Abstract
The following chapter reports on the health impacts of perfluoroalkylated compounds in the context of in vitro and in vivo immunotoxicology studies as well as epidemiology studies. In general, elevated serum PFAA levels reported in adults and children correlate with observed changes in health to include decreases in serum vaccine titers and IgE levels, or increases in antinuclear antibodies, asthma, the common cold, and gastroenteritis. Laboratory studies demonstrate direct, in vitro effects of perfluorinated compounds modulating TNF-α, IL-6 and IFN-γ. These studies may be linked mechanistically to alterations reporting decreases in vaccine antibody titers in human reports and dose-responsive, decreases in IgM antibody production in animal models. To some extent, perfluoroalkylated compounds are thought to modulate gene regulation via peroxisome proliferator activated receptor alpha (PPARα) and to a lesser extent via peroxisome proliferator activated receptor gamma (PPARγ), yet species differences affecting the expression of this receptor complicates this interpretation as an underlying mechanism in humans. Mechanisms of action beyond PPAR-mediated effects represents new directions and are also discussed. As we learn more about the relationship between perfluoroalkylated compounds and emerging health issues, this may challenge current benchmark thresholds in drinking water to ensure adequate protection for human health.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
10.1 Immunotoxicity in Human Studies: Epidemiology
In an ongoing epidemiological study of humans living near a PFC production facility in West Virginia, levels of IgA, IgE (females only), and C-reactive protein decreased with increasing PFOA serum concentration in adults. Additionally, antinuclear antibodies, a marker of autoimmunity, increased with increasing PFOA serum concentration (Fletcher et al. 2009). In another study, there was no association between serum PFOA concentrations and immunoglobin levels in male workers (Costa et al. 2009). It is not until we explore the effects of PFOA and PFOS on children exposed in utero or post-natal development, that the epidemiology studies suggest a stronger link with immune dysfunction.
Most studies linking PFOA and PFOS to changes in immunity have been typically examined within the scope of maternal and child health. Specifically, perfluorinated contaminant blood levels and health of mothers and children have been monitored over time to learn about susceptibility to disease or vaccine titers. In one study, the relationship between maternal PFOA and PFOS exposure and hospitalization due to incidence of childhood infectious disease was examined. Fei and colleagues (2010) measured PFOA and PFOS in maternal blood during the first trimester of pregnancy in nearly 1,400 women from the Danish National Birth Cohort. Mean serum PFOA was 5.6 ng/ml and PFOS was 35.3 ng/ml. However, these data did not unequivocally support that prenatal exposure to PFOA and PFOS increased the risk of hospitalizations due to infectious diseases during early childhood. Limitations of the study include social and behavioral factors that may have influenced the correlation between PFCs and age-related immune responses.
The incidence of infant allergies, infectious disease and changes in IgE levels in cord blood have also been examined with regards to maternal PFC exposure. Okada et al. (2012) measured PFOS and PFOA in maternal serum after the second trimester (n = 343) and total IgE concentration in cord blood (n = 231). Maternal self-administered questionnaires indicated no significant association with maternal PFOA levels and incidence of infant allergies and infectious disease. However, cord blood IgE levels in female infants only, decreased significantly with increasing maternal serum PFOA. As a point of reference, mean maternal PFOA concentration was 1.4 ng/mL and IgE levels in cord blood was 0.62 IU/mL. In contrast to this study, Wang et al. (2011) reported that PFOA and PFOS concentrations in cord blood were positively correlated with cord blood IgE levels, but only in male offspring. However, following these children to the age of 2 revealed no association between PFCs and atopic dermatitis.
A sub-project of the Norwegian Mother and Child Cohort Study examined maternal serum concentrations of PFOA and PFOS and the antibody titers of 3-year old children (Granum et al. 2013). Average maternal serum concentrations were 1.1 ng/ml for PFOA and 5.6 ng/ml for PFOS. In 3 year old children, a positive association was observed between maternal PFOA and perfluorononanoic acid (PFNA) with number of episodes of common cold, as well as between PFOA and perfluorohexane sulfonate (PFHxS) with number of episodes of gastroenteritis.
