Abstract
Radiation therapy plays a central role in patients with locally advanced NSCLC who are not eligible for surgery. In fit patients, radiation is administered with concurrent chemotherapy leading to improved survival compared to either modality alone or the sequence of both. Different strategies to improve local control have been explored. Multiple dose escalation protocols produced higher local control rates and promising 2-year survival rates at radiation doses above 70 or even 80 Gy. However, higher doses are currently not recommended following the results of the recent phase III RTOG 0617 trial comparing standard dose radiotherapy with highdose (74 Gy) conformal radiotherapy which demonstrated a significant increase in the risk of death in the high dose arm. Altered fractionation regimens using concomitant boost or hyperfractionated and/or accelerated radiation therapy have reported to be successful, but logistics limited its use in routine practice. Technical advances in radiation therapy include PET CT planning, visualization of tumour hypoxia by dynamic PET-CT, stereotactic boost on hypoxic areas, proton beam therapy, IMRT and image-guided radiation therapy. The best systemic regimen to be used concurrently with radiation has yet to be defined; as has the role of induction and consolidation therapy in addition to concurrent chemoradiotherapy. Monoclonal antibodies such as bevacizumab and cetuximab have not been able to improve outcomes and the results of the phase III study of the novel anti-folate pemetrexed in combination with cisplatin compared to standard etoposide/cisplatin are awaited. The role of targeted agents in molecularly selected subgroups and the optimal treatment approach in unfit and elderly patients has yet to be defined and are the subject of ongoing clinical trials.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Anaplastic Lymphoma Kinase
- Intensity Modulate Radiation Therapy
- Advanced Lung Cancer
- Proton Beam Therapy
- Elective Nodal Irradiation
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Although surgery is generally viewed as the optimum treatment, only about 30 % of patients with non small cell lung cancer (NSCLC) are eligible for potentially curative resection [1]. Surgery may be followed by radiation therapy and/or chemotherapy depending onstage and quality of resection. About 50 % of patients receive palliative treatments only; most of those have advanced stage or metastatic disease. Palliative treatments include symptomatic radiation therapy, systemic treatment and best supportive care or a combination of those. The remaining 20 % of patients constitute an intermediate prognosis group, who has locally advanced disease. Locally advanced NSCLC usually refers to NSCLC tumors that are located within the thorax, i.e. harbor no systemic metastases but are not eligible for surgical resection, either because of the invasion of intra-thoracic structures or because of extensive ipsi- or contra-lateral mediastinal involvement. Patients with locally advanced disease such as stage IIIA with macroscopic disease in more than one nodal station or stage IIIB lung cancer are usually treated non-surgically. The high locoregional (80 %) and systemic (60 %) relapse rates of locally advanced disease mandate combined local and systemic treatment modalities [2]. Locally advanced NSCLC generally undergo chest radiotherapy (RT), with or without chemotherapy [3].
Initial studies of radiation therapy were performed with 200–260 kV orthovoltage or Cobalt-60 radiation therapy in the 1960s. They showed controversial benefit of irradiation, because the techniques did not allow sufficient dose to be delivered to the tumor. Subsequent attempts were made to improve the radiation dose delivery. The Veterans Lung Group (VALG) randomized chest irradiation vs. placebo vs. chemotherapy in 800 patients with localized inoperable NSCLC (mostly due to bulky disease) and Karnofsky performance status over 50 %. Target dose was 40–50 Gy, but 33 % received <40 Gy. One-year survival improved from 14 to 18 % [4]. The Vanderbilt trial in 1990 [5] randomized 319 patients with locally advanced, unresectable NSCLC to vindesine weekly, or irradiation to 60 Gy (2 Gy/fx), or both. Radiation-based modalities showed better response rates (30 % for RT, 34 % for chemoradiation and 10 % for chemotherapy) although median survival rates were similar 8.6 vs 9.4 vs 10.1 months and corresponding 5-year survival rates were 3 % vs 3 % vs 1 %. Consistent with this clinical dose response, an analysis of RTOG chemoradiotherapy trials demonstrated that biologically equivalent dose (BED) is strongly associated with local control (p < 0.0001), which in turn impacts on survival [6]. More recently, this correlation between BED and local control has been illustrated again by the successful treatments of early stage NSCLC with stereotactic radiotherapy when BED >100 Gy are delivered. However, these high dose, hypofractionated regimens cannot be delivered safely in stage III disease due to the volume of disease and proximity of the organs at risk (OAR). Strategies to improve local control with radiotherapy in locally advanced NSCLC include dose escalation with or without altered fractionation leading to a shortened overall treatment time (concept of acceleration) and individualized radiation dose escalation based on normal tissue dose constraints (isotoxic radiotherapy) facilitated by the use of modern radiotherapy techniques such as intensity modulated radiation therapy (IMRT). Additional strategies include combination with chemotherapy in routine practice or targeted therapies in clinical trials.
The aim of this chapter will be to assess the contribution of chemoradiation and advances in radiation oncology to local control and survival rates in the context of the multidisciplinary management of locally advanced NSCLC.
Chemotherapy and Radiation Therapy
Integrating Chemotherapy in the Radiation Therapy-Based Treatment Plan
The standard of care in the 70s–80s in locally advanced disease had been radiation therapy albeit with poor results. The broader use of cisplatinum in the 80s opened an area for improvements of care in lung cancer. The first evidence of a benefit of chemotherapy in addition to radiation therapy was established by the Cancer and Leukemia Group B(CALGB)8433 trial in 1990 for patients treated from 1984 through 1987 [7]. The CALGB 8433 trial included patients with excellent performance status to receive a cisplatinum and vinblastin induction chemotherapy regimen followed radiation therapy. Both median progression-free survival and overall survival improved, the latter by 4 months [7]. There was also a significantly higher proportion of long term survivors, and metastasis-free survival was improved in this study, while there was hardly any impact on local control. Similarly, Kubota et al. showed that a platinum-based chemotherapy followed by thoracic irradiation significantly increased the number of long-term survivors in locally advanced NSCLC, when compared with chemotherapy alone, although no increase in overall survival could be demonstrated [8]. Several other trials compared cisplatinum-based chemotherapy given concurrently to radiation therapy did not reproduce the survival benefit observed in 1992 in the split-course radiotherapy EORTC trial using a 3-week planned treatment gap (2-year survival of 26 vs 13 %) [9]. Later studies comparing induction chemotherapy/irradiation versus concurrent chemotherapy/irradiation demonstrated the superiority of concurrent chemotherapy/irradiation on survival.
In 1995, the Non-small Cell Lung Cancer Collaborative Group published one of the first meta-analyses with data from 52 randomized clinical trials, 22 of which focused on locally advanced NSCLC. It showed an overall survival benefit of chemotherapy with radical radiotherapy with a hazard ratio of 0.90, and an absolute benefit of 3 and 2 % at 2 and 5 years, respectively [10]. The highest evidence is for the use of platinum compounds [10–12]. The choice of chemotherapy doublets remains debated. A meta-analysis by Delbaldo et al. in 2004 suggested that a doublet regimen led to a significant increase in tumor response and overall survival when compared to single-agent regimen in combination with radiation therapy. Adding a third agent increased tumor control but had no impact on overall survival, while increasing toxicity [13]. Thus, the standard treatment should be a platinum-based doublet. There is no difference between cisplatin- and carboplatin-based regimen [11] and as such, chemotherapy agents may be adjusted to patient characteristics.
It is noteworthy that the median age of lung cancer patients at diagnosis is 71 years old (including 35 % of patients ≥75 years old) and few studies randomized patients over 70 years old, or with poor performance status. Over 50 % of patients present with comorbidities making them unfit for chemoradiation. As such, despite the high level of evidence of data favoring chemoradiation, and the feasibility of concomitant chemoradiation for fit elderly patients [14], patients eligible for this treatment regimen should be carefully selected and monitored. A Japanese phase III trial demonstrated improved survival of daily concurrent low-dose carboplatin compared to radiotherapy alone in a population older than 70 and ECOG performance status of 0–2, indicating that such an approach is feasible for selected elderly patients (median OS: 22.4 vs 16.9 months, HR 0.68, P = 0.0179) [15].
Optimal Timing for Chemotherapy
The question of optimal timing for chemotherapy with respect to radiotherapy has been repeatedly raised from the late 1980s to the early 2000s. Roughly a dozen randomized studies have been published in barely over a decade, yielding consistent results: concomitant chemoradiation improves both overall survival and progression-free survival. Aupérin et al. conducted a meta-analysis in 2010 based on individual patient data, pooling results from 6 trials (1,205 patients) [16]. There was a significant benefit of concomitant chemoradiation as compared with sequential radiation therapy and chemotherapy (HR = 0.84; 95 % CI 0.74–0.95): the absolute survival benefit was 5.7 % at 3 years. Progression-free survival analysis showed a trend towards a benefit of concomitant chemoradiation with a hazard ratio of 0.90 (95 % CI 0.79–1.01). Concomitant chemoradiation also had a significant impact on locoregional progression (HR = 0.77; 95 % CI 0.62–0.95) with an absolute decrease of 6.0 % at 3 years, but not on distant progression. Along with the effect of dose on survival, this advantage on both local control and survival but not distant control again suggests a role of local control on survival. More recently, confirmatory meta-analyses showed an absolute survival benefit of 4 % at 2 years and 2.2 % at 5 years (HR = 0.89; 95 % CI 0.81–0.98) for chemotherapy and radiation therapy in non-operated patients [11]. The survival advantage was stronger for concomitant chemoradiation, and for platinum-based chemotherapy regimens [12]. The ASCO guidelines subsequently recommended that cisplatin-based chemotherapy be administrated in patients with stage IIINSCLC [17].
