Abstract
This chapter deals with lower-limb prostheses and, more specifically, the relationship between socket design and the quality of gait and mobility. Prosthetic sockets and suspension systems provide an intimate contact with the residual limb, and their interaction is important for overall comfort, fit, and mobility function. Even though technological advances have led to the enhancement of socket/limb interfaces, prosthesis users still suffer from a variety of problems, particularly related to the high and repetitive loading of the limb during gait. In this chapter, socket designs are reviewed, along with clinical issues relating to their use. This is followed by an examination of the effect of the socket/limb interface on the quality of gait. The chapter concludes with future perspectives and trends in prosthetic/limb interface approaches and technology.
Access provided by CONRICYT-eBooks. Download reference work entry PDF
Similar content being viewed by others
Keywords
- Prostheses
- Amputation
- Fit
- Gait
- Socket
- Rehabilitation
- Walking
- Motion analysis
- Mobility
- Residual limb
- Transtibial
- Transfemoral
- Partial foot
Introduction
Lower-limb loss is mainly caused by trauma, diabetes, tumors, congenital limb deficiency, and peripheral vascular disease (PVD) (Smith et al. 2004). According to Smith et al. (2004), lower-limb amputations worldwide are primarily attributed to PVD, which is frequently linked to diabetes mellitus. Furthermore, statistics reveal an increasing number of diabetic patients worldwide. The rate of lower-limb amputations in individuals with diabetes is 15 times higher than healthy people. In the United States alone, 82% of all amputations occur because of PVD (Seymour 2002).
A prosthesis or artificial limb is the foremost element in the rehabilitation process following an amputation. Prosthetic limbs for lower-limb amputees typically consist of a socket, a soft liner as cushion at the skin-socket interface, and suspension system to securely maintain the prosthetic limb in place, which itself is comprised of pylons, connectors, and prosthetic foot and knee (in the case of a transfemoral prosthesis) components. These components are assembled and aligned and may be cosmetically finished to match the appearance of the sound limb.
Prosthetic components and systems have evolved tremendously in recent decades to a level that affords individuals with amputations high-level mobility function and the ability to do many of the things of their non-amputee counterparts. However, despite these key technological and clinical advances in prosthetic care, numerous problems persist among prosthetic users. Many problems are related to the residuum/prosthesis interface, comprised of the socket, liners, and suspension components. The socket and suspension play an imperative role, facilitating weight bearing on the prosthetic limb, and also control to move the limb and to retain balance when standing and walking. When these aspects are well managed, prosthetic rehabilitation can lead to successful patient outcomes including safe, effective, efficient, and comfortable prosthetic use during mobility.
State of the Art
In this section, a comprehensive overview is provided relating to prosthetic interface design focusing on the contemporary technologies and clinical practices applied within the P&O industry. The section describes commercially available technologies, including various socket, liner, and suspension designs as well as the existing evidence relating to their clinical use. As achieving an optimal fit between the prosthesis and residual limb is one of the primary goals and also challenges, this topic is thoroughly covered in the latter parts of this section. This includes the techniques by which socket fit is measured and evaluated.
Prosthesis/Limb Interface
A prosthesis is attached to the residual limb and the rest of the body using certain components. These, including the socket, liner, and suspension, come in close contact with the soft tissue and skin. A prosthetic socket encompasses the residual limb and connects other distal parts of the prosthesis to the individual. Suspension is the means by which a socket is held in place over the residuum. In general, suspension means can be categorized as internal (anatomic and atmospheric) or external methods (straps and hinges). In addition to that, liners are soft inserts that assist in suspension and at the same time provide added comfort within the typically hard socket shell. Traditionally liners have been made of foam materials, while more contemporary designs tend to utilize silicon gel materials.
Prosthetic sockets are fabricated from different materials and have various designs based on the level of amputation and activity. Traditionally, sockets were made of leather or wood, but in line with the advances in material science, new thermoplastic , thermoset , and composite materials offer advantages including durability, flexibility, and high strength-to-weight ratios. Other aspects of socket designs have also evolved, aimed at improving the fit, comfort, and weight-bearing capacity. Some of these advancements are applicable broadly across amputee populations, while others are uniquely applicable to a particular subgroup. A common differentiation is based on the amputation level, with different socket designs being appropriate for transtibial and transfemoral amputations, as well as less commonly presented amputation levels including partial foot and pelvic level amputations.
Conventional techniques for fabricating sockets involve taking plaster impressions of the residuum to produce a positive mold which is rectified to facilitate the fabrication of an optimal fitting socket. Computer-aided technology has also been used in the fabrication of socket systems. The systems digitize the shape of the residual limb using optical or laser scanners, for CNC fabrication of a positive mold. These techniques are not presented in detail here, but the reader is instead referred to other resources for this information (Smith et al. 2004).
For transtibial amputations, the patellar tendon-bearing (PTB) socket design has been widely used around the world. These sockets were commonly fabricated of thermoplastic or lamination material (Radcliffe et al. 1961). First introduced in 1959, the concept was to provide an intimate fit with the residuum unlike previous designs (Fergason and Smith 1999). In a PTB socket, the anterior socket wall covers the distal third of the patella. An inward bar or counter that is located immediately below the patella and at the center of the patellar ligament serves as a weight-bearing surface and suspension means. The key weight-bearing area and pressure-tolerant surface is the medial wall, dented at the medial tibial flare. A relief area for the distal fibula and fibula head is formed on the lateral wall. The posterior wall applies force in the anterior direction to keep the patellar tendon on the bar and terminates proximally somewhat higher than the patellar bar.
A major innovation relating to prosthetic interfaces has been the development of silicone suction suspension (Fillauer et al. 1989) and the Iceross (Baars and Geertzen 2005; Kristinsson 1993) sockets. Used for both transtibial and transfemoral amputations, these systems were characterized by total surface bearing (TSB), hydrostatic loading, and improved techniques of suspension (Staats and Lundt 1987; Sewell et al. 2000). These systems are designed to distribute the loads consistently over the residual limb without any undercut or relief areas to reduce the peak pressure (Beil and Street 2004). A gel or silicone liner (soft socket) that is surrounded by a hard socket provides cushioning for the sensitive bony areas and dissipates the load throughout the socket. The silicone liners are mainly suspended by pin and lock mechanisms, seals around the liner circumference, or recently by magnetic systems (Eshraghi et al. 2013a).
Suction suspension provides the most secure attachment to the residual limb. For almost half a century, the suction socket was the main socket type for transfemoral amputees. In the original method, the residual limb’s skin served as a gasket to seal the socket brim against air penetration. The requirements are that the skin is pliable and artifact free (e.g., deep scar). During the fitting, the circumference of the socket should be reduced carefully to avoid blood flow restriction and ensure constant friction between the skin and the socket. A valve is placed in the distal socket that once opened allows air out of the socket as the residual limb enters the socket during donning. Once all of the air exits the socket space, the valve is closed to create atmospheric pressure.
A more recent evolution of the suction suspension, which has gained broad clinical interest, is the vacuum-assisted socket or VASS. Both suction suspension and elevated vacuum suspension use the difference in atmospheric pressure to attach the residual limb to the socket (Fig. 1). The main difference is that suction systems typically use a passive expulsion valve to create negative pressure once the limb starts to move, while vacuum systems use an active pump to produce a negative pressure difference regardless of the limb position. In the advanced versions of these systems, the pressure is electronically monitored and automatically adjusted by the onboard pump. The main advantages of elevated vacuum are believed to include better accommodation to the residual limb’s volume fluctuation by promoting normal fluid exchange, decreasing forces on the residual limb, and enhancing proprioception and pistoning (Board et al. 2001; Klute et al. 2011; Gerschutz et al. 2010).
