Abstract
Oxidative stress and inflammation are hallmarks of virtually all (chronic) liver diseases. Not surprisingly, understanding the role of oxidative stress and its deleterious consequences has been and still is an important research topic in hepatology. A thorough understanding of oxidative stress and its impact on liver homeostasis is essential to identify novel targets for the treatment of liver diseases. In this chapter, we will review the current knowledge on the role of oxidative stress in hepatocellular injury. Hepatocytes have received a large share of the attention in research on oxidative stress. That will also be the case in this chapter. Nevertheless, we will also address the role of other liver cell types, such as endothelial cells, hepatic stellate cells, and Kupffer cells in oxidative stress-mediated liver injury.
*Author contributed equally with all other contributors.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Key words
- Liver
- Oxidative stress
- Cell death
- Signal transduction
- Reactive oxygen species
- Cytokines
- Apoptosis
- Necrosis
- Mitochondria
- Hepatocytes
- Stellate cells
- Kupffer cells
- Endothelial cells
1 Oxidative Stress and Hepatocellular Injury
Oxidative stress and inflammation are hallmarks of virtually all (chronic) liver diseases. Not surprisingly, understanding the role of oxidative stress and its deleterious consequences has been and still is an important research topic in hepatology. A thorough understanding of oxidative stress and its impact on liver homeostasis is essential to identify novel targets for the treatment of liver diseases. In this chapter, we will review the current knowledge on the role of oxidative stress in hepatocellular injury. Hepatocytes have received a large share of the attention in research on oxidative stress. That will also be the case in this chapter. Nevertheless, we will also address the role of other liver cell types, such as endothelial cells, hepatic stellate cells, and Kupffer cells in oxidative stress-mediated liver injury.
2 Oxidative Stress and Antioxidant Defenses
Oxidative stress is defined as the inappropriate exposure to reactive oxygen species (ROS). It results from the imbalance between pro-oxidants and antioxidants and leads to cell damage. ROS represent a variety of species, including superoxide anions (O2 •−), hydrogen peroxide (H2O2), and hydroxyl radicals (HO•) [1]. The stability and (biological) half-life of these species are variable: the hydroxyl radical is highly reactive, whereas superoxide anions and hydrogen peroxide are more stable. Hydroxyl radicals can be generated through the Haber–Weiss reaction, in which superoxide anions react with hydrogen peroxide, or through the Fenton reaction, in which hydrogen peroxide reacts with iron.
Excessive oxidation of cellular substrates by ROS can lead to cellular injury. Therefore, cells are equipped with various antioxidant defenses, which can significantly delay or prevent the oxidation of substrates [1].
One of these antioxidant defenses are the superoxide dismutases (SODs), a family of enzymes specialized in eliminating superoxide anions. Three distinct SODs have been identified in mammals: Copper-zinc SOD in the cytosol and nucleus (SOD1 or CuZnSOD), manganese SOD in the mitochondria (SOD2 or MnSOD), and extracellular SOD (SOD3 or EC-SOD) [2]. Although they are structurally unrelated and encoded by different genes, they all have the same function, namely converting the superoxide radical to hydrogen peroxide [3]. In general, the generated hydrogen peroxide is less reactive and/or further converted into water and oxygen.
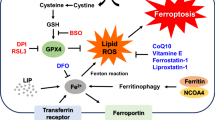
Several enzymes are able to convert hydrogen peroxide into water and oxygen. Catalase, localized in the peroxisomes, can enzymatically decompose hydrogen peroxide. Glutathione peroxidases (GPx) are a family of enzymes, which catalyze the reaction of glutathione (GSH) and H2O2 into water and oxidized glutathione (GSSG). Glutathione is highly present in virtually all cells. It is localized in the cytosol as well as in intracellular organelles such as the endoplasmic reticulum, the nucleus, and the mitochondria. Glutathione is exclusively synthesized in the cytosol in a two-step process by the rate-limiting enzyme γ-glutamylcysteine synthetase (γ-GCS or GCL: glutamate-cysteine ligase) followed by γ-glutamyl transpeptidase (γ-GT) [4]. Oxidized glutathione can be reduced again to GSH by the enzyme GSH reductase (GR), a reaction requiring NADPH. This possibility to recycle GSH makes it a crucial antioxidant defense mechanism for cells.
Several redox-sensitive transcription factors are involved in antioxidant responses such as activator protein-1 (AP-1), nuclear factor-κB (NF-κB), and Nrf2.
AP-1 is a heterodimeric transcription factor that binds to the TPA response element (TRE), which is present in the promoter region of many genes, including antioxidant genes, like heme oxygenase-1, genes involved in cell proliferation, but also genes involved in fibrogenesis, e.g., TGF-β and collagen type 1. Many mitogens and pro-inflammatory signals lead to increased AP-1 nuclear binding and corresponding gene transactivation. It is known that lipid peroxidation products (such as 4HNE) and ROS can induce AP-1 and subsequent transcriptional regulation of target genes, including the ones mentioned above.
NF-κB is also a redox-sensitive transcription factor, consisting of homo- or heterodimers of structurally related subunits. NF-κB activity is mostly regulated at the translational level. Under normal conditions, it is present in the cytosol of cells in an inactive form, due to its binding to the inhibitory subunits IκB. The activation of NF-κB consists of the phosphorylation of the inhibitory subunits, followed by its subsequent degradation [5]. Upon dissociation of IκB from NF-κB, NF-κB can translocate to the nucleus where it can bind to promoter regions of genes which have the κB element. These are genes involved in, e.g., inflammation, cell survival (including antioxidant enzymes), and adhesion. Most, if not all, inducers of NF-κB rely on the production of ROS and their reactions with cellular macromolecules.
