Abstract
Not only is stroke second only to cardiac ischemia as a leading cause of death worldwide, but it also drastically impaired the quality of life of the survivors through its crippling neurological sequelae which account for the third leading cause of disability. Instead of merely a loss of functioning neurons from ischemia, stroke triggers a cascade of adverse events including inflammation, oxidative stress, and apoptosis that perpetuates the initial ischemic damage. Current therapeutic strategies, including the use of thrombolytic agents and other non-pharmaceutical approaches, have their limitations either because of the risk of complications or focusing only on the prevention of brain damage and rehabilitation. More importantly, none has been convincingly shown to improve neurological outcome in patients with stroke once the brain tissue is infarcted. Accumulating evidence has indicated that, instead of being only neuroprotective, stem cells actually possess neurorestorative function for promoting recovery of the injured brain tissue. Accordingly, cell transplant therapy with adipose-derived mesenchymal stem cells (ADSC) has recently emerged as a potentially feasible therapeutic option not only because of their abundance and relative ease of being harvested, but also because of the possibility of autologous implantation and their demonstrated multiple beneficial biological actions against stroke in experimental settings, namely paracrine effects, transdifferentiation, and immunomodulation, that could enhance brain plasticity such as neurogenesis, remyelination, synaptogenesis, and angiogenesis in the recovery process. The nature and source of ADSC as well as their demonstrated therapeutic potential against stroke, the clinical perspective in stroke treatment, and the potential risks are reviewed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
1.1 The Layout of the Chapter
To cover the essential knowledge on this topic, the chapter is divided into several sections, including an outline of stroke as a life-threatening disease and the current medical strategies, the introduction of adipose-derived mesenchymal stem cells (ADSC) as a treatment tool for stroke and its therapeutic advantages, description of the general methodology of ADSC isolation, the mechanisms of action of ADSC against stroke, the current status of experimental and clinical studies as well as the perspectives of ADSC applications and the potential risks and limitations.
1.2 Stroke, Current Treatment Strategies, and Their Limitations
Stroke, which can be of ischemic or hemorrhagic origins due to a disruption of blood supply to the brain tissue, has been reported to be the second leading cause of death worldwide (Feigin et al. 2014). Not only is stroke a ruthless killer, but it also leaves behind devastating neurological deficits (i.e., those of motor, sensory, and cognitive) that account for their being the third leading cause of disability (Rosado-de-Castro et al. 2013). The cost for chronic care and rehabilitation as well as the remarkable impairment of the quality of life for the affected individuals impose an enormous socioeconomic burden on a society (Go et al. 2013).
The current mainstay of treatment for acute ischemic stroke, which accounts for over 80 % of all cases of stroke (Liu et al. 2013), includes the use of thrombolytic agents (e.g. recombinant tissue plasminogen activator, rtPA) that are supposed to be given within 4.5 h after the attack (Del Zoppo et al. 2009) with the hope of resuming patency of the supplying artery to restore the function of tissue surrounding the core region of infarction (i.e. ischemic penumbra) to minimize the ischemic insult rather than the irreversible infarction itself (Smith et al. 2011). However, the narrow therapeutic time window and the significant risk of symptomatic intracranial hemorrhage (i.e. up to 5.6 %) and death (Wardlaw et al. 2009; Seet and Rabinstein 2012) substantially hinder its use which is only suitable for only 2–4 % of patients with ischemic stroke (Molina 2011). The popularity of rtPA use is further hampered by its limited efficacy in disability prevention which is only six patients per 1000 ischemic strokes and its lack of beneficial impact on mortality rate (Hacke et al. 2004). As a result, various non-pharmaceutical strategies have been proposed including neuroprotective approaches such as hypothermia, ischemic/hypoxic conditioning, acupuncture, certain medical gases, and transcranial laser therapy as well as mechanical endovascular recanalization and recovery devices for treating the chronic phase of stroke (Chen et al. 2014b).
Since ischemic injury of the brain involves a cascade of events, a multi-faceted therapeutic approach is preferred (Chen et al. 2014b). The clinical possibility of cell therapy (i.e., “cell replacement therapy” or “cell transplant therapy”) for central nervous system disorders, including stroke, gained much attention in the year 2000 (Bjorklund and Lindvall 2000; Zivin 2000) when the first clinical trial on neuronal cellular transplantation in patients with stroke was reported (Kondziolka et al. 2000). Although it was not stem cell that was transplanted, it opened up the avenue for exploring the therapeutic potential of stem cell transplantation for stroke (Cairns and Finklestein 2003).
1.3 Stem Cells: Their Natures, Sources, and Therapeutic Potentials
The two distinctive properties that distinguish stems cells from other somatic cells are “self-renewal” and “potency” (Kuhl and Kuhl 2013). Self-renewal refers to the process in which a stem cell undergoes mitotic cell division to produce at least one daughter cell with equal developmental potential as the mother cell, in other words, another stem cell . On the other hand, potency is the ability of a stem cell to differentiate into different mature specialized cell types (i.e. multi-lineage differentiation). Regarding the use of stems cells in the treatment of stroke, experimental studies using embryonic stem cells (Chang et al. 2013; Drury-Stewart et al. 2013), mesenchymal stem cells (Ikegame et al. 2011), hematopoietic stem cells (Tsuji et al. 2014), neural stem cells (Andres et al. 2011), induced pluripotent stem cells (iPSC) (Oki et al. 2012), and also multipotent adult progenitor cells (Mora-Lee et al. 2012) in animal models of stroke have been reported with unanimous positive therapeutic results. Although mesenchymal stem cells were first identified four decades ago as adherent cells with fibroblastoid morphology being able to differentiate into cells of mesodermal origin such as osteocytes, chondrocytes, and adipocytes (Friedenstein et al. 1974), they were later found to be also capable of differentiating into ectodermal and endodermal elements (Lakshmipathy and Verfaillie 2005; Ikegame et al. 2011). The fact further highlights their observed therapeutic versatility against a variety of diseases of different pathological origins as reflected in their abilities of vascular endothelial (Li et al. 2013a), neuronal (Gao et al. 2013), and musculoskeletal (Gardner et al. 2013) repairs.
2 Adipose-Derived Stem Cells: Therapeutic Advantages, Sources, and Isolation
2.1 Advantages of Therapeutic use of Adipose-Derived Mesenchymal Stem Cells Compared with Stem Cells of Other Origins
Compared with embryonic stem cells , autologous mesenchymal stem cells have the advantage of being self-derived without the concern of ethics and that of possible infection from unknown donors. The reported sources of mesenchymal stem cells include bone marrow (Skvortsova et al. 2008), adipose tissue (Gutierrez-Fernandez et al. 2013a), embryo (Liu et al. 2009), placenta (Kranz et al. 2010), dental pulp and periodontal ligament (Moshaverinia et al. 2014; Vasandan et al. 2014). Other sources, including palatine tonsil (Janjanin et al., 2008), dermis (Feisst et al. 2014), and skeletomuscular system (Aydin et al. 2014; Mason et al. 2014), have also been reported. In particular, the two most readily available sources of autologous ADSC, bone marrow and adipose tissue, have been widely investigated both experimentally and clinically regarding their therapeutic potentials in treating a myriad of diseases, especially ischemic and microvascular disorders (Calio et al. 2014; Liu et al. 2014).
Previous studies have shown that not only are adipose-derived stem cells (ADSC) (also known as “adipose-derived mesenchymal stem cells”, “adipose tissue-derived multipotent stromal cells” or “adipose-derived mesenchymal stromal cells”) relatively easy to obtain with less invasive procedures compared to bone marrow stem cells, but the former also exhibit better proliferative activity, differentiating capacity, immunomodulatory function, and trophic factor-releasing ability than the latter including greater production of vascular endothelial growth factor (VEGF), angiopoietin-1, and hepatocyte growth factor (HGF) (Ikegame et al., 2011) as well as interleukin 1 receptor (IL-1R), IL-6, IL-8, granulocyte colony-stimulating factor (G-CSF), granulocyte-macrophage colony-stimulating factor (GM-CSF), monocyte chemotactic protein 1, nerve growth factor (Banas et al., 2008; Ikegame et al. 2011), and transforming growth factor (TGF)-β1 (Melief et al. 2013b). Furthermore, the lack of major histocompatibility complex class II (MHC-II) expression in adipose-derived stem cells also enables their storage and allogeneic administration to individuals with acute ischemic stroke (Gutierrez-Fernandez et al. 2012). On the other hand, although the discovery of iPSC seems to offer a solution to the problem of the limited availability of stem cells through reprogramming of autologous somatic cells (Takahashi and Yamanaka, 2006), the requirement for the activation of potentially tumorigenic genes (e.g. c-myc) for its induction (Araki et al. 2011) has raised much clinical concerns. ADSC, therefore, appear to be an applicable clinical tool for routine clinical practice.
