Abstract
From metabolic disorders, osteoporosis is found in ochronotic arthropathy of the spine and large joints of the extremities. It is assumed that it is the secondary form of osteoporosis caused by immobilisation of severely affected individuals. Babel et al. (1960) presented a family affected by alkaptonuria, phenylketonuria and congenital cataract. Alkaptonuria sporadically occurs in coincidence with psoriasis. In 1955, we had the opportunity to present unique coincidence of alkaptonuric ochronosis and ankylosing spondylitis in a 51-year-old male patient (Urbánek and Siťaj 1955). Our patient came from the family in which 4 out of 5 siblings had ochronotic arthropathy. On the basis of analysis of clinical and X-ray findings in the area of spine, it could be anticipated that ochronotic arthropathy and AS mutually interact. Our patient had typical ochronotic changes, especially the calcifications of intervertebral discs less pronounced than other patients in the same stage of the disease. Premature rigidity of the spine caused by AS probably prevented development of ochronotic changes expected at his age. On the other hand, in spite of classical AS signs (indistinct sacroiliac joints, ossification of paraspinal ligaments, obliteration of intervertebral joints), the patient experienced inadequately mild pain in the whole course of the disease. The results from our long-term observation of a large group of patients reveal that relatively mild pain is typical for ochronotic arthropathy.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
From metabolic disorders, osteoporosis is found in ochronotic arthropathy of the spine and large joints of the extremities. It is assumed that it is the secondary form of osteoporosis caused by immobilisation of severely affected individuals. Babel et al. (1960) presented a family affected by alkaptonuria, phenylketonuria and congenital cataract. Alkaptonuria sporadically occurs in coincidence with psoriasis. In 1955, we had the opportunity to present unique coincidence of alkaptonuric ochronosis and ankylosing spondylitis in a 51-year-old male patient (Urbánek and Siťaj 1955). Our patient came from the family in which 4 out of 5 siblings had ochronotic arthropathy. On the basis of analysis of clinical and X-ray findings in the area of spine, it could be anticipated that ochronotic arthropathy and AS mutually interact. Our patient had typical ochronotic changes, especially the calcifications of intervertebral discs less pronounced than other patients in the same stage of the disease. Premature rigidity of the spine caused by AS probably prevented development of ochronotic changes expected at his age. On the other hand, in spite of classical AS signs (indistinct sacroiliac joints, ossification of paraspinal ligaments, obliteration of intervertebral joints), the patient experienced inadequately mild pain in the whole course of the disease. The results from our long-term observation of a large group of patients reveal that relatively mild pain is typical for ochronotic arthropathy.
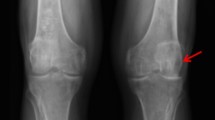
Ochronotic arthropathy is a disease associated with degenerative changes in the spine manifested with severe pain in the spine and large joints such as the shoulder, hip and knee joints.
Lumbar and thoracic spine is most frequently affected. Medical finding: significant stiffness of the spine and reduced spine mobility may resemble symptoms present in ankylosing spondylitis. However, X-ray findings are different and typical for each disease. Acute exacerbation of ochronotic arthropathy may clinically resemble rheumatoid arthritis.
The scientific literature describes the coexistence of ochronosis and rheumatoid arthritis or ochronosis and ankylosing spondylitis in 2.4/1,000 and 0.5/1,000 cases, respectively (Ball 1989).
FormalPara Male patient, born in 1937Karimzadeh et al. (2009) described the case of a 72-year-old patient whose medical history included an attack of arthritis urica 20 years ago caused by a dietary mistake which was relieved after 7–10 days. Now he has been hospitalised due to pain, swelling and redness of DIP and PIP joints of both hands and due to the presence of white material from a tumorous object on the third and forth finger of the hand. Objective examination was accompanied by pain in the hand joints and spine limited mobility of the shoulder and knee joints, hip joints and lumbar spine, redness and swelling and limited mobility of DIP joints. The examination also revealed bluish black pigmentation of the sclera, auricles and hands.