Dong et al. (2013) investigated the relationship between perfluorinated compounds and incidence of childhood asthma. This was a cross-sectional study of 231 children age 10–15 years with physician-diagnosed asthma and 225 age-matched non-asthmatic controls recruited from two hospitals in Northern Taiwan. Serum was collected for measurement of ten perfluorinated compounds while absolute eosinophil counts, total IgE, eosinophilic cationic protein and asthmas were assessed. Both PFOA and PFOS serum levels were significantly associated with biomarkers and asthma severity scores in the children. Serum levels of PFOS in asthmatic and non-asthmatic children were 45.5 ± 37.5 and 33.4 ± 26.4 ng/mL, respectively, while serum levels of PFOA in asthmatic and non-asthmatic children were 1.5 ± 1.3 and 1.0 ± 1.1 ng/mL respectively.
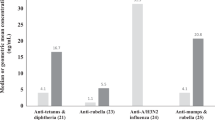
In a prospective study, a birth cohort of 587 singleton births during 1999–2001 from the National Hospital in the Faroe Islands examined children’s antibody levels to diphtheria and tetanus vaccines in the context of perfluorinated compounds (Grandjean et al. 2012). Serum antibody concentrations were measured in mothers and children at age 5 years pre-booster, approximately 4 weeks after the booster, and at age 7 years. Previously, prenatal exposures to perfluorinated compounds were assessed in the mother during week 32 of pregnancy. Average maternal serum concentrations analyzed at 32 weeks of pregnancy were 3.2 ng/ml for PFOA and 27.3 ng/ml for PFOS. Serum concentrations were collected from the children at 5 years of age (mean of 4.06 ng/ml for PFOA and 16.7 mg/ml for PFOS) and serum antibody concentrations were collected at 5 and 7 years of age. Prenatal exposure to PFOA and PFOS were negatively associated with antibody titers against diphtheria. Maternal PFOS exposure was most strongly associated with responses in 5 year olds and postnatal exposure to both PFOA and PFOS were most strongly associated with responses in 7 year olds. The authors also examined deviations from the clinically protective level of 0.1 IU/L and reported that both pre- and postnatal exposure to PFOS and postnatal PFOA exposure were associated with increased odds of antibody titers being below clinically protective levels. The researchers learned that a twofold increase in levels of PFOS and PFOA at age 5 lead to a several fold decrease in protective antibodies against diphtheria and tetanus.
When gathering additional data, Grandjean and Budtz-Jørgensen (2013) estimated benchmark doses based on their 2012 study, under the assumption that previously published benchmark doses (BMDs) are not adequately protective of children or of the general public given potential suppression of immune responses. A BMD of 1.3 ng/ml for PFOS and 0.3 ng/ml for PFOA were determined. Additionally, they calculated a BMDL (benchmark dose level, or lower one-sided 95 % confidence limit of the BMD) of 1 μg/l and a reference dose (RfD) of 1 ng/l. The US EPA provisional health advisory for drinking water is 0.4 μg/l for PFOA and 0.2 μg/l for PFOS (2010/2015 PFOA Stewardship Program). As the latter is grounded on developmental and subchronic toxicity, these references levels are not likely to encompass immunotoxicity that are derived using serum levels (i.e., and RfD of 1 ng/l). If a BMD based on serum vaccine titers were acknowledged, then current limits may be several hundred-fold too high.