Transtibial prosthesis with Harmony® elevated vacuum system by Otto Bock (Ottobock HealthCare, North America; Austin, TX USA. http://www.ottobock.com)
The elevated vacuum system has a pump to pull air out of the socket from between the inner socket and the residual limb to keep the tissue against the socket walls, hence inhibiting movement in all directions. Recently, Össur introduced a sleeveless vacuum system, called the Unity (Fig. 2). Unlike the other available systems, such as Harmony (Otto Bock), the system incorporates a Seal-In liner to enhance prosthetic suspension. Basically, the system is claimed to provide the same benefits of other vacuum-assisted systems, such as high level of suspension, security, improved comfort and skin health, and better gait, without the restrictions that a sleeve imposes on the amputee.
Unity sleeveless vacuum system for transtibial and transfemoral prostheses by Össur ehf, Reykjavik Iceland (http://www.ossur.com)
Evidence relating to the VASS shows improvements in residual limb health, including a decrease in skin problems, such as sores and promotion of wound healing (Traballesi et al. 2012). The blood supply is also believed to be improved within the limb, because the socket acts as a vascular pump that promotes blood circulation. Potential caveats of the system, partially related to improper use of the device, can result if, for example, the user dons the socket incorrectly and then turns on the pump causing the vacuum to pull the limb into the socket with such force that it may create a blood blister or other soft tissue injury.
Transfemoral socket designs are quite different from the transtibial sockets, mainly due to the difference in residual limb size, shape, tissue and skin coverage, and bony prominences. Two main socket designs for the transfemoral prosthesis are the quadrilateral socket and the ischial containment socket. These two designs are differentiated by the proximal brim contours; in the quadrilateral socket, the posterior brim lies parallel to the ground and has a wide seat (called the ischial seat), while in the ischial containment, the ischium and the ischial ramus are inside the socket. The ischial containment socket creates a bony lock that improves mediolateral stability and gait (Fairley 2004). An evolution is the ischial-ramal containment socket (MAS or Marlo Anatomical Socket). It was designed to contain the ischial ramus and the ischial tuberosity, thus providing a bony lock within the socket for improved stability. There is also evidence that this design can reduce energy cost of walking in transfemoral amputees compared with the ischial containment socket (Traballesi et al. 2011). The soft liners are similar to the transtibial designs and use the same suspension types, such as pin and lock , seal, or magnet. Also, vacuum and suction systems are used for both transfemoral and transtibial prostheses .
Variations of hard socket designs include reduced thickness of socket walls or the use of more compliant materials, mainly aimed to provide freedom of movement by increased muscle activity, reduce the weight of the prosthesis, provide better proprioception, improve perspiration, and enhance comfort. Examples of these design variations include the Icelandic-Swedish-New York (ISNY) system and Scandinavian Flexible Socket (SFS). One commonly used design is a flexible thermoplastic socket with a rigid or semirigid fenestrated frame. Kristinsson described that “To label a socket as flexible I would say that you should be able to deform it by your hands, and the material should not be elastic enough to stretch under the loads it will be subjected to.” Yet, the frame design is very important as it must support the flexible inner socket, and the combination of socket and frame must be structurally stable and robust to counteract the reaction forces.
New socket designs are continually being introduced. For example, Martin Bionics have introduced the Socket-less Socket™, utilizing a system of strategically placed struts and cushioned support surfaces to contain and support the limb (Fig. 3). The technology, currently available for knee disarticulation and transfemoral prostheses, claims a number of advantages over more conventional socket designs. Rather than a static shape, the Socket-less technology is claimed to have greater control and adjustability of the socket fit. Another design is for hip disarticulation level of amputation, called “Bikini socket” (Fig. 3). With iliac crest stabilizers, this socket is claimed to provide a more direct biomechanical link between the prosthesis and user, resulting in greater control, and functional outcomes and comfort. With less material, these designs are able to decrease overall weight of the prosthesis. Another similar approach toward modular socket designs is the basis for the LIM Innovations “Infinite” socket available for both transtibial and transfemoral amputations (Fig. 4). The system includes a soft upper brim, specific adjustable features, and carbon fiber strut structure. The design is customized to fit the amputee’s exact anatomy through 3D scanning, a software, and custom manufacturing methods.
Infinite transfemoral socket by LIM Innovations® (https://www.liminnovations.com)
Most of the research literature pertains to transtibial, knee disarticulation, and transfemoral amputations; however, a small body of work is focused on other amputation levels. Partial foot amputations and those at the level of ankle joint, such as Syme’s, may be less challenging in terms of socket design and suspension compared with higher amputation levels as the lever arm is quite long and the amputee is more stable during standing and walking. Some partial foot amputees can ambulate over the amputation site for some daily activities, without a prosthesis. Those that have lost parts of the foot, such as toes and/or metatarsal bones, may need only minor changes to their shoes or insoles in the form of fillers, and thus, the term socket might not apply to them. In general, given that most of the limb is intact and unaltered in the case of partial amputation, gait limitations and alterations are less pronounced than with higher amputation levels (Dillon and Barker 2008). Main areas of focus relating to partial foot amputations have included the design of interfaces to restore effective foot length and also instruments to monitor the in-socket pressure distributions (Alvarez-Camacho et al. 2014; Dillon and Barker 2006).
Hip disarticulations and trans-pelvic amputations have also received limited attention in the published literature, likely due to the fact that this level of amputation is not very common. Generally, these levels of amputation have the highest rejection rates and therefore lowest levels of prosthetic use (Smith et al. 2004), and one of the primary reasons for this, as stated by amputees, is the uncomfortable socket. Not only is it biomechanically more difficult to develop a well-fit socket, but most prosthetists also have inadequate experience of fabricating and fitting sockets at these less-frequently encountered levels of amputation. Gel liners are used for both hip disarticulation and trans-pelvic levels to protect the soft tissues. The hip disarticulation socket is usually suspended by locking onto above the iliac crest around the waist.
The use of suction sockets has seen some success in this challenging population with high-level amputations, providing greater comfort and fit, and resulting in higher patient compliance and improved mobility (Zaffer et al. 1999). The Canadian prosthesis design is still the most common design not only for hip disarticulations but also trans-pelvic and very short transfemoral amputations (Fernández and Formigo 2005). However, patient outcomes have not generally been very good. Limited compliance with these systems has been found, largely due to intolerance of socket fit and limited ability to ambulate. Challenges, in general, include poor gait patterns, socket discomfort, loss of mobility, instability, and high energy consumption (Ludwigs et al. 2010).
Socket Fit
Socket fit can be affected by numerous factors, relating to the patient’s condition, rehabilitation process, and technical aspects. Factors include residual limb volume, skin health, blood circulation, activity level, muscle activity, cause of amputation (vascular or traumatic), level of amputation, method of amputation surgery, as well as the amount of time since the surgery. Physiotherapy and gait training further influence outcomes. On the technical side, socket design including the presence or absence of soft liner or sleeve, suspension concept, and accessories all play a role, as does the prosthetist’s skill in capturing an accurate impression (e.g., casting or scanning) of the residual limb and appropriately modifying it to fabricate the socket.
The effect of volume fluctuations is among the most pervasive issues relating to socket fit, because it can cause other problems, such as skin breakdown, pistoning, increased shear forces, increased pressure on bony prominences, decreased comfort, and gait deviations (Sanders and Fatone 2011). The main cause of volume change is socket pressure on the soft tissue. To manage this, traditionally socks are added during the day.
During the day, volume fluctuation can increase pressure in certain regions because of the abatement of soft tissue within the socket, thus exposing bony areas to the socket walls. This can lead to pain and possible tissue breakdown. Another problem that arises from volume change or reduced socket fit is “pistoning,” in which the limb has excessive movement in the socket, particularly during the loading and unloading cycles of gait. This can lead to greater shear forces between the socket and limb and higher peak pressures during the loading response phase of gait (Beil and Street 2004). In addition to socket fit, the suspension system or accessories, such as belts and straps, may contribute to issues related to pistoning.
