Abstract
Special techniques can sometimes maximize the information obtained from nerve biopsy. The teasing apart of nerve fascicles to free single myelinated fibers for individual study, which has a long history dating to the days of Gombault (1886), has contributed greatly to understanding the pathological processes affecting peripheral nerve. In recent years, image analysis methods have permitted automated measurement of various parameters that occasionally prove helpful in characterizing the process afflicting the nerve under study. Although we do not rely heavily on these techniques, this chapter provides a brief discussion. The references will guide those seeking more detailed information.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Special techniques can sometimes maximize the information obtained from nerve biopsy. The teasing apart of nerve fascicles to free single myelinated fibers for individual study, which has a long history dating to the days of Gombault (1886), has contributed greatly to understanding the pathological processes affecting peripheral nerve. In recent years, image analysis methods have permitted automated measurement of various parameters that occasionally prove helpful in characterizing the process afflicting the nerve under study. Although we do not rely heavily on these techniques, this chapter provides a brief discussion. The references will guide those seeking more detailed information.
3.1 Fiber Teasing
Fiber teasing allows assessment of the pattern of nerve disease along several internodes of the same myelinated fiber. The most sensitive method for detecting segmental myelin changes, in principle, allows workers to determine whether these changes are primary or secondary to axon disease.
Dyck and colleagues provide the most comprehensive discussion of fiber teasing methodology and interpretation (Dyck et al. 1984; Dyck and Giannini 1993). We do not routinely employ nerve teasing in the assessment of biopsy specimens. Rather, we reserve this technique for special situations or research applications; some, but by no means all, workers share this approach (Logigian et al. 1994; Oh 1990; Schaumburg et al. 1992). Teasing is a difficult and tedious work and, as Dyck indicates, even an experienced technologist can prepare only 150–300 fibers a day (Dyck and Giannini 1993). Since the information gained from teased fiber examination is nonspecific, economic considerations mandate that diligent and experienced technologists may best utilize their energy in other areas.
When teasing is not performed properly, the information derived may be unreliable. Examining too few fibers risks drawing conclusions from a nonrepresentative sample. This result is especially likely when the technologist is not highly experienced and causes excessive fiber trauma, for even the most gentle teasing produces myelin artifact (Williams and Hall 1971). Large myelinated fibers are easiest to tease free, and as a result, a biased selection may thus be obtained. Dyck and colleagues have emphasized the need for appropriate sampling, suggesting that at least 100 fibers are necessary (Dyck and Giannini 1993). Assessment of demyelination “clustering” for deciding whether demyelination is primary or secondary requires at least five internodes per teased fiber. The literature, however, abounds with papers reporting results and even “normative data” based on as few as 20–50 teased fibers. Many papers even neglect to indicate how many fibers were studied.
As reviewed in Chap. 1 (Table 1.1), sural nerve biopsy may be a diagnostic procedure for many diseases, foremost among them vasculitis, amyloidosis, and leprosy. These three diagnoses, and indeed all others on the list of diseases for which sural nerve biopsy may be a diagnostic procedure, are not made on the basis of fiber teasing results. Workers most often use teased fibers to detect segmental myelin changes. In addition, teased fibers may permit distinction between primary and secondary demyelination. However, examining teased fibers does not lead to a specific diagnosis. In contrast, electron microscopy in demyelinating neuropathy can reveal macrophage-mediated myelin stripping, widened myelin lamellae, or various inclusions, all of which permit an etiologic diagnosis. Indeed, the long-standing belief based on teased fiber studies that segmental demyelination and remyelination in CMT-1 is secondary to axonal disease and the recent demonstrations that defects may be in either myelin or axonal proteins leads one to wonder how meaningful the identification of demyelination as “secondary” really is.