Overall, these studies showed that concomitant chemoradiation is a standard of care for locally advanced NSCLC in patients who are medically eligible. Concomitant chemoradiation has however consistently been associated with a higher rate of certain types of toxicity, with as much as 18 % grade 3–4 esophageal toxicity (i.e. a relative risk of 4.9). Conversely, there has generally been no significant increase in lung toxicity [16].
Thus, although the benefit of chemoradiation over radiotherapy alone is widely accepted, the proper treatment sequence remains unclear. Several trials have studied the impact of induction or consolidation chemotherapy with chemoradiation [18, 19, 102, 103]. These trials showed no benefit of either induction or consolidation chemotherapy, but higher hematological toxicity rates. However, the CALGB 39801 trial hinted towards a benefit of induction chemotherapy in patients with poor pre-treatment performance status or significant weight loss, even though the survival rates were rather low in this study [18]. On the other hand, the PulmonArt trial showed a trend toward a better progression-free survival after consolidation cisplatinum-based chemotherapy [19]. A retrospective analysis of induction and consolidation chemotherapy suggested that one major prognostic factor was completion of the whole radiation therapy course, regardless of the chemotherapy sequence [20]. Van Houtte presented the results of a meta-analysis of 6 randomized trials, assessing the role of induction versus consolidation chemotherapy (with radical radiation therapy) at the World Congress of Lung Cancer of the International Association for the Study of Lung cancer (IASLC) in 2013 (Abstract P2.24-021). There was neither significant difference in survival nor disease free survival between the two sequences. Pros for induction chemotherapy include a potential to reduce tumor volumes before irradiation, which might improve the compliance with radiotherapy. Waiting times until irradiation might be long and unavoidable. Additionally, induction chemotherapy may help estimate the radiation sensitivity.
Advances in Radiation Therapy
Respiratory motion, gross tumor volume (GTV) definition variations between physicians and setup errors are potential sources of error in radiotherapy. Respiratory motion varies from day to day, and tumor and normal tissues can shrink, grow, and shift in response to radiation therapy and potentially other concomitant therapies. Motion management should be associated with image-guided means to ensure that radiation therapy is delivered as planned and to enable adaptive radiation therapy [21], which fits with the definition of image-guided radiation therapy (IGRT).
IGRT
Organ motion causes an averaging or blurring of the static dose distribution along the path of motion. Different methods can be used for tumor motion management while limiting the amount of normal tissues irradiated during treatment. Such motion management methods include forced shallow breathing by abdominal compression or breath hold motion encompassing techniques, and respiratory synchronized techniques such as respiratory gating and real-time tracking (AAPM Task Group 76).
Assessment of Tumor Motion
Computed tomography (CT) may image the entire range of tumor motion using slow CT, inhalation and exhalation breath-hold CT, or 4D or Respiration Correlated CT (listed by increasing workload). However, fast CT acquisition can introduce large systematic errors with respect to beam tumor alignment because the tumor snapshot position may not be the average tumor position. To solve this problem, inhalation and exhalation breath hold techniques, respiratory gating and respiration correlated or 4D CT have been used. During 4D CT, images are acquired at each couch position for many respiratory phases, which are recorded using external infrared markers or measuring airflow. The image acquisition is time-synchronized with the respiratory signal acquisition, allowing all images of a particular stage of the respiratory cycle to be concatenated into a complete 3D CT image. All of the phases put together make up a 4D CT data set. Incorporating the 4D information into the treatment planning may be performed using the mid-ventilation phase, representing the tumor‘s average position, and the extent of motion observed from all data sets to account for the motion. Maximum Intensity Projections (MIPs), which reflect the highest pixel value encountered from all CTs along the viewing ray for each pixel, giving rise to an artificial intensity display of the brightest object along each ray on the projection image may also be used. Alternatively, the tumor may be contoured on each phase and use the union of the contours (internal target volume ITV).
Management of Tumor Motion
Shallow Breathing or Breath-Hold Techniques
A stereotactic body frame cannot fully suppress breathing induced motion, and even with 5 mm antero-posterior and latero-lateral and 10 mm cranio-caudal margins about 15 % of the targets might be partially missed. Breath hold techniques may be used for compliant patients but increase treatment time.
Respiratory Synchronized Techniques
Need to establish a correlation between the real-time external breathing signal and the internal tumor motion and this correlation is verified during the course of treatment. Internal motion can be assessed by time resolved imaging techniques such as old generation “slow” CT scanning, which, due to its slow acquisition time, offers information on tumor position probability. The drawbacks are kinetic artifacts and blurred tumor borders. Alternatively, fast helical multi-slice CT acquisitions freeze the image of the tumor at one location at one particular moment in the breathing cycle. They can be used for respiratory cycle phase reconstruction. Respiratory motion is irregular and individual respiratory patterns cannot be fully assumed by observation prior to treatment.
The breathing pattern may rather be observed from an external signal allowing real-time observation, such as infrared reflective markers placed on the patient’s surface coupled with infra-red cameras. Tumor motion can be measured using the tumor itself, a marker implanted in or near the tumor or a surrogate organ such as the diaphragm. Respiratory gating involves the administration of radiation during certain intervals within a particular portion of the patient’s breathing cycle, commonly referred to as the beam-on-area or gating window [22]. For respiratory-gating, one might decide to delineate the tumor volume in the sorted treatment phase only, while accounting for uncertainties regarding patient’s breathing during CT-scanning being representative of the breathing during treatment and the correlation between external signal and internal tumor motion (irregular breathing, tumor response, baseline shifts). The choice of the gate width is a trade-off between minimizing motion and beam-on time. Another means of accommodating respiratory motion is tumor tracking, which repositions the radiation beam dynamically so as to follow tumor movements. This can be achieved by synchronizing the linear accelerator’s collimating system and movements with the target motion. With conventional multileaf collimation, the beam-collimating device needs to be aligned so that the leaf motion coincides with the major axis of the tumor motion. This however only allows one dimension to be compensated efficiently. Full 3D compensation may be realized with accelerators dedicated to whole-body stereotactic irradiation mounted on a robotic arm to allow tracking of respiratory motion. Tracking approaches rely on an accurate prediction model of the breathing motion to anticipate the future position of the tumor.
Verification of tumor position during treatment is generally performed using fluoroscopy or pairs of stereoscopic X-ray images co-registered with digitally reconstructed radiographs (DRR).
IMRT
Advantages and Principles of IMRT
Radiation therapy for locally advanced lung cancer may be limited by both the close vicinity of critical organs (e.g. heart, spinal cord, esophagus or, unexpectedly, bony structures) and the size of the irradiated target volume and subsequent amount of normal lung tissue to receive a significant dose. Another major issue is the physical uncertainties associated with dose delivery on moving targets. By shaping the dose distribution, IMRT enables better dose conformity to the PTV while sparing normal structures from high radiation doses. A retrospective dosimetric study by Liu et al. showed that in most cases of locally advanced lung cancer, IMRT plans resulted in lower doses to the heart, spinal cord, esophagus, and eventually resulted in a decrease of the lung V20 as shown in example in Fig. 6.1 [23].
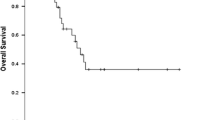
Although no prospective randomized study comparing 3D conformal radiation therapy (3DCRT) to IMRT in lung cancer has yet been published, retrospective studies suggest that IMRT be at least as effective as 3DCRT, in terms of overall survival (median survival time of 1.40 years in the IMRT group versus 0.85 years in the 3DCRT group), distant metastases-free survival and toxicity (hazard ratio of 0.33) [24].
The basic principles of IMRT derives from the fact that a set of intensity-modulated beams from multiple directions can be designed to produce dose homogeneity within the tumor similar to that from conventional radiotherapy but with superior conformity, especially for concave or other complex-shaped target volumes, thereby sparing nearby normal tissues. IMRT attempts to achieve more optimal absorbed-dose distributions by varying the beam intensity (fluency) within each incident beam, usually by subdividing the beam into a number of smaller segments and modulating each to achieve its selected fluency contribution. Furthermore, IMRT treatment planning allows the physician to implement his desired absorbed-dose distribution and the optimization involves a series of parameters to achieve this dose distribution [26].
