Abstract
Epithelial cells form organized structures such as tubes and alveoli, the organization of which is controlled by conserved complexes of polarity proteins. Mammary gland development requires extensive epithelial remodeling coordinated with proliferation and apoptosis to generate the highly branched epithelial ductal network that extends into a complex fatty stroma. Mammary epithelial cells dynamically regulate cell polarity during branching morphogenesis, and therefore the mammary gland represents a unique model to understand epithelial remodeling during normal development. Moreover, the mammary gland undergoes extensive remodeling during the progression of breast cancer, which is associated with a loss of apical-basal polarity and epithelial organization. In this chapter, we present the mammary gland as a model to understand unique roles for polarity proteins in epithelial remodeling. We also discuss novel signaling pathways regulated by polarity proteins that function in normal mammary gland development, as well as breast cancer initiation, invasion, and metastasis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Overview of Mammary Gland Development
The mammary gland consists of a treelike structure of epithelial ducts embedded in a complex stroma, consisting of fat cells, fibroblasts, and immune cells (Fig. 8.1) (Sternlicht 2006). The ducts are formed from an epithelial bilayer: an inner luminal layer that lines the ductal cavity and an outer myoepithelial layer that contacts the basement membrane. Although these two major cell types are both epithelial, their organization and functions are quite distinct; luminal cells are polarized cuboidal epithelial cells with distinct apical and basolateral domains (apical-basal polarity) that are separated by tight junctions (Fig. 8.1). These cells form E-cadherin-based adherens junctions that maintain ductal integrity. Luminal epithelial cells are also characterized by the expression of intermediate filament cytokeratins 8/18 (CK8/18), whereas myoepithelial cells express distinct cytoskeletal markers, including cytokeratin 5 and 14 (CK5 and CK14), as well as α-smooth muscle actin (α-SMA) (Williams and Daniel 1983). Myoepithelial cells do not contact the lumen but instead interact with the basement membrane through integrins. Furthermore, myoepithelial cells form cell-cell adhesions through P-cadherin, but do not form tight junctions (Chanson et al. 2011); therefore, they do not exhibit apical-basal polarity (Fig. 8.1).
Overview of the mammary gland. Diagram of a bilayered mammary duct with inner luminal epithelial cells and outer myoepithelial cells. The terminal end bud is multilayered with microlumen (arrows) and is covered by a cap cell layer that contains mammary stem cells. Components of the mammary stroma include adipocytes, immune cells, and fibroblast. An enlarged region of a duct shows the location of polarity and adhesion complexes in luminal epithelial cells with apical-basal polarity
The mammary gland is a unique epithelial tissue since most of the development occurs after birth. At mid-gestation, the murine mammary epithelium arises from the ectoderm to form a mammary bud, which undergoes limited growth and branching to form a rudimentary tree in the embryo (Sternlicht 2006). After birth the mammary gland grows isometrically with the animal; then at puberty, changes in circulating hormones initiate a program of enhanced growth and branching of the mammary epithelium (Sternlicht et al. 2006).
In the mouse, pubertal mammary morphogenesis initiates with the formation of bulbous epithelial structures at the distal tips of growing ducts, termed terminal end buds (Fig. 8.1). End buds are multilayered and highly dynamic structures, with higher rates of both proliferation and apoptosis compared to the subtending ducts (Hinck and Silberstein 2005; McCaffrey and Macara 2009; Ball 1998). High proliferation likely generates the increased cell numbers necessary for growing the duct, and apoptosis is necessary for clearing the central lumen (Mailleux et al. 2007; Parsa et al. 2008). The leading outermost layer of the end bud consists of cap cells, which are enriched in stem cell activity during mammary gland development (Bai and Rohrschneider 2010; Kenney et al. 2001). At pregnancy, the mammary epithelium again undergoes extensive proliferation, branching, and differentiation into milk-producing alveolar structures (Oakes et al. 2008). After lactation is complete, an apoptotic program eliminates the bulk of alveolar cells, and the mammary gland returns to a state that is highly reminiscent of the virgin gland before pregnancy (Stein et al. 2007). Therefore, the mammary gland represents a highly dynamic epithelium for which to understand the role of cell polarity proteins during epithelial morphogenesis.
2 Mammary Epithelial Models for Studying Morphogenesis and Polarity
Polarity proteins have a wide range of biological effects across numerous species and tissue types, and remarkably, the same proteins can have distinct functions in different tissues or at different developmental stages within the same tissue (Thompson 2012; Tepass 2012; McCaffrey and Macara 2012; Nance and Zallen 2011; Martin-Belmonte and Perez-Moreno 2011). This highlights the fact that polarity proteins have multifaceted and complex interactions with numerous pathways that impinge on biological processes like survival, proliferation, apoptosis, and differentiation. Not surprisingly then, different experimental models used to evaluate polarity protein function may reveal different roles for those proteins. For example, while 2D cultures may capture some aspects of basic polarized cell biology, 3D cultures more closely model the in vivo environment (McCaffrey and Macara 2011; Page et al. 2012; Weaver et al. 2002). In addition, organotypic cultures that contain multiple cell types can reveal more complex signaling that occurs between different cell types (Ridky et al. 2010; Macias et al. 2011), and in vivo models can yield further insights into complex regulatory mechanisms such as stem cell renewal and differentiation, as well as tumorigenesis and metastasis (Shackleton et al. 2006; Cardiff et al. 2000).
The mammary gland represents an excellent system for understanding various aspects of polarity protein function with culture models that range from simple cell lines that are relatively easily maintained to more complex cultures of primary cells and organotypic cultures, which requires more expertise. For example, mouse mammary gland cell lines (e.g., NMuMG, EpH4) are capable of forming polarized cysts when cultured in 3D extracellular matrix (Hall et al. 1982; Niemann et al. 1998; Viloria-Petit et al. 2009). Human breast cells are also capable of forming cysts when cultured in 3D matrix. A commonly used human mammary cell is the immortalized, but non-transformed, MCF10A cell line, which were derived from a fibrocystic breast patient (Debnath et al. 2003; Dow et al. 2007; Whyte et al. 2010). These cells express some luminal markers and are polarized in the sense that they form a central lumen and orient the Golgi apically between the nucleus and lumen; however, the apical determinant Crb3 is suppressed in these cells, and they do not form an apical membrane or functional tight junctions (Fogg et al. 2005). Therefore, MCF10A cells lack complete apical-basal polarity, which needs to be considered with interpreting polarity data obtained from these cells.
Another source for human mammary epithelial cells (HMECs) are primary cells isolated from breast reduction surgery (Lindley and Briegel 2010; Stampfer and Bartley 1988). A limitation of primary HMECs is that they have a limited life in culture; however this has been overcome by the generation of numerous immortalized and transformed derivatives (Yaswen and Stampfer 2001; Dimri et al. 2005). An advantage of primary mammary cells from mice or humans is that they can be cultured as “organoids,” which are isolated from mammary glands as multicellular clusters and then embedded and grown in 3D extracellular matrix gels (Fig. 8.2). These are distinct from 3D cultures of cell lines in that they contain both luminal and myoepithelial cell types, with a bilayer organization that resembles the mammary gland in vivo (Pasic et al. 2011; Ewald et al. 2008; Macias et al. 2011). Remarkably, organoids undergo dynamic remodeling of polarity during lumen formation and branching morphogenesis in response to growth factor stimuli (Fig. 8.2) and therefore represent an excellent model for understanding epithelial morphogenesis in vitro (Akhtar and Streuli 2013; Ewald et al. 2008).
Mouse and human primary mammary epithelial cells can also be cultured in at low density as suspension cultures to enrich stem and progenitor cells. Under these conditions, differentiated cells die by anoikis, whereas stem and progenitor cells survive and grow into balls of cells called mammospheres (Dontu et al. 2004). Mammospheres contain differentiated cells, as well as a stem cell population that is maintained by asymmetric cell divisions and enables mammospheres to be sustained following serial passages (Cicalese et al. 2009).
