Abstract
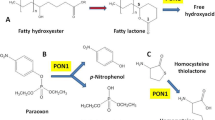
Serum paraoxonase 1 (PON1) has been shown to act as an important guardian against cellular damage from oxidized lipids in low-density lipoprotein (LDL), plasma membrane, against toxic agents such as pesticide residues including organophosphates and against bacterial endotoxin. PON1 associated with circulating high-density lipoprotein (HDL) has the ability to prevent the generation of pro inflammatory oxidized phospholipids by reactive oxygen species. The activities of the HDL-associated PON1 and several other anti-inflammatory factors in HDL are in turn negatively regulated by these oxidized lipids. In rabbits, mice, and humans there appears to be an increase in the formation of these oxidized lipids during the acute phase response. This results in the association of acute phase proteins with HDL and inhibition of the HDL-associated PON1 that renders HDL pro inflammatory.
In populations, low serum HDL-cholesterol is a risk factor for atherosclerosis and efforts are directed toward therapies to improve the quality and the relative concentrations of LDL and HDL. Apolipoprotein A-I (apoA-I) has been shown to reduce atherosclerotic lesions in laboratory animals. ApoA-I, however, is a large protein that is costly and needs to be administered parenterally. Our group has developed apoA-I mimetic peptides that are much smaller than apoA-I (18 amino acids long vs 243 in ApoA-I itself). These HDL mimetic peptides are much more effective in removing the oxidized phospholipids and other oxidized lipids. They improve LDL and HDL composition and function and reduce lesion formation in animal models of atherogenesis. Following is a brief description of some of the HDL mimetic peptides that can improve HDL and the effect of the peptide on PON1 activity.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
8.1 In Search of Agents to Improve HDL Function
Experiments in animal models of atherosclerosis [1, 2] and preliminary human studies [3] have made apolipoprotein A-I (apoA-I), the main protein in high-density lipoprotein (HDL), an attractive therapeutic target. The preliminary human studies [3] suggested that therapeutic benefit might be achieved by administering weekly intravenous doses over a period of 5–6 weeks. Subsequent larger clinical trials [4], however, suggested that longer periods of intravenous administration will be required for significant improvements to be achieved. This made the idea an unlikely therapy for the large number of patients with atherosclerosis.
8.2 The Search for an Ideal Agent: HDL Mimetic Peptide
Anantharamaia and colleagues originally designed an 18 amino acid peptide that mimicked the class A amphipathic helixes contained in apoA-I while it did not have any sequence homology with apoA-I but [5–7]. Because it contained 18 amino acids and formed a class A amphipathic helix the peptide was called 18A. The lipid-binding properties and stability of the 18A peptide were improved by blocking the carboxy terminus using an amide group and blocking the amino terminus through the addition of an acetyl group. Because of the presence of the two phenylalanine residues on the hydrophobic face this peptide was named 2F. The 2F peptide failed to alter lesions in a mouse model of atherosclerosis [8] while mimicking many of the lipid-binding properties of apoA-I. We tested a series of peptides for their ability to inhibit low-density lipoprotein (LDL)-induced monocyte chemotactic activity, which is primarily due to the production of monocyte chemoattractant-1 (MCP-1). This was achieved using a human artery wall cell culture assay. Subsequently, the peptide 4F was shown to be superior [8]. The peptide 4F has the same structure as 2F except for two additional phenylalanine residues on the hydrophobic face of the peptide (replacing two leucine residues).
