Abstract
A fundamental question in health policy is how the newly forming Accountable Care Organizations (ACO) will achieve high quality and efficient care for patients and populations. ACO’s have been operating for about 2 years and information is beginning to be released about their performance. However, there is several years of information from an important precursor to Medicare ACO’s – the Physician Group Practice Demonstration (PGPD)2. The University of Michigan (UM) was one of 10 large physician organizations that participated in the PGPD from 2005–2010, and achieved shared savings and high quality for all 5 years. UM is an integrated academic healthcare system with experience in managed care clinical and governance integration and a unified EMR. For the PGPD, UM implemented numerous transitional care and care coordination activities. UM system characteristics and interventions were probably all important in “bending the curve”. In addition, attribution of sicker patients by attribution to the multispecialty group instead of just primary care physicians, the presence of skilled specialists and generalists who are comfortable caring for sick patients, and employed faculty physicians who are comfortable with an academic mission, may also have contributed. Future information about the performance of the many different types of healthcare systems participating in the ACO programs may very well point to many different healthcare system configurations, including Academic Healthcare Systems, which can achieve high quality and efficient patient care.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Care Coordination
- Patient Center Medical Home
- Transitional Care
- Accountable Care Organization
- Quality Management Program
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
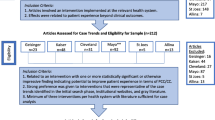
A fundamental question in health policy is how the newly forming Accountable Care Organizations (ACO) will achieve high quality and efficient care for patients and populations. In Medicare there are nearly 300 Accountable Care Organizations in two major programs: the Pioneer Demonstration, which involves more financial risk for the ACO, and the Medicare Shared Savings Program, which has less risk [1]. These ACO’s have been operating for about 2 years and information is beginning to be released about their performance. However, there are already several years of information from an important precursor to Medicare ACO’s – the Physician Group Practice Demonstration (PGPD) [2]. The University of Michigan (UM) was one of ten large physician organizations that participated in the PGPD from 2005 to 2010. Two groups, including the UM, were very successful and achieved shared savings and quality targets for all 5 years of the Demonstration. Seven of the groups eventually earned shared savings (two groups for 1 year only, two groups for 2 years, one group for 3 years and two groups for all 5 years) reaching about $100 million in savings for Medicare over the 5 years, and $80 million in aggregate shared savings distributed among successful groups [2]. The University of Michigan saved Medicare about $22 million and received $17.6 million in shared savings over the 5 years of the PGPD. All groups had high quality, as measured by ambulatory quality measures similar to current PQRS (Physician Quality Reporting System) [3, 4] measures of physician clinical performance in major chronic diseases (diabetes, heart failure, CAD) and in preventative care.
Reviews and analysis of the PGPD have appeared in the literature over the past few years, and analyses are available on the CMS website [2]. Although many policy makers and researchers do not consider the PGPD a success [5, 6], it was one of the prototypes and inspirations for the current ACO demonstrations and programs. Those who consider it a qualified success [7–9] generally cite structural and organizational characteristics of the PGPD groups, their electronic medical record (EMR), risk adjustment, and care coordination infrastructure. Although these characteristics are important, it is not possible for policy makers to understand this complex socio-medical quasi-experiment at the level of the individual healthcare system by reviewing claims and interviewing participants. This chapter explores the University of Michigan’s characteristics and care processes that contributed to its financial success within the particular structural and financial model of the PGPD.
Brief Overview of the PGPD
The structure of the PGPD included retrospective patient assignment to each participating physician group based on the plurality of outpatient E&M costs. Retrospective assignment means that patients were assigned to the University of Michigan at the end of each performance year depending upon the pleurality of theirs costs, and therefore, during the performance year, UMHS did not know if a particular patient would eventually be assigned. The assignment was based on the Tax ID number of the physicians (TIN), and the University of Michigan Healthcare System (UMHS), as a large, integrated healthcare system, has one TIN for its providers. The PGPD participants were responsible for all Medicare costs incurred by their assigned patients (except for Medicare D) no matter where the care was received. Because the PGPD, like current ACO’s, was part of fee for service Medicare, patients could receive care from the PGPD participating group practice, or anywhere else. Medicare D was excluded because those costs were covered by Medicare through the Medicare D program and not through the PGPD [4].