Urine had a normal colour, but after being left in the light for 30 min, the colour changed to black. Laboratory examinations showed hyperuricaemia. Examination of the white matter obtained from the fingers in depolarizing microscope revealed typical microcrystals of monosodium urate monohydrate. Hand X-ray revealed erosions with sclerotic changes. The lumbar spine contained signs of late stage ochronosis: calcifications and ossifications of intervertebral discs, narrowing of intervertebral space with a vacuum phenomenon and osteoporosis. The treatment included 30 mg of prednisolone daily and after improvement of arthritis 100 mg of allopurinol daily.
The patient showed characteristic radiographic signs of chronic arthritis urica, increase in uric acid in the serum and the presence of tophi. There were also pigmentations on the skin, auricle, sclera, as well as radiographic signs of ochronosis. The presence of uric acid arthropathy is not common in the case of alkaptonuria and ochronosis; nevertheless, this patient fulfilled the diagnostic criteria of both diseases.
FormalPara Male patient, 54 years oldThe clinical picture of ochronotic spondylosis and arthropathy sometimes resembles ankylosing spondylitis. Peric et al. (2007) described a case study of a 54-year-old patient. In 1999 he was examined due to pain in the right knee, lumbar spine and left heel. He had experienced lumbago and the sensation of spine stiffness, more pronounced after exercising, for 20 years. Gradually, the pain became permanent and was accompanied by knee arthritis and knee and Achilles tendon enthesopathy.
The family history did not include ankylosing spondylitis, ochronosis, seronegative spondyloarthropathy or inflammatory bowel disease, uveitis, conjunctivitis, iridocyclitis, psoriasis or urethritis. In 2000 he developed knee and shoulder joint arthritis; Achilles tendon was affected as well. Objective examination described brown-black pigmentations on auricles, nose cartilage and the sclera. There was also dorsal kyphosis, head and neck protrusion, significant limitation of spine mobility in all directions (Schober 0 cm), decreased scope of mobility and pain of the shoulder joints and hip joints, knee synovitis, left ankle arthritis and tendinitis of Achilles tendon.
Erythrocyte sedimentation rate was 10 mm/h, CRP 8 mg/L (normal level up to 6). Antigen HLA B27 positivity was revealed in laboratory examinations. The concentration of homogentisic acid in the urine was severalfold increased. Urine examination revealed its dark colouration.
X-ray documentation contained a description of quadratisation of thoracolumbar vertebrae, marginal syndesmophytes from Th10 to LI, intervertebral space narrowing, accentuation of thoracic kyphosis, lumbar lordosis reduction, numerous calcifications in the area of intervertebral discs and disc vacuum phenomenon.
MRI revealed erosive inflammatory changes in SI joints – second-grade sacroiliitis, narrowing of joint space in hip joints, subchondral sclerosis and enthesopathic changes in greater trochanters.
The patient has ochronosis with typical clinical and radiological findings and positivity of increased amount of homogentisic acid in urine. Moreover, he meets the New York criteria for ankylosing spondylitis.
FormalPara Female patient, born in 1952Balaban et al. (2006) observed a 54-year-old woman with a seronegative spondyloarthropathy. Family history did not include any metabolic disease, diabetes mellitus, hypertension, ulcerative colitis, acute frontal uveitis, trauma and genetic or hereditary disease. For 2 years, the patient suffered from pain and reduced mobility of the lumbar spine. With time, night pain appeared.
Objective examination described black pigmentation in the area of the auricles and on the hands, face, sclera and nails. Arthrological examination revealed strong thoracic kyphosis, loss of lumbar lordosis and flexion in hip and knee joints. The clinical finding resembled ankylosing spondylitis. Pain was also present, as well as reduced scope of shoulder joint mobility and reduction of thorax expansion to 2 cm. Laboratory results revealed higher erythrocyte sedimentation rate and CRP. HLA B27, rheumatoid factor, were not present.
X-ray showed intervertebral disc calcifications as in the case of ochronotic arthropathy. Due to persistent pain in SI joints, a MRI examination was also performed, showing erosive changes associated with bilateral sacroiliitis. The condition was evaluated as the coexistence of ochronotic arthropathy and second-grade sacroiliitis.