Finally, in vivo mouse models are another important tool for understanding gene function in the mammary gland, particularly for understanding stem cell and tumorigenic functions. Several mammary gland-specific promoters are available to selectively express or knock out genes in the mammary epithelium. Commonly used promoters include the mouse mammary tumor virus long terminal repeat (MMTV), the whey acidic protein (WAP), and β-lactoglobulin (BLG) promoters, which predominantly target luminal epithelial cells (Borowsky 2011). In addition, the keratin 14 or keratin 5 promoters can be used to target myoepithelial cells (Van Keymeulen et al. 2011; Taddei et al. 2008); however, the keratin 14 promoter is active in stem cells during mammary embryogenesis, which results in expression in all mammary cell types (Van Keymeulen et al. 2011).
The ability to transplant mouse mammary gland stem cells into the mammary fat pad to regenerate the ductal epithelium is another useful tool for studying polarity in mammary morphogenesis (Deome et al. 1959; Daniel et al. 1968; Shackleton et al. 2006; Stingl et al. 2006). Mammary stem cells isolated from a donor are injected into the mammary fat pad of a prepubertal recipient mouse that has had the ductal epithelium removed surgically. Lentivirus can be used to express cDNA or shRNA in stem cells to study gene function, and when coupled with transplants, this represents a rapid and cost-effective alternative to generating transgenic and knockout mice (McCaffrey and Macara 2009).
3 Cell Polarity and Branching Morphogenesis
During pubertal development, the mammary epithelium undergoes dynamic changes in apical-basal polarity, particularly in the end bud. The terminal end bud is comprised of a mixture of polarized and non-polarized luminal epithelial cells; the polarized cells contact the developing central lumen, as well as microlumen, which may coalesce to form the primary lumen in subtending ducts and are surrounded by non-polarized cells (Fig. 8.1) (Ewald et al. 2012). For instance, whereas aPKCζ is usually localized to the apical membrane in polarized cells, it localizes with β-catenin, Scrib, and Numb at all cell membranes in non-polarized interior cells, and Par3 appears diffusely localized in the cytoplasm (Ewald et al. 2008; Ewald et al. 2012). As such, terminal end buds show characteristics of neoplastic hyperplasia, including a partial loss of apical-basal polarity and loosened cell-cell interactions. However, there is no invasion of these inner end bud cells into the highly organized extracellular matrix during ductal growth (Ewald et al. 2008).
Cellular and molecular mechanisms underlying branching morphogenesis have been investigated using 3D organotypic cultures (Fig. 8.2). In response to growth factors secreted by myoepithelial cells, luminal cells remodel to become multilayered, and then a process of collective migration pushes cells forward to initiate branching (Ewald et al. 2008). Surprisingly, unlike some branched tissues like the Drosophila airway epithelium, collective movements during mammary branching do not have leader cells; instead, cells rearrange in a seemingly random order and in the absence of leading actin-rich protrusions (Ewald et al. 2008; Ewald et al. 2012). Diverse molecular pathways are involved in the control of mammary gland morphogenesis. For instance, Rac1 and MLCK activities are required for branching initiation, whereas ROCK is necessary to restore the bilayered epithelial architecture once branching has ceased (Ewald et al. 2008). Furthermore, the interaction between β1-integrins and laminin provides traction to the end buds and facilitates duct elongation (Klinowska et al. 1999). Association of β1-integrin with the basement membrane is also necessary for the establishment of apical-basal polarity in luminal cells and lumen formation (Akhtar and Streuli 2013). In contrast to MDCK cells, where Rac1 activation is required for the orientation of apical polarity (O’Brien et al. 2001; Yu et al. 2005), in mammary glands the integrin-linked kinase (ILK) acts downstream of β1-integrin to polarize microtubules along the apical-basal axis, control internal cell polarity, and drive lumen formation (Akhtar and Streuli 2013). Additionally, alterations in the expression, localization, or activity of diverse polarity proteins, including Scrib, Par4 (Lkb1), Llgl (Hugl1/2), and the Par3/aPKC complex, are associated with impairments in ductal morphogenesis, although the molecular mechanisms involved are not known (McCaffrey and Macara 2009; Whyte et al. 2010; Russ et al. 2012; Zhan et al. 2008; Partanen et al. 2012a).
The dynamic nature of the mammary gland is also evident during pregnancy, when the mammary epithelium remodels into a milk-secreting tissue in response to hormonal regulation by prolactin. During lactation the prolactin receptor (PRLR) locates preferentially in the basal membrane, where it activates a JAK2/STAT5 cascade that promotes proliferation and differentiation of milk-producing alveolar cells (Morales et al. 2012). The polarized distribution of PRLR to the basal membrane is dependent on NHERF1, a polarity scaffold that directly interacts with PRLR, as well as other proteins including Ezrin, and β-catenin. Interestingly, NHERF1 is localized to the apical membrane in luminal epithelial cell of mature virgin mammary ducts, but then undergoes a dynamic repositioning to the basal membrane during lactation, which is necessary for proper PRLR localization, alveolar differentiation, and milk production (Fig. 8.3b) (Morales et al. 2012; Stemmer-Rachamimov et al. 2001). Moreover, the interaction of mammary cells with the extracellular matrix is key for proper alveologenesis, since β1-integrin ablation prevents prolactin-induced differentiation of luminal epithelia due to defective STAT5 activation (Naylor et al. 2005). Together these studies highlight the importance of apical-basal polarity in positioning signaling modules, which is essential for hormonally regulated cell differentiation.
Lineage specification in the mammary gland. (a) The mammary gland is hierarchally organized with mammary stem cells, bipotent progenitors, unipotent progenitors, and differentiated luminal and myoepithelial cells. Stem cells asymmetrically position Numb during divisions, which is dependent on p53. (b) Reorganization of a NHERF/Ezrin complex from the apical domain to the basal domain occurs during pregnancy. Basal NHERF/Ezrin positions the prolactin receptor basally, which is necessary for Stat5 activation and differentiation of milk-producing cells
4 Stem Cells and Mammary Gland Development
The mammary gland exhibits plasticity and grows extensively during puberty but also can cycle through multiple rounds of expansion and involution during pregnancy. Furthermore, transplantation of a single mammary epithelial cell into a cleared fat pad can regenerate the entire mammary ductal tree, indicating the presence of mammary stem cells (MaSC) with tremendous regenerative capability (Shackleton et al. 2006). The terminal end bud is a reservoir during development for active stem cells, which reside in a cap cell layer, the outermost layer of the end bud (Fig. 8.1) (Bai and Rohrschneider 2010). Furthermore, terminal end buds contain bipotent progenitor cells that express both luminal and myoepithelial markers, indicating that the terminal end bud may also represent a stem cell niche that regulates stem and progenitor cell differentiation (Kenney et al. 2001; McCaffrey and Macara 2009). This is in part regulated by Par3 since the depletion of Par3 from the mammary epithelium results in enlarged terminal end buds with an expanded pool of bipotent progenitors that are defective in differentiation and the ability to reorganizing into mature ducts (McCaffrey and Macara 2009).
Different cell surface markers have been used to isolate MaSC and lineage committed progenitors from the mammary gland [for a detailed review, see (Visvader 2009)]. At present there is no consensus whether a common progenitor can differentiate into all mature mammary epithelial cell lineages or if two different lineage-restricted precursor cells (luminal/alveolar and myoepithelial) are required during mammary tree expansion (Shackleton et al. 2006; Van Keymeulen et al. 2011). A unified hypothesis (Fig. 8.3a) suggests that unipotent progenitor cells are responsible of normal tissue maintenance and remodeling, while pluripotent cells participate in embryonic development or can be activated under certain circumstances (such as transplantation or tissue regeneration) to give rise to both luminal and myoepithelial lineages (Keller et al. 2011; Visvader and Lindeman 2011).
Regardless of the origin of the stem and progenitor cells, asymmetric cell divisions are necessary to establish the luminal and myoepithelial lineages while maintaining the pool of MaSCs (Fig. 8.3a) (Cicalese et al. 2009). Mammosphere assays show that p53 expression is required for asymmetric Numb segregation, via an unknown mechanism (Cicalese et al. 2009). This may involve the Par complex because in other cell types, aPKC and Par3 interact with Numb and aPKC directly phosphorylates Numb to control polarized distribution (Smith et al. 2007; Nishimura and Kaibuchi 2007). Asymmetric Numb may be important for mammary cell fate decisions; Numb is a negative regulator of Notch signaling, and Notch is involved in specifying luminal progenitors and the luminal cell fate (Pece et al. 2004; Gönczy 2008). In turn, Numb regulates p53 ubiquitination and degradation (Colaluca et al. 2008), creating then a feedback loop that might restrict the stem cell fate to only one of the daughter cells. Segregation of cell fate determinants and asymmetric cell division require establishment of a polarity axis (in response to external clues, such interaction between cellular integrins and ECM), in conjunction with cell polarization. In this sense, deletion of β1-integrin expression (Taddei et al. 2008) or alterations in the function of polarity proteins (Cdc42, Par3, aPKC, Pins/LGN) in mammary epithelial cells is associated with defects in mitotic spindle orientation or progenitor differentiation (Bray et al. 2011; McCaffrey and Macara 2009; Hao et al. 2010; Jaffe et al. 2008; Zheng et al. 2010).