As with current ACO’s, the financial goal was to “bend the curve” or decrease Medicare growth compared to the Medicare growth of the local market area. The financial model measured risk adjusted growth compared to the local area risk adjusted growth, referenced to an unchanging baseline year. Shared savings were 80 % of savings beyond a 2 % corridor. This risk corridor is analogous to a confidence interval in statistics and meant that PGPD participants had to save at least 2 % before savings were available to share. (For example, if a PGPD participant saved 2.1 %, they only shared in 0.1 % of the savings.) Risk adjustment was done based on customized, claims based algorithm that accounted for burden of disease called hierarchical claims categories (HCC’s) [10].
In order to receive shared savings, assuming the participating physician group had decreased Medicare growth and was eligible, the physician group practice had to achieve quality targets on 32 ambulatory quality measures which were measures for chronic disease and prevention similar to current Medicare Physician Quality Reporting System [11] measures. Seven of these were measured by claims and 25 were done by chart review of a sample of beneficiaries, similar to HEDIS methodology. Just about all these structural characteristics were changed for both the Pioneer ACO Demonstration Program and the Medicare Shared Savings Program (MSSP).
Characteristics Associated with UMHS’s Success in the PGPD
A true understanding of which healthcare system characteristics led to UM’s success in the PGPD would require analyzing data from the local market area comparison group (south eastern and south central Michigan), and some of the published literature does make use of these data [12, 13]. However, some insight is given by the fact that the UMHS has several characteristics widely considered important for success in efficient care of Medicare patients. These characteristics include: integrated structure with coordinated governance and employed physicians; system-wide electronic medical record (EMR); managed care/risk experience including capacity for administrative data analysis; and care coordination infrastructure across the care continuum.
Integrated Structure and Electronic Medical Record (EMR)
The University of Michigan Medical School and Hospital and Health System is part of the University of Michigan (UM) [14]. UM is a constitutional entity of the State of Michigan and final authority resides with the Board of Regents elected by the voters of the State of Michigan. The Medical School and Hospital and Health Clinics are integrated into the University of Michigan Health System (UMHS). UMHS is led by an Executive Vice President of Medical Affairs, to whom the CEO of the Hospital and Health Clinics and the Dean of the Medical School report, and who in turn reports to the President of the University of Michigan. Table 12.1 shows UMHS characteristics. All physicians are salaried faculty of the Medical School, and salaries are generally determined by a complex performance review related to academic (research, teaching) and clinical (mainly productivity and compliance with clinical quality measures) metrics. The mix of academic and clinical activities varies widely among faculty physicians. The Faculty Group Practice is the structure that organizes and manages the clinical activities of the UM Medical School faculty, and is a large multispecialty group practice. UMHS also includes a home health care agency and a DME/infusion/orthotics group.
During the PGPD, UMHS had a uniform, patient-centered, web-based EMR in the hospital, ambulatory clinical areas, home health and DME. This EMR supported provider notes, as well as other clinical and administrative (scheduling, billing) data. For most of the PGPD, chronic disease registries were programmed into the EMR and used to support ambulatory quality measurement and performance improvement (see below). During the last years of the PGPD, the EMR supported computerized order entry and ePrescribing. About 2 years after the PGPD ended, UMHS migrated to the Epic EMR system.
Experience with Managed Care and Provider Risk
UMHS has substantial experience with managed care and provider risk. From 1985 to 2006 UMHS owned and operated MCARE, a full service, wholly owned Managed Care Organization eventually covering over 200,000 lives in Southeast and South Central Michigan. MCARE operated traditional HMO, PPO, and Point of Service products for regional employers, as well as a Qualified Health Plan for Medicaid in Michigan. From 1997 to 2002 MCARE included a Medicare risk plan (Medicare Plus Choice). UMHS providers took full risk for their assigned populations, including commercial (HMO, PPO, POS), Medicaid, and Medicare for most of MCARE’s existence. MCARE was financially sound at the time it was sold to Blue Cross Blue Shield of Michigan (BCBSM) in 2006. Many of the UMHS physician and administrative leaders, and skilled claims and administrative data analysts who were involved in MCARE went on to lead population-based clinical transformation efforts, including the PGPD, and continue to be involved to this day with several similar clinical redesign efforts in which the UMHS is involved.