FormalPara Female patient, born in 1930Kihara et al. (1994) described the case of a 64-year-old female patient whose parents were related, and the mother, grandmother and brother suffered from rheumatoid arthritis. In 1992, the patient started to experience increased pain in their shoulders, left knee and LS spine and pain associated with arthritis of the wrists and small joints of the hands.
Objective examination revealed bilateral brown pigmentation of the sclera, bluish black colouration of the auricle, arthritis of wrists, MTP and PIP joints. Laboratory results showed rheumatoid factor positivity (273 IU/ml) in synovial fluid and positive dark colour of urine in the light.
X-ray showed bone bridging and osteosclerosis of the spine, narrowing of intervertebral space from Thl2 to L2, marginal osteophytes and small erosions in the shoulder and knee joints, osteopaenia and narrowing of the wrist joints. Diagnosis of alkaptonuria and ochronosis with increased secretion of homogentisic acid and pigmentation on the sclera and auricles was confirmed in this patient. Generally ochronotic arthropathic changes are more frequent in large joints and the spine, and the small hand joints remain unaffected. The patient with symmetric arthritis of hand joints, X-ray changes and the presence of the rheumatoid factor fulfilled the diagnostic criteria for the development of rheumatoid arthritis. The described case was confirmed as the coexistence of ochronosis and rheumatoid arthritis.
Recently, we also presented the case of a 50-year-old woman with coincidence of ochronosis and RA with considerable clinical activity and rapid progression of destructive changes on hip and knee joints (Rovenský et al. 2000).
References
Babel, J., Bamatter, F., Courvoisier, B., Franceschetti, A., Klein, D., Lapiné, A.: Familial amino acid metabolic disorders (alkaptonuria, phenylpyruvic oligophrenia, congenital cataract in the same family). Schweiz. Med. Wochenschr. 90, 863–866 (1960)
Balaban, B., Taskaynatan, M., Yasar, E., Tan, K., Kalyon, T.: Ochronotic spondylarthropathy: spinal involvement resembling ankylosing spondylitis. Clin. Rheumatol. 25, 598–601 (2006)
Ball, G.V.: Ankylosing spondylitis. In: McCarty, D.J. (ed.) Arthritis and Allied Condition. A Textbook of Rheumatology, 11th edn, pp. 934–943. Lea & Febiger, Philadelphia (1989)
Karimzadeh, H., Mohtasham, N., Karimfar, M., Salesi, M., Bonakdar, Z.S.: A case of ochronosis with gout and Monckeberg arteries. Rheumatol. Int. 29, 1507–1510 (2009)
Kihara, T., Yasuda, M., Watanabe, H., Suenaga, Y., Shiokawa, S., Wada, T., Nonaka, S., Suzuki, T., Nobunaga, M.: Coexistence of ochronosis and rheumatoid arthritis. Clin. Rheumatol. 13, 135–138 (1994)
Peric, P., Curkovic, B., Potocki, K., Babic-Naglic, D., Perie, S., Cerovski, B., Kehler, T., Vidovic, T.: Coexistence of ochronosis and B 27 positive ankylosing spondylitis. Coll. Antropol. 31, 637–640 (2007)
Rovenský, J., Letkovská, A., Schumacher, H.R., Urbánek, T., Bošák, V.: Coexistence of ochronosis and rheumatoid arthritis: a cause of delay in diagnosis and treatment. J. Clin. Rheumatol. 6, 214–217 (2000)
Urbánek, T., Siťaj, Š.: Simultaneous occurrence of alkaptonuria, ochronotic arthropathy and Bechterews disease. Fysiatr. Vestn. Cesk. Fysiatr. Spol. 33, 85–91 (1955)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Rovenský, J., Lukáčová, O. (2015). Coincidence of Alkaptonuric Ochronosis with Other Diseases. In: Rovenský, J., Urbánek, T., Oľga, B., Gallagher, J. (eds) Alkaptonuria and Ochronosis. Springer, Cham. https://doi.org/10.1007/978-3-319-15108-3_23
Download citation
DOI: https://doi.org/10.1007/978-3-319-15108-3_23
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-15107-6
Online ISBN: 978-3-319-15108-3
eBook Packages: MedicineMedicine (R0)