Abstract
Head and neck cancers refer to heterogeneous group of tumors extending from the lips to the lower esophagus. Squamous cell cancer is the most common histologic variant, accounting approximately 90–95 % of head and neck cancers. The incidence of head and neck cancer still continues to increase worldwide with approximately half million cases per year [1]. In the United States, it is estimated about 55.070 new head and neck cancers will occur in 2014 which account for up to 3 % of cancer cases [2]. In 2014, it is estimated that 12.000 deaths will occur from head and neck cancer in the United States. In Europe, it is estimated about 139.000 new cases of head and neck cancer per year [3]. In Europe, the 1-year survival rate was 72 %, whereas 5-year survival rate was only 42 % for head and neck cancers in adults [3].
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Overall Survival
- Epidermal Growth Factor Receptor
- Neck Cancer
- Epidermal Growth Factor Receptor Inhibitor
- Locoregional Control
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
FormalPara OverviewHead and neck cancers comprise a heterogeneous group of malignancies which have an unsatisfactory prognosis despite intensive local treatment. Recurrences of these heterogeneous tumors can be observed both inside and outside the treated area, and metastases can occur at more distal locations. Therefore, treatment of head and neck cancers requires effective systemic treatment in addition to the standard surgical and radiation treatments. The main aim of multimodal treatment approach is to improve locoregional control and improve survival as well as to achieve preservation of the organ. The use of antineoplastic chemotherapy for patients with potentially curable, advanced, and locoregional disease is generally distinguished from the treatment of recurrent or metastatic stages of disease. Neoadjuvant treatment strategies for tumor reduction before surgery have yet to gain acceptance in locoregionally advanced head and neck squamous cell cancers. But the optimal sequencing of chemotherapy, radiotherapy, and surgery has still remained a subject of controversy for several decades. Concomitant chemoradiotherapy has been shown to improve survival and is considered a standard treatment for locoregionally advanced head and neck squamous cell cancers. Induction chemotherapy protocols before radiotherapy have been used in patients with high risk of distant metastases or for extensive laryngeal cancers, prior to definitive treatment. Despite the improvement of therapeutic management of head and neck cancers, mortality rates of this patients remains high. Thus, molecular targeted therapies have been developed to help increase specificity and reduce toxicity. Targeting epidermal growth factor receptor (EGFR) with specific antibodies has shown clinical activity in palliative and curative settings of head and neck cancers. But the benefit of EGFR antibodies was small; thus, other EGFR inhibitors and novel biologicals of molecular pathways of head and neck cancer are currently being evaluated either as single agents or in combination with other treatment modalities in patients with advanced or metastatic head and neck cancers.
1 Introduction
Head and neck cancers refer to heterogeneous group of tumors extending from the lips to the lower esophagus. Squamous cell cancer is the most common histologic variant, accounting approximately 90–95 % of head and neck cancers. The incidence of head and neck cancer still continues to increase worldwide with approximately half million cases per year [1]. In the United States, it is estimated about 55,070 new head and neck cancers will occur in 2014 which account for up to 3 % of cancer cases [2]. In 2014, it is estimated that 12,000 deaths will occur from head and neck cancer in the United States. In Europe, it is estimated about 139,000 new cases of head and neck cancer per year [3]. In Europe, the 1-year survival rate was 72 %, whereas 5-year survival rate was only 42 % for head and neck cancers in adults [3].
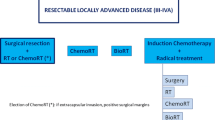
Multidisciplinary approach should be used in all head and neck cancers. The choice of treatment of head and neck cancers depends on the site of the primary tumor, extension of the disease, or the aim of organ preservation. The use of antineoplastic chemotherapy for patients with potentially curable, advanced, and locoregional disease is generally distinguished from the treatment of recurrent or metastatic stages of disease. Approximately 30–40 % of the American Joint Committee on Cancer (AJCC) early-stage I/II head and neck cancers are usually treated with single modality such as radiotherapy or surgery with similar outcomes. Despite single-modality treatment is recommended for early-stage patients, multimodality treatment approaches are recommended for approximately 60 % of AJCC stages III and IV patients [4]. The aim of using chemotherapy with multimodality treatment is to increase cure rates in patients with inoperable or advanced head and neck cancer patients. Neoadjuvant treatment strategies for tumor reduction before surgery have yet to gain acceptance in locoregionally advanced head and neck squamous cell cancers. But the optimal sequencing of chemotherapy, radiotherapy, and surgery has still remained a subject of controversy for several decades [4, 5].
Many chemotherapeutic agents have shown activity as single agents in the metastatic setting squamous cell carcinoma of the head and neck (SCCHN) cancer, but platinum-based chemotherapy consisting of either cisplatin or carboplatin is the recommended first-line treatment for inoperable recurrent or metastatic SCCHN [4, 6]. Targeting epidermal growth factor receptor (EGFR) with specific antibodies have shown clinical activity in palliative and curative settings of head and neck cancers [7–9]. But the benefit of EGFR antibodies was small; thus, other EGFR inhibitors and novel biologicals of molecular pathways of head and neck cancer are currently being evaluated either as single agents or in combination with other treatment modalities in patients with advanced or metastatic head and neck cancers [5].
2 Concurrent Chemotherapy and Radiotherapy
The treatment alternatives continue to improve in patients with locally advanced HNSCC. In early 1990s, 157 previously untreated patients with advanced squamous HNSCC randomly treated with alternating chemotherapy and radiotherapy or radiotherapy alone [10]. In this study, complete response rate was 43 and 22 % (P = 0.03) in combined therapy and radiotherapy arms, respectively. The median survival was 16.5 months in the combined therapy group and 11.7 months in the radiotherapy group (P < 0.05). In the 5-year update of this study, the estimated 5-year overall survival (OS) was 24 and 10 % in combined therapy and radiotherapy arms, respectively (P = 0.01) [11]. Five-year progression-free survival (PFS) was also significantly better in combination treatment arm (21 % vs. 9 %, P = 0.008).
