Abstract
Cirrhosis is a major cause of morbidity and mortality worldwide. In contrast with the traditional view that cirrhosis is irreversible, clinical and experimental studies suggest that the removal of the causative agent can lead to reversibility of early stages of cirrhosis. Patients with advanced fibrosis or cirrhosis may also benefit from targeted therapies that favor fibrosis resolution and restoration of a normal liver architecture. Cirrhosis is a dynamic process characterized by the accumulation of extracellular matrix proteins that distort the hepatic architecture by forming a fibrous scar and the subsequent development of nodules of regenerating hepatocytes. Regression of advanced liver fibrosis is associated with reabsorption of fibrous scar and the disappearance of collagen-producing myofibroblasts. To develop therapies that favor cirrhosis resolution, it is essential to identify the main molecular mechanisms that mediate the removal of the fibrosis scar. Key players in this process are hepatic stellate cells, macrophages, metalloproteinases, and their inhibitors. This chapter summarizes the current evidence that cirrhosis is potentially reversible, the mechanisms leading to fibrosis progression and resolution and the potential targeted therapies for patients with advanced fibrosis.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Cirrhosis is one of the main causes of morbidity and mortality worldwide. At early stages, liver diseases are mostly asymptomatic, so many patients are diagnosed upon the development of liver-related complications (i.e., ascites, variceal bleeding, etc.) [1]. In patients with established cirrhosis, the removal of the causative agent (i.e., response to viral hepatitis therapy, alcohol cessation, etc.) may lead to, at a certain degree, reversibility of the disease. This fact is related to the capability of the liver to dissolve the fibrous bands and restore a nearly normal liver architecture. While there is no doubt that even advanced fibrosis is reversible, it is uncertain if other abnormalities found in advanced cirrhosis (i.e., microthrombosis, avascular nodules, etc.) are reversible.
Liver fibrosis results from chronic damage to the liver with the accumulation of extracellular matrix (ECM) proteins, which is characteristic of most types of chronic liver diseases [2]. The main causes of fibrosis and cirrhosis in industrialized countries include hepatitis C infection (HCV), alcohol abuse, and nonalcoholic steatohepatitis (NASH). The accumulation of ECM proteins distorts the hepatic architecture by forming a fibrous scar and the subsequent development of nodules of regenerating hepatocytes defines cirrhosis. Cirrhosis produces hepatocellular dysfunction and increased intrahepatic resistance to blood flow, resulting in hepatic insufficiency and portal hypertension, respectively [3].
Advanced fibrosis and cirrhosis were historically thought to be passive and irreversible processes, due to the collapse of the hepatic parenchyma and its substitution by a collagen-rich tissue [4]. Currently, fibrosis is considered a model of the wound healing response to chronic liver injury [5]. Liver fibrosis received little attention until the 1980s, when hepatic stellate cells (HSCs) were identified as the main collagen-producing cells in the liver [6]. This cell type undergoes a dramatic phenotypic activation in chronic liver diseases with the acquisition of fibrogenic properties [7]. Besides HSCs, portal myofibroblasts and cells of bone marrow origin have been shown to have fibrogenic potential [8, 9]. At the clinical level, rapid and slower fibrosers were identified, and genetic and environmental factors influencing fibrosis progression have been partially described [10]. The demonstration that even advanced liver fibrosis and cirrhosis are potentially reversible has greatly stimulated researchers to identify targeted therapies [11]. Biotechnology and pharmaceutical companies are increasingly interested in developing antifibrotic programs, and clinical trials are currently underway. However, the most effective therapy to treat advanced fibrosis and cirrhosis is still to remove the causative agent [12]. A number of drugs are able to reduce the accumulation of scar tissue in experimental models of chronic liver injury. Lack of clinical trials is due to the need for long follow-up studies and liver biopsies and should be ameliorated by the current effort to develop noninvasive markers to assess liver fibrosis.
Pathogenesis of Cirrhosis
Early Phase: Liver Fibrogenesis
After an acute liver injury (e.g., viral hepatitis), parenchymal cells regenerate and replace the necrotic or apoptotic cells. This process is associated with an inflammatory response and a limited deposition of ECM. If the hepatic injury persists, this reparative process perpetuates. Eventually, liver regeneration fails and hepatocytes are substituted by abundant ECM including fibrillar collagen. The distribution of this fibrous material depends on the origin of the liver injury.
Liver fibrosis is associated with major alterations in both the quantity and composition of ECM [13]. In advanced stages, the liver contains approximately six times more ECM, including collagens (I, III, and IV), fibronectin, undulin, elastin, laminin, hyaluronan, and proteoglycans. Accumulation of ECM results from both increased synthesis and decreased degradation [14]. Decreased activity of ECM-removing matrix metalloproteinases (MMPs) is mainly due to an overexpression of their specific inhibitors (tissue inhibitors of metalloproteinases (TIMPs)). HSCs are the main ECM-producing cells in the injured liver [15]. In the normal liver, HSCs reside in the space of Disse and are a major storage site of vitamin A. Following chronic injury, HSCs activate or transdifferentiate into myofibroblast-like cells, acquiring contractile, pro-inflammatory, and fibrogenic properties [16]. Activated HSCs migrate and accumulate at the sites of tissue repair, secreting large amounts of ECM and regulating ECM degradation. Other cells like myofibroblasts [17] and cells from bone marrow origin [18]) can be a source of fibrogenic cells in the injured liver. The relative importance of each cell type in liver fibrogenesis may depend on the origin of the liver injury.