Management of Physical Uncertainties in IMRT
However, there are potential drawbacks to steep dose gradients, including physical uncertainties regarding ability to deliver the dose to moving targets and to account for potentially changing dose heterogeneity patterns along the beam path. The first of these issues is due to breathing motions. Dynamic IMRT (as opposed to step and shoot IMRT) uses moving leaves while the dose is delivered. As the tumor and the multi-leaf collimator move simultaneously, it is uncertain whether the tumor will actually receive the planned dose, or just remain hidden by the leaves during the whole treatment sequence. After a large number of fractions, this so-called interplay effect, can cause a blurred dose distribution with an increased peripheral beam penumbra, leading to a less conformal dose distribution [26]. Blurring is increased by setup errors and intra or inter-fraction motion. When applied in actual treatment plans, these theoretical findings seem to have a limited impact on dose distribution [26]. This blurring effect may have significant impact incases with large organ motion, where real-time image guidance using tumor gating or tracking are indeed necessary.
This concern may be exacerbated when using flattening filter free (FFF) beams, which are getting more common in the last generation of linear accelerators, especially when dealing with stereotactic irradiation. The flattening filter’s role is to make the photon beam dose distribution uniform at reference depth within the allowed variations and its use significantly reduces the photon dose rate. While FFF beams allow much higher dose rates, which make for shorter treatment with fewer organ motions within the fraction [27], using FFF beams for large treatment fields might raise the question of dose uniformity within the target volumes. When used in dynamic IMRT, FFF beams seem even more susceptible to the interplay effect. This may be partially compensated using increased number of fields and fractions [28].
The impact of tumor and organ motion on dose distribution might be partially compensated for by using respiratory gating or tumor tracking. Additional changes include anatomical changes (patient and target geometry, tumor shrinkage, lung density changes…) over the course of treatment. In dosimetric studies, anatomical changes seem to have a larger effect on actual dose delivery than inter-fractional baseline shifts with an absolute difference in CTVT mean dose over 1 % [29]. This difference might be explained by the fact that respiratory motion is partly taken into account in the PTV margins. These changes may be best assessed by regular 4D-CT scans, measuring both anatomical changes and baseline shifts. As this is technically difficult, as well as time consuming, a mid-treatment 4D-CT scan may be recommended to assess the need for dosimetric adjustment.
Another concern is dose heterogeneity, which is inherent in IMRT. By increasing the number of beams, even though the dose conformity to the PTV may be higher, the dose distribution tends to be more heterogeneous. Adding a homogeneity dose constraint (e.g. standard deviation of the dose distribution less than 3 %, much like what would be seen in 3DCRT) may be used to increase the dose in the PTV while maintaining OAR dose constraints [30].
Low Doses in IMRT
Regarding normal lung irradiation, due to the increase in beam number in IMRT, lung V20 is significantly lower using IMRT in Liao’s retrospective study (37 % using 3DCRT versus 34 % using IMRT) [24]. Other studies have shown similar results of normal tissue sparing using IMRT, for lung and other critical structures. However, because of the increase in beam number, lung V5 is increased in IMRT (57 % versus 65 %) [24–31]. Low doses to a large amount of lung tissue can also result in late toxicity such as lung fibrosis. However, in the retrospective series of patients treated at the MD Anderson Cancer Center, only 5 % of patients demonstrated grade 2 (symptomatic) or higher fibrosis after 18 months [32]. Other toxicities also seem manageable, with under 20 % of grade 3 or higher esophageal toxicity in the MD Anderson patient series, under 10 % of grade 3 or higher dermatitis, and a Karnofsky Performance Status that remained stable in over 60 % of patients [32]. Similar topilot IMRT studies in other tumor types like head and neck tumors, unexpected toxicities may arise along the beam paths, due to the increased number of entry points. High dose voxels can occur in normal tissues, such as vertebra, ribs, or normal lung tissue, as an involuntary consequence of sometimes too harsh dose-constraints. Uyterlinde et al. recently reported a large number of vertebral fractures, in as many as 8 % of patients treated with IMRT and concurrent chemotherapy for NSCLC [33]. Although these results come from a small patient sample, they must be viewed as an incentive to be aware of unexpected toxicities, as with any new technique. Overall, even though most of the data on IMRT in lung cancer remains retrospective or purely theoretical, it seems to be a promising technique. Clinical outcomes with IMRT in locally advanced lung cancer are reported as good as or better than with 3DCRT, and with fewer and less severe toxicities.
Patterns of Care with IMRT
SEER analyses [34] suggested an increasing use of IMRT in stage III lung cancer between 2001 (0.5 %) and 2007 (14.7 %). Such increase is not related to clinical parameters but was rather observed in freestanding centers (as opposed to university hospitals) in an attempt to value (with Medicare reimbursement) high technology radiation therapy. This SEER-based study confirmed that the risk of radiation-induced pneumonitis and esophagitis is not increased with IMRT.
While IMRT is not approved in lung cancer (except for sulcus, paraspinal and some paracardiac tumors), it is performed in up to 100 % in some institutions.
Finally, patterns of practice are rapidly changing and the level of evidence for IMRT is increasing. 4D planning appears necessary with tumor motion monitoring limiting amplitudes to ≤1 cm and reduced CTV/PTV margins. Large tumors, in close proximity of OAR, such as the spinal cord, brachial plexus, esophagus, mediastinum, might be treated more efficiently with IMRT than with just conformal irradiation. Attention to cold and hot spots and attempts to limit the low doses to the normal lung (limited field number?) as well as carefully accounting for tissue heterogeneity/dose calculation algorithms/affected beamlets should be encouraged. Strict QA programs verifying reproducibility in all steps of the planning process to dose delivery are necessary. Of note, several technological advances may be analyzed indistinctly. For example, randomized studies are ongoing to determine the benefit of IMRT using 4DCT planning vs. 3DCRT (ClinicalTrials.gov: NCT00520702) and of image Guided Adaptive Conformal Photon vs. Proton Therapy in the concurrent setting (ClinicalTrials.gov: NCT00495170). Prospective randomized clinical trials are still needed to back up these findings. Several prospective studies are presented on the NCI clinicaltrials.gov website (NCT00921739, NCT01836692, NCT01166204, NCT00497250, NCT01617980, NCT01577212, NCT00938418, NCT00690963, NCT01411098747, NCT01429766, NCT01822496, NCT01912625, NCT01024829, NCT01059188, NCT01391260, NCT01494415, NCT01580579).
Dose
Dose Escalation
The standard dose regimen with standard 2D radiation therapy was established by the RTOG 7301 at 60 Gy in 2 Gy/fx [35]. However, median survival was about 10 months, with 3-year survival <10 %. Several other studies conducted in the 1980 sattempted to increase the dose to improve local control. They showed a strong correlation between total dose and local control and overall survival of locally advanced NSCLC [36]. The randomized phase I/II RTOG 8311 trial tested dose escalation (60, 64.8, 69.6, 74.5, and 79.2 Gy) using a hyperfractionated 1.2 Gy twice-daily regimen in 848 patients. The 69.6 Gy group had better outcomes than the lower doses groups. It was assumed that doses above 70 Gy did not increase survival further as a result of radiation-induced lung toxicity because of the volume of normal lung tissue irradiated [37]. Later studies increased the total dose with conformal irradiation [2] from 65 to 102 Gy with acceptable acute grade 3–4 lung and esophageal toxicity rates (4−12 %) with little reporting of late toxicities [38, 39]. Compared to historical results, dose escalation protocols produced higher local control rates (50−60 %) than standard radiotherapy, with 2-year survival rates around 40 %. The higher esophageal toxicity did not result in significant radiation protraction or interruption. Acute heart toxicities occurred in 8 % of a cohort of 50 patients treated with total doses up to 74 Gy [38, 39]. A retrospective study conducted by the Memorial Sloan Kettering in 2007 included 82 patients with inoperable NSCLC Stage I-IIIB [40]. A dose ≥80 Gy was used conformal radiation therapy with sequential chemotherapy. For stage III, 5-year local control and survival rates were 39 and 31 %, with advantage benefit of dose escalation consistent with other studies. Kong et al. [41] showed a benefit of dose escalation on 5-year survival with corresponding improvements with dose in local control. Further, phase I studies like one published by Rosenzweig et al. including 104 patients (65 % stage III and 6 % recurrent) receiving conformal irradiation without elective nodal irradiation showed significantly improved overall survival with dose ≥80.0 Gy, with induction chemotherapy given to 16 % of patients and no concurrent chemotherapy [42]. Crude late pulmonary toxicity was 7 %. The maximal tolerated dose with a normal tissue control probability (NTCP) constraint of 25 % was 84.0 Gy. The RTOG 84–07 (1984–1989) concomitant boost phase I/II trial used 45 Gy on large fields including primary + regional nodes and a 18 Gy boost on primary and involved nodes only to a total dose of 63 Gy. Dose was escalated from 63 to 70.2 Gy/5.5 or 5 weeks [43]. Acute and late toxicities increased within reasonable rates but survival was not statistically different between arms. For patients with Stage III/KPS > 70/no weight loss (i.e. eligible for CALGB 8433) 2-year overall survival was about 20 %.
