Abstract
Surgical placement of dental implants is governed by the prosthetic design and the morphology and quality of the alveolar bone. Often, implant placement may be difficult, if at all possible, due to alveolar ridge aberrations. In consequence, prosthetically dictated implant positioning commonly entails bone augmentation procedures. We herein discuss the unique biologic potential, the clinical relevance, and perspectives of bone morphogenetic protein (BMP) technologies (focus on rhBMP-2) for alveolar bone augmentation. We also address merits and short-comings of current treatment protocol including bone biomaterials and guided bone regeneration (GBR). In perspective, our studies suggest that BMPs have an unparalleled, dose-dependent potential to augment alveolar bone and in turn support dental implant fixation and functional loading. Inclusion of BMPs for alveolar augmentation to facilitate dental implant fixation may thus not only enhance predictability of existing clinical protocol but radically change current treatment paradigms making conventional “grafting” and GBR procedures altogether obsolete.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Prosthetic rehabilitation of the edentulous or partially edentulous patient presents considerable clinical as well as patient-centered challenges. Alveolar ridge aberrations, a sequel to bone remodeling following tooth extractions, periodontal disease, resective surgery, or traumatically induced or of congenital origin must be mastered in addition to prosthetic technical challenges. Patient expectations regarding esthetic and functional outcomes as well as expectations of a minimally invasive, painless, and rapid completion of the prosthetic rehabilitation must equally effectively be mastered. As bone-anchored (osseointegrated) dental implant-based prosthetic rehabilitation supported by favorable long-term survival rates (Albrektsson et al. 1988; Adell et al. 1990; Henry et al. 1996; Lekholm et al. 1999) has become a preferred approach, surgical augmentation of the deficit alveolar ridge and adjoining mucosal tissues has increasingly become a required addition as much as dental implant installation in itself represents a surgical event. In perspective, it is estimated that approximately 12 million dental implants are sold/placed annually worldwide of which 2 million units in the U.S. alone (iData Research Inc.) indicating a substantial need for patient-centered, clinically-relevant, and evidence-based routines for dental implant surgery and alveolar augmentation.
Current surgical protocol includes inlay/onlay access flap procedures for alveolar preservation and horizontal or vertical alveolar ridge augmentation (Simion et al. 2007; de Freitas et al. 2014a). Modified Caldwell-Luc and transalveolar osteotomy protocols have been introduced to gain access and augment the subantral space to increase the vertical dimension of the alveolar base for implant anchorage in the posterior maxilla (Boyne and James 1980; Summers 1994). As these procedures have gained general acceptance, a number of autogenous bone preparations, cadaver-sourced or synthetic bone biomaterials, as well as membranes for guided tissue/bone regeneration as stand-alone protocols or in combinations have been introduced for alveolar augmentation (Fig. 1). Controlled clinical studies examining their capacity to support alveolar augmentation, dental implant osseointegration, and survival have been conducted and subjected to systematic reviews (Esposito et al. 2009, 2010; Horvath et al. 2013).
Considered the gold standard or benchmark, autogenous bone preparations require a donor site adding undesirable morbidity to the surgical event as well as present limitations relative to graft volumes attenuating their clinical attraction for alveolar augmentation (Clavero and Lundgren 2003; Andersson 2008). While readily commercially accessible, cadaver-sourced allogeneic or xenogeneic bone biomaterials, and synthetic biomaterials, should not be expected to support osteogenic bone formation as discerned from an expanding portfolio of histological evaluations (Pinholt et al. 1992; Caplanis et al. 1997; von Arx et al. 2001; Pöhling et al. 2006; Hong et al. 2014). As an example, such studies unequivocally demonstrate that a bovine bone mineral, a biphasic calcium phosphate, and a ß-tricalcium phosphate biomaterial delay, if not obstruct, osteogenic bone formation rendering them unattractive surrogates for autogenous bone grafts (Pöhling et al. 2006; Hong et al. 2014). Similarly, allogeneic demineralized bone matrix (DBM) preparations apparently should not be expected to enhance osteogenic bone formation, even under optimal circumstances for wound healing (Caplanis et al. 1997). In perspective, it appears that bone biomaterials—whether cadaver-sourced or synthetic—become encapsulated in dense connective tissue without projecting any meaningful bone metabolic activity to eventually or not undergo biodegradation (Fig. 2). Thus, projected clinical success appears limitedly, if at all, influenced by osteoconductive or other properties generated by implanted bone biomaterials.
Critical-size, supraalveolar, peri-implant defect treated with guided tissue/bone regeneration (GBR) using an occlusive space-providing ePTFE membrane (green arrowheads), with or without an allogeneic demineralized bone matrix (DBM/DFDBA). Clinical panels show the supraalveolar defect with the ePTFE membrane, with DBM rehydrated in autologous blood, and with the membrane in place prior to wound closure for primary intention healing. Note limited regeneration of alveolar bone in absence and presence of DBM suggesting that the innate regenerative potential of alveolar bone is limited, and that the DBM biomaterial has limited, if any, osteoinductive and/or osteoconductive properties to support bone regeneration. Green lines delineate the level of the surgically reduced alveolar crest. Healing interval 16 weeks. From Caplanis et al. (1997), figure copyrighted by and modified with permission from Quintessence Publishing
The intuitive observation (Levander 1938; Lacroix 1945), the critical discovery (Urist 1965), and the eventual purification, cloning, and characterization of bone morphogenetic proteins (BMPs) (Wozney et al. 1988; Wang et al. 1990; Celeste et al. 1990; Özkaynak et al. 1990; Sampath et al. 1992; Hötten et al. 1994, 1996) prompted research evaluating treatment concepts using purified or recombinant forms of BMPs in support of local bone formation for orthopedic, spine, and in turn craniofacial indications (Bishop and Einhorn 2007; Hsu and Wang 2008; Wikesjö et al. 2009). Recombinant human BMP-2 (rhBMP-2) combined with an absorbable collagen sponge (ACS) carrier was approved in 2002 for spine fusion and long bone fracture repair by the US Food and Drug Administration, as it also was approved for craniofacial indications in 2007 (McKay et al. 2007).
2 Alveolar Augmentation
Compiled over the last decades, a number of studies using clinically relevant translational models and canine, porcine, and nonhuman primate platforms including discriminating critical-size supraalveolar peri-implant defects (Wikesjö et al. 2006) and clinical modeling (Hanisch et al. 1997a, b, c; Jovanovic et al. 2007; Lee et al. 2013a) illuminate the potential of BMPs to augment alveolar bone in craniofacial settings. This text selectively focuses on advances that display the remarkable biologic and clinical potential BMPs, in particular rhBMP-2, may bring to alveolar augmentation and in turn implant dentistry.