Several changes in the socket design and suspension systems have been made in an effort to address the aforementioned problems. Patellar tendon-bearing (PTB) sockets were widely used for transtibial amputees for years. This socket design exerts high loads on certain areas of the limb. While these areas are typically called pressure tolerant, the users may struggle with reddened skin, calluses, and soft tissue breakdown over the course of time. The peak pressures in the PTB socket can reach 300–400 kPa, whereas in a total contact socket or a TSB socket, pressure is reduced to less than 200 kPa (Beil and Street 2004). A TSB, providing better distribution of loads, can therefore aid in venous return and decreasing the skin reddening on the distal residual limb.
In a transfemoral prosthesis, the current standard of care focuses on the proximal aspect of the socket to gain a stable connection during stance phase. The brim (the most proximal aspect of the socket) contains the ischial ramus and the associated trim lines above the ischial tuberosity. The main purpose of this design is to provide a stance stability mechanism by forming a bony lock with the pelvis in the coronal plane (Kahle and Highsmith 2014), which can prevent the socket from lateral shift and femoral abduction. Enhanced suspension also reduces motion within the socket during swing (Klute et al. 2011). Vacuum-assisted suspension provides dynamic suspension, either through an electronic or manual pump. Thus, recently the VASS has become an effective option for transfemoral amputation.
In terms of suspension systems, pin and lock systems have advantages such as ease of donning and enhanced suspension. Nevertheless, the silicone liner is apt to squeeze the residual limb proximally and cause large distal suction during the swing phase of gait, promoting tissue breakdown and skin problems at the distal end (Beil and Street 2004). This problem is more pronounced in highly active users, leading to a potential contraindication for the use of pin and lock systems in this demographic. Overall, in any design, socket fit may be jeopardized due to volume loss during the day. The elevated vacuum system is claimed to help maintain the limb volume as constant as possible. However, current evidence is not adequate to fully support this.
Evaluation of Socket Fit
It is not easy to determine the socket fit objectively. In clinical practice, visual inspections including the use of check sockets and subjective feedback of amputees are the most commonly used methods to evaluate socket fit. Even though more objective methods have been researched and developed, in general they have not been advanced enough to be practically adopted in clinical practice. Important factors to consider in the evaluation of socket fit include but are not limited to in-socket pressure, skin condition, amount of pistoning, the presence or absence and level of pain as well as skin and soft tissue problems, quality of mobility, and comfort level.
In-socket pressure can be measured with different types of transducers (Laing et al. 2011; Polliack et al. 2000; Sanders et al. 1998; Zhang et al. 1998); or estimated using simulation techniques (Commean et al. 1997; Lin et al. 2004; Silver-Thorn et al. 1996). Measuring in-socket pressures can provide important information in case total surface bearing has been achieved or not. Friction within the prosthetic socket has a twofold effect as it helps to retain the prosthesis on the residuum, but at the same time, it may distort the soft tissue (Mak et al. 2001). If high friction occurs at an interface, stress may be localized, and this can lead to the deformation of the remaining tissue. Conversely, Zhang et al. found that lubricating the skin will increase the interface pressure (Zhang et al. 1996). Liners and prosthetic sockets may alter the pressure applied to the residual limb. Without understanding the changes imposed on the soft tissue and skin by different socket designs and suspension systems, it is impossible to effectively evaluate the overall prosthetic fit. Moreover, prosthetic interface pressure is believed to be a determinant of the amputee’s comfort (Dou et al. 2006; Jia et al. 2004; Sanders et al. 2006a; Sewell et al. 2000).
Another important measure of socket fit is pistoning (Commean et al. 1997; Madsen et al. 2000; Sanders et al. 2006b). Pistoning is defined as the relative movement, either between the liner and socket or the residual limb and bone, skin, and liner/socket. Various measurement techniques have been used so far, including the spiral computerized tomography (CT) (Madsen et al. 2000), Roentgenology (Söderberg et al. 2003), ultrasound (Convery and Murray 2000), cineradiography, radiography (Narita et al. 1997) as well as photoelectric sensors, and custom-made transducers (Abu Osman et al. 2010; Sanders et al. 2006b). The most recent methods use the 3D motion analysis system to quantify pistoning (Gholizadeh et al. 2011, 2012a, b). Several studies have measured pistoning during gait. Primarily, the methods for pistoning measurement involve complicated settings and techniques, mostly limited to the research laboratory. While it is important for clinicians to assess socket fit, it still remains impractical to measure socket fit through the current pistoning measurement approaches.
Volume accommodation strategies, such as socks, liquid- or air-filled bladders and pads within the prosthetic socket, and adjustable sockets, are used to compensate for volume loss (Sanders et al. 2015; Pirouzi et al. 2014). Sock plies can be worn over the liners (e.g., pelite liners (PTB), pin/lock or Seal-In systems). Yet, this method is not feasible for suction systems that require close contact between the socket and skin for maintaining a vacuum. Some studies have explored methods of measuring the socket ply thickness as an indirect measure of socket fit (Sanders et al. 2015). Moreover, reducing the socket size using air bladders or socks is said to further promote fluid volume loss (Sanders et al. 2012, 2013). The physiological processes that lead to volume loss are not well understood; however, a physical analogy can be made to a sponge, where fluid is rapidly expelled when the amputee is active and the residual limb is squeezed inside a tight socket (because of addition of sock or bladder size). Yet, that fluid does not simply recover when the socket is released (Sanders et al. 2013). To address this issue, a recent method called “socket release” has been introduced to lessen volume change. In this technique, no material is removed from or added to the socket, but the amputee temporarily doffs the prosthesis to facilitate recovery of fluid volume by relieving interface stresses within the socket immediately after a period of activity (Sanders et al. 2015). Removing the prosthesis decreases interstitial fluid pressures, which allows the residual limb’s blood vessels to expand, increasing blood volume within the limb.
Effect of Socket Design and Fit on Gait
Prosthetic Mobility
Prosthetic devices should be appropriate for the user’s medical and physical condition, capabilities, and mobility goals. A prosthesis should also aim to provide safe, efficient, and biomechanically appropriate gait. Hence, an important goal in the rehabilitation of lower-limb amputees is to enable functional mobility, seen as one of the most significant aspects of achieving independence (Sansam et al. 2009).
Amputees typically present with differences in their walking compared with non-amputees, and minimizing these differences, or gait deviations, is a common rehabilitation goal. Gait deviations are most often seen in the spatiotemporal, kinematic, and kinetic measurements of gait, meaning that the placement and timing of steps, movements of the parts of the lower limbs, and the loads passing through them can all be altered as a result of prosthetic use.
Spatiotemporal parameters, being the simplest to measure, are also the most commonly studied and reported. These most frequently include walking speed, step length, cadence, and stride length (Sagawa et al. 2011). In general, amputees walk more slowly, having lower cadences and shorter stride and steps lengths. The said parameters also characterize a global predictor of gait (Montero-Odasso et al. 2004, 2005). Other spatiotemporal parameters for amputee gait analysis include step time ratio and stance time.
In terms of kinematics, a number of differences in movements are commonly observed. Pelvic range of motion is increased in the frontal plane in lower-limb amputees compared with healthy individuals. At slow walking speed, a significant difference was found in the pelvic range of motion (ROM) compared with able-bodied subjects (Su et al. 2007). Lower-limb amputees lift the pelvis (hip hiking) on the swing leg; this motion is frequently seen in unilateral amputees and viewed as a compensatory mechanism for the incapability to dorsiflex the prosthetic ankle. Hip hiking serves to increase foot clearance and decrease the possibility of tripping; however, it can also increase metabolic energy and decrease gait efficiency (Sagawa et al. 2011). Bilateral hip hiking has been observed in persons with bilateral transtibial amputation, potentially resulting in higher energy expenditure than found in unilateral amputees (Su et al. 2007). Other kinematic gait asymmetries that have been reported include a higher range of motion at the prosthetic side hip and knee compared with the sound limb in transtibial amputees during walking (Bateni and Olney 2002).