Later trials, like the CALGB 30105 phase II trial, used dose-intense chemoradiation combinations. The CALGB used induction chemotherapy followed by concurrent chemoradiation in stage III NSCLC with dose-escalated thoracic conformal radiotherapy (74 Gy, once daily, 2 Gy per fraction) in both arms [44]. Patients were randomized between carboplatin/gemcitabine, which arm was closed prematurely due to an unacceptably high rate of grade 4–5 pulmonary toxicity attributed to radiosensitization by gemcitabine. The carboplatin/paclitaxel arm yielded a median survival of 24 months with a 12 % rate of grade 3 or higher pulmonary toxicity [44]. These promising results formed the basis for the experimental arm of the phase III RTOG 0617 trial.
The Randomized Phase III RTOG 0617 compared Standard- Dose (60 Gy) Versus High dose (74 Gy) Conformal Radiotherapy with in patients with Stage IIIA/IIIB Non-Small Cell Lung Cancer. The 2 × 2 factorial design consisted of weekly concurrent carboplatin–paclitaxel chemotherapy with randomization between 60 Gy or 74 Gy, and two cycles of Concurrent and Consolidation Carboplatin/Paclitaxel with or without cetuximab. The high dose arm was closed prematurely after showing 85 documented events and a likely detrimental effect with high dose radiotherapy, which correlated with patient-reported deteriorated quality of life [104]. Updated analysis after 207 events demonstrated a significant increased risk of death in the high dose arms (median survival 28.7 months (60 Gy arm) vs. 19.5 months (74 Gy), p = 0.0007), with a 37 % increased risk of local failure in the high dose arms. There were also a trend for more treatment-related deaths in the high dose arms (10 vs. 2) [105]. Why the RTOG 0617 trial is not consistent with the results of previous phase II trials remains investigational and methodological issues are being looked for. While the exact reasons for such deleterious effects are yet unknown, it was shown that these results are consistent with patient-reported quality of life (ASTRO 2013). Hypotheses include accelerated repopulation due to protracted irradiation, increased reported protocol deviations, under-reporting of lung and cardiac treatment-related deaths in patients who received excessive radiation dose to heart and lung in the high dose arms, and a possible negative interaction between cetuximab and high dose radiotherapy.
Altered Fractionation
Altered fractionation regimens using concomitant boost or hyperfractionated and/or accelerated radiation therapy have been conducted in locally advanced lung cancer. The CHART (Hard hyperfractionation through Continuous Hyperfractionated Accelerated RadioTherapy) trial has demonstrated that overcoming the accelerated repopulation effect by delivering 54 Gy three times daily in 12 consecutive days results in a significant survival benefit compared to conventional regimens [45]. However, logistics of delivering irradiation thrice daily for 12 days limited its use in routine practice. Alternatively, many combinations using either different timings or different drugs were subsequently used to improve local control, distant control and survival. Several phase II trials like the RTOG 9204 (twice daily irradiation with chemotherapy) showed improved local control at the expense of higher esophageal toxicities [46]. More recently, an individual patient data meta-analysis of 10 randomized trials (2,000 patients) comparing hyperfractionated and/or accelerated radiotherapy to conventional fractionation has confirmed the advantage of altered fractionation, increasing 5-year survival rates by 3 %. Dose escalation and dose redistribution based on functional imaging is at the heart of the EU Framework Program 7 (FP7) funded PET Boost trial (ClinicalTrials.gov Identifier: NCT0102482). The overall treatment dose is escalated by increasing the dose-per-fraction until specified dose constraints are met. The patients are randomized to receive the standard regimen (66 Gy given in 24 fractions of 2.75 Gy) with either an integrated boost to the primary tumor as a whole or to the 50 % SUVmax area of the primary tumor based on the pre-treatment FDG-PET CT scan.
Dose Volume
If local control may be improved by radiotherapy dose escalation according to several studies, toxicity, including esophageal toxicity, and more particularly pulmonary toxicity seems to be related to radiation volume. In locally advanced non-small cell lung cancer, eliminating elective nodal irradiation allows to maximize tumor dose and minimize normal tissue toxicity in combined modality treatments. The use of staging modalities such as positron emission tomography allows encompassing the tumor volume with more accuracy. Several retrospective, randomized phase III studies and a meta-analysis of 1,705 patients from 4 RTOG trials (7811, 7917, 8311, 8407) have confirmed that involved-field irradiation results in a regional nodal failure rate of less than 10 % [47–49] and suggest that it can be performed in routine practice. To that extent, PET CT is highly recommended for suitable diagnostic work up and pre therapeutic staging [50].
Multimodal Imaging for Radiation Therapy Planning and Dose Painting
PET CT in Radiotherapy Planning
PET CT has emerged as an important imaging modality for radiotherapy planning in locally advanced lung cancer as shown in Fig. 6.2 [50, 51]. It helps distinguish between tumor and atelectasia and allows more accurate staging than CT [52, 53]. This results in about a third of patients not receiving the planned curative irradiation and may result in better outcomes in curative disease on PET CT even without dose escalation [54]. However, such data must be interpreted with caution as they are probably a consequence of stage migration. Another study assessed staging changes on hybrid PET/CT scans repeated within 120 days of an initial staging PET/CT [55]. Radiation treatment planning based on repeat PET CT identified significant upstaging in more than half of patients. For a subset of patients who underwent both scans on the same instrument, SUV velocity predicted upstaging, but the difference between those upstaged and those not was statistically significant.
Accounting for Hypoxia in RT Planning
Hypoxia has consistently been associated with tumor radioresistance and tumor angiogenesis. Blood flow and volume are both indirect measures of tumor angiogenesis and can be assessed by perfusion studies. Several studies however suggest that there is no correlation between perfusion parameters, using Dynamic contrast-enhanced CT (DCE-CT) that quantifies vasculature properties, and metabolic activity using PET CT in large tumors [54]. Both imaging modalities are however able to show intra-tumor heterogeneity.
An extensively investigated tracer for visualization of tumor hypoxia by dynamic PET-CT is fluorine-18-labeled fluoromisonidazole (18F-FMISO; half life 110 min). Preclinical and clinical studies have revealed a correlation between oxygen measurements and 18F-FMISO uptake. Small preliminary studies demonstrated an association between high tumor-to-muscle FMISO uptake ratios and risk of relapse as well as prediction of outcomes based on FMISO uptake decrease on repeat FMISO PET CT. The HIL trial (Heidelberg team, NCT01617980) currently investigates the correlation between 18F-FMISO PET-CT and functional MRI for tumor hypoxia imaging in patients with inoperable stage IIINSCLC, treated with 4D-CT based IMRT. Other tracers, such as the [(18)F]HX4 is a promising hypoxia PET-tracer, are being studied [56]. In a series of 15 patients, the majority of NSCLC lesions showed considerable [(18)F]HX4 uptake. The heterogeneous uptake pattern was stable between 2 and 4 h with PET imaging at 4 h being superior.
Stereotactic Irradiation as a Boost on Hypoxic Areas
Most experience with stereotactic irradiation is based on limited stage disease management, for inoperable patients. Its use has recently expanded for the management of operable early stages in comparison with surgery (several ongoing randomized phase III trials). The definitions of stereotactic irradiation are various as are the equipments to deliver the dose stereotactically (often in the hypofractionated mode) and the methods used for motion management. There has been limited room for stereotactic ablative radiation therapy (SABR) in the management locally advanced NSCLCC for such clear reasons as tumor bulk (potentially deteriorated coverage, red shell constituting a danger zone on normal tissues outside the PTV). However, SABR is increasingly used either as consolidative planned boost (+/− dose escalation) [57] or as a stereotactic boost for residual disease (or in the recurrent setting). Preliminary retrospective data in patients with stage III disease including N2 disease suggest that a risk adaptive systematic dose escalation strategy with SABR (25 Gy in 5 fractions following 50 Gy conformal irradiation) following external beam radiotherapy is feasible [57]. Such systematic boost strategies may be particularly interesting to boost hypoxic regions. However, moderate to severe acute toxicities were encountered in about 25 % of patients, emphasizing the need for optimal patient selection for hypofractionated SABR. Another study prospectively investigated the role of SABR to deliver a boost on residual disease [58]. Patients without metastatic disease and with radiologic evidence of limited residual disease (≤5 cm) within the site of the primary tumor and good or complete nodal response after standard chemoradiation to a target dose of 60 Gy were considered eligible for an SABR boost. The total combined dose biological equivalent dose was >100 Gy to the residual primary tumor, in two 10 Gy-fractions for peripheral tumors, or three 6.5 Gy- fractions for central tumors according to the RTOG protocol 0813 definitions. After a median follow-up of 13 months, out of 33 patients, four patients developed acute grade 3 radiation-induced pneumonitis, and 1 developed late and persistent grade 3 pneumonitis. At the time of analysis, the actuarial local control rate at the primary tumor site was 83 %. Linear accelerator-based SBRT for dose escalation of limited residual NSCLC after definitive CRT was feasible and did not increase the risk for toxicity above that for standard radiation therapy. Proper daily intra-fractional IGRT methods are necessary and tumor tracking should be recommended whenever possible to best account for intra-fraction movements [59], especially when hypofractionation is used.