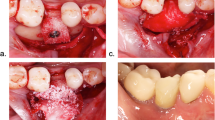
Using a discriminating onlay defect model for vertical alveolar ridge augmentation, Sigurdsson and colleagues first showed that a BMP construct—rhBMP-2 soak-loaded onto an ACS carrier—has the potential to induce clinically relevant bone formation (Sigurdsson et al. 1997). Ten-mm dental implants placed 5 mm into the surgically reduced edentulous mandibular alveolar ridge leaving 5 mm of the implant residing above the alveolar crest were draped with rhBMP-2/ACS (rhBMP-2 at 0.4 mg/mL) or in contralateral jaw quadrants ACS soak-loaded with buffer (control) and then submerged underneath the mucoperiosteal flaps for primary intention healing (Fig. 3). The experimental sites were subject to histometric evaluation following a 16-week healing interval. Sites receiving rhBMP-2/ACS displayed significant bone formation intimately anchored to the implant surface reaching the top of the exposed dental implants. The control showed as expected limited, if any, bone formation. These observations should be compared with the limited native regenerative potential of the alveolar bone in this defect model shown following the use of space-providing membranes for guided tissue/bone regeneration also including implantation of an allogeneic demineralized bone matrix preparation (Caplanis et al. 1997; Wikesjö et al. 2004). Nevertheless, rhBMP-2/ACS-induced bone formation exhibited considerably variable geometry; at times only a thin layer of bone wallpapered the root of the threads of the bone-anchoring implant surface. Apparently, the ACS carrier was ineffective to consistently support relevant rhBMP-2 induced bone formation also shown in parallel studies using a panel of rhBMP-2 concentrations (Tatakis et al. 2002; Wikesjö et al. 2003; Lu et al. 2013). This apparent variability in bone formation could have several geneses including rhBMP-2 dose and release kinetics or bioavailability, but also reflect ACS structural integrity, biodegradation, degree of soak-load, or any combination(s) thereof.
Critical-size, supraalveolar, peri-implant defect implanted with rhBMP-2/ACS (0.4 mg/mL) or ACS without rhBMP-2 (control). Clinical panels show the supraalveolar defect with rhBMP-2/ACS before and after wound closure for primary intention healing. The photomicrographs show defect sites implanted with rhBMP-2/ACS exhibiting bone formation reaching or exceeding the implant platform, the newly formed bone showing osseointegration to the titanium implant surface (high magnification insert). Control sites show limited, if any, bone formation. Green lines delineate the level of the surgically reduced alveolar crest. Healing interval 16 weeks. From Sigurdsson et al. (1997), figure copyrighted by and modified with permission from Wiley-Blackwell
Several approaches have been explored in an effort to enhance the performance of rhBMP-2/ACS for onlay indications such as alveolar augmentation. They have included dose-variation (Tatakis et al. 2002), the use of space-providing macroporous membranes or titanium mesh devices to shield the rhBMP-2/ACS from compressive forces reducing the potential volume for tissue to form into (Wikesjö et al. 2003, 2004; Lee et al. 2013b), as well as supplementing the ACS with bulking agents to withstand compressive forces compromising bone augmentation (Barboza et al. 2000, 2004; Miranda et al. 2005; Lu et al. 2013). Whereas dose-variation (rhBMP-2 at 0.05, 0.1, and 0.2 mg/mL) significantly failed to influence rhBMP-2/ACS-induced bone formation (Tatakis et al. 2002), the use of macroporous space-providing devices allowed significantly enhanced rhBMP-2/ACS (rhBMP-2 at 0.2 mg/mL)-induced bone formation/alveolar augmentation compared with unshielded sites supporting the tissue engineering principle that the geometry/volume of new bone formation can be ascertained in the design of a space-providing device/matrix (Fig. 4) (Wikesjö et al. 2003, 2004).
Critical-size, supraalveolar, peri-implant defects treated with rhBMP-2/ACS (0.2 mg/mL), a porous, space-providing ePTFE membrane for guided tissue regeneration, or rhBMP-2/ACS combined with the porous, ePTFE membrane. The clinical panels show the supraalveolar defect with rhBMP-2/ACS and with the porous ePTFE membrane. Note how rhBMP-2-induced bone fills the space provided by the membrane (green arrowheads) whereas rhBMP-2/ACS alone provides very irregular bone formation (top left). The ePTFE membrane alone (bottom left) provides limited, if any, regeneration of alveolar bone. Green lines delineate the level of the surgically reduced alveolar crest. Healing interval 8 weeks. From Wikesjö et al. (2003, 2004), figure copyrighted by and modified with permission from Wiley-Blackwell
The use of bulking agents including granular hydroxyapatite and ß-tricalcium combinations has likewise been shown to significantly support enhanced rhBMP-2/ACS-induced alveolar augmentation. However, bulking agents also introduce compromises related to biodegradation; slowly or nonresorbable biomaterials may compromise the structural integrity of the newly formed bone including osseointegration of dental implants (Barboza et al. 2000, 2004; Miranda et al. 2005; Lu et al. 2013) while for bioresorbable conduits the resorption process per se may solicit inflammatory reactions compromising bone formation and/or maintenance (Sigurdsson et al. 1996).
3 Clinical Modeling
Several studies have used clinical modeling as a proxy to illuminate potential utility of rhBMP-2/ACS in clinical settings, that is evaluating rhBMP-2/ACS using typified clinical defects applied to large animal, usually canine, porcine or nonhuman primate platforms. Such studies have used alveolar saddle-type defects (Hunt et al. 2001; Jovanovic et al. 2003, 2007), chronic post-extraction defects (Barboza et al. 2000, 2004), dental implant dehiscence defects (Hanisch et al. 2003), chronic peri-implantitis defects (Hanisch et al. 1997a, b), and sinus augmentation for extended dental implant bone anchorage in the posterior maxilla (Hanisch et al. 1997c; Lee et al. 2013a).
Comparing rhBMP-2/ACS (rhBMP-2 at 0.20 mg/mL)-induced bone formation with that of the innate regenerative potential in saddle-type defects using a guided tissue regeneration membrane shielding the defect site from competing mucosal ingress, Jovanovic and coworkers showed that rhBMP-2/ACS outperformed the membrane predicate benchmark (Jovanovic et al. 2007). Defect sites receiving rhBMP-2/ACS showed complete to almost complete defect resolution whereas sites receiving the membrane commonly experienced exposures and compromised wound healing/regeneration. In turn, sites receiving an rhBMP-2/ACS-membrane combination also became subject to exposures and compromised healing. In parallel studies, Jovanovic et al. (2003) showed that the geometry/volume of induced bone formation allowed placement and dental implant osseointegration allowing long-term (12 months) functional loading comparable to that in the adjoining resident bone.