While comparisons are often made between amputee and non-amputee gait, gait parameters are also commonly assessed in terms of asymmetry or differences between the two limbs or sides of the body. The gait patterns of a person with a unilateral lower-limb amputation are typically much more asymmetrical compared with that of healthy individuals, in terms of timing, joint angles, as well as loading patterns (Bateni and Olney 2002; Isakov et al. 2000). In particular, the prosthetic side step length tends to be longer than the sound limb because of the shorter stance time on the prosthetic side (Bateni and Olney 2002; Board et al. 2001; Isakov et al. 2000; McNealy and Gard 2008; Sanderson and Martin 1997; Andrysek et al. 2007). This seems to be at least partially attributed to the tendency for unilateral amputees to use their intact leg to compensate for the prosthesis’ deficiencies (Su et al. 2007). However, longer time spent loading the intact limb, often also at higher loads (Nolan and Lees 2000; Esposito et al. 2015), can be problematic toward the long-term health of the sound limb (Pinzur et al. 1991).
During the loading phase, knee flexion acts as a shock absorber that is vital in preventing wear and tear on lower-limb joints (Isakov et al. 2000). The magnitude of stance-phase knee flexion for able-bodied individuals or the sound side of lower-limb amputees is almost 15–18° during walking (Sagawa et al. 2011). For transtibial amputees, prosthetic side knee flexion is typically only 9–12° (Isakov et al. 2000; Powers et al. 1998; Su et al. 2007) and negative or absent for transfemoral amputees (Segal et al. 2006). Knee flexion can be affected by many factors, such as the type of socket (Isakov et al. 2000), barefoot or shoed walking (Han et al. 2003), and rehabilitation protocol (Sjödahl et al. 2002).
As to the extent to which prosthetic rehabilitation should aim to minimize gait deviations and asymmetries, this remains a bit of a point of controversy within the clinical and research community. Given the physical and functional differences between the intact and prosthetic legs, high symmetry levels in all gait parameters may not be attainable, and trade-offs need to be considered, as well as the biomechanical limitations of prosthetic components. Several studies have found higher reliance on the sound leg by increased loading and stance time, which was attributed to ankle loss in transtibial amputees (Lemaire and Fisher 1994; Melzer et al. 2001). Other studies, however, support the idea that amputees may not need to rely on the intact leg because of the compensatory mechanisms adopted by the amputated leg (Silverman et al. 2008). While the amputee-related literature is seeing an increasingly greater use of gait symmetry measures (Winter and Sienko 1988), a greater understanding may be needed as to the use of these metrics.
Numerous studies have aimed to understand the influence of different prosthetic components on the quality of gait patterns. Some studies reported the positive effects from certain prosthetic components. For instance, some prosthesis users stated more confidence with their prosthetic foot and applied less force on the sound limb (Van der Linden et al. 1999). The use of a proper socket and appropriate fitting enabled a reduced degree of gait asymmetry by improved control of the prosthesis position (Board et al. 2001). The use of different knee mechanisms has been shown to influence a number of gait parameters, such as gait velocity (Furse et al. 2011) as well as kinematic and kinetics (Thiele et al. 2014; Taheri and Karimi 2012; Kaufman et al. 2012; Andrysek et al. 2007).
Gait Measurement Techniques
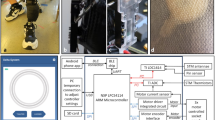
A variety of techniques are available for use depending on the gait measures of interest, the accuracy of measurement required, and resources available. Many clinicians rely on observational gait assessments, requiring minimal resources and time to identify spatiotemporal and kinematic gait deviations. However, more objective and accurate methods are typically incorporated when conducting research. Most commonly utilized is the instrumented gait lab, comprised of optical means for tracking movements of defined parts of the body in three dimensions (Fig. 5). Such systems capture spatiotemporal and kinematic measurements of body segments, and when combined with force plate data, kinetic measures, including joint moments and powers, can also be derived. Many researchers have used 3D motion analysis to investigate the gait parameters of transtibial amputees during different activities using various prosthetic components (Bateni and Olney 2002; Rusaw and Ramstrand 2010; Sanderson and Martin 1997).
3D motion analysis with reflective markers (Image on left adopted from Russell et al. (2006))
Depending on the specific research objectives, gait laboratory measurements may be augmented by other approaches. For example, where the interest exists to measure the pressures on the plantar foot, or within the socket/limb interface, various pressure transducers can be incorporated at these regions of the body. Inertial-based measurement unit (IMU) similarly can provide important information about the relative movements of the limbs, or gait events of features, such as heel strike and toe off , or terminal swing impact (Boutaayamou et al. 2015; Furse et al. 2011).
Gait laboratories are of particular importance in the study of the influences of socket and suspension. One example relates to the quantification of pistoning (Eshraghi et al. 2012). Common methods of measuring pistoning movement of the stump or the position of the bone include radiography (Narita et al. 1997; Söderberg et al. 2003; Papaioannou et al. 2010), photographic methods (Gholizadeh et al. 2011), motion analysis techniques or marker-based methods (Childers and Siebert 2015; Gholizadeh et al. 2012b), spiral computerized tomography (Madsen et al. 2000), and photoelectric sensors (Sanders et al. 2006b).
Another important area of measurement is interfacial pressures. Transducers embedded into the socket or thin sensor pads inserted between the skin and liner/socket are typically used to measure pressure (Williams et al. 1992; Polliack et al. 2000). The pressures at the socket/limb interface can vary considerably among individuals, as well as the location within the socket. Moreover, pressure levels are influenced by the ambulation task or walking style, socket fit, residual limb shape, and prosthetic alignment, as well as the socket, liner, and suspension accessories used (Dou et al. 2006; Jia et al. 2004; Mak et al. 2001; Eshraghi et al. 2013b).
Prosthesis/Limb Interfaces and Gait/Mobility
A large body of research has aimed to assess the influence of various prosthetic components on the gait of lower-limb amputees (Goujon et al. 2006; Schmalz et al. 2002; Torburn et al. 1995; Van der Linden et al. 1999). Some of the most commonly and frequently studied components include foot-ankle devices and knee joint mechanisms. Despite their important role in gait and mobility, prosthetic sockets and suspension systems have received more modest attention in terms of the research literature.
Fit of the residuum inside the prosthetic socket and effectiveness of prosthetic suspension (measured primarily in terms of pistoning, pressure distributions on the limb) have been associated, albeit primarily indirectly, with changes in gait patterns and energy consumption during ambulation (Baars and Geertzen 2005; Bateni and Olney 2002; Isakov et al. 2000; Sanderson and Martin 1997). For example, the TSB socket having more uniform contact pressure has been found to improve gait by decreasing pistoning during walking (Hachisuka et al. 1998b; Kristinsson 1993; Narita et al. 1997; Yigiter et al. 2002). In contrast, pin/lock suspension systems have been found to cause pain and discomfort inside the prosthetic socket due to increased pistoning, leading to long-term skin changes and pain (Beil and Street 2004).
A recent review of research literature reported the main studies that evaluated the effect of transtibial socket design on gait variables (Safari and Meier 2015). The findings suggest that prosthetic socket design, and in particular socket suspension, has an effect on gait symmetry. In a PTB socket, a sleeve or a supracondylar wedge can improve gait symmetry (Wirta et al. 1990). A TSB socket further improves gait symmetry over the PTB socket (Yigiter et al. 2002), and the highest symmetry is achieved with vacuum-assisted suction sockets (Board et al. 2001). On the other hand, the type of suspension provided by the liner material (urethane vs silicone) and the elastomeric liner (Seal-In vs sleeve suspension) showed no effect on gait parameters (Åström and Stenström 2004).