Several phase I/II clinical trials currently investigate the role of stereotactic irradiation in locally advanced non-small cell lung cancer (NCI clinicaltrials.gov : NCT01657617, NCT01656460, NCT01746810, NCT01300299, NCT01463423, NCT01051037, NCT01899989, NCT01781741, NCT01345851, NCT00945451, NCT01711697, NCT01543672).
Future Drugs
Pemetrexed
Pemetrexed inhibits enzymes involved in nucleotide synthesis by acting as afolate competitor. Compared to gemcitabine, pemetrexed, in association with cisplatin, increased overall survival in metastatic non-squamous NSCLC [60]. Preclinical studies have shown that pemetrexed is a potential radiosensitizer with radiosensitization depending on drug concentration and tumor type, with an enhancement ratio as high as 1.6 in the LXI lung tumor cell line [61]. Several phase I and II studies have demonstrated that combining pemetrexed with concurrent radiation only yielded moderate toxicities [62–64], was efficient in locally advanced stage III NSCLC and can be safely given at full systemic doses with thoracic radiation therapy [65, 66]. The negative CALGB 30407 trial included squamous NSCLC where activity of pemetrexed is known to be limited [66]. Subsequent trials only included non-squamous NSCLC. The PROCLAIM phase III trial started in 2008, and compared cisplatin plus pemetrexed to cisplatin plus etoposide with concurrent 66 Gy thoracic radiation therapy followed by consolidation chemotherapy [67]. Its aim is to determine if concurrent pemetrexed/cisplatin would translate into a survival benefit. The study enrolled nearly 600 patients. There was a similarly high dose-intensity in both arms, and preliminary results demonstrated significantly lower incidences of overall adverse events and some toxicities including granulocytopenia and infections in the pemetrexed/cisplatin arm [106]. Full presentation of the study results including potential late toxicities is awaited.
More recently, in 2010, the French Thoracic Oncology Group (IFCT) started the IFCT 0803 phase III trial, comparing cisplatin plus pemetrexed with concurrent 66 Gy thoracic irradiation, with or without cetuximab [68]. This “best of” trial combined all up-to-date advances together, i.e. chemoradiation, induction chemotherapy, high dose irradiation (66 Gy), pemetrexed, cetuximab, and a platinum-based doublet. The IFCT 0803 trial just terminated accrual of 106 patients. Garrido et al. recently presented the data of the pemetrexed-cisplatinum (500 mg/m2, 75 mg/m2 d1 q21d) induction and chemoradiation phase II study in non-squamous NSCLC. Progression free survival (1-year rate of 51 %) was similar to that observed in other cisplatinum-based induction and concurrent protocols. The overall response rate was 59 % with 13 % having progressive disease. Dose-intensity was maintained in 71 % of patients. Grade 3–4 toxicities (esophagitis, neutropenia) during the chemoradiation phase were around 10 %, which is generally considered acceptable for locally advanced NSCLC undergoing radical chemoradiation.
Cetuximab
Cetuximab is a monoclonal antibody targeting epidermal growth-factor receptor (EGFR). There have been suggestions, in the FLEX phase III for example, that patients who had a higher expression of EGFR in their tumors (as measured by immunohistochemistry) had a better response than patients with low expression [69]. There was also a strong rationale from preclinical studies [67] and the RTOG 0324 study, to add cetuximab to chemoradiation. Preliminary results from the RTOG 0617 trial at the 15th World Conference on Lung Cancer (Abstract PL03 2013) however suggest that there is no clinical benefit from the addition of cetuximab to chemoradiation in patients with unresectable stage III NSCLC.
Furthermore, the addition of cetuximab is associated with increased toxicity. The cetuximab analysis was carried out on 465 patients, with a median follow-up of 19 months. Weekly cetuximab was added to weekly chemotherapy with carboplatin and paclitaxel, given concurrently with radiation. Median overall survival for patients treated with chemoradiation with or without cetuximab was 23 months, the 18-month overall survival rate 60 %, and median progression-free survival 10 months in both arms. Overall combined adverse events were reported by 85 % of patients treated with chemoradiation with cetuximab vs 70 % without cetuximab, while overall non hematological adverse events were reported by 71 % vs. 51 % of patients, respectively (p <0.0001).
New Targeted Therapies and Other Therapeutics
Patients with EGFR-mutated locally advanced NSCLC have lower local recurrence rates following radiotherapy and/or chemotherapy, raising the hypothesis that EGFR mutation might confer sensitivity to some EGFR inhibitors in a way that is synergistic with irradiation [70, 71]. Tolerance studies have shown that standard dose of EGFR inhibitors such as erlotinib or gefitinib could be given during chemoradiation without significantly increasing toxicities [72, 73]. However, so far, most studies investigating the use of EGFR-tyrosine kinase inhibitors with chemoradiation have been rather disappointing, with survival rates lower or close to those seen with chemoradiation alone [73–77]. In particular, the SWOG S0023 study, comparing gefitinib and placebo after cisplatin/etoposide/63 Gy and consolidation docetaxel in stage III NSCLC, showed an increased mean survival time in the placebo arm (35 versus 23 months in the experimental arm), leading to premature trial closure [74]. Similarly, the use of gefitinib after resection of stage III NSCLC was not associated with increased survival [78]. These study results suggest that the use of EGFR-TKI in an EFGR mutation unselected stage III NSCLC population is not warranted and future study should focus on the integration of EGFR-TKI to chemotherapy in patients with activating EGFR mutations.
Available evidence clearly indicates that the mutational landscape, including EGFR mutations [79–86] and ALK translocations [87, 88], of non-small cell lung cancers is relevant to therapeutics to yield personalized medicine.
One recent breakthrough was the discovery of chromosomal rearrangements of the anaplastic lymphoma kinase gene (ALK) in non small cell lung cancers, which can be targeted using oral ALK inhibitors such as crizotinib. Crizotinib was shown superior to standard chemotherapy in patients with previously treated and untreated, advanced non-small-cell lung cancer with ALK rearrangement [107]. Further, preliminary retrospective data suggest that crizotinib not only can be delivered during irradiation but also yields interesting control rates in oligoprogressive lung cancer treated with chemoradiation [89, 90]. Clinical trials in stage III ALK positive NSCLC would be of interest, although their conduction is a challenge due to the low incidence of this rare molecular alteration comprising only 4 % of NSCLC patients. A randomized phase II trial in molecularly selected patients with stage III NSCLC is currently ongoing (RTOG1306).
Anti-angiogenics such as bevacizumab have shown promises in metastatic setting when combined with chemotherapy in NSCLC and has become a first-line therapy in many facilities [91, 92]. However, when used in a radiotherapy setting, bevacizumab is associated with major toxicities, including tracheo-esophageal fistulae, pulmonary hemorrhage, particularly in squamous histology tumors [93, 94], with no survival benefit. As such, there are currently no ongoing trial using bevacizumab concurrently with radiotherapy with lung cancer and its use should be avoided in this setting. Others anti-angiogenics have been assessed in association with chemoradiation or radiation therapy alone in NSCLC. The use of the anti-angiogenic agents (AE-941 or thalidomide) was associated with increased toxicity, mainly thrombo-embolic events, but did not increase survival [95, 96].
Many other targeted agents have been tested in clinical trials, such as efaproxiral, which reduces hemoglobin oxygen-binding affinity, increasing tissue pO2, as a mean to overcome tumor hypoxia. In this study, efaproxiral, combined with radiotherapy after induction chemotherapy resulted in 20.6 months survival, with low toxicity incidence, which makes it a promising drug [97]. A new vaccine to MUC-1, L-BP25, has shown great promise in stage IIIB and IV NSCLC in a phase II trial, with an increase in median survival (30.6 versus 13.3 months) in stage IIIB disease [98]. Based on these results, the phase III START trial randomized 1320 patients with unresectable stage III NSCLC who had disease control after first line chemo-radiotherapy to receive either L-BP25 (Stimuvax) or placebo after priming with cyclophosphamide 300 mg/m2 [108]. The primary endpoint overall survival was not met (25.6 vs 22.3 months, HR 0.88, p = 0.12). However, when analyzing the large subgroup of patients (n = 806) who have received standard concurrent chemoradiotherapy as opposed to sequential treatment, overall survival was increased in the vaccination arm by almost 10 months (30.8 vs 20.6 months, HR 0.78, p = 0.016). Following this encouraging observation a phase III study (START 2) including only patients treated with standard concurrent chemoradiotherapy has been initiated.
Another phase III study investigating the use of GV 1001, a telomerase peptide vaccine, after chemoradiation is planned, following a phase II study showing a significant increase in overall survival (19 versus 3.5 months) in immune responders [99].
