Abstract
Although echocardiography remains a primary tool in diagnostic assessment, other techniques, such as cardiac magnetic resonance (CMR) and positron emission tomography (PET), have become extremely important in the general evaluation of hypertrophic cardiomyopathy (HCM). In particular, CMR overcomes technical limitations of echocardiography and offers important information on myocardial fibrosis in a disease in which its identification could be important, especially from a prognostic standpoint. Moreover, CMR is the gold standard for evaluating left ventricular (LV) size and mass. PET gives important information about microvascular dysfunction, which is believed to be impaired in HCM and may have have an important role on treatment and prognostic stratification. In conclusion, HCM is a complex disease that deserves a multiparametric assessment in order to establish an accurate diagnosis and to understand the many pathophysiologic and morphologic features that characterize the disease.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Positron Emission Tomography
- Single Photon Emission Compute Tomography
- Cardiac Magnetic Resonance
- Right Ventricle
- Late Gadolinium Enhancement
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Echocardiography has a primary role in diagnostic assessment of HCM, but other techniques, such as cardiac magnetic resonance (CMR) and positron emission tomography (PET), recently became extremely important and helpful in the general evaluation of the disease and their use is now extremely widespread especially at referral centers.
2 Cardiac Magnetic Resonance
If echocardiography has a main role in the diagnosis and prognostic assessment of hypertrophic cardiomyopathy (HCM), in many clinical scenarios, technical limitations and heterogeneous phenotypic expression make such evaluation difficult, and cardiac magnetic resonance (CMR) has emerged as a useful imaging modality to complement routine transthoracic echocardiography [1, 2]. CMR offers not only high spatial resolution and complete 3D coverage of the entire heart but can also allow visualization of myocardial scarring in vivo using late gadolinium enhancement (LGE). Therefore, in many cardiomyopathy (CMP) reference centers, CMR has become a routinely used imaging tool in patients with HCM and it is indicated for establishing the diagnosis in patients with a suspicion of the disease but with no clear diagnostic elements arising from the use of other diagnostic tests [3].
2.1 Diagnostic Value
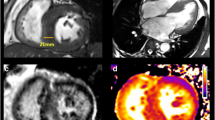
CMR is considered the gold standard for evaluating the complex chamber morphology and function (Fig. 12.1), as well as the heterogeneous distribution of hypertrophy found in HCM patients. In addition, CMR is the best method available to assess the papillary muscle and mitral valve abnormalities, perfusion abnormalities, and fibrosis with LGE [4]. Furthermore, when dealing with left ventricular (LV) obstruction, CMR can characterize the underlying mechanisms, such as MV anatomy, septal systolic anterior motion contact, and subvalvular apparatus [5–7]. Isolated or concomitant midventricular obstruction related to midventricular hypertrophy is also readily demonstrated. CMR is advantageous in identifying the presence and various distribution of LV hypertrophy, particularly when regions of increased wall thickness are focal, such as the anterior free wall, posterior septum, and apex, and they are not well visualized by echocardiography [8].
Cardiac magnetic resonance (CMR) of a 35-year-old man with hypertrophic cardiomyopathy (HCM) showing severe asymmetric hypertrophy (maximal wall thickness at the basal septum is 27 mm) and left ventricular outflow tract (LV OT) obstruction. End-diastolic 4 chamber view (a); end-diastolic 2 chamber view (b); end-diastolic 3 chamber view (c); end-diastolic short-axis view
The distribution of hypertrophy and distortion of septal anatomy is different among patients with a clinical diagnosis of HCM made later in life compared with younger patients. HCM morphology can be classified into five main subtypes: sigmoid, reverse curve, apical, symmetric, and neutral (Fig. 12.2) [9, 10]. LV apical aneurysms could also be present in HCM and are frequently associated with a midventricular obstruction. They can be a substrate for life-threatening arrhythmias and location of intraventricular thrombi. Echocardiography is not always helpful in their visualization and Contrast-enhanced CMR demonstrates that they are composed predominantly of fibrosis [11].