There is evidence that the vacuum-assisted sockets can increase stance duration symmetry and step length compared with the TSB sockets, possibly due to improved proprioception and suspension (Safari and Meier 2015). These sockets potentially control residual limb volume loss over long periods of use and promote wound healing (Gerschutz et al. 2010), potentially by producing a negative interface pressure during swing phase and small positive interface pressure during stance phase, absorbing fluid into the residual limb, particularly in a more conical residuum (Beil et al. 2002).
Stance time and single-limb support time were higher on the non-amputated side with the PTB sockets and a SACH foot, while the prosthetic side exhibited higher step length, step time, and swing time (Isakov et al. 2000). The knee angle at heel strike was larger in the prosthetic limb than in the non-amputated limb. The maximum swing knee flexion and knee flexion during loading response and at toe off were not significantly different between the intact and prosthetic limbs, but suspension type was not mentioned. It is however unclear from this study to what extent these gait differences can be attributed to the prosthetic foot or socket.
In a single-subject case report, Rogers et al. (2008) compared gait parameters of a participant wearing three different vacuum-assisted suction sockets: one conventional socket and two with different wall-compliant features over the fibular head and distal tibia (Rogers et al. 2008). The participant’s walking speed and cadence were highest when using the socket with the most compliant features and associated with lower inter-socket pressures by up to 50 percent. GRFs were, however, found to be similar for all three sockets. While this pilot study offers interesting insights into the influence of socket compliance on spatiotemporal gait parameters, the potential root of this relationship remains unclear, as does the applicability of the findings to the general amputee population.
Residuum discomfort may cause changes in gait parameters, because the amputee becomes reluctant to bear load over the prosthetic socket during walking. The Seal-In suspension can relieve the distal end pressure by applying more load to the proximal tissues of the residual limb. Both pin/lock and Seal-In liners control pistoning; however, the Seal-In liner may limit pistoning more successfully (Gholizadeh et al. 2012a, b). Recently, Bruneli et al. (2013) reported that the Seal-in liner caused a reduction in the energy cost of walking compared with the suction socket and sleeve, especially when walking on a slope. Furthermore, amputees could walk faster with the Seal-In suspension system (Brunelli et al. 2013).
The direct effect of socket or interface properties on mobility variables has been rarely studied. In one research, the thickness of prosthetic gel liners (a thin 3-mm liner and a thick 9-mm liner) was reported to affect gait variables (Boutwell et al. 2012). The joint angles and ground reaction forces as well as speed of walking were evaluated, but the discussion mainly focused on walking speed. No differences were found in the magnitudes of prosthetic-side pelvic obliquity or stance-phase knee flexion between liners nor in the peak fore-aft GRF during weight acceptance. Also, the timing of the peak vertical GRF was unaffected during weight acceptance, but the magnitude of this peak was significantly higher with the 9-mm liner. The self-selected walking speed did not change. The interface between the residual limb and socket may allow relative translations and rotations during activities such as walking, which may be increased by high compliance from the combined compression of gel liner and residuum soft tissue. The thicker gel liner could potentially allow greater relative motion between the residual limb and the socket, which subjects may have perceived as less stable or secure (Boutwell et al. 2012).
In conclusion, many different related parameters have been reported to assess the mobility performance of prosthetic components, including sockets and suspension systems. However, the majority has not been explored in detail, and the diversity of outcomes to designate the gait of lower-limb amputees remains a challenge, since limited consensus among researchers and clinicians exists about the important aspects of gait. Based on the literature, the analyses of gait in transtibial amputees provide reliable and useful information about walking strategies. Nevertheless, further studies are needed to evaluate the influence of prosthetic socket fit and design on mobility more profoundly and for different levels of amputation.
Future Directions
It is well established that socket design and fit strongly impact the quality of mobility among lower-limb prosthesis users. Developing better sockets and interfaces requires understanding of the clinical problems that persist and need to be addressed. Moreover, scientific and technological advancements are needed in developing the tools that can aid in understanding of the biomechanics of amputee gait and mobility and facilitating the means by which more effective interface designs can be achieved.
To solve the volume change and its effect on mobility, experimental approaches include the use of bladders within the socket that are filled with fluid or air once the limb loses volume (Sanders et al. 2006a; Greenwald et al. 2003; Ogawa et al. 2008). However, challenges with such systems often lie in their complexity and increased cost as well as maintenance requirements. Even though the VASS system has been shown to have benefits for amputees, there is still gap in the literature, particularly with regard to the kinetic, kinematic, and temporal characteristics of gait.
It is worth emphasizing here that the method of socket design and fabrication has a tremendous effect on the fit. An important step in the fabrication process of sockets is to accurately capture the shape of the residual limb. Digitization of the limb shape is continually improving with advancements in affordable optics and software that facilitate effective post-processing and rectification of the shape. While these approaches and tools are becoming ever more viable, practical, and useful, significant strides are also being made in the utilization of digitized data to directly fabricate sockets. Additive manufacturing, including selective laser sintering (SLS) and fused deposition modeling (FDM), is starting to play a role in the fabrication of orthotics, and work is ongoing to extend application to prosthetic sockets as well. Additive manufacturing presents a number of potential benefits, such as the ability to reproduce identical devices, utilization of complex geometries, and the use of integrated compliant features to improve and fit and comfort of the prosthesis (Faustini et al. 2005; Rogers et al. 2008). However, a number of challenges also exist with the direct fabrication of sockets using additive manufacturing. While a variety of materials can be applied for additive manufacturing, the use of composite and reinforced materials that provide high strength-to-weight ratios has limitations. Bonding between layers of the deposited material and the inability of reinforcing material to flow between the layers make it difficult to achieve comparable strength levels of socket structures that are made with conventional methods. While these technical challenges are primarily associated with the FDM, limitation of the SLS currently lies in a much higher fabrication cost, compared with the FDM as well as conventional manual methods (Telfer et al. 2012). In summary, the use of additive manufacturing for custom fabrication of prosthetic sockets is becoming more and more of a reality; however, clinical, technical, and financial issues still need to be addressed before these techniques can be made viable for mainstream use (Jin et al. 2015).
One procedure that has the potential to eliminate the need for conventional socket systems altogether is bone anchorage (Fig. 6). Osseointegration of external prostheses was introduced in Sweden in 1990 and has been studied and developed for the last 25 years (Hagberg and Brånemark 2009). A titanium implant provides the anchorage by the formation of bony tissue around it without growth of fibrous tissue at the bone-implant interface. The conventional socket and suspension accessories are not needed anymore as the prosthesis is attached directly to the bone. There are studies showing advantages of this method over the use of standard socket interfaces (Van de Meent et al. 2013). Among these are improved gait (Frossard et al. 2010), reduced skin issues, improved stability and comfort (Hagberg et al. 2005, 2008), easier donning and doffing, excellent suspension, unrestricted hip movement, and better body perception (Lundberg et al. 2011) and quality of life. Disadvantages include long rehabilitation process, risk of infection, risk of fractures and loosening of the implant, poor cosmesis of the permanent abutment, limits on high-impact activities such as running or jumping, and the need for daily care of the abutment skin area. Hence, currently the procedure is mainly recommended as an option for transfemoral amputees that experience major problems with conventional sockets. However, if the costs of care and postoperative management issues can be addressed, including but not limited to infection and technical problems, osseointegration may become a more mainstream part of care in near future.
Direct attachment of prosthesis to skeleton by an intramedullary implant into the femur (Van de Meent et al. 2013)
The influence of prosthetic socket design and fit on gait and mobility is an important topic, and as such it has been the sole focus of this chapter. Typically, the primary goal of providing rehabilitative care and a prosthetic limb to an individual with a lower-limb amputation is to facilitate functional mobility. And, the means and quality of the prosthesis as well as body interface are arguably the most important prosthesis-related parts of this rehabilitation process. The published literature covered in this chapter provides evidence and new insights about the effects that both conventional and more contemporary socket and suspension systems have on aspects of gait as well as mobility function. A better understanding can be gained from these studies to help inform clinicians and other rehabilitation professionals toward implementing evidence-based practices and achieving better rehabilitation care and patient outcomes. The clinical evidence is by no means perfect or complete, but it does provide some initial clues about how different interface systems affect biomechanics as well as gait and mobility function. Therefore, some guidance as to how these systems might be most appropriately and effectively utilized as part of clinical care is afforded. However, further research and evidence is needed, considering the variety of patient demographics, outcome measures, and the every-emerging waves of new prosthetic technologies. It is hoped that readers of this chapter have been provided with an adequate understanding of the topic, including where the gaps in knowledge still lie, to better inform their works in the areas of research, product development, education, or clinical care.