2.2 Source- and Donor-Dependent Variability in ADSC Quality
Previous animal experimental studies have used adipose tissue from different regions for autologous ADSC isolation, including inguinal (Chen et al. 2012) and peri-epididymal (Leu et al. 2010; Jiang et al. 2014) fat depots. Besides, other studies using human ADSC for animal studies also showed positive therapeutic results (Kang et al. 2003b; Kim et al. 2007; Yang et al. 2012; Liu et al. 2014). Therefore, it appears that the source of ADSC has no remarkable bearing on the treatment outcomes. As a result, although subcutaneous adipose tissue especially that from the abdomen, thigh, and buttock removed through fat-extracting body-shaping procedures such as liposuction and lipectomy (Chia and Theodorou 2012) used to be regarded as medical waste products, it now serves as a readily available clinical source of adipose-derived stem cells. On the issue of the optimal source of ADSC, a previous clinically-oriented study comparing the properties of ADSC isolated from human adipose tissues of different depots, including abdominal subcutaneous fat, omentum, pericardial adipose tissue, and thymic remnants, has demonstrated that ADSC isolated from different sources exhibited varied proliferation and differentiation capacities that should be taken into account to serve a specific therapeutic purpose (Russo et al. 2014). For instance, ADSC isolated from intrathoracic depots exhibited a longer average doubling time and a higher proportion of CD34+ cells compared with those isolated from subcutaneous fat or the omentum. Moreover, subcutaneous and pericardial adipose tissue yielded ADSC with enhanced adipogenic differentiation potential, while ADSC from the omentum displayed high levels of osteogenic markers (Russo et al. 2014). Another study that underscores the importance of the origins of ADSC from a therapeutic point of view is its finding that adipose tissues of slightly different origins in close vicinity (i.e., epicardial fat, pericardial fat, and the right atrium) exhibited significantly different capacities of secreting trophic and inflammatory cytokines, different degrees of upregulation of inflammation- and fibrosis-related genes, as well as different therapeutic effects in a rat model of myocardial infarction to which mesenchymal stem cells from right atrium and epicardial fat were even found to be detrimental (Naftali-Shani et al. 2013). On the other hand, specific origins of ADSC may also be taken into account for special therapeutic needs. For instance, a clonogenic population of metabolically active stem cells has been reported to reside in adult human brown adipose tissue that may be activated to participate in energy homeostasis in vivo and, therefore, may be of therapeutic importance for obesity and related metabolic disorders (Silva et al. 2014).
The correlation between donor-dependent variability and the quality of ADSC has also been widely investigated. For instance, one study demonstrated a negative association of donor age with the proliferation and differentiation potential of ADSC (Choudhery et al. 2014). Donors of advanced age has also been reported to reduce the yield of ADSC expressing low-affinity nerve growth factor receptor (CD271) (Cuevas-Diaz Duran et al. 2013) and also produce ADSC of impaired angiogenic capacities (De Barros et al. 2013). On the other hand, infant-derived cells have been shown to be morphologically more elongated with long telomeres, and exhibit augmented angiogenic and osteogenic abilities compared with older cells (Wu et al. 2013). Nevertheless, other studies using adipose tissue from human adults showed that donor age, body-mass index, and harvest site do not influence cell yield and proliferation rate (Buschmann et al. 2013). Moreover, doubling time, telomere length, the osteogenic and chondrogenic differentiation capacity, as well as osteogenic paracrine activity were also found to be similar among ADSC from adult donors of different ages (Ding et al. 2013; Wu et al. 2013). Consistently, another experimental study investigating the impact of donor age on the function of adipose-derived stem cells also demonstrated that aged ADSC from rats still retained potential to support axon regeneration (Mantovani et al. 2012). One interesting finding is that ADSC from older donors were found to exhibit compromised adipogenic potential that actually favors their application in regeneration therapy (Ding et al. 2013). The overall promising proliferation and differentiation capabilities of ADSC regardless of the donor’s age, therefore, open up an avenue to their clinical application, taken into account that the elderly will be the greatest beneficiaries of autologous stem cell treatment. On the other hand, the morphology, proliferation rate, and doubling time of ADSC have also been shown to vary with the nature of the coatings on which they were cultured (Marycz et al. 2013).
2.3 Isolation, Culture, and Identification of Adipose-Derived Mesenchymal Stem Cells
The isolation, culturing, and identification of ADSC are straightforward, including the procedures of mincing, digestion, filtering, centrifugation, culturing, and flow cytometric identification as described previously (Leu et al. 2010). Briefly, the harvested adipose tissue is minced into < 1 mm3 size pieces using a pair of sharp, sterile surgical scissors to maximize the surface areas for enzyme digestion (Fig. 9.1). Then 200–300 μL of sterile saline is added to every 0.5 g of tissue to prevent dehydration. Sterile saline (37 °C) is added to the homogenized adipose tissue in a ratio of 3:1 (saline: adipose tissue), followed by the addition of stock collagenase solution to a final concentration of 0.5 Units/mL. The tubes with the contents are placed and secured on a Thermaline shaker and incubated with constant agitation for 60 ± 15 min at 37 °C. After 40 min of incubation, the content is triturated with a 25 mL pipette for 2–3 min. The cells obtained are placed back to the rocker for incubation. The contents of the flask were transferred to 50 mL tubes after digestion, followed by centrifugation at 600 g, for 5 min at room temperature. The fat layer and saline supernatant from the tube are poured out gently in one smooth motion or removed using vacuum suction. The cell pellet thus obtained is resuspended in 40 mL saline and then centrifuged again at 600 g for 5 min at room temperature. After being resuspended again in 5 mL saline, the cell suspension is filtered through a 100 μm filter into a 50 mL conical tube to which 2 mL of saline is added to rinse the remaining cells through the filter. The flow-through is pipetted to a 40 μm filter into a new 50 mL conical tube. The tubes are centrifuged for a third time at 600 g for 5 min at room temperature. The cells, which are a mixture of lymphocytes, macrophages, fibroblasts , endothelial cells, and other cell populations, are resuspended in saline. An aliquot of cell suspension can then be removed for cell culturing in DMEM-low glucose medium contain 10 % FBS for two weeks. Flow cytometric analysis is subsequently used for the identification of cellular characteristics after cell labeling with appropriate antibodies. The flow cytometric characteristics and typical morphology of ADSC are also shown in Fig. 9.1. A previous study comparing the phenotypes of different mesenchymal stem cells isolated from human term placental chorionic villi, umbilical cord , adult bone marrow and adipose tissue demonstrated that, although the phenotypes were mostly similar among stem cells of different origins, vascular cell adhesion molecule 1 (VCAM-1) (i.e. CD106) was highly expressed on chorionic villi-derived mesenchymal stem cells, whereas it was moderately expressed on bone marrow-derived mesenchymal stem cells and absent on ADSC (Yang et al. 2013). Another study also showed consistent results (Zhu et al. 2012).
Simplified procedures of harvesting, processing, culturing, and characterization of adipose-derived stem cells. After being removed from the human body through procedures such as liposuction and lipectomy, the adipose tissue is minced to small pieces of size less than 1 mm3 to maximize the efficiency of enzymatic digestion for freeing the cells from connective tissue. After cell-harvesting through filtration and centrifugation, the cells are purified with the number of cells expanded through culturing. The cultured cells subsequently undergo flow cytometric analysis for the identification of surface markers characteristic of mesenchymal stem cells. (Note the typical spindle-shaped morphology of mesenchymal stem cells at right lower corner)
2.4 Automated Devices for Adipose-Derived Stem Cell Isolation
Compared with other tissues from which stem cells are isolated, adipose tissue has been shown to have at least two log greater concentrations of available stem and progenitor cells. This knowledge enables the direct utilization of these useful cellular elements without prior ex vivo expansion (Hicok and Hedrick 2011). Indeed, the Celution system, which is a closed, commercially available automated platform for adipose tissue processing for the isolation of adipose-derived stem and progenitor cells, has been described in 2011 (Hicok and Hedrick 2011). The system has been reported to take only 2.5 h for processing and successfully applied clinically (Marino et al. 2013). The “stromal vascular fraction” (SVF) thus obtained comprises both live and dead cells. Therefore, one noteworthy concern is that the cell debris may contribute to subsequent inflammatory responses that would potentially alter cell differentiation (Ye and Gimble 2011). Accordingly, several approaches have been proposed for retrieving the viable cells from SVF, including fluorescence-activated cell sorting (FACS), magnetic activated cell sorting (MACS), and dielectrophoresis (Wu and Morrow 2012). The former two involve the use of antibodies, while the latter retrieves life cells based on the presence of charge on their surface.