5 Overview of Breast Cancer
Breast cancer is the most common cancer among women (Parkin et al. 1999). It progresses in a stepwise fashion through multiple stages including flat epithelial atypia (FAE), atypical ductal hyperplasia (ADH), ductal carcinoma in situ (DCIS), and invasive ductal carcinoma (IDC) (Bombonati and Sgroi 2011). FAE is considered a benign lesion and is characterized by ducts with nonuniform diameters, lined by single or multilayered epithelial cells (Schnitt 2003). The cells adjacent to the lumen retain at least some aspects of apical-basal polarity, whereas cells in the underlying layers do not contact the lumen and therefore lack apical-basal polarity. Whereas ADH are small hyperplastic lesions that still retain some ductal structures, DCIS are larger and are characterized by uniform proliferative pre-malignant cells that have not invaded across the basement membrane (Ellis 2010; Zagouri et al. 2007). Up to 50 % of patients with DCIS will develop IDC, in which the carcinoma breaches the basement membrane. Therefore, mammary ductal and cellular organization changes throughout breast cancer progression, and loss of apical-basal polarity can occur at the earliest stages.
There are multiple breast cancer subtypes, which can be grouped based on the presence or absence of molecular markers and have distinct clinical outcomes. Luminal A breast cancers express markers of luminal epithelial cells, are estrogen receptor positive, and have the best prognosis (Rakha et al. 2008). Luminal B also express markers of luminal epithelial cells; however, they have reduced expression of genes associated with estrogen receptor signaling and have a poorer prognosis. HER2 breast cancers have amplified expression of the ErbB2 receptor tyrosine kinase and represent a poor prognosis subtype. Finally, triple-negative/basal-like breast cancers have the poorest prognosis and are negative for estrogen receptor, progesterone receptor, and ErbB2, but express markers of basal myoepithelial cells (Rakha et al. 2008). More recently, genome-wide expression profiling of breast cancers has led to a more refined classification system and the identification of an additional triple-negative cancer subtype called claudin low, which exhibits low expression of luminal differentiation markers (like claudins) and high expression of basal/mesenchymal and stem cell markers (Prat et al. 2010). Interestingly, the gene expression profile of the different breast cancer subtypes has a striking resemblance to expression profiles of cells along the stem/progenitor/differentiated cell spectrum, and it has been proposed that the cell of origin for the different breast cancer subtypes arises from distinct stem, progenitor, and differentiated cell populations (Visvader 2009). Strikingly, over 95 % of basal-like breast cancers have altered expression of at least one core component of the Crbs/Pals1/Patj, Par3/Par6/aPKC, or Scrib/Llgl/Dlg complexes, whereas they are disrupted in only 65 % of luminal A/B and 79 % of Her2-enriched tumors (TCGA 2012). Therefore, although the role of cell polarity proteins are best understood in luminal epithelial cells, we expect that they may have distinct functions in basal or stem cells, and therefore the functions of polarity proteins may be different depending on the cancer subtype.
6 Cell Polarity and Breast Cancer Progression
Cell polarity genes are essential regulators of epithelial organization that also function in growth control (Fig. 8.4). Furthermore, in some cases, loss of a polarity protein is sufficient for the development of benign or malignant lesions, indicating that they can function as tumor suppressors. For example, when Scrib is depleted from Comma-D cells (a mouse mammary cell line) and then transplanted orthotopically into the mammary fat pad, the glands exhibit epithelial overgrowth with solid ducts that lack a central lumen (Zhan et al. 2008). This effect is, at least in part, due to fact that loss of Scrib protects cells from apoptosis (Zhan et al. 2008). Interestingly, 10 % of the Scrib-depleted mammary glands form palpable tumors with a well-differentiated glandular phenotype (Zhan et al. 2008). Given the low penetrance and long latency, cooperating events are likely necessary for tumor formation in Scrib-depleted glands.
Regulation of breast cancer progression by polarity proteins. Polarity proteins regulate diverse cellular processes of apoptosis, proliferation, cell junction remodeling, extracellular matrix (ECM) remodeling, and epithelial-mesenchymal transition (EMT). Each of these processes impinges on various stages of breast cancer progression from loss of epithelial organization and growth control, through invasion and metastasis. The dashed line represents that Scrib, Dlg, AF-6, and Patj regulate invasion through an undefined process. The dotted line signifies that Lkb1 regulates ECM remodeling, although it is not known whether this affects invasion and metastasis
The disruption of other polarity proteins can also induce early stages of tumor progression. When primary mouse mammary epithelial cells are depleted of the apical scaffold Par3 and transplanted orthotopically, the resulting ducts are dilated and multilayered, a phenotype that is reminiscent of the early stages of human breast cancers (McCaffrey and Macara 2009). Moreover, Par3-depleted ducts are significantly more proliferative than control ducts; however, they also have increased apoptosis, which offsets hyper-proliferation and limits tumor progression since palpable tumors are not observed (McCaffrey and Macara 2009; McCaffrey et al. 2012). These examples demonstrate that polarity proteins play a critical role in maintaining the ductal epithelium, and their loss can trigger early stages of cancer formation.
Given the low penetrance and long latency of tumors from Scrib-deficient cells, and the lack of palpable tumor formation in Par3-depleted mammary glands, it is likely that disrupted cell polarity cooperates with other events to promote tumorigenesis. For example, expression of Myc in the mammary gland is weakly tumorigenic, partly because Myc expression induces apoptosis through a pathway involving the GTPase Rac1, Jun N-terminal kinase (JNK), c-Jun, and the proapoptotic protein Bim (Amundadottir et al. 1995; Zhan et al. 2008). Activation of this apoptotic pathway depends on the scaffold Scrib, and when Scrib is lost, Myc-induced apoptosis is short circuited enabling the formation of larger tumors (Zhan et al. 2008). Remarkably, mislocalization of Scrib is also able to enhance Myc-induced tumorigenesis (Zhan et al. 2008), supporting the view that polarity protein function can be disrupted by changes in expression or by changes in subcellular localization.
Disrupting other polarity proteins can also cooperate with Myc to promote mammary tumorigenesis. Homozygous deletion of Lkb1 (also called Par4) from the mammary epithelium dramatically reduces tumor latency and increases both the number and size of tumors, compared to Myc alone (Partanen et al. 2012b). Interestingly, mice with heterozygous expression of Lkb1 have an intermediate effect, indicating that even partial loss of Lkb1 expression sensitizes mice to Myc-induced tumors (Partanen et al. 2012b). However, unlike Scrib, loss of Lkb1 does not suppress Myc-induced apoptosis, indicating that polarity proteins can have diverse mechanisms in promoting Myc-driven tumors (Fig. 8.4). Instead, loss of Lkb1 leads to disrupted apical-basal polarity and cell junction defects, which caused mislocalization of the serine protease hepsin away from cell borders and compromised basement membrane organization (Lutzner et al. 2012). Importantly, low levels of Lkb1 correlate with elevated cytoplasmic hepsin in human breast cancers (Lutzner et al. 2012), indicating that the effects of loss of Lkb1 may be a general effect, independent of oncogenic functions of Myc specifically.
Disruption of Par3 also promotes oncogene-induced tumorigenesis and further promotes invasion and metastasis. Expression of the intracellular domain of the Notch receptor (NICD) in the mammary epithelium induces nonmetastatic tumors that are slow growing and retain E-cadherin and ZO-1 staining at cell-cell junctions (Hu et al. 2006; McCaffrey et al. 2012). However, depletion of Par3 from NICD-expressing tumors drastically reduces tumor latency, increases tumor growth, and promotes lung metastasis (McCaffrey et al. 2012). Interestingly, depletion of Par3 from an ErbB2 breast cancer model also promotes invasion and metastasis but does not affect primary tumor growth (Xue et al. 2012). Therefore, the growth-promoting effects of loss of Par3 may be dependent on the tumor context and the underlying signaling pathways regulating growth of that tumor. A striking example of this is that loss of Par3 in skin papilloma actually has the opposite effect and reduces tumor growth (Iden et al. 2012).