Nuclear erythroid-related factor 2 (Nrf-2) is a redox-sensitive transcription factor. In response to an oxidative event, Nrf2 dissociates from KEAP (kelch-like ECH-associated protein 1) and translocates to the nucleus. Here it can bind to its response element ARE (antioxidant response element) to transactivate antioxidant genes. Several antioxidant enzymes like glutamate–cysteine ligase (GCL) and heme oxygenase-1 (HO-1) are under the control of AREs via the phosphorylation of the transcription factor Nrf2 [6, 7].
3 Oxidative Stress in Liver Diseases
Oxidative stress plays an important role in many types of liver diseases including non-alcoholic fatty liver disease (NAFLD), cholestatic liver diseases, alcohol-induced liver injury, and viral hepatitis.
3.1 Non-alcoholic Fatty Liver Disease
Liver injury in NAFLD is characterized by fat accumulation (steatosis), the infiltration of inflammatory cells, and a varying extent of ballooning degeneration of the hepatocytes [8]. NAFLD is the general name for fatty liver disease with steatosis but without severe and overt inflammation, whereas non-alcoholic steatohepatitis (NASH) is the subsequent stage of this disease, characterized by overt inflammation [9]. It is widely accepted that NASH has a two-hit pathogenesis (although some recent reports also imply a “multiple hit” model) [10]. Steatosis is the “first hit”: during this stage, free fatty acids (FFAs) accumulate in the cells. FFA accumulation is caused by an increase in fatty acid uptake either from dietary sources or from lipolysis in adipose tissue. The “second hit,” leading to NASH, involves oxidative stress, decreased hepatic ATP production, and induction of pro-inflammatory cytokines. Progression of steatosis to NASH is an undesired process because it leads to hepatocellular injury. There are various hypotheses regarding the progression of steatosis to NASH. It has been proposed that the lipotoxicity of FFAs increases the vulnerability of the liver to a “second hit,” and that this vulnerability is dependent on environmental and/or genetic factors [10].
Another hypothesis is that the impaired β-oxidation leads to hepatic steatosis and accumulation of lipid intermediates and subsequent impairment of insulin signaling and insulin-resistance, a phenomenon often observed in patients with NASH. In addition, the sustained inflammation and increased levels of TNF may also lead to impaired insulin-signaling via aberrant and sustained phosphorylation of insulin receptor substrate-1 (IRS-1) [11].
As mentioned before, oxidative stress plays a crucial role in the pathogenesis of NASH. Sources for ROS in NASH are mitochondria and peroxisomes, as the β-oxidation occurs in these organelles. Increased β-oxidation in these organelles might be a compensatory mechanism for the excessive FFA accumulation in the hepatocytes and leads to excessive ROS production and oxidative stress [12].
3.2 Cholestasis
Cholestasis is the reduction of bile flow which results in elevated serum levels of potentially toxic bile acids. There are several causes of cholestasis in humans. The most common causes are primary biliary cirrhosis and sclerosing cholangitis. In addition to these disorders, cholestasis can result from biliary atresia, familial cholestatic syndromes resulting from defects in bile acid transporters, exposure to certain drugs, pregnancy, graft-versus-host disease, infection, and Alagille syndrome [13–15].
Several animal models as well as human studies suggest a role for oxidative stress in cholestatic liver diseases. In the bile duct ligation (BDL) model, an animal model for cholestatic liver disease, products of lipid peroxidation were present in hepatic mitochondrial membranes [16]. In addition, increased serum and/or tissue levels of 4-hydroxynonenal (4HNE) and malondialdehyde (MDA), both stable end products of lipid peroxidation, were observed after BDL [17]. However, although this was associated with the influx of inflammatory cells, it was not associated with liver damage. Accordingly, several studies proposed that oxidative stress is a consequence of cholestatic liver disease rather than a cause for injury in these diseases [18].
3.3 Xenobiotic-Induced Liver Diseases (Alcohol, Paracetamol)
Xenobiotics are generally metabolized by hepatocytes, in particular by members of the enzyme family cytochrome P450 (CYP family). Several cytochrome P450 enzymes are important in metabolizing common xenobiotics. A well-known harmful xenobiotic is ethanol. Alcohol-induced liver disease is one of the most common causes of liver disease. Ethanol is metabolized by CYP2E1, producing ROS through reduction of oxygen to superoxide anions, which are dismutated to hydroxyl radicals, a highly oxidative substance. Consequently, lipid peroxidation occurs that leads to the depletion of cellular antioxidants (especially glutathione). This disturbance of the redox equilibrium leads to oxidative stress.
Another xenobiotic is paracetamol (or acetaminophen, APAP), widely used as an analgesic and antipyretic drug. Upon an APAP overdose, the metabolizing capacity of glucuronidating enzymes is exceeded and the drug is metabolized by CYP2E1 or CYP3A4 into N-acetylbenzoquinoneimine (NAPQI), an extremely toxic and oxidizing component. Normally, NAPQI is neutralized by glutathione; however, at high concentrations, the glutathione store is depleted and the excess NAPQI binds to cellular proteins eventually resulting in mitochondrial dysfunction and cell death [19, 20]. Interestingly, acetaminophen toxicity can be attenuated by the addition of glutathione precursors like N-acetylcysteine.