UMHS’s experience with population management during the 1990s–2000s also included innovative provider-based health-care plans UMHS operated for salaried employees, dependents and retirees of the Ford Motor Company (Partnership Health) and GM (Active Health). These were population-based, company funded products in which the care delivery model and benefit structure were jointly designed by the UMHS and employers to improve care coordination and align incentives. These plans featured many elements now included in many ACO and Patient – Centered Medical Home (PCMH) care delivery models as well as other innovative features (member selection of a coordinating physician, personalized care plans that could be used to change plan benefits, care coordination through nurse navigators, and disease management programs) [15]. Although these plans were terminated during the downturn in the auto industry, evaluation at the time demonstrated savings and improved clinical quality, particularly for patients with chronic diseases.
The University of Michigan is self-insured and bears full risk for about 80,000 employees, dependents, and retirees who receive the vast majority of their care through UMHS. UMHS also accepts risk for approximately10,000 Medicaid managed care patients. In addition to this insurance risk, UMHS has multiple performance-based payment arrangements for both hospital and professional payments. The state of Michigan has a dominant insurer, Blue Cross and Blue Shield of Michigan (BCBSM) that also has a managed care component, Blue Care Network. Through BCBSM, which insured many of its commercial patients, UMHS participated in performance-based payment programs for the hospital, and for physician performance in the management of chronic disease for several years before and during the PGPD. The BCBSM performance-based payment program helps to support UMHS’s chronic disease registry development and some chronic disease quality improvement activities. Eventually, BCBSM incentivized development of a Patient Centered Medical Home (PCMH) model for commercial patients. As the primary care clinics became certified as PCMH’s for commercial patients, Medicare and Medicaid patients were also included. The PCMH was developing during the last year of the PGPD. Because of this experience UMHS also participates in a Center for Medicaid and Medicare Innovation Demonstration that involved PCMH development for Medicare and Medicaid patients, the all-payer Advanced Primary Care Demonstration, which began in late 2011.
Clinical Redesign and Models of Care
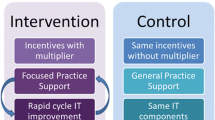
The integrated structure of the UMHS, its system-wide EMR, and its experience with managed care and both insurance and performance risk were major factors when UMHS decided to participate in the PGPD in 2005. The healthcare system leadership believed then (and still does) that a new business model is coming and UMHS, as an Academic Medical Center, needs to learn how to operate in this emerging business environment. The strategy adopted to improve efficiency and quality of care for Medicare beneficiaries at UMHS involved clinical redesign and models of care and had three key elements: (1) avoid unnecessary re-hospitalizations: (2) coordinate care of high risk, high cost Medicare beneficiaries, including the frail elderly and or dual eligible (enrolled in both Medicaid and Medicare) patients; and (3) coordinate with care delivery models and innovations that were already in place at UMHS, many “left over” from managed care experiences.
This strategy led to the development or enhancement of clinical programs related to transitional care, including a large sub-acute care service in community nursing homes [16], care management of dual eligible patients and frail elders, and a renewed focus on and coordination among existing clinical programs that had grown up during the 1990s when managed care was growing. In addition, in order to meet the quality requirements of the PGPD, a clinical quality improvement program based on physician feed-back and chronic disease registries was able to make use of the infrastructure that was being developed for commercial patients and to enhance this infrastructure for Medicare beneficiaries. Table 12.2 lists these programs and their key characteristics; these programs are described in more detail in the following sections. When the PGPD ended, UMHS participated in the Transition Demonstration from 1/1/2011 to 12/31/2011 (which tests several design features of the Pioneer ACO and MSSP); the Pioneer ACO Demonstration from 1/1/2012 to 12/31/2012, and changed to the CMS MSSP program on 1/1/2013 when it partnered with several large physician groups in Southern Michigan. In addition, since 2012 UMHS has participated in the Michigan Primary Care Transformation (MiPCT) project, a 3-year, multi-payer, project implemented in eight states aimed at reforming primary care payment models and expanding the capabilities of patient-centered medical homes (PCMH).