3 ADSC as a Therapeutic Option Against Stroke: Principles and Mechanisms
3.1 Therapeutic Actions of ADSC Implicated in Pathophysiological Changes of Stroke
The therapeutic role of ADSC against stroke could best be understood by reviewing the essential pathological changes and the physiological recovery mechanisms involved. Ischemia-induced inflammatory responses in stroke involve not just the neurons, but also other components of the neurovascular unit (del Zoppo 2009). This finding underscores the importance of immunomodulation in the management of stroke instead of merely restoring tissue perfusion (Iadecola and Anrather 2011). In addition, investigation of brain recovery from ischemic stroke has revealed the plasticity of the repairing process that involves axonal outgrowth and myelination (Ueno et al. 2012). Moreover, beside necrosis, apoptosis initiated after the stroke attack also results in irreversible loss of cellular elements in the central nervous system (Ouyang and Giffard 2013). Furthermore, although resuming patency of the obstructed vessel through fibrinolysis or angioplasty theoretically salvages the region at risk of ischemic infarction, the resulting ischemia-reperfusion injury actually triggers a cascade of inflammatory events (Iadecola and Anrather 2011; Liu et al. 2014). The major contributor to injuries following reperfusion is the reactive oxygen species (ROS) generated both from inflammatory cells and damaged mitochondria (Manzanero et al. 2013).
Pathologically, similar to the microscopic changes observed in animal models of stroke, evidence of reactive gliosis has been reported in human subjects after ischemic stroke including increased numbers of glial fibrillary acidic protein (GFAP)-positive reactive astrocytes and ED1-positive activated microglia as well as enhanced expression of chondroitin sulphate proteoglycans (CSPG) in the cortical penumbra regions (Huang et al. 2014). Hence, stroke involves a series of pathological changes that require a number of corresponding measures for the subsequent repairing. This is reflected in the results of a previous study that demonstrated the activation of hundreds of genes responsible for not only tissue repair, but also nervous system development and cell proliferation both in the penumbra and core of infarct as early as 24 h after ischemic stroke in rats (Ramos-Cejudo et al. 2012), highlighting the complexity of the repairing process. Since it is proposed that stem cells , which are known to participate in physiological tissue repair in various organs, may have a significant role to play in the recovery process after stroke (Gutierrez-Fernandez et al. 2012), numerous previous studies have been conducted to investigate the therapeutic potential of ADSC using the known recovery mechanisms of stroke as referring parameters.
3.2 Observed Therapeutic Effects of ADSC Against Stroke
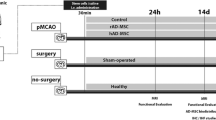
To date, most results of the therapeutic use of ADSC against stroke came from animal studies for which middle cerebral artery occlusion (MCAO) is the commonly used model. The parameters for assessment were based on the established pathological changes after stroke at molecular, cellular, and functional levels. For instance, the findings of increased levels of chemokine receptor type 4 (CXCR4), stromal cell-derived factor 1 (SDF-1), IL-8/Gro, Doublecortin (DCX) (i.e., marker of migrating neuroblasts), von Willebran factor (vWF), and endothelial cell markers as well as enhanced microvessel proliferation after ADSC treatment in a rat ischemic stroke model in one study (Leu et al. 2010), together with consistent observation of augmented expressions of basic fibroblast growth factor (bFGF) and VEGF with enhanced angiogenesis in the brain in another animal investigation (Wang et al. 2008), highlight the roles of ADSC in nerve repair and revascularization in the ischemic brain. Reinforcing evidence was provided by another study that demonstrated elevated levels of VEGF, synaptophysin (SYP), oligodendrocyte (Olig-2) and neurofilament (NF) in rats after ADSC treatment compared to those in untreated animals 14 days after MCAO (Gutierrez-Fernandez et al. 2013b). The reduction in expression of GFAP in the previous studies also signifies an amelioration of reactive gliosis after ADSC treatment (Leu et al. 2010; Gutierrez-Fernandez et al. 2013b; Jiang et al. 2014). Besides, the suppressed mRNA expressions of Bax and caspase 3 as well as the increased expression of Bcl-2 in animals with stroke after ADSC treatment compared to those in the untreated group suggest an anti-apoptotic function of ADSC (Leu et al. 2010; Jiang et al. 2014). On the other hand, intravenous infusion of human ADSC has also been reported to attenuate neurological deficits (Kim et al. 2007; Yang et al. 2012), brain edema, atrophy, glial proliferation , inflammation , and apoptosis (Kim et al. 2007) in a rat model of hemorrhagic stroke.
However, the effect of ADSC treatment on infarct volume after experimental ischemic stroke is equivocal. Although one study demonstrated a significant reduction (Leu et al. 2010), other studies demonstrated no notable change in infarct volume (Gutierrez-Fernandez et al. 2013b; Jiang et al. 2014) despite the same number of cells being administered each time (2 × 106) and the unanimous findings of significantly improved neurological function, reduced cell death, and enhanced cellular proliferation in all studies (Leu et al. 2010; Gutierrez-Fernandez et al. 2013b; Jiang et al. 2014). The discrepancies in infarct volume among the studies may partly be explained by the differences in the choice of ligation procedure (i.e. permanent (Gutierrez-Fernandez et al. 2013b) vs. transient (Leu et al. 2010; Jiang et al. 2014)), the timing and frequency of ADSC administration (once at 30 min after stroke (Gutierrez-Fernandez et al. 2013b) vs. 3 times at 0, 12 and 24 h after stroke (Leu et al. 2010) vs. once at 3 days after stroke induction (Jiang et al. 2014)), the time of sacrificing animals for histological analysis after induction (14 days (Gutierrez-Fernandez et al. 2013b) vs. 21 days (Leu et al. 2010) vs. 28 days (Jiang et al. 2014)), and the route of ADSC administration (systemic intravenous (Leu et al. 2010; Gutierrez-Fernandez et al., 2013b) vs. intra-carotid arterial (Jiang et al. 2014)). Therefore, although the timing of sacrificing animals and the route of cell injection do not seem to be the significant causes of discrepancies in the size of infarct, it appears that an early timing and increased frequency of ADSC administration (Leu et al. 2010) offered significant benefit in the reduction of infarct volume in a rodent experimental setting of ischemic stroke. Accordingly, a meta-analysis demonstrated that the efficacy in structural restoration drops by 1.5 % for each day delay in treatment and that a significant dose-response relationship exists between the number of stem cells administered and the improvement of structural outcome after ischemic stroke (Lees et al. 2012). Another interesting comparison based on animal experimentation between the therapeutic effects of autologous and allogeneic cells on structural and functional outcomes after ischemic stroke revealed that the former is more effective in preserving structural integrity, while the latter is more beneficial for functional outcome (Lees et al. 2012).
3.3 Mechanisms Underlying Therapeutic Actions of ADSC from Experimental Studies
Taken together, experimental investigations, both in vitro and in vivo, have provided significant insight into some of the mechanisms involved in repair of the nervous system after stroke. The mechanisms underlying the above-mentioned therapeutic benefits of ADSC against stroke can be summarized into (i) paracrine effects, (ii) transdifferentiation, and (iii) immunomodulation (Fig. 9.2) .
Summary of reported mechanisms underlying adipose-derived stem cell treatment for stroke. The three major mechanisms by which adipose-derived stem cells exert therapeutic functions include paracrine effects , transdifferentiation, and immunomodulation . The paracrine effects stem from the release of a variety of trophic factors from stem cells that elicit a number of biological responses such as angiogenesis, neurogenesis, and abatement of apoptosis. Transdifferentiation of stem cells involves the transformation of implanted stem cells into specific cellular elements with distinct functions and cell markers (e.g., neuron-like, endothelium-like, or glial-like cells). Immunomodulation includes stem cell-mediated modification of the immunological system, such as inhibition of T cell polarization for alleviating immune responses, suppression of transformation of monocytes to antigen-presenting immunogenic cells (e.g., dendritic cells) for inducing tolerance, and the release of various immuomodulatory cytokines for suppressing inflammatory reactions. APC: Antigen-presenting cell; VEGF: Vascular endothelial growth factor; FGF2: Fibroblast growth factor 2; HGF: Hepatocyte growth factor; IGF-1: Insulin-like growth factor-1; BMP2: Bone morphogenetic protein 2; BDNF: Brain-derived neurotrophic factor; NGF: Nerve growth factor; GFAP: Glial fibrillary acidic protein; MAP2: Microtubule-associated protein 2; NeuN: Neuronal nuclei; vWF: von Willebran factor
3.3.1 Paracrine Effects
Although several previous experimental studies have demonstrated the presence of ADSC in the brain up to several weeks after being administered , the scarcity of stem cells in brain tissue could not account for the observed therapeutic outcomes (Leu et al. 2010; Jiang et al. 2014). The finding of stem cells not yet embedded into the brain tissue (Gutierrez-Fernandez et al. 2011; Ikegame et al. 2011) also precludes the possibility of their direct participation as fully functional neurons, implying their help through other mechanisms in the recovery process (Gutierrez-Fernandez et al. 2011). In concert with that finding, ADSC has been reported to produce a number of trophic factors including VEGF, angiopoietin-1, and HGF (Ikegame et al. 2011), insulin-like growth factor-1 (IGF-1) (Wei et al. 2009), TGF-β1 (Melief et al. 2013b), bone morphogenetic protein 2 (BMP2) and fibroblast growth factor 2 (FGF2) (Moriyama et al. 2012) as well as nervous system-related molecules including nerve growth factor (Banas et al. 2008; Ikegame et al. 2011), brain-derived neurotrophic factor (BDNF) (Iadecola and Anrather 2011; Liu et al. 2014), GFAP, nestin, and microtubule-associated protein 2 (MAP2) (Yang et al. 2011). Therefore, based on the actions of these trophic factors, it is rational to attribute the observed enhancement of angiogenesis and neurogenesis as well as the abatement of apoptosis to the paracrine effects of the administered ADSC (Leu et al. 2010; Gutierrez-Fernandez et al. 2012) .