Chronic post-extraction alveolar defect sites were used in other studies to evaluate rhBMP-2/ACS (rhBMP-2 at 0.40 mg/mL) combined with various bulking agents including hydroxyapatite, bioactive glass and demineralized/mineralized bone matrix (Barboza et al. 2000, 2004). Wrapped into the ACS matrix slowly or nonresorbable adjuvants supported “clinically relevant augmentation however, the quality of bone is compromised” questioning the relevance of at least these common biomaterials for sites intended for osseointegration of dental implants.
In still other studies, Hanisch et al. (1997a, b) using a nonhuman primate platform evaluated rhBMP-2/ACS as a stand-alone therapy for resolution of chronic peri-implantitis defects (rhBMP-2 at 0.43 mg/mL), peri-implantitis representing a biofilm-induced inflammatory lesion progressively depriving dental implants from their alveolar support. rhBMP-2/ACS supported significant resolution of the advanced chronic peri-implantitis defects, mean defect fill approximating 77 % of the 3.4 mm peri-implant defect versus 24 % for the sham-surgery control. Importantly, the newly formed bone osseointegrated to a titanium implant surface that had been exposed to a biofilm-induced inflammatory lesion over 12 months, osseointegration reaching 40 % following a 16-week healing interval. These singularly unique observations become even more critically important considering the increasing awareness of peri-implantitis and the hereto absence of effective clinical solutions.
One main clinical indication for bone augmentation in implant dentistry includes augmentation of the maxillary sinus to extend the alveolar base coronally to allow placement and anchorage of dental implants for prosthetic reconstruction in the posterior maxilla. Unlike alveolar onlay grafts, maxillary sinus augmentation is considered an inlay indication, implanted graft materials secured within the sinus antral walls without interference from local environmental factors such as for alveolar onlay indications. Hanisch et al. (1997c) evaluated rhBMP-2/ACS (rhBMP-2 at 0.43 mg/mL) for maxillary sinus augmentation using a nonhuman primate platform. Following a staged protocol, dental implants were placed 3 months following implantation of the rhBMP-2/ACS construct into the maxillary sinus and allowed to osseointegrate for 3 months. Sites receiving rhBMP-2/ACS showed a two-fold mean increase in vertical bone augmentation compared with the ACS carrier control (6 vs. 2.6 mm), newly formed bone exhibiting the same density and osseointegration as the adjoining resident bone. This study first provided the evidence of clinically relevant bone augmentation by rhBMP-2/ACS in maxillary sinus serving as a baseline for clinical evaluations and eventual regulatory approval of this indication.
Autogenous cancellous bone has long been regarded the gold standard for bone grafting due to its content of bone forming cells and serving as a matrix for bone growth. Lee et al. (2013a) compared bone formation/osseointegration following sinus augmentation using rhBMP-2/ACS (rhBMP-2 at 0.43 mg/mL) versus a particulated fresh autogenous cancellous bone graft harvested from the iliac crest using a Yucatan mini-pig platform. This study used a protocol placing dental implants in conjunction with the augmentation procedure rather than using a staged protocol. Histologic evaluation following an 8-week healing interval revealed significant augmentation of the maxillary sinus following implantation of rhBMP-2/ACS covering most of the dental implant bone-anchoring surfaces compared with irregular bone formation including active resorption in sites receiving the autogenous bone graft. Notably, the rhBMP-2/ACS-induced bone exhibited significantly greater density compared with that of the autogenous bone graft (52 % vs. 33 %). The observations in this study imply significant clinical time-savings using the rhBMP-2/ACS technology due to the augmentation protocol can be used in parallel with implant placement with superior outcomes without need to access a donor site and associated morbidity; greater bone density of predicable geometry without evidence of osteoclastic resorption overall suggesting that rhBMP-2/ACS appears a realistic and effective alternative to autogenous bone grafts in patients requiring maxillary sinus augmentation and should thus be considered the new standard for this indication.
4 Alternative Carrier Technologies
Ideal delivery systems for growth factors/BMPs for alveolar augmentation should meet several criteria conceptually critical to successful regeneration. They should be injectable for ease-of-use implantable and minimally invasive approaches; they should be space-providing allowing structurally integrity/wound stability for a regenerate to form also in noncontained sites (onlay indications); they should be macroporous for rapid ingrowth of cells and vascular support from adjoining tissue resources; they should allow appropriate release/bioavailability of the biologic; and they should feature a biodegradation profile/rapid clearance allowing the regenerate uneventful maturation (Herberg et al. 2008).
Only few rhBMP-2 delivery systems exhibiting structural integrity have been evaluated in discriminating craniofacial models. An early proof-of-principal report describes the application of rhBMP-2 (rhBMP-2 at 0.2 mg/mL) in an allogeneic DBM/fibrin clot construct to unsupported augment difficult to treat horizontal alveolar defects using a canine platform (Fig. 5) (Sigurdsson et al. 2001). Ten-mm, dental implants were placed into the rhBMP-2-induced alveolar ridge at 8 and 16 weeks. Block biopsies for histometric analysis were collected at 24 weeks. Roughly 90 % of the bone-anchoring implant surfaces were invested in rhBMP-2-induced bone leaving not more than the apex of the implants interfacing resident bone; all dental implants showing a high degree (~55 %) of osseointegration. There were no significant differences in bone density between rhBMP-2-induced and resident bone. However, the use of cadaver-derived biomaterials such as the allogeneic demineralized bone matrix may with difficulty receive public acceptance for elective procedures in preference for synthetic carrier technologies.
Surgically created horizontal alveolar ridge defect implanted with rhBMP-2 combined with allogeneic DBM rehydrated in autologous blood. Clinical panels show the rhBMP-2 construct placed onto the surgically reduced alveolar ridge prior to wound closure for primary intention healing. Endosseous dental implants were placed into the rhBMP-2 induced alveolar ridge at 8 and 16 weeks. The animals were euthanized at 24 weeks. Left and right photomicrographs show implants placed at 8 and 16 weeks, respectively. Approximately 90 % of the bone-anchoring surface of the implants was housed in rhBMP-2 induced bone. There was no significant difference in bone density between rhBMP-2 induced and the contiguous resident bone. Also osseointegration (approximately 55 %) was similar in induced and resident bone irrespective of whether the implants were placed at week 8 or 16. From Sigurdsson et al. (2001), figure copyrighted by and modified with permission from Quintessence Publishing
A subsequent study thus evaluated a synthetic calcium phosphate cement (α-BSM®, ETEX Corporation, Cambridge, MA) as a candidate carrier for rhBMP-2 using the critical-size supraalveolar defect model (Fig. 6) (Wikesjö et al. 2002). Block biopsies for histometric analysis collected following a 16-week healing interval showed that rhBMP-2/α-BSM® (rhBMP-2 at 0.40 and 0.75 mg/mL) induced substantial and clinically relevant augmentation of the alveolar ridge while control sites receiving α-BSM® without rhBMP-2 exhibited limited, if any, new bone formation. Vertical alveolar augmentation comprised almost the entire 5-mm exposed implants; the newly formed bone density approximating 60 %, cortication, bone–implant contact approximating 27 %, and limited α-BSM® residuals. Clearly, this calcium phosphate cement technology presents considerable promise for a number of indications in the craniofacial skeleton since the α-BSM® may easily be shaped to desired contour and sets to resist compression to provide space for rhBMP-2-induced bone formation. Moreover, the α-BSM® is injectable for ease-of-use and may well prove useful for augmentation of the maxillary sinus in conjunction with placement of dental implants pin-pointing bone formation at the implant body using either a modified Caldwell–Luc or transalveolar osteotomy approach.
