management of STEMI that embrace assessment and continuous quality improvement of Emergency Medical Services Systems (EMS) to expand the capability to perform a 12-lead electrocardiogram (ECG), transmit it, and activate the STEMI care team prior to hospital arrival [29]. Improvement of door-to-intervention time and improvement of STEMI outcomes rely on improvement of EMS dispatch and response.
In rural settings or communities without quick and timely access to a PCI-capable medical facility, an alternative approach is prehospital fibrinolysis, demonstrated in multiple randomized controlled trials as safe and effective in reducing ischemia time in STEMI patients. Although none of the individual trials showed a significant reduction in mortality with prehospital fibrinolytic therapy, a meta-analysis of the highest quality trials showed a 17 % reduction in mortality. The greatest reduction in mortality was seen with reperfusion initiated within 60–90 min after the onset of symptoms [30]. This approach requires experienced and well-trained personnel, utilization of computer-assisted ECG with capability of rapid transmission to a central station, and equipping ambulances with the appropriate medicine kits and supplies. These resources are frequently lacking in rural areas, and therefore prehospital fibrinolysis is not available in many US communities.
4.2 Management in the Emergency Department
4.2.1 Triage and Evaluation
Accurate diagnosis and exclusion of alternate diagnoses are crucial for successful STEMI management in the emergency room. All patients presenting with symptoms suggestive of an acute MI should be rapidly triaged and a 12-lead ECG performed and shown to an experienced physician within 10 min of arrival. A targeted history and focused physical examination should be quickly performed. Five baseline parameters account for >90 % of the prognostic predictors of 30-day mortality from acute MI: age, systolic blood pressure on presentation, the Killip classification (Table 20.2), heart rate, and location of MI [31].
4.2.2 Initial Management
In definitive STEMI, time in the emergency department should be minimal, and the patient should be taken directly to the catheterization laboratory while supportive measures are undertaken.
4.2.2.1 Oxygen
Supplemental oxygen by a nasal cannula is indicated only for hypoxic patients with suspected MI. Oxygen should be administered only if there is evidence of hypoxemia (oxygen saturation <90 %), as the potential harm from hyperoxia can worsen outcomes [32]. Supplemental oxygen should be used with caution in patients with chronic obstructive pulmonary disease and carbon dioxide retention [30].
4.2.2.2 Aspirin
Unless there is a clear history of aspirin allergy (not intolerance), the immediate use of aspirin in doses of at least 162–325 mg significantly reduces mortality. To achieve therapeutic levels in the blood faster, aspirin is usually chewed to promote buccal absorption.
4.2.2.3 Reduction of Cardiac Pain
4.2.2.3.1 Nitrates
Nitrates enhance coronary flow by coronary vasodilation and reduce ventricular preload by systemic venodilation. The venodilation diminishes venous return to the heart, reducing ventricular volume and pressure, and thus a reduction in ventricular preload occurs. The use of nitrates is not associated with reduction in mortality.
Nitrates are initially administered sublingually (0.4 mg nitroglycerin sublingual tablet) followed by close observation for improvement in symptoms or change in hemodynamics. If an initial dose is well tolerated and appears of benefit, further nitrates should be administered, with monitoring of vital signs. Marked hypotension (systolic blood pressure <90 mmHg), bradycardia, and suspected right ventricular infarction are contraindications to nitroglycerin [33].
If chest pain persists or recurs, intravenous nitroglycerin may help to control ischemic pain; this requires close monitoring of blood pressure. Intravenous nitroglycerin should be initiated at 5–10 μg/min and gradually increased with a goal of 10–30 % reduction of systolic blood pressure and/or relief of chest pain. Long-acting nitrate preparations should not be used. Moreover, nitrates should not be given within 24 h of use of phosphodiesterase (PDE) inhibitors (e.g., sildenafil) because the combination may result in severe systemic vasodilation and life-threatening hypotension.
Another important aspect in the use of nitrates is nitrate tolerance. Although this is most commonly observed with chronic nitrate therapy for chronic angina, it remains a characteristic of nitrate therapy in general. The mechanism by which nitrate tolerance occurs is not fully understood. One proposed mechanism is thought to be by reduction of nitric oxide availability via inhibiting conversion of nitroglycerin to 1,2-glyceryl dinitrate by directly impairing the function of mitochondrial aldehyde dehydrogenase-2 (mtALDH) enzyme [34]. Another theory postulates that nitrate tolerance is secondary to the reduced bioactivity of nitric oxide, supported by findings in animal models that exhibited tolerance to nitrates despite high levels of nitric oxide [35].
4.2.2.3.2 Analgesia
Morphine is the drug of choice to treat pain not relieved by maximally tolerated anti-ischemic therapy associated with STEMI. An initial dose of 2–4 mg as an intravenous bolus is given with increments of 2–4 mg repeated at 5–10 min intervals. Morphine may cause hypotension and respiratory depression; these side effects preclude further use of the drug.
Morphine acts by decreasing anxiety and restlessness triggered by activation of the autonomic nervous system, suppression of which results in reduction of myocardial oxygen demand. In patients with pulmonary edema, morphine has additional benefits of peripheral arterial and venous dilatation, reduced work of breathing, and slowing of heart rate due to increased vagal tone. Nausea and vomiting may be troublesome side effects of large doses of morphine and can be treated with a phenothiazine. In high doses, morphine overdose may be problematic, and classic signs of opioid intoxication may develop including depressed mental status, decreased respiratory rate, decreased bowel sounds, and pinpoint miotic constricted pupils.