CMR is also helpful in defining the degree of hypertrophy, which in some cases is massive (Fig. 12.3), and of LV mass, overcoming the limitations of echocardiography [12]. As demonstrated by Olivotto et al. [13], LV mass index in HCM patients significantly exceeds that of control individuals. Interestingly, LV mass index assessed by CMR showed only a modest relationship to maximal LV thickness assessed at echocardiography.
The right ventricle (RV) is often not well visualized by echocardiography, whereas CMR provides optimal assessment of RV volume, systolic function, and wall thickness. According to Maron et al. [14], significant RV hypertrophy (end-diastolic RV free wall thickness ≥8 mm) could be demonstrated by CMR in more than one third of HCM patients. In a substantial proportion of patients, RV wall mass is also increased.
Microvascular dysfunction and subsequent ischemia may be present in HCM. As demonstrated by Petersen et al. [15], although resting myocardial blood flow is similar in HCM patients and healthy controls, during hyperemia, it is significantly lower in patients. In addition, this decrease in coronary reserve is related to the extent of LV hypertrophy.
2.2 Role in Differential Diagnosis
CMR is helpful in the differential diagnosis between HCM and other pathologic conditions characterized by LV hypertrophy. In particular, hypertrophy pattern and LGE distribution—although heterogeneous in HCM—are often distinctive in other diseases mimicking HCM, such as some infiltrative/storage CMP [15–17] (Chap. 27).
2.3 Genotype-Positive/Phenotype-Negative Individuals
CMR plays a role in assessing a particular patient subgroup within the HCM disease spectrum, i.e., genetically affected family members without clinical or morphologic evidence of disease. In this setting, CMR can recognize subtle abnormalities usually not detected by echocardiography [16]. One feature described in this subset of patients is the presence of myocardial crypts, characterized by small invaginations inside the myocardium [17] (Fig. 12.4). Another morphological characteristic observed to be different in comparison with a healthy control population is the presence of longer mitral leaflets [6]. Interestingly, the MV is often abnormal in patients with HCM, and it is possible that abnormalities in its structure could be a primary feature linked to genetic mutation(s) [18]. Valente et al. [19] analyzed 40 genotype-positive/phenotype-negative patients using echocardiography and CMR and found a quite good diagnostic agreement, although CMR measurements of LV wall thickness were 19 % lower than echo, and 10 % of cases had LV hypertrophy appreciated only by CMR.
2.4 Assessment of Myocardial Fibrosis
Images acquired following the injection of gadolinium can help in detecting fibrosis in HCM, as in other heart diseases. The presence of myocardial fibrosis can be observed frequently in HCM hearts, and its presence is believed to be a pathological substrate for cardiac arrhythmias (Fig. 12.5).
Different late gadolinium enhancement (LGE) patterns in hypertrophic cardiomyopathy (HCM). Patchy septal LGE (a) in a patient with severe asymmetric hypertrophy. Anterior and circumferential LGE in a patient with systolic obliteration (b). Apical LGE in apical HCM (c). Insertion point LGE (d) in a patient with mild hypertrophy
In the seminal study by Choudhury et al. [20], myocardial scarring visualized by LGE was a common finding in asymptomatic or mildly symptomatic HCM patients (81 %). Also, Moon et al. [21] described a high prevalence of LGE in patients with HCM (79 %). During follow-up, the extent of scar visualized by CMR was associated with progressive ventricular dilation and clinical markers of sudden death (SD). Adabag et al. [22] found that myocardial fibrosis assessed using LGE was associated with greater likelihood and increased frequency of ventricular tachyarrhythmias on ambulatory Holter electrocardiography (ECG). LGE was distributed in different patterns (most commonly within the interventricular septum or in the areas of most extensive hypertrophy) [23]. Extensive LGE was observed in end-stage HCM with significant systolic LV dysfunction. In general, LGE correlates with LV wall thickening and inversely correlates with LV ejection fraction (EF) [24].