Critical-size, supraalveolar peri-implant defect treated with rhBMP-2 in a calcium phosphate cement (α-BSM®) or α-BSM® without rhBMP-2 (control). Clinical panels show the supraalveolar peri-implant defect before and after application of α-BSM®. Photomicrographs show representative observations for jaw quadrants receiving rhBMP-2/α-BSM® at 0.4 mg/mL. Note substantial new bone formation at sites treated with rhBMP-2/α-BSM® compared to the control (far right) exhibiting limited, if any, evidence of new bone formation. The rhBMP-2-induced bone exhibits similar trabeculation, osseointegration, and cortex formation as the contiguous resident bone. Green arrows delineate the apical extension of the supraalveolar peri-implant defects. Healing interval 16 weeks. From Wikesjö et al. (2002), figure copyrighted by and modified with permission from Wiley-Blackwell
5 rhBMP-2 Coated Dental Implants
Conceptually, dental implants coated with a bone inductive factor may stimulate local bone formation and osseointegration (Hall et al. 2007). This hypothesis has engaged our laboratories in a series of studies with the intent to develop a dental implant coated with rhBMP-2. Initial in vitro retention assays evaluating a panel of dental implant surface technologies demonstrated that an anodized titanium surface with open pores appeared the most effective vehicle for rhBMP-2 (Hall et al. 2007). Subsequent in vivo evaluations of rhBMP-2-coated titanium disk implants inserted into the ventral thoracic region in rats showed significant bone formation within a 14-day healing interval engaging the anodized titanium disk implants (Hall et al. 2007). Studies evaluating rhBMP-2-coated anodized screw-type dental implants placed into the edentulated posterior mandible (Type II bone) in dogs (Wikesjö et al. 2008a) or into the edentulated posterior maxilla (Type IV bone) in nonhuman primates (Wikesjö et al. 2008b) showed robust bone formation in a dose-dependent order. Collectively, these initial proof-of-concept studies using qualified ectopic and orthotopic small and large animal models demonstrate that rhBMP-2 can be successfully delivered to induce local bone formation and osseointegration using a dental implant as a carrier.
Subsequent studies focused on indications for the rhBMP-2-coated implant including alveolar augmentation using the critical-size supraalveolar peri-implant defect model (Wikesjö et al. 2008c; Leknes et al. 2008). Anodized screw-type dental implants soak-loaded with rhBMP-2 at 0.75, 1.5, and 3.0 mg/mL were evaluated following an 8-week healing interval. Jaw quadrants receiving control implants showed limited new bone formation whereas implants coated with rhBMP-2 at 0.75 and 1.5 mg/mL showed clinically relevant bone formation/alveolar augmentation reaching the implant platform (Fig. 7). The quality of the newly formed bone approximated that of the adjoining mature resident bone including cortex formation within 8 weeks. In contrast, implants coated with rhBMP-2 at 3.0 mg/mL showed sparsely trabecular immature bone formation exceeding the implant platform without cortication. These studies evaluating rhBMP-2 coated dental implants using the critical-size supraalveolar peri-implant defect model thus reveal an inverse relationship between rhBMP-2 concentration/dose and induced bone formation/maturation. Whereas lower rhBMP-2 concentrations support clinically relevant vertical/horizontal alveolar augmentation, the higher concentration apparently extends/delays bone formation/maturation. These studies also imply that rhBMP-2-induced bone formation benefits from space provision, the lingual aspects of the implants exhibiting a wider alveolar base generally display more robust bone formation than corresponding buccal surfaces, important to the clinical surgical management.
Critical-size, supraalveolar peri-implant defect including dental implants coated with rhBMP-2 at 0.75 mg/mL following placement and wound closure, and healing at 4 and 8 weeks. Radiographs show bone formation reaching the implant platform at 4 and 8 weeks. Photomicrographs show bone formation with an established cortex reaching or exceeding the implant platform. Green arrows delineate a 5 mm notch placed level with the resident alveolar bone. From Wikesjö et al. (2008c) and Leknes et al. (2008), figure copyrighted by Wiley-Blackwell
6 Alveolar Augmentation in Clinical Settings
rhBMP-2 soak-loaded onto the ACS carrier has met increasing yet guarded acceptance for the management of craniofacial indications including alveolar augmentation for implant dentistry. We recently conducted a systematic review of the field; some of our major findings summarized herein (de Freitas et al. 2014b). To date, relatively few clinical trials have been conducted to evaluate the on-label clinical efficacy and safety of rhBMP-2/ACS or its off-label use combined with other biomaterials for alveolar ridge augmentation. Interpretation of the results is convoluted by the use of varying rhBMP-2 concentrations, and a wide absolute dose range for the same indication. Whereas rhBMP-2 concentrations at 0.43, 0.75, and 1.5 mg/mL have been tested in experimental clinical settings, the only US. Food and Drug Administration-approved and commercially available concentration to date is rhBMP-2 at 1.5 mg/mL. rhBMP-2/ACS kits are commercially available in sizes ranging from 0.7 to 8.0 cc including rhBMP-2 doses ranging from 1.05 to 12.0 mg, respectively, allowing the clinician to tailor the rhBMP-2 dose applied to the surgical site by increasing the number of rhBMP-2 soak-loaded ACSs. For simplicity, we chose to only present results related to the commercially available product in Table 1, i.e., rhBMP-2/ACS at the 1.5 mg/mL concentration.