Clinical Models to Avoid Unnecessary Re-Hospitalizations
Transitional Care Programs
The University of Michigan Faculty Group Practice implemented a transitional care and complex care management program shortly after beginning participation in the PGPD in 2005 [17]. These related programs use the same team, which initially consisted of 4.5 nurses, 2 social workers, and 2 patient care advocates, supported by a physician medical director (the complex care management program is described below). The centerpiece of both is a post-acute care call-back program to address the poor coordination between the acute and ambulatory care settings, and to identify complex patients being discharged from the hospital or Emergency Department (ED). Additional transitional care programs were developed over the 5 years of the PGPD and eventually included: acute-care discharge process redesign; transitional care clinics in geriatrics and cardiology; a sub-acute service in local high volume skilled nursing (e.g. sub-acute care) facilities; and finally implementation of transitional care coordination in all U-M primary care clinics as the PCMH program was rolled out and the PGPD was ending.
The post-acute callback program focused on Medicare patients discharged from the hospital or the ED. Since mid-2005 this program has called about up to 15,000 patients per year discharged from the UM hospital or ED within 24 h of discharge during the week; Friday and weekend discharges are called on Monday. The post-acute call-back program consists of a team of nurses, nurse assistants and social workers, as described above, supported by a physician medical director with direct access to a consultant pharmacist and a home care service provider. The team focuses on complex Medicaid, Medicare, dual-eligible and uninsured patients. These nurse and social work care managers work closely with inpatient discharge planning, and ambulatory care clinics, home care providers, mental health providers, and social service organizations to support patients and their families during the gap between an acute-care hospitalization and clinic appt. Many patient questions and areas of confusion have been discovered. Roughly one third of patients called need 2 h of registered nurse time to address clinical problems. Problems include medication confusion (medication reconciliation is the major activity done by the call-back nurses); home care services that did not come; no follow-up appointment, cannot get to a clinic appointment, or do not understand why they should go; patients unsafe at home.
The post-acute call-back program has been analyzed for its effects. During a 2-year period that was specifically evaluated, May 2008 to May 2010, the program handled 31,339 of 49,744 inpatient and ED Medicare discharges. Internal administrative evaluations have suggested decreased readmissions and ED visits after the program was implemented compared to before it was implemented, and similar decreased readmissions and ED visits for patients who were called compared with those who were not called.
Improving hospital discharge: Beginning in 2008, UMHS began to participate in BOOST (Better Outcomes for Older Adults Through Safe Transitions Project sponsored by the Society of Hospital Medicine) [18] and M*STAAR (Michigan – State Action on Avoidable Rehospitalizations). Both programs stress identification of patients in the hospital who are at risk for readmission after discharge, notification of patients’ primary care providers of the patients’ admission and discharge and important tests that need to be followed up, and provision of high quality discharge instructions and teaching to patients and their caregivers prior to discharge. Although not directly targeted to the PGPD, this program facilitates communication between the hospital discharging physicians and nurses, and the call-back program and sub-acute program.
Sub-acute Nursing Home (NH) Service: Discharge process redesign and frail elder programs (see below) coordinate with the UMHS sub-acute service. In this service, begun during the second year of the PGPD, three geriatric faculty members practice full-time in five local high volume skilled nursing (sub-acute care) facilities supported by four geriatric nurse practitioners and the University of Michigan’s electronic medical record in the nursing homes. This service handles about 45 % of the approximately 1,200 Medicare patients who are discharged to sub-acute facilities each year from UM Hospital. This innovative program has substantially reduced acute care length of stay for nursing home patients and had (and continues to have because like the other programs, it is ongoing) a small but measureable effect on NH readmissions to acute care hospitals [16].