References
Abu Osman N, Spence W, Solomonidis S, Paul J, Weir A (2010) The patellar tendon bar! Is it a necessary feature? Med Eng Phys 32(7):760–765
Alvarez-Camacho M, Urrusti J, Acero MC, Galván D-GC, Rodriguez-Reyes G, Mendoza-Cruz F (2014) Device to assess in-socket pressure distribution for partial foot amputation. Rev Invest Clin 66:S131–S141
Andrysek J, Redekop S, Naumann S (2007) Preliminary evaluation of an automatically stance-phase controlled pediatric prosthetic knee joint using quantitative gait analysis. Arch Phys Med Rehabil 88(4):464–470
Åström I, Stenström A (2004) Effect on gait and socket comfort in unilateral trans-tibial amputees after exchange to a polyurethane concept. Prosthetics Orthot Int 28(1):28–36
Baars E, Geertzen J (2005) Literature review of the possible advantages of silicon liner socket use in trans-tibial prostheses. Prosthetics Orthot Int 29(1):27–37
Bateni H, Olney SJ (2002) Kinematic and kinetic variations of below-knee amputee gait. JPO: J Prosthet Orthot 14(1):2–10
Beil TL, Street GM (2004) Comparison of interface pressures with pin and suction suspension systems. J Rehabil Res Dev 41(6):821–828
Beil TL, Street GM, Covey SJ (2002) Interface pressures during ambulation using suction and vacuum-assisted prosthetic sockets. J Rehabil Res Dev 39(6):693–700
Board W, Street G, Caspers C (2001) A comparison of trans-tibial amputee suction and vacuum socket conditions. Prosthetics Orthot Int 25(3):202–209
Boutaayamou M, Schwartz C, Stamatakis J, Denoël V, Maquet D, Forthomme B, Croisier J-L, Macq B, Verly JG, Garraux G (2015) Development and validation of an accelerometer-based method for quantifying gait events. Med Eng Phys 37(2):226–232
Boutwell E, Stine R, Hansen A, Tucker K, Gard S (2012) Effect of prosthetic gel liner thickness on gait biomechanics and pressure distribution within the transtibial socket. J Rehabil Res Dev 49(2):227–240
Brunelli S, Delussu AS, Paradisi F, Pellegrini R, Traballesi M (2013) A comparison between the suction suspension system and the hypobaric Iceross Seal-In® X5 in transtibial amputees. Prosthetics Orthot Int 37(6):436–444
Childers WL, Siebert S (2015) Marker-based method to measure movement between the residual limb and a transtibial prosthetic socket. Prosthetics Orthot Int 0309364615610660. 40(6):720–768
Commean PK, Smith KE, Vannier MW (1997) Lower extremity residual limb slippage within the prosthesis. Arch Phys Med Rehabil 78(5):476–485
Convery P, Murray K (2000) Ultrasound study of the motion of the residual femur within a trans-femoral socket during gait. Prosthetics Orthot Int 24(3):226–232
Dillon MP, Barker TM (2006) Can partial foot prostheses effectively restore foot length? Prosthetics Orthot Int 30(1):17–23
Dillon MP, Barker TM (2008) Comparison of gait of persons with partial foot amputation wearing prosthesis to matched control group: observational study. J Rehabil Res Dev 45(9):1317
Dou P, Jia X, Suo S, Wang R, Zhang M (2006) Pressure distribution at the stump/socket interface in transtibial amputees during walking on stairs, slope and non-flat road. Clin Biomech 21(10):1067–1073. https://doi.org/10.1016/j.clinbiomech.2006.06.004
Eshraghi A, Abu Osman NA, Gholizadeh H, Karimi M, Ali S (2012) Pistoning assessment in lower limb prosthetic sockets. Prosthetics Orthot Int 36(1):15–24
Eshraghi A, Abu Osman NA, Gholizadeh H, Ahmadian J, Rahmati B, Abas WABW (2013a) Development and evaluation of new coupling system for lower limb prostheses with acoustic alarm system. Scientific Reports 3. https://doi.org/10.1038/srep02270
Eshraghi A, Abu Osman NA, Gholizadeh H, Ali S, Saevarsson SK, Abas WABW (2013b) An experimental study of the interface pressure profile during level walking of a new suspension system for lower limb amputees. Clin Biomech 28(1):55–60. https://doi.org/10.1016/j.clinbiomech.2012.10.002
Esposito ER, Whitehead JMA, Wilken JM (2015) Sound limb loading in individuals with unilateral transfemoral amputation across a range of walking velocities. Clin Biomech 30(10):1049–1055
Fairley M (2004) MAS socket: a transfemoral revolution. O&P J 6. http://www.oandp.com/articles/2004-06_03.asp
Faustini MC, Crawford RH, Neptune RR, Rogers WE, Bosker G (2005) Design and analysis of orthogonally compliant features for local contact pressure relief in transtibial prostheses. J Biomech Eng 127(6):946–951
Fergason J, Smith DG (1999) Socket considerations for the patient with a transtibial amputation. Clin Orthop Relat Res 361:76–84
Fernández A, Formigo J (2005) Are Canadian prostheses used? A long-term experience. Prosthetics Orthot Int 29(2):177–181
Fillauer CE, Pritham CH, Fillauer KD (1989) Evolution and development of the silicone suction socket (3S) for below-knee prostheses. JPO: J Prosthet and Orthot 1(2):92–103
Frossard L, Hagberg K, Häggström E, Gow DL, Brånemark R, Pearcy M (2010) Functional outcome of transfemoral amputees fitted with an osseointegrated fixation: temporal gait characteristics. JPO: J Prosthet Orthot 22(1):11–20
Furse A, Cleghorn W, Andrysek J (2011) Improving the gait performance of nonfluid-based swing-phase control mechanisms in transfemoral prostheses. IEEE Trans Biomed Eng 58(8):2352–2359
Gerschutz MJ, Denune JA, Colvin JM, Schober G (2010) Elevated vacuum suspension influence on lower limb amputee’s residual limb volume at different vacuum pressure settings. JPO: J Prosthet Orthot 22(4):252–256
Gholizadeh H, Osman NAA, Lúvíksdóttir ÁG, Eshraghi A, Kamyab M, Abas WABW (2011) A new approach for the pistoning measurement in transtibial prosthesis. Prosthetics Orthot Int 35(4):360–364