Maxillary sinus augmentation using rhBMP-2/ACS as a stand-alone therapy has been evaluated in three studies using rhBMP-2 concentrations at 0.43, 0.75, and 1.5 mg/mL (Boyne et al. 1997, 2005; Triplett et al. 2009). All surgeries were performed using a lateral window modified Caldwell–Luc approach. The mean rhBMP-2 dose ranged between 2.9 and 20.8 mg per site complicating interpretation of the results. Nevertheless, implantation of rhBMP-2/ACS yielded clinically meaningful bone augmentation ranging between 7.8 and 10.2 mm. No consistent differences in bone formation could be observed among rhBMP-2 concentrations and no specific analysis was performed regarding dose variations. Compared with autogenous bone graft, rhBMP-2/ACS yielded 1.6 mm (95 %CI: 0.5–2.7) less bone formation (de Freitas et al. 2014a); yet both treatments allowed implant placement. Radiographic bone density at 4–6 months post-surgery was significantly greater for the autogenous bone graft, whereas a reversal was observed after implant loading; rhBMP-2/ACS yielding the greater bone density.
rhBMP-2/ACS has also been evaluated for preservation of the alveolar ridge following tooth extractions, an inlay application. In a randomized clinical trial, Fiorellini et al. (2005) demonstrated that surgical implantation of rhBMP-2/ACS at the commercially available 1.5 mg/mL concentration maintained the height of the alveolar ridge (mean ± SD: 0.0 ± 1.2 vs. −1.2 ± 1.2 mm), while also yielding a wider alveolar ridge at the sub- (3.3 ± 2.5 vs. 0.6 ± 2.2 mm) and mid-crestal (4.0 ± 2.5 vs. 1.6 ± 2.5 mm) levels compared with untreated tooth extraction sockets. The mean rhBMP-2 dose per site was 1.9 mg; a dose–effect relationship was reported.
Recently, de Freitas et al. (2014a) reported a study evaluating application of rhBMP-2/ACS for alveolar ridge augmentation—onlay application—in the atrophic anterior maxilla. This randomized clinical trial compared rhBMP-2/ACS (rhBMP-2 at 1.5 mg/mL) and the “gold standard” autogenous bone graft for horizontal augmentation. The surgical protocol also included the placement of a customized titanium mesh device to provide for space provision, wound stability, and conditions for primary intention healing. At the subcrestal level, rhBMP-2/ACS yielded significantly greater radiographic horizontal bone augmentation compared with autogenous bone graft (1.5 ± 0.7 vs. 0.5 ± 0.9 mm); no differences between treatments were observed at the mid- and apical crestal levels. Whereas the sample size in this study was limited (n = 24), the authors were still able to conclude: “rhBMP-2/ACS appears a realistic alternative for augmentation of the edentulous atrophic anterior maxilla.”
Some of the studies have included histological evaluations of core biopsies obtained in conjunction with dental implant placement (Boyne et al. 2005; Triplett et al. 2009; Kao et al. 2012; de Freitas et al. 2014b). General histological findings demonstrate limited or no residual ACS, woven and lamellar bone including a cell-rich fibrovascular marrow, limited number of osteoblasts and osteoclasts, and no or limited inflammatory infiltrates. These findings validate the preclinical results described earlier in this chapter.
Safety is always a major concern regarding the clinical use of biologics and this has become particularly true for rhBMP-2/ACS. Adverse effects related to on- and off-label rhBMP-2/ACS use for spine surgery have gained considerable attention and publication of independent reviews of earlier publications and data disclosure under the Yale Open Data Access (YODA) project (Carragee et al. 2012; Laine et al. 2013; Resnick and Bozic 2013). Safety data for application of rhBMP-2/ACS in craniofacial settings are mostly limited to that reported in industry-sponsored studies. Frequent post-surgery events include transient oral and facial erythema, edema, sensory loss and pain; some subjects experiencing significant facial swelling, findings in agreement with anecdotal reports from clinicians using rhBMP-2/ACS. rhBMP-2 antibody formation appears a rare event (<3 %) with most individuals exhibiting antibodies to bovine type I collagen used in the carrier (23 %) (Boyne et al. 1997, 2005; Fiorellini et al. 2005; Triplett et al. 2009). As evidenced by an increasing off-label use of rhBMP-2/ACS for craniofacial applications, safety concerns are likely to heighten.
The debate generated by the YODA project is critical for the future use of biologics in general and BMPs in particular. However, extrapolating findings and conclusions from orthopedic settings to craniofacial applications is unwarranted. Whereas the use of autogenous bone grafts for posterolateral spine procedures may not need a second surgical/donor site, this is rarely the case for craniofacial applications. Intraoral sites yield limited amounts of autogenous bone, generally constrained to cortical bone, and access to extraoral donor sites incurs increased costs and morbidity that is not usually expected for outpatient procedures like implant dentistry. Thus, any biologics intended for bone augmentation in craniofacial settings does not need to surpass the clinical efficacy offered by autogenous bone grafts as long as treatment complexity and morbidity are reduced.
In conclusion, rhBMP-2/ACS appears a promising alternative to autogenous bone grafts and other biomaterials for alveolar ridge augmentation also including the maxillary sinus. Safety reports do not appear to represent major concerns for the proposed indications. Further research and development is needed for dose and carrier optimization. Caution should be exercised since most clinical data available are derived from few randomized clinical trials of limited follow-up.