In another phase III trial, 295 unresectable HNSCC patients randomly assigned to single daily fractionated radiotherapy or identical radiotherapy with concurrent three cycles bolus cisplatin, given on days 1, 22, and 43 or a split course of single daily fractionated radiotherapy and three cycles of concurrent infusional fluorouracil and bolus cisplatin chemotherapy, 30 Gy given with the first cycle and 30–40 Gy given with the third cycle [12]. The 3-year OS rate was significantly increased with concurrent cisplatin and radiotherapy arms (37 % vs. %23, P = 0.014) compared to radiotherapy alone arm, whereas no significant survival advantage was observed with split course concurrent arm compared to radiotherapy arm (3-year OS; 27 % vs. 23 %).
A meta-analysis of 63 randomized trials (10,741 patients) between 1965 and 1993 showed absolute 4 % survival benefit at 2 and 5 years with adding chemotherapy in the locoregional treatment of HNSCC [13]. In this meta-analysis, no significant benefit with adjuvant or neoadjuvant treatment was observed. Despite the significant benefit was shown with concomitant chemoradiotherapy , the heterogeneity of the results prohibits clear conclusions. In the updated meta-analysis of 93 randomized trials (17,346 patients) between 1965 and 2000, the hazard ratio of death was 0.88 (P < 0.0001) with an absolute benefit for chemotherapy of 4.5 % at 5 years [14].
In the chemotherapy database (Meta-Analysis of Chemotherapy in Head, Neck Cancer and Nasopharynx Carcinoma ) of 120 randomized trials and about 25,000 patients, concomitant cisplatin-based chemoradiotherapy provided the most significant benefit on locoregional control and survival both in HNSCC and nasopharyngeal carcinomas [15].
Concurrent chemoradiotherapy leads to improve disease control not only in unresectable HNSCC but also in resectable stages III and IV HNSCC compared to radiotherapy alone. In a phase III randomized study, efficacy of radiotherapy versus combination chemotherapy and radiotherapy in resectable stages III and IV HNSCC was compared [16]. In this randomized study, 100 resectable stages III and IV HNSCC patients were randomized to either radiotherapy alone, 68–72 Gy at 1.8–2.0 Gy per day, or to radiotherapy with concurrent chemotherapy, 5-fluorouracil, 1,000 mg/m2/day and cisplatin 20 mg/m2/day, both given as continuous intravenous infusions over 4 days beginning on day 1 and day 22 of the radiotherapy. With a median 3-year follow-up, relapse-free survival (RFS) was significantly higher in the combination treatment arm compared to radiotherapy arm alone (67 % vs. 52 %, P = 0.03). Primary site preservation was achieved in 57 % and 35 % of patients with concurrent chemoradiotherapy and radiotherapy arms, respectively (P = 0.02). Also hematogenous metastases were significantly lower in concurrent chemoradiotherapy compared to radiotherapy arm alone (10 % vs. 21 %, P = 0.04). After a median 5-year follow-up, OS was not significant between treatment arms, but 5-year OS was significantly higher in patients with successful primary site preservation in the chemoradiotherapy arm [17]. In summary, the addition of concurrent chemotherapy to definitive radiotherapy in patients with resectable stages III and IV HNSCC improved recurrence-free interval and primary site preservation.
Concurrent chemoradiotherapy also has a beneficial role in the organ-preservation treatment of the larynx and for advanced nasopharyngeal cancer. In a randomized phase III Intergroup R91-11 trial, 547 locally advanced larynx cancer patients were randomly assigned to induction cisplatin plus fluorouracil followed by radiotherapy, radiotherapy with concurrent administration of cisplatin, or radiotherapy alone [18]. Two-year results showed that larynx preservation was achieved in 88 and 75 % in radiotherapy with concurrent cisplatin and induction chemotherapy followed by radiotherapy arms, respectively (P = 0.005), and 70 % in radiotherapy arm alone (P < 0.0001). In this study, locoregional control was also significantly better with radiotherapy and concurrent cisplatin (78 % vs. 61 % in induction cisplatin plus fluorouracil followed by radiotherapy and 56 % in radiotherapy alone). In the long-term results with a median 10.8-year follow-up, both chemotherapy arms significantly improved laryngectomy-free survival compared to radiotherapy alone [19]. In summary, in Intergroup R91-11 trial locoregional control and larynx preservation were significantly improved with concomitant chemoradiotherapy compared with the induction arm or radiotherapy alone in advanced larynx cancer.
A randomized phase III trial was designed to compare concurrent chemoradiotherapy with radiotherapy alone in 350 patients with locoregionally advanced nasopharyngeal carcinoma [20]. Two-year PFS was 76 % in the concurrent chemoradiotherapy arm and 69 % in the radiotherapy alone arm (P = 0.10). The primary end point was not met in this trial, but PFS was significantly prolonged in patients with advanced tumor and node stages. After median 5.5-year follow-up, OS was statistically significant in concurrent chemoradiotherapy arm compared to radiotherapy arm alone (70.3 % vs. 58.6 %, P = 0.49) [21]. Another phase III randomized study concurrent chemoradiotherapy versus radiotherapy alone for 284 patients with advanced nasopharyngeal carcinoma showed that 5-year OS and PFS were significantly improved with concurrent arm compared to radiotherapy arm alone [22]. A meta-analysis of 1,528 patients with locally advanced nasopharyngeal cancer from 6 randomized trials showed that the addition of chemotherapy to radiotherapy increased both PFS and OS by 34 and 20 % at 4 years after treatment [23]. Another meta-analysis of 1,753 patients with locally advanced nasopharyngeal cancer from eight randomized trials showed 6 % absolute survival benefit at 5 years with the addition of chemotherapy to standard radiotherapy with a median 6-year follow-up [24].