The degree to which teased fibers surpass semithin cross sections in revealing subtle myelin changes is unclear. In a seminal study of chronic inflammatory demyelinating polyneuropathy (CIDP, Prineas and McLeod 1976), all nerves in which 20 % or more of fibers showed segmental demyelination had evidence of the same on electron microscopy. Of 12 cases in which 1–10 % of fibers showed segmental demyelination, only 2 had EM changes. Only rarely will EM demonstrate segmental demyelination when teased fibers do not (McLeod et al. 1973). While such data suggests a considerably greater sensitivity of teased fibers, it is important to appreciate that the incidence of segmental myelin changes in controls is not zero. Research criteria for the diagnosis of CIDP require that at least 12 % of teased fibers should show segmental myelin changes (Ad Hoc Subcommittee 1991). Other authors have reported that 3.9–20 % of internodes are abnormal in control nerves on average (Behse 1990; Dyck and Giannini 1993; Tsakuda et al. 1987) with some normals showing even more frequent changes. Furthermore, the incidence of pathological alterations increases in aged controls (Dyck and Giannini 1993). By itself, paranodal myelin retraction, which teased fiber studies very easily detect, is difficult to interpret at any time, because this condition can occur in the earliest stage of segmental demyelination, in axonal degeneration (Williams and Hall 1971), and in normals (Arnold and Harriman 1970).
Evidence of axonal degeneration by demonstration of linear rows of myelin ovoids or of degeneration and regeneration by way of uniformly shortened internodes can also be seen in “normal” nerve, the incidence increasing with age (Arnold and Harriman 1970). Workers cannot regard as unequivocally abnormal up to 4 % of teased fibers showing rows of myelin ovoids (Arnold and Harriman 1970; Dyck and Giannini 1993). In addition, up to 16 % of fibers can show evidence of axonal regeneration in “normal” nerve (Behse 1990). In patients over 60 years of age, Arnold and Harriman (1970) reported that at least 6 of 24 teased fibers should show evidence of axonal degeneration or regeneration before a nerve could be considered abnormal.
Thus, the amount of “pathology” seen in normal nerves limits the usefulness of teased fiber studies in detecting subtle changes, especially with increasing age. Teased fiber abnormalities other than “wrinkled” myelin were seen in 7.5–37.5 % of 9 controls used by Behse (1990), the eldest only 54 years of age. Indeed, most normative data are based on the younger age group even though several studies (Jacobs and Love 1985; O’Sullivan and Swallow 1968; Vital et al. 1990) have shown a dramatic increase in nonspecific changes with age. Approximately half of nerves assessed in our laboratory come from patients over 60 years of age (Fig. 1.1).
A recent study of correlation between nerve conduction studies and sural nerve biopsy reported that in 11 of 52 instances (21 %) when both cross-sectional and teased fiber (minimum of 50 fibers) examinations were employed, the histological diagnoses were discordant (Logigian et al. 1994). However, in 48 % of these biopsies, three independent observers could not agree on the interpretations of the pathology. Thus, the subjective nature of nerve biopsy interpretation represents a greater source of error than whether or not fiber teasing is performed. Notably, the discordance between electrophysiological findings and biopsy results (63 % concordant, 14 % minimally discordant, and 23 % discordant) did not change when only teased fiber results were considered (Logigian et al. 1994).
In conclusion, light microscopic examination of 20 or more semithin cross sections, supplemented by careful electron microscopic review of selected nerve fascicles, leaves little need for teased fiber preparations. In some diseases, such as tomaculous neuropathies, teased fibers provide an elegant and convincing means of illustrating the pathology; however, we cannot identify a situation where our approach would lead to the loss of diagnostically useful information. We recognize the value of fiber teasing for research in peripheral nerve disease, especially when workers can study large numbers of fibers in multiple nerves. Yet, in the daily practice of peripheral nerve pathology, this approach seems insufficiently informative to justify its cost.
3.2 The Morphometric Study of Nerve Biopsies
Several quantitative analytic tools are available to those seeking to describe nerve pathology with greater precision than a subjective assessment of morphology allows. These “morphometric” techniques have become a sometimes useful adjunct to morphology. In our routine practice, other than an estimate of the severity of MF and UF loss, we only infrequently perform morphometric analysis, because morphology, not morphometry, gives specific diagnostic information.