Novel techniques for quantifying myocardial extracellular volume, such as T1 mapping, may be promising, particularly for assessing diffuse myocardial interstitial fibrosis in HCM [25]. To date, the roles of these techniques, especially concerning prognostic stratification or relationship with other features such as ventricular arrhythmias, remain undefined.
There is debate around whether genotype-positive/phenotype-negative HCM patients have myocardial fibrosis. Even if some case reports describe the presence of LGE in this condition [26, 27], there is a lack of data on this specific patient population. Moreover, it is possible that these patients may have subtle myocardial fibrosis not detected by LGE. Patients without overt LV hypertrophy and a genetic mutation have a higher myocardial extracellular volume expansion when assessed measuring T1 times pre- and postgadolinium infusion [28].
3 Single-Photon-Emission Computed Tomography
Single photon emission computed tomography (SPECT) with thallium-201 radiochemical thallium chloride [201Tl] demonstrates perfusion abnormalities in patients with HCM [29–31]. Abnormal stress myocardial perfusion imaging identifies HCM patients at increased risk of syncope, LV dilatation, reduced exercise capacity, sudden cardiac arrest, and cardiovascular death [31–33]. A possible exception may be found in patients with apical HCM, who seem to maintain a benign prognosis despite the presence of reversible thallium defects [34]. Abnormalities in regional myocardial perfusion, in addition to regional hypertrophy, contribute to early regional diastolic dysfunction in patients with HCM [35].
Fixed 201Tl perfusion defects, possibly representing fibrosis, detected during dipyridamole stress test in patients with HCM are associated with syncope, larger LV cavity dimensions, and reduced exercise capacity [36]. Reduced 201Tl washout was strongly associated with exertional chest pain in HCM patients and was observed in myocardial regions with normal as well as increased thickness [37]. Myocardial perfusion was used to demonstrate the beneficial effects of pharmacologic therapy [29, 30] or surgical or transcatheter septal ablation [38, 39]. Regional fatty acid metabolism abnormalities were demonstrated with 201Tl SPECT and [123]I-beta-methyl-p-iodophenylpentadecanoic acid (123I-BMIPP) mismatch in HCM patients [40–42]. These abnormalities seem to occur before reduction of oxidative metabolism, measured by [18F]-fluorodeoxyglucose (FDG) and 11C-acetate positron emission tomography (PET), in patients with HCM [43]. Studies evaluating the role of regional myocardial sympathetic nerve activity with 123I-metaiodobenzylguanidine (MIBG) suggest sympathetic dysinnervation in patients with HCM [44, 45]. Cardiac sympathetic nervous activity was related to degree of hypertrophy, systolic and diastolic function, and ventricular arrhythmias [46, 47].
4 Positron Emission Tomography
The usefulness of PET in patients with HCM was first reported by Grover-McKay et al. [48]. These authors demonstrated that the hypertrophied septum of patients with HCM is viable and not ischemic at rest, as it exhibits normal uptake of the fatty acid tracer 11C-palmitate and normal or only mildly reduced myocardial perfusion. However, it is metabolically different from normal myocardium, as it fails to take up the glucose analog [18F]-FDG despite normal uptake in the rest of the myocardium. Later studies confirmed this finding and demonstrated heterogeneity of [18F]-FDG uptake in hypertrophied segments, possibly reflecting a metabolic abnormality [49]. This heterogeneity was suggested to be related to regional systolic function [50] and was increased in patients with HCM diagnosed at a young age compared with patients diagnosed at middle to old age [51].
Studies using PET with [13N]-ammonia or [15O]-water to assess myocardial blood flow demonstrate that patients with HCM have a blunted response to the vasodilators dipyridamole and adenosine compared with normal controls or patients with secondary hypertrophy, thus suggesting microvascular dysfunction [52–56]. A direct increase in the number of cardiovascular events, including unfavorable LV remodeling, progressive HF, ventricular tachyarrhythmias, and death, was found with increasing coronary reserve impairment [54, 56]. A relationship between LGE CMR and heterogeneous resting myocardial blood flow [57] or microvascular function studied by stress PET were found [58]. Studies with 11C-12177 (CGP) or 11C-hydroxyephedrine (HED) PET demonstrated the presence of cardiac sympathetic dysinnervation: reduced β-adrenergic receptor density with reduced norepinephrine reuptake by presynaptic terminals [59, 60]. These abnormalities seem to be particularly prominent in patients with HF [61].