Care Coordination for High-Risk, High-Cost, Complex Patients
Complex Care Coordination: Care coordination for complex Medicaid, Dual Eligible and homeless/uninsured complex patients is performed through the Complex Care Management Program (CCMP). The CCMP consists of 6.5 centrally located Complex Care Managers (nurses and social workers and two patient care advocates, see above), supported by a medical director, who provide chronic care management services to complex, high utilizing patients in vulnerable populations. Complex Care Managers work closely with multiple agencies within and outside UMHS, including visiting nurses, medical social workers, and community health and mental health providers. The care managers undergo standardized training and use both panel management software and the EMR. Most patients are recruited into the CCMP after they are discharged from the hospital, are evaluated by the post-acute call back service (i.e., the same nurse/social work team), and are considered to be complex based on standard criteria. Physicians, social workers, and home care providers can also refer patients. We have found that identifying patients for complex care management through a hospitalization is a very efficient way to assure that care coordination resources are directed to the high risk, high cost patients who need these resources. Over time a higher proportion of complex care managers are social workers with mental health proficiency, reflecting the importance of mental and behavioral health conditions and social services in meeting the needs of complex care patients. The characteristics, operation, and outcomes of the CCMP during and after the PGPDP have been described elsewhere [17].
Palliative Care: Patients with advanced disease beyond curable interventions, or with highly complex health status, often have preferences about their care. UMHS has a multidisciplinary palliative care and hospice program begun in 2006 that reaches across the care continuum and into the community to work with patients and families to formulate and implement such highly personal care goals. This program is anchored by an accredited palliative and hospice care fellowship (among the first programs accredited in the US) with highly experienced faculty in several Medical School departments. The program includes acute care and nursing home consult services, UMHS faculty group practice members who visit local hospices to provide services to UMHS patients, and ambulatory palliative care clinics in geriatrics and oncology.
Other Relevant Infrastructure
Geriatrics Services: For many years, UMHS has had a respected and relatively large Geriatrics clinical service. The Geriatrics clinic provides primary care and care coordination for about 5,500 frail and complex elderly who need social and personal care support. The clinic features faculty geriatricians and a multidisciplinary team with social work, nursing and pharmacy, and provides educational opportunities for interdisciplinary trainees. The Geriatrics Clinic participates in the Patient Centered Medical Home Program (see below) and is co-located with Geriatric Psychiatry, and with cognitive and movement disorder neurology clinics. Complex care management is provided by four social workers. The Geriatrics clinic has strong links to the transitional care programs, to the CCMP, and to community programs. Additional programs developed by the clinical social workers include information and referral services, caregiver and patient counseling, and links to a large day-care program for patients with cognitive impairment.
Patient-Centered Medical Home
UMHS implemented primary care redesign consistent with the Patient Centered Medical Home (PCMH) model beginning in 2008 [19]. Not all aspects of the PCMH were implemented at once in all the clinics. Full implementation took over a year and in many ways, the PCMH continues to develop. The goal of the UMHS PCMH is to empower patients to take a very active role in their own care, to learn about their conditions, to create action plans and to set goals with their provider to achieve better health.
The University of Michigan is following the joint principles of the Patient Centered Medical Home issued in 2007 by the American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians and American Osteopathic Association [19], the National Committee for Quality Assurance (NCQA), as well as the domains of function established by BCBSM.
The UMHS PCMH program includes 23 primary care clinics (all of the primary care clinics), the Geriatrics clinic, and about 196 providers. All these clinics have been designated as PCMH’s under the guidelines set by BCBSM since 2009 that are consistent with, and somewhat more rigorous, than those of NCQA [20].
The domains of function established by BCBSM and met by the UMHS PCMH program include:
-
An explicit working relationship with the patient and caregiver.
-
Registries for chronic diseases including: diabetes, CHF, CAD, asthma, CKD and COPD. These registries offer valuable clinical information to the primary care physician and specialist to provide the patient with the best care that meets their needs.
-
Leadership reports that provide feedback to leadership, health center staff and clinicians about how their patients are doing based on national benchmarks.