Morphometry has, nevertheless, been important in the evolution of understanding of peripheral nerve function and disease. Quantitative techniques allow presentation of large amounts of data in compact graphs or scatter plots. Informed reading of the peripheral nerve literature also requires a certain familiarity with the various quantitative measures in use. Thus, the discussion below reviews some of the more important morphometric techniques but is by no means comprehensive. For more detailed information, we refer the reader to studies by Behse (1990), Dyck and co-workers (1984), Gibbels (1989), Hunter et al. (2007), and Thomas (1970).
To maximize the usefulness of fiber density measures, each laboratory should ideally use its own normals, prepared with a standard technique. The effect of tissue shrinkage resulting from use of different fixatives should be considered when comparing data from different laboratories. Workers should compare abnormal nerves only to age-matched normals. Some literature control data includes patients with stroke or ALS, on the assumption that these processes do not cause alterations in peripheral sensory nerves. Pollock and colleagues (1984) have shown that there may be alterations in the sural nerve of a hemiplegic limb. Moreover, a growing literature suggests that alterations of sensory fibers can occur in motor neuron diseases (Isaacs et al. 2007). Paid normal volunteers, where a full neurological history and physical examination can be performed along with electrophysiological studies, represent the best source of control data (Dyck and Giannini 1993). In the absence of such data, the rigorous approach described by Stoebner et al. (1989) is commendable. Their normal nerves came mostly from patients in acute (≤48 h) coma with no previous history of neuropathy, with normal electrophysiological testing of peripheral nerves, and with the specimen removed during organ harvest for transplantation. Because severely cachectic or bed-bound patients are at risk for nutritional and pressure palsies, workers should not consider them to have normal peripheral nerves.
3.2.1 Fiber Counts and Histograms
3.2.1.1 Myelinated Fibers
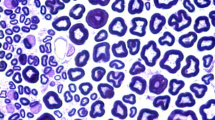
Investigators have invested much time and effort in studying the absolute number and density of fibers of various diameters in peripheral nerve (Tables 3.1 and 3.2). Myelinated fiber density (MF/mm2 of endoneurial cross-sectional area) is the standard measure, typically determined using toluidine blue-stained semithin (1 μm) sections. Modern image analysis technology has largely automated such measurements (da Silva et al. 2007; Hunter et al. 2007), although some interaction between technologist and computer still must occur. Dyck and colleagues have considered methodological issues in detail (Dyck et al. 1984).
The total number of fibers in the whole sural nerve varied by nearly a factor of two in one study, from 5,060 to 9,460 fibers (Behse 1990). Although favored by some authors, such measurements are more difficult to perform on nerve biopsy specimens than fiber density. Fiber density is more commonly used despite its dependency on several factors including fixation (10–36 % discrepancy) (Behse 1990; Tohgi et al. 1977), proper sampling (Behse et al. 1974; Dyck et al. 1984), and, in neuropathic nerves, hypertrophy of endoneurial contents (Behse et al. 1974). Fiber density decreases with age, one study showing values in the eighth decade falling to 70 % of those in the third decade (Tohgi et al. 1977). Most observers report similar data (Jacobs and Love 1985; O’Sullivan and Swallow 1968). At least part of this drop results from an increase of endoneurial area with age (Jacobs and Love 1985). Large MFs are more severely influenced in this regard than small MFs. However, the intrinsic variability of MF density does not allow distinction of “old” from “young” nerves on an individual basis.
In children, absolute sural nerve MF numbers probably increase in the first few years of life (Gutrecht and Dyck 1970; Jacobs and Love 1985), although not all investigators have observed this (Ferriere et al. 1985). Fiber density drops dramatically from values of about 20,000 MF/mm2 at birth to adult values by the age of 10 (Gutrecht and Dyck 1970; Jacobs and Love 1985; Ouvrier et al. 1987). This decrease occurs in parallel with an increase in endoneurial area from birth to the second decade, as axons enlarge and the interstitial space increases.
Myelinated fibers in the sural nerve range from 3 to 14 μm in diameter, defined as the combined width of axon and myelin. Histograms of MF numbers vs. diameter are bimodal, one mode clustering around a diameter of 4 μm, another around a peak of 10 μm, with an overlap between the two groups (Fig. 3.1a, b). Using a cutoff of 7 μm, Behse (1990) found that in normal nerves, 32–45 % fall above and 68–55 % below this value.