Proton Therapy
Proton beam therapy (and particle beam therapy) represents an attractive technological advance due to physical characteristics of protons that allow more precise dose delivery into the tumor (spread out Bragg peak) while potentially sparing normal tissues. Yet there are only three validated indications (eye tumors, skull base chordomas/chondrosarcomas, some pediatric and sarcoma tumors) while lung cancer represents a substantial challenge in terms of motion management, tissue composition and density and imaging guidance and is an intense field of research. Lopez Guerra et al. compared the outcomes of 250 patients with NSCLC who were treated with 66 Gy of photons or 74 Gy Equivalent (GyE) of protons [100]. Their 1-year diffusing capacity of lung for carbon monoxide (DLCO) declined significantly more in the conformal chemoradiation group as compared to proton beam therapy after adjustment for pre-treatment characteristics. Sejpal et al. focused on survival in 202 patients with locally advanced unresectable NSCLC who were treated with 74 GyE of proton beam therapy or 63 Gy of either IMRT or conformal chemoradiation with a median follow-up of 1.5 years [101]. Median overall survival rates were 24, 18, and 18 months for proton beam therapy, IMRT, and chemoradiation, respectively. Eight phase I/II trials and one randomized phase III trial including proton beam therapy for locally advanced non-small cell lung cancer are currently reported on the NCI clinical trials database (NCI clinicaltrials.govNCT00881712, NCT01770418, NCT00915005, NCT01629498, NCT01993810, NCT01386697, NCT01076231, NCT01108666, NCT01565772). To date, proton beam therapy should only be performed within clinical trials.
Conclusion and Perspectives
The standard treatment to date remains high dose (60–66 Gy) cisplatinum-based chemoradiation. Induction or consolidation chemotherapy may also be used. The next years will be dedicated to building the level of evidence for new techniques such as IMRT, stereotactic irradiation and proton beam therapy along with using optimal multi-modality imaging that includes PET CT and online and adaptive image guidance/ motion management. Optimizing combinations with chemotherapy and/or targeted therapies will be further investigated to improve local control and survival. Quality of life and patient reported outcomes, cost effectiveness and personalized therapies may also become current practice in locally advanced NSCLC.
References
Little AG, et al. Patterns of surgical care of lung cancer patients. Ann Thorac Surg. 2005;80:2051–6; discussion 2056.
Girard N, Mornex F. Radiotherapy for locally advanced non-small cell lung cancer. Eur J Cancer (Oxf Engl). 2009;199045 Suppl 1:113–25.
Mauguen A, et al. Surrogate endpoints for overall survival in chemotherapy and radiotherapy trials in operable and locally advanced lung cancer: a re-analysis of meta-analyses of individual patients’ data. Lancet Oncol. 2013;14:619–26.
Roswit B, et al. The survival of patients with inoperable lung cancer: a large-scale randomized study of radiation therapy versus placebo. Radiology. 1968;90:688–97.
Johnson DH, et al. Thoracic radiotherapy does not prolong survival in patients with locally advanced, unresectable non-small cell lung cancer. Ann Intern Med. 1990;113:33–8.
Machtay M, et al. Defining local-regional control and its importance in locally advanced non-small cell lung carcinoma. J Thorac Oncol. 2012;7:716–22.
Dillman RO, et al. A randomized trial of induction chemotherapy plus high-dose radiation versus radiation alone in stage III non-small-cell lung cancer. N Engl J Med. 1990;323:940–5.
Kubota K, et al. Role of radiotherapy in combined modality treatment of locally advanced non-small-cell lung cancer. J Clin Oncol. 1994;12:1547–52.
Schaake-Koning C, et al. Effects of concomitant cisplatin and radiotherapy on inoperable non-small-cell lung cancer. N Engl J Med. 1992;326:524–30.
Chemotherapy in non-small cell lung cancer: a meta-analysis using updated data on individual patients from 52 randomised clinical trials. Non-small Cell Lung Cancer Collaborative Group. BMJ. 1995;311:899–909.
Aupérin A, et al. Concomitant radio-chemotherapy based on platin compounds in patients with locally advanced non-small cell lung cancer (NSCLC): a meta-analysis of individual data from 1764 patients. Ann Oncol. 2006;17:473–83.
Okawara G, Mackay JA, Evans WK, Ung YC, Lung Cancer Disease Site Group of Cancer Care Ontario’s Program in Evidence-based Care. Management of unresected stage III non-small cell lung cancer: a systematic review. J Thorac Oncol. 2006;1:377–93.
Delbaldo C, et al. Benefits of adding a drug to a single-agent or a 2-agent chemotherapy regimen in advanced non-small-cell lung cancer: a meta-analysis. JAMA. 2004;292:470–84.
Topkan E, Parlak C, Topuk S, Guler OC, Selek U. Outcomes of aggressive concurrent radiochemotherapy in highly selected septuagenarians with stage IIIB non-small cell lung carcinoma: retrospective analysis of 89 patients. Lung Cancer. 2013;81:226–30.
Atagi S, et al. Thoracic radiotherapy with or without daily low-dose carboplatin in elderly patients with non-small-cell lung cancer: a randomised, controlled, phase 3 trial by the Japan Clinical Oncology Group (JCOG0301). Lancet Oncol. 2012;13:671–8.
Aupérin A, et al. Meta-analysis of concomitant versus sequential radiochemotherapy in locally advanced non-small-cell lung cancer. J Thorac Oncol. 2010;28:2181–90.
Pisters KMW, et al. Cancer Care Ontario and American Society of Clinical Oncology adjuvant chemotherapy and adjuvant radiation therapy for stages I-IIIA resectablenon small-cell lung cancer guideline. J Thorac Oncol. 2007;25:5506–18.
Belani CP, et al. Combined chemoradiotherapy regimens of paclitaxel and carboplatin for locally advanced non-small-cell lung cancer: a randomized phase II locally advanced multi-modality protocol. J Thorac Oncol. 2005;23:5883–91.
Van Meerbeeck JP, et al. Mature results of PulmonArt: involved-field 3D radiotherapy (RT) and docetaxel/cisplatin chemotherapy (CT) in a randomised phase 2 study comparing concurrent CT-RT followed by consolidation CT, with induction CT followed by concurrent CT-RT in patients (pts) with stage III non-small cell lung cancer (NSCLC): B5-06. J Thorac Oncol. 2007;2(8):S349–50.
Garrido P, et al. Predictors of long-term survival in patients with lung cancer included in the randomized Spanish Lung Cancer Group 0008 phase II trial using concomitant chemoradiation with docetaxel and carboplatin plus induction or consolidation chemotherapy. Clin Lung Cancer. 2009;10:180–6.
Guckenberger M, Wilbert J, Richter A, Baier K, Flentje M. Potential of adaptive radiotherapy to escalate the radiation dose in combined radiochemotherapy for locally advanced non-small cell lung cancer. Int J Radiat Oncol Biol Phys. 2011;79:901–8.
Giraud P, et al. Respiratory gating techniques for optimization of lung cancer radiotherapy. J Thorac Oncol. 2011;6:2058–68.
Liu HH, et al. Feasibility of sparing lung and other thoracic structures with intensity-modulated radiotherapy for non-small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2004;58(4):1268–79.
Liao ZX, et al. Influence of technologic advances on outcomes in patients with unresectable, locally advanced non-small-cell lung cancer receiving concomitant chemoradiotherapy. Int J Radiat Oncol Biol Phys. 2010;76(3):775–81.
Prescribing, recording, and reporting photon-beam intensity-modulated radiation therapy (IMRT): contents. J ICRU. 2010;10:NP–NP.
Bortfeld T, Jiang SB, Rietzel E. Effects of motion on the total dose distribution. Semin Radiat Oncol. 2004;14(1):41–51.
Thomas EM, et al. Effects of flattening filter-free and volumetric-modulated arc therapy delivery on treatment efficiency. J Appl Clin Med Phys. 2013;14:4328.
Ong CL, Dahele M, Slotman BJ, Verbakel WFAR. Dosimetric impact of the interplay effect during stereotactic lung radiation therapy delivery using flattening filter-free beams and volumetric modulated arc therapy. Int J Radiat Oncol Biol Phys. 2013;86:743–8.
Schmidt ML, Hoffmann L, Kandi M, Møller DS, Poulsen PR. Dosimetric impact of respiratory motion, interfraction baseline shifts, and anatomical changes in radiotherapy of non-small cell lung cancer. Acta Oncol. 2013;52:1490–6.
Schwarz M, et al. Impact of geometrical uncertainties on 3D CRT and IMRT dose distributions for lung cancer treatment. Int J Radiat Oncol Biol Phys. 2006;65(4):1260–9.
Chapet O, et al. Potential benefits of using non coplanar field and intensity modulated radiation therapy to preserve the heart in irradiation of lung tumors in the middle and lower lobes. Radiother Oncol. 2006;80:333–40.
Jiang Z-Q, et al. Long-term clinical outcome of intensity-modulated radiotherapy for inoperable non-small cell lung cancer: the MD Anderson experience. Int J Radiat Oncol Biol Phys. 2012;83(1):332–9.
Uyterlinde W, Chen C, Sonke JJ, De Bois J, Belderbos J, Van Den Heuvel M. Vertebral fractures in NSCLC patients treated with IMRT and concurrent chemotherapy. World lung cancer 2013:O14.02.