References
Adell R, Eriksson B, Lekholm U, Brånemark P-I, Jemt T (1990) A long-term follow-up study of osseointegrated implants in the treatment of totally edentulous jaws. Int J Oral Maxillofac Implant 5:347–359
Albrektsson T, Dahl E, Enbom L, Engevall S, Engquist B, Eriksson AR, Feldmann G, Freiberg N, Glantz P-O, Kjellman O, Kristersson L, Kvint S, Köndell P-Å, Palmquist J, Werndahl L, Åstrand P (1988) Osseointegrated oral implants: a Swedish multicenter study of 8139 consecutively inserted Nobelpharma implants. J Periodontol 59:287–296
Andersson L (2008) Patient self-evaluation of intra-oral bone grafting treatment to the maxillary frontal region. Dent Traumatol 24:164–169
Barboza EP, Leite Duarte ME, Geolás L, Sorensen RG, Riedel GE, Wikesjö UME (2000) Ridge augmentation following implantation of recombinant human bone morphogenetic protein-2 in the dog. J Periodontol 71:488–496
Barboza E, Caúla AL, Caúla F, Oliveira de Souza R, Neto LG, Sorensen RG, Li XJ, Wikesjö UME (2004) Effect of recombinant human bone morphogenetic protein-2 in an absorbable collagen sponge with space-providing biomaterials on the augmentation of chronic alveolar ridge defects. J Periodontol 75:702–708
Bishop GB, Einhorn TA (2007) Current and future clinical applications of bone morphogenetic proteins in orthopaedic trauma surgery. Int Orthop 31:721–727
Boyne PJ, James RA (1980) Grafting of the maxillary sinus floor with autogenous marrow and bone. J Oral Surg 38:613–616
Boyne PJ, Lilly LC, Marx RE, Moy PK, Nevins M, Spagnoli DB, Triplett RG (2005) De novo bone induction by recombinant human bone morphogenetic protein-2 (rhBMP-2) in maxillary sinus floor augmentation. J Oral Maxillofac Surg 63:1693–1707
Boyne PJ, Marx RE, Nevins M, Triplett G, Lazaro E, Lilly LC, Alder M, Nummikoski P (1997) A feasibility study evaluating rhBMP-2/absorbable collagen sponge for maxillary sinus floor augmentation. Int J Periodontics Restorative Dent 17:11–25
Caplanis N, Sigurdsson TJ, Rohrer MD, Wikesjö UME (1997) Effect of allogeneic, freeze-dried, demineralized bone matrix on guided bone regeneration in supraalveolar peri-implant defects in dogs. Int J Oral Maxillofac Implant 12:634–642
Carragee EJ, Baker RM, Benzel EC, Bigos SJ, Cheng I, Corbin TP, Deyo RA, Hurwitz EL, Jarvik JG, Kang JD, Lurie JD, Mroz TE, Oner FC, Peul WC, Rainville J, Ratliff JK, Rihn JA, Rothman DJ, Schoene ML, Spengler DM, Weiner BK (2012) A biologic without guidelines: the YODA project and the future of bone morphogenetic protein-2 research. Spine J 12:877–880
Celeste AJ, Iannazzi JA, Taylor RC, Hewick RM, Rosen V, Wang EA, Wozney JM (1990) Identification of transforming growth factor-ß family members present in bone-inductive protein purified from bovine bone. Proc Natl Acad Sci USA 87:9843–9847
Clavero J, Lundgren S (2003) Ramus or chin grafts for maxillary sinus inlay and local onlay augmentation: comparison of donor site morbidity and complications. Clin Implant Dent Relat Res 5:154–160
de Freitas RM, Susin C, Spin-Neto R, Marcantonio C, Wikesjö UME, Violin Dias Pereira LA, Marcantonio E Jr (2014a) Horizontal ridge augmentation of the atrophic anterior maxilla using rhBMP-2/ACS or autogenous bone grafts: a proof-of-concept randomized clinical trial. J Clin Periodontol 40:968–975
de Freitas RM, Spin-Neto R, Marcantonio E Jr, Pereira L A, Wikesjö UME, Susin C (2014b) Alveolar ridge and maxillary sinus augmentation using rhBMP-2: a systematic review. Clin Implant Dent Relat Res (in press)
Esposito M, Grusovin MG, Felice P, Karatzopoulos G, Worthington HV, Coulthard P (2009) The efficacy of horizontal and vertical bone augmentation procedures for dental implants—a Cochrane systematic review. Eur J Oral Implantol 2:167–184
Esposito M, Grusovin MG, Rees J, Karasoulos D, Felice P, Alissa R, Worthington H, Coulthard P (2010) Effectiveness of sinus lift procedures for dental implant rehabilitation: a Cochrane systematic review. Eur J Oral Implantol 3:7–26
Fiorellini JP, Howell TH, Cochran D, Malmquist J, Lilly LC, Spagnoli D, Toljanic J, Jones A, Nevins M (2005) Randomized study evaluating recombinant human bone morphogenetic protein-2 for extraction socket augmentation. J Periodontol 76:605–613
Hall J, Sorensen RG, Wozney JM, Wikesjö UME (2007) Bone formation at rhBMP-2 coated titanium implants in the rat ectopic model. J Clin Periodontol 34:444–451
Hanisch O, Sorensen RG, Kinoshita A, Spiekermann H, Wozney JM, Wikesjö UME (2003) Effect of recombinant human bone morphogenetic protein-2 in dehiscence defects with non-submerged immediate implants: an experimental study in Cynomolgus monkeys. J Periodontol 74:648–657
Hanisch O, Tatakis DN, Boskovic MM, Rohrer MD, Wikesjö UME (1997a) Bone formation and reosseointegration in peri-implantitis defects following surgical implantation of rhBMP-2. Int J Oral Maxillofac Implant 12:604–610
Hanisch O, Tatakis DN, Rohrer MD, Wöhrle PS, Wozney JM, Wikesjö UME (1997b) Bone formation and osseointegration stimulated by rhBMP-2 following subantral augmentation procedures in nonhuman primates. Int J Oral Maxillofac Implant 12:785–792
Hanisch O, Cortella CA, Boskovic MM, James RA, Slots J, Wikesjö UME (1997c) Experimental peri-implant tissue breakdown around hydroxyapatite-coated implants. J Periodontol 68:59–66
Henry PJ, Laney WR, Jemt T, Harris D, Krogh PH, Polizzi G, Zarb GA, Herrmann I (1996) Osseointegrated implants for single-tooth replacement: a prospective 5-year multicenter study. Int J Oral Maxillofac Implant 11:450–455
Herberg S, Siedler M, Pippig S, Schuetz A, Dony C, Kim C-K, Wikesjö UME (2008) Development of an injectable composite as a carrier for growth factor enhanced periodontal regeneration. J Clin Periodontol 3:976–984
Hong J-Y, Lee J-S, Pang E-K, Jung U-W, Choi S-H, Kim C-K (2014) Impact of different synthetic bone fillers on healing of extraction sockets: an experimental study in dogs. Clin Oral Implant Res 25:e30–e37
Horvath A, Mardas N, Mezzomo LA, Needleman IG, Donos N (2013) Alveolar ridge preservation. A systematic review. Clin Oral Invest 17:341–363
Hötten G, Neidhardt H, Jacobowsky B, Pohl J (1994) Cloning and expression of recombinant human growth/differentiation factor 5. Biochem Biophys Res Commun 204:646–652