MF loss that affects large diameter fibers more than small diameter fibers, such as shown for CMT-1 (Fig. 3.1c), is a common and entirely nonspecific pattern of axon depletion. The opposite pattern, with more severe relative depletion of small myelinated fibers (Fig. 3.1d, Table 7.7), occurs infrequently but can provide a diagnostic clue with a limited number of potential etiologies.
When regenerating clusters are frequent, the relative proportion of small myelinated fibers increases, potentially creating a false impression of relative loss of large myelinated fibers. A shift of both peaks of a bimodal histogram to the left provides evidence of axonal atrophy (Ohi et al. 1985).
3.2.1.2 Unmyelinated Fibers
Unmyelinated fibers (UFs) range between 0.1 and 3.0 μm in diameter (although an UF 2–3 μm in diameter is rare), in a unimodal distribution with a peak at 1.0–1.3 μm (Behse 1990). Workers perform unmyelinated fiber quantitation on electron micrographs, although Johnson and colleagues (1994) have advocated immunocytochemical identification of axons by light microscopy as a rapid means of estimating UF density. Morphometry is technically more difficult for UFs than for MFs because of the greater number of sources of error when working with UFs; particularly distinguishing axons from other circular profiles within Schwann cells can prove difficult.
Unmyelinated fiber density varies even more than MF density (Table 3.1). Selective loss of UFs occurs only rarely and has a similar differential diagnosis to that of selective small MF loss (Table 7.7). With axonal degeneration and regeneration, the number of unmyelinated fibers can increase above the normal range, and the distribution becomes bimodal, with an increased number of very small (“miniature”) unmyelinated axons (Behse et al. 1975). When attempting to quantify UFs for purposes of assessing damage to this population of axons, one must decide what proportion of the counted axons are regenerating sprouts: these sprouts can be quite numerous and lead to the false conclusion that unmyelinated fibers are not affected. Thus, the process of counting unmyelinated fibers can be quite complex. Gibbels (1989) and Ochoa (1969b) provide comprehensive discussions.
3.2.2 Usefulness of Fiber Counts and Histograms in Assessment of Nerve Biopsy
As Tables 3.1 and 3.2 indicate, MF and UF densities vary widely in normal nerves, and decline with age, partially due to an increased endoneurial area. With axonal degeneration and regeneration, the formation of regenerating clusters may mask axonal loss. The substantial variability seen within normals makes fiber counts of little value for detecting mild neuropathy. With unmyelinated axons, direct visualization of axonal degeneration or indirect evidence such as denervated Schwann cell bands or excess collagen pocket formation (vide infra) is likely to testify to pathology before the actual UF count or density drops low enough to unequivocally indicate abnormality (Behse and Carlsen 1978).
An even more telling argument against the utility of fiber counts, detecting a subtle reduction of axon numbers puts the pathologist no nearer an etiologic diagnosis. The same considerations apply to interpreting changes in the fiber size–frequency histogram. With the exception of selective small fiber loss, even severe changes are nonspecific.
Consequently, we do not believe that precise quantitation of myelinated and unmyelinated axons has great value in the practice of diagnostic sural nerve pathology. Morphometry is undoubtedly valuable in research applications, especially when combining data from many nerves, permitting detection of important trends and leading to understanding of peripheral nerve pathophysiology (Behse 1990). In most instances, however, a quick count of myelinated axons on several representative sections using an eye piece reticule of known dimensions provides sufficient quantitative information.
3.2.3 The G-Ratio
The ratio of the diameter of an axon without its myelin to the diameter of the axon with its myelin is called the “G-ratio.” A high G-ratio indicates a thinner myelin sheath. Theoretical considerations suggest that a value of 0.6–0.7 is optimal for rapid conduction (Waxman 1980), and indeed normal nerves have a G-ratio close to this range. The G-ratio is somewhat higher (i.e., relatively thinner myelin) for small myelinated axons but generally varies between 0.5 and 0.8 for all fibers (Behse 1990; Jacobs and Love 1985). Because of relative hypomyelination at birth and during the first and second decades of life (Schroder et al. 1978), this age group has a higher G-ratio (Jacobs and Love 1985). Beyond 60 years of age, the scatter in G-ratio values increases greatly. This increased scatter presumably results from recurrent demyelination and remyelination causing some axons to have high G-ratios and axonal atrophy causing some fibers to have low G-ratios (Jacobs and Love 1985).