A complex interplay among different hepatic cell types takes place during hepatic fibrogenesis [19]. Damaged hepatocytes release reactive oxygen species (ROS) and fibrogenic mediators and induce the infiltration by inflammatory cells. Apoptosis of damaged hepatocytes stimulates the fibrogenic actions of liver myofibroblasts [20]. Inflammatory cells, either lymphocytes or polymorphonuclear cells, activate HSCs to secrete collagen [21]. Activated HSCs secrete inflammatory chemokines, express cell adhesion molecules, and modulate the activation of lymphocytes [22]. Therefore, a vicious circle in which inflammatory and fibrogenic cells stimulate each other is likely to occur [23]. Fibrosis is influenced by different T-helper (Th) subsets, with the Th2 response associated with more active fibrogenesis [24]. Kupffer cells are resident macrophages that play a major role in liver inflammation by releasing ROS and cytokines [25]. Finally, changes in the composition of the ECM can directly stimulate fibrogenesis . Type IV collagen, fibrinogen, and urokinase-type plasminogen activator stimulate resident HSCs by activating latent cytokines such as transforming growth factor beta 1 (TGFβ1) [26]. Fibrillar collagens can bind discoidin domain receptors in HSCs and stimulate collagen synthesis. Moreover, the altered ECM can serve as a reservoir for growth factors and MMPs [27].
Established Cirrhosis
Established cirrhosis results when bridging fibrosis is eventually accompanied by regenerative nodules [28] (Fig. 8.1). In early phases, incomplete septal cirrhosis can be found. It is characterized by the presence of very slender septa radiating from enlarged fields toward the center of the lobule. There are distended efferent vessels around the septum. This type of cirrhosis produces only portal hypertension, and liver failure is not usually observed. The prognosis of these patients is acceptable if the portal hypertension is controlled. If the cause of liver injury is not removed, the hepatic wound healing response to injury progresses and early cirrhosis develops. In this stage of the liver disease, thin fibrous septa with dissecting nodules are present. As liver damage progresses, wide scars containing clusters of regenerative hepatocytes commonly appear and advanced cirrhosis develops [29, 30]. This stage of the disease is characterized by the accumulation of abundant fibrillar collagen, which is resistant to the collagenolytic actions of MMPs. Moreover, advanced cirrhosis comprises major changes in hepatic microcirculation, endothelial integrity and function, and abnormal hepatocyte organization.
Fibrosis reversibility at different states of chronic liver disease. The capacity of the liver to reverse from fibrosis or cirrhosis to a nearly normal architecture depends on the stage of the liver disease. The genetic and environmental factors regulating fibrosis reversibility are known. While patients with moderate cirrhosis and early cirrhosis can fully reverse upon cessation of the cause of liver injury, the reversibility of patients with advanced cirrhosis can be hampered by cross-linking of collagen and the presence of avascular nodules. The degree of liver fibrosis can be estimated histologically (Metavir stages), by increase in portal pressure (hepatic venous pressure gradient (HVPG)) or by liver stiffness (in kPa)
Formation of nodules is the hallmark of advanced cirrhosis. They are divided into dissection and regenerative nodules [31]. Dissection nodules contain remnants of portal tracts and central veins. They contain thin fibrous septa as well as dilated sinusoids especially at their periphery, which appear like multiple central veins produced by the inflow of arterial blood from the surrounding wide scars. Regenerative nodules favored by the rich arterial blood of scar tissue arise in the midst of scars. They are round nodules with a fibrous pseudo capsule with bile ductules due to obstruction of bile flow [32]. Because of their size, they compress the vessels of the capsule, contributing to the perpetuation of the cirrhosis. Importantly, regenerative nodules may undergo dysplastic and malignant changes.
According to the degree of fibrosis and the type of nodules, cirrhosis can be classified into different progressive stages: incomplete septal cirrhosis (incomplete bridging fibrosis, no nodules), early cirrhosis (thin bridging fibrosis with dissecting nodules), moderately advanced cirrhosis (thick bridging fibrosis with dissecting nodules), and advanced cirrhosis (wide septa with regenerative hyperplastic nodules). Histopathologically, advanced cirrhosis can be divided into micro and macronodular [33]. Micronodular cirrhosis is characterized by uniformly small nodules (< 3 mm in diameter) and regular bands of connective tissue. Macronodular cirrhosis is characterized by nodules that vary in size (3 mm to 5 cm in diameter) and contain some normal lobular structure (portal tracts, terminal hepatic venules). Collapse of the normal liver architecture is suggested by the concentration of portal tracts within the fibrous scars. Regeneration in micronodular cirrhosis can result in macronodular or mixed cirrhosis. Conversion from micronodular to macronodular cirrhosis takes more than 2 years.
Vascular changes play a major role in the pathogenesis of advanced cirrhosis [28]. Complete septa may link central veins to central veins, creating anastomoses between draining vessels. Septa linking adjacent portal tracts create vascular anastomoses between afferent vessels of the portal tracts involved. Vascular structures in central–central and portal–portal septa are not the major determinants of a detrimental change in intrahepatic circulation [34]. The key phenomenon in the emergence of a truly cirrhotic state is the development of fibrous vascularized septa linking portal tracts and central veins. Therefore portal–central bridging fibrosis creates direct anastomoses between the afferent (hepatic artery, portal vein) and efferent (centrilobular veins) vessels of the liver, allowing a fraction of the blood to bypass the lobular parenchyma, without functionally contacting a metabolically active parenchyma. In advanced cirrhosis, most of the hepatic blood supply appears to pass through the liver via these channels [35, 36]. Further vascular changes in developing an established liver cirrhosis are due to vascular thrombosis . Thrombosis of medium and large portal veins and hepatic veins is a common occurrence in cirrhosis , and these lesions are important in causing progression of cirrhosis. Investigations on neo-angiogenesis in cirrhosis have focused attention on hypoxia of liver tissue [37]. Hypoxia may result from several mechanisms: impairment in sinusoidal permeability and perfusion, intrahepatic shunts, vasoconstriction, and thrombosis and capillarization of sinusoids. Liver tissue hypoxia aggravates fibrosis progression, so that fibrosis and hypoxia may aggravate each other in the presence of persistent parenchymal injury, leading to a vicious cycle that disrupts the normal tissue repair and thereby promotes the development and progression of cirrhosis [38].