Consistently, another intriguing finding is the discovery of therapeutic effects against stroke using cell-free ADSC culture medium (Cho et al. 2012; Egashira et al. 2012). One study applying human adipose-derived stem cell-conditioned medium to the lateral ventricle of a rat model of ischemic stroke 8 h after MCAO continuously for 7 days demonstrated not only a reduction of infarction volume and preservation of motor function, but also enhanced endothelial cell proliferation , reduced neural cell apoptosis, and suppressed astrogliosis in the penumbra regions (Cho et al. 2012). Another similar study using intracerebroventricular administration of concentrated murine adipose-derived stem cell-conditioned medium in a murine model of MCAO-induced ischemic stroke shed some light on the importance of the timing of treatment (Egashira et al. 2012). The result of that study showed that, while administration of conditioned medium prior to MACO exhibited a dose-dependent reduction in infarction volume of the brain and administration 5 min after MACO was still effective, the therapeutic effect vanished if conditioned medium was administered 2 h after MCAO (Egashira et al. 2012). By contrast, the former study reported effectiveness up to 8 h after MCAO before starting conditioned medium treatment (Cho et al. 2012). Other than the possible variations arising from the differences in the source of conditioned medium and the animal model used, the discrepancy in therapeutic effects between the two studies appears to be due to the way of conditioned medium administration. While the former adopted the approach of continuous intracerebroventricular infusion (Cho et al. 2012), the latter used single intracerebroventricular injection (Egashira et al. 2012) . Again, consistent with the results of previous experimental studies using ADSC transplantation for ischemic stroke (Leu et al. 2010; Gutierrez-Fernandez et al. 2012), it appears that early timing and repeated (if not continuous) treatment are of therapeutic advantage for both ADSC transplantation and conditioned medium therapy. In vitro, murine ADSC-derived conditioned medium has also been demonstrated to reduce glutamate-induced excitotoxicity in human neuroblastoma cells (Egashira et al. 2012).
3.3.2 Transdifferentiation
The role of direct cell participation regarding the use of ADSC for the treatment of ischemic stroke remains controversial. Previous studies using bone marrow-derived mesenchymal stem cells demonstrated that physical presence of the infused stem cells depends on the route of administration. Implantation of stem cells in the injured brain was evident when the cells were given through the carotid artery (Gutierrez-Fernandez et al. 2011; Jiang et al. 2014) but not through the intravenous route (Gutierrez-Fernandez et al. 2011) . Neurological deficits, however, were improved regardless of the presence of implanted stem cells in the brain (Gutierrez-Fernandez et al. 2011; Jiang et al. 2014), raising the question regarding the therapeutic significance of stem cell implantation in stroke. Indeed, it has been shown that only a small fraction (around 0.02 %) of intravenously administered bone marrow-derived hematopoietic stem cells migrate to the ischemic brain, and most of the transplanted cells express microglial but not neural protein markers (Schwarting et al. 2008). For ADSC, while a study failed to identify evidence of migration or implantation of cells into the damaged brain after their intravenous injection in an animal model of stroke despite significant functional recovery (Gutierrez-Fernandez et al. 2013b), other experimental studies (Kim et al. 2007; Leu et al. 2010; Yang et al. 2012) have demonstrated presence of the transplanted ADSC several weeks after intravenous administration with the expression of von Willebran factor, a marker of endothelial cell (Kim et al. 2007; Leu et al. 2010) . Another study using ADSC to treat a rat model of hemorrhagic stroke through right lateral cerebral ventricular injection demonstrated the differentiation of the infused ADSC into neuron-like (NeuN+) and glial-like cells (GFAP+) in region surrounding the hematoma (Chen et al. 2012). Despite the relatively small number of ADSC to explain the overall functional recovery in the reported studies, their presence signifies “transdifferentitation” as a possible mechanism underlying the positive therapeutic impact (Gutierrez-Fernandez et al. 2013a). Indeed, the capacity of neural differentiation for ADSC has been extensively investigated (Cardozo et al. 2010; Kompisch et al. 2010; Liao et al. 2010; Qian et al. 2010; Abdanipour et al. 2011; Yu et al. 2011; Ahmadi et al. 2012). It has also been reported that, compared with bone marrow-derived mesenchymal stem cells , ADSC have superior neurogenic potential (Kang et al. 2004) . Consistently, previous studies using ADSC after induced neural differentiation for treating experimental ischemic stroke were also found to be effective in improving functional recovery (Kang et al. 2003b; Yang et al. 2011). On the other hand, another finding of interest is the requirement for direct physical contact between human ADSC and murine neural stem cells in vitro for induction of neuronal differentiation of the latter, further emphasizing the existence of a mechanism that involves cell-cell interaction other than that of transdifferentiation and paracrine effects in promoting neurogenesis (Kang et al. 2003a) .
3.3.3 Immunomodulation
Taking into account the immunological nature of stroke-elicited damage and the subsequent repairing process (Iadecola and Anrather 2011) , it is not surprising to find that ADSC exert their therapeutic actions at least partly through immunomodulation. Indeed, ADSC have been reported to produce a variety of immunomodulatory cytokines, including IL-1R, IL-6, IL-8, IL-18, toll-like receptor (TLR)-4, TGF-β1, plasminogen activator inhibitor-1 (PAI-1), G-CSF, GM-CSF, and monocyte chemotactic protein 1 (Banas et al. 2008; Leu et al. 2010; Ikegame et al. 2011; Melief et al. 2013b). Moreover, ADSC have been shown to suppress the differentiation of monocytes towards antigen-presenting immunogenic cells and promote differentiation towards an anti-inflammatory IL-10-producing cell type through the production of IL-6 (Melief et al. 2013a). Consistently, coculturing ADSC with allogeneic dendritic cells revealed that ADSC could negatively modulate immunity and induce immune tolerance through downregulating costimulatory molecules (i.e., CD80, CD83, CD86, and secretion of IL-12 and tumor necrosis factor (TNF)-alpha), while induce dendritic cell tolerance through upregulating indoleamine-2,3-dioxygenase (IDO). Cocultured dendritic cells were also found to inhibit CD4+ T cell activation and naive T cells toward Th1 helper cell polarization (Peng et al. 2012). Again, another credit given to ADSC as compared with bone marrow-derived mesenchymal stem cells in the aspect of immunomodulation in stroke treatment is the finding of a higher immunomodulatory capacity in the former than that in the latter (Melief et al. 2013b) .
4 Clinical Use of ADSC Against Stroke: Present Status, Perspectives, and Limitations
4.1 Clinical Application of ADSC: Probabilities and Possibilities
Given the promising experimental outcomes of applying stem cells to the treatment of stroke and the in-depth understanding of the underlying mechanisms, a number of clinical trials are either reported or still on-going in recent years despite the majority of them are small, nonrandomized, and uncontrolled. The cells administered included bone marrow mononuclear cells (Correa et al. 2005; Li et al. 2013b), bone marrow-derived mesenchymal stem cells, (Bang et al. 2005; Suarez-Monteagudo et al. 2009; Lee et al. 2010; Bringas et al. 2011; Honmou et al. 2011), human teratocarcinoma-derived neurons (Kondziolka et al. 2000), peripheral blood hematopoietic progenitor/stem cells (Chen et al. 2014a), umbilical cord-derived mesenchymal stem cells (Han et al. 2011; Jiang et al. 2013), as well as human (Rabinovich et al. 2005) and porcine fetal cells (Savitz et al. 2005). Except for premature termination of the study adopting porcine fetal cells because of overt complications (Savitz et al. 2005), the results of other published trials support the safety and effectiveness of stem cell/progenitor cells as a therapeutic tool in the clinical setting of ischemic and hemorrhagic stroke as reflected in the overall significantly improved neurological functions of the treated patients up to 5 years of follow-up (Lee et al. 2010). On the other hand, results on the use of ADSC in clinical trial have not been reported. To date, there is only one study still recruiting patients to explore the safety and effectiveness of applying autologous ADSC in patients after stroke on the National Institutes of Health clinical trial registry database (www.clinicaltrials.gov). Therefore, albeit optimistic, the exact therapeutic impact of ADSC on disease progression and functional recovery in the clinical setting of stroke remains to be elucidated for the years to come.