5 Computed Tomography
Cardiac CT has the advantage of clearly delineating the myocardium, thus providing detailed characterization of the HCM phenotype, including accurate wall thickness measurements, and highly reproducible measurements of ventricular volumes, EF, and mass [62, 63]. In addition, it permits simultaneous imaging of coronary arteries, RV and LV volume and mass, and global and regional function [64, 65]. However, this imaging method was not extensively studied in HCM patients and thus is useful only in selected clinical scenarios, following suboptimal echocardiographic images when CMR is contraindicated, or to exclude concomitant coronary disease (Table12.1).
6 Conclusion
Various imaging techniques contribute to the general assessment of HCM. EAch of them has stength and weakness (Table12.1) and a multiparametric evaluation is pivotal in this setting.
References
Lima JA, Desai MY (2004) Cardiovascular magnetic resonance imaging: current and emerging applications. J Am Coll Cardiol 44(6):1164–1171. doi:10.1016/j.jacc.2004.06.033
Reichek N, Gupta D (2008) Hypertrophic cardiomyopathy: cardiac magnetic resonance imaging changes the paradigm. J Am Coll Cardiol 52(7):567–568. doi:10.1016/j.jacc.2008.05.014
Moon JC, McKenna WJ (2009) The emerging role of cardiovascular magnetic resonance in refining the diagnosis of hypertrophic cardiomyopathy. Nat Clin Pract Cardiovasc Med 6(3):166–167. doi:10.1038/ncpcardio1442
Nagueh SF, Bierig SM, Budoff MJ, Desai M, Dilsizian V, Eidem B, Goldstein SA, Hung J, Maron MS, Ommen SR, Woo A (2011) American Society of Echocardiography clinical recommendations for multimodality cardiovascular imaging of patients with hypertrophic cardiomyopathy: Endorsed by the American Society of Nuclear Cardiology, Society for Cardiovascular Magnetic Resonance, and Society of Cardiovascular Computed Tomography. J Am Soc Echocardiogr 24(5):473–498. doi:10.1016/j.echo.2011.03.006
Kwon DH, Setser RM, Thamilarasan M, Popovic ZV, Smedira NG, Schoenhagen P, Garcia MJ, Lever HM, Desai MY (2008) Abnormal papillary muscle morphology is independently associated with increased left ventricular outflow tract obstruction in hypertrophic cardiomyopathy. Heart 94(10):1295–1301. doi:10.1136/hrt.2007.118018
Maron MS, Olivotto I, Harrigan C, Appelbaum E, Gibson CM, Lesser JR, Haas TS, Udelson JE, Manning WJ, Maron BJ (2011) Mitral valve abnormalities identified by cardiovascular magnetic resonance represent a primary phenotypic expression of hypertrophic cardiomyopathy. Circulation 124(1):40–47. doi:10.1161/CIRCULATIONAHA.110.985812
Harrigan CJ, Appelbaum E, Maron BJ, Buros JL, Gibson CM, Lesser JR, Udelson JE, Manning WJ, Maron MS (2008) Significance of papillary muscle abnormalities identified by cardiovascular magnetic resonance in hypertrophic cardiomyopathy. Am J Cardiol 101(5):668–673. doi:10.1016/j.amjcard.2007.10.032
Rickers C, Wilke NM, Jerosch-Herold M, Casey SA, Panse P, Panse N, Weil J, Zenovich AG, Maron BJ (2005) Utility of cardiac magnetic resonance imaging in the diagnosis of hypertrophic cardiomyopathy. Circulation 112(6):855–861. doi:10.1161/CIRCULATIONAHA.104.507723