In advanced cirrhosis, there is a local predominance of vasoconstrictors over vasodilators, resulting in a tonic contraction of perisinusoidal HSC cells that increase vascular resistance. Moreover, thrombosis in small vessels occurs and intrahepatic arterial shunts develop [39]. Hepatocytes proliferate in ischemic areas in a disorganized manner, forming regenerative nodules. Pressure in the portal venous system progressively increases, leading to the development of portocollateral veins and esophageal varices [40]. The resulting portal hypertension leads to splanchnic vasodilatation that increases hepatic venous blood flow. Systemic vascular resistance is decreased and eventually there is a marked activation of systemic vasoconstrictor systems that worsen portal hypertension and favor ascites formation. Hepatocellular function is progressively impaired and there is decreased function of the reticuloendothelial system leading to endotoxinemia and increased risk of bacterial infections [41]. Eventually, hepatocellular function fails, leading to severe coagulopathy and hepatic encephalopathy [42]. A profound circulatory dysfunction due to impaired myocardial function and decreased systemic vascular resistance is frequently seen. In very late stages of cirrhosis, renal vasoconstriction develops, leading to the hepatorenal syndrome [43]. In this phase of the disease, most patients die unless a liver transplantation is rapidly performed.
Reversibility of Advanced Fibrosis and Cirrhosis: Clinical Evidence
The reversibility of chronic liver diseases depends on the stage of the disease (Fig. 8.1). Thus, while advanced fibrosis and early cirrhosis may be reversible, reversal of advanced cirrhosis may be hampered by the presence of collagen cross-linking and avascular areas. Therefore, the current paradigm that cirrhosis is reversible should clearly be tempered. It is unclear if the abnormalities of the intrahepatic vasculature regress in human cirrhotic liver. The so-called veno-portal adhesions may persist even in cases of extensive fibrosis regression, and evident “arterialized” sinusoids appear in the context of intrahepatic arterio-venous shunts [44]. A better staging system of cirrhosis is clearly needed for prognostic purposes and to design prospective studies on cirrhosis reversal.
There are many clinical observations that the removal of the causative agent leads to improvement of liver fibrosis even in patients with F4 (cirrhosis) . This observation has been described in patients with alcohol-induced liver injury, chronic hepatitis C , B, and D, secondary biliary cirrhosis, NASH, and autoimmune hepatitis [11, 45–72] (Table 8.1). Obviously, reversal of advanced fibrosis is a slow process that may take months or even years. The time is probably influenced by the underlying cause of the liver disease and its severity. One of the limiting factors is the capacity of the chronically damaged liver to reabsorb scar tissue [73]. In patients with ongoing liver injury, the fibrosis scar is characterized by the presence of thin reticulin fibers and inflammatory cells. This thin fibrotic bands are probably fully reversible. In contrast, long standing fibrosis, which typically contains extensive collagen cross-linking by tissue transglutaminase, presence of elastin, dense acellular/paucicellular ECM, and decreased expression and/or activity of specific metalloproteinases, is largely irreversible [74, 75]. This scenario is probably present in patients with very advanced fibrosis after decades of continuous liver injury. Moreover, there is mounting evidence that long-term fibrogenesis occurring in humans is much less reversible than in rodents, so the current optimism about full reversibility of cirrhosis should be tempered [76].
Mechanisms Involved in Fibrosis Resolution
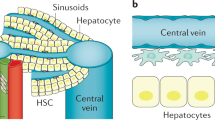
The mechanisms of resolution of advanced fibrosis have been largely studied in animal models, while data from humans are scarce. For architectural remodeling to occur, the balance between the factors promoting matrix accumulation (synthesis of matrix by fibrogenic factors) and remodeling (matrix breakdown mediated by MMPs) needs to alter, shifting from one that favors matrix accumulation to one of net matrix degradation [77]. Restoration of fibrolytic activity is initiated upon suppression of hepatic TIMPs, following elimination of hepatic myofibroblasts by apoptosis, senescence, or reversion to a quiescent phenotype, suggesting that clearance of activated HSCs is a key step in the onset of fibrosis regression [78]. Recent studies suggest that among these potential outcomes, deactivation of myofibroblastic HSCs into a quiescent phenotype is the prevailing event in fibrosis resolution [79, 80]. Moreover, myeloid cell subsets (“restorative” macrophages and dendritic cells), which constitute a major source of MMP critical for fibrosis resolution, and endothelial cells, which maintain HSCs in a quiescent phenotype, have also been identified as contributing to the resolution of fibrosis (Fig. 8.2).
Cellular pathogenesis of fibrosis progression and resolution. In the normal liver, hepatic stellate cells (HSCs) display a quiescent phenotype. Continuous liver injury leads to a wound healing response with the infiltration of inflammatory cells that secrete a number of soluble factors and cytokines that lead to activation of HSCs into collagen-producing cells. In turn, activated HSCs perpetuate liver fibrogenesis and promote inflammation by secreting a number of profibrogenic mediators. If the causal agent is removed, fibrosis resolution initiates by stimulation of collagen degradation and removal of HSCs (either by apoptosis or by regression to quiescence). There are different sites during fibrogenesis and fibrosis resolution that represent potential sites for intervention. Agents capable of reducing HSCs’ accumulation or collagen synthesis or those that promote collagen degradation and/or HSCs’ apoptosis have been tested in experimental models in rodents. The usefulness and safety of most of these agents to reverse liver fibrosis should be tested in well-designed clinical trials
Increased Collagenolytic Activity
Fibrillar collagens (I and III) are degraded by interstitial MMPs. During fibrosis resolution, MMP activity increases due to a rapid decrease in the expression of TIMP-1. Partial degradation of fibrillar collagen occurs, and the altered interaction between activated HSCs and ECM favors apoptosis [75]. Removal of activated HSCs by apoptosis precedes fibrosis resolution. Stimulation of death receptors in activated HSCs and a decrease in survival factors, including TIMP-1, can precipitate HSC apoptosis [81]. However, reversibility may only be partial as regenerating nodules and alterations of hepatic microcirculation, both associated with advanced fibrosis, are difficult to revert.