4 Signaling Pathways in Hepatocellular Injury: Involvement of Different Organelles
4.1 Plasma Membrane
In general, the plasma membranes of mammalian cells are exposed to an oxidizing environment, while the cytosol is a reducing environment. If the defense systems are inadequate, oxidative damage will occur to proteins, lipids, and carbohydrates. This damage can be directly, by inhibition of transmembrane transporters and other membrane proteins, or indirectly mediated by lipid peroxidation products.
Lipid peroxidation is the main damaging effect of oxidative stress. Lipids in the cell or organelle membranes are mainly polyunsaturated fatty acids and cholesterol. Upon lipid peroxidation, these lipids are oxidized, which results in the formation of aldehydic by-products such as 4-hydroxy-2-nonenal (4HNE) and malondialdehyde (MDA). This leads to increased cell membrane permeability, decreased cell membrane fluidity, inactivation of membrane proteins, and loss of polarity of mitochondrial membranes. Moreover, 4HNE and MDA have long half-lives, which make them detrimental as they can diffuse over long distances, thereby amplifying the effect of oxidative stress.
As a consequence, oxidative stress can adversely affect the function of cellular organelles such as mitochondria, endoplasmic reticulum, and lysosomes.
4.2 Mitochondria
Mitochondrial function is based on membrane potential, which depends on membrane integrity. Mitochondrial DNA (mtDNA) is extremely sensitive to oxidative damage due to its location (close to the ROS producing mitochondrial inner membrane), the absence of protective histones, and incomplete DNA repair mechanisms in mitochondria. Accumulation of mtDNA damage results in mitochondrial dysfunction, leading to increased ROS production.
Oxidative stress leads to activation of JNK (c-Jun N-terminal kinase, a member of the MAP-kinase family) and translocation of phosphorylated (P)-JNK to the mitochondria, which leads to increased mitochondrial ROS production. This process is a critical step in hepatocellular injury, because it can trigger the mitochondrial membrane permeability transition (MPT) and the collapse of membrane potential, mitochondrial swelling, and rupture of the outer mitochondrial membrane [21].
4.3 Endoplasmic Reticulum
The membrane of the endoplasmic reticulum can also be damaged by lipid peroxidation. Disruption of the ER membrane leads to calcium disequilibrium, which is considered to be one of the initial and pivotal events of ER stress-mediated cell death. ROS and lipid peroxidation directly disable the sarco-endoplasmic reticulum Ca2+-ATPase (SERCA). The impairment of SERCAs can further lead to Ca2+ release from the ER lumen, the accumulation of unfolded proteins in the ER lumen, and ultimately, the disruption of ER homeostasis, i.e., ER stress [22–24]. ER stress causes the activation of the Unfolded Protein Response (UPR). The UPR describes a series of compensatory responses and signaling between organelles to mediate cellular adaptations in order to promote cell survival. However, when ER stress is excessive or chronic, or when the UPR is compromised, pro-apoptotic pathways are activated. A key event in this pro-apoptotic pathway is the induction of CHOP (C/EBP homologous protein) expression [25]. Induced expression of CHOP leads to ROS formation by enhancing the translation of mRNA to stimulate the UPR. Furthermore, ER stress and accompanying CHOP induction is also associated with Ca2+ leakage and subsequent cell death in hepatitis C virus-infected cells [26]. All of these events may lead to hepatocellular injury and cell death.
For the proteins to fold into the correct tertiary and quaternary structures, disulphide bonds have to be created. This requires a highly oxidizing environment that is maintained by a low GSH/GSSG ratio. Oxidative protein folding is a source of ROS, predominantly hydrogen peroxide. Normally, the antioxidant defense can cope with this exposure to elevated ROS. However, under conditions of increased protein folding, this system can be exhausted. In addition, protein misfolding can also give rise to ROS [27].
Exogenous oxidants can also activate the UPR. For example, 7-ketocholesterol, an oxidant product of cholesterol, induces the complete UPR, whereas others only mildly or partly stimulate the UPR [28].
During ER stress, mitochondria display increased ROS production: calcium leaking from the ER is taken up by the mitochondria, which results in the opening of the permeability transition pore and subsequent cytochrome c release. This abrogates the normal electron transport chain, and as a result, leads to increased ROS generation. The increased calcium concentrations in the mitochondria stimulate Krebs cycle dehydrogenases, further boosting ROS production. The increased ROS production leads to opening of the calcium channels in the ER, resulting in a vicious circle.
4.4 Lysosomes
Lysosomes are involved in necrotic, apoptotic, and autophagic cell death. The key factor in determining the type of cell death is the magnitude of the lysosomal membrane permeabilization (LMP) and the amount of proteolytic enzymes released into the cytosol [29]. Massive breakdown of lysosomes results in unregulated necrosis, whereas selective permeabilization of lysosomes triggers apoptosis. Several mechanisms for the controlled permeabilization of lysosomes have been proposed. One hypothesis includes the accumulation of lysosomotropic detergents such as sphingosine in the lysosomes, facilitating the release of lysosomal enzymes into the cytoplasm [30]. Another hypothesis involves ROS-mediated lysosomal destabilization. In this hypothesis, LMP is suggested to precede mitochondrial dysfunction, thereby creating a feedback loop between mitochondrial-derived ROS and LMP to control cell death. In addition, intralysosomal accumulation of free iron indirectly mediates lysosomal membrane damage via generation of ROS [31, 32].