10.2 Immunotoxicity in Human Studies: In Vitro
Only a few studies investigate the direct, in vitro effects of perfluorinated compounds on human cells. Using donated blood from 11 volunteers, peripheral blood mononuclear cells (PBMCs) were isolated and tested for NK cytolytic activity following in vitro exposure to PFOA or PFOS (Brieger et al. 2011). Viability of PMBCs was not affected, yet suppression of NK cytolytic activity and increasing TNF-α following lipopolysaccharide (LPS) stimulation was observed. Using a human promyelocytic cell line (THP-1), cellular mechanisms of PFC immunotoxicity have been examined by other researchers (Corsini et al. 2011, 2012, 2014). In addition to PFOS and PFOA, perfluorobutane sulfonic acid (PFBS), perfluorodecanoic acid (PFDA), perfluorooctanesulfonic acid (PFOSA), and a fluorotelomer (8:2 Telomer) all suppressed LPS-induced TNF-α production. PFOSA, PFOS, PFDA, and fluorotelomer affected IL-6 and IFN-γ release. All compounds except PFOA suppressed PHA-induced IL-10 release. These studies also report that PFOA and PFOS have different effects on immune cells and that PFOA-mediated suppression of cytokine production appeared to be dependent on PPARα activation whereas the actions of PFOS were independent of PPARα activation. Furthermore, leukocytes from female donors appeared to be more sensitive to PFCs than male donors, suggesting sex differences with regard to immune responses. These in vitro studies in the context of epidemiology studies, demonstrate that perfluorinated chemicals affect immunological cells by altering cytokine expression and these observations, although early in this investigation, can be linked mechanistically to alterations reported in decreased vaccine antibody titers reported in human studies.
10.3 Immunotoxicity in Rodent Models
Preliminary concerns about PFC immunotoxicity were based early reports that indicated reduction in relative spleen and thymus weights and suppression of the T cell dependent antibody response (TDAR). PFOA, PFOS, and ammonium perfluorooctanoate (APFO, a precursor compound to PFOA) in rodent models have demonstrated that these compounds suppress TDAR and, in the case of PFOS, suppress TDAR at doses within the range of exposures for the general human population (Peden-Adams 2008; reviewed in DeWitt et al. 2009, 2012). Since SRBC-specific IgM production is considered predictive of immunotoxicity and decreased host resistance (Luster et al. 1992, 1993; Selgrade 1999), these alterations in murine immune function are useful in extrapolating to human health risk (Selgrade 2007). Consequently, the focus of further research reports have concentrated on possible mechanisms of action related to this aspect of immune function.
PFOS and PFOA have both been shown to alter antigen-specific antibody production to a T cell dependent antigen, namely sheep red blood cells (SRBC). Using a B6C3F1 mouse model and SRBC challenge, PFOS decreased IgM production (as measured by the plaque-forming cell response) in both male and female mice (1.66 and 16.6 μg/kg/day, respectively, lowest observed adverse effect level [LOAEL] for each sex) at blood concentrations of 91.5 ± 22.2 ng/g and 666 ± 108 ng/g (mean ± SD) by 52 % and 50 %, respectively (Peden-Adams et al. 2008). Moreover, TDAR suppression due to PFC exposure has been supported with replication in at least four reported studies (Peden-Adams et al. 2008; DeWitt et al. 2008; Zhang et al. 2013; Dong et al. 2009).
Keyhole limpet hemocyanin (KLH) antigenic challenge (T cell dependent antigen) has also been used to test adaptive immune function following exposure to PFCs. Conversely, KLH-specific IgG levels were not affected in female Sprague-Dawley rats following exposure to PFOS (Lefebvre et al. 2008). Depending on the methodology, plaque-forming cell or ELISA, it is not uncommon to observe different outcomes in these assays, even with two T cell dependent antigens (Loveless et al. 2007; White et al. 2007).
Adaptive immunity to a T cell independent antigenic challenge also varies following exposure to PFCs. Using TNP-LPS challenge, a T cell independent antigen, IgM antibody production was decreased at 0.334 mg PFOS/kg/d (334 μg/kg/day; 12). In a separate study with C57BL/6 female mice, the T cell independent antibody response also was suppressed after 15 days of drinking water exposure to 1.88 mg/kg of PFOA (DeWitt, unpublished data).
In addition to effects on adaptive immunity, PFOS and PFOA also effect cell populations in the bone marrow (Qazi et al. 2012). Specifically, a high dose, 10 day dietary exposure significantly reduced the total numbers of cells in the bone marrow including myeloid, pro/pre B, immature B and early mature B cells. Partial or complete restoration of the cell number occurred following 10 days of withdrawal of these compounds. At the lower dose of 0.002 %, only PFOA reduced the B-lymphoid cell population.