An increased G-ratio may indicate demyelination and remyelination, axonal regeneration (regenerating axonal sprouts are thinly myelinated), or primary hypomyelination. A uniformly high G-ratio, well beyond the range seen in normals or other neuropathies, is the hallmark of Dejerine–Sottas (CMT-3) syndrome. A low G-ratio may reflect hypermyelination, axonal atrophy, or both.
3.2.4 Endoneurial Area and Cell Counts
Normal endoneurial area of the sural nerve (excluding Renaut bodies and the subperineurial space) measures approximately 0.6–1.2 mm2 (Behse 1990). This area can increase in a nonspecific manner with neuropathy, although hypertrophic neuropathies bring about the greatest increases of up to fourfold or more (Behse et al. 1974). The enlarged endoneurial area results from collagen deposition, “empty” interstitial space, and increased cellularity (Behse et al. 1974) and leads to a spurious reduction in fiber density.
Investigators have counted Schwann cells and fibroblast nuclei in both normal and abnormal sural nerves. Nuclei of nonmyelinating Schwann cells ranged in number from 700 to 3,900/mm2 in 28 normals (Kanda et al. 1991), while Ochoa and Mair (1969a) observed between 1,700 and 2,700 Schwann cell nuclei of UF or MF type per mm2 in six normals. Schwann cell nuclei outnumber fibroblast nuclei by about 10:1 (Ochoa and Mair 1969a).
3.2.5 Regenerating Clusters
Regenerating clusters are hallmarks of axonal degeneration with regeneration (Fig. 4.24). These clusters are defined by the presence of three or more closely packed myelinated fibers and may be seen in normal nerves (Behse et al. 1975). Twenty, perhaps 40, clusters per mm2 probably represents the upper limit of normal, but usually, normal nerves have a considerably smaller number (Behse and Carlsen 1978; Fujimura et al. 1991). The myelinated fiber “cluster ratio,” which corrects for alterations in endoneurial area and for reductions in number of myelinated fibers, is defined as the number of regenerating clusters per 1,000 MFs (Gabreels-Festen et al. 1991). With an upper limit of 20 clusters per mm2, a “typical” nerve with MF density of 10,000/mm2 and endoneurial area of 1 mm2 would give a cluster ratio of two as an upper limit of normal.
3.2.6 Assessment of Unmyelinated Fiber Loss
We have discussed above the insensitivity of fiber counts for detection of UF depletion. Up to 1.8 % of unmyelinated axons can demonstrate active degeneration in normals, although the value is typically 0.5 % or less (Behse et al. 1975; Gibbels 1989). However, indirect measures may show greater sensitivity in this regard (Behse et al. 1975). Schwann cell subunits (ScSus) refer to unmyelinated fibers only and are defined as a group of cross-sectional profiles surrounded by a common basement membrane. A ScSu usually has two to five interdigitating or apposed profiles but can have up to 20 (Behse and Carlsen 1978). The profiles represent Schwann cell processes or their associated unmyelinated axons. The number of unmyelinated axons per ScSu ranges from 1 to 4 and decreases with age and neuropathy (Behse et al. 1975; Kanda et al. 1991). A ScSu without axons is referred to as “denervated.” Such denervated ScSus may result from loss of unmyelinated axons (Ochoa and Mair 1969b) or may reflect proliferation of Schwann cell processes (Kanda et al. 1991). Denervated ScSu are distinguished from bands of Büngner, which are conglomerations of Schwann cells previously associated with myelinated axons (Table 7.10).