5 Injury to Different Hepatic Cell Type Populations
Liver injury is associated with various responses from different cell types in liver. In response to toxic stimuli, hepatocytes usually become damaged or die, whereas endothelial cells (EC), Kupffer cells (KC), and hepatic stellate cells (HSC) become activated.
5.1 Hepatocytes
Hepatocyte injury can result in hepatocyte cell death via apoptosis, necrosis, necroptosis, or autophagy [33, 34]. In a damaged liver all these forms of cell death will be present; however, one may be predominant over the others. They also share some of the same executive pathways and therefore hybrid modes of cell death occur, displaying characteristics of different modes of cell death. For example, cell death may start as apoptosis, but can switch to necroptosis. In the following paragraphs the different forms of cell death are briefly described.
Apoptosis is an ATP-dependent process, also known as programmed cell death. Apoptosis is characterized by DNA condensation, nuclear fragmentation, plasma membrane blebbing, cell shrinkage, and the formation of apoptotic bodies. Two distinct pathways of apoptosis have been described: the organelle-mediated pathway (or intrinsic pathway) and the receptor-mediated pathway (or extrinsic pathway). Both pathways overlap downstream with the activation of effector caspases (caspase-3, -6 and -7), which results in cleavage of intracellular substrates such as lamin A, poly (ADP-ribose) polymerase (PARP), and Inhibitor of Caspase-Activated DNase (ICAD) to induce apoptotic cell death. Apoptotic features include cell shrinkage, nuclear fragmentation, apoptotic DNA fragmentation, and ultimately, cell death [35].
Necrosis is a passive process that is characterized by metabolic disruption, energy depletion (loss of ATP), mitochondrial swelling, and rupture of the plasma membrane. Subsequently, the release of cellular content into the extracellular environment and systemic circulation triggers an inflammatory response.
Necrosis was long thought to be an uncontrolled form of cell death; however, recently it was appreciated that there is an “in between” variant between apoptosis and necrosis, called necroptosis. Morphologically, necroptotic cell death resembles necrosis as it is characterized by cell swelling, mitochondrial dysfunction, plasma membrane permeabilization, and release of cytoplasmic content into the extracellular space. However, it is regulated via stimulation of death receptors in a similar manner as in apoptosis. Necroptosis seems to serve as a back-up mechanism for apoptosis in cells, which have become resistant to apoptosis such as virus-infected cells. It has been demonstrated that these cells are highly sensitive to necroptosis [36]. This form of cell death is also associated with high mitochondrial ROS production and, unlike apoptosis, it does not involve DNA fragmentation [37].
Autophagy represents a homeostatic cellular mechanism for the turnover of organelles and proteins through a lysosome-dependent degradation pathway. During starvation, autophagy facilitates cell survival through the recycling of metabolic precursors. Additionally, autophagy can modulate other vital processes such as programmed cell death (e.g., apoptosis), inflammation, and adaptive immune mechanisms and thereby influence the pathogenesis of diseases. Selective pathways can target distinct cargoes (e.g., mitochondria or proteins) for autophagic degradation. At present, the causal relationship between autophagy and various forms of cell death remains unclear, as it has been reported that autophagy can act both as an agonist and as an antagonist of cell death. It has also been described that autophagy is a cell death effector pathway under conditions of impaired apoptosis [38].
Autophagy can occur in association with necroptosis triggered by caspase inhibition. Autophagy and apoptosis have been shown to be coincident or antagonistic, depending on the experimental context, and share cross talk between signal transduction pathways. Autophagy may modulate the outcome of other regulated forms of cell death such as necroptosis [39].
Different ROS can cause different modes of cell death. We have previously demonstrated that the superoxide anions induce mainly apoptosis in primary rat hepatocytes and to a much lesser extent necrosis [40]. Superoxide anion-induced apoptosis was caspase-dependent (caspase-9, -6, and -3 were involved). In contrast, we have shown that hydrogen peroxide is not toxic at low doses, but causes necrosis at higher concentrations (or at low concentrations when hydrogen peroxide detoxification is inhibited).
Exposure to ROS has been shown to activate signal transduction pathways, such as phosphorylation of ERK1/2 and JNK MAP kinases. In hepatocytes, activation of ERK is anti-apoptotic, whereas activation of JNK is pro-apoptotic. Superoxide anions also induce the antioxidant enzyme HO-1. This induction is not sufficient to prevent superoxide-induced hepatocyte cell death. However, when HO-1 is induced before exposure to superoxide anions, the primary hepatocytes are protected against superoxide anion-induced apoptosis [41]. Carbon monoxide, one of the products of the enzymatic reaction of HO-1, is partially responsible for this protective effect as exogenously added CO inhibits superoxide anion-induced caspase activation, PARP cleavage, JNK activation, and apoptosis [41]. CO is suggested to down-regulate the ERK1/2 MAPK pathway and prevent transplant-induced hepatic ischemia/reperfusion injury [42]. In addition, CO is known to activate p38 MAPK. The activation of p38 MAPK protects liver against ischemia/reperfusion injury and has antioxidant effects in systemic liver inflammation [43, 44]. As stated above, superoxide anions also activate pro-apoptotic pathways, e.g., JNK. Apparently, the activation of pro-apoptotic pathways overrules the activation of survival pathways. Inhibition of JNK blocks superoxide anion-induced apoptosis and caspase-9 activation. This could indicate that JNK triggers the mitochondrial apoptotic pathway after exposure to superoxide anions. The well-known anti-apoptotic transcription factor NF-kB is not involved in the protection against superoxide anions-induced apoptosis.