3 Induction Chemotherapy
Concurrent chemoradiotherapy is considered as the standard treatment for locally advanced head and neck cancer of the hypopharynx, oropharynx, and larynx. Multiple phase III trials and meta-analyses showed a significant OS and locoregional control benefit of concurrent chemotherapy with radiotherapy. Although chemoradiotherapy has become the standard treatment approach for patients with locally advanced unresectable HNSCC, induction chemotherapy trials with cisplatin plus fluorouracil or taxane with cisplatin plus fluorouracil regimen followed with radiotherapy or chemoradiotherapy aimed to increase survival, organ preservation, and disease control rate.
A randomized study in patients with a squamous cell carcinoma of the oropharynx for whom curative radiotherapy or surgery was considered feasible and was assigned to neoadjuvant chemotherapy followed by locoregional treatment to the same locoregional treatment without chemotherapy [25]. In chemotherapy arm, three cycles of chemotherapy consisting of cisplatin plus fluorouracil (CF) were delivered every 3 weeks. The median survival was 5.1 years in neoadjuvant treatment group, whereas the median survival was 3.3 years in locoregional treatment arm (P = 0.03). A meta-analysis of 63 randomized trials showed that the addition of CF regimen to locoregional treatment significantly improved the 5-year survival (6.5 % absolute survival benefit), whereas no significant benefit of locoregional control was shown with the addition of induction chemotherapy regimens [13].
The results of five randomized controlled trials comparing induction docetaxel plus CF have been published. In phase III, TAX 323 trial , 358 patients with locoregionally advanced or unresectable disease of HNSCC were randomly assigned to docetaxel plus CF (TCF) or CF regimen for four cycles every 3 weeks [26]. Radiotherapy was performed within 4–7 weeks after completing chemotherapy if progression was not developed. The primary end point was PFS. With a median 32.5-month follow-up, the median PFS was 11.0 and 8.2 months in the TCF and CF induction arms, respectively (P = 0.007). The response rate of induction with TCF was also significantly higher in TCF arm compared to CF arm (68 % vs. 54 %, P = 0.006). Median OS was 18.8 and 14.5 months with TCF and CF induction arms, respectively (P = 0.02). A randomized phase III TAX 324 trial, randomly assigned 501 patients with locoregionally advanced or unresectable disease of HNSCC either TCF or CF induction chemotherapy, followed by chemoradiotherapy with weekly carboplatin therapy and radiotherapy for 5 days per week [27]. In TAX 324 trial primary end point was OS. The estimated 3-year survival was 62 and 48 % in TCF and CF induction arms, respectively (P = 0.006). The median OS was 71 months in TCF arm and 30 months in CF arm (P = 0.006). In the long-term results of TAX 324 trial, 5-year OS was 52.0 and 42 % in TCF and CF arms, respectively, with a median 72.2-month follow-up [28]. Median OS was 70.6 months in TCF arm and 34.8 months in CF arm (P = 0.014). Median PFS was also significantly improved with TCF regimen compared to CF regimen (38.1 and 13.2 months, P = 0.011).
GORTEC trial was conducted as a phase III trial for organ preservation of hypopharynx and larynx [29]. In this trial, patients who had larynx and hypopharynx cancer that required total laryngectomy were randomly assigned to receive three cycles of TCF or CF. Patients who responded to chemotherapy received radiotherapy with or without additional chemotherapy. Patients who did not respond to chemotherapy underwent total laryngectomy followed by radiotherapy with or without additional chemotherapy. The primary end point was 3-year larynx-preservation rate. In TCF arm, 3-year larynx-preservation rate was significantly improved compared to CF arm (70.3 % vs. 57.5 %, P = 0.03).
An individual patient data meta-analysis of 1,772 patients in five randomized trial demonstrated that TCF regimen was significantly associated with improved survival (absolute 7.4 % benefit at 5 years) compared to CF regimen as induction chemotherapy in locally advanced head and neck cancer [30]. Also, TCF arm was associated with significant improved PFS, locoregional control with reduced distant failure.
In another phase III PARADIGM trial , efficacy of TCF induction chemotherapy followed by concurrent chemoradiotherapy with cisplatin-based concurrent chemoradiotherapy alone in patients with locally advanced head and neck cancer was compared [31]. The primary end point was OS. In TCF arm, 3-year OS was 73 %, whereas 78 % in chemoradiotherapy arm alone (P = 0.77). A phase III randomized DeCIDE trial was randomly assigned two cycles of TCF induction chemotherapy followed with chemoradiotherapy or chemoradiotherapy alone in patients with N2/N3 locally advanced HNSCC [32]. The primary end point was OS. In DeCIDE trial, 3-year OS was 75.0 and 73.0 % in induction arm and chemoradiotherapy arms, respectively (P = 0.7).