In some contexts, polarity proteins may act as oncogenes to promote breast tumorigenesis. For example, Par6 is overexpressed in hyperplastic benign breast lesions, and overexpression of Par6 in MCF10A cells induces hyper-proliferation, which acts through the MAPK pathway and is dependent on Par6 binding to Cdc42 and aPKC (Nolan et al. 2008). In addition, aPKCι itself is overexpressed in breast cancers, and in this case, expression correlates with more advanced tumors (Kojima et al. 2008; Paget et al. 2011). Screening of human breast cancer cell lines identified several with high levels of aPKCι activation; knocking down aPKCι expression in these cell lines reduced tumor cell proliferation and induced markers of senescence, indicating that aPKCι overexpression may promote tumorigenesis by repressing senescence (Paget et al. 2011).
In addition to cooperating in parallel with oncogenes and tumor suppressors, polarity proteins can associate with oncogenes or tumor suppressors themselves to modulate tumor progression (Fig. 8.4). When bound to oncogenes, polarity proteins themselves may not act as classical oncogenes—where gain of function promotes tumorigenesis—but rather they function to enable oncogene-mediated tumor progression. For example, ErbB2 activation by induced dimerization promotes proliferation, inhibits apoptosis, and disrupts epithelial organization and apical-basal polarity (Aranda et al. 2006). Whereas Par6/aPKC has no role in ErbB2-mediated proliferation, they are necessary to both disrupt polarity and inhibit apoptosis. Interestingly, activated ErbB2 was shown to bind Par6/aPKC and displace Par3; therefore, activation of ErbB2 affects apical-basal polarity by disrupting the Par complex (Aranda et al. 2006). The contribution of the Par polarity complex in ErbB2-/Her2-positive breast cancers may occur at multiple levels. The 14-3-3σ tumor suppressor gene is frequently lost in ErbB2-amplified tumors, and genetic deletion of the 14-3-3σ locus in mice disrupts cell-cell junctions and apical-basal polarity and accelerates ErbB2-dependent tumor onset (Ling et al. 2010). Intriguingly, 14-3-3σ can bind Par3, and loss of 14-3-3σ mislocalizes Par3 from the plasma membrane (Ling et al. 2011; Ling et al. 2010), demonstrating another mechanism by which the Par complex can be disrupted in ErbB2 breast cancers.
7 Polarity and Epithelial-Mesenchymal Transitions (EMT) During Breast Cancer
Multiple mechanisms are employed by breast tumor cells to invade and disseminate from the primary tumor. At one end of the spectrum is collective migration, in which cells move as a group held together by cell-cell junctions. As described above, this is important for branching morphogenesis; however, collective invasion of groups of cells has also been observed in breast and other tumor cells (Friedl and Gilmour 2009; McCaffrey et al. 2012). At the other end of the spectrum is a single cell invasion, in which single cells can take various forms, such as amoeboid or mesenchymal, to invade through the extracellular matrix; interestingly, cells can dynamically change between invasion modes, demonstrating that invading cells exhibit remarkable plasticity (Friedl and Wolf 2009). Although invading cells have often, if not always, lost apical-basal polarity, they retain front-rear polarity, in which many apical-basal polarity proteins relocate to the leading edge to coordinate cytoskeletal remodeling (Godde et al. 2010).
Epithelial cells can be reprogrammed to become more mesenchymal, the so-called epithelial-mesenchymal transitions (EMT), which can promote a single cell mode of invasion. EMT is characterized by loss of E-cadherin and cell-cell junctions, loss of apical-basal polarity, and a switch in the expression of epithelial cytoskeletal cytokeratins to mesenchymal cytoskeletal proteins like vimentin (Thiery et al. 2009). Furthermore, EMT confers stem cell-like properties to mammary cells, such as self-renewal and survival in low adhesion conditions (Mani et al. 2008; Morel et al. 2008).
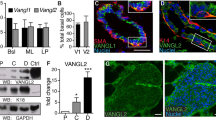
EMT reprogramming is primarily driven by three families of transcription factors, Zeb, Twist, and Snail, which target the polarity machinery (Thiery et al. 2009). For example, Zeb1 suppresses expression of Crumbs3, Lgl2, and Patj (Fig. 8.4) (Aigner et al. 2007; Russ et al. 2012). Knockdown of Lgl2 induces a spindly “mesenchymal” phenotype; however, whether they undergo EMT is not clear since the expression of EMT markers was not reported. However, re-expression of Lgl2 is able to suppress Snail-induced EMT (Russ et al. 2012). However, simultaneously knockdown of two polarity proteins does not induce expression of mesenchymal markers, despite cells becoming invasive (Fig. 8.4) (Chatterjee et al. 2012). Moreover, knockdown of Par3 can induce invasion and metastasis, all in the absence of EMT (McCaffrey et al. 2012; Xue et al. 2012). Collectively, this indicates that loss of apical-basal polarity may be necessary for EMT; however, silencing of apical-basal polarity proteins is not sufficient to induce an EMT phenotype. These data support a model in which disrupted apical-basal polarity can induce invasion through diverse mechanisms that are independent of a mesenchymal mode of invasion (Fig. 8.4).
8 Cell Polarity and Invasion and Metastasis and Cell Polarity
The vast majority of breast cancer-related deaths result from metastasis to distant organs. Metastatic progression is a multistep process involving local invasion, entry into the circulatory or lymphatic system, exit at distant sites, and finally survival and growth of disseminated tumor cells. Although classically thought of as a late stage in tumor progression, there is substantial evidence that dissemination may occur early in the progression of breast cancer (Hüsemann et al. 2008; Podsypanina et al. 2008).
There is substantial evidence that disrupted apical-basal polarity can alter cell invasion. Whereas knocking down apical-basal proteins Scrib, AF-6, Patj, and Dlg alone had little effect on invasion of MCF10A cells, depletion of two proteins from different polarity complexes was sufficient to induce invasion (Fig. 8.4) (Chatterjee et al. 2012). This suggests that apical-basal polarity acts through multiple mechanisms or that polarity complexes can act redundantly to suppress cell invasion. It may also depend on the polarity protein targeted and how they affect other polarity components. For example, Par3 is mislocalized in the mammary epithelium of Lkb1 knockout mice (Partanen et al. 2012b).
Interestingly, loss of a single polarity protein is sufficient to promote invasion when an oncogene is also present (Chatterjee et al. 2012; Dow et al. 2008). In MCF10A cells with activated ErbB2, loss of Scrib, Dlg, or AF-6 promoted invasion, which was dependent on the ability of ErbB2 to interact with Par6/aPKC, again suggesting that multiple hits to the polarity machinery are necessary for invasion (Chatterjee et al. 2012). The cooperation of polarity in oncogene-mediated invasion is not limited to ErbB2 cancers. Depletion of Scrib in MCF10A cells expressing an activated Ras oncogene also induces extensive invasion (Dow et al. 2008). In this system, Scrib normally functions to suppress Ras-induced invasion, by blocking Raf-MEK-ERK signaling downstream of Ras (Dow et al. 2008).
In some contexts, signaling through polarity proteins is required for invasion, and disruption polarity signaling actually blocks invasion. For example, TGFβ is a potent inducer of invasion, and when mouse mammary epithelial cells are treated with TGFβ, they undergo robust invasion in 3D cultures (Viloria-Petit et al. 2009). However, expressing a Par6 mutant that no longer interacts with the TGFβ receptor disrupts signaling, and TGFβ no longer stimulates invasion (Viloria-Petit et al. 2009). This dependency on Par6 for growth factor receptor-mediated invasion is consistent with results from cells with active ErbB2 receptor; however the mechanisms are distinct. In response to TGFβ, Par6 is recruited to the receptor and phosphorylated, which then recruits an E3 ubiquitin ligase, Smurf1 (Viloria-Petit et al. 2009). However, in response to ErbB2 activation, Par6 is recruited to the receptor, but invasion acts through an Akt-dependent mechanism (Chatterjee et al. 2012). This demonstrates that polarity proteins may cooperate with distinct oncogenic signals through different effector pathways, with a similar end result of enhanced invasion.