5.2 Kupffer Cells
Kupffer cells, the liver-specific macrophages, are generally seen as the main source of oxidative stress in the liver next to neutrophils. ROS generation by Kupffer cells occurs via an oxidant burst. Prolonged production of oxidants involves activated complement factors. Kupffer cells produce hydrogen peroxide, superoxide anions, and hydroxyl radicals. NADPH oxidase is the principal enzyme involved in ROS production.
Kupffer cells are also involved in NASH. Serum leptin levels correlate with NAFLD/NASH severity. Leptin induces NADPH oxidase and inducible nitric oxide synthase (iNOS) in Kupffer cells and, as a result, superoxide anions and nitric oxide are produced. These compounds can react to form peroxynitrite, which is a strong oxidant. Peroxynitrite can also cause posttranslational modifications such as nitrosylation of proteins. Ultimately, this leads to activation of macrophages and production of TNF-α and MCP-1 [45].
DAMPS (damage- or danger-associated molecular patterns) are also known to activate Kupffer cells. For example, ATP is released after necrosis/apoptosis of hepatocytes and is then considered a DAMP. ATP can bind to the P2X7 receptor. This receptor is upstream of NADPH oxidase and can activate NADPH oxidase and subsequent ROS production by increasing the expression of the p47 phox subunit and the binding of p47 phox to the membrane subunit gp91 phox [46].
5.3 Endothelial Cells
Kupffer cells and liver sinusoidal endothelial cells (LSECs) together constitute the largest scavenger cell system in the body and they are responsible for the elimination of a wide range of potentially injurious particles, pathogens and molecules from the blood. Particulate matter (>200 nm in diameter) is phagocytosed by the Kupffer cells, whereas LSECs mediate clearance of soluble macromolecules and colloids <200 nm in diameter via receptor-mediated endocytosis [47].
In any injury, the tightly regulated microcirculation in the liver is disrupted as there is a shift towards more vasoconstrictive forces over vasodilating agents. This causes vasoconstriction, mostly because of an induction of the vasoconstrictor endothelin-1 (ET-1) which cannot be overcome by the vasodilator nitric oxide (NO), generated by endothelial nitric oxide synthase (eNOS) and, in case of inflammation, iNOS. Vasoconstriction leads to hypoxia, which can further aggravate liver damage. ET-1 is induced by oxidative stress, whereas receptor-mediated NO release is reduced by hydrogen peroxide. ET-1 can normally induce NO production by promoting the translocation of eNOS to the plasma membrane. This will restore the balance between vasoconstriction and vasodilation. However, upon acute oxidative stress exposure, eNOS cannot translocate to the plasma membrane, although normal phosphorylation of eNOS can still occur, leading to a reduction of NO production. Subacute oxidative stress also causes reduced NO production [48].
Oxidative stress can further affect these mechanisms. It has been demonstrated that exposure of LSECs to hydrogen peroxide induces the production of eicosanoids such as thromboxane A2 (TXA2), prostaglandin I2 (PGI2), and PGE2 via up-regulation of cyclooxygenase-2 (COX2), thromboxane synthase, and the phosphorylation of cytosolic phospholipase A2 (cPLA2). This causes vasodilatation. However, the combination of high ET-1 and hydrogen peroxide causes a decrease in the production of the vasodilating eicosanoids by LSECs. As a result, this combination leads to vasoconstriction [49].
The synergistic effect of NO and hydrogen peroxide is due to the inhibition of hydrogen peroxide degradation, since NO inhibits catalase (predominantly in hepatocytes) and/or glutathione peroxidases (prevailing in endothelial cells) [50].
In diabetes, there is oxidative injury to the vessel walls. In the liver, there are also ultrastructural changes in the hepatic microcirculation. It has been shown in in vivo models of diabetes that LSEC porosity is increased by ~50 %, and an increase in nitrosative stress has also been shown by demonstrating the presence of nitrosylated proteins in the sinusoidal endothelium, which was reduced by antioxidants [51].
5.4 Hepatic Stellate Cells
Hepatic stellate cells become activated in chronically injured liver. Upon activation, they proliferate and produce excessive amounts of extracellular matrix which eventually results in fibrosis and end stage cirrhosis. The exact cause of HSC activation is not known; however, many conditions and mechanisms have been shown to contribute to HSC activation, including oxidative stress. Oxidative stress has both paracrine and autocrine effects on HSC.
Paracrine effects include products that activate HSCs from oxidative-stress-damaged hepatocytes and oxidative stress-activated Kupffer cells.
These paracrine effects were investigated in co-culture experiments of hepatic stellate cells and hepatocytes or Kupffer cells. For example, co-culture of primary hepatic stellate cells with HepG2 cells (a human hepatoma cell line) manipulated to express increased levels of CYP2E1 showed higher rates of proliferation as well as induced levels of the fibrogenic activation markers α-smooth muscle actin (α-SMA) and collagen. This could be inhibited by the addition of antioxidants and CYP2E1 inhibitors [52, 53].