Induction chemotherapy with definitive radiotherapy regimens also can be used as an aim for organ preservation of the larynx and hypopharynx. A phase III VALCSG (the Department of Veterans Affairs Laryngeal Cancer Study Group ) study randomly assigned 332 patients with previously untreated advanced (stages III or IV) laryngeal squamous carcinoma to receive either three cycles of CF regimen and radiation therapy or surgery and radiation therapy [33]. The estimated 2-year survival was 68 % in both arms with a median of 33-month follow-up (P = 0.98). Total laryngectomy was avoided in 64 % of patients, and on multivariate analyses, T4 and N2 disease were both significant predictors of local treatment failure. Recurrence pattern was also significantly differed between two treatment arms; local failure significantly higher (P = 0.0005) and distant metastases significantly lower (P = 0.016) in the chemotherapy arm compared to the surgery arm. A phase III EORTC (the European Organization for Research and Treatment Cancer) trial aimed to compare a larynx-preservation rate with induction chemotherapy plus definitive radiation therapy in patients previously untreated and operable squamous cell carcinomas of the hypopharynx [34]. In the induction chemotherapy arm, complete response of local disease was reported in 54 % of patients and in 51 % of patients with regional disease. The median survival was 44 and 25 months in induction arm and surgery arms, respectively (P = 0.006), which was less than superiority margin; thus, two treatment arms were accepted as equal. Larynx preservation was achieved in 42 and 35 % of patients in the 3rd and the 5th year with the induction treatment.
In summary, the individual patient data meta-analysis demonstrated that TCF regimen as induction chemotherapy significantly improved OS, PFS, and and locoregional and distant failure compared to CF for locally advanced HNSCC. But the trials presented in this meta-analysis were heterogeneous studies in terms of study design, used doses of chemotherapy drugs, and use of chemoradiotherapy. The TCF induction followed with concomitant chemoradiotherapy with up-front concomitant chemoradiotherapy trials, DeCIDE and PARADIGM, did not demonstrate a significant difference between treatment arms. The main limitations in PARADIGM trial were the use of different chemoradiotherapy regimens and nonstandard split course bifractionated docetaxel plus hydroxyurea-based chemoradiotherapy regimen between two treatment arms. Patients with only N2/N3 disease inclusion was the main limitation of DeCIDE trial. In conclusion, concomitant chemoradiotherapy is still the standard treatment in locoregionally advanced HNSCC. There is no evidence from randomized trials suggesting that TCF followed by chemoradiotherapy is superior to chemoradiotherapy alone. Thus, there is no consensus of optimal sequencing of induction chemotherapy and/or chemoradiotherapy [4]. But, induction chemotherapy with definitive radiotherapy regimens can be used as an aim for organ preservation of the larynx and hypopharynx as in EORTC and VALCSG trials [3]. Phase III trials of induction chemotherapy protocols in locally advanced stages III and IV head cancer are summarized in Table 2.1.
4 Adjuvant Chemotherapy /Radiotherapy
Many factors can influence survival and locoregional control after primary treatment of head and neck cancers. In two randomized trials, the role of adjuvant chemoradiation was clarified. In randomized EORTC 22931 trial, 334 patients with resected locally advanced head and neck cancer were randomly assigned to radiotherapy alone or with concomitant cisplatin (100 mg/m2, on days 1, 22, and 43 of radiotherapy) [35]. High-risk disease was defined as T3 or T4 primary with any nodal stage (except T3N0 laryngeal cancer), positive surgical margins, positive extracapsular extension, positive perineural invasion, or vascular invasion. In EORTC trial, 5-year PFS, OS, and locoregional control were significantly improved in postoperative concurrent chemoradiotherapy arm compared to postoperative radiotherapy alone arm (47 % vs. 36 %; P = 0.04, 53 % 40 %; P = 0.02 and 82 % vs. 69; P = 0.007, respectively) with a median 60-month follow-up.
In RTOG (the Radiation Therapy Oncology Group) 9501 trial , 459 patients with resected high-risk HNSCC randomly assigned to radiotherapy alone or the same doses of RT with concomitant cisplatin (100 mg/m2, on days 1, 22, and 43 of radiotherapy) as EORTC trial [36]. In RTOG 9501 trial, high-risk factors were defined as positive surgical margins, positive two or more lymph nodes, or extracapsular nodal extension. In concurrent chemoradiotherapy arm, 2-year locoregional control and DFS were significantly improved compared to radiotherapy arm alone but OS did not differ significantly between treatment groups with a median of 45.9-month follow-up. In the updated results of RTOG 9501 trial at 10 years, locoregional control and DFS were significantly improved only in patients with extracapsular nodal spread or positive margins [37].
In the combined analysis of EORTC 22931 and RTOG 9501 trials for defining risk levels in operated locally advanced HNSCC, extracapsular nodal extension and/or positive surgical margins were found the only risk factors associated with the benefit of concomitant adjuvant chemotherapy and radiotherapy [38]. Thus, the presence of extracapsular nodal extension and/or positive surgical margins is considered a definitive indication of adjuvant treatment according to the current guidelines [3, 4].
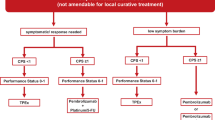
5 Systemic Chemotherapy for Metastatic Head and Neck Cancer
The median OS was generally less than 1 year for incurable recurrent or metastatic HNSCC despite intensive chemotherapy and targeted agents [6]. Cisplatin, carboplatin, docetaxel, paclitaxel, methotrexate, fluorouracil, capecitabine, and pemetrexed are commonly used single agents for palliative treatment of incurable recurrent or metastatic HNSCC patients [4]. Despite platinum doublets studies in phase III trials significantly improved response rate, no significant effect on OS was observed [39, 40]. Also no specific platin-based regimen superior to another platin-based regimen despite adding different schedules of taxanes [6, 41]. In symptomatic patients, to increase response rate, platinum-based, multi-agent combination regimens can be given, and single-agent chemotherapy regimens can be given to asymptomatic patients with low tumor burden.