Some ScSu alterations are sensitive indicators of UF loss. Denervated ScSu can appear in normals and increase in number before a drop in the UF density can be detected. In normal adult nerves, 4–37 % of ScSus (up to 10,000/mm2) are denervated, but the frequency of this finding increases with age and nonspecifically with neuropathy (Behse et al. 1975; Behse 1990; Gibbels 1989; Low et al. 1978). Ohnishi and colleagues (1974) and Pollock et al. (1984) obtained much lower values of 40–219 denervated Schwann cell “clusters” per mm2 but did not provide the criteria used to identify these structures.
The number of profiles per ScSu also increases with neuropathy. Investigators usually do not observe more than six profiles in a ScSu (<5 %), but 50 % or more of ScSus in patients with neuropathy can have this number of profiles (Behse et al. 1975). In normal nerves, collagen pockets occur in 10–24 % of ScSus (3,000–20,000/mm2), and this number increases with age or neuropathy (Behse 1990; Gibbels 1989; Low et al. 1978; Pollock et al. 1984). Solitary Schwann cell profiles number from 10 to 30,000/mm2 in normal nerves and also increase in number with age and neuropathy (Behse et al. 1975; Behse 1990; Gibbels 1989).
Only scanty pediatric normative data exist. Three children 2 to 13 years of age had 0–90 denervated ScSus/mm2 and 250–1,220 collagen pockets/mm2 (Ouvrier et al. 1981). Ochoa and Mair (1969b) found fewer than 1,000 denervated ScSus/mm2 in 2 children aged 15 and 16 years and 3,700 denervated ScSus/mm2 in an adult aged 59, illustrating how dramatically the frequency of this finding increases with age.
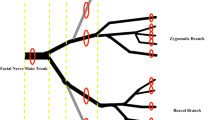
3.2.7 Internode Length
The length of a normal myelinated internode is a function of axon diameter and somatic growth. Teased fibers permit measurement of internode length for axons of various internodal diameters. A plot of internode length vs. fiber diameter for 20–50 teased fibers captures this relationship in an elegant fashion (Fullerton et al. 1965). Some variability in internode length is normal, but in peripheral neuropathy, certain patterns of alterations can occur. When a regenerating axon is remyelinated, the internodes tend to be a uniformly short length of about 200–400 μm. Not coincidentally, this range is similar to the internode length at birth (Jacobs and Love 1985). Thus, in axonal degeneration and regeneration, the histogram demonstrates numerous fibers of various diameters with uniformly short internodes. In contrast, random segmental demyelination results in residual long original internodes intermingled with short remyelinated internodes, producing a wide range of internode lengths along the same fiber. This technique can thus provide information about axon and myelin alterations in a peripheral nerve. Unfortunately, internode length varies by factor of two or more even in normals (Behse 1990), and axonal and myelin changes are increasingly prominent with normal aging (Arnold and Harriman 1970; Jacobs and Love 1985). Thus, as with most of the other morphometric techniques discussed above, pathologists often cannot distinguish mild or moderate pathology from the variability seen in normal, and especially older, patients.
3.3 Summary: The Utility of Morphometric Analysis
The data gathered by morphometric analysis can be displayed with fiber size–frequency histograms, G-ratio plots, and internode length vs. axon diameter displays. These approaches will give an elegant presentation of considerable information about the nature of the axonal and myelin changes in the nerve under study. However, from the perspective of a pathologist trying to make an etiologic diagnosis, we see little essential information emerging from the effort and expense that these methods entail; none of the various morphometric parameters give information about the specific cause of a neuropathy. Because of a large intrinsic variability in peripheral nerve parameters, quantitation does not permit detection of subtle changes. Too often, an impressive array of computer-generated plots and histograms is substituted for thorough review of many nerve cross sections. As a result, a focal but critical finding may be missed, such as a single vessel showing vasculitis, infiltration with atypical cells, or an epineurial granuloma. In practice, of the various measures reviewed above, we regard the presence of increased numbers of regenerating clusters as a valuable sign of myelinated fiber degeneration and regeneration. We also employ a subjective impression of increased numbers of denervated ScSus as an indicator of unmyelinated axon disease. We use diameter–frequency histograms and teased fiber study for research or education.