8.3 Animal Models of Atherosclerosis and the Effects of HDL Mimetic Peptides
ApoAI mimetic peptides reduced the development of atherosclerotic lesions in young mice [9, 10]. Lesion regression in old apolipoprotein E null mice was produced when 4F was given together with a statin [11]. Synergy between D-4F (made from all D amino acids) and pravastatin was then tested in these studies. The oral doses for each that were ineffective when given as single agent was first determined. Significant increase in HDL cholesterol levels, apoA-I levels, and paraoxonase-1 (PON1) activity was achieved with oral administration of the combination. Rendering HDL anti-inflammatory, significantly preventing lesion formation in young apolipoprotein E null mice, and causing regression of established lesions in old apolipoprotein E null mice were among additional effects observed. Mice that received the combination for 6 months had lesion areas that were much smaller when compared to those before the start of treatment [11]. In mice maintained on chow alone en face lesion area was three times higher than that after 6 months of treatment with the combination. In addition in the remaining lesions there was a significant 22 % reduction in macrophage content, indicating an overall 79 %. Reduction in macrophages. The combination of statin and D-4F increased intestinal apoA-I synthesis by a significant 60 %. In studies in Cynomolgous monkeys also, oral administration of D-4F plus pravastatin rendered HDL anti-inflammatory [11]. These results suggested that the combination of an HDL-based therapy and a statin might be a useful anti-atherosclerosis treatment strategy. The fact that the benefit of apolipoprotein mimetic peptides in atherosclerosis was not limited to 4F was unraveled subsequently. We found that peptides including D-[113–122] apoJ, an apolipoprotein J mimetic peptide [12], and peptides too small to form a helical structure [13] were efficacious as well (Fig. 8.1). The efficacy of these peptides was demonstrated in a rabbit model of atherosclerosis as well [14].
D-[113–122]apoJ in apoE-null mouse plasma in vitro. D-[113–122]apoJ or scrambled D-[113–122]apoJ (Scr.[113–122]apoJ peptide) were added to apoE-null mouse plasma at a concentration of 250 ng/mL. The solutions were gently mixed, layered with argon gas, and the tubes were sealed and incubated for 1 h at 37 °C with gentle mixing. The samples were then fractionated by FPLC and lipid hydroperoxide content of LDL (a), lipid hydroperoxide content of HDL (b), and PON1 activity (c) were determined. The values shown are the Mean ± SD. The data shown are representative of two separate experiments
8.4 The Mechanism of Action of HDL Mimetic Peptides
The mechanism of action of the HDL mimetic peptides seems to be based to their ability to remove oxidized lipids from lipoproteins [15–17], promote reverse cholesterol transport from macrophages, and render HDL anti-inflammatory [15, 16]. Atherosclerosis is a long-term inflammatory process that is mediated in part by the oxidation of phospholipids, which induce vascular cells to express cytokines, adhesion molecules, and procoagulant molecules [18, 19]. The mechanism of action of the HDL mimetic peptides appears to be related to their ability to bind and remove these pro inflammatory oxidized lipids [15, 16]. In addition, the HDL mimetic peptides are efficacious in inflammatory processes that have an infectious etiology and in models of vascular diseases that are not classified as atherosclerosis. This suggests that oxidized lipids may be important mediators of a variety of inflammatory conditions other than atherosclerosis as they have been shown to effective in preventing diabetic manifestations, graft rejection, cognitive deficiency in mouse model of hyperlipemia, in collagen induced arthritis model and in animal model of Alzheimer’s Disease.