It has also been shown that ROS can induce hepatic stellate cell death. We have shown in hepatic stellate cells, similar to hepatocytes, that different ROS induce different modes of cell death. Superoxide anions induce apoptosis of HSCs in a caspase-independent manner [54]. HSCs were relatively resistant to hydrogen peroxide-induced necrosis, probably related to the induction of glutathione levels during stellate cell activation [55].
Lipid peroxidation products, especially 4HNE, can also activate HSC. A positive correlation between hepatic 4HNE and hepatic hydroxyproline content has been observed. Moreover, HSC are stimulated by 4HNE to produce collagen type 1, via signaling pathways involving kinases that modulate redox-sensitive transcription factors such as AP-1.
Acetaldehyde, the first metabolite of ethanol, also has direct effects on collagen production by HSC [56]: acetaldehyde induces hydrogen peroxide accumulation in stellate cells that in turn activate protein kinase C and phosphatidylinositol 3-kinase pathways [57, 58]. Recently, it was shown that acetaldehyde mediates β-catenin stabilization (by inhibiting its phosphorylation) and nuclear translocation in activated hepatic stellate cells. In addition to hydrogen peroxide, acetaldehyde also induces the production of superoxide anions and 4HNE. Exposure to oxidative stress results in the depletion of cellular glutathione stores and redox imbalance. In this environment redox sensors (NXN, a Wnt pathway regulator) are oxidized, leading to β-catenin stabilization [59].
Direct effects of oxidative stress on HSC activation have also been demonstrated.
Hepatic stellate cells can produce ROS themselves since they contain both the phagocytic as well as the non-phagocytic NADPH oxidase. NOX1, the non-phagocytic form of NADPH oxidase, is induced upon stimulation of HSC with platelet-derived growth factor (PDGF). ROS produced by NOX1 inactivates phosphatase and tensin homolog (PTEN) by oxidizing this protein. This, in turn, leads to activation of the Akt/FOXO4 pathway and, subsequently, downregulation of p27, a cell cycle repressor. Therefore, PDGF leads to HSC proliferation via NOX1-mediated ROS production [60].
NOX2, the phagocytic form of NADPH oxidase, is also present on hepatic stellate cells. It has been demonstrated that stellate cells, like macrophages, have the ability to phagocytose, in particular apoptotic bodies of hepatocytes. The engulfment of apoptotic bodies (from hepatocytes) by HSC was shown to be directly fibrogenic. This is mediated by NOX2, as NOX2-mediated ROS production is directly linked to increased collagen promoter activity.
Both NOX1 and NOX2 are inhibited in the p47 phox knockout model. P47 phox is the subunit known to be involved in the structural organization of the NOX subunits into a functional NADPH complex. The production of ROS by HSC induces PDGF [61]. PDGF signals through the PDGF-receptor to Ras and Raf-1 with subsequent activation of the MAPK pathway. In addition, MAPK activation was also shown to be induced by lipid peroxidation products (4HNE). These results indicate that proliferative pathways for HSC often involve ROS generation.
References
Halliwell B, Gutteridge JMC (1989) Free radicals in biology and medicine. Clarendon, Oxford, p 543
Miao L, St Clair DK (2009) Regulation of superoxide dismutase genes: implications in disease. Free Radic Biol Med 47:344–356
Fridovich I (1995) Superoxide radical and superoxide dismutases. Annu Rev Biochem 64:97–112
Rahman I, MacNee W (2000) Oxidative stress and regulation of glutathione in lung inflammation. Eur Respir J 16:534–554
Baeuerle PA, Baltimore D (1996) NF-kappa B: ten years after. Cell 87:13–20
Keum YS, Owuor ED, Kim BR, Hu R, Kong AN (2003) Involvement of Nrf2 and JNK1 in the activation of antioxidant responsive element (ARE) by chemopreventive agent phenethyl isothiocyanate (PEITC). Pharm Res 20:1351–1356
Kobayashi M, Yamamoto M (2005) Molecular mechanisms activating the Nrf2-Keap1 pathway of antioxidant gene regulation. Antioxid Redox Signal 7:385–394
Brunt EM, Tiniakos DG (2010) Histopathology of nonalcoholic fatty liver disease. World J Gastroenterol 16:5286–5296
Brunt EM (2010) Pathology of nonalcoholic fatty liver disease. Nat Rev Gastroenterol Hepatol 7:195–203
Tilg H, Moschen AR (2010) Evolution of inflammation in nonalcoholic fatty liver disease: the multiple parallel hits hypothesis. Hepatology 52:1836–1846
Tilg H (2010) The role of cytokines in non-alcoholic fatty liver disease. Dig Dis 28:179–185
Dowman JK, Tomlinson JW, Newsome PN (2010) Pathogenesis of non-alcoholic fatty liver disease. QJM 103:71–83