4.2 ADSC Against Stroke: Concerns and Speculations
Despite the promising outcomes of applying ADSC to the treatment of stroke in experimental settings, there have been serious concerns about possible tumorigenesis in the clinical scenario because of the multilineage differentiation potential of ADSC (Lee et al. 2012). A study investigating the fate of human ADSC from different human donors after being subcutaneously injected into immunodeficient SCID mice showed that the cells survived for at least 17 months with subsequent differentiation into fibroblasts of the subdermic connective tissue and into mature adipocytes of fat tissue, exclusively at the site of injection without evidence of migration or fusion with host cells (Lopez-Iglesias et al. 2011), underscoring the safety of ADSC transplantation. Moreover, the use of terminally differentiated ADSC may be a possible option for minimizing the risk especially when the protocols for in vitro transdifferentiation of ADSC into neuronal lineage have been well-documented (Cardozo et al. 2010; Kompisch et al. 2010; Liao et al. 2010; Qian et al. 2010; Abdanipour et al. 2011; Yu et al. 2011; Ahmadi et al. 2012). Indeed, the use of induced ADSC has been endorsed as a promising therapeutic option in stroke treatment (Yang et al. 2011; Shen et al. 2013). Furthermore, it has been shown that iPSC can be generated from human ADSC without transducing c-myc so that the proliferative and differentiation capacity of ADSC can be enhanced without increasing the risk of oncogenesis (Aoki et al. 2010).
On the other hand, taken into account the therapeutic advantage of early stem cell administration at the acute stage of stroke, the use of automated devices for adipose-derived stem cell isolation for direct injection without ex vivo expansion and purification may be a feasible option for daily clinical practice because of the high concentration of useful stem and progenitor cells from adipose tissue compared with other sources (Hicok and Hedrick 2011). At the other end of the spectrum, the use of gene-transfer techniques for producing stem cells over-expressing different neurotrophic factors, such as BDNF, glial derived neurotrophic factor (GDNF), or neurotrophin-3 (NT-3), has been reported to be effective options in the treatment of ischemic stroke in animal models (Chen et al. 2013). Finally, considering the wide therapeutic applicability and easy harvesting of ADSC, the establishment of autologous or allogeneic cell banks for ADSC storage to facilitate urgent or scheduled use is no longer a far-fetched idea (West et al. 2014).
Abbreviations
- ADSC:
-
Adipose-derived mesenchymal stem cells
- APC:
-
Antigen-presenting cell
- BDNF:
-
Brain-derived neurotrophic factor
- bFGF:
-
Basic fibroblast growth factor
- BMP2:
-
Bone morphogenetic protein 2
- CSPG:
-
Chondroitin sulphate proteoglycans
- CXCR4:
-
Chemokine receptor type 4
- DCX:
-
Doublecortin
- FACS:
-
Fluorescence-activated cell sorting
- FGF2:
-
Fibroblast growth factor 2
- G-CSF:
-
granulocyte colony-stimulating factor
- GDNF:
-
Glial derived neurotrophic factor
- GFAP:
-
Glial fibrillary acidic protein
- GM-CSF:
-
Granulocyte-macrophage colony-stimulating factor
- HGF:
-
Hepatocyte growth factor
- IDO:
-
Indoleamine-2,3-dioxygenase
- IGF-1:
-
Insulin-like growth factor-1
- IL:
-
Interleukin
- IL-1R:
-
Interleukin 1 receptor
- iPSC:
-
Induced pluripotent stem cells
- MACS:
-
Magnetic activated cell sorting
- MAP2:
-
Microtubule-associated protein 2
- MCAO:
-
Middle cerebral artery occlusion
- MHC-II:
-
Major histocompatibility complex class II
- NeuN:
-
Neuronal nuclei
- NF:
-
Neurofilament
- NGF:
-
Nerve growth factor
- NT-3:
-
Neurotrophin-3
- Olig-2:
-
Oligodendrocyte
- PAI-1:
-
Plasminogen activator inhibitor-1
- ROS:
-
Reactive oxygen species
- rtPA:
-
Recombinant tissue plasminogen activator
- SDF-1:
-
Stromal cell-derived factor 1
- SVF:
-
Stromal vascular fraction
- SYP:
-
Synaptophysin
- TGF-β1:
-
Transforming growth factor beta 1
- TLR-4:
-
Toll-like receptor-4
- TNF-alpha:
-
Tumor necrosis factor-alpha
- VCAM-1:
-
Vascular cell adhesion molecule 1
- VEGF:
-
Vascular endothelial growth factor
- vWF:
-
Von Willebran factor
References
Abdanipour A, Tiraihi T, Delshad A (2011) Trans-differentiation of the adipose tissue-derived stem cells into neuron-like cells expressing neurotrophins by selegiline. Iran Biomed J 15:113–121
Ahmadi N, Razavi S, Kazemi M, Oryan S (2012) Stability of neural differentiation in human adipose derived stem cells by two induction protocols. Tissue Cell 44:87–94
Andres RH, Horie N, Slikker W, Keren-Gill H, Zhan K, Sun G, Manley NC, Pereira MP, Sheikh LA, McMillan EL, Schaar BT, Svendsen CN, Bliss TM, Steinberg GK (2011) Human neural stem cells enhance structural plasticity and axonal transport in the ischaemic brain. Brain 134:1777–1789
Aoki T, Ohnishi H, Oda Y, Tadokoro M, Sasao M, Kato H, Hattori K, Ohgushi H (2010) Generation of induced pluripotent stem cells from human adipose-derived stem cells without c-MYC. Tissue Eng Part A 16:2197–2206
Araki R, Hoki Y, Uda M, Nakamura M, Jincho Y, Tamura C, Sunayama M, Ando S, Sugiura M, Yoshida MA, Kasama Y, Abe M (2011) Crucial role of c-Myc in the generation of induced pluripotent stem cells. Stem Cells 29:1362–1370
Aydin A, Duruksu G, Erman G, Subasi C, Aksoy A, Unal ZS, Karaoz E (2014) Neurogenic differentiation capacity of subacromial bursal tissue-derived stem cells. J Orthop Res 32:151–158
Banas A, Teratani T, Yamamoto Y, Tokuhara M, Takeshita F, Osaki M, Kawamata M, Kato T, Okochi H, Ochiya T (2008) IFATS collection: in vivo therapeutic potential of human adipose tissue mesenchymal stem cells after transplantation into mice with liver injury. Stem Cells 26:2705–2712
Bang OY, Lee JS, Lee PH, Lee G (2005) Autologous mesenchymal stem cell transplantation in stroke patients. Ann Neurol 57:874–882
Bjorklund A, Lindvall O (2000) Cell replacement therapies for central nervous system disorders. Nat Neurosci 3:537–544
Bringas ML, Suarez C, Sanchez C, Alvarez LM, Valdes P, Salazar S, Chongo D, Jahanshahi M (2011) Cognitive changes after stem cell transplantation in a patient with subcortical stroke. BMJ Case Rep 2011:bcr0320113944
Buschmann J, Gao S, Harter L, Hemmi S, Welti M, Werner CM, Calcagni M, Cinelli P, Wanner GA (2013) Yield and proliferation rate of adipose-derived stromal cells as a function of age, body mass index and harvest site-increasing the yield by use of adherent and supernatant fractions? Cytotherapy 15:1098–1105
Cairns K, Finklestein SP (2003) Growth factors and stem cells as treatments for stroke recovery. Phys Med Rehabil Clin N Am 14:S135–142
Calio ML, Marinho DS, Ko GM, Rodrigues R, Carbonel AF, Oyama LM, Ormanji M, Guirao TP, Calio PL, Reis LA, de Jesus Simoes M, do Nascimento TL, Teixeira Ferreira A, Bertoncini CR (2014) Transplantation of bone marrow mesenchymal stem cells decreases oxidative stress, apoptosis, and hippocampal damage in brain of a spontaneous stroke model. Free Radic Biol Med 70:141–154
Cardozo A, Ielpi M, Gomez D, Argibay P (2010) Differential expression of Shh and BMP signaling in the potential conversion of human adipose tissue stem cells into neuron-like cells in vitro. Gene Expr 14:307–319
Chang DJ, Oh SH, Lee N, Choi C, Jeon I, Kim HS, Shin DA, Lee SE, Kim D, Song J (2013) Contralaterally transplanted human embryonic stem cell-derived neural precursor cells (ENStem-A) migrate and improve brain functions in stroke-damaged rats. Exp Mol Med 45:e53
Chen C, Wang Y, Yang GY (2013) Stem cell-mediated gene delivering for the treatment of cerebral ischemia: progress and prospectives. Curr Drug Targets 14:81–89