-
Same day visit availability (30 % of schedule) and extended hours including weekends to meet the needs of the patients.
-
Staff training and implementation of self-management support for patients with chronic diseases, helping patients to set self-management goals and to establish action plans to help them improve their overall health.
-
Community outreach with access to a social worker as well as community resources to support the patient.
-
ePrescribing.
-
Coordination of care across all domains of the health care system, facilitated by the established registries, information technology and health information exchange, and with a particular focus on transitions of care from inpatient to outpatient.
The PCMH was implemented in the last year of the PGPD. Only about 50 % of attributed patients in the PGPD were in the UMHS primary care clinics. Another 25 % had primary care providers elsewhere (and may have also have seen a UMHS primary care provider), while about 25 % had no primary care at all. We do not know how primary care utilization was distributed among our market control group, but we expect that in our local area, patients do not use primary care physicians as much as in other areas of the country.
Specialty Clinic Services
Aspects of the PCMH were and still are available in major ambulatory specialty clinics at UMHS – geriatrics (as mentioned above), cardiology, endocrinology, and pulmonary. Patients in these clinics are included on chronic disease registries. Physicians receive point of care reminders for relevant chronic disease management and preventative interventions, provider feedback on clinical quality performance, and team support for care coordination and transitional care activities. Within the UMHS integrated system, the specialists are part of the ACO and many take their role of chronic disease management seriously. Some care coordination and disease management systems have historically existed within the UMHS specialty clinics often started by researchers or set up to improve disease management during the time of managed care contracts.
Key among such programs are the heart failure disease management program and the coagulation clinic. The heart failure disease management program has a medical director, nurse supported patient and caregiver care coordination and self-management support, a post-acute transitional care clinic, and a performance improvement program. The large, centralized, system wide anticoagulation monitoring program manages warfarin treatment for any patient with a UMHS physician and is housed within cardiology.
In these clinics, if a patient has a dominant chronic disease or a dominant current disease (cancer, major surgical problem, etc.), the specialist may be acting as the patient’s “principle physician” either on a continuous basis (as with some cardiologists and pulmonologists) or on a time-limited basis (oncologist). This management model may have the potential, when appropriate care is known and/or incentives are aligned, to be more efficient than having a primary care physician attempt to manipulate within a “medical neighborhood” [21], and attempt to “gatekeep” or co-manage outside his/her area of expertise and potentially outside the preferences of the patient. For example, the UMHS cancer center has multiple programs for patient and caregiver support, although not as developed as the recently described cancer medical home. A recent paper described the success of UMHS in decreasing hospitalizations of cancer patients during the PGPD [13].
Quality Measurement and Performance Improvement Program
The Quality Management Program
The Quality Management Program (QMP), begun in the late 1990s in response to managed care activities of UMHS, has major responsibility for quality measurement and improvement for chronic diseases in the ambulatory setting. The QMP develops and maintains chronic disease registries, provides point-of-care reminders to clinicians, identifies gaps in care, utilizes interactive voice response technology to engage patients in self-management of depression and heart failure, maintains >25 evidence based clinical practice guidelines and >600 specialty referral guidelines, and assesses and reports on institutional, departmental and provider quality of care. In addition it receives and analyses claims data from several payers including CMS/Medicare, the state of Michigan/Medicaid, and BCBSM for multiple commercial insurance programs. The QMP has dedicated senior analysts who are adept at analyses using EMR data, healthcare system administrative data, and claims data from payers. These analyses support feedback to clinicians and clinical leaders. In addition, QMP data analysts provide analyses and reports to healthcare system leaders who are responsible for implementing care redesign interventions such as the PGPD and the PCMH, and are important resources supporting communication with payers regarding data quality, attribution issues, and financial monitoring.
Challenges Faced by UMHS in the PGPD and in Future ACO Efforts
Despite the many characteristics of the UMHS that led to success in the PGPD and could lead to success in the future, UMHS also had and still has substantial challenges as it tries to manage population health and redesign clinical care. These challenges are in part related to the fact that UMHS is an academic healthcare system. As such it has: (1) adverse patient selection that cannot fully be corrected by risk adjustment; (2) important missions of education and research in addition to clinical care; (3) high costs both because it is an academic healthcare system and it is located in a relatively high cost area. However, the design of the PGPD may have helped to counter some of these challenges.