6 EGFR Inhibitors for HNSCC
Overexpression of EGFR was observed approximately in 90 % of HNSCC patients and is associated with poor prognosis [5, 42]. EGFR gene amplification was also associated with poor survival and locoregional recurrence in head and neck cancer. Cetuximab is a chimeric IgG1 monoclonal antibody that specifically binds to EGFR. Cetuximab inhibits DNA double-strand break repair that demonstrates synergistic activity with chemotherapy and radiotherapy [43].
In a randomized phase III trial, 424 patients with locoregionally advanced head and neck cancer were randomly assigned to treatment with high-dose radiotherapy alone or high-dose radiotherapy plus weekly cetuximab [8]. Cetuximab was initiated as loading dose 400 mg/m2 1 week before radiotherapy followed by a weekly dose of 250 mg/m2 during radiotherapy. The primary end point of this study was the duration of control of locoregional disease. Locoregional control was significantly improved in patients treated with cetuximab plus radiotherapy compared to radiotherapy alone arm (24.4 months vs. 14.9 months, P = 0.005). The median OS also significantly improved in cetuximab plus radiotherapy compared to radiotherapy alone arm with a median 54-month follow-up (49.0 months vs. 29.3 months, P = 0.03). In the subgroup analysis, the beneficial effect was prominent especially oropharyngeal cancers. In the long-term evaluation of this trial, 5-year OS was 45.6 and 36.4 % in cetuximab plus radiotherapy and radiotherapy alone arms, respectively (P = 0.018) [9]. Additionally, OS benefit was limited to only patients who developed an acneiform rash of at least grade 2 severity.
In phase III EXTREME trial , 442 patients with incurable or metastatic HNSCC randomly assigned to receive platinum-based therapy alone or in combination with cetuximab as a first-line palliative regimen [7]. In cetuximab plus chemotherapy arm, cetuximab monotherapy was given until disease progression or unacceptable toxicity if at least stable disease was achieved after a maximum of six cycles of chemotherapy. The primary end point was OS. EXTREME trial demonstrated a significant OS benefit with the addition of cetuximab to platinum-based therapy; median OS improved from 7.4 to 10.1 months (P = 0.04).
The OS benefit of cetuximab was shown either as curative treatment or palliative treatment. Cetuximab is the only targeted therapy to be routinely used in clinical practice in the treatment of recurrent or metastatic HNSCC. Other EGFR agents and various biologic agents are under study. Several phase III trials of both cetuximab and novel targeting agents are still ongoing.
7 Conclusion
Multidisciplinary approach should be used in all head and neck cancers. The choice of treatment of head and neck cancers depends on the site of the primary tumor, the extension of the disease, or the aim of organ preservation. The use of antineoplastic chemotherapy for patients with potentially curable, advanced, and locoregional disease is generally distinguished from the treatment of recurrent or metastatic stages of disease. The aim of using chemotherapy with multimodality treatment is to increase cure rates in patients with inoperable or advanced head and neck cancer patients. Molecular targeted therapies have been developed to help increase specificity and reduce toxicity. Anti-EGFR antibodies have shown clinical activity in palliative and curative settings of head and neck cancers, and other EGFR inhibitors and novel biologicals of molecular pathways of head and neck cancer are currently being evaluated either as single agents or in combination with other treatment modalities in patients with advanced or metastatic head and neck cancers.
Abbreviations
- CF:
-
Cisplatin-fluorouracil
- EORTC:
-
European Organization for Research and Treatment Cancer
- GETTEC:
-
French Groupe d’Etude des Tumeurs de la Tête et du Cou trial
- GORTEC:
-
French Head and Neck Oncology Radiotherapy Group
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- TCF:
-
Docetaxel-cisplatin-fluorouracil
- VALCSG:
-
The Department of Veterans Affairs Laryngeal Cancer Study Group
References
Parkin DM, Bray F, Ferlay J, Pisani P (2005) Global cancer statistics, 2002. CA Cancer J Clin 55(2):74–108
Siegel R, Ma J, Zou Z, Jemal A (2014) Cancer statistics, 2014. CA Cancer J Clin 64(1):9–29. doi:10.3322/caac.21208
Gregoire V, Lefebvre JL, Licitra L, Felip E, Group E-E-EGW (2010) Squamous cell carcinoma of the head and neck: EHNS-ESMO-ESTRO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 21(Suppl 5):v184–v186. doi:10.1093/annonc/mdq185