8.5 HDL Mimetic Peptides, Oxidized Lipids and PON1
On an atherogenic diet, PON1 activity decreased by 52 % in atherosclerosis susceptible mice, C57BL/6 J (BL/6), but not in fatty streak resistant mice, C3H/HeJ (C3H) [20]. In apolipoprotein E knockout mice on the chow diet also plasma PON1 activity was significantly decreased as compared to controls. Furthermore, in LDL receptor knockout mice when they were fed a 0.15 %-cholesterol-enriched diet a significant decrease in PON1 activity was observed. Injection of mildly oxidized LDL but not native LDL resulted in a 59 % decrease in PON1 activity in BL/6 mice but not in C3H mice on a chow diet. A threefold reduction in mRNA levels for PON1 was observed following treatment of HepG2 cells in culture with mildly oxidized LDL (but not native LDL). We additionally reported that, the total cholesterol/HDL cholesterol ratio was 3.1 ± 0.9 as compared to 2.9 ± 0.4 in the controls in normolipidemic patients with angiographically documented coronary artery disease who did not have diabetes and were not on lipid-lowering medication [20]. This difference was however not statistically significant. In a subset of these normolipidemic patients, despite similar normal HDL levels, the PON1 activity was low (48 ± 6.6 versus 98 ± 17 U/ml for controls; p = 0.009). As predicted the HDL from these patients failed to protect against LDL oxidation in co-cultures of human artery wall cells. Forte and colleagues showed [21] that compared with controls on the chow diet, ApoE−/− mice had elevated lysophosphatidylcholine and bioactive oxidized phospholipids (1-palmitoyl- 2-oxovaleryl-sn-glycero-3-phosphocholine and 1-palmitoyl-2-glutaryl-sn-glycero- 3-phosphocholine). In these mice on a chow diet elevated oxidized phospholipids may, in part, contribute to spontaneous lesions. PON1 activity in these mice decreased by 38 %. It has been suggested that removal of oxidized fatty acids from HDL might cause the return of PON1 activity. We have observed that when ApoE-deficient mouse plasma is incubated with PON1 and FPLC fractionation of lipoproteins is performed, PON1 is found in the post HDL region in addition to in HDL-containing fractions. We have shown that early during the incubation, PON is present in HDL-like particles that contain cholesterol, apoA-I, and other HDL constituents and co-elute with albumin. It is possible that 4F accelerates apoA-I cycling, pre-beta formation and remodeling of HDL. We have also observed that when human plasma is incubated with 4F in vitro, PON1 activity is increased. As for the underlying mechanism, one possibility could be the removal of oxidized lipids from HDL and reactivation of PON1 by 4F. Another might be the changes in lipid–protein interaction such as that in phospholipid–apoA-I–PON1 interactions. The peptide 4F therefore might have beneficial effects supporting HDL function in individuals under conditions that result in low PON1 by removing oxidized lipids and reactivating antioxidant enzymes including PON1.
8.6 The Role of Intestine in Systemic Inflammation and Effect on PON1
In recent years our group has focused on the role of small intestine in systemic inflammation, HDL protective capacity and cardiovascular function. This came about when we observed that oral administration of the peptide 4F reduced systemic inflammation while the plasma levels of the peptide were very low [22]. To test the hypothesis that intestine is a major site of action for D-4F, we fed LDLR−/− mice a Western diet (WD) and administered the peptide orally or subcutaneously (SQ). Whereas peptide levels in small intestine only varied by 1.66 ± 0.33-fold, plasma and liver D-4F levels were 298-fold and 96-fold higher, respectively, after SQ administration. Levels of metabolites of arachidonic and linoleic acids known to bind with high affinity to D-4F were significantly reduced liver, hepatic bile and in intestine, to a similar degree whether administered orally or SQ. Levels of 20-HETE however, which is known to bind the peptide with low affinity, were unchanged. D-4F treatment increased HDL-cholesterol levels, PON 1 activity and reduced plasma serum amyloid A (SAA) and triglyceride level similarly after oral or SQ administration. SAA levels correlated significantly with plasma levels of metabolites of arachidonic and linoleic acids. Feeding 15-HETE in chow (without WD) significantly decreased HDL-cholesterol and PON1 activity and increased plasma SAA and triglyceride levels, all of which were significantly ameliorated by SQ D-4F. Administering 4F along with 15-HETE prevented the reduction in PON 1 activity (Fig. 8.2). We therefore concluded that D-4F administration reduced levels of free metabolites of arachidonic and linoleic acids in the small intestine and this was associated with increased PON1 activity and decreased inflammation in LDL receptor deficient mice [22].