The use of nonsteroidal anti-inflammatory drugs (NSAIDs) has been associated with increased risk of adverse cardiovascular events in patients with STEMI and should be avoided throughout the hospitalization for STEMI [36, 37].
4.2.2.4 Anticoagulation
Thrombin (Factor IIa) is the central mediator of clot formation as it induces platelet activation, conversion of fibrinogen to fibrin, and activation of factor XIII, leading to fibrin cross-linking and clot stabilization. Research over the past three decades has resulted in the development of various antithrombotic agents and combination strategies with the intention to promote culprit artery patency, prevent thrombotic reocclusion after pharmacologic or mechanical reperfusion, and reduce bleeding complications. Several strategies are available and accepted in practice guidelines. Local hospital systems are encouraged to generate their most feasible treatment algorithm that complies with the latest practice guidelines.
Anticoagulant agents used in the management of STEMI can be divided into two major groups:
-
1.
Antithrombin (anti-factor IIa) agents:
-
(a)
Indirect thrombin inhibitors, e.g., unfractionated heparin and low-molecular-weight heparin
-
(b)
Direct thrombin inhibitors, e.g., bivalirudin
-
(a)
-
2.
Anti-factor Xa agents:
-
For example, fondaparinux
-
Table 20.3 outlines different clinical characteristics of anticoagulants used in management of STEMI (also see Chap. 23).
4.2.2.4.1 Unfractionated Heparin (UFH)
Heparin use is a class I indication for STEMI patients who will undergo primary PCI or fibrinolytic therapy [30]. Unfractionated heparin binds to antithrombin III and inhibits the activation of thrombin and therefore lacks the ability to inhibit thrombin that is clot bound. It has a molecular weight range of 12,000–30,000 Da. The usual dose is an intravenous initial bolus of 60 U/kg (4,000 U maximum) followed by a 12 U/kg/h (1,000 U/h maximum) infusion, given promptly, with a goal-activated partial thromboplastin time (aPTT) of 1.5–2.0 times normal. A disadvantage of unfractionated heparin is its unpredictable anticoagulation effects, due to variability in protein binding and the time delay until therapeutic levels are achieved. Unfractionated heparin use in myocardial infarction has an abundance of data and usually is part of the standard treatment arm in trials comparing newer agents or combinations of antithrombotic regimens. It currently can be used in all three-treatment strategies: to support PCI, fibrinolytics [38], or medical management. In patients receiving fibrinolytic therapy and aspirin, the addition of UFH is of proven benefit in patients treated with fibrin-specific thrombolytics, which are now preferred [39]. UFH may also be of benefit for patients receiving streptokinase who are at high risk for systemic thromboembolism. Thus, all patients with STEMI should be treated with anticoagulant therapy regardless of choice of fibrinolytic agent.
4.2.2.4.2 Low-Molecular-Weight Heparin (LMWH)
LMWHs are glycosaminoglycans with chains of residues of D-glucosamine and uronic acid in an alternate fashion. Compared to UFH, these agents have a molecular weight that ranges from 4,000 to 6,000 Da. The usual dose is an intravenous bolus of 30 mg of enoxaparin, followed by 1 mg/kg subcutaneous injection every 12 h. Unlike unfractionated heparin, LMWHs are stronger inhibitors of factor Xa than thrombin; therefore, the anticoagulation effect cannot be measured routinely. The advantages of LMWHs are a longer half-life, better bioavailability, and dose-independent clearance, resulting in more rapid predictable anticoagulation compared to unfractionated heparin. However, LMWH is associated with increased risk of major and minor bleeding in the clinical trials [40–43]. Due to this fact and given the lack of superiority to unfractionated heparin, many experts do not use LMWH in patients undergoing primary PCI and choose unfractionated heparin or bivalirudin. In current practice guidelines, LMWH with doses adjusted to age, weight, and renal function can be used as an adjunct preferentially in those patients undergoing therapy with fibrinolysis [30].
Neither unfractionated heparin nor LMWH crosses the placenta and thus does not result in fetal anticoagulation. In general, the use of LMWH is preferred over UFH due to the efficacy and ease of administration. However, UFH appears to be a more appropriate alternative to LMWH when more control of anticoagulation is needed (e.g., near the time of delivery) or patients with severe renal insufficiency [44, 45]. Current practice guidelines do not specify use of one form of heparin over the other, mostly due to lack of data from clinical trials that target this patient population.
4.2.2.4.3 Direct Thrombin Inhibitors
These agents bind directly to thrombin and can be used safely in patients with previous heparin-induced thrombocytopenia. Both Hirulog and bivalirudin were compared to heparin in STEMI. In patients undergoing reperfusion by fibrinolysis, direct thrombin inhibitors significantly reduced recurrence of MI but did not reduce mortality and had significantly higher rates of major bleeding [43]. When used in patients undergoing reperfusion by PCI, bivalirudin had significantly lower major bleeding and was associated with a significant reduction of 30-day and 1-year mortality; however, it was associated with increased stent thrombosis compared to heparin and glycoprotein IIb/IIIa receptor blockers [46].