Quantitatively linking an immunological effect to onset of disease is key to improving species extrapolation and characterization of potential human health risks. The following studies demonstrate such a link. A LOAEL has been established at 0.5 mg/kg PFOS total dose (serum level = 666 ± 108 ng/g) in female B6C3F1 mice for decreased SRBC-IgM production (Peden-Adams et al. 2008). At comparable exposure levels, Guruge and colleagues (2009) reported susceptibility to influenza A-induced mortality. Taken together, these reports suggest that PFOS-induce humoral immune suppression at lower levels of exposure may be enough to compromise a host to disease onset. This is further corroborated by a study demonstrating that the PFC response may be predicative of susceptibility to influenza virus (Burleson and Burleson 2010) and recent studies in humans that indicate PFOS and PFOA may be associated with decreased responses to childhood vaccines (Grandjean et al. 2012; Granum et al. 2012).
As rodents are useful in characterizing immunotoxicity, these models are not without caveats. For instance, immunotoxicity outcomes vary between species and gender following exposure to PFOS and PFOA. Mice seem to be more sensitive to the effects of PFOS and PFOA as compared to rats (Loveless et al. 2008; DeWitt et al. 2008; Yang et al. 2002; Peden-Adams et al. 2008; Lefebvre et al. 2008). In both a rat and mouse model, males were more sensitive to the noted effects on antibody production (Peden-Adams et al. 2008; Lefebvre et al. 2008). In fact, a tenfold difference in the LOAEL (based on dose and approximately sevenfold difference based on serum PFOS concentrations) was reported between males and females (Peden-Adams et al. 2008). B6C3F1 mice exposed during gestation demonstrated an increased male sensitivity to PFOS-induced suppression of IgM antibody production (Keil et al. 2008). As we learn more about possible mechanisms of action of PFCs, gender and species disparities may be explained in part by differences PPARα expression.
10.4 Mechanisms of Action in Immunotoxicity
The weight of evidence suggests that the primary mechanism of action for PFC-induced modulation of cellular processes is via the activation of PPARs (reviewed by Anderson et al. 2008; Butenhoff et al. 2012; Rosen et al. 2010). Both PFOS and PFOA bind to the peroxisome proliferator activated receptor alpha (PPARα). These transcription factors (PPARα and PPARγ) are ubiquitous and regulate gene expression by modulating lipid pathways, increasing permeability of mitochondrial membranes, affecting glucose regulation, cell proliferation, and inflammatory processes (Post et al. 2012; Starkov and Wallace 2002). Activation of PPARα by PFCs has been a major focus of mechanistic studies, with a greater role for PPARα as compared to PPARγ in mediating toxicity (Post et al. 2012; Takacs and Abbott 2007; Vanden Heuvel et al. 2006).
It is considered that immunotoxicity varies between species and gender due to the differential expression of these PPAR transcription factors in humans and in rodent models. Human hepatic PPARα expression is only one-tenth that of rodents (Kennedy et al. 2004). In general, males endure a longer half-life elimination rate as compared to females (Kudo et al. 2006).
Some studies have suggested other routes of toxicity for PFCs, however, many of these proposed pathways are not independent of the influence of PPAR. This is largely due to the fact that PPAR transcription factors are extensively expressed on lymphocytes, hepatocytes, cardiac cells, and microglia with the potential to affect numerous physiological pathways. Further examination of alternate mechanisms of actions by PFCs is certainly necessary to facilitate a more complete consideration of human health effects.