HSC Apoptosis
Follow-up of rats exposed to carbon tetrachloride for 8 weeks has shown that the recovery phase is associated with an early decrease in hepatic TIMP-1 and a parallel decrease in the density of activated HSCs due to apoptosis. Experiments in TIMP-1 transgenic mice and with TIMP-1 scavengers demonstrated the causal relationship between hepatic TIMP-1 expression, failure of fibrolysis, and increased HSC survival [82]. Further studies identified nuclear factor-kappa B (NF-κB) as an important transcription factor in the upregulation of antiapoptotic genes in activated HSCs and showed that inhibitors of NF-κB signaling induce apoptosis of activated HSCs and reversal of fibrosis [83].
HSC Senescence
Senescent hepatic myofibroblasts may contribute to the regression of fibrosis because they stop proliferating, upregulate the expression of matrix degrading enzymes, and downregulate the expression of ECM proteins. Moreover, senescent hepatic myofibroblasts can be cleared by natural killer cells [84]. Thus, senescence of hepatic myofibroblasts can prevent further proliferation of these ECM-producing cells, promote ECM degradation, and accelerate myofibroblast clearance from the site of injury.
Reversion of HSC Phenotype to an Inactivated State
Recent cell tracking studies have further documented earlier in vitro studies showing that activated HSCs can undergo deactivation to a quiescent phenotype following cessation of liver injury [79, 80]. However, reverted HSCs do not reacquire all of the characteristics of quiescent cells, but rather retain an activated intermediate state with enhanced susceptibility to a fibrogenic stimulus. These data raise the intriguing possibility that reverted HSCs contribute to fibrosis reversal but may promote more rapid and severe fibrosis progression upon recurrence of liver injury.
Scar-Associated Macrophages
Scar tissue contains numerous monocyte-derived macrophages. These monocyte-derived macrophages are a potent source of MMPs, including collagenases such as MMP13, gelatinases (MMPs 2 and 9) and elastases [85]. Besides these collagenases, recent data indicate that vascular endothelial growth factor (VEGF) also plays a role in fibrosis resolution. VEGF promotes sinusoidal permeability, monocyte-endothelial cell adhesion, and the resulting scar-associated macrophages accumulation necessary for fibrosis resolution. VEGF does indeed play a dual role in fibrosis and fibrosis resolution as it has previously been found to play a role in fibrogenesis via a pro-inflammatory effect acting primarily on endothelial cells. Work by a number of groups has demonstrated that macrophages are crucial to the resolution of fibrosis [86, 87]. The removal of the macrophage population at the onset of spontaneous fibrosis resolution in rodent models of liver injury prevents remodeling of fibrosis. Additionally, deletion of the macrophage population is associated with a critical drop in liver levels of key enzymes such as MMP13 and MMP12, identifying the macrophage as a crucial source of these enzymes in fibrosis resolution [88].
Can We Favor Cirrhosis and/or Advanced Fibrosis Resolution?
While the mechanisms and genetic and environmental factors regulating fibrosis progression are well characterized, the modulators of fibrosis reversibility are largely unknown. Clinical and translational studies should identify the main cellular and molecular mechanisms that mediate cirrhosis reversibility. These studies will lead to the identification of potential therapeutic targets to favor disease reversibility. As discussed earlier, regression of advanced fibrosis even at the stage of early cirrhosis can be achieved following treatment of the underlying cause in a variety of chronic liver diseases. However, despite the identification of numerous effective antifibrotic pharmacological targets in experimental models, no clinical translation has yet been achieved. This lack of translation may be due to the fact that fibrosis progression is very slow in humans and therefore long clinical trials (i.e., 3–5 years) are required to demonstrate antifibrotic effects. Moreover, there is a clear need for noninvasive markers of fibrosis progression/regression, which may allow precise monitoring of the evolution of fibrosis. Altogether, therapeutic trials primarily focused on antifibrotic endpoints remain scarce and have thus far failed to demonstrate any benefit. The pathways and drivers mediating fibrosis resolution are complex and may differ at different stages of cirrhosis. An additional obstacle is that patients with advanced fibrosis and/or cirrhosis are particularly susceptible to develop hepatotoxic effects, as well as liver cancer , which is a concern to develop long-term clinical trials.
Several therapeutic strategies have been tested to reduce liver fibrosis in patients with chronic liver diseases. Corticosteroids exert antifibrogenic actions in autoimmune hepatitis and acute alcoholic hepatitis [89]. Other anti-inflammatory therapies like colchicine or interleukin-10 have been tested but they induced undesirable side effects. A different strategy targets activation and proliferation of HSCs. These strategies include antioxidants (e.g., vitamin E, silimarin, phosphatidylcholine, S-adenosil-metionin) as well as modulators of intracellular pathways of HSCs biological responses [90, 91]. A promising strategy is to inhibit the renin–angiotensin system inhibition, specifically by using angiotensin II receptor type 1 antagonists (AT1) [92]. These strategies have been successful for the treatment of cardiac fibrosis as well as renal fibrosis. Administration of inhibitors of the renin–angiotensin system to treat arterial hypertension in transplanted patients showed a slower progression of hepatic fibrogenesis . Conversely, administration of losartan for 18 months showed that it is well tolerated in chronic hepatitis C patients while diminishing fibrogenic gene expression [93].
The use of different therapeutic strategies may differ according to the etiology of the liver disease. In patients with hepatitis C, therapy with interferon-γ and ribavirin induces antifibrogenic effects regardless of their antiviral action [51]. However, interferon-γ has important side effects [94]. The recent development of highly active oral therapies against HCV opens a new era in the field of fibrosis resolution. These drugs are well tolerated, suggesting that even patients with advanced cirrhosis would clear the viral infection in the coming years. Studies identifying key mediators of cirrhosis reversibility are anticipated in the coming years. Such studies can help in the identification of new targeted therapies that favor fibrosis reversibility. Regarding patients with NASH, therapies increasing insulin sensitivity (e.g., thiazolidinediones and statins) have been shown to decrease the degree of fibrosis [95, 96]. Other therapies that are effective in experimental NASH include profibrogenic cytokines inhibitors (TGFβ1, platelet-derived growth factor(PDGF)) [97–99], chemokine receptors antagonists [88], interleukin-10 [100, 101], and cannabinoid receptor blockers [102]. However, their use in humans is hampered by undesirable side effects.
References
Bataller R, Brenner DA. Liver fibrosis. J Clin Invest. 2005;115:209–18.