4.2.2.4.4 Factor Xa Inhibitors
Administration of fondaparinux, a factor Xa inhibitor, was evaluated in STEMI clinical trials compared to placebo, unfractionated heparin, or enoxaparin. The use of fondaparinux is reasonable in patients with STEMI undergoing reperfusion with PCI, although concomitant unfractionated heparin is recommended to prevent occurrence of guide catheter clots and stent thrombosis [47, 48].
4.2.2.5 Antiplatelet Agents (Also See Chap. 23)
In the acute management of STEMI, these agents inhibit platelet aggregation, the release of granule contents, and platelet-mediated vasoconstriction.
4.2.2.5.1 Aspirin
Aspirin, a powerful cyclooxygenase enzyme inhibitor, controls the first step in the biosynthesis of the arachidonic acid derivatives, prostaglandins, and thromboxanes, namely, thromboxane A2 that stimulates platelet aggregation. The use of aspirin in STEMI has been associated with significant reduction in mortality in multiple clinical trials [49, 50]. Dose of aspirin and route of administration in acute STEMI management were outlined above. The use of aspirin is a class I recommendation for management of STEMI patients undergoing reperfusion with either PCI or fibrinolytic therapy. Aspirin remains highly beneficial even in patients not undergoing reperfusion [30].
4.2.2.5.2 P2Y12 Receptor Blockers
These agents block platelet adenosine diphosphate receptor P2Y12 with a more potent antiplatelet effect than aspirin but less than glycoprotein IIb/IIIa inhibitors. Thienopyridines ticlopidine (rarely used nowadays), clopidogrel, prasugrel, and the cyclopentyltriazolopyrimidine ticagrelor are available only in oral formulation; cangrelor is an intravenous agent but is not approved for use in STEMI (Table 20.4). Newer P2Y12 receptor blockers (prasugrel and ticagrelor) have more potent antiplatelet effect than clopidogrel; prasugrel should not be given to elderly patients above the age of 75 years, patients with low weight under 60 Kg, and patients with a history of prior stroke or transient ischemic attack. Ticagrelor is formulated as a twice a day medication, with medication adherence being a potential concern, and because of its potency, concomitant dose of aspirin should be limited to less than 100 mg daily. The use of P2Y12 receptor blockers in patients with STEMI has shown most benefit when used as an additive to aspirin. Unless contraindicated, these agents should be started immediately and continued for at least 1 year.
4.2.2.5.3 Glycoprotein IIb/IIIa Inhibitors
These drugs are potent agents that inhibit the final common pathway for platelet aggregation and clot formation. Currently, only three agents are available in the United States: abciximab, tirofiban, and eptifibatide. In reperfusion using fibrinolysis, multiple studies demonstrated that glycoprotein IIb/IIIa inhibitors with half-dose fibrinolysis improved coronary artery blood flow in STEMI patients. No significant mortality benefit was seen, and the risk of major and minor bleeding was higher [51–53]. Therefore, according to current practice guidelines, the use of these agents upstream prior to arrival to the catheterization laboratory or concomitant use with fibrinolytic agents is not recommended. There is evidence supporting administration of glycoprotein IIb/IIIa agents at the time of PCI as they improve coronary artery flow to the infarct area and ultimately improves mortality outcomes. Thus, the guidelines recommendations were for limited use in the catheterization laboratory at the time of primary PCI only. Abciximab has historically been the glycoprotein IIb/IIIa inhibitor widely used during PCI, because it was the most studied in clinical trials. There is growing evidence that eptifibatide and tirofiban may be acceptable alternatives to abciximab in STEMI patients [54] (Chap. 23).
4.2.3 Reperfusion
In most patients with STEMI, early reperfusion improves myocardial salvage and significantly reduces mortality. Timing is of paramount importance for myocardial salvage, as the benefits of reperfusion decline as time elapses. Reperfusion strategies encompass three options: fibrinolytic therapy, catheter-based reperfusion, and coronary artery bypass surgery.
4.2.3.1 Optimal Reperfusion Strategy Selection
Assessment of optimal reperfusion options for STEMI can be challenging integrating multiple complex decisions, making it difficult to formulate a simple equation or a one-size-fits-all approach. An integrated assessment of the time since onset of symptoms, risk of death after STEMI, risk of bleeding related to fibrinolysis, and time required for transportation to a PCI-capable facility needs to be taken into account. PCI is preferred when there is greater risk related to the clinical presentation of the STEMI, such as development of cardiogenic shock or risk of bleeding if fibrinolysis is given. If PCI is done in a timely fashion with short door-to-balloon time, this approach should be adopted. Fibrinolysis is the preferred reperfusion strategy where there is no skilled PCI facility accessible, limited by long transportation time, or lack of an experienced operator and team. Notably, when fibrinolysis is performed early, particularly in the prehospital setting, and followed by coronary angiography and PCI when appropriate, the 1-year survival rate is comparable to that achieved with primary PCI [55].
4.2.3.2 Catheter-Based Reperfusion Strategies
Reperfusion of the myocardium affected by the infarct artery is based on passage of a balloon catheter over a guide wire. This approach now includes coronary angiography augmented with administration of potent antiplatelet agents, deployment of coronary stents, and aspiration thrombectomy as needed [19, 56].