Adverse Selection. As an Academic Healthcare System, UMHS experiences adverse selection. Patients who are referred for highly specialized care, and those with complex or severe chronic disease, often ended up in its attributed population because attribution was by plurality of outpatient costs and patients were attributed to the entire faculty group practice, not just faculty in primary care. This attribution methodology identified some patients with very high costs and pushed up the average yearly per capital cost of attributed beneficiaries. Many of UMHS’s attributed Medicare beneficiaries had high costs in oncology, cardiology, or even ophthalmology, and there were more dual eligible patients than in the surrounding market area. However, among these high-risk high cost patients, there may be waste and poorly coordinated care, and therefore more opportunities to improve care efficiency.
Multiple missions: research and education. As an academic healthcare center, UMHS has many faculty members who participate in research and education as well as clinical care. Complex patients with serious illnesses are drawn to skilled, academic physicians, and many specialists may be engaged in research to define appropriate care. Therefore, high-risk high cost patients may be seeing physicians in an academic medical center who are able and willing to manage these patients efficiently. Some academic physicians may also respond to incentives related to their work in education and research rather than incentives based solely on productivity.
Medical education costs and relatively high cost market area. In an academic healthcare system direct and indirect medical education payments from Medicare contribute to costs. Other costs of academic medical centers for staffing, research support and technology can also potentially contribute to high costs of care. In addition, according to the Dartmouth Atlas, UMHS is located in a relatively high cost market area. However, the PGPD and other ACO financial models do not target lower costs, but rather, decreased growth of costs.
Conclusion
Based on UMHS characteristics as an Academic Healthcare Center, and the intersection of these characteristics with the PGPD attribution and financial methodology, it seems plausible that the success of UMHS in the PGPD was based on efficient and high quality care of high cost high-risk patients. UMHS internal analyses, CMS analyses, and published studies of the PGPD are consistent in pointing toward the hypothesis that some of the success of UMHS and the other successful participants in the PGPD may have been due to efficient care of sicker patients. Clinical and governance integration, a unified EMR, and numerous transitional care and care coordination activities are probably all very important in “bending the curve”. In addition, attribution of sicker patients by attribution to the multispecialty group instead of just primary care physicians, the presence of skilled specialists and generalists who are comfortable caring for sick patients, and employed faculty physicians who are comfortable with an academic mission, may also have contributed. Future information about the performance of the many different types of healthcare systems participating in the ACO programs may very well point to many different healthcare system configurations, including Academic Healthcare Systems, which can achieve high quality and efficient patient care.
Abbreviations
- BCBSM:
-
Blue Cross Blue Shield of Michigan
- CCMP:
-
Complex Care Management Program
- CMMI:
-
Centers for Medicaid and Medicare Innovation
- EMR:
-
Electronic Medical Record
- HCC:
-
Heirarchical Claims Categories
- M*STARR:
-
Michigan-State Action on Avoidable Rehospitalizations
- MSSP:
-
Medicare Shared Savings Program
- NCQA:
-
National Committee for Quality Assurance
- PCMH:
-
Patient Centered Medical Home
- PGPD:
-
Physician Group Practice Demonstration
- QMP:
-
Quality Management Program
- UMHS:
-
University of Michigan Healthcare System
References
Accountable Care Organizations (ACO). Centers for Medicare & Medicaid Services Website. http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ACO/. Accessed 13 May 2014.
Kautter J, Pope GC, Leung M, Trisolini M, Adamache W, Smith K, Trebino D, Kaganova J, Patterson L, Berzin O, Schwartz M. Evaluation of the Medicare Physician Group Practice Demonstration final report. Research Triangle Park: RTI International; 2012.
Trisolini M, Kautter J, Pope GC, Bapat B, Olmsted E, Urato M. Physician Group Practice Demonstration quality measurement and reporting specifications. 2005. http://www.cms.gov/Medicare/Demonstration-Projects/DemoProjectsEvalRpts/downloads/Quality_Specs_Report.pdf. Accessed 13 May 2014.