References
Ad Hoc subcommittee of the American Academy of Neurology AIDS task force. Research criteria for diagnosis of chronic inflammatory demyelinating polyneuropathy (1991) Neurology 41:617–618
Arnold N, Harriman DGF (1970) The incidence of abnormality in control human peripheral nerves studied by single axon dissection. J Neurol Neurosurg Psychiatry 33:55–61
Behse F (1990) Morphometric studies on the human sural nerve. Acta Neurol Scand 82(Suppl 132):1–38
Behse F, Carlsen F (1978) Histology and ultrastructure of alterations in neuropathy. Muscle Nerve 1:368–374
Behse F, Buchthal F, Carlsen F, Knappeis GG (1974) Endoneurial space and its constituents in the sural nerve of patients with neuropathy. Brain 97:773–784
Behse F, Buchthal F, Carlsen F, Knappeis GG (1975) Unmyelinated fibres and Schwann cells of sural nerve in neuropathy. Brain 98:493–510
da Silva AP, Jordão CE, Fazan VP (2007) Peripheral nerve morphometry: comparison between manual and semi-automated methods in the analysis of a small nerve. J Neurosci Methods 159:153–157
Dyck PJ, Giannini LA (1993) Pathologic alterations of nerves. In: Dyck PJ, Thomas PK et al (eds) Peripheral neuropathy, 3rd edn. WB Saunders, Philadelphia, pp 522–544
Dyck PJ, Karnes J, Lais A et al (1984) Pathologic alterations of the peripheral nervous system of humans. In: Dyck PJ, Thomas PK et al (eds) Peripheral neuropathy, 2nd edn. WB Saunders, Philadelphia, pp 760–870
Ferriere G, Denef JF, Rodriguez J, Guzzetta F (1985) Morphometric studies of normal sural nerves in children. Muscle Nerve 8:697–704
Fujimura H, Lacroix C, Said G (1991) Vulnerability of nerve fibres to ischaemia. A quantitative light and electron microscope study. Brain 114:1929–1942
Fullerton PM, Gilliatt RW, Lascelles RG, Morgan-Hughes JA (1965) The relation between fibre diameter and internodal length in chronic neuropathy. J Physiol 178:26P–28P
Gabreels-Festen AAWM, Joosten EMG, Gabreels FJM et al (1991) Hereditary motor and sensory neuropathy of neuronal type with onset in early childhood. Brain 114:1855–1870
Gibbels E (1989) Morphometry of unmyelinated nerve fibers. Clin Neuropathol 8:179–187
Gombault M (1886) Sur les lesions de la nevrite alcoolique. C R Acad Sci (D) 102:439–440
Gutrecht JA, Dyck PJ (1970) Quantitative teased fiber and histological studies of human sural nerve during postnatal development. J Comp Neurol 138:117–130
Hunter D, Moradzadeh A, Whitlock EL, Brenner MJ (2007) Binary imaging analysis for comprehensive quantitative histomorphometry of peripheral nerve. J Neurosci Methods 166:116–124
Isaacs JD, Dean AF, Shaw CE et al (2007) Amyotrophic lateral sclerosis with sensory neuropathy: part of a multisystem disorder? J Neurol Neurosurg Psychiatry 78:750–753
Jacobs JM, Love S (1985) Qualitative and quantitative morphology of human sural nerve at different ages. Brain 108:897–924
Johnson PC, Beggs JL, Olafsen AG et al (1994) Unmyelinated nerve fiber estimation by immunocytochemistry. Correlation with electron microscopy. J Neuropathol Exp Neurol 53:176–183
Kanda T, Tsukagoshi H, Oda M et al (1991) Morphological changes in unmyelinated nerve fibres in the sural nerve with age. Brain 114:585–599
Logigian EL, Kelly JJ, Adelman LS (1994) Nerve conduction and biopsy correlation in over 100 consecutive patients with suspected polyneuropathy. Muscle Nerve 17:1010–1020
Low PA, McLeod JG, Prineas JW (1978) Hypertrophic Charcot-Marie-Tooth disease: light and electron microscope studies of the sural nerve. J Neurol Sci 35:93–115