Pfister DG, Ang KK, Brizel DM, Burtness BA, Busse PM, Caudell JJ, Cmelak AJ, Colevas AD, Dunphy F, Eisele DW, Gilbert J, Gillison ML, Haddad RI, Haughey BH, Hicks WL Jr, Hitchcock YJ, Kies MS, Lydiatt WM, Maghami E, Martins R, McCaffrey T, Mittal BB, Pinto HA, Ridge JA, Samant S, Schuller DE, Shah JP, Spencer S, Weber RS, Wolf GT, Worden F, Yom SS, McMillian NR, Hughes M, National Comprehensive Cancer N (2013) Head and neck cancers, version 2.2013. Featured updates to the NCCN guidelines. J Natl Compr Canc Netw 11(8):917–923
Schmitz S, Ang KK, Vermorken J, Haddad R, Suarez C, Wolf GT, Hamoir M, Machiels JP (2014) Targeted therapies for squamous cell carcinoma of the head and neck: current knowledge and future directions. Cancer Treat Rev 40(3):390–404. doi:10.1016/j.ctrv.2013.09.007
Price KA, Cohen EE (2012) Current treatment options for metastatic head and neck cancer. Curr Treat Options Oncol 13(1):35–46. doi:10.1007/s11864-011-0176-y
Vermorken JB, Mesia R, Rivera F, Remenar E, Kawecki A, Rottey S, Erfan J, Zabolotnyy D, Kienzer HR, Cupissol D, Peyrade F, Benasso M, Vynnychenko I, De Raucourt D, Bokemeyer C, Schueler A, Amellal N, Hitt R (2008) Platinum-based chemotherapy plus cetuximab in head and neck cancer. N Engl J Med 359(11):1116–1127. doi:10.1056/NEJMoa0802656
Bonner JA, Harari PM, Giralt J, Azarnia N, Shin DM, Cohen RB, Jones CU, Sur R, Raben D, Jassem J, Ove R, Kies MS, Baselga J, Youssoufian H, Amellal N, Rowinsky EK, Ang KK (2006) Radiotherapy plus cetuximab for squamous-cell carcinoma of the head and neck. N Engl J Med 354(6):567–578. doi:10.1056/NEJMoa053422
Bonner JA, Harari PM, Giralt J, Cohen RB, Jones CU, Sur RK, Raben D, Baselga J, Spencer SA, Zhu J, Youssoufian H, Rowinsky EK, Ang KK (2010) Radiotherapy plus cetuximab for locoregionally advanced head and neck cancer: 5-year survival data from a phase 3 randomised trial, and relation between cetuximab-induced rash and survival. Lancet Oncol 11(1):21–28. doi:10.1016/S1470-2045(09)70311-0
Merlano M, Vitale V, Rosso R, Benasso M, Corvo R, Cavallari M, Sanguineti G, Bacigalupo A, Badellino F, Margarino G et al (1992) Treatment of advanced squamous-cell carcinoma of the head and neck with alternating chemotherapy and radiotherapy. N Engl J Med 327(16):1115–1121. doi:10.1056/NEJM199210153271602
Merlano M, Benasso M, Corvo R, Rosso R, Vitale V, Blengio F, Numico G, Margarino G, Bonelli L, Santi L (1996) Five-year update of a randomized trial of alternating radiotherapy and chemotherapy compared with radiotherapy alone in treatment of unresectable squamous cell carcinoma of the head and neck. J Natl Cancer Inst 88(9):583–589
Adelstein DJ, Li Y, Adams GL, Wagner H Jr, Kish JA, Ensley JF, Schuller DE, Forastiere AA (2003) An intergroup phase III comparison of standard radiation therapy and two schedules of concurrent chemoradiotherapy in patients with unresectable squamous cell head and neck cancer. J Clin Oncol 21(1):92–98
Pignon JP, Bourhis J, Domenge C, Designe L (2000) Chemotherapy added to locoregional treatment for head and neck squamous-cell carcinoma: three meta-analyses of updated individual data. MACH-NC Collaborative Group. Meta-Analysis of Chemotherapy on Head and Neck Cancer. Lancet 355(9208):949–955
Pignon JP, le Maitre A, Maillard E, Bourhis J, Group M-NC (2009) Meta-analysis of chemotherapy in head and neck cancer (MACH-NC): an update on 93 randomised trials and 17,346 patients. Radiother Oncol 92(1):4–14. doi:10.1016/j.radonc.2009.04.014
Bourhis J, Le Maitre A, Baujat B, Audry H, Pignon JP, Meta-Analysis of Chemotherapy in Head NCCG, Meta-Analysis of Radiotherapy in Carcinoma of Head NCG, Meta-Analysis of Chemotherapy in Nasopharynx Carcinoma Collaborative G (2007) Individual patients’ data meta-analyses in head and neck cancer. Curr Opin Oncol 19(3):188–194. doi:10.1097/CCO.0b013e3280f01010
Adelstein DJ, Saxton JP, Lavertu P, Tuason L, Wood BG, Wanamaker JR, Eliachar I, Strome M, Van Kirk MA (1997) A phase III randomized trial comparing concurrent chemotherapy and radiotherapy with radiotherapy alone in resectable stage III and IV squamous cell head and neck cancer: preliminary results. Head Neck 19(7):567–575
Adelstein DJ, Lavertu P, Saxton JP, Secic M, Wood BG, Wanamaker JR, Eliachar I, Strome M, Larto MA (2000) Mature results of a phase III randomized trial comparing concurrent chemoradiotherapy with radiation therapy alone in patients with stage III and IV squamous cell carcinoma of the head and neck. Cancer 88(4):876–883
Forastiere AA, Goepfert H, Maor M, Pajak TF, Weber R, Morrison W, Glisson B, Trotti A, Ridge JA, Chao C, Peters G, Lee DJ, Leaf A, Ensley J, Cooper J (2003) Concurrent chemotherapy and radiotherapy for organ preservation in advanced laryngeal cancer. N Engl J Med 349(22):2091–2098. doi:10.1056/NEJMoa031317