Binder J, Ommen SR, Gersh BJ, Van Driest SL, Tajik AJ, Nishimura RA, Ackerman MJ (2006) Echocardiography-guided genetic testing in hypertrophic cardiomyopathy: septal morphological features predict the presence of myofilament mutations. Mayo Clin Proc 81(4):459–467. doi:10.4065/81.4.459
Bos JM, Theis JL, Tajik AJ, Gersh BJ, Ommen SR, Ackerman MJ (2008) Relationship between sex, shape, and substrate in hypertrophic cardiomyopathy. Am Heart J 155(6):1128–1134. doi:10.1016/j.ahj.2008.01.005
Holloway CJ, Betts TR, Neubauer S, Myerson SG (2010) Hypertrophic cardiomyopathy complicated by large apical aneurysm and thrombus, presenting as ventricular tachycardia. J Am Coll Cardiol 56(23):1961. doi:10.1016/j.jacc.2010.01.078
Armstrong AC, Gidding S, Gjesdal O, Wu C, Bluemke DA, Lima JA (2012) LV mass assessed by echocardiography and CMR, cardiovascular outcomes, and medical practice. JACC Cardiovasc Imaging 5(8):837–848. doi:10.1016/j.jcmg.2012.06.003
Olivotto I, Maron MS, Autore C, Lesser JR, Rega L, Casolo G, De Santis M, Quarta G, Nistri S, Cecchi F, Salton CJ, Udelson JE, Manning WJ, Maron BJ (2008) Assessment and significance of left ventricular mass by cardiovascular magnetic resonance in hypertrophic cardiomyopathy. J Am Coll Cardiol 52(7):559–566. doi:10.1016/j.jacc.2008.04.047
Maron MS, Hauser TH, Dubrow E, Horst TA, Kissinger KV, Udelson JE, Manning WJ (2007) Right ventricular involvement in hypertrophic cardiomyopathy. Am J Cardiol 100(8):1293–1298. doi:10.1016/j.amjcard.2007.05.061
Petersen SE, Jerosch-Herold M, Hudsmith LE, Robson MD, Francis JM, Doll HA, Selvanayagam JB, Neubauer S, Watkins H (2007) Evidence for microvascular dysfunction in hypertrophic cardiomyopathy: new insights from multiparametric magnetic resonance imaging. Circulation 115(18):2418–2425. doi:10.1161/CIRCULATIONAHA.106.657023
Germans T, Russel IK, Gotte MJ, Spreeuwenberg MD, Doevendans PA, Pinto YM, van der Geest RJ, van der Velden J, Wilde AA, van Rossum AC (2010) How do hypertrophic cardiomyopathy mutations affect myocardial function in carriers with normal wall thickness? Assessment with cardiovascular magnetic resonance. J Cardiovasc Magn Reson 12:13. doi:10.1186/1532-429X-12-13
Maron MS, Rowin EJ, Lin D, Appelbaum E, Chan RH, Gibson CM, Lesser JR, Lindberg J, Haas TS, Udelson JE, Manning WJ, Maron BJ (2012) Prevalence and clinical profile of myocardial crypts in hypertrophic cardiomyopathy. Circ Cardiovasc Imaging 5(4):441–447. doi:10.1161/CIRCIMAGING.112.972760
Woo A, Jedrzkiewicz S (2011) The mitral valve in hypertrophic cardiomyopathy: it’s a long story. Circulation 124(1):9–12. doi:10.1161/CIRCULATIONAHA.111.035568
Valente AM, Lakdawala NK, Powell AJ, Evans SP, Cirino AL, Orav EJ, MacRae CA, Colan SD, Ho CY (2013) Comparison of echocardiographic and cardiac magnetic resonance imaging in hypertrophic cardiomyopathy sarcomere mutation carriers without left ventricular hypertrophy. Circ Cardiovasc Genet 6(3):230–237. doi:10.1161/CIRCGENETICS.113.000037
Choudhury L, Mahrholdt H, Wagner A, Choi KM, Elliott MD, Klocke FJ, Bonow