10.5 Proinflammatory Cytokines
Both PFOS and PFOA bind to the peroxisome proliferator activated receptor alpha (PPARα) and a significant number of PPARα agonists have been shown to reduce inflammation (Griesbacher et al. 2008). Therefore, it would seem that PFCs would reduce expression of cytokines or other related inflammatory markers. However, this is not the case. Increases in serum levels of the proinflammatory cytokines IL-6 and TNF-α associated with PFOS and PFOA exposure have been reported in mouse models. Qazi et al. (2009) reported increased basal serum concentrations of IL-6 in male C57Bl/6 mice, but not TNF-α following exposure to 400 mg/kg total dose (0.02 % in diet for 10 days of either PFOS or PFOA). This pattern of increased basal serum IL-6 but not TNF-α was also reported by Dong et al. (2011) in male C57Bl/6 mice exposed to 50 and 125 mg/kg total dose of PFOS. Mollenhauer et al. (2011) reported increased serum IL-6 and decreased serum TNF-α at 1 mg/kg total dose following LPS injection and PFOS exposure for 28 days.
Proinflammatory cytokines are produced by peritoneal macrophages in the presence of PFCs. Following LPS challenge in vitro or in vivo, peritoneal macrophages responded by producing more TNF-α and IL-6 at PFOS concentrations ranging from 25 to 400 mg/kg total dose (Qazi et al. 2009; Dong et al. 2011). PFOA exposure also increases ex vivo TNF-α production after both in vitro and in vivo LPS stimulation at 400 mg/kg total dose (Qazi et al. 2009). Dong et al. (2011) observed increased ex vivo production of TNF-α and IL-6 from mixed spleen cell cultures at 125 mg PFOS/kg total dose while Qazi et al. (2009) reported similar results at 400 mg PFOS/kg total dose for TNF-α production, but not IL-6 production. Most PPARα agonists are known to reduce inflammation, yet this is not the case with PFCs. This is likely to suggest that PFCs possess multiple mechanisms of action on immune function that are not typical PPARα agonist mediated effects.
10.6 Conclusions
We have learned from rodent models that both PFOS and PFOA induce a dose-responsive suppression on adaptive immunity in mice. One of the primary differences between these two is that PFOA reduced the number of B and T cells (Yang et al. 2002), while PFOS induced suppression of antigen-specific antibody responses independent of significant reductions in B and T cell numbers (Dong et al. 2012; Peden-Adams et al. 2008; Keil et al. 2008). The mechanism(s) involved in PFC-induced suppression of adaptive immunity is likely linked with altered cytokine signaling that arises from interaction of PFCs with PPARα, but may also be related to the interaction of PFCs with other signaling molecules, such as NFκB (Corsini et al. 2012).
When extrapolating rodent studies to humans, it is concerning that suppression of adaptive immunity occurs at PFC exposure levels that are within a reasonable range for human exposure. Furthermore, the few human epidemiology studies currently available generally report that T-cell dependent production of antibody following vaccination is suppressed. This is further weighted with comparable observations in rodent models. However, mechanisms of action beyond PPARα-mediated effects require further examination. Human and rodent studies are far from complete and it is clear that we must learn more about mechanism(s) of immunotoxicity to reduce PFC-associated health effects and improve regulatory exposure limits.