PCI for patients with STEMI involves one of three options.
4.2.3.2.1 Primary PCI
This refers to the use of PCI for reperfusion in lieu of fibrinolysis therapy, and is the preferred strategy of reperfusion in STEMI patients, when executed by a skilled interventional cardiologist in a timely manner. It requires presentation of the patient to a high-volume, well-equipped center with experienced support staff. Timely performed primary PCI results in higher rates of infarct artery patency and restoration of TIMI 3 flow with significantly lower incidence of recurrent ischemia, reinfarction, emergency repeat revascularization procedures, intracranial hemorrhage, and death. Successful primary PCI lowers the incidence of long-term complications of STEMI that result from longer ischemic times or unsuccessful fibrinolytic therapy, leading to shorter hospital stays and earlier resumption of daily activities [57].
Current clinical practice guidelines recommend primary PCI for patients with STEMI with symptoms of ischemia of less than 12-h duration and those who have contraindications to fibrinolytic therapy. For patients who develop acute severe heart failure or cardiogenic shock related to STEMI, primary PCI should be performed irrespective of time of delay from MI onset. PCI of a non-infarct artery should not be performed at the time of PCI in hemodynamically stable patients, as it is associated with worse clinical outcomes. However, a recent meta-analysis from three randomized controlled trials in patients with STEMI suggests that immediate complete revascularization improves outcomes compared to culprit vessel-only revascularization, which would indicate a paradigm shift in clinical practice [58].
Placement of coronary stents at the time of primary PCI is recommended, as implantation of stents has been associated with less restenosis and need for reintervention, but does not reduce death or reinfarction. Dual antiplatelet therapy is needed for at least 1 year after placement of drug-eluting stents; newer-generation drug-eluting stents may require dual antiplatelet therapy for lesser time, as low as 6 months, to lower the risks of bleeding associated with the use of these agents. If financial or social barriers may limit patient compliance, higher bleeding risk or anticipated need for surgical or invasive procedures in the upcoming year is identified; bare metal stent implantation should be performed, as the period required for dual antiplatelet therapy is significantly less [30].
4.2.3.2.2 Fibrinolytic-Facilitated PCI
This refers to treatment of patients with STEMI with fibrinolysis as a bridge to intended immediate PCI. However, this option carries higher risk of major bleeding including intracranial hemorrhage. Current clinical practice guidelines state that fibrinolytic-facilitated PCI is a reasonable approach if primary PCI cannot be performed or is not readily available immediately, with transfer to PCI-capable facility as soon as logistically feasible and ideally within 24 h but not performing PCI within 2–3 h after administration of fibrinolytic therapy.
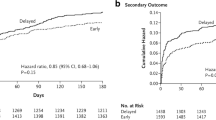
4.2.3.2.3 Delayed (Rescue) PCI
This refers to performance of PCI in STEMI patients with reperfusion failure of the infarct artery or infarct artery reocclusion after initial fibrinolysis therapy. It also refers to PCI performed in patients treated with an initial noninvasive strategy who develop cardiogenic shock, acute severe HF, or unstable postinfarction angina, if invasive management is not considered futile or inappropriate.
Rescue PCI is recommended on the basis of outcomes of several clinical trials that demonstrated that PCI performed on patients who failed to achieve adequate reperfusion and/or continuing ischemia after initial fibrinolysis had less incidence of reinfarction; however, there was no improvement in survival rates among those patients. Some studies report higher rates of bleeding and stroke in patients undergoing rescue PCI [30, 59, 60].
Current clinical practice guidelines strongly recommend a delayed PCI approach for hemodynamically unstable patients or those with intermediate- or high-risk findings on predischarge noninvasive ischemia testing [30]. Delayed PCI is reasonable in stable patients ideally within 24 h but not within 2–3 h after administration of fibrinolytic therapy; it should not be performed for a totally occluded artery for more than 24 h if patients are hemodynamically and electrically stable and asymptomatic.
4.2.3.3 Fibrinolytic Therapy
The objective of fibrinolysis is recanalizing the thrombotic occlusion, resulting in restoration of coronary flow; this is designed to reduce the infarct size and improve cardiac function and overall short- and long-term survival. The major advantage of this strategy is that it is widely available, easily administered, and relatively inexpensive. However, the use of these agents can have serious and sometimes detrimental complications, causing worsening mortality and associated significant morbidity. Only approximately half of patients presenting with STEMI are eligible for fibrinolytic therapy (Table 20.5), and only half of those treated with fibrinolytic agents will achieve complete reperfusion with TIMI grade 3 flow.
Administration of fibrinolytics in STEMI reduces mortality if given early, with the most favorable outcomes if given less than 2 h after symptom onset [61] (Table 20.6). TIMI 3 flow is assessed by improvement in or relief of chest pain, resolution of ST elevation, and the presence of reperfusion arrhythmias (e.g., accelerated idioventricular rhythm). These variables have been used for assessment of effectiveness of fibrinolysis but are not accurate. Lack of resolution of ST elevation is associated with a worse prognosis and should prompt consideration of proceeding to angiography and rescue PCI.