Feeding LDLR−/− mice 15-HETE administered in mouse chow (without the WD) decreased plasma HDL-cholesterol levels, increased plasma triglyceride levels, decreased PON activity, and increased plasma SAA levels, all of which was ameliorated by D-4F treatment. Female LDLR−/− mice (10–11 months of age; n = 20 per group) were fed laboratory rodent chow (Ralston Purina) prepared and presented to the mice as described in Materials and Methods. The chow did or did not contain 15-HETE at a concentration of 1 ug per gram diet to provide each mouse on average with 5 ug of 15-HETE per day. The mice received daily SQ injections of saline or SQ saline containing D-4F at a dosage of 900 ug/mouse/day. After 2 weeks on the diet, 2–3 h after the last SQ dose, the mice were bled, and their plasma was analyzed for PON1 activity and other analytes. The data shown are mean ± SD
8.7 Summary
Under conditions of excess inflammatory pressure the ability of HDL to protect itself and other lipid-containing molecules and structures might be reduced, HDL be damaged, antioxidant enzymes such as PON1 be inactivated, and even HDL itself act as a proinflammatory molecule. Fortunately PON1 has the ability to prevent lipid oxidation and may even inactivate oxidized lipids once formed, and thus protect HDL against the inflammatory pressure. Reduction of lipid and protein oxidation by agents such as HDL mimetic peptides may prove to be an effective way of supporting the protective role of HDL.
References
Badimon JA, Badimon L, Fuster V. Regression of atherosclerotic lesions by high density lipoprotein plasma fraction in the cholesterol-fed rabbit. J Clin Invest. 1990;85:1234–41.
Plump AS, Scott CJ, Breslow JL. Human apolipoprotein A-I gene expression increases high density lipoprotein and suppresses atherosclerosis in the apolipoprotein E-deficient mouse. Proc Natl Acad Sci U S A. 1994;91:9607–11.
Nissen SE, Tsunoda T, Tuzcu EM, Schoenhagen P, Cooper CJ, Yasin M, et al. Effect of recombinant apoA-I Milano on coronary atherosclerosis in patients with acute coronary syndromes: a randomized controlled trial. JAMA. 2003;290:2292–300.
Tardif JC, Grégoire J, L’Allier PL, Ibrahim R, Lespérance J, Heinonen TM, Kouz S, Berry C, Basser R, Lavoie MA, Guertin MC, Rodés-Cabau J, Effect of rHDL on Atherosclerosis-Safety and Efficacy (ERASE) Investigators. Effects of reconstituted high-density lipoprotein infusions on coronary atherosclerosis: a randomized controlled trial. JAMA. 2007;297:1675–82.
Anantharamaiah GM, Jones JL, Brouillette CG, Schmidt CF, Chung BH, Hughes TA, et al. Studies of synthetic peptide analogs of amphipathic helix I: structure of peptide/DMPC complexes. J Biol Chem. 1985;260:10248–55.
Venkatachalapathi YV, Phillips MC, Epand RM, Epand RF, Tytler EM, Segrest JP, et al. Effect of end group blockage on the properties of a class A amphipathic helical peptide. Proteins Struct Funct Genet. 1993;15:349–59.
Yancey PG, Bielicki JK, Johnson WJ, Lund-Katz S, Palgunachari MN, Anantharamaiah GM, et al. Efflux of cellular cholesterol and phospholipid to lipid-free apolipoproteins and class A amphipathic peptides. Biochemistry. 1995;34:7955–65.
Datta G, Chaddha M, Hama S, Navab M, Fogelman AM, Garber DW, et al. Effects of increasing hydrophobicity on the physical–chemical and biological properties of a class A amphipathic helical peptide. J Lipid Res. 2001;42:1096–104.
Navab M, Anantharamaiah GM, Hama S, Garber DW, Chaddha M, Hough G, et al. Oral administration of an apoA-I mimetic peptide synthesized from D-amino acids dramatically reduces atherosclerosis in mice independent of plasma cholesterol. Circulation. 2002;105:290–2.
Li X, Chyu KY, Faria Neto JR, Yano J, Nathwani N, Ferreira C, et al. Differential effects of apolipoprotein A-I mimetic peptide on evolving and established atherosclerosis in apolipoprotein E-null mice. Circulation. 2004;110:1701–5.