References
2010/2015 PFOA Stewardship Program|PFOA and Fluorinated Telomers|OPPT|OPPTS|US EPA
Andersen ME, Butenhoff JL, Chang S-C, Farrar DG, Kennedy GL et al (2008) Perfluoroalkyl acids and related chemistries–toxicokinetics and modes of action. Toxicol Sci 102:3–14
Brieger A, Bienefeld N, Hasan R, Goerlich R, Haase H (2011) Impact of perfluorooctanesulfonate and perfluorooctanoic acid on human peripheral leukocytes. Toxicol In Vitro 25:960–968. doi:10.1016/j.tiv.2011.03.005
Burleson FG, Burleson GR (2010) Host resistance assays including bacterial challenge models. Methods Mol Biol 598:97–108. doi:10.1007/978-1-60761-401-2_7
Butenhoff JL, Chang S-C, Olsen GW, Thomford PJ (2012) Chronic dietary toxicity and carcinogenicity study with potassium perfluorooctanesulfonate in Sprague Dawley rats. Toxicology 293:1–15. doi:10.1016/j.tox.2012.01.003
Corsini E, Avogadro A, Galbiati V, dell’Agli M, Marinovich M et al (2011) In vitro evaluation of the immunotoxic potential of perfluorinated compounds (PFCs). Toxicol Appl Pharmacol 250:108–116. doi:10.1016/j.taap.2010.11.004
Corsini E, Sangiovanni E, Avogadro A, Galbiati V, Viviani B et al (2012) In vitro characterization of the immunotoxic potential of several perfluorinated compounds (PFCs). Toxicol Appl Pharmacol 258:248–255
Corsini E, Luebke RW, Germolec DR, DeWitt JC (2014) Perfluorinated compounds: emerging POPs with potential immunotoxicity. Toxicol Lett 230(2):263–270
Costa G, Sartori S, Consonni D (2009) Thirty years of medical surveillance in perfluorooctanoic acid production workers. J Occup Environ Med 51(3):364–372
Dewitt JC, Copeland CB, Strynar MJ, Luebke RW (2008) Perfluorooctanoic acid-induced immunomodulation in adult C57BL/6J or C57BL/6N female mice. Environ Health Perspect 116:644–650. doi:10.1289/ehp.10896
DeWitt JC, Shnyra A, Badr MZ, Loveless SE, Hoban D et al (2009) Immunotoxicity of perfluorooctanoic acid and perfluorooctane sulfonate and the role of peroxisome proliferator-activated receptor alpha. Crit Rev Toxicol 39:76–94. doi:10.1080/10408440802209804
DeWitt JC, Peden-Adams MM, Keller JM, Germolec DR (2012) Immunotoxicity of perfluorinated compounds: recent developments. Toxicol Pathol 40:300–311. doi:10.1177/0192623311428473
Dong G-H, Zhang Y-H, Zheng L, Liu W, Jin Y-H et al (2009) Chronic effects of perfluorooctanesulfonate exposure on immunotoxicity in adult male C57BL/6 mice. Arch Toxicol 83:805–815. doi:10.1007/s00204-009-0424-0
Dong G-H, Liu M-M, Wang D, Zheng L, Liang Z-F et al (2011) Sub-chronic effect of perfluorooctanesulfonate (PFOS) on the balance of type 1 and type 2 cytokine in adult C57BL6 mice. Arch Toxicol 85:1235–1244. doi:10.1007/s00204-011-0661-x
Dong G-H, Wang J, Zhang Y-H, Liu M-M, Wang D, Zheng L, Jin Y-H (2012) Induction of p53-mediated apoptosis in splenocytes and thymocytes of C57BL/6 mice exposed to perfluorooctane sulfonate (PFOS). Toxicol Appl Pharmacol 264(2):292–299
Dong GH, Tung KY, Tsai CH, Liu MM, Wang D, Liu W, Chen PC, Jin YH, Hsieh WS, Lee YL (2013) Serum polyfluoroalkyl concentrations, asthma outcomes, and immunological markers in a case-control study of Taiwanese children. Environ Health Perspect 121(4):507
Fei C, McLaughlin JK, Lipworth L, Olsen J (2010) Prenatal exposure to PFOA and PFOS and risk of hospitalization for infectious diseases in early childhood. Environ Res 110:773–777. doi:10.1016/j.envres.2010.08.004
Fletcher T, Steenland K, Savitz D (2009) PFOA and immune biomarkers in adults exposed to PFOA in drinking water in the mid Ohio Valley. Status Rep by C8 Sci Panel. Available: http://www.c8sciencepanel.org/pdfs/Status_Report_C8_and_Immune_markers_March2009.pdf