Of the polarity complexes, only the Par complex has yet been shown to directly promote breast cancer metastasis in vivo. In addition to being necessary for TGFβ-dependent invasion, Par6 is also necessary for lung metastasis. Expressing a mutant that cannot be phosphorylated by the TGFβ receptor in the mouse mammary tumor EMT-6 cells blocks Par6 signaling, and both the incidence of metastasis and the number of metastatic colonies in the lungs are markedly decreased (Viloria-Petit et al. 2009). Furthermore, Par3 is frequently downregulated in human breast cancer, which correlates with metastatic progression, and two studies report that loss of Par3 promotes breast cancer metastasis (McCaffrey et al. 2012; Xue et al. 2012). Although tumorigenic, expression of NICD alone in the mammary epithelium does not progress to metastatic disease (Hu et al. 2006; McCaffrey et al. 2012). However, depletion of Par3 induces both local invasion and metastasis to the lungs. Mechanistically, loss of Par3 induces robust activation of Jak2/Stat3 signaling, an important mediator of immune function and breast cancer metastasis (McCaffrey et al. 2012; Ranger et al. 2009). Importantly, Stat3 activation is necessary for metastasis in Par3-depleted cells, because inhibiting Stat3 signaling with pharmacological inhibitors or shRNA reduces invasion in vitro and metastasis in vivo. Transcriptional profiling revealed that loss of Par3 upregulated MMP9, which induced remodeling of the extracellular matrix to enable invasion. Loss of Par3 causes mislocalization and activation of aPKC, which is necessary for Jak/Stat3 activation. Notably, cell-cell adhesions are retained, and cells do not undergo an overt EMT to become invasive (Fig. 8.4) (Macara and McCaffrey 2013; McCaffrey et al. 2012). Similarly, loss of Par3 increases invasion and metastasis in an ErbB2 orthotopic transplant model (Xue et al. 2012). As has been reported previously, loss of Par3 induces global Rac1 activation by mislocalizing the Rac1 guanine nucleotide exchange factor Tiam1 (Chen and Macara 2005; Nishimura et al. 2005; Xue et al. 2012). Interestingly, altered Rac1 activity causes deregulated actin and E-cadherin dynamics at cell-cell junctions, thereby reducing cell cohesion and enabling invasion and metastasis (Xue et al. 2012). Furthermore, despite changes in E-cadherin dynamics, the cells do not show evidence of EMT (Xue et al. 2012). Therefore, loss of Par3 can cooperate with different oncogenes to induce metastasis, using complimentary mechanisms, but in the absence of EMT (Fig. 8.4).
9 Conclusions
Cell polarity is a dynamic event during epithelial morphogenesis and cancer progression in the mammary gland. A key function of apical-basal polarity proteins is to localize diverse signaling pathways at appropriate positions within cells to regulate cell proliferation, apoptosis, differentiation, and cell migration. Disruption of either expression or localization of the polarity machinery deregulates these events, which promotes cancer initiation as well as progression of invasive and metastatic breast cancer.
References
Aigner K, Dampier B, Descovich L, Mikula M, Sultan A, Schreiber M, Mikulits W, Brabletz T, Strand D, Obrist P, Sommergruber W, Schweifer N, Wernitznig A, Beug H, Foisner R, Eger A (2007) The transcription factor ZEB1 (deltaEF1) promotes tumour cell dedifferentiation by repressing master regulators of epithelial polarity. Oncogene 26(49):6979–6988. doi:10.1038/sj.onc.1210508, 1210508 [pii]
Akhtar N, Streuli CH (2013) An integrin–ILK–microtubule network orients cell polarity and lumen formation in glandular epithelium. Nat Cell Biol 15(1):17–27. doi:10.1038/ncb2646
Amundadottir LT, Johnson MD, Merlino G, Smith GH, Dickson RB (1995) Synergistic interaction of transforming growth factor alpha and c-myc in mouse mammary and salivary gland tumorigenesis. Cell Growth Differ 6(6):737–748
Aranda V, Haire T, Nolan ME, Calarco JP, Rosenberg AZ, Fawcett JP, Pawson T, Muthuswamy SK (2006) Par6-aPKC uncouples ErbB2 induced disruption of polarized epithelial organization from proliferation control. Nat Cell Biol 8(11):1235–1245. doi:10.1038/ncb1485, ncb1485 [pii]
Bai L, Rohrschneider LR (2010) s-SHIP promoter expression marks activated stem cells in developing mouse mammary tissue. Genes Dev 24(17):1882–1892. doi:10.1101/gad.1932810, 24/17/1882 [pii]
Ball SM (1998) The development of the terminal end bud in the prepubertal-pubertal mouse mammary gland. Anat Rec 250(4):459–464. doi:10.1002/(SICI)1097-0185(199804)250:4<459::AID-AR9>3.0.CO;2-S
Bombonati A, Sgroi DC (2011) The molecular pathology of breast cancer progression. J Pathol 223(2):308–318. doi:10.1002/path.2808
Borowsky AD (2011) Choosing a mouse model: experimental biology in context – the utility and limitations of mouse models of breast cancer. Cold Spring Harb Perspect Biol 3(9):a009670. doi:10.1101/cshperspect.a009670
Bray K, Brakebusch C, Vargo-Gogola T (2011) The Rho GTPase Cdc42 is required for primary mammary epithelial cell morphogenesis in vitro. Small GTPases 2(5):247–258. doi:10.4161/sgtp.2.5.18163
Cardiff RD, Moghanaki D, Jensen RA (2000) Genetically engineered mouse models of mammary intraepithelial neoplasia. J Mammary Gland Biol Neoplasia 5(4):421–437
Chanson L, Brownfield D, Garbe JC, Kuhn I, Stampfer MR, Bissell MJ, LaBarge MA (2011) Self-organization is a dynamic and lineage-intrinsic property of mammary epithelial cells. Proc Natl Acad Sci U S A 108(8):3264–3269. doi:10.1073/pnas.1019556108, 1019556108 [pii]
Chatterjee S, Seifried L, Feigin ME, Gibbons DL, Scuoppo C, Lin W, Rizvi ZH, Lind E, Dissanayake D, Kurie J, Ohashi P, Muthuswamy SK (2012) Dysregulation of cell polarity proteins synergize with oncogenes or the microenvironment to induce invasive behavior in epithelial cells. PLoS One 7(4):e34343. doi:10.1371/journal.pone.0034343, PONE-D-11-13121 [pii]
Chen X, Macara IG (2005) Par-3 controls tight junction assembly through the Rac exchange factor Tiam1. Nat Cell Biol 7(3):262–269. doi:10.1038/ncb1226, ncb1226 [pii]
Cicalese A, Bonizzi G, Pasi CE, Faretta M, Ronzoni S, Giulini B, Brisken C, Minucci S, Di Fiore PP, Pelicci PG (2009) The tumor suppressor p53 regulates polarity of self-renewing divisions in mammary stem cells. Cell 138(6):1083–1095. doi:10.1016/j.cell.2009.06.048, S0092-8674(09)00840-X [pii]
Colaluca IN, Tosoni D, Nuciforo P, Senic-Matuglia F, Galimberti V, Viale G, Pece S, Di Fiore PP (2008) NUMB controls p53 tumour suppressor activity. Nature 451(7174):76–80. doi:10.1038/nature06412, nature06412 [pii]
Daniel CW, De Ome KB, Young JT, Blair PB, Faulkin LJ Jr (1968) The in vivo life span of normal and preneoplastic mouse mammary glands: a serial transplantation study. Proc Natl Acad Sci U S A 61(1):53–60