Forastiere AA, Zhang Q, Weber RS, Maor MH, Goepfert H, Pajak TF, Morrison W, Glisson B, Trotti A, Ridge JA, Thorstad W, Wagner H, Ensley JF, Cooper JS (2013) Long-term results of RTOG 91-11: a comparison of three nonsurgical treatment strategies to preserve the larynx in patients with locally advanced larynx cancer. J Clin Oncol 31(7):845–852. doi:10.1200/JCO.2012.43.6097
Chan AT, Teo PM, Ngan RK, Leung TW, Lau WH, Zee B, Leung SF, Cheung FY, Yeo W, Yiu HH, Yu KH, Chiu KW, Chan DT, Mok T, Yuen KT, Mo F, Lai M, Kwan WH, Choi P, Johnson PJ (2002) Concurrent chemotherapy-radiotherapy compared with radiotherapy alone in locoregionally advanced nasopharyngeal carcinoma: progression-free survival analysis of a phase III randomized trial. J Clin Oncol 20(8):2038–2044
Chan AT, Leung SF, Ngan RK, Teo PM, Lau WH, Kwan WH, Hui EP, Yiu HY, Yeo W, Cheung FY, Yu KH, Chiu KW, Chan DT, Mok TS, Yau S, Yuen KT, Mo FK, Lai MM, Ma BB, Kam MK, Leung TW, Johnson PJ, Choi PH, Zee BC (2005) Overall survival after concurrent cisplatin-radiotherapy compared with radiotherapy alone in locoregionally advanced nasopharyngeal carcinoma. J Natl Cancer Inst 97(7):536–539. doi:10.1093/jnci/dji084
Lin JC, Jan JS, Hsu CY, Liang WM, Jiang RS, Wang WY (2003) Phase III study of concurrent chemoradiotherapy versus radiotherapy alone for advanced nasopharyngeal carcinoma: positive effect on overall and progression-free survival. J Clin Oncol 21(4):631–637
Huncharek M, Kupelnick B (2002) Combined chemoradiation versus radiation therapy alone in locally advanced nasopharyngeal carcinoma: results of a meta-analysis of 1,528 patients from six randomized trials. Am J Clin Oncol 25(3):219–223
Baujat B, Audry H, Bourhis J, Chan AT, Onat H, Chua DT, Kwong DL, Al-Sarraf M, Chi KH, Hareyama M, Leung SF, Thephamongkhol K, Pignon JP, Group M-NC (2006) Chemotherapy in locally advanced nasopharyngeal carcinoma: an individual patient data meta-analysis of eight randomized trials and 1753 patients. Int J Radiat Oncol Biol Phys 64(1):47–56. doi:10.1016/j.ijrobp.2005.06.037
Domenge C, Hill C, Lefebvre JL, De Raucourt D, Rhein B, Wibault P, Marandas P, Coche-Dequeant B, Stromboni-Luboinski M, Sancho-Garnier H, Luboinski B, French Groupe d’Etude des Tumeurs de la Tete et du C (2000) Randomized trial of neoadjuvant chemotherapy in oropharyngeal carcinoma. French Groupe d’Etude des Tumeurs de la Tete et du Cou (GETTEC). Br J Cancer 83(12):1594–1598. doi:10.1054/bjoc.2000.1512
Vermorken JB, Remenar E, van Herpen C, Gorlia T, Mesia R, Degardin M, Stewart JS, Jelic S, Betka J, Preiss JH, van den Weyngaert D, Awada A, Cupissol D, Kienzer HR, Rey A, Desaunois I, Bernier J, Lefebvre JL, Group ETS (2007) Cisplatin, fluorouracil, and docetaxel in unresectable head and neck cancer. N Engl J Med 357(17):1695–1704. doi:10.1056/NEJMoa071028
Posner MR, Hershock DM, Blajman CR, Mickiewicz E, Winquist E, Gorbounova V, Tjulandin S, Shin DM, Cullen K, Ervin TJ, Murphy BA, Raez LE, Cohen RB, Spaulding M, Tishler RB, Roth B, Viroglio Rdel C, Venkatesan V, Romanov I, Agarwala S, Harter KW, Dugan M, Cmelak A, Markoe AM, Read PW, Steinbrenner L, Colevas AD, Norris CM Jr, Haddad RI, Group TAXS (2007) Cisplatin and fluorouracil alone or with docetaxel in head and neck cancer. N Engl J Med 357(17):1705–1715. doi:10.1056/NEJMoa070956
Lorch JH, Goloubeva O, Haddad RI, Cullen K, Sarlis N, Tishler R, Tan M, Fasciano J, Sammartino DE, Posner MR, Group TAXS (2011) Induction chemotherapy with cisplatin and fluorouracil alone or in combination with docetaxel in locally advanced squamous-cell cancer of the head and neck: long-term results of the TAX 324 randomised phase 3 trial. Lancet Oncol 12(2):153–159. doi:10.1016/S1470-2045(10)70279-5
Pointreau Y, Garaud P, Chapet S, Sire C, Tuchais C, Tortochaux J, Faivre S, Guerrif S, Alfonsi M, Calais G (2009) Randomized trial of induction chemotherapy with cisplatin and 5-fluorouracil with or without docetaxel for larynx preservation. J Natl Cancer Inst 101(7):498–506. doi:10.1093/jnci/djp007
Blanchard P, Bourhis J, Lacas B, Posner MR, Vermorken JB, Hernandez JJ, Bourredjem A, Calais G, Paccagnella A, Hitt R, Pignon JP, Meta-Analysis of Chemotherapy in H, Neck Cancer IPCG (2013) Taxane-cisplatin-fluorouracil as induction chemotherapy in locally advanced head and neck cancers: an individual patient data meta-analysis of the meta-analysis of chemotherapy in head and neck cancer group. J Clin Oncol 31(23):2854–2860. doi:10.1200/JCO.2012.47.7802
Haddad R, O’Neill A, Rabinowits G, Tishler R, Khuri F, Adkins D, Clark J, Sarlis N, Lorch J, Beitler JJ, Limaye S, Riley S, Posner M (2013) Induction chemotherapy followed by concurrent chemoradiotherapy (sequential chemoradiotherapy) versus concurrent chemoradiotherapy alone in locally advanced head and neck cancer (PARADIGM): a randomised phase 3 trial. Lancet Oncol 14(3):257–264. doi:10.1016/S1470-2045(13)70011-1