Grandjean P, Budtz-Jørgensen E (2013) Immunotoxicity of perfluorinated alkylates: calculation of benchmark doses based on serum concentrations in children. Environ Health 12:35. doi:10.1186/1476-069X-12-35
Grandjean P, Andersen EW, Budtz-Jørgensen E, Nielsen F, Mølbak K et al (2012) Serum vaccine antibody concentrations in children exposed to perfluorinated compounds. JAMA 307:391–397. doi:10.1001/jama.2011.2034
Granum B, Haug LS, Namork E, Stølevik SB, Thomsen C, Aaberge IS, van Loveren H, Lovik M, Nygaard UC (2013) Pre-natal exposure to perfluoroalkyl substances may be associated with altered vaccine antibody levels and immune-related health outcomes in early childhood. J Immunotoxicol 10(4):373–379
Griesbacher T, Pommer V, Schuligoi R, Tiran B, Peskar B a (2008) Anti-inflammatory actions of perfluorooctanoic acid and peroxisome proliferator-activated receptors (PPAR) alpha and gamma in experimental acute pancreatitis. Int Immunopharmacol 8:325–329. doi:10.1016/j.intimp.2007.08.005
Guruge KS, Hikono H, Shimada N, Murakami K, Hasegawa J et al (2009) Effect of perfluorooctane sulfonate (PFOS) on influenza A virus-induced mortality in female B6C3F1 mice. J Toxicol Sci 34:687–691
Keil DE, Mehlmann T, Butterworth L, Peden-Adams MM (2008) Gestational exposure to perfluorooctane sulfonate suppresses immune function in B6C3F1 mice. Toxicol Sci 103:77–85. doi:10.1093/toxsci/kfn015
Kennedy GL, Butenhoff JL, Olsen GW, O’Connor JC, Seacat AM, Perkins RG, Farrar DG (2004) The toxicology of perfluorooctanoate. Crit Rev Toxicol 34(4):351–384
Kudo N, Suzuki-Nakajima E, Mitsumoto A, Kawashima Y (2006) Responses of the liver to perfluorinated fatty acids with different carbon chain length in male and female mice: in relation to induction of hepatomegaly, peroxisomal beta-oxidation and microsomal 1-acylglycerophosphocholine acyltransferase. Biol Pharm Bull 29:1952–1957
Lefebvre DE, Curran I, Armstrong C, Coady L, Parenteau M et al (2008) Immunomodulatory effects of dietary potassium perfluorooctane sulfonate (PFOS) exposure in adult Sprague-Dawley rats. J Toxicol Environ Health A 71:1516–1525. doi:10.1080/15287390802391943
Loveless SE, Ladics GS, Smith C, Holsapple MP, Woolhiser MR et al (2007) Interlaboratory study of the primary antibody response to sheep red blood cells in outbred rodents following exposure to cyclophosphamide or dexamethasone. J Immunotoxicol 4:233–238. doi:10.1080/15476910701385687
Loveless SE, Hoban D, Sykes G, Frame SR, Everds NE (2008) Evaluation of the immune system in rats and mice administered linear ammonium perfluorooctanoate. Toxicol Sci 105:86–96. doi:10.1093/toxsci/kfn113
Luster MI, Portier C, Pait DG, White KL, Gennings C et al (1992) Risk assessment in immunotoxicology. I. Sensitivity and predictability of immune tests. Fundam Appl Toxicol 18:200–210
Luster MI, Portier C, Pait DG, Rosenthal GJ, Germolec DR et al (1993) Risk assessment in immunotoxicology. II. Relationships between immune and host resistance tests. Fundam Appl Toxicol 21:71–82
Mollenhauer MAM, Bradshaw SG, Fair PA, McGuinn WD, Peden-Adams MM (2011) Effects of perfluorooctane sulfonate (PFOS) exposure on markers of inflammation in female B6C3F1 mice. J Environ Sci Health A Tox Hazard Subst Environ Eng 46:97–108. doi:10.1080/10934529.2011.532418
Okada E, Sasaki S, Saijo Y, Washino N, Miyashita C et al (2012) Prenatal exposure to perfluorinated chemicals and relationship with allergies and infectious diseases in infants. Environ Res 112:118–125