Kautter J, Pope GC, Trisolini M, Grund S. Medicare Physician Group Practice Demonstration design: quality and efficiency pay-for-performance. Health Care Financ Rev. 2007;29(1):15–29.
Wilensky GR. Lessons from the Physician Group Practice Demonstration – a sobering reflection. N Engl J Med. 2011;365(18):1659–61.
Iglehart JK. Assessing an ACO prototype–Medicare’s Physician Group Practice Demonstration. N Engl J Med. 2011;364(3):198–200.
Fisher ES, McClellan MB, Bertko J, et al. Fostering accountable health care: moving forward in Medicare. Health Aff. 2009;28(2):W219–31.
Sebelius K. Report to Congress: Physician Group Practice Demonstration evaluation report. 2009. http://www.cms.gov/Medicare/Demonstration-Projects/DemoProjectsEvalRpts/downloads/PGP_RTC_Sept.pdf. Accessed 13 May 2014.
Berwick DM. Making good on ACOs’ promise – the final rule for the Medicare Shared Savings Program. N Engl J Med. 2011;365(19):1753–6.
Pope GC, Kautter J, Ellis RP, et al. Risk adjustment of Medicare capitation payments using the CMS-HCC model. Health Care Financ Rev. 2004;25(4):119–41.
Physician Quality Reporting System (Physician Quality Reporting or PQRS) formerly known as the Physician Quality Reporting Initiative (PQRI). Centers for Medicare & Medicaid Services Website. http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/pqrs/index.html. Accessed 13 May 2014.
Colla CH, Wennberg DE, Meara E, et al. Spending differences associated with the Medicare Physician Group Practice Demonstration. JAMA J Am Med Assoc. 2012;308(10):1015–23.
Colla CH, Lewis VA, Gottlieb DJ, Fisher ES. Cancer spending and accountable care organizations: evidence from the Physician Group Practice Demonstration. Healthcare. 2013;1(3–4): 100–7.
University of Michigan Health System. http://www.med.umich.edu/. Accessed 13 May 2014.
Stiles RA, Mick SS, Wise CG. The logic of transaction cost economics in health care organization theory. Health Care Manag Rev. 2001;26(2):85–92.
Joshi DK, Bluhm RA, Malani PN, Fetyko S, Denton T, Blaum CS. The successful development of a subacute care service associated with a large academic health system. J Am Med Dir Assoc. 2012;13(6):564–7.
Williams BC, Paik JL, Haley LL, Grammatico GM. Centralized care management support for “high utilizers” in primary care practices at an academic medical center. Care Manag J. 2014; 15(1):26–33.
Project BOOST: better outcomes by optimizing safe transitions. Society of Hospital Medicine Website. 2014. http://www.hospitalmedicine.org/AM/Template.cfm?Section=Home&TEMPLATE=/CM/HTMLDisplay.cfm&CONTENTID=27659. Accessed 13 May 2014.
Joint Principles of the Patient-Centered Medical Home. Patient-Centered Primary Care Collaborative website. 2007. http://www.aafp.org/dam/AAFP/documents/practice_management/pcmh/initiatives/PCMHJoint.pdf. Accessed 13 May 2014.
Patient-Centered Medical Home Recognition. National Committee for Quality Assurance (NCQA). 2014. http://www.ncqa.org/Programs/Recognition/PatientCenteredMedicalHomePCMH.aspx. Accessed 13 May 2013.
Fisher ES. Building a medical neighborhood for the medical home. N Engl J Med. 2008; 359(12):1202–5.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Blaum, C.S., Williams, B.C., Spahlinger, D.A. (2015). University of Michigan Case Study: The Physician Group Practice Demonstration. In: Powers, J. (eds) Healthcare Changes and the Affordable Care Act. Springer, Cham. https://doi.org/10.1007/978-3-319-09510-3_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-09510-3_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-09509-7
Online ISBN: 978-3-319-09510-3
eBook Packages: MedicineMedicine (R0)