The major complications of fibrinolysis relate to bleeding. Most bleeding is not serious, but intracranial hemorrhage is the most serious complication [62]. Streptokinase (no longer marketed in the United States) had antibody-mediated resistance due to its antigenicity; therefore, patients should not receive streptokinase for STEMI if they have been treated with streptokinase products within the year.
4.2.3.4 Coronary Artery Bypass Surgery (CABG)
Despite exponential improvement of intraoperative myocardial preservation, CABG has a limited role in the acute management of STEMI. However, CABG remains indicated for cardiogenic shock, failed PCI, high-risk anatomy, and surgical repair of a mechanical complication of STEMI such as ventricular septal rupture, free-wall rupture, or severe mitral regurgitation from papillary muscle dysfunction.
4.3 Hospital Management
Following the initial management of STEMI including reperfusion, patients are usually admitted to the coronary care unit (CCU) for continuous ECG monitoring for potentially fatal arrhythmias that may develop after STEMI. Additional pharmacological and non-pharmacological interventions in management of STEMI are crucial.
4.3.1 Inhibition of the Renin-Angiotensin-Aldosterone System
An angiotensin-converting enzyme (ACE) inhibitor should be administered within the first 24 h to all patients with anterior STEMI, congestive heart failure, or an ejection fraction less than or equal to 40 %, unless contraindicated. Lisinopril, enalapril, ramipril, benazepril, and captopril are examples of most commonly used ACE inhibitors. If there is intolerance to ACE inhibitors, an angiotensin II-AT1 receptor blocker (ARB) should be given, e.g., losartan, valsartan, and candesartan. An aldosterone antagonist should be given to all patients with STEMI and no contraindications who are already receiving an ACE inhibitor and beta-blocker and who have an ejection fraction less than or equal to 40 % and either symptomatic heart failure or diabetes mellitus [30] (Chap. 36).
4.3.2 Beta-Blockers
Early use of beta-blockers in STEMI has been documented to reduce early and late mortality in multiple clinical trials. Perhaps reduction of reinfarction rates and cardiac arrest is the main cause [63] (Chap. 5).
According to current guidelines, oral beta-blocker therapy (e.g., metoprolol, carvedilol, bisoprolol) should be initiated in the first 24 h for patients who do not have evidence of (1) heart failure, (2) low cardiac output state, (3) increased risk of cardiogenic shock, or (4) other relative contraindications to beta-blockade (heart block, active asthma, or reactive airway disease). Intravenous beta-blockers could be given if the patient is hypertensive and does not have any of the aforementioned conditions.
Beta-blockers should be continued during and after hospitalization for all patients with STEMI who have no contraindications to their use. If there were initial contraindications to beta-blockers in the first 24 h after STEMI, this should be reevaluated to determine their subsequent eligibility. The long-term duration of routine beta-blocker therapy after uncomplicated MI in patients without HF or hypertension has not been prospectively studied. The current practice guidelines recommend a 3-year treatment course, unless left ventricular ejection fraction is impaired or ongoing angina occurs [30].
4.3.3 Nitrates
Nitrates may be helpful in managing angina-type chest pain in patients with coronary disease in vascular beds other than the infarct-related artery. Patients with vasospastic angina may particularly benefit from nitrates. Other than for symptom management, nitrates do not affect long-term outcomes of coronary patients, and there is no role for the routine use of oral nitrates in the convalescent phase of STEMI [30].
4.3.4 Calcium Channel Blockers
There is no beneficial effect on infarct size or the rate of reinfarction with the use of calcium channel blockers during either the acute or the convalescent phase of STEMI. Calcium channel blockers can be used to relieve ischemia, lower blood pressure, or control the ventricular response rate to atrial fibrillation in patients who are intolerant of beta-blockers; the most commonly used agents are amlodipine and nifedipine. Control of ventricular response rate to atrial fibrillation can be achieved with verapamil or diltiazem (Chap. 37). Caution is advised for those who have underlying left ventricular dysfunction [30].
4.3.5 Statins
High-intensity statin therapy should be initiated or continued in all patients with STEMI and no contraindications to its use. It is reasonable to obtain a fasting lipid profile in patients with STEMI, preferably within 24 h of presentation. Statin therapy after STEMI appears to be beneficial even in patients with baseline low-density lipoprotein levels <70 mg/dL [30]. Atorvastatin, rosuvastatin, and simvastatin are among the most commonly used (Chap. 28).
4.3.6 Counseling, Education, and Cardiac Rehabilitation
Prior to discharge from the hospital, all patients treated for STEMI have to be educated about physical activity; lifestyle modifications including dietary counseling, smoking cessation, influenza vaccination, weight management, and control of blood pressure; modification of lipid profile; treatment of depression; and sexual counseling. Some evidence has shown that behavior changes in addition to early postdischarge follow-up after recovery from STEMI are linked to improved outcomes.
Referral to a cardiac rehabilitation program with supervised physical exercise and an educational component has been recommended for most STEMI patients after discharge. The objectives of these programs are to increase functional capacity, reduce and improve anginal symptoms, reduce disability, improve quality of life, modify coronary risk factors, and reduce morbidity and mortality rates. Even in the setting of contemporary reperfusion and cardioprotective drug therapies, exercise-based cardiac rehabilitation programs improve clinical patient outcomes; current practice guidelines list referral to a cardiac rehabilitation program as a class I recommendation [30, 64, 65].