Friedman SL. Liver fibrosis—from bench to bedside. J Hepatol. 2003;38 Suppl 1:S38–53.
Gines P, Cardenas A, Arroyo V, Rodes J. Management of cirrhosis and ascites. N Engl J Med. 2004;350:1646–54.
Klion FM, Schaffner F. Hemochromatosis following hepatitis in a patient with systemic iron overload. Arch Pathol. 1968;86:342–7.
Albanis E, Friedman SL. Hepatic fibrosis. Pathogenesis and principles of therapy. Clin Liver Dis. 2001;5:315–34, v–vi.
Friedman SL, Roll FJ, Boyles J, Bissell DM. Hepatic lipocytes: the principal collagen-producing cells of normal rat liver. Proc Natl Acad Sci U S A. 1985;82:8681–5.
Geerts A. History, heterogeneity, developmental biology, and functions of quiescent hepatic stellate cells. Semin Liver Dis. 2001;21:311–35.
Ramadori G, Saile B. Portal tract fibrogenesis in the liver. Lab Invest. 2004;84:153–9.
Forbes SJ, Russo FP, Rey V, Burra P, Rugge M, Wright NA, Alison MR. A significant proportion of myofibroblasts are of bone marrow origin in human liver fibrosis. Gastroenterology. 2004;126:955–63.
Bataller R, North KE, Brenner DA. Genetic polymorphisms and the progression of liver fibrosis: a critical appraisal. Hepatology. 2003;37:493–503.
Hammel P, Couvelard A, O'Toole D, Ratouis A, Sauvanet A, Flejou JF, Degott C, et al. Regression of liver fibrosis after biliary drainage in patients with chronic pancreatitis and stenosis of the common bile duct. N Engl J Med. 2001;344:418–23.
Bataller R, Brenner DA. Hepatic stellate cells as a target for the treatment of liver fibrosis. Semin Liver Dis. 2001;21:437–51.
Benyon RC, Iredale JP. Is liver fibrosis reversible? Gut 2000;46:443–6.
Arthur MJ. Fibrogenesis II. Metalloproteinases and their inhibitors in liver fibrosis. Am J Physiol Gastrointest Liver Physiol. 2000;279:G245–9.
Gabele E, Brenner DA, Rippe RA. Liver fibrosis: signals leading to the amplification of the fibrogenic hepatic stellate cell. Front Biosci. 2003;8:d69–77.
Milani S, Herbst H, Schuppan D, Kim KY, Riecken EO, Stein H. Procollagen expression by nonparenchymal rat liver cells in experimental biliary fibrosis. Gastroenterology. 1990;98:175–84.
Kinnman N, Housset C. Peribiliary myofibroblasts in biliary type liver fibrosis. Front Biosci. 2002;7:d496–503.
Suskind DL, Muench MO. Searching for common stem cells of the hepatic and hematopoietic systems in the human fetal liver: CD34 + cytokeratin 7/8 + cells express markers for stellate cells. J Hepatol. 2004;40:261–8.
Kmiec Z. Cooperation of liver cells in health and disease. Adv Anat Embryol Cell Biol. 2001;161:Iii–xiii, 1–151.
Canbay A, Friedman S, Gores GJ. Apoptosis: the nexus of liver injury and fibrosis. Hepatology 2004;39:273–8.
Casini A, Ceni E, Salzano R, Biondi P, Parola M, Galli A, Foschi M, et al. Neutrophil-derived superoxide anion induces lipid peroxidation and stimulates collagen synthesis in human hepatic stellate cells: role of nitric oxide. Hepatology. 1997;25:361–7.
Vinas O, Bataller R, Sancho-Bru P, Gines P, Berenguer C, Enrich C, Nicolas JM, et al. Human hepatic stellate cells show features of antigen-presenting cells and stimulate lymphocyte proliferation. Hepatology. 2003;38:919–29.
Maher JJ. Interactions between hepatic stellate cells and the immune system. Semin Liver Dis. 2001;21:417–26.
Shi Z, Wakil AE, Rockey DC. Strain-specific differences in mouse hepatic wound healing are mediated by divergent T helper cytokine responses. Proc Natl Acad Sci U S A. 1997;94:10663–8.
Naito M, Hasegawa G, Ebe Y, Yamamoto T. Differentiation and function of Kupffer cells. Med Electron Microsc. 2004;37:16–28.
Gressner AM, Weiskirchen R, Breitkopf K, Dooley S. Roles of TGF-beta in hepatic fibrosis. Front Biosci. 2002;7:d793–807.
Olaso E, Ikeda K, Eng FJ, Xu L, Wang LH, Lin HC, Friedman SL. DDR2 receptor promotes MMP-2-mediated proliferation and invasion by hepatic stellate cells. J Clin Invest. 2001;108:1369–78.
Roskams T, Baptista A, Bianchi L, Burt A, Callea F, Denk H, De Groote J, et al. Histopathology of portal hypertension: a practical guideline. Histopathology. 2003;42:2–13.
Sherlock S, Dooley J. Diseases of the liver and biliary system. Blackwell Science Ltd; Hoboken, NJ 2002.
Nevens F, Staessen D, Sciot R, Damme Van B, Desmet V, Fevery J, De Groote J, et al. Clinical aspects of incomplete septal cirrhosis in comparison with macronodular cirrhosis. Gastroenterology. 1994;106:459–63.
Anthony PP, Ishak KG, Nayak NC, Poulsen HE, Scheuer PJ, Sobin LH. The morphology of cirrhosis. Recommendations on definition, nomenclature, and classification by a working group sponsored by the World Health Organization. J Clin Pathol. 1978;31:395–414.
Goldblatt PJ, Gunning WT 3rd. Ultrastructure of the liver and biliary tract in health and disease. Ann Clin Lab Sci. 1984;14:159–67.
Wanless IR. Micronodular transformation (nodular regenerative hyperplasia) of the liver: a report of 64 cases among 2500 autopsies and a new classification of benign hepatocellular nodules. Hepatology. 1990;11:787–97.