Hötten GC, Matsumoto T, Kimura M, Bechtold RF, Kron R, Ohara T, Tanaka H, Satoh Y, Okazaki M, Shrai T, Pan H, Kawai S, Pohl JS, Kudo A (1996) Recombinant human growth/differentiation factor 5 stimulates mesenchyme aggregation and chondrogenesis responsible for the skeletal development of limbs. Growth Factors 13:65–74
Hsu WK, Wang JC (2008) The use of bone morphogenetic protein in spine fusion. Spine J 8:419–425
Hunt DR, Jovanovic SA, Wikesjö UME, Wozney JM, Bernard GW (2001) Hyaluronan supports recombinant human bone morphogenetic protein-2 induced bone reconstruction of advanced alveolar ridge defects in dogs. A pilot study. J Periodontol 72:651–658
Jovanovic SA, Hunt DR, Bernard GW, Spiekermann H, Nishimura R, Wozney JM, Wikesjö UME (2003) Long-term functional loading of dental implants in rhBMP-2 induced bone. A histologic study in the canine ridge augmentation model. Clin Oral Implant Res 14:793–803
Jovanovic SA, Hunt DR, Bernard GW, Spiekermann H, Wozney JM, Wikesjö UME (2007) Bone reconstruction following implantation of rhBMP-2 and guided bone regeneration in canine alveolar ridge defects. Clin Oral Implant Res 18:224–230
Kao DW, Kubota A, Nevins M, Fiorellini JP (2012) The negative effect of combining rhBMP-2 and Bio-Oss on bone formation for maxillary sinus augmentation. Int J Periodontics Restorative Dent 32:61–67
Lacroix P (1945) Recent investigations on the growth of bone. Nature 156:576
Laine C, Guallar E, Mulrow C, Taichman DB, Cornell JE, Cotton D, Griswold ME, Localio AR, Meibohm AR, Stack CB, Williams SV, Goodman SN (2013) Closing in on the truth about recombinant human bone morphogenetic protein-2: evidence synthesis, data sharing, peer review, and reproducible research. Ann Intern Med 158:916–918
Lee J, Susin C, Rodriguez NA, de Stefano J, Prasad HS, Buxton AN, Wikesjö UME (2013a) Sinus augmentation using rhBMP-2/ACS in a mini-pig model: relative efficacy of autogenous fresh particulate iliac bone grafts. Clin Oral Implant Res 24:497–504
Lee J, Lee EN, Yoon J, Chung S-M, Prasad H, Susin C, Wikesjö UME (2013b) Comparative study of Chinese hamster ovary cell versus Escherichia coli-derived bone morphogenetic protein-2 using the critical-size supraalveolar peri-implant defect model. J Periodontol 84:415–422
Lekholm U, Gunne J, Henry P, Higuchi K, Lindén U, Bergström C, van Steenberghe D (1999) Survival of the Brånemark implant in partially edentulous jaws: a 10-year prospective multicenter study. Int J Oral Maxillofac Implant 14:639–645
Leknes KN, Yang J, Qahash M, Polimeni G, Susin C, Wikesjö UME (2008) Alveolar ridge augmentation using implants coated with recombinant human bone morphogenetic protein-2 (rhBMP-2). Radiographic observations. Clin Oral Implant Res 19:1027–1033
Levander G (1938) A study of bone regeneration. J Surg Gynecol Obstet 67:705–714
Lu SX, Fiorini T, Lee J, Prasad HS, Buxton AN, Bisch FC, Dixon DR, Susin C, Wikesjö UME (2013) Evaluation of a compression resistant carrier for recombinant human bone morphogenetic protein-2. J Clin Periodontol 40:688–697
McKay WF, Peckham SM, Badura JM (2007) A comprehensive clinical review of recombinant human bone morphogenetic protein-2 (INFUSE® Bone Graft). Int Orthop 31:729–734
Miranda DAO, Blumenthal NM, Sorensen RG, Wozney JM, Wikesjö UME (2005) Evaluation of recombinant human bone morphogenetic protein-2 on the repair of alveolar ridge defects in baboons. J Periodontol 76:210–220
Özkaynak E, Rueger DC, Drier EA, Corbett C, Ridge RJ, Sampath TK, Oppermann H (1990) OP-1 cDNA encodes an osteogenic protein in the TGF-ß family. EMBO J 9:2085–2093
Pinholt EM, Haanaes HR, Roervik M, Donath K, Bang G (1992) Alveolar ridge augmentation by osteoinductive materials in goats. Scand J Dent Res 100:361–365
Pöhling S, Pippig SD, Hellerbrand K, Siedler M, Schütz A, Dony C (2006) Superior effect of MD05, beta-tricalcium phosphate coated with recombinant human growth/differentiation factor-5, compared to conventional bone substitutes in the rat calvarial defect model. J Periodontol 77:1582–1590
Resnick D, Bozic KJ (2013) Meta-analysis of trials of recombinant human bone morphogenetic protein-2: what should spine surgeons and their patients do with this information? Ann Intern Med 158:912–913
Sampath TK, Maliakal JC, Hauschka PV, Jones WK, Sasak H, Tucker RF, White KH, Coughlin JE, Tucker MM, Pang RH, Corbett C, Özkaynak E, Oppermann H, Rueger D (1992) Recombinant human osteogenic protein-1 (hOP-1) induces new bone formation in vivo with a specific activity comparable with natural bovine osteogenic protein and stimulates osteoblast proliferation and differentiation in vitro. J Biol Chem 267:20352–20362
Sigurdsson TJ, Fu E, Tatakis DN, Rohrer MD, Wikesjö UME (1997) Bone morphogenetic protein-2 for peri-implant bone regeneration and osseointegration. Clin Oral Implant Res 8:367–374
Sigurdsson TJ, Nguyen S, Wikesjö UME (2001) Alveolar ridge augmentation with rhBMP-2 and bone-to-implant contact in induced bone. Int J Periodontics Restorative Dent 21:461–473
Sigurdsson TJ, Nygaard L, Tatakis DN, Fu E, Turek TJ, Jin L, Wozney JM, Wikesjö UME (1996) Periodontal repair in dogs: evaluation of rhBMP-2 carriers. Int J Periodontics Restorative Dent 16:525–537
Simion M, Fontana F, Rasperini G, Maiorana C (2007) Vertical ridge augmentation by expanded-polytetrafluoroethylene membrane and a combination of intraoral autogenous bone graft and deproteinized anorganic bovine bone (Bio Oss). Clin Oral Implant Res 18:620–629
Summers RB (1994) The osteotome technique: part 3–less invasive methods of elevating the sinus floor. Compendium Continuing Educ Dent 15:698–704
Tatakis DN, Koh A, Jin L, Wozney JM, Rohrer MD, Wikesjö UME (2002) Peri-implant bone regeneration using rhBMP-2/ACS in a canine model: a dose-response study. J Periodontal Res 37:93–100
Triplett RG, Nevins M, Marx RE, Spagnoli DB, Oates TW, Moy PK, Boyne PJ (2009) Pivotal, randomized, parallel evaluation of recombinant human bone morphogenetic protein-2/absorbable collagen sponge and autogenous bone graft for maxillary sinus floor augmentation. J Oral Maxillofac Surg 67:1947–1960
Urist MR (1965) Bone: formation by autoinduction. Science 150:893–899