Debnath J, Muthuswamy SK, Brugge JS (2003) Morphogenesis and oncogenesis of MCF-10A mammary epithelial acini grown in three-dimensional basement membrane cultures. Methods 30(3):256–268, S104620230300032X [pii]
Deome KB, Faulkin LJ Jr, Bern HA, Blair PB (1959) Development of mammary tumors from hyperplastic alveolar nodules transplanted into gland-free mammary fat pads of female C3H mice. Cancer Res 19(5):515–520
Dimri G, Band H, Band V (2005) Mammary epithelial cell transformation: insights from cell culture and mouse models. Breast Cancer Res 7(4):171–179. doi:10.1186/bcr1275, bcr1275 [pii]
Dontu G, Jackson KW, McNicholas E, Kawamura MJ, Abdallah WM, Wicha MS (2004) Role of Notch signaling in cell-fate determination of human mammary stem/progenitor cells. Breast Cancer Res 6(6):R605–R615. doi:10.1186/bcr920, bcr920 [pii]
Dow LE, Elsum IA, King CL, Kinross KM, Richardson HE, Humbert PO (2008) Loss of human Scribble cooperates with H-Ras to promote cell invasion through deregulation of MAPK signalling. Oncogene 27(46):5988–6001. doi:10.1038/onc.2008.219, onc2008219 [pii]
Dow LE, Kauffman JS, Caddy J, Zarbalis K, Peterson AS, Jane SM, Russell SM, Humbert PO (2007) The tumour-suppressor Scribble dictates cell polarity during directed epithelial migration: regulation of Rho GTPase recruitment to the leading edge. Oncogene 26(16):2272–2282. doi:10.1038/sj.onc.1210016, 1210016 [pii]
Ellis IO (2010) Intraductal proliferative lesions of the breast: morphology, associated risk and molecular biology. Mod Pathol 23:S1–S7. doi:10.1038/modpathol.2010.56
Ewald AJ, Brenot A, Duong M, Chan BS, Werb Z (2008) Collective epithelial migration and cell rearrangements drive mammary branching morphogenesis. Dev Cell 14(4):570–581. doi:10.1016/j.devcel.2008.03.003, S1534-5807(08)00111-1 [pii]
Ewald AJ, Huebner RJ, Palsdottir H, Lee JK, Perez MJ, Jorgens DM, Tauscher AN, Cheung KJ, Werb Z, Auer M (2012) Mammary collective cell migration involves transient loss of epithelial features and individual cell migration within the epithelium. J Cell Sci 125(11):2638–2654. doi:10.1242/jcs.096875
Fogg VC, Liu CJ, Margolis B (2005) Multiple regions of Crumbs3 are required for tight junction formation in MCF10A cells. J Cell Sci 118(Pt 13):2859–2869. doi:10.1242/jcs.02412, 118/13/2859 [pii]
Friedl P, Gilmour D (2009) Collective cell migration in morphogenesis, regeneration and cancer. Nat Rev Mol Cell Biol 10(7):445–457. doi:10.1038/nrm2720, nrm2720 [pii]
Friedl P, Wolf K (2009) Plasticity of cell migration: a multiscale tuning model. J Cell Biol 188(1):11–19. doi:10.1083/jcb.200909003
Godde NJ, Galea RC, Elsum IA, Humbert PO (2010) Cell polarity in motion: redefining mammary tissue organization through EMT and cell polarity transitions. J Mammary Gland Biol Neoplasia 15(2):149–168. doi:10.1007/s10911-010-9180-2
Gönczy P (2008) Mechanisms of asymmetric cell division: flies and worms pave the way. Nat Rev Mol Cell Biol 9(5):355–366. doi:10.1038/nrm2388
Hall HG, Farson DA, Bissell MJ (1982) Lumen formation by epithelial cell lines in response to collagen overlay: a morphogenetic model in culture. Proc Natl Acad Sci 79:4672–4676
Hao Y, Du Q, Chen X, Zheng Z, Balsbaugh JL, Maitra S, Shabanowitz J, Hunt DF, Macara IG (2010) Par3 controls epithelial spindle orientation by aPKC-mediated phosphorylation of apical pins. Curr Biol 20(20):1809–1818. doi:10.1016/j.cub.2010.09.032, S0960-9822(10)01150-4 [pii]
Hinck L, Silberstein GB (2005) Key stages in mammary gland development: the mammary end bud as a motile organ. Breast Cancer Res 7(6):245–251. doi:10.1186/bcr1331, bcr1331 [pii]
Hu C, Dievart A, Lupien M, Calvo E, Tremblay G, Jolicoeur P (2006) Overexpression of activated murine Notch1 and Notch3 in transgenic mice blocks mammary gland development and induces mammary tumors. Am J Pathol 168(3):973–990. doi:10.2353/ajpath.2006.050416, S0002-9440(10)62157-8 [pii]
Hüsemann Y, Geigl JB, Schubert F, Musiani P, Meyer M, Burghart E, Forni G, Eils R, Fehm T, Riethmüller G, Klein CA (2008) Systemic spread is an early step in breast cancer. Cancer Cell 13(1):58–68. doi:10.1016/j.ccr.2007.12.003
Iden S, van Riel Wilhelmina E, Schäfer R, Song J-Y, Hirose T, Ohno S, Collard John G (2012) Tumor type-dependent function of the par3 polarity protein in skin tumorigenesis. Cancer Cell 22(3):389–403. doi:10.1016/j.ccr.2012.08.004
Jaffe AB, Kaji N, Durgan J, Hall A (2008) Cdc42 controls spindle orientation to position the apical surface during epithelial morphogenesis. J Cell Biol 183(4):625–633. doi:10.1083/jcb.200807121, jcb.200807121 [pii]
Keller PJ, Arendt LM, Kuperwasser C (2011) Stem cell maintenance of the mammary gland: it takes two. Cell Stem Cell 9(6):496–497. doi:10.1016/j.stem.2011.11.008, S1934-5909(11)00536-4 [pii]
Kenney NJ, Smith GH, Lawrence E, Barrett JC, Salomon DS (2001) Identification of stem cell units in the terminal end bud and duct of the mouse mammary gland. J Biomed Biotechnol 1(3):133–143. doi:10.1155/S1110724301000304, S1110724301000304 [pii]
Klinowska TC, Soriano JV, Edwards GM, Oliver JM, Valentijn AJ, Montesano R, Streuli CH (1999) Laminin and beta1 integrins are crucial for normal mammary gland development in the mouse. Dev Biol 215(1):13–32. doi:10.1006/dbio.1999.9435
Kojima Y, Akimoto K, Nagashima Y, Ishiguro H, Shirai S, Chishima T, Ichikawa Y, Ishikawa T, Sasaki T, Kubota Y, Inayama Y, Aoki I, Ohno S, Shimada H (2008) The overexpression and altered localization of the atypical protein kinase C lambda/iota in breast cancer correlates with the pathologic type of these tumors. Hum Pathol 39(6):824–831. doi:10.1016/j.humpath.2007.11.001, S0046-8177(07)00603-X [pii]
Lindley LE, Briegel KJ (2010) Molecular characterization of TGFbeta-induced epithelial-mesenchymal transition in normal finite lifespan human mammary epithelial cells. Biochem Biophys Res Commun 399(4):659–664. doi:10.1016/j.bbrc.2010.07.138, S0006-291X(10)01471-3 [pii]
Ling C, Su VMT, Zuo D, Muller WJ (2011) Loss of the 14-3-3 tumor suppressor is a critical event in ErbB2-mediated tumor progression. Cancer Discov 2(1):68–81. doi:10.1158/2159-8290.cd-11-0189
Ling C, Zuo D, Xue B, Muthuswamy S, Muller WJ (2010) A novel role for 14-3-3 in regulating epithelial cell polarity. Genes Dev 24(9):947–956. doi:10.1101/gad.1896810
Lutzner N, De-Castro Arce J, Rosl F (2012) Gene expression of the tumour suppressor LKB1 is mediated by Sp1, NF-Y and FOXO transcription factors. PLoS One 7(3):e32590. doi:10.1371/journal.pone.0032590, PONE-D-11-21365 [pii]
Macara IG, McCaffrey L (2013) Cell polarity in morphogenesis and metastasis. Phil Trans R Soc B 368(20130012):1–5. doi:10.1098/rstb.2013.0012