Huet PM, Pomier-Layrargues G, Villeneuve JP, Varin F, Viallet A. Intrahepatic circulation in liver disease. Semin Liver Dis. 1986;6:277–86.
Oikawa H, Masuda T, Sato S, Yashima A, Suzuki K, Sato S, Satodate R. Changes in lymph vessels and portal veins in the portal tract of patients with idiopathic portal hypertension: a morphometric study. Hepatology. 1998;27:1607–10.
Malmqvist U. Effects of long-term portal hypertension on structure, active force and content of contractile and structural proteins in smooth muscle of the rat portal vein. Acta Physiol Scand. 1994;150:171–179.
Rosmorduc O, Housset C. Hypoxia: a link between fibrogenesis, angiogenesis, and carcinogenesis in liver disease. Semin Liver Dis. 2010;30:258–70.
Cannito S, Paternostro C, Busletta C, Bocca C, Colombatto S, Miglietta A, Novo E, et al. Hypoxia, hypoxia-inducible factors and fibrogenesis in chronic liver diseases. Histol Histopathol. 2014;29:33–44.
Groszmann RJ, Abraldes JG. Portal hypertension: from bedside to bench. J Clin Gastroenterol. 2005;39:S125–30.
Foutch PG, Sullivan JA, Gaines JA, Sanowski RA. Cutaneous vascular spiders in cirrhotic patients: correlation with hemorrhage from esophageal varices. Am J Gastroenterol. 1988;83:723–6.
Deaciuc IV, Spitzer JJ. Hepatic sinusoidal endothelial cell in alcoholemia and endotoxemia. Alcohol Clin Exp Res. 1996;20:607–14.
Baltzan MA, Olszewski J, Zervas N. Chronic porto-hepatic encephalopathy. J Neuropathol Exp Neurol. 1957;16:410–21.
Papper S. The hepatorenal syndrome. Clin Nephrol. 1975;4:41–4.
Pinzani M, Vizzutti F. Fibrosis and cirrhosis reversibility: clinical features and implications. Clin Liver Dis. 2008;12:901–13, x.
Pares A, Caballeria J, Bruguera M, Torres M, Rodes J. Histological course of alcoholic hepatitis. Influence of abstinence, sex and extent of hepatic damage. J Hepatol. 1986;2:33–42.
Pessione F, Ramond MJ, Peters L, Pham BN, Batel P, Rueff B, Valla DC. Five-year survival predictive factors in patients with excessive alcohol intake and cirrhosis. Effect of alcoholic hepatitis, smoking and abstinence. Liver Int. 2003;23:45–53.
Bardou-Jacquet E, Legros L, Soro D, Latournerie M, Guillygomarc'h A, Le Lan C, Brissot P, et al. Effect of alcohol consumption on liver stiffness measured by transient elastography. World J Gastroenterol. 2013;19:516–22.
Poynard T, McHutchison J, Manns M, Trepo C, Lindsay K, Goodman Z, Ling MH, et al. Impact of pegylated interferon alfa-2b and ribavirin on liver fibrosis in patients with chronic hepatitis C. Gastroenterology. 2002;122:1303–13.
Lissen E, Clumeck N, Sola R, Mendes-Correa M, Montaner J, Nelson M, DePamphilis J, et al. Histological response to pegIFNalpha-2a (40KD) plus ribavirin in HIV-hepatitis C virus co-infection. AIDS. 2006;20:2175–81.
Heathcote EJ, Shiffman ML, Cooksley WG, Dusheiko GM, Lee SS, Balart L, Reindollar R, et al. Peginterferon alfa-2a in patients with chronic hepatitis C and cirrhosis. N Engl J Med. 2000;343:1673–80.
Camma C, Di Bona D, Schepis F, Heathcote EJ, Zeuzem S, Pockros PJ, Marcellin P, et al. Effect of peginterferon alfa-2a on liver histology in chronic hepatitis C: a meta-analysis of individual patient data. Hepatology. 2004;39:333–42.
Casado JL, Quereda C, Moreno A, Perez-Elias MJ, Marti-Belda P, Moreno S. Regression of liver fibrosis is progressive after sustained virological response to HCV therapy in patients with hepatitis C and HIV coinfection. J Viral Hepat. 2013;20:829–37.
Yuen MF, Seto WK, Chow DH, Tsui K, Wong DK, Ngai VW, Wong BC, et al. Long-term lamivudine therapy reduces the risk of long-term complications of chronic hepatitis B infection even in patients without advanced disease. Antivir Ther. 2007;12:1295–303.
Kweon YO, Goodman ZD, Dienstag JL, Schiff ER, Brown NA, Burchardt E, Schoonhoven R, et al. Decreasing fibrogenesis: an immunohistochemical study of paired liver biopsies following lamivudine therapy for chronic hepatitis B. J Hepatol. 2001;35:749–55.
Xu B, Lin L, Xu G, Zhuang Y, Guo Q, Liu Y, Wang H, et al. Long-term lamivudine treatment achieves regression of advanced liver fibrosis/cirrhosis in patients with chronic hepatitis B. J Gastroenterol Hepatol. 2015;30(2):372–8.
Marcellin P, Gane E, Buti M, Afdhal N, Sievert W, Jacobson IM, Washington MK, et al. Regression of cirrhosis during treatment with tenofovir disoproxil fumarate for chronic hepatitis B: a 5-year open-label follow-up study. Lancet 2013;381:468–75.
Marcellin P, Heathcote EJ, Buti M, Gane E, de Man RA, Krastev Z, Germanidis G, et al. Tenofovir disoproxil fumarate versus adefovir dipivoxil for chronic hepatitis B. N Engl J Med. 2008;359:2442–55.
Poynard T, Munteanu M, Ngo Y, Moussalli J, Lebray P, Thabut D, Benhamou Y, et al. FibroTest is effective in patients with normal transaminases, when accuracy is standardized on fibrosis stage prevalence. J Viral Hepat. 2008;15:472–3; author reply 474.
Hadziyannis SJ, Tassopoulos NC, Heathcote EJ, Chang TT, Kitis G, Rizzetto M, Marcellin P, et al. Long-term therapy with adefovir dipivoxil for HBeAg-negative chronic hepatitis B for up to 5 years. Gastroenterology. 2006;131:1743–51.