Peden-Adams MM, Keller JM, Eudaly JG, Berger J, Gilkeson GS et al (2008) Suppression of humoral immunity in mice following exposure to perfluorooctane sulfonate. Toxicol Sci 104:144–154. doi:10.1093/toxsci/kfn059
Post GB, Cohn PD, Cooper KR (2012) Perfluorooctanoic acid (PFOA), an emerging drinking water contaminant: a critical review of recent literature. Environ Res 116:93–117
Qazi MR, Bogdanska J, Butenhoff JL, Nelson BD, DePierre JW et al (2009) High-dose, short-term exposure of mice to perfluorooctanesulfonate (PFOS) or perfluorooctanoate (PFOA) affects the number of circulating neutrophils differently, but enhances the inflammatory responses of macrophages to lipopolysaccharide (LPS) in a similar fashion. Toxicology 262:207–214. doi:10.1016/j.tox.2009.06.010
Qazi MR, Nelson BD, DePierre JW, Abedi-Valugerdi M (2012) High-dose dietary exposure of mice to perfluorooctanoate or perfluorooctane sulfonate exerts toxic effects on myeloid and B-lymphoid cells in the bone marrow and these effects are partially dependent on reduced food consumption. Food Chem Toxicol 50(9):2955–2963
Rosen MB, Schmid JR, Corton JC, Zehr RD, Das KP et al (2010) Gene expression profiling in wild-type and PPARα-null mice exposed to perfluorooctane sulfonate reveals PPARα-independent effects. PPAR Res 2010. doi:10.1155/2010/794739
Selgrade MK (1999) Use of immunotoxicity data in health risk assessments: uncertainties and research to improve the process. Toxicology 133:59–72
Selgrade MK (2007) Immunotoxicity: the risk is real. Toxicol Sci 100:328–332. doi:10.1093/toxsci/kfm244
Starkov AA, Wallace KB (2002) Structural determinants of fluorochemical-induced mitochondrial dysfunction. Toxicol Sci 66:244–252
Takacs ML, Abbott BD (2007) Activation of mouse and human peroxisome proliferator-activated receptors (alpha, beta/delta, gamma) by perfluorooctanoic acid and perfluorooctane sulfonate. Toxicol Sci 95:108–117. doi:10.1093/toxsci/kfl135
Vanden Heuvel JP, Thompson JT, Frame SR, Gillies PJ (2006) Differential activation of nuclear receptors by perfluorinated fatty acid analogs and natural fatty acids: a comparison of human, mouse, and rat peroxisome proliferator-activated receptor-alpha, -beta, and -gamma, liver X receptor-beta, and retinoid X rec. Toxicol Sci 92:476–489. doi:10.1093/toxsci/kfl014
Wang I-J, Hsieh W-S, Chen C-Y, Fletcher T, Lien G-W et al (2011) The effect of prenatal perfluorinated chemicals exposures on pediatric atopy. Environ Res 111:785–791
White KL, Sheth CM, Peachee VL (2007) Comparison of primary immune responses to SRBC and KLH in rodents. J Immunotoxicol 4:153–158. doi:10.1080/15476910701337688
Yang Q, Abedi-Valugerdi M, Xie Y, Zhao X-Y, Möller G et al (2002) Potent suppression of the adaptive immune response in mice upon dietary exposure to the potent peroxisome proliferator, perfluorooctanoic acid. Int Immunopharmacol 2:389–397
Zhang YH, Wang J, Dong GH, Liu MM, Wang D, Zheng L, Jin YH (2013) Mechanism of perfluorooctanesulfonate (PFOS)-induced apoptosis in the immunocyte. J Immunotoxicol 10(1):49–58
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Keil, D.E. (2015). Immunotoxicity of Perfluoroalkylated Compounds. In: DeWitt, J. (eds) Toxicological Effects of Perfluoroalkyl and Polyfluoroalkyl Substances. Molecular and Integrative Toxicology. Humana Press, Cham. https://doi.org/10.1007/978-3-319-15518-0_10
Download citation
DOI: https://doi.org/10.1007/978-3-319-15518-0_10
Publisher Name: Humana Press, Cham
Print ISBN: 978-3-319-15517-3
Online ISBN: 978-3-319-15518-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)