Macias H, Moran A, Samara Y, Moreno M, Compton JE, Harburg G, Strickland P, Hinck L (2011) SLIT/ROBO1 signaling suppresses mammary branching morphogenesis by limiting basal cell number. Dev Cell 20(6):827–840. doi:10.1016/j.devcel.2011.05.012, S1534-5807(11)00204-8 [pii]
Mailleux AA, Overholtzer M, Schmelzle T, Bouillet P, Strasser A, Brugge JS (2007) BIM regulates apoptosis during mammary ductal morphogenesis, and its absence reveals alternative cell death mechanisms. Dev Cell 12(2):221–234. doi:10.1016/j.devcel.2006.12.003, S1534-5807(06)00566-1 [pii]
Mani SA, Guo W, Liao M-J, Eaton EN, Ayyanan A, Zhou AY, Brooks M, Reinhard F, Zhang CC, Shipitsin M, Campbell LL, Polyak K, Brisken C, Yang J, Weinberg RA (2008) The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell 133(4):704–715. doi:10.1016/j.cell.2008.03.027
Martin-Belmonte F, Perez-Moreno M (2011) Epithelial cell polarity, stem cells and cancer. Nat Rev Cancer 12:23. doi:10.1038/nrc3169
McCaffrey LM, Macara IG (2009) The Par3/aPKC interaction is essential for end bud remodeling and progenitor differentiation during mammary gland morphogenesis. Genes Dev 23(12):1450–1460. doi:10.1101/gad.1795909, 23/12/1450 [pii]
McCaffrey LM, Macara IG (2011) Epithelial organization, cell polarity and tumorigenesis. Trends Cell Biol 21(12):727–735. doi:10.1016/j.tcb.2011.06.005, S0962-8924(11)00126-7 [pii]
McCaffrey LM, Macara IG (2012) Signaling pathways in cell polarity. Cold Spring Harb Perspect Biol 4(6):pii: a009654. doi:10.1101/cshperspect.a009654, cshperspect.a009654 [pii]
McCaffrey LM, Montalbano J, Mihai C, Macara IG (2012) Loss of the Par3 polarity protein promotes breast tumorigenesis and metastasis. Cancer Cell 22(5):601–614. doi:10.1016/j.ccr.2012.10.003, S1535-6108(12)00437-0 [pii]
Morales FC, Hayashi Y, van Pelt CS, Georgescu MM (2012) NHERF1/EBP50 controls lactation by establishing basal membrane polarity complexes with prolactin receptor. Cell Death Dis 3:e391. doi:10.1038/cddis.2012.131
Morel AP, Lievre M, Thomas C, Hinkal G, Ansieau S, Puisieux A (2008) Generation of breast cancer stem cells through epithelial-mesenchymal transition. PLoS One 3(8):e2888. doi:10.1371/journal.pone.0002888
Nance J, Zallen JA (2011) Elaborating polarity: PAR proteins and the cytoskeleton. Development 138(5):799–809. doi:10.1242/dev.053538
Naylor MJ, Li N, Cheung J, Lowe ET, Lambert E, Marlow R, Wang P, Schatzmann F, Wintermantel T, Schuetz G, Clarke AR, Mueller U, Hynes NE, Streuli CH (2005) Ablation of beta1 integrin in mammary epithelium reveals a key role for integrin in glandular morphogenesis and differentiation. J Cell Biol 171(4):717–728. doi:10.1083/jcb.200503144, jcb.200503144 [pii]
Niemann C, Brinkmann V, Spitzer E, Hartmann G, Sachs M, Naundorf H, Birchmeier W (1998) Reconstitution of mammary gland development in vitro: requirement of c-met and c-erbB2 signaling for branching and alveolar morphogenesis. J Cell Biol 143(2):533–545
Nishimura T, Kaibuchi K (2007) Numb controls integrin endocytosis for directional cell migration with aPKC and PAR-3. Dev Cell 13(1):15–28. doi:10.1016/j.devcel.2007.05.003, S1534-5807(07)00198-0 [pii]
Nishimura T, Yamaguchi T, Kato K, Yoshizawa M, Nabeshima Y, Ohno S, Hoshino M, Kaibuchi K (2005) PAR-6-PAR-3 mediates Cdc42-induced Rac activation through the Rac GEFs STEF/Tiam1. Nat Cell Biol 7(3):270–277. doi:10.1038/ncb1227, ncb1227 [pii]
Nolan ME, Aranda V, Lee S, Lakshmi B, Basu S, Allred DC, Muthuswamy SK (2008) The polarity protein Par6 induces cell proliferation and is overexpressed in breast cancer. Cancer Res 68(20):8201–8209. doi:10.1158/0008-5472.CAN-07-6567, 68/20/8201 [pii]
O’Brien LE, Jou TS, Pollack AL, Zhang Q, Hansen SH, Yurchenco P, Mostov KE (2001) Rac1 orientates epithelial apical polarity through effects on basolateral laminin assembly. Nat Cell Biol 3(9):831–838. doi:10.1038/ncb0901-831
Oakes SR, Rogers RL, Naylor MJ, Ormandy CJ (2008) Prolactin regulation of mammary gland development. J Mammary Gland Biol Neoplasia 13(1):13–28. doi:10.1007/s10911-008-9069-5
Page H, Flood P, Reynaud EG (2012) Three-dimensional tissue cultures: current trends and beyond. Cell Tissue Res 352(1):123–131. doi:10.1007/s00441-012-1441-5
Paget JA, Restall IJ, Daneshmand M, Mersereau JA, Simard MA, Parolin DAE, Lavictoire SJ, Amin MS, Islam S, Lorimer IAJ (2011) Repression of cancer cell senescence by PKCι. Oncogene 31(31):3584–3596. doi:10.1038/onc.2011.524
Parkin DM, Pisani P, Ferlay J (1999) Global cancer statistics. CA Cancer J Clin 49(1):33–64, 31
Parsa S, Ramasamy SK, De Langhe S, Gupte VV, Haigh JJ, Medina D, Bellusci S (2008) Terminal end bud maintenance in mammary gland is dependent upon FGFR2b signaling. Dev Biol 317(1):121–131. doi:10.1016/j.ydbio.2008.02.014, S0012-1606(08)00110-3 [pii]
Partanen JI, Tervonen TA, Myllynen M, Lind E, Imai M, Katajisto P, Dijkgraaf GJ, Kovanen PE, Makela TP, Werb Z, Klefstrom J (2012a) Tumor suppressor function of Liver kinase B1 (Lkb1) is linked to regulation of epithelial integrity. Proc Natl Acad Sci U S A 109(7):E388–E397. doi:10.1073/pnas.1120421109
Partanen JI, Tervonen TA, Myllynen M, Lind E, Imai M, Katajisto P, Dijkgraaf GJP, Kovanen PE, Makela TP, Werb Z, Klefstrom J (2012b) Tumor suppressor function of Liver kinase B1 (Lkb1) is linked to regulation of epithelial integrity. Proc Natl Acad Sci 109(7):E388–E397
Pasic L, Eisinger-Mathason TS, Velayudhan BT, Moskaluk CA, Brenin DR, Macara IG, Lannigan DA (2011) Sustained activation of the HER1-ERK1/2-RSK signaling pathway controls myoepithelial cell fate in human mammary tissue. Genes Dev 25(15):1641–1653. doi:10.1101/gad.2025611, 25/15/1641 [pii]
Pece S, Serresi M, Santolini E, Capra M, Hulleman E, Galimberti V, Zurrida S, Maisonneuve P, Viale G, Di Fiore PP (2004) Loss of negative regulation by Numb over Notch is relevant to human breast carcinogenesis. J Cell Biol 167(2):215–221. doi:10.1083/jcb.200406140, jcb.200406140 [pii]
Podsypanina K, Du YCN, Jechlinger M, Beverly LJ, Hambardzumyan D, Varmus H (2008) Seeding and propagation of untransformed mouse mammary cells in the lung. Science 321(5897):1841–1844. doi:10.1126/science.1161621
Prat A, Parker JS, Karginova O, Fan C, Livasy C, Herschkowitz JI, He X, Perou CM (2010) Phenotypic and molecular characterization of the claudin-low intrinsic subtype of breast cancer. Breast Cancer Res 12(5):R68. doi:10.1186/bcr2635, bcr2635 [pii]
Rakha EA, Reis-Filho JS, Ellis IO (2008) Basal-like breast cancer: a critical review. J Clin Oncol 26(15):2568–2581. doi:10.1200/jco.2007.13.1748
Ranger JJ, Levy DE, Shahalizadeh S, Hallett M, Muller WJ (2009) Identification of a Stat3-dependent transcription regulatory network involved in metastatic progression. Cancer Res 69(17):6823–6830. doi:10.1158/0008-5472.CAN-09-1684, 0008-5472.CAN-09-1684 [pii]