Gholizadeh H, Abu Osman N, Kamyab M, Eshraghi A, Lúvíksdóttir A, Wan Abas WAB (2012a) Clinical evaluation of two prosthetic suspension systems in a bilateral transtibial amputee. Am J Phys Med Rehabil 91(10):894–898
Gholizadeh H, Abu Osman NA, Eshraghi A, Ali S, S’varsson SK, WAB WA, Pirouzi GH (2012b) Transtibial prosthetic suspension: less pistoning versus easy donning and doffing. J Rehabil Res Dev 49(9):1321–1330
Goujon H, Bonnet X, Sautreuil P, Maurisset M, Darmon L, Fode P, Lavaste F (2006) A functional evaluation of prosthetic foot kinematics during lower-limb amputee gait. Prosthetics Orthot Int 30(2):213–223
Greenwald RM, Dean RC, Board WJ (2003) Volume management: smart variable geometry socket (SVGS) technology for lower-limb prostheses. JPO: J Prosthet Orthot 15(3):107–112
Hachisuka K, Dozono K, Ogata H, Ohmine S, Shitama H, Shinkoda K (1998b) Total surface bearing below-knee prosthesis: advantages, disadvantages, and clinical implications. Arch Phys Med Rehabil 79(7):783–789
Hagberg K, Brånemark R (2009) One hundred patients treated with osseointegrated transfemoral amputation prostheses – rehabilitation perspective. J Rehabil Res Dev 46(3)
Hagberg K, Häggström E, Uden M, Brånemark R (2005) Socket versus bone-anchored trans-femoral prostheses: hip range of motion and sitting comfort. Prosthetics Orthot Int 29(2):153–163
Hagberg K, Brånemark R, Gunterberg B, Rydevik B (2008) Osseointegrated trans-femoral amputation prostheses: prospective results of general and condition-specific quality of life in 18 patients at 2-year follow-up. Prosthetics Orthot Int 32(1):29–41
Han TR, Chung SG, Shin HI (2003) Gait patterns of transtibial amputee patients walking indoors barefoot. Am J Phys Med Rehabil 82(2):96–100
Isakov E, Keren O, Benjuya N (2000) Trans-tibial amputee gait: time-distance parameters and EMG activity. Prosthetics Orthot Int 24(3):216–220
Jia X, Zhang M, Lee WC (2004) Load transfer mechanics between trans-tibial prosthetic socket and residual limb—dynamic effects. J Biomech 37(9):1371–1377
Jin Y-a, Plott J, Chen R, Wensman J, Shih A (2015) Additive manufacturing of custom orthoses and prostheses – a review. Procedia CIRP 36:199–204
Kahle JT, Highsmith MJ (2014) Transfemoral interfaces with vacuum assisted suspension comparison of gait, balance, and subjective analysis: ischial containment versus brimless. Gait Posture 40(2):315–320
Kaufman KR, Frittoli S, Frigo CA (2012) Gait asymmetry of transfemoral amputees using mechanical and microprocessor-controlled prosthetic knees. Clin Biomech 27(5):460–465
Klute GK, Berge JS, Biggs W, Pongnumkul S, Popovic Z, Curless B (2011) Vacuum-assisted socket suspension compared with pin suspension for lower extremity amputees: effect on fit, activity, and limb volume. Arch Phys Med Rehabil 92(10):1570–1575
Kristinsson Ö (1993) The ICEROSS concept: a discussion of a philosophy. Prosthetics Orthot Int 17(1):49–55
Laing S, Lee PV, Goh JC (2011) Engineering a trans-tibial prosthetic socket for the lower limb amputee. Ann Acad Med Singap 40(5):252
Lemaire ED, Fisher FR (1994) Osteoarthritis and elderly amputee gait. Arch Phys Med Rehabil 75(10):1094–1099
Lin C-C, Chang C-H, Wu C-L, Chung K-C, Liao I (2004) Effects of liner stiffness for trans-tibial prosthesis: a finite element contact model. Med Eng Phys 26(1):1–9
Ludwigs E, Bellmann M, Schmalz T, Blumentritt S (2010) Biomechanical differences between two exoprosthetic hip joint systems during level walking. Prosthetics Orthot Int 34(4):449–460
Lundberg M, Hagberg K, Bullington J (2011) My prosthesis as a part of me: a qualitative analysis of living with an osseointegrated prosthetic limb. Prosthetics Orthot Int 35(2):207–214
Madsen MT, Hailer J, Commean PK, Vannier MW (2000) A device for applying static loads to prosthetic limbs of transtibial amputees during spiral CT examination. J Rehabil Res Dev 37(4):383–387
Mak AF, Zhang M, Boone DA (2001) State-of-the-art research in lower-limb prosthetic biomechanics-socket interface: a review. J Rehabil Res Dev 38(2):161–174
McNealy LL, Gard SA (2008) Effect of prosthetic ankle units on the gait of persons with bilateral trans-femoral amputations. Prosthetics Orthot Int 32(1):111–126
Melzer I, Yekutiel M, Sukenik S (2001) Comparative study of osteoarthritis of the contralateral knee joint of male amputees who do and do not play volleyball. J Rheumatol 28(1):169–172
Montero-Odasso M, Schapira M, Varela C, Pitteri C, Soriano ER, Kaplan R, Camera LA, Mayorga L (2004) Gait velocity in senior people an easy test for detecting mobility impairment in community elderly. J Nutr Health Aging 8(5):340–343
Montero-Odasso M, Schapira M, Soriano ER, Varela M, Kaplan R, Camera LA, Mayorga LM (2005) Gait velocity as a single predictor of adverse events in healthy seniors aged 75 years and older. J Gerontol Ser A Biol Med Sci 60(10):1304–1309
Narita H, Yokogushi K, Shi S, Kakizawa M, Nosaka T (1997) Suspension effect and dynamic evaluation of the total surface bearing (TSB) trans-tibial prosthesis: a comparison with the patellar tendon bearing (PTB) trans-tibial prosthesis. Prosthetics Orthot Int 21(3):175–178
Nolan L, Lees A (2000) The functional demands on the intact limb during walking for active trans-femoral and trans-tibial amputees. Prosthetics Orthot Int 24(2):117–125
Ogawa A, Obinata G, Hase K, Dutta A, Nakagawa M (2008) Design of lower limb prosthesis with contact pressure adjustment by MR fluid. In: Engineering in Medicine and Biology Society, EMBS 2008. 30th Annual International Conference of the IEEE. IEEE, pp 330–333.