McLeod JG, Prineas JW, Walsh JC (1973) The relationship of conduction velocity to pathology in peripheral nerves: a study of the sural nerve in 90 patients. In: Desmedt JE (ed) New developments in electromyography and clinical neurophysiology, vol 2. S Karger, Basel, pp 248–258
Ochoa J, Mair WGP (1969a) The normal sural nerve in man. I: ultrastructure and number of fibres and cells. Acta Neuropathol 13:197–216
Ochoa J, Mair WGP (1969b) The normal sural nerve in man. II. changes in the axons and Schwann cells due to aging. Acta Neuropathol 13:217–239
Oh SJ (1990) Diagnostic usefulness and limitations of the sural nerve biopsy. Yonsei Med J 31:1–26
Ohi T, Kyle RA, Dyck PJ (1985) Axonal attenuation and secondary segmental demyelination in myeloma neuropathies. Ann Neurol 17:255–261
Ohnishi A, Dyck PJ (1974) Loss of small peripheral sensory neurons in Fabry disease. Arch Neurol 31:120–127
O’Sullivan DJ, Swallow M (1968) The fiber size and content of the radial and sural nerves. J Neurol Neurosurg Psychiatry 31:464–470
Ouvrier RA, McLeod JG, Morgan GJ et al (1981) Hereditary motor and sensory neuropathy of neuronal type with onset in early childhood. J Neurol Sci 51:181–197
Ouvrier RA, McLeod JG, Conchin T (1987) Morphometric studies of sural nerve in childhood. Muscle Nerve 10:47–53
Pollock M, Nukada H, Allpress S et al (1984) Peripheral nerve morphometry in stroke patients. J Neurol Sci 65:341–352
Prineas JW, McLeod JG (1976) Chronic relapsing polyneuritis. J Neurol Sci 27:427–458
Schaumburg HH, Berger AR, Thomas PK (1992) Disorders of peripheral nerves, 2nd edn. FA Davis Co, Philadelphia, p 45
Schroder JM, Bohl J, Brodda K (1978) Changes of the ratio between myelin thickness and axon diameter in the human developing sural nerve. Acta Neuropathol 43:169–178
Stevens JC, Lofgren EP, Dyck PJ (1973) Histometric evaluation of branches of peroneal nerve: technique for combined biopsy of muscle nerve and cutaneous nerve. Brain Res 52:37–59
Stoebner P, Mezin P, Vila A (1989) Microangiopathy of endoneurial vessels in hypoxemic chronic obstructive pulmonary disease (COPD). A quantitative ultrastructural study. Acta Neuropathol 78:388–395
Tackmann W, Spalke G, Oginszus HJ (1976) Quantitative histometric studies and relation of number and diameter of myelinated nerve fibres to electrophysiological parameters in normal sensory nerve of man. J Neurol 212:71–84
Thomas PK (1970) The quantitation of nerve biopsy findings. J Neurol Sci 11:285–295
Tohgi H, Tsukagoshi H, Toyokura Y (1977) Quantitative changes with aging in normal sural nerves. Acta Neuropathol 38:213–220
Tsakuda N, Koh CS, Inoue A et al (1987) Demyelinating neuropathy associated with hepatitis B virus infection. Detection of immune complexes composed of hepatitis B virus surface antigen. J Neurol Sci 77:203–216
Vital A, Vital C, Rigal B et al (1990) Morphological study of the aging human peripheral nerve. Clin Neuropathol 19:10–15
Waxman SG (1980) Determinants of conduction velocity in myelinated nerve fibers. Muscle Nerve 3:141–150
Williams PL, Hall SM (1971) Prolonged in vivo observations of normal peripheral nerve fibres and their acute reactions to crush and deliberate trauma. J Anat 108:397–408
Author information
Authors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Bilbao, J.M., Schmidt, R.E. (2015). Quantitative Techniques. In: Biopsy Diagnosis of Peripheral Neuropathy. Springer, Cham. https://doi.org/10.1007/978-3-319-07311-8_3
Download citation
DOI: https://doi.org/10.1007/978-3-319-07311-8_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-07310-1
Online ISBN: 978-3-319-07311-8
eBook Packages: MedicineMedicine (R0)