Kim WR, Ludwig J, Lindor KD (2000) Variant forms of cholestatic diseases involving small bile ducts in adults. Am J Gastroenterol 95:1130–1138
Qureshi WA (1999) Intrahepatic cholestatic syndromes: pathogenesis, clinical features and management. Dig Dis 17:49–59
Poupon R, Chazouilleres O, Poupon RE (2000) Chronic cholestatic diseases. J Hepatol 32:129–140
Sokol RJ, Devereaux M, Khandwala RA (1991) Effect of dietary lipid and vitamin E on mitochondrial lipid peroxidation and hepatic injury in the bile duct-ligated rat. J Lipid Res 32:1349–1357
Parola M, Leonarduzzi G, Robino G, Albano E, Poli G et al (1996) On the role of lipid peroxidation in the pathogenesis of liver damage induced by long-standing cholestasis. Free Radic Biol Med 20:351–359
Copple BL, Jaeschke H, Klaassen CD (2010) Oxidative stress and the pathogenesis of cholestasis. Semin Liver Dis 30:195–204
Jaeschke H, Bajt ML (2006) Intracellular signaling mechanisms of acetaminophen-induced liver cell death. Toxicol Sci 89:31–41
Nelson SD (1990) Molecular mechanisms of the hepatotoxicity caused by acetaminophen. Semin Liver Dis 10:267–278
Tsujimoto Y, Nakagawa T, Shimizu S (2006) Mitochondrial membrane permeability transition and cell death. Biochim Biophys Acta 1757:1297–1300
Ikesugi K, Mulhern ML, Madson CJ, Hosoya K, Terasaki T et al (2006) Induction of endoplasmic reticulum stress in retinal pericytes by glucose deprivation. Curr Eye Res 31:947–953
Badiola N, Penas C, Minano-Molina A, Barneda-Zahonero B, Fado R et al (2011) Induction of ER stress in response to oxygen-glucose deprivation of cortical cultures involves the activation of the PERK and IRE-1 pathways and of caspase-12. Cell Death Dis 2:e149
Mekahli D, Bultynck G, Parys JB, De Smedt H, Missiaen L (2011) Endoplasmic-reticulum calcium depletion and disease. Cold Spring Harb Perspect Biol 3(6):pii: a004317. doi:10.1101/cshperspect.a004317
Oyadomari S, Mori M (2004) Roles of CHOP/GADD153 in endoplasmic reticulum stress. Cell Death Differ 11:381–389
Benali-Furet NL, Chami M, Houel L, De Giorgi F, Vernejoul F et al (2005) Hepatitis C virus core triggers apoptosis in liver cells by inducing ER stress and ER calcium depletion. Oncogene 24:4921–4933
Higa A, Chevet E (2012) Redox signaling loops in the unfolded protein response. Cell Signal 24:1548–1555
Pedruzzi E, Guichard C, Ollivier V, Driss F, Fay M et al (2004) NAD(P)H oxidase nox-4 mediates 7-ketocholesterol-induced endoplasmic reticulum stress and apoptosis in human aortic smooth muscle cells. Mol Cell Biol 24:10703–10717
Li W, Yuan X, Nordgren G, Dalen H, Dubowchik GM et al (2000) Induction of cell death by the lysosomotropic detergent MSDH. FEBS Lett 470:35–39
Kagedal K, Zhao M, Svensson I, Brunk UT (2001) Sphingosine-induced apoptosis is dependent on lysosomal proteases. Biochem J 359:335–343
Terman A, Gustafsson B, Brunk UT (2006) The lysosomal-mitochondrial axis theory of postmitotic aging and cell death. Chem Biol Interact 163:29–37
Terman A, Kurz T, Gustafsson B, Brunk UT (2006) Lysosomal labilization. IUBMB Life 58:531–539
Malhi H, Gores GJ, Lemasters JJ (2006) Apoptosis and necrosis in the liver: a tale of two deaths? Hepatology 43:S31–S44
Schoemaker M, Moshage H (2004) Defying death: the hepatocyte’s survival kit. Clin Sci (Lond) 107:13–25
Mahmood Z, Shukla Y (2010) Death receptors: targets for cancer therapy. Exp Cell Res 316:887–899
Li M, Beg AA (2000) Induction of necrotic-like cell death by tumor necrosis factor alpha and caspase inhibitors: novel mechanism for killing virus-infected cells. J Virol 74:7470–7477
Giampietri C, Starace D, Petrungaro S, Filippini A, Ziparo E (2014) Necroptosis: molecular signalling and translational implications. Int J Cell Biol 2014:490275
Maiuri MC, Zalckvar E, Kimchi A, Kroemer G (2007) Self-eating and self-killing: crosstalk between autophagy and apoptosis. Nat Rev Mol Cell Biol 8:741–752
Ryter SW, Choi AM (2013) Autophagy: an integral component of the mammalian stress response. J Biochem Pharmacol Res 1:176–188
Conde de la Rosa L, Schoemaker M, Vrenken T, Buist-Homan M, Havinga R et al (2006) Superoxide anions and hydrogen peroxide induce hepatocyte death by different mechanisms: involvement of JNK and ERK MAP kinases. J Hepatol 44:918–929
Conde de la Rosa L, Vrenken T, Hannivoort R, Buist-Homan M, Havinga R et al (2008) Carbon monoxide blocks oxidative stress-induced hepatocyte apoptosis via inhibition of the p54 JNK isoform. Free Radic Biol Med 44:1323–1333
Kaizu T, Ikeda A, Nakao A, Tsung A, Toyokawa H et al (2008) Protection of transplant-induced hepatic ischemia/reperfusion injury with carbon monoxide via MEK/ERK1/2 pathway downregulation. Am J Physiol Gastrointest Liver Physiol 294:G236–G244