von Arx T, Cochran DL, Hermann JS, Schenk RK, Buser D (2001) Lateral ridge augmentation using different bone fillers and barrier membrane application. A histologic and histomorphometric pilot study in the canine mandible. Clin Oral Implant Res 12:260–269
Wang EA, Rosen V, D’Alessandro JS, Bauduy M, Cordes P, Harada T, Israel DI, Hewick RM, Kerns KM, LaPan P, Luxenburg DP, McQuaid D, Moutsatsos IK, Nove J, Wozney JM (1990) Recombinant human bone morphogenetic protein induces bone formation. Proc Natl Acad Sci USA 87:2220–2224
Wikesjö UME, Sorensen RG, Kinoshita A, Wozney JM (2002) rhBMP-2/α-BSM® induces significant vertical alveolar ridge augmentation and dental implant osseointegration. Clin Implant Dent Relat Res 4:173–181
Wikesjö UME, Qahash M, Thomson RC, Cook AD, Rohrer MD, Wozney JM, Hardwick WR (2003) Space-providing expanded polytetrafluoroethylene devices define alveolar augmentation at dental implants induced by recombinant human bone morphogenetic protein-2. Clin Implant Dent Relat Res 5:112–123
Wikesjö UME, Qahash M, Thomson RC, Cook AD, Rohrer MD, Wozney JM, Hardwick WR (2004) rhBMP-2 Significantly enhances guided bone regeneration. Clin Oral Implant Res 15:194–204
Wikesjö UME, Susin C, Qahash M, Polimeni G, Leknes KN, Shanaman RH, Prasad HS, Rohrer MD, Hall J (2006) The critical-size supraalveolar peri-implant defect model: characteristics and use. J Clin Periodontol 33:846–854
Wikesjö UME, Xiropaidis AV, Qahash M, Lim WH, Sorensen RG, Rohrer MD, Wozney JM, Hall J (2008a) Bone formation at recombinant human bone morphogenetic protein-2-coated titanium implants in the posterior mandible (type II bone) in dogs. J Clin Periodontol 35:985–991
Wikesjö UME, Huang Y-H, Xiropaidis AV, Sorensen RG, Rohrer MD, Prasad HS, Wozney JM, Hall J (2008b) Bone formation at recombinant human bone morphogenetic protein-2-coated titanium implants in the posterior maxilla (type IV bone) in nonhuman primates. J Clin Periodontol 35:992–1000
Wikesjö UME, Qahash M, Polimeni G, Susin C, Shanaman RH, Rohrer MD, Wozney JM, Hall J (2008c) Alveolar ridge augmentation using implants coated with recombinant human bone morphogenetic protein-2. Histologic observations. J Clin Periodontol 35:1001–1010
Wikesjö UME, Qahash M, Huang Y-H, Xiropaidis AV, Polimeni G, Susin C (2009a) Bone morphogenetic proteins for periodontal and alveolar indications; biological observations—clinical implications. Orthod Craniofac Res 12:263–270
Wozney JM, Rosen V, Celeste AJ, Mitsock LM, Whitters MJ, Kriz RW, Hewick RM, Wang EA (1988) Novel regulators of bone formation: molecular clones and activities. Science 242:1528–1534
Further Reading
Fiorini T, Susin C, Lee J, Wikesjö UME (2011) Animal models for alveolar bone augmentation (Chapter 9). In: Ballo A (ed) Implant dentistry research guide: basic, translation and clinical research. Nova Publishers, Hauppauge, NY
Huang Y-H, Polimeni G, Qahash M, Wikesjö UME (2008) Bone morphogenetic proteins and osseointegration. Current knowledge—future possibilities. Periodontol 2000 (47):206–223
Lee J, Fiorini T, Wikesjö UME, Susin C (2011) Animal models for sinus augmentation (Chapter 10). In: Ballo A (ed) Implant dentistry research guide: basic, translation and clinical research. Nova Publishers, Hauppauge, NY
Moreno de Freitas R, Spin-Neto R, Violin Dias Pereira LA, Marcantonio Junior E, Wikesjö UME, Susin C (2013) Alveolar ridge and maxillary sinus augmentation using rhBMP-2: systematic review. Clin Implant Dent Relat Res
Wozney JM, Wikesjö UME (2008) rhBMP-2: biology and applications in oral and maxillofacial surgery and periodontics. In: Lynch SE, Wisner-Lynch LA, Nevins M, Marx RE (eds) Tissue engineering: applications in oral and maxillofacial surgery and periodontics, 2nd edn. Quintessence Publishing Company, Chicago, pp 159–177
Wikesjö UME, Polimeni G, Qahash M (2005) Tissue engineering with recombinant human bone morphogenetic protein-2 for alveolar augmentation and oral implant osseointegration: experimental observations and clinical perspectives. Clin Implant Dent Relat Res 7:112–119
Wikesjö UME, Huang Y-H, Polimeni G, Qahash M (2007) Bone morphogenetic proteins: a realistic alternative to bone grafting for alveolar reconstruction. Oral Maxillofac Surg Clin North America 19:535–551
Wikesjö UME, Simion M, Reddy MS (2008) Alveolar augmentation: past, present, and future. In: Jokstad A (ed) Osseointegration and dental implants. Proceedings from the Toronto osseointegration conference revisited, 9–10 May 2008, Wiley-Blackwell, Oxford, pp 183–196 (Chapter 9, Biomaterials and substances for site optimizing)
Wikesjö UME, Qahash M, Huang Y-H, Xiropaidis AV, Polimeni G, Susin C (2009b) Bone morphogenetic proteins for periodontal and alveolar indications; biological observations—clinical implications. Orthod Craniofac Res 12:263–270
Wikesjö UME, Lee J, Susin C (2010) Bone, bone morphogenetic protein-2, implant dentistry: focused review. In: Gottlander R, van Steenberghe D (eds) Proceedings of the First P-I Brånemark Scientific Symposium, Gothenburg 2009. Osseointegration and related treatment modalities: future perspectives, quality of life, and treatment simplification. Quintessence Publishing Company, Chicago, pp 61–71
Acknowledgments
Earlier versions of this text have been published for reviews in journals and book chapters. The text is continuously subject to revisions and updating as new information becomes available in our laboratory. Studies elaborated herein conducted in our laboratories were supported by WL Gore and Associates, Genetics Institute, Wyeth Research, Medtronic, Daewoong Pharmaceuticals and Nobel Biocare.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Wikesjö, U.M.E., Susin, C., Lee, J. (2015). Alveolar Augmentation: Focus on Growth Factors (BMPs). In: Zreiqat, H., Dunstan, C., Rosen, V. (eds) A Tissue Regeneration Approach to Bone and Cartilage Repair. Mechanical Engineering Series. Springer, Cham. https://doi.org/10.1007/978-3-319-13266-2_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-13266-2_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-13265-5
Online ISBN: 978-3-319-13266-2
eBook Packages: EngineeringEngineering (R0)