Shirvani SM, et al. Intensity modulated radiotherapy for stage III non-small cell lung cancer in the United States: predictors of use and association with toxicities. Lung Cancer. 2013;82:252–9.
Perez CA, Bauer M, Edelstein S, Gillespie BW, Birch R. Impact of tumor control on survival in carcinoma of the lung treated with irradiation. Int J Radiat Oncol Biol Phys. 1986;12:539–47.
Bayman N, Blackhall F, McCloskey P, Taylor P, Faivre-Finn C. How can we optimise concurrent chemoradiotherapy for inoperable stage III non-small cell lung cancer? Lung Cancer. 2014;83:117–25.
Cox JD, et al. A randomized phase I/II trial of hyperfractionated radiation therapy with total doses of 60.0 Gy to 79.2 Gy: possible survival benefit with greater than or equal to 69.6 Gy in favorable patients with Radiation Therapy Oncology Group stage III non-small-cell lung carcinoma: report of Radiation Therapy Oncology Group 83–11. J Clin Oncol. 1990;8:1543–55.
Kong F-M, Zhao L, Hayman JA. The role of radiation therapy in thoracic tumors. Hematol Oncol Clin North Am. 2006;20:363–400.
Bellière A, et al. Feasibility of high-dose three-dimensional radiation therapy in the treatment of localised non-small-cell lung cancer. Cancer Radiother. 2009;13:298–304.
Sura S, Yorke E, Jackson A, Rosenzweig KE. High-dose radiotherapy for the treatment of inoperable non-small cell lung cancer. Cancer J. 2007;13:238–42.
Kong F-M, et al. High-dose radiation improved local tumor control and overall survival in patients with inoperable/unresectable non-small-cell lung cancer: long-term results of a radiation dose escalation study. Int J Radiat Oncol Biol Phys. 2005;63:324–33.
Rosenzweig KE, et al. Results of a phase I dose-escalation study using three-dimensional conformal radiotherapy in the treatment of inoperable nonsmall cell lung carcinoma. Cancer. 2005;103:2118–27.
Byhardt RW, et al. A phase I/II study to evaluate accelerated fractionation via concomitant boost for squamous, adeno, and large cell carcinoma of the lung: report of Radiation Therapy Oncology Group 84–07. Int J Radiat Oncol Biol Phys. 1993;26:459–68.
Salama JK, et al. Pulmonary toxicity in Stage III non-small cell lung cancer patients treated with high-dose (74 Gy) 3-dimensional conformal thoracic radiotherapy and concurrent chemotherapy following induction chemotherapy: a secondary analysis of Cancer and Leukemia Group B (CALGB) trial 30105. Int J Radiat Oncol Biol Phys. 2011;81:e269–74.
Hatton M, et al. Induction chemotherapy and continuous hyperfractionated accelerated radiotherapy (chart) for patients with locally advanced inoperable non-small-cell lung cancer: the MRC INCH randomized trial. Int J Radiat Oncol Biol Phys. 2011;81:712–8.
Komaki R, et al. Randomized phase II chemotherapy and radiotherapy trial for patients with locally advanced inoperable non-small-cell lung cancer: long-term follow-up of RTOG 92–04. Int J Radiat Oncol Biol Phys. 2002;53:548–57.
Rosenzweig KE, Sura S, Jackson A, Yorke E. Involved-field radiation therapy for inoperable non small-cell lung cancer. J Clin Oncol. 2007;25:5557–61.
Yuan S, et al. A randomized study of involved-field irradiation versus elective nodal irradiation in combination with concurrent chemotherapy for inoperable stage III nonsmall cell lung cancer. Am J Clin Oncol. 2007;30:239–44.
Emami B, et al. The impact of regional nodal radiotherapy (dose/volume) on regional progression and survival in unresectable non-small cell lung cancer: an analysis of RTOG data. Lung Cancer. 2003;41:207–14.
De Ruysscher D, Nestle U, Jeraj R, Macmanus M. PET scans in radiotherapy planning of lung cancer. Lung Cancer. 2012;75:141–5.
De Ruysscher D, et al. Effects of radiotherapy planning with a dedicated combined PET-CT-simulator of patients with non-small cell lung cancer on dose limiting normal tissues and radiation dose-escalation: a planning study. Radiother Oncol. 2005;77:5–10.
MacManus M, et al. Use of PET and PET/CT for radiation therapy planning: IAEA expert report 2006–2007. Radiother Oncol. 2009;91:85–94.
Mac Manus MP, et al. The use of fused PET/CT images for patient selection and radical radiotherapy target volume definition in patients with non-small cell lung cancer: results of a prospective study with mature survival data. Radiother Oncol. 2013;106:292–8.
Van Elmpt W, et al. Characterization of tumor heterogeneity using dynamic contrast enhanced CT and FDG-PET in non-small cell lung cancer. Radiother Oncol. 2013;109:65–70.
Geiger GA, et al. Stage migration in planning PET/CT scans in patients due to receive radiotherapy for non-small-cell lung cancer. Clin Lung Cancer. 2013. doi:10.1016/j.cllc.2013.08.004.
Zegers CML, et al. Hypoxia imaging with [18F]HX4 PET in NSCLC patients: defining optimal imaging parameters. Radiother Oncol. 2013;109:58–64.
Karam SD, et al. Dose escalation with stereotactic body radiation therapy boost for locally advanced non small cell lung cancer. Radiat Oncol. 2013;8:179.
Feddock J, et al. Stereotactic body radiation therapy can be used safely to boost residual disease in locally advanced non-small cell lung cancer: a prospective study. Int J Radiat Oncol Biol Phys. 2013;85:1325–31.
Udrescu C, Mornex F, Tanguy R, Chapet O. ExacTrac Snap Verification: a new tool for ensuring quality control for lung stereotactic body radiation therapy. Int J Radiat Oncol Biol Phys. 2013;85:e89–94.
Scagliotti GV, et al. Phase III study comparing cisplatin plus gemcitabine with cisplatin plus pemetrexed in chemotherapy-naive patients with advanced-stage non-small-cell lung cancer. J Clin Oncol. 2008;26(21):3543–51.
Bischof M, Weber K-J, Blatter J, Wannenmacher M, Latz D. Interaction of pemetrexed disodium (ALIMTA, multitargetedantifolate) and irradiation in vitro. Int J Radiat Oncol Biol Phys. 2002;52:1381–8.
Cardenal F, et al. Phase I study of concurrent chemoradiation with pemetrexed and cisplatin followed by consolidation pemetrexed for patients with unresectable stage III non-small cell lung cancer. Lung Cancer. 2011;74:69–74.
Mornex F. Pemetrexed (PEM) and Cisplatin (CIS) in concurrent combination with high dose of thoracic Radiation (RT), after induction Chemotherapy (CT), in patients (PTS) with locally advanced Non-Small Cell Lung Cancer (NSCLC): a phase I study. Int J Radiat Oncol Biol Phys. 2010;78(3):S501–2.
Seiwert TY, et al. A phase I study of pemetrexed, carboplatin, and concurrent radiotherapy in patients with locally advanced or metastatic non-small cell lung or esophageal cancer. Clin Cancer Res. 2007;13:515–22.
Choy H, et al. Phase 2 study of pemetrexed plus carboplatin, or pemetrexed plus cisplatin with concurrent radiation therapy followed by pemetrexed consolidation in patients with favorable-prognosis inoperable stage IIIA/B non-small-cell lung cancer. J Thorac Oncol. 2013;8:1308–16.
Govindan R, et al. Randomized phase II study of pemetrexed, carboplatin, and thoracic radiation with or without cetuximab in patients with locally advanced unresectable non-small-cell lung cancer: Cancer and Leukemia Group B trial 30407. J Clin Oncol. 2011;29:3120–5.
Vokes EE, Senan S, Treat JA, Iscoe NA. PROCLAIM: a phase III study of pemetrexed, cisplatin, and radiation therapy followed by consolidation pemetrexed versus etoposide, cisplatin, and radiation therapy followed by consolidation cytotoxic chemotherapy of choice in locally advanced stage III non-small-cell lung cancer of other than predominantly squamous cell histology. Clin Lung Cancer. 2009;10:193–8.
Tredaniel J, et al. A phase II study of cetuximab, pemetrexed, cisplatin, and concurrent radiotherapy in patients with locally advanced, unresectable, stage III, non squamous, non-small cell lung cancer (NSCLC). Rev Mal Respir. 2011;28:51–7.
Pirker R, et al. Cetuximab plus chemotherapy in patients with advanced non-small-cell lung cancer (FLEX): an open-label randomised phase III trial. Lancet. 2009;373:1525–31.
Mak RH, et al. Outcomes after combined modality therapy for EGFR-mutant and wild-type locally advanced NSCLC. Oncologist. 2011;16:886–95.
Chinnaiyan P, et al. Mechanisms of enhanced radiation response following epidermal growth factor receptor signaling inhibition by erlotinib (Tarceva). Cancer Res. 2005;65:3328–35.