Lin SM, Yu ML, Lee CM, Chien RN, Sheen IS, Chu CM, Liaw YF. Interferon therapy in HBeAg positive chronic hepatitis reduces progression to cirrhosis and hepatocellular carcinoma. J Hepatol. 2007;46:45–52.
Papatheodoridis GV, Petraki K, Cholongitas E, Kanta E, Ketikoglou I, Manesis EK. Impact of interferon-alpha therapy on liver fibrosis progression in patients with HBeAg-negative chronic hepatitis B. J Viral Hepat. 2005;12:199–206.
Ratnam D, Dev A, Nguyen T, Sundararajan V, Harley H, Cheng W, Lee A, et al. Efficacy and tolerability of pegylated interferon-alpha-2a in chronic hepatitis B: a multicenter clinical experience. J Gastroenterol Hepatol. 2012;27:1447–53.
Schiff E, Simsek H, Lee WM, Chao YC, Sette H Jr., Janssen HL, Han SH, et al. Efficacy and safety of entecavir in patients with chronic hepatitis B and advanced hepatic fibrosis or cirrhosis. Am J Gastroenterol. 2008;103:2776–83.
Kim MN, Kim SU, Kim BK, Park JY, Kim do Y, Ahn SH, Han KH. Long-term changes of liver stiffness values assessed using transient elastography in patients with chronic hepatitis B receiving entecavir. Liver Int. 2014;34:1216–23.
Farci P, Roskams T, Chessa L, Peddis G, Mazzoleni AP, Scioscia R, Serra G, et al. Long-term benefit of interferon alpha therapy of chronic hepatitis D: regression of advanced hepatic fibrosis. Gastroenterology. 2004;126:1740–49.
Samiullah S, Bikharam D, Nasreen. Treatment of chronic hepatitis delta virus with peg-interferon and factors that predict sustained viral response. World J Gastroenterol. 2012;18:5793–8.
Sikora SS, Srikanth G, Agrawal V, Gupta RK, Kumar A, Saxena R, Kapoor VK. Liver histology in benign biliary stricture: fibrosis to cirrhosis … and reversal? J Gastroenterol Hepatol. 2008;23:1879–84.
Corpechot C, Carrat F, Poujol-Robert A, Gaouar F, Wendum D, Chazouilleres O, Poupon R. Noninvasive elastography-based assessment of liver fibrosis progression and prognosis in primary biliary cirrhosis. Hepatology. 2012;56:198–208.
Mummadi RR, Kasturi KS, Chennareddygari S, Sood GK. Effect of bariatric surgery on nonalcoholic fatty liver disease: systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2008;6:1396–402.
Moretto M, Kupski C, da Silva VD, Padoin AV, Mottin CC. Effect of bariatric surgery on liver fibrosis. Obes Surg. 2012;22:1044–9.
Mattar SG, Velcu LM, Rabinovitz M, Demetris AJ, Krasinskas AM, Barinas-Mitchell E, Eid GM, et al. Surgically-induced weight loss significantly improves nonalcoholic fatty liver disease and the metabolic syndrome. Ann Surg. 2005;242:610–7 (discussion 618–20).
Dixon JB, Bhathal PS, Hughes NR, O'Brien PE. Nonalcoholic fatty liver disease: Improvement in liver histological analysis with weight loss. Hepatology. 2004;39:1647–54.
Ismail MH, Pinzani M. Reversal of hepatic fibrosis: pathophysiological basis of antifibrotic therapies. Hepat Med. 2011;3:69–80.
Hayasaka A, Ilda S, Suzuki N, Kondo F, Miyazaki M, Yonemitsu H. Pyridinoline collagen cross-links in patients with chronic viral hepatitis and cirrhosis. J Hepatol. 1996;24:692–8.
Issa R, Zhou X, Constandinou CM, Fallowfield J, Millward-Sadler H, Gaca MD, Sands E, et al. Spontaneous recovery from micronodular cirrhosis: evidence for incomplete resolution associated with matrix cross-linking. Gastroenterology. 2004;126:1795–808.
Novo E, Marra F, Zamara E, Valfre di Bonzo L, Monitillo L, Cannito S, Petrai I, et al. Overexpression of Bcl-2 by activated human hepatic stellate cells: resistance to apoptosis as a mechanism of progressive hepatic fibrogenesis in humans. Gut. 2006;55:1174–82.
Ramachandran P, Iredale JP. Liver fibrosis: a bidirectional model of fibrogenesis and resolution. QJM 2012;105:813–7.
Pellicoro A, Ramachandran P, Iredale JP. Reversibility of liver fibrosis. Fibrogenesis Tissue Repair. 2012;5:S26.
Troeger JS, Mederacke I, Gwak GY, Dapito DH, Mu X, Hsu CC, Pradere JP, et al. Deactivation of hepatic stellate cells during liver fibrosis resolution in mice. Gastroenterology. 2012;143:1073–83, e1022.
Kisseleva T, Cong M, Paik Y, Scholten D, Jiang C, Benner C, Iwaisako K, et al. Myofibroblasts revert to an inactive phenotype during regression of liver fibrosis. Proc Natl Acad Sci U S A. 2012;109:9448–53.
Iredale JP. Hepatic stellate cell behavior during resolution of liver injury. Semin Liver Dis. 2001;21:427–36.
Yoshiji H, Kuriyama S, Yoshii J, Ikenaka Y, Noguchi R, Nakatani T, Tsujinoue H, et al. Tissue inhibitor of metalloproteinases-1 attenuates spontaneous liver fibrosis resolution in the transgenic mouse. Hepatology. 2002;36:850–60.
Elsharkawy AM, Wright MC, Hay RT, Arthur MJ, Hughes T, Bahr MJ, Degitz K, et al. Persistent activation of nuclear factor-kappaB in cultured rat hepatic stellate cells involves the induction of potentially novel Rel-like factors and prolonged changes in the expression of IkappaB family proteins. Hepatology. 1999;30:761–9.