Papaioannou G, Mitrogiannis C, Nianios G, Fiedler G (2010) Assessment of amputee socket–stump–residual bone kinematics during strenuous activities using Dynamic Roentgen Stereogrammetric Analysis. J Biomech 43(5):871–878
Pinzur M, Asselmeier M, Smith D (1991) Dynamic electromyography in active and limited walking below-knee amputees. Orthopedics 14 (5):535–537; .Discussion 537–538
Pirouzi G, Abu Osman NA, Oshkour AA, Ali S, Gholizadeh H, Wan Abas WA (2014) Development of an air pneumatic suspension system for transtibial prostheses. Sensors 14(9):16754–16765
Polliack A, Sieh R, Craig D, Landsberger S, McNeil D, Ayyappa E (2000) Scientific validation of two commercial pressure sensor systems for prosthetic socket fit. Prosthetics Orthot Int 24(1):63–73
Powers CM, Rao S, Perry J (1998) Knee kinetics in trans-tibial amputee gait. Gait Posture 8(1):1–7
Radcliffe CW, Foort J, Inman VT, Eberhart H (1961) The patellar-tendon-bearing below-knee prosthesis. University of California, Biomechanics Laboratory
Rogers B, Bosker G, Faustini M, Walden G, Neptune RR, Crawford R (2008) Case report: variably compliant transtibial prosthetic socket fabricated using solid freeform fabrication. JPO: J Prosthet Orthot 20(1):1–7
Rusaw D, Ramstrand N (2010) Sagittal plane position of the functional joint centre of prosthetic foot/ankle mechanisms. Clin Biomech 25 (7):713–720. https://doi.org/10.1016/j.clinbiomech.2010.04.005
Russell KA, Palmieri RM, Zinder SM, Ingersoll CD (2006) Sex differences in valgus knee angle during a single-leg drop jump. J Athl Train 41(2):166–171
Safari MR, Meier MR (2015) Systematic review of effects of current transtibial prosthetic socket designs – part 2: quantitative outcomes. J Rehabil Res Dev 52(5):509–528
Sagawa Y, Turcot K, Armand S, Thevenon A, Vuillerme N, Watelain E (2011) Biomechanics and physiological parameters during gait in lower-limb amputees: a systematic review. Gait Posture 33(4):511–526
Sanders JE, Fatone S (2011) Residual limb volume change: systematic review of measurement and management. J Rehabil Res Dev 48(8):949
Sanders JE, Bell DM, Okumura RM, Dralle AJ (1998) Effects of alignment changes on stance phase pressures and shear stresses on transtibial amputees: measurements from 13 transducer sites. IEEE Trans Rehabil Eng 6(1):21–31
Sanders J, Jacobsen A, Fergason J (2006a) Effects of fluid insert volume changes on socket pressures and shear stresses: Case studies from two trans-tibial amputee subjects. Prosthetics Orthot Int 30(3):257–269
Sanders JE, Karchin A, Fergason JR, Sorenson EA (2006b) A noncontact sensor for measurement of distal residual-limb position during walking. J Rehabil Res Dev 43(4):509
Sanders JE, Harrison DS, Allyn KJ, Myers TR, Ciol MA, Tsai EC (2012) How do sock ply changes affect residual-limb fluid volume in people with transtibial amputation? J Rehabil Res Dev 49(2):241–256. https://doi.org/10.1682/jrrd.2011.02.0022
Sanders JE, Cagle JC, Harrison DS, Myers TR, Allyn KJ (2013) How does adding and removing liquid from socket bladders affect residual limb fluid volume? J Rehabil Res Dev 50(6):845
Sanders JE, Hartley TL, Phillips RH, Ciol MA, Hafner BJ, Allyn KJ, Harrison DS (2015) Does temporary socket removal affect residual limb fluid volume of trans-tibial amputees? Prosthetics Orthot Int. https://doi.org/10.1177/0309364614568413
Sanderson DJ, Martin PE (1997) Lower extremity kinematic and kinetic adaptations in unilateral below-knee amputees during walking. Gait Posture 6(2):126–136
Sansam K, Neumann V, O’Connor R, Bhakta B (2009) Predicting walking ability following lower limb amputation: a systematic review of the literature. J Rehabil Med 41(8):593–603
Schmalz T, Blumentritt S, Jarasch R (2002) Energy expenditure and biomechanical characteristics of lower limb amputee gait: The influence of prosthetic alignment and different prosthetic components. Gait Posture 16 (3):255-263. https://doi.org/10.1016/S0966-6362(02)00008-5
Segal AD, Orendurff MS, Klute GK, McDowell ML, Pecoraro JA, Shofer J, Czerniecki JM (2006) Kinematic and kinetic comparisons of transfemoral amputee gait using C-Leg and Mauch SNS prosthetic knees. J Rehabil Res Dev 43(7):857–870
Sewell P, Noroozi S, Vinney J, Andrews S (2000) Developments in the trans-tibial prosthetic socket fitting process: a review of past and present research. Prosthetics Orthot Int 24(2):97–107
Seymour R (2002) Prosthetics and orthotics: lower limb and spinal. Lippincott Williams & Wilkins, Philadelphia
Silverman AK, Fey NP, Portillo A, Walden JG, Bosker G, Neptune RR (2008) Compensatory mechanisms in below-knee amputee gait in response to increasing steady-state walking speeds. Gait Posture 28(4):602–609
Silver-Thorn MB, Steege JW, Childress DS (1996) A review of prosthetic interface stress investigations. J Rehabil Res Dev 33:253–266
Sjödahl C, Jarnlo G-B, Söderberg B, Persson B (2002) Kinematic and kinetic gait analysis in the sagittal plane of trans-femoral amputees before and after special gait re-education. Prosthetics Orthot Int 26(2):101–112
Smith DG, Michael JW, Bowker JH, Surgeons AAoO (2004) Atlas of amputations and limb deficiencies: surgical, prosthetic, and rehabilitation principles. American Academy of Orthopaedic Surgeons, Rosemont
Söderberg B, Ryd L, Persson BM (2003) Roentgen stereophotogrammetric analysis of motion between the bone and the socket in a transtibial amputation prosthesis: a case study. JPO: J Prosthet Orthot 15(3):95–99
Staats TB, Lundt J (1987) The UCLA total surface bearing suction below-knee prosthesis. Clin Prosthet Orthot 11(3):118–130
Su P-F, Gard SA, Lipschutz RD, Kuiken TA (2007) Gait characteristics of persons with bilateral transtibial amputations. J Rehabil Res Dev 44(4):491–501
Taheri A, Karimi MT (2012) Evaluation of the gait performance of above-knee amputees while walking with 3R20 and 3R15 knee joints. J Res Med Sci 17(3):258
Telfer S, Pallari J, Munguia J, Dalgarno K, McGeough M, Woodburn J (2012) Embracing additive manufacture: implications for foot and ankle orthosis design. BMC Musculoskelet Disord 13(1):1
Thiele J, Westebbe B, Bellmann M, Kraft M (2014) Designs and performance of microprocessor-controlled knee joints. Biomed Te/Biomed Eng 59(1):65–77
Torburn L, Powers CM, Guiterrez R, Perry J (1995) Energy expenditure during ambulation in dysvascular and traumatic below-knee amputees: a comparison of five prosthetic feet. J Rehabil Res Dev 32:111–111
Traballesi M, Delussu AS, Averna T, Pellegrini R, Paradisi F, Brunelli S (2011) Energy cost of walking in transfemoral amputees: comparison between Marlo Anatomical Socket and Ischial Containment Socket. Gait Posture 34(2):270–274
Traballesi M, Delussu A, Fusco A, Iosa M, Averna T, Pellegrini R, Brunelli S (2012) Residual limb wounds or ulcers heal in transtibial amputees using an active suction socket system. A randomized controlled study. Eur J Phys Rehabil Med 48(4):613–623
Van de Meent H, Hopman MT, Frölke JP (2013) Walking ability and quality of life in subjects with transfemoral amputation: a comparison of osseointegration with socket prostheses. Arch Phys Med Rehabil 94(11):2174–2178
Van der Linden M, Solomonidis S, Spence W, Li N, Paul J (1999) A methodology for studying the effects of various types of prosthetic feet on the biomechanics of trans-femoral amputee gait. J Biomech 32(9):877–889
Williams R, Porter D, Roberts V, Regan J (1992) Triaxial force transducer for investigating stresses at the stump/socket interface. Med Biol Eng Comput 30(1):89–96
Winter DA, Sienko SE (1988) Biomechanics of below-knee amputee gait. J Biomech 21(5):361–367
Wirta RW, Golbranson FL, Mason R, Calvo K (1990) Analysis of below-knee suspension systems: effect on gait. J Rehabil Res Dev 27(4):385–396
Yigiter K, Sener G, Bayar K (2002) Comparison of the effects of patellar tendon bearing and total surface bearing sockets on prosthetic fitting and rehabilitation. Prosthetics Orthot Int 26(3):206–212
Zaffer SM, Braddom RL, Conti A, Goff J, Bokma D (1999) Total hip disarticulation prosthesis with suction socket: report of two cases1. Am J Phys Med Rehabil 78(2):160–162
Zhang M, Turner-Smith A, Roberts V, Tanner A (1996) Frictional action at lower limb/prosthetic socket interface. Med Eng Phys 18(3):207–214
Zhang M, Turner-Smith A, Tanner A, Roberts V (1998) Clinical investigation of the pressure and shear stress on the trans-tibial stump with a prosthesis. Med Eng Phys 20(3):188–198
Author information
Authors and Affiliations
Corresponding author
Section Editor information
Rights and permissions
Copyright information
© 2018 Springer International Publishing AG, part of Springer Nature
About this entry
Cite this entry
Eshraghi, A., Andrysek, J. (2018). Influence of Prosthetic Socket Design and Fitting on Gait. In: Handbook of Human Motion. Springer, Cham. https://doi.org/10.1007/978-3-319-14418-4_76
Download citation
DOI: https://doi.org/10.1007/978-3-319-14418-4_76
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-14417-7
Online ISBN: 978-3-319-14418-4
eBook Packages: EngineeringReference Module Computer Science and Engineering