Choong NW, et al. Phase I trial of erlotinib-based multimodality therapy for inoperable stage III non-small cell lung cancer. J Thorac Oncol. 2008;3:1003–11.
Rothschild S, et al. Gefitinib in combination with irradiation with or without cisplatin in patients with inoperable stage III non-small cell lung cancer: a phase I trial. Int J Radiat Oncol Biol Phys. 2011;80:126–32.
Kelly K, et al. Phase III trial of maintenance gefitinib or placebo after concurrent chemoradiotherapy and docetaxel consolidation in inoperable stage III non-small-cell lung cancer: SWOG S0023. J Clin Oncol. 2008;26:2450–6.
Komaki R, et al. Phase II trial of erlotinib and radiotherapy following chemoradiotherapy for patients with stage III non-small cell lung cancer. ASCO Meet abstract. 2011. 29:7020.
Ready N, et al. Chemoradiotherapy and gefitinib in stage III non-small cell lung cancer with epidermal growth factor receptor and KRAS mutation analysis: cancer and leukemia group B (CALEB) 30106, a CALGB-stratified phase II trial. J Thorac Oncol. 2010;5:1382–90.
Stinchcombe TE, et al. Induction chemotherapy with carboplatin, irinotecan, and paclitaxel followed by high dose three-dimension conformal thoracic radiotherapy (74 Gy) with concurrent carboplatin, paclitaxel, and gefitinib in unresectable stage IIIA and stage IIIB non-small cell lung cancer. J Thorac Oncol. 2008;3:250–7.
Goss GD, et al. Gefitinib versus placebo in completely resected non-small-cell lung cancer: results of the NCIC CTG BR19 study. J Clin Oncol. 2013;31:3320–6.
Lynch TJ, et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N Engl J Med. 2004;350:2129–39.
Maemondo M, et al. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med. 2010;362:2380–8.
Mitsudomi T, et al. Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. Lancet Oncol. 2010;11:121–8.
Zhou C, et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol. 2011;12:735–42.
Rosell R, et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2012;13:239–46.
Yang JC-H, et al. Afatinib for patients with lung adenocarcinoma and epidermal growth factor receptor mutations (LUX-Lung 2): a phase 2 trial. Lancet Oncol. 2012;13:539–48.
Sequist LV, et al. Phase III study of afatinib or cisplatin plus pemetrexed in patients with metastatic lung adenocarcinoma with EGFR mutations. J Clin Oncol. 2013;31:3327–34.
Wu Y-L, et al. Afatinib versus cisplatin plus gemcitabine for first-line treatment of Asian patients with advanced non-small-cell lung cancer harbouring EGFR mutations (LUX-Lung 6): an open-label, randomised phase 3 trial. Lancet Oncol. 2014;15:213–22.
Shaw AT, et al. Crizotinib versus chemotherapy in advanced ALK-positive lung cancer. N Engl J Med. 2013;368:2385–94.
Kwak EL, et al. Anaplastic lymphoma kinase inhibition in non-small-cell lung cancer. N Engl J Med. 2010;363:1693–703.
Gan GN, et al. Stereotactic radiation therapy can safely and durably control sites of extra-central nervous system oligoprogressive disease in anaplastic lymphoma kinase-positive lung cancer patients receiving crizotinib. Int J Radiat Oncol Biol Phys. 2014. doi:10.1016/j.ijrobp.2013.11.010.
Weickhardt AJ, et al. Local ablative therapy of oligoprogressive disease prolongs disease control by tyrosine kinase inhibitors in oncogene-addicted non-small-cell lung cancer. J Thorac Oncol. 2012;7:1807–14.
Sandler A, et al. Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med. 2006;355:2542–50.
Reck M, et al. Phase III trial of cisplatin plus gemcitabine with either placebo or bevacizumab as first-line therapy for nonsquamous non-small-cell lung cancer: AVAil. J Clin Oncol. 2009;27:1227–34.
Spigel DR, et al. Tracheoesophageal fistula formation in patients with lung cancer treated with chemoradiation and bevacizumab. J Clin Oncol. 2010;28:43–8.
Stinchcombe T, et al. Phase I/II trial of bevacizumab (B) and erlotinib (E) with induction (IND) and concurrent (CON) carboplatin (Cb)/paclitaxel (P) and 74 Gy of thoracic conformal radiotherapy (TCRT) in stage III non-small cell lung cancer (NSCLC). ASCO Meet Abstr. 2011;29:7016.
Hoang T, et al. Randomized phase III study of thoracic radiation in combination with paclitaxel and carboplatin with or without thalidomide in patients with stage III non-small-cell lung cancer: the ECOG 3598 study. J Clin Oncol. 2012;30:616–22.
Lu C, et al. Chemoradiotherapy with or without AE-941 in stage III non-small cell lung cancer: a randomized phase III trial. J Natl Cancer Inst. 2010;102:859–65.
Choy H, et al. Phase II multicenter study of induction chemotherapy followed by concurrent efaproxiral (RSR13) and thoracic radiotherapy for patients with locally advanced non-small-cell lung cancer. J Clin Oncol. 2005;23:5918–28.
Butts C, et al. A multi-centre phase IIB randomized controlled study of BLP25 liposome vaccine (L-BLP25 or Stimuvax) for active specific immunotherapy of non-small cell lung cancer (NSCLC): updated survival analysis: B1-01. J Thorac Oncol. 2007;2:S332–3.
Brunsvig PF, et al. Telomerase peptide vaccination in NSCLC: a phase II trial in stage III patients vaccinated after chemoradiotherapy and an 8-year update on a phase I/II trial. Clin Cancer Res. 2011;17:6847–57.
Lopez Guerra JL, et al. Changes in pulmonary function after three-dimensional conformal radiotherapy, intensity-modulated radiotherapy, or proton beam therapy for non-small-cell lung cancer. Int J Radiat Oncol Biol Phys. 2012;83:e537–43.
Sejpal S, et al. Early findings on toxicity of proton beam therapy with concurrent chemotherapy for nonsmall cell lung cancer. Cancer. 2011;117:3004–13.
Park K, Ahn YC, Ahn JS, et al. A multinational phase III randomized trial with or without consolidation chemotherapy using docetaxel and cisplatin after concurrent chemoradiation in inoperable stage III non-small cell lung cancer. J Clin Oncol 32:5s, 2014 (suppl; abstr 7500).
Huber RM, Engel-Riedel W, Kollmeier J, et al. GILT study: Oral vinorelbine (NVBo) and cisplatin (P) with concomitant radiotherapy (RT) followed by either consolidation (C) with NVBo plus P plus best supportive care (BSC) or BSC alone in stage (st) III non-small cell lung cancer (NSCLC): Final results of a phase (ph) III study. J Clin Oncol 30, 2012 (suppl; abstr 7001).
Bradley JD, Paulus R, Komaki R, et al. Randomized phase III comparison of standard-dose (60 Gy) versus high-dose (74 Gy) conformal chemoradiotherapy ± cetuximab for stage IIIA/IIIB non-small cell lung cancer: Preliminary findings on radiation dose in RTOG 0617. Abstract LBA2. 53rd ASTRO Annual Meeting, 2011.
Bradley JD, Paulus R, Komaki R, et al. A randomized phase III comparison of standard-dose (60 Gy) versus high-dose (74 Gy) conformal chemoradiotherapy with or without cetuximab for stage III non-small cell lung cancer: Results on radiation dose in RTOG 0617. J Clin Oncol 31, 2013 (suppl; abstr 7501).
Vokes E, Wang L, Vansteenkiste J, et al. Preliminary Safety and Treatment Delivery Data During Concurrent Phase of Chemoradiation Therapy of the PROCLAIM Trial: A Phase 3 Trial of Pemetrexed, Cisplatin, and Radiotherapy Followed by Consolidation Pemetrexed Versus Etoposide, Cisplatin, and Radiotherapy Followed by Consolidation Cytotoxic Chemotherapy of Choice in Patients With Stage III Nonsquamous Cell Lung Cancer. J Thor Oncol 8, 2013 ( suppl 2; abstr P1.09–009).
Mok T, Kim DW, Wu YL, et al. First-line crizotinib versus pemetrexed–cisplatin or pemetrexed–carboplatin in patients (pts) with advanced ALK-positive non-squamous non-small cell lung cancer (NSCLC): results of a phase III study (PROFILE 1014). J Clin Oncol 32:5s, 2014 (suppl; abstr 8002).
Butts CA, Socinski MA, Mitchell P, et al. START: A phase III study of L-BLP25 cancer immunotherapy for unresectable stage III non-small cell lung cancer. J Clin Oncol 31, 2013 (suppl; abstr 7500).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Thariat, J., Lapierre, A., Früh, M., Mornex, F. (2015). Advances in Radiotherapy for Locally Advanced NSCLC. In: Peters, S., Besse, B. (eds) New Therapeutic Strategies in Lung Cancers. Springer, Cham. https://doi.org/10.1007/978-3-319-06062-0_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-06062-0_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-06061-3
Online ISBN: 978-3-319-06062-0
eBook Packages: MedicineMedicine (R0)