4.4 Complications of STEMI
See Table 20.7 for summary of complications following STEMI.
5 Concluding Remarks
Acute myocardial infarction occurs because of disruption of a vulnerable atherosclerotic plaque. The location of the plaque, the degree of inflammation within the plaque, and the integrity of the fibrous cap on the plaque are factors that determine the risk of plaque rupture, hence development of myocardial infarction. When intracoronary thrombus forms, it may obstruct the coronary lumen entirely, leading to STEMI or sudden cardiac death; lesser severe obstruction may result in no symptoms, unstable angina, or NSTEMI.
It is essential that initial assessment and management be rapid but methodical and evidence based. Early revascularization is the mainstay of improving outcomes. PCI supported by appropriate antithrombotic therapy is the preferred approach when rapidly available. Guideline-directed medical therapy, secondary prevention, and lifestyle modification complement successful long-term management.
References
Toyokuni S. Reactive oxygen species-induced molecular damage and its application in pathology. Pathol Int. 1999;49(2):91–102.
Verma S. Fundamentals of reperfusion injury for the clinical cardiologist. Circulation. 2002;105(20):2332–6.
Buja LM. Myocardial ischemia and reperfusion injury. Cardiovasc Pathol. 2005;14(4):170–5.
Fujita M, Nakae I, Kihara Y, Hasegawa K, Nohara R, Ueda K, et al. Determinants of collateral development in patients with acute myocardial infarction. Clin Cardiol. 1999;22(9):595–9.
Reimer K, Lowe JE, Rasmussen MM, Jennings RB. The wave front phenomenon of ischemic cell death. 1. Myocardial infarct size vs. duration of coronary occlusion in dogs. Circulation. 1977;56(5):786–94.
Murry CE, Jennings RB, Reimer K. Preconditioning with ischemia: a delay of lethal cell injury in ischemic myocardium. Circulation. 1986;74(5):1124–36.
Yellon DM, Downey JM. Preconditioning the myocardium: from cellular physiology to clinical cardiology. Physiol Rev. 2003;83:1113–51.
Bolli R. The late phase of preconditioning. Circ Res. 2000;87(11):972–83.
Zhao Z, Corvera JS, Halkos ME, Kerendi F, Wang N, Guyton RA, et al. Inhibition of myocardial injury by ischemic postconditioning during reperfusion: comparison with ischemic preconditioning. Am J Physiol Heart Circ Physiol. 2003;579–88.
Tsang A, Hausenloy DJ, Mocanu MM, Yellon DM. Postconditioning: a form of “modified reperfusion” protects the myocardium by activating the phosphatidylinositol 3-kinase-Akt pathway. Circ Res. 2004;95(3):230–2.
Hahn J-Y, Song YB, Kim EK, Yu CW, Bae J-W, Chung W-Y, et al. Ischemic postconditioning during primary percutaneous coronary intervention: the effects of postconditioning on myocardial reperfusion in patients with ST-segment elevation myocardial infarction (POST) randomized trial. Circulation. 2013;128(17):1889–96.
Yellon DM, Hausenloy DJ. Myocardial reperfusion injury. N Engl J Med. 2007;357(11):1121–35.
Hale SL, Dae MW, Kloner R. Hypothermia during reperfusion limits “no-reflow” injury in a rabbit model of acute myocardial infarction. Cardiovasc Res. 2003;59(3):715–22.
Heusch G, Schulz R, Haude M, Erbel R. Coronary microembolization. J Mol Cell Cardiol. 2004;37(1):23–31.
Marban E. Myocardial stunning and hibernation. The physiology behind the colloquialisms. Circulation. 1991;83(2):681–8.
Burchfield JS, Xie M, Hill J. Pathological ventricular remodeling: mechanisms: part 1 of 2. Circulation. 2013;128(4):388–400.
Eaton LW, Weiss JL, Bulkley B. Regional cardiac dilatation after acute myocardial infarction: recognition by two-dimensional echocardiography. N Engl J Med. 1979;300:57–62.
Alonso-Orcajo N, Izquierdo-García F, Simarro E. Atrial rupture and sudden death following atrial infarction. Int J Cardiol. 1994;46(1):82–4.
Bonow RO, Mann DL, Zipes DP, Libby PM. Braunwald’s heart disease – a textbook of cardiovascular medicine. 9th ed. Philadelphia: Saunders Elsevier; 2011.
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, et al. Third universal definition of myocardial infarction. J Am Coll Cardiol. 2012;60(16):1581–98.
McGill HC, McMahan C, Zieske aW, Sloop GD, Walcott JV, Troxclair D, et al. Associations of coronary heart disease risk factors with the intermediate lesion of atherosclerosis in youth. Arterioscler Thromb Vasc Biol. 2000;20(8):1998–2004.
Kolodgie FD, Virmani R, Burke aP, Farb A, Weber DK, Kutys R, et al. Pathologic assessment of the vulnerable human coronary plaque. Heart. 2004;90(12):1385–91.
Geng Y-J, Henderson LE, Levesque EB, Muszynski M, Libby P. Fas is expressed in human atherosclerotic intima and promotes apoptosis of cytokine-primed human vascular smooth muscle cells. Arterioscler Thromb Vasc Biol. 1997;17(10):2200–8.
Vengrenyuk Y, Carlier S, Xanthos S, Cardoso L, Ganatos P. A hypothesis for vulnerable plaque rupture due to stress-induced debonding around cellular microcalcifications in thin fibrous caps source. Proc Natl Acad Sci USA. 2014(i).
Kolodgie FD. Differential accumulation of proteoglycans and hyaluronan in culprit lesions: insights into plaque erosion. Arterioscler Thromb Vasc Biol. 2002;22(10):1642–8.
Antman EM, Anbe DT, Armstrong PW, et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines Committee. Circulation. 2004;110:e82.
Mensah G, Hand MM, Antman EM, Ryan TJ, Schriever R, Smith SC. Development of systems of care for ST-elevation myocardial infarction patients: the patient and public perspective. Circulation. 2007;116(2):e33–8.
Ting HH, Bradley EH, Wang Y, Nallamothu BK, Gersh BJ, Roger VL, et al. Delay in presentation and reperfusion therapy in ST-elevation myocardial infarction. Am J Med. 2008;121(4):316–23.
Rokos IC, French WJ, Koenig WJ, Stratton SJ, Nighswonger B, Strunk B, et al. Integration of pre-hospital electrocardiograms and ST-elevation myocardial infarction receiving center (SRC) networks: impact on Door-to-Balloon times across 10 independent regions. JACC Cardiovasc Interv. 2009;2(4):339–46. American College of Cardiology Foundation.
O’Gara PT, Kushner FG, Ascheim DD, Casey DE, Chung MK, de Lemos J, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013;61(4):e78–140.
Lee KL, Woodlief LH, Topol EJ, Weaver WD, Betriu A, Col J, et al. Predictors of 30-day mortality in the era of reperfusion for acute myocardial infarction. Circulation. 1995;91:1659–68.
Moradkhan R, Sinoway LI. Revisiting the role of oxygen therapy in cardiac patients. J Am Coll Cardiol. 2010;56(13):1013–6. Elsevier Inc.
Hamon M, Agostini D, Le Page O, Riddell JW, Hamon M. Prognostic impact of right ventricular involvement in patients with acute myocardial infarction: meta-analysis. Crit Care Med. 2008;36(7):2023–33.
Chen Z, Zhang J, Stamler JS. Identification of the enzymatic mechanism of nitroglycerin bioactivation. Proc Natl Acad Sci. 2002;99(12):8306–11.
Laursen JB, Mülsch A, Boesgaard S, Mordvintcev P, Trautner S, Gruhn N, Nielsen-Kudsk JE, Busse RAJ, Aldershvile J. In vivo nitrate tolerance is not associated with reduced bioconversion of nitroglycerin to nitric oxide. Circulation. 1996;94(9):2241–7.
Mcgettigan P, Henry D. Clinician’s corner cardiovascular risk and inhibition of cyclooxygenase. JAMA. 2014;296(13), 1633–44.
Gislason GH, Jacobsen S, Rasmussen JN, Rasmussen S, Buch P, Friberg J, et al. Risk of death or reinfarction associated with the use of selective cyclooxygenase-2 inhibitors and nonselective nonsteroidal antiinflammatory drugs after acute myocardial infarction. Circulation. 2006;113(25):2906–13.
Mahaffey KW, Granger CB, Collins R, Ohman EM, Bleich SD, Col JJ, Califf RM. Overview of randomized trials of intravenous heparin in patients with acute myocardial infarction with thrombolytic therapy. Am J Cardiol. 1996;77:551–6.
Topol EJ, TG Investigators, et al. An international randomized trial comparing four thrombolytic strategies for acute myocardial infarction. N Engl J Med. 1993;329(10):673–82.
Antman EM. Enoxaparin as adjunctive antithrombin therapy for ST-elevation myocardial infarction: results of the ENTIRE-Thrombolysis in Myocardial Infarction (TIMI) 23 trial. Circulation. 2002;105(14):1642–9.
Ross aM, Molhoek P, Lundergan C, Knudtson M, Draoui Y, Regalado L, et al. Randomized comparison of enoxaparin, a low-molecular-weight heparin, with unfractionated heparin adjunctive to recombinant tissue plasminogen activator thrombolysis and aspirin: second trial of Heparin and Aspirin Reperfusion Therapy (HART II). Circulation. 2001;104(6):648–52.
Antman EM, Morrow D, McCabe CH, Murphy S, Ruda M, Sadowski Z. Enoxaparin versus unfractionated heparin with fibrinolysis for ST-elevation myocardial infarction. N Engl J Med. 2006;354(14):1477–88.
Yusuf S, Mehta SR, Chrolavicius S, et al. Direct thrombin inhibitors in acute coronary syndromes: principal results of a meta-analysis based on individual patients’ data. Lancet. 2002;359(9303):294–302.
Ginsberg JS, Kowalchuk G, Hirsh J, Brill-Edwards PBR. Heparin therapy during pregnancy risks to the fetus and mother. Arch Intern Med. 1989;149(10):2233.
Greer I, Nelson-Piercy C. Low-molecular-weight heparins for thromboprophylaxis and treatment of venous thromboembolism in pregnancy: a systematic review of safety and efficacy. Blood. 2005;106(2):401–7.
Guagliumi G, Peruga JZ, Brodie BR, Dudek D, Kornowski R, Hartmann F, et al. Bivalirudin during primary PCI in acute myocardial infarction. N Engl J Med. 2008;358:2218–30.
Yusuf S, Mehta SR, Chrolavicius S, et al. Effects of fondaparinux on mortality and reinfarction in patients with acute. JAMA. 2006;295(13):1519–30.
Mehta SR, Granger CB, Eikelboom JW, Bassand J-P, Wallentin L, Faxon DP, et al. Efficacy and safety of fondaparinux versus enoxaparin in patients with acute coronary syndromes undergoing percutaneous coronary intervention: results from the OASIS-5 trial. J Am Coll Cardiol. 2007;50(18):1742–51.
ISIS-2: Second International Study of Infarct Survival. Randomised trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. Lancet. 1988;2:349–60.
Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ. 2002;324(7329):71–86.
Van de Werf FJ, Armstrong PW, Granger CWL. Efficacy and safety of tenecteplase in combination with enoxaparin, abciximab, or unfractionated heparin: the ASSENT-3 randomised trial in acute myocardial infarction. Lancet. 2001;358(9282):605–13.
Topol EJ. Reperfusion therapy for acute myocardial infarction with fibrinolytic therapy or combination reduced fibrinolytic therapy and platelet glycoprotein IIb/IIIa inhibition: the GUSTO V randomised trial. Lancet. 2001;357(6):1905–14.
Giugliano RP, Roe MT, Woodlief LH, Harrington R, Hannan KL, Califf RM, et al. Combination reperfusion therapy with eptifibatide and reduced-dose tenecteplase for ST-elevation myocardial infarction. J Am Coll Cardiol. 2003;41(8):1251–60.
De Luca G, Ucci G, Cassetti E, Marino P. Benefits from small molecule administration as compared with abciximab among patients with ST-segment elevation myocardial infarction treated with primary angioplasty: a meta-analysis. J Am Coll Cardiol. 2009;53(18):1668–73. American College of Cardiology Foundation.
Danchin N, Coste P, Ferrières J, Steg P-G, Cottin Y, Blanchard D, et al. Comparison of thrombolysis followed by broad use of percutaneous coronary intervention with primary percutaneous coronary intervention for ST-segment-elevation acute myocardial infarction: data from the French registry on acute ST-elevation myocardial inf. Circulation. 2008;118(3):268–76.
Valentin F, Walsh RA, Harrington RA. Hurst’s the heart. 13th ed. New York: McGraw-Hill; 2011.
Keeley EC, Boura J, Grines CL. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361(9351):13–20.
Sekercioglu N, Spencer F, Cruz Lopes L, Guyatt GH. Culprit vessel only vs immediate complete revascularization in patients with acute ST-segment elevation myocardial infarction: systematic review and meta-analysis. Clin Cardiol. 2014;18:14–6.
Hughes S, Abrams KR, Ph D, Stevens SE, Sc M, Uren NG, et al. Rescue angioplasty after failed thrombolytic therapy for acute myocardial infarction. N Engl J Med. 2005;353:2758–68.
Wijeysundera HC, Vijayaraghavan R, Nallamothu BK, Foody JM, Krumholz HM, Phillips CO, et al. Rescue angioplasty or repeat fibrinolysis after failed fibrinolytic therapy for ST-segment myocardial infarction: a meta-analysis of randomized trials. J Am Coll Cardiol. 2007;49(4):422–30.
Boersma E, Maas aC, Deckers JW, Simoons ML. Early thrombolytic treatment in acute myocardial infarction: reappraisal of the golden hour. Lancet. 1996;348(9030):771–5.
Hochman JS, Tamis JE, Thompson TD, Weaver WD, White HD, Van de Werf F, Aylward P, Topol EJ, Califf R. Sex, clinical presentation, and outcome in patients with acute coronary syndromes. Global use of strategies to open occluded coronary arteries in acute coronary syndromes IIb investigators. N Engl J Med. 1999;341(4):226–32.
Lau J, Antman E. Cumulative meta-analysis of therapeutic trials for myocardial infarction. N Engl J Med. 1992;327:248–54.
Suaya J, Stason WB, Ades P, Normand S-LT, Shepard DS. Cardiac rehabilitation and survival in older coronary patients. J Am Coll Cardiol. 2009;54(1):25–33. American College of Cardiology Foundation. 951–59.
Taylor RS, Brown A, Ebrahim S, Jolliffe J, Noorani H, Rees K, et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med. 2004;116(10):682–92.
Cheitlin MD, et al. Myocardial infarction without atherosclerosis. JAMA. 1975;231:951.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Abdou, M.H., Engberding, N., Wenger, N.K. (2015). Pathophysiology and Management of Myocardial Infarction. In: Jagadeesh, G., Balakumar, P., Maung-U, K. (eds) Pathophysiology and Pharmacotherapy of Cardiovascular Disease. Adis, Cham. https://doi.org/10.1007/978-3-319-15961-4_20
Download citation
DOI: https://doi.org/10.1007/978-3-319-15961-4_20
Publisher Name: Adis, Cham
Print ISBN: 978-3-319-15960-7
Online ISBN: 978-3-319-15961-4
eBook Packages: MedicineMedicine (R0)