Chen DC, Lin SZ, Fan JR, Lin CH, Lee W, Lin CC, Liu YJ, Tsai CH, Chen JC, Cho DY, Lee CC, Shyu WC (2014a) Intracerebral implantation of autologous peripheral blood stem cells in stroke patients: a randomized phase II study. Cell Transplant (in press)
Chen F, Qi Z, Luo Y, Hinchliffe T, Ding G, Xia Y, Ji X (2014b) Non-pharmaceutical therapies for stroke: mechanisms and clinical implications. Prog Neurobiol 115:246–269
Chen J, Tang YX, Liu YM, Chen J, Hu XQ, Liu N, Wang SX, Zhang Y, Zeng WG, Ni HJ, Zhao B, Chen YF, Tang ZP (2012) Transplantation of adipose-derived stem cells is associated with neural differentiation and functional improvement in a rat model of intracerebral hemorrhage. CNS Neurosci Ther 18:847–854
Chia CT, Theodorou SJ (2012) 1000 consecutive cases of laser-assisted liposuction and suction-assisted lipectomy managed with local anesthesia. Aesthetic Plast Surg 36:795–802
Cho YJ, Song HS, Bhang S, Lee S, Kang BG, Lee JC, An J, Cha CI, Nam DH, Kim BS, Joo KM (2012) Therapeutic effects of human adipose stem cell-conditioned medium on stroke. J Neurosci Res 90:1794–1802
Choudhery MS, Badowski M, Muise A, Pierce J, Harris DT (2014) Donor age negatively impacts adipose tissue-derived mesenchymal stem cell expansion and differentiation. J Transl Med 12:8
Correa P, Felix R, Mendonca ML, Freitas G, Azevedo J, Dohmann H, Alves S, Mesquita C (2005) Dual-head coincidence gamma camera FDG-PET before and after autologous bone marrow mononuclear cell implantation in ischaemic stroke. Eur J Nucl Med Mol Imaging 32:999
Cuevas-Diaz Duran R, Gonzalez-Garza MT, Cardenas-Lopez A, Chavez-Castilla L, Cruz-Vega DE, Moreno-Cuevas JE (2013) Age-related yield of adipose-derived stem cells bearing the low-affinity nerve growth factor receptor. Stem Cells Int 2013:372164
De Barros S, Dehez S, Arnaud E, Barreau C, Cazavet A, Perez G, Galinier A, Casteilla L, Planat-Benard V (2013) Aging-related decrease of human ASC angiogenic potential is reversed by hypoxia preconditioning through ROS production. Mol Ther 21:399–408
del Zoppo GJ (2009) Inflammation and the neurovascular unit in the setting of focal cerebral ischemia. Neuroscience 158:972–982
Del Zoppo GJ, Saver JL, Jauch EC, Adams HP, Jr. (2009) Expansion of the time window for treatment of acute ischemic stroke with intravenous tissue plasminogen activator: a science advisory from the American Heart Association/American Stroke Association. Stroke 40:2945–2948
Ding DC, Chou HL, Hung WT, Liu HW, Chu TY (2013) Human adipose-derived stem cells cultured in keratinocyte serum free medium: Donor’s age does not affect the proliferation and differentiation capacities. J Biomed Sci 20:59
Drury-Stewart D, Song M, Mohamad O, Guo Y, Gu X, Chen D, Wei L (2013) Highly efficient differentiation of neural precursors from human embryonic stem cells and benefits of transplantation after ischemic stroke in mice. Stem Cell Res Ther 4:93
Egashira Y, Sugitani S, Suzuki Y, Mishiro K, Tsuruma K, Shimazawa M, Yoshimura S, Iwama T, Hara H (2012) The conditioned medium of murine and human adipose-derived stem cells exerts neuroprotective effects against experimental stroke model. Brain Res 1461:87–95
Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, Moran AE, Sacco RL, Anderson L, Truelsen T, O’Donnell M, Venketasubramanian N, Barker-Collo S, Lawes CM, Wang W, Shinohara Y, Witt E, Ezzati M, Naghavi M, Murray C (2014) Global and regional burden of stroke during 1990–2010: findings from the Global Burden of Disease Study 2010. Lancet 383:245–254
Feisst V, Brooks AE, Chen CJ, Dunbar PR (2014) Characterization of mesenchymal progenitor cell populations directly derived from human dermis. Stem Cells Dev 23(6):631–642
Friedenstein AJ, Deriglasova UF, Kulagina NN, Panasuk AF, Rudakowa SF, Luria EA, Ruadkow IA (1974) Precursors for fibroblasts in different populations of hematopoietic cells as detected by the in vitro colony assay method. Exp Hematol 2:83–92
Gao S, Zhao P, Lin C, Sun Y, Wang Y, Zhou Z, Yang D, Wang X, Xu H, Zhou F, Cao L, Zhou W, Ning K, Chen X, Xu J (2013) Differentiation of human-adipose derived stem cells into neuron-like cells which are compatible with photocurable three-dimensional scaffolds. Tissue Eng Part A 20(7–8):1271–1284
Gardner OF, Archer CW, Alini M, Stoddart MJ (2013) Chondrogenesis of mesenchymal stem cells for cartilage tissue engineering. Histol Histopathol 28:23–42
Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB (2013) Heart disease and stroke statistics–2013 update: a report from the American Heart Association. Circulation 127:e6–e245
Gutierrez-Fernandez M, Rodriguez-Frutos B, Alvarez-Grech J, Vallejo-Cremades MT, Exposito-Alcaide M, Merino J, Roda JM, Diez-Tejedor E (2011) Functional recovery after hematic administration of allogenic mesenchymal stem cells in acute ischemic stroke in rats. Neuroscience 175:394–405
Gutierrez-Fernandez M, Fuentes B, Rodriguez-Frutos B, Ramos-Cejudo J, Vallejo-Cremades MT, Diez-Tejedor E (2012) Trophic factors and cell therapy to stimulate brain repair after ischaemic stroke. J Cell Mol Med 16:2280–2290
Gutierrez-Fernandez M, Rodriguez-Frutos B, Otero-Ortega L, Ramos-Cejudo J, Fuentes B, Diez-Tejedor E (2013a) Adipose tissue-derived stem cells in stroke treatment: from bench to bedside. Discov Med 16:37–43
Gutierrez-Fernandez M, Rodriguez-Frutos B, Ramos-Cejudo J, Teresa Vallejo-Cremades M, Fuentes B, Cerdan S, Diez-Tejedor E (2013b) Effects of intravenous administration of allogenic bone marrow- and adipose tissue-derived mesenchymal stem cells on functional recovery and brain repair markers in experimental ischemic stroke. Stem Cell Res Ther 4:11
Hacke W, Donnan G, Fieschi C, Kaste M, von Kummer R, Broderick JP, Brott T, Frankel M, Grotta JC, Haley EC Jr Kwiatkowski T, Levine SR, Lewandowski C, Lu M, Lyden P, Marler JR, Patel S, Tilley BC, Albers G, Bluhmki E, Wilhelm M, Hamilton S, Investigators AT, Investigators ET, Investigators Nr-PSG (2004) Association of outcome with early stroke treatment: pooled analysis of ATLANTIS, ECASS, and NINDS rt-PA stroke trials. Lancet 363:768–774
Han H, Chang SK, Chang JJ, Hwang SH, Han SH, Chun BH (2011) Intrathecal injection of human umbilical cord blood-derived mesenchymal stem cells for the treatment of basilar artery dissection: a case report. J Med Case Rep 5:562
Hicok KC, Hedrick MH (2011) Automated isolation and processing of adipose-derived stem and regenerative cells. Methods Mol Biol 702:87–105
Honmou O, Houkin K, Matsunaga T, Niitsu Y, Ishiai S, Onodera R, Waxman SG, Kocsis JD (2011) Intravenous administration of auto serum-expanded autologous mesenchymal stem cells in stroke. Brain 134:1790–1807
Huang L, Wu ZB, Zhuge Q, Zheng W, Shao B, Wang B, Sun F, Jin K (2014) Glial scar formation occurs in the human brain after ischemic stroke. Int J Med Sci 11:344–348
Iadecola C, Anrather J (2011) The immunology of stroke: from mechanisms to translation. Nat Med 17:796–808
Ikegame Y, Yamashita K, Hayashi S, Mizuno H, Tawada M, You F, Yamada K, Tanaka Y, Egashira Y, Nakashima S, Yoshimura S, Iwama T (2011) Comparison of mesenchymal stem cells from adipose tissue and bone marrow for ischemic stroke therapy. Cytotherapy 13:675–685
Janjanin S, Djouad F, Shanti RM, Baksh D, Gollapudi K, Prgomet D, Rackwitz L, Joshi AS, Tuan RS (2008) Human palatine tonsil: a new potential tissue source of multipotent mesenchymal progenitor cells. Arthritis Res Ther 10:R83
Jiang Y, Zhu W, Zhu J, Wu L, Xu G, Liu X (2013) Feasibility of delivering mesenchymal stem cells via catheter to the proximal end of the lesion artery in patients with stroke in the territory of the middle cerebral artery. Cell Transplant 22:2291–2298