Cohen EE, Karrison T, Kocherginsky M, Huang CH, Agulnik M, Mittal BB, Yunus F, Samant S, Brockstein B, Raez LE, Mehra R, Kumar P, Ondrey FG, Seiwert TY, Villaflor VM, Haraf DJ, EE V (2012) DeCIDE: a phase III randomized trial of docetaxel (D), cisplatin (P), 5-fluorouracil (F) (TPF) induction chemotherapy (IC) in patients with N2/N3 locally advanced squamous cell carcinoma of the head and neck (SCCHN). J Clin Oncol, 2012 ASCO annual meeting abstracts, vol 30, No 15_suppl (May 20 Suppl), 5500
Induction chemotherapy plus radiation compared with surgery plus radiation in patients with advanced laryngeal cancer. The Department of Veterans Affairs Laryngeal Cancer Study Group (1991). N Engl J Med 324(24):1685–1690. doi:10.1056/NEJM199106133242402
Lefebvre JL, Chevalier D, Luboinski B, Kirkpatrick A, Collette L, Sahmoud T (1996) Larynx preservation in pyriform sinus cancer: preliminary results of a European Organization for Research and Treatment of Cancer phase III trial. EORTC Head and Neck Cancer Cooperative Group. J Natl Cancer Inst 88(13):890–899
Bernier J, Domenge C, Ozsahin M, Matuszewska K, Lefebvre JL, Greiner RH, Giralt J, Maingon P, Rolland F, Bolla M, Cognetti F, Bourhis J, Kirkpatrick A, van Glabbeke M, European Organization for R, Treatment of Cancer T (2004) Postoperative irradiation with or without concomitant chemotherapy for locally advanced head and neck cancer. N Engl J Med 350(19):1945–1952. doi:10.1056/NEJMoa032641
Cooper JS, Pajak TF, Forastiere AA, Jacobs J, Campbell BH, Saxman SB, Kish JA, Kim HE, Cmelak AJ, Rotman M, Machtay M, Ensley JF, Chao KS, Schultz CJ, Lee N, Fu KK, Radiation Therapy Oncology Group I (2004) Postoperative concurrent radiotherapy and chemotherapy for high-risk squamous-cell carcinoma of the head and neck. N Engl J Med 350(19):1937–1944. doi:10.1056/NEJMoa032646
Cooper JS, Zhang Q, Pajak TF, Forastiere AA, Jacobs J, Saxman SB, Kish JA, Kim HE, Cmelak AJ, Rotman M, Lustig R, Ensley JF, Thorstad W, Schultz CJ, Yom SS, Ang KK (2012) Long-term follow-up of the RTOG 9501/intergroup phase III trial: postoperative concurrent radiation therapy and chemotherapy in high-risk squamous cell carcinoma of the head and neck. Int J Radiat Oncol Biol Phys 84(5):1198–1205. doi:10.1016/j.ijrobp.2012.05.008
Bernier J, Cooper JS, Pajak TF, van Glabbeke M, Bourhis J, Forastiere A, Ozsahin EM, Jacobs JR, Jassem J, Ang KK, Lefebvre JL (2005) Defining risk levels in locally advanced head and neck cancers: a comparative analysis of concurrent postoperative radiation plus chemotherapy trials of the EORTC (#22931) and RTOG (# 9501). Head Neck 27(10):843–850. doi:10.1002/hed.20279
Jacobs C, Lyman G, Velez-Garcia E, Sridhar KS, Knight W, Hochster H, Goodnough LT, Mortimer JE, Einhorn LH, Schacter L et al (1992) A phase III randomized study comparing cisplatin and fluorouracil as single agents and in combination for advanced squamous cell carcinoma of the head and neck. J Clin Oncol 10(2):257–263
Forastiere AA, Metch B, Schuller DE, Ensley JF, Hutchins LF, Triozzi P, Kish JA, McClure S, VonFeldt E, Williamson SK et al (1992) Randomized comparison of cisplatin plus fluorouracil and carboplatin plus fluorouracil versus methotrexate in advanced squamous-cell carcinoma of the head and neck: a Southwest Oncology Group study. J Clin Oncol 10(8):1245–1251
Gibson MK, Li Y, Murphy B, Hussain MH, DeConti RC, Ensley J, Forastiere AA, Eastern Cooperative Oncology G (2005) Randomized phase III evaluation of cisplatin plus fluorouracil versus cisplatin plus paclitaxel in advanced head and neck cancer (E1395): an intergroup trial of the Eastern Cooperative Oncology Group. J Clin Oncol 23(15):3562–3567. doi:10.1200/JCO.2005.01.057
Kalyankrishna S, Grandis JR (2006) Epidermal growth factor receptor biology in head and neck cancer. J Clin Oncol 24(17):2666–2672. doi:10.1200/JCO.2005.04.8306
Milas L, Mason K, Hunter N, Petersen S, Yamakawa M, Ang K, Mendelsohn J, Fan Z (2000) In vivo enhancement of tumor radioresponse by C225 antiepidermal growth factor receptor antibody. Clin Cancer Res 6(2):701–708
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Sendur, M.A.N., Aksoy, S. (2015). Current Systemic Therapy Options for Head and Neck Cancers. In: Beyzadeoglu, M., Ozyigit, G., Selek, U. (eds) Radiation Therapy for Head and Neck Cancers. Springer, Cham. https://doi.org/10.1007/978-3-319-10413-3_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-10413-3_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-10412-6
Online ISBN: 978-3-319-10413-3
eBook Packages: MedicineMedicine (R0)