Navab M, Anantharamaiah GM, Hama S, Hough G, Reddy ST, Frank JS, et al. D-4F and statins synergize to render HDL anti-inflammatory in mice and monkeys and cause lesion regression in old apolipoprotein E-null mice. Arterioscler Thromb Vasc Biol. 2005;25:1426–32.
Navab M, Anantharamaiah GM, Reddy ST, Van Lenten BJ, Wagner AC, Hama S, et al. An oral apoJ peptide renders HDL antiinflammatory in mice and monkeys and dramatically reduces atherosclerosis in apolipoprotein E-null mice. Arterioscler Thromb Vasc Biol. 2005;25:1932–7.
Navab M, Anantharamaiah GM, Reddy ST, Hama S, Hough G, Frank JS, et al. Oral small peptides render HDL antiinflammatory in mice and monkeys and reduce atherosclerosis in apoE null mice. Circ Res. 2005;97:524–32.
Van Lenten BJ, Wagner AC, Navab M, Anantharamaiah GM, Hama S, Reddy ST, et al. Lipoprotein inflammatory properties and serum amyloid A levels but not cholesterol levels predict lesion area in cholesterol-fed rabbits. J Lipid Res. 2007;48:2344–53.
Navab M, Anantharamaiah GM, Reddy ST, Hama S, Hough G, Grijalva VR, et al. Oral D-4F causes formation of pre-β high-density lipoprotein and improves high-density lipoprotein-mediated cholesterol efflux and reverse cholesterol transport from macrophages in apolipoprotein E-null mice. Circulation. 2004;109:3215–20.
Navab M, Anantharamaiah GM, Reddy ST, Hama S, Hough G, Grijalva VR, et al. Apolipoprotein A-I mimetic peptides. Arterioscler Thromb Vasc Biol. 2005;25:1325–31.
Datta G, Epand RF, Epand RM, Chaddha M, Kirksey MA, Garber DW, et al. Aromatic residue position on the non polar face of class A amphipathic helical peptides determines biological activity. J Biol Chem. 2004;18(279):26509–17.
Berliner JA, Watson AD. A role for oxidized phospholipids in atherosclerosis. N Engl J Med. 2005;353:9–12.
Gargalovic PS, Imura M, Zhang B, Gharavi NM, Clark MJ, Pagnon J, et al. Identification of inflammatory gene modules based on variations of human endothelial cell responses to oxidized lipids. Proc Natl Acad Sci U S A. 2006;103:12741–6.
Navab M, Hama-Levy S, Van Lenten BJ, Fonarow GC, Cardinez CJ, Castellani LW, et al. Mildly oxidized LDL induces an increased apolipoprotein J/paraoxonase ratio. J Clin Invest. 1997;99:2005–19.
Forte TM, Subbanagounder G, Berliner JA, Blanche PJ, Clermont AO, Jia Z, et al. Altered activities of anti-atherogenic enzymes LCAT, paraoxonase, and platelet-activating factor acetylhydrolase in atherosclerosis susceptible mice. J Lipid Res. 2002;43:477–85.
Navab M, Reddy ST, Anantharamaiah GM, Hough G, Buga GM, Danciger J. D-4F-mediated reduction in metabolites of arachidonic and linoleic acids in the small intestine is associated with decreased inflammation in low-density lipoprotein receptor-null mice. J Lipid Res. 2012;53:437–45.
Author information
Authors and Affiliations
Corresponding authors
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Vakili, L. et al. (2014). Systemic Inflammation, Intestine, and Paraoxonase-1. In: Camps, J. (eds) Oxidative Stress and Inflammation in Non-communicable Diseases - Molecular Mechanisms and Perspectives in Therapeutics. Advances in Experimental Medicine and Biology, vol 824. Springer, Cham. https://doi.org/10.1007/978-3-319-07320-0_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-07320-0_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-07319-4
Online ISBN: 978-3-319-07320-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)