Jiang W, Liang G, Li X, Li Z, Gao X, Feng S, Wang X, Liu M, Liu Y (2014) Intracarotid transplantation of autologous adipose-derived mesenchymal stem cells significantly improves neurological deficits in rats after MCAo. J Mater Sci Mater Med 25:1357–1366
Kang SK, Jun ES, Bae YC, Jung JS (2003a) Interactions between human adipose stromal cells and mouse neural stem cells in vitro. Brain Res Dev Brain Res 145:141–149
Kang SK, Lee DH, Bae YC, Kim HK, Baik SY, Jung JS (2003b) Improvement of neurological deficits by intracerebral transplantation of human adipose tissue-derived stromal cells after cerebral ischemia in rats. Exp Neurol 183:355–366
Kang SK, Putnam LA, Ylostalo J, Popescu IR, Dufour J, Belousov A, Bunnell BA (2004) Neurogenesis of Rhesus adipose stromal cells. J Cell Sci 117:4289–4299
Kim JM, Lee ST, Chu K, Jung KH, Song EC, Kim SJ, Sinn DI, Kim JH, Park DK, Kang KM, Hyung Hong N, Park HK, Won CH, Kim KH, Kim M, Kun Lee S, Roh JK (2007) Systemic transplantation of human adipose stem cells attenuated cerebral inflammation and degeneration in a hemorrhagic stroke model. Brain Res 1183:43–50
Kompisch KM, Lange C, Steinemann D, Skawran B, Schlegelberger B, Muller R, Schumacher U (2010) Neurogenic transdifferentiation of human adipose-derived stem cells? a critical protocol reevaluation with special emphasis on cell proliferation and cell cycle alterations. Histochem Cell Biol 134:453–468
Kondziolka D, Wechsler L, Goldstein S, Meltzer C, Thulborn KR, Gebel J, Jannetta P, DeCesare S, Elder EM, McGrogan M, Reitman MA, Bynum L (2000) Transplantation of cultured human neuronal cells for patients with stroke. Neurology 55:565–569
Kranz A, Wagner DC, Kamprad M, Scholz M, Schmidt UR, Nitzsche F, Aberman Z, Emmrich F, Riegelsberger UM, Boltze J (2010) Transplantation of placenta-derived mesenchymal stromal cells upon experimental stroke in rats. Brain Res 1315:128–136
Kuhl SJ, Kuhl M (2013) On the role of Wnt/beta-catenin signaling in stem cells. Biochim Biophys Acta 1830:2297–2306
Lakshmipathy U, Verfaillie C (2005) Stem cell plasticity. Blood Rev 19:29–38
Lee JS, Hong JM, Moon GJ, Lee PH, Ahn YH, Bang OY (2010) A long-term follow-up study of intravenous autologous mesenchymal stem cell transplantation in patients with ischemic stroke. Stem Cells 28:1099–1106
Lee JS, Bae GY, Lee MO, Cha HJ (2012) Oncogenic challenges in stem cells and the link to cancer initiation. Arch Pharm Res 35:235–244
Lees JS, Sena ES, Egan KJ, Antonic A, Koblar SA, Howells DW, Macleod MR (2012) Stem cell-based therapy for experimental stroke: a systematic review and meta-analysis. Int J Stroke 7:582–588
Leu S, Lin YC, Yuen CM, Yen CH, Kao YH, Sun CK, Yip HK (2010) Adipose-derived mesenchymal stem cells markedly attenuate brain infarct size and improve neurological function in rats. J Transl Med 8:63
Li M, Li S, Yu L, Wu J, She T, Gan Y, Hu Z, Liao W, Xia H (2013a) Bone mesenchymal stem cells contributed to the neointimal formation after arterial injury. PLoS One 8:e82743
Li ZM, Zhang ZT, Guo CJ, Geng FY, Qiang F, Wang LX (2013b) Autologous bone marrow mononuclear cell implantation for intracerebral hemorrhage-a prospective clinical observation. Clin Neurol Neurosurg 115:72–76
Liao D, Gong P, Li X, Tan Z, Yuan Q (2010) Co-culture with Schwann cells is an effective way for adipose-derived stem cells neural transdifferentiation. Arch Med Sci 6:145–151
Liu X, Ye R, Yan T, Yu SP, Wei L, Xu G, Fan X, Jiang Y, Stetler RA, Liu G, Chen J (2013) Cell based therapies for ischemic stroke: from basic science to bedside. Prog Neurobiol 115:92–115
Liu XL, Zhang W, Tang SJ (2014) Intracranial transplantation of human adipose-derived stem cells promotes the expression of neurotrophic factors and nerve repair in rats of cerebral ischemia-reperfusion injury. Int J Clin Exp Pathol 7:174–183
Liu YP, Seckin H, Izci Y, Du ZW, Yan YP, Baskaya MK (2009) Neuroprotective effects of mesenchymal stem cells derived from human embryonic stem cells in transient focal cerebral ischemia in rats. J Cereb Blood Flow Metab 29:780–791
Lopez-Iglesias P, Blazquez-Martinez A, Fernandez-Delgado J, Regadera J, Nistal M, Miguel MP (2011) Short and long term fate of human AMSC subcutaneously injected in mice. World J Stem Cells 3:53–62
Mantovani C, Raimondo S, Haneef MS, Geuna S, Terenghi G, Shawcross SG, Wiberg M (2012) Morphological, molecular and functional differences of adult bone marrow- and adipose-derived stem cells isolated from rats of different ages. Exp Cell Res 318:2034–2048
Manzanero S, Santro T, Arumugam TV (2013) Neuronal oxidative stress in acute ischemic stroke: sources and contribution to cell injury. Neurochem Int 62:712–718
Marino G, Moraci M, Armenia E, Orabona C, Sergio R, De Sena G, Capuozzo V, Barbarisi M, Rosso F, Giordano G, Iovino F, Barbarisi A (2013) Therapy with autologous adipose-derived regenerative cells for the care of chronic ulcer of lower limbs in patients with peripheral arterial disease. J Surg Res 185:36–44
Marycz K, Krzak-Ros J, Donesz-Sikorska A, Smieszek A (2013) The morphology, proliferation rate, and population doubling time factor of adipose-derived mesenchymal stem cells cultured on to non-aqueous SiO, TiO, and hybrid sol-gel-derived oxide coatings. J Biomed Mater Res A doi:10.1002/jbm.a.35072.
Mason S, Tarle SA, Osibin W, Kinfu Y, Kaigler D (2014) Standardization and safety of alveolar bone-derived stem cell isolation. J Dent Res 93:55–61
Melief SM, Geutskens SB, Fibbe WE, Roelofs H (2013a) Multipotent stromal cells skew monocytes towards an anti-inflammatory interleukin-10-producing phenotype by production of interleukin-6. Haematologica 98:888–895
Melief SM, Zwaginga JJ, Fibbe WE, Roelofs H (2013b) Adipose tissue-derived multipotent stromal cells have a higher immunomodulatory capacity than their bone marrow-derived counterparts. Stem Cells Transl Med 2:455–463
Molina CA (2011) Reperfusion therapies for acute ischemic stroke: current pharmacological and mechanical approaches. Stroke 42:S16–19
Mora-Lee S, Sirerol-Piquer MS, Gutierrez-Perez M, Gomez-Pinedo U, Roobrouck VD, Lopez T, Casado-Nieto M, Abizanda G, Rabena MT, Verfaille C, Prosper F, Garcia-Verdugo JM (2012) Therapeutic effects of hMAPC and hMSC transplantation after stroke in mice. PLoS One 7:e43683
Moriyama M, Moriyama H, Ueda A, Nishibata Y, Okura H, Ichinose A, Matsuyama A, Hayakawa T (2012) Human adipose tissue-derived multilineage progenitor cells exposed to oxidative stress induce neurite outgrowth in PC12 cells through p38 MAPK signaling. BMC Cell Biol 13:21
Moshaverinia A, Xu X, Chen C, Ansari S, Zadeh HH, Snead ML, Shi S (2014) Application of stem cells derived from the periodontal ligament or gingival tissue sources for tendon tissue regeneration. Biomaterials 35:2642–2650
Naftali-Shani N, Itzhaki-Alfia A, Landa-Rouben N, Kain D, Holbova R, Adutler-Lieber S, Molotski N, Asher E, Grupper A, Millet E, Tessone A, Winkler E, Kastrup J, Feinberg MS, Zipori D, Pevsner-Fischer M, Raanani E, Leor J (2013) The origin of human mesenchymal stromal cells dictates their reparative properties. J Am Heart Assoc 2:e000253
Oki K, Tatarishvili J, Wood J, Koch P, Wattananit S, Mine Y, Monni E, Tornero D, Ahlenius H, Ladewig J, Brustle O, Lindvall O, Kokaia Z (2012) Human-induced pluripotent stem cells form functional neurons and improve recovery after grafting in stroke-damaged brain. Stem Cells 30:1120–1133
Ouyang YB, Giffard RG (2013) microRNAs affect BCL-2 family proteins in the setting of cerebral ischemia. Neurochem Int (in press)
Peng W, Gao T, Yang ZL, Zhang SC, Ren ML, Wang ZG, Zhang B (2012) Adipose-derived stem cells induced dendritic cells undergo tolerance and inhibit Th1 polarization. Cell Immunol 278:152–157