Krizhanovsky V, Yon M, Dickins RA, Hearn S, Simon J, Miething C, Yee H, et al. Senescence of activated stellate cells limits liver fibrosis. Cell 2008;134:657–67.
Yang L, Kwon J, Popov Y, Gajdos GB, Ordog T, Brekken RA, Mukhopadhyay D, et al. Vascular endothelial growth factor promotes fibrosis resolution and repair in mice. Gastroenterology. 2014;146:1339–50, e1331.
Fallowfield JA, Mizuno M, Kendall TJ, Constandinou CM, Benyon RC, Duffield JS, Iredale JP. Scar-associated macrophages are a major source of hepatic matrix metalloproteinase-13 and facilitate the resolution of murine hepatic fibrosis. J Immunol. 2007;178:5288–95.
Ramachandran P, Pellicoro A, Vernon MA, Boulter L, Aucott RL, Ali A, Hartland SN, et al. Differential Ly-6C expression identifies the recruited macrophage phenotype, which orchestrates the regression of murine liver fibrosis. Proc Natl Acad Sci U S A. 2012;109:E3186–95.
Baeck C, Wei X, Bartneck M, Fech V, Heymann F, Gassler N, Hittatiya K, et al. Pharmacological inhibition of the chemokine C-C motif chemokine ligand 2 (monocyte chemoattractant protein 1) accelerates liver fibrosis regression by suppressing Ly-6C(+) macrophage infiltration in mice. Hepatology. 2014;59:1060–72.
Dufour JF, DeLellis R, Kaplan MM. Reversibility of hepatic fibrosis in autoimmune hepatitis. Ann Intern Med. 1997;127:981–5.
Mato JM, Camara J, Fernandez de Paz J, Caballeria L, Coll S, Caballero A, Garcia-Buey L, et al. S-adenosylmethionine in alcoholic liver cirrhosis: a randomized, placebo-controlled, double-blind, multicenter clinical trial. J Hepatol. 1999;30:1081–9.
Lieber CS, Weiss DG, Groszmann R, Paronetto F, Schenker S. I. Veterans affairs cooperative study of polyenylphosphatidylcholine in alcoholic liver disease: effects on drinking behavior by nurse/physician teams. Alcohol Clin Exp Res. 2003;27:1757–64.
Bataller R, Sancho-Bru P, Gines P, Brenner DA. Liver fibrogenesis: a new role for the renin-angiotensin system. Antioxid Redox Signal. 2005;7:1346–55.
Colmenero J, Bataller R, Sancho-Bru P, Dominguez M, Moreno M, Forns X, Bruguera M, et al. Effects of losartan on hepatic expression of nonphagocytic NADPH oxidase and fibrogenic genes in patients with chronic hepatitis C. Am J Physiol Gastrointest Liver Physiol. 2009;297:G726–34.
Di Bisceglie AM, Shiffman ML, Everson GT, Lindsay KL, Everhart JE, Wright EC, Lee WM, et al. Prolonged therapy of advanced chronic hepatitis C with low-dose peginterferon. N Engl J Med. 2008;359:2429–41.
Mahady SE, Webster AC, Walker S, Sanyal A, George J. The role of thiazolidinediones in non-alcoholic steatohepatitis—a systematic review and meta analysis. J Hepatol. 2011;55:1383–90.
Dima A, Marinescu AG, Dima AC. Non-alcoholic fatty liver disease and the statins treatment. Rom J Intern Med. 2012;50:19–25.
George J, Roulot D, Koteliansky VE, Bissell DM. In vivo inhibition of rat stellate cell activation by soluble transforming growth factor beta type II receptor: a potential new therapy for hepatic fibrosis. Proc Natl Acad Sci U S A. 1999;96:12719–24.
Yoshiji H, Kuriyama S, Noguchi R, Ikenaka Y, Yoshii J, Yanase K, Namisaki T, et al. Amelioration of liver fibrogenesis by dual inhibition of PDGF and TGF-beta with a combination of imatinib mesylate and ACE inhibitor in rats. Int J Mol Med. 2006;17:899–904.
Gonzalo T, Beljaars L, van de Bovenkamp M, Temming K, van Loenen AM, Reker-Smit C, Meijer DK, et al. Local inhibition of liver fibrosis by specific delivery of a platelet-derived growth factor kinase inhibitor to hepatic stellate cells. J Pharmacol Exp Ther. 2007;321:856–65.
Thompson K, Maltby J, Fallowfield J, McAulay M, Millward-Sadler H, Sheron N. Interleukin-10 expression and function in experimental murine liver inflammation and fibrosis. Hepatology. 1998;28:1597–606.
Zhang LJ, Zheng WD, Chen YX, Huang YH, Chen ZX, Zhang SJ, Shi MN, et al. Antifibrotic effects of interleukin-10 on experimental hepatic fibrosis. Hepatogastroenterology. 2007;54:2092–8.
Julien B, Grenard P, Teixeira-Clerc F, Nhieu Van JT, Li L, Karsak M, Zimmer A, et al. Antifibrogenic role of the cannabinoid receptor CB2 in the liver. Gastroenterology. 2005;128:742–55.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Abbreviations
- ECM
-
Extracellular matrix proteins
- HCV
-
Hepatitis C infection
- HSC
-
Hepatic stellate cells
- MMPs
-
Metalloproteinases
- NASH
-
Nonalcoholic steatohepatitis
- NF-κB
-
Nuclear factor kappa B
- PDGF
-
Platelet-derived growth factor
- ROS
-
Reactive oxygen species
- TIMPs
-
Tissue inhibitors of metalloproteinases
- TGFβ1
-
Transforming growth factor beta 1
- VEGF
-
Vascular endothelial growth factor
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Odena, G., Stein, E., Bataller, R. (2015). Reversal of Cirrhosis. In: Keaveny, A., Cárdenas, A. (eds) Complications of Cirrhosis. Springer, Cham. https://doi.org/10.1007/978-3-319-13614-1_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-13614-1_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-13613-4
Online ISBN: 978-3-319-13614-1
eBook Packages: MedicineMedicine (R0)