Ridky TW, Chow JM, Wong DJ, Khavari PA (2010) Invasive three-dimensional organotypic neoplasia from multiple normal human epithelia. Nat Med 16(12):1450–1455. doi:10.1038/nm.2265
Russ A, Louderbough JM, Zarnescu D, Schroeder JA (2012) Hugl1 and Hugl2 in mammary epithelial cells: polarity, proliferation, and differentiation. PLoS One 7(10):e47734. doi:10.1371/journal.pone.0047734, PONE-D-12-22224 [pii]
Schnitt SJ (2003) The diagnosis and management of pre-invasive breast disease Flat epithelial atypia—classification, pathologic features and clinical significance. Breast Cancer Res 5(5):263. doi:10.1186/bcr625
Shackleton M, Vaillant F, Simpson KJ, Stingl J, Smyth GK, Asselin-Labat ML, Wu L, Lindeman GJ, Visvader JE (2006) Generation of a functional mammary gland from a single stem cell. Nature 439(7072):84–88. doi:10.1038/nature04372, nature04372 [pii]
Smith CA, Lau KM, Rahmani Z, Dho SE, Brothers G, She YM, Berry DM, Bonneil E, Thibault P, Schweisguth F, Le Borgne R, McGlade CJ (2007) aPKC-mediated phosphorylation regulates asymmetric membrane localization of the cell fate determinant Numb. EMBO J 26(2):468–480. doi:10.1038/sj.emboj.7601495, 7601495 [pii]
Stampfer MR, Bartley JC (1988) Human mammary epithelial cells in culture: differentiation and transformation. Cancer Treat Res 40:1–24
Stein T, Salomonis N, Gusterson BA (2007) Mammary gland involution as a multi-step process. J Mammary Gland Biol Neoplasia 12(1):25–35. doi:10.1007/s10911-007-9035-7
Stemmer-Rachamimov AO, Wiederhold T, Nielsen GP, James M, Pinney-Michalowski D, Roy JE, Cohen WA, Ramesh V, Louis DN (2001) NHE-RF, a merlin-interacting protein, is primarily expressed in luminal epithelia, proliferative endometrium, and estrogen receptor-positive breast carcinomas. Am J Pathol 158(1):57–62. doi:10.1016/S0002-9440(10)63944-2, S0002-9440(10)63944-2 [pii]
Sternlicht MD (2006) Key stages in mammary gland development: the cues that regulated ductal branching morphogenesis. Breast Cancer Res 8(1):201. doi:10.1186/bcr1368
Sternlicht MD, Kouros-Mehr H, Lu P, Werb Z (2006) Hormonal and local control of mammary branching morphogenesis. Differentiation 74(7):365–381. doi:10.1111/j.1432-0436.2006.00105.x
Stingl J, Eirew P, Ricketson I, Shackleton M, Vaillant F, Choi D, Li HI, Eaves CJ (2006) Purification and unique properties of mammary epithelial stem cells. Nature 439(7079):993–997. doi:10.1038/nature04496, nature04496 [pii]
Taddei I, Deugnier MA, Faraldo MM, Petit V, Bouvard D, Medina D, Fassler R, Thiery JP, Glukhova MA (2008) Beta1 integrin deletion from the basal compartment of the mammary epithelium affects stem cells. Nat Cell Biol 10(6):716–722. doi:10.1038/ncb1734, ncb1734 [pii]
TCGA CGAN (2012) Comprehensive molecular portraits of human breast tumours. Nature 490(7418):61–70. doi:10.1038/nature11412, nature11412 [pii]
Tepass U (2012) The apical polarity protein network in Drosophila epithelial cells: regulation of polarity, junctions, morphogenesis, cell growth, and survival. Annu Rev Cell Dev Biol 28:655–685. doi:10.1146/annurev-cellbio-092910-154033
Thiery JP, Acloque H, Huang RY, Nieto MA (2009) Epithelial-mesenchymal transitions in development and disease. Cell 139(5):871–890. doi:10.1016/j.cell.2009.11.007, S0092-8674(09)01419-6 [pii]
Thompson BJ (2012) Cell polarity: models and mechanisms from yeast, worms and flies. Development 140(1):13–21. doi:10.1242/dev.083634
Van Keymeulen A, Rocha AS, Ousset M, Beck B, Bouvencourt G, Rock J, Sharma N, Dekoninck S, Blanpain C (2011) Distinct stem cells contribute to mammary gland development and maintenance. Nature 479(7372):189–193. doi:10.1038/nature10573, nature10573 [pii]
Viloria-Petit AM, David L, Jia JY, Erdemir T, Bane AL, Pinnaduwage D, Roncari L, Narimatsu M, Bose R, Moffat J, Wong JW, Kerbel RS, O’Malley FP, Andrulis IL, Wrana JL (2009) A role for the TGFbeta-Par6 polarity pathway in breast cancer progression. Proc Natl Acad Sci U S A 106(33):14028–14033. doi:10.1073/pnas.0906796106, 0906796106 [pii]
Visvader JE (2009) Keeping abreast of the mammary epithelial hierarchy and breast tumorigenesis. Genes Dev 23(22):2563–2577. doi:10.1101/gad.1849509, 23/22/2563 [pii]
Visvader JE, Lindeman GJ (2011) The unmasking of novel unipotent stem cells in the mammary gland. EMBO J 30(24):4858–4859. doi:10.1038/emboj.2011.415, emboj2011415 [pii]
Weaver VM, Lelievre S, Lakins JN, Chrenek MA, Jones JC, Giancotti F, Werb Z, Bissell MJ (2002) beta4 integrin-dependent formation of polarized three-dimensional architecture confers resistance to apoptosis in normal and malignant mammary epithelium. Cancer Cell 2(3):205–216, S1535610802001253 [pii]
Whyte J, Thornton L, McNally S, McCarthy S, Lanigan F, Gallagher WM, Stein T, Martin F (2010) PKCzeta regulates cell polarisation and proliferation restriction during mammary acinus formation. J Cell Sci 123(Pt 19):3316–3328. doi:10.1242/jcs.065243, 123/19/3316 [pii]
Williams JM, Daniel CW (1983) Mammary ductal elongation: differentiation of myoepithelium and basal lamina during branching morphogenesis. Dev Biol 97(2):274–290, 0012-1606(83)90086-6 [pii]
Xue B, Krishnamurthy K, Allred DC, Muthuswamy SK (2012) Loss of Par3 promotes breast cancer metastasis by compromising cell–cell cohesion. Nat Cell Biol 15(2):189–200. doi:10.1038/ncb2663
Yaswen P, Stampfer MR (2001) Epigenetic changes accompanying human mammary epithelial cell immortalization. J Mammary Gland Biol Neoplasia 6(2):223–234
Yu W, Datta A, Leroy P, O’Brien LE, Mak G, Jou TS, Matlin KS, Mostov KE, Zegers MM (2005) Beta1-integrin orients epithelial polarity via Rac1 and laminin. Mol Biol Cell 16(2):433–445. doi:10.1091/mbc.E04-05-0435
Zagouri F, Sergentanis TN, Zografos GC (2007) Precursors and preinvasive lesions of the breast: the role of molecular prognostic markers in the diagnostic and therapeutic dilemma. World J Surg Oncol 5(1):57. doi:10.1186/1477-7819-5-57
Zhan L, Rosenberg A, Bergami KC, Yu M, Xuan Z, Jaffe AB, Allred C, Muthuswamy SK (2008) Deregulation of scribble promotes mammary tumorigenesis and reveals a role for cell polarity in carcinoma. Cell 135(5):865–878. doi:10.1016/j.cell.2008.09.045
Zheng Z, Zhu H, Wan Q, Liu J, Xiao Z, Siderovski DP, Du Q (2010) LGN regulates mitotic spindle orientation during epithelial morphogenesis. J Cell Biol 189(2):275–288. doi:10.1083/jcb.200910021, jcb.200910021 [pii]
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Rejon, C., McCaffrey, L. (2015). Cell Polarity in Mammary Gland Morphogenesis and Breast Cancer. In: Ebnet, K. (eds) Cell Polarity 2. Springer, Cham. https://doi.org/10.1007/978-3-319-14466-5_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-14466-5_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-14465-8
Online ISBN: 978-3-319-14466-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)