Qian DX, Zhang HT, Ma X, Jiang XD, Xu RX (2010) Comparison of the efficiencies of three neural induction protocols in human adipose stromal cells. Neurochem Res 35:572–579
Rabinovich SS, Seledtsov VI, Banul NV, Poveshchenko OV, Senyukov VV, Astrakov SV, Samarin DM, Taraban VY (2005) Cell therapy of brain stroke. Bull Exp Biol Med 139:126–128
Ramos-Cejudo J, Gutierrez-Fernandez M, Rodriguez-Frutos B, Exposito Alcaide M, Sanchez-Cabo F, Dopazo A, Diez-Tejedor E (2012) Spatial and temporal gene expression differences in core and periinfarct areas in experimental stroke: a microarray analysis. PLoS One 7:e52121
Rosado-de-Castro PH, Pimentel-Coelho PM, da Fonseca LM, de Freitas GR, Mendez-Otero R (2013) The rise of cell therapy trials for stroke: review of published and registered studies. Stem Cells Dev 22:2095–2111
Russo V, Yu C, Belliveau P, Hamilton A, Flynn LE (2014) Comparison of human adipose-derived stem cells isolated from subcutaneous, omental, and intrathoracic adipose tissue depots for regenerative applications. Stem Cells Transl Med 3:206–217
Savitz SI, Dinsmore J, Wu J, Henderson GV, Stieg P, Caplan LR (2005) Neurotransplantation of fetal porcine cells in patients with basal ganglia infarcts: a preliminary safety and feasibility study. Cerebrovasc Dis 20:101–107
Schwarting S, Litwak S, Hao W, Bahr M, Weise J, Neumann H (2008) Hematopoietic stem cells reduce postischemic inflammation and ameliorate ischemic brain injury. Stroke 39:2867–2875
Seet RC, Rabinstein AA (2012) Symptomatic intracranial hemorrhage following intravenous thrombolysis for acute ischemic stroke: a critical review of case definitions. Cerebrovasc Dis 34:106–114
Shen CC, Yang YC, Chiao MT, Chan SC, Liu BS (2013) Low-level laser stimulation on adipose-tissue-derived stem cell treatments for focal cerebral ischemia in rats. Evid Based Complement Alternat Med 2013:594906
Silva FJ, Holt DJ, Vargas V, Yockman J, Boudina S, Atkinson D, Grainger DW, Revelo MP, Sherman W, Bull DA, Patel AN (2014) Metabolically active human brown adipose tissue derived stem cells. Stem Cells 32:572–581
Skvortsova VI, Gubskiy LV, Tairova RT, Povarova OV, Cheglakov IB, Holodenko RV, Holodenko IV, Yarygin KN, Yarygin VN (2008) Use of bone marrow mesenchymal (stromal) stem cells in experimental ischemic stroke in rats. Bull Exp Biol Med 145:122–128
Smith WS, English JD, Johnston SC (2011) Chapter 370. Cerebrovascular diseases. In: Longo D, Fauci A, Kasper D, Hauser S, Jameson J, Loscalzo J (eds) Harrison’s principles of internal medicine, 18th edn. McGraw Hill, New York
Suarez-Monteagudo C, Hernandez-Ramirez P, Alvarez-Gonzalez L, Garcia-Maeso I, de la Cuetara-Bernal K, Castillo-Diaz L, Bringas-Vega ML, Martinez-Aching G, Morales-Chacon LM, Baez-Martin MM, Sanchez-Catasus C, Carballo-Barreda M, Rodriguez-Rojas R, Gomez-Fernandez L, Alberti-Amador E, Macias-Abraham C, Balea ED, Rosales LC, Del Valle Perez L, Ferrer BB, Gonzalez RM, Bergado JA (2009) Autologous bone marrow stem cell neurotransplantation in stroke patients. an open study. Restor Neurol Neurosci 27:151–161
Takahashi K, Yamanaka S (2006) Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 126:663–676
Tsuji M, Taguchi A, Ohshima M, Kasahara Y, Sato Y, Tsuda H, Otani K, Yamahara K, Ihara M, Harada-Shiba M, Ikeda T, Matsuyama T (2014) Effects of intravenous administration of umbilical cord blood CD34 cells in a mouse model of neonatal stroke. Neuroscience 263C:148–158
Ueno Y, Chopp M, Zhang L, Buller B, Liu Z, Lehman NL, Liu XS, Zhang Y, Roberts C, Zhang ZG (2012) Axonal outgrowth and dendritic plasticity in the cortical peri-infarct area after experimental stroke. Stroke 43:2221–2228
Vasandan AB, Shankar SR, Prasad P, Sowmya Jahnavi V, Bhonde RR, Jyothi Prasanna S (2014) Functional differences in mesenchymal stromal cells from human dental pulp and periodontal ligament. J Cell Mol Med 18:344–354
Wang JH, Liu N, Du HW, Weng JS, Chen RH, Xiao YC, Zhang YX (2008) [Effects of adipose-derived stem cell transplantation on the angiogenesis and the expression of bFGF and VEGF in the brain post focal cerebral ischemia in rats]. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi 24:958–961
Wardlaw JM, Murray V, Berge E, Del Zoppo GJ (2009) Thrombolysis for acute ischaemic stroke. Cochrane Database Syst Rev 7:CD000213
Wei X, Zhao L, Zhong J, Gu H, Feng D, Johnstone BH, March KL, Farlow MR, Du Y (2009) Adipose stromal cells-secreted neuroprotective media against neuronal apoptosis. Neurosci Lett 462:76–79
West CC, Murray IR, Gonzalez ZN, Hindle P, Hay DC, Stewart KJ, Peault B (2014) Ethical, legal and practical issues of establishing an adipose stem cell bank for research. J Plast Reconstr Aesthet Surg 67(6):745–751
Wu AY, Morrow DM (2012) Clinical use of dieletrophoresis separation for live adipose derived stem cells. J Transl Med 10:99
Wu W, Niklason L, Steinbacher DM (2013) The effect of age on human adipose-derived stem cells. Plast Reconstr Surg 131:27–37
Yang KL, Lee JT, Pang CY, Lee TY, Chen SP, Liew HK, Chen SY, Chen TY, Lin PY (2012) Human adipose-derived stem cells for the treatment of intracerebral hemorrhage in rats via femoral intravenous injection. Cell Mol Biol Lett 17:376–392
Yang YC, Liu BS, Shen CC, Lin CH, Chiao MT, Cheng HC (2011) Transplantation of adipose tissue-derived stem cells for treatment of focal cerebral ischemia. Curr Neurovasc Res 8:1–13
Yang ZX, Han ZB, Ji YR, Wang YW, Liang L, Chi Y, Yang SG, Li LN, Luo WF, Li JP, Chen DD, Du WJ, Cao XC, Zhuo GS, Wang T, Han ZC (2013) CD106 identifies a subpopulation of mesenchymal stem cells with unique immunomodulatory properties. PLoS One 8:e59354
Ye J, Gimble JM (2011) Regulation of stem cell differentiation in adipose tissue by chronic inflammation. Clin Exp Pharmacol Physiol 38:872–878
Yu JM, Bunnell BA, Kang SK (2011) Neural differentiation of human adipose tissue-derived stem cells. Methods Mol Biol 702:219–231
Zhu X, Du J, Liu G (2012) The comparison of multilineage differentiation of bone marrow and adipose-derived mesenchymal stem cells. Clin Lab 58:897–903
Zivin JA (2000) Cell transplant therapy for stroke: hope or hype. Neurology 55:467
Conflict of Interest
The author declares no conflict of interests. No part of the manuscript has been previously published in any language and all illustrations are original.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Conclusions
Conclusions
Taken into consideration the possibility of autologous transplantation without significant reduction in therapeutic potency with the donor’s age, the absence of serious ethical issues and concerns regarding disease transmission from allogeneic sources, the abundance, the relative ease of acquisition and culturing, the superior immunomodulatory function compared with stem cells from other sources, as well as the promising therapeutic efficacy in the treatment of stroke in the experimental settings, it is conceivable that ADSC will have an important role to play in the clinical setting of stroke treatment. Results from large-scaled, randomized, and well-controlled clinical trials are eagerly awaited to turn the possibility into reality.
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Sun, CK. (2015). Transplantation of Adipose-Derived Stem Cells in Stroke. In: Zhao, LR., Zhang, J. (eds) Cellular Therapy for Stroke and CNS Injuries. Springer Series in Translational Stroke Research. Springer, Cham. https://doi.org/10.1007/978-3-319-11481-1_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-11481-1_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-11480-4
Online ISBN: 978-3-319-11481-1
eBook Packages: MedicineMedicine (R0)