Amersi F, Shen XD, Anselmo D, Melinek J, Iyer S et al (2002) Ex vivo exposure to carbon monoxide prevents hepatic ischemia/reperfusion injury through p38 MAP kinase pathway. Hepatology 35:815–823
Brugger J, Schick MA, Brock RW, Baumann A, Muellenbach RM et al (2010) Carbon monoxide has antioxidative properties in the liver involving p38 MAP kinase pathway in a murine model of systemic inflammation. Microcirculation 17:504–513
Chatterjee S, Ganini D, Tokar EJ, Kumar A, Das S et al (2013) Leptin is key to peroxynitrite-mediated oxidative stress and kupffer cell activation in experimental non-alcoholic steatohepatitis. J Hepatol 58:778–784
Chatterjee S, Rana R, Corbett J, Kadiiska MB, Goldstein J et al (2012) P2X7 receptor-NADPH oxidase axis mediates protein radical formation and kupffer cell activation in carbon tetrachloride-mediated steatohepatitis in obese mice. Free Radic Biol Med 52:1666–1679
Seternes T, Sorensen K, Smedsrod B (2002) Scavenger endothelial cells of vertebrates: a nonperipheral leukocyte system for high-capacity elimination of waste macromolecules. Proc Natl Acad Sci U S A 99:7594–7597
Karaa A, Kamoun WS, Clemens MG (2005) Oxidative stress disrupts nitric oxide synthase activation in liver endothelial cells. Free Radic Biol Med 39:1320–1331
Karaa A, Kamoun WS, Xu H, Zhang J, Clemens MG (2006) Differential effects of oxidative stress on hepatic endothelial and kupffer cell eicosanoid release in response to endothelin-1. Microcirculation 13:457–466
Rauen U, Li T, de Groot H (2007) Inhibitory and enhancing effects of NO on H(2)O(2) toxicity: dependence on the concentrations of NO and H(2)O(2). Free Radic Res 41:402–412
McMahon AC, Parry SN, Benson VL, Witting PK, Le Couteur DG (2013) Beneficial effects of the synthetic antioxidant tert-butyl bisphenol on the hepatic microcirculation in a rat model of diabetes mellitus. Acta Diabetol 50:645–649
Nieto N, Friedman SL, Cederbaum AI (2002) Stimulation and proliferation of primary rat hepatic stellate cells by cytochrome P450 2E1-derived reactive oxygen species. Hepatology 35:62–73
Nieto N, Friedman SL, Cederbaum AI (2002) Cytochrome P450 2E1-derived reactive oxygen species mediate paracrine stimulation of collagen I protein synthesis by hepatic stellate cells. J Biol Chem 277:9853–9864
Dunning S, Hannivoort R, de Boer J, Buist-Homan M, Faber K et al (2009) Superoxide anions and hydrogen peroxide inhibit proliferation of activated rat stellate cells and induce different modes of cell death. Liver Int 29:922–932
Dunning S, Ur Rehman A, Tiebosch MH, Hannivoort RA, Haijer FW et al (2013) Glutathione and antioxidant enzymes serve complementary roles in protecting activated hepatic stellate cells against hydrogen peroxide-induced cell death. Biochim Biophys Acta 1832:2027–2034
Moshage H, Casini A, Lieber CS (1990) Acetaldehyde selectively stimulates collagen production in cultured rat liver fat-storing cells but not in hepatocytes. Hepatology 12:511–518
Svegliati-Baroni G, Ridolfi F, Di Sario A, Saccomanno S, Bendia E et al (2001) Intracellular signaling pathways involved in acetaldehyde-induced collagen and fibronectin gene expression in human hepatic stellate cells. Hepatology 33:1130–1140
Svegliati-Baroni G, Inagaki Y, Rincon-Sanchez AR, Else C, Saccomanno S et al (2005) Early response of alpha2(I) collagen to acetaldehyde in human hepatic stellate cells is TGF-beta independent. Hepatology 42:343–352
Arellanes-Robledo J, Reyes-Gordillo K, Shah R, Dominguez-Rosales JA, Hernandez-Nazara ZH et al (2013) Fibrogenic actions of acetaldehyde are beta-catenin dependent but wingless independent: a critical role of nucleoredoxin and reactive oxygen species in human hepatic stellate cells. Free Radic Biol Med 65:1487–1496
Cui W, Matsuno K, Iwata K, Ibi M, Matsumoto M et al (2011) NOX1/nicotinamide adenine dinucleotide phosphate, reduced form (NADPH) oxidase promotes proliferation of stellate cells and aggravates liver fibrosis induced by bile duct ligation. Hepatology 54:949–958
Adachi T, Togashi H, Suzuki A, Kasai S, Ito J et al (2005) NAD(P)H oxidase plays a crucial role in PDGF-induced proliferation of hepatic stellate cells. Hepatology 41:1272–1281
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Tiebosch, M.H., Karimian, G., Moshage, H. (2015). Oxidative Stress and Hepatocellular Injury. In: Albano, E., Parola, M. (eds) Studies on Hepatic Disorders. Oxidative Stress in Applied Basic Research and Clinical Practice. Humana Press, Cham. https://doi.org/10.1007/978-3-319-15539-5_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-15539-5_4
Publisher Name: Humana Press, Cham
Print ISBN: 978-3-319-15538-8
Online ISBN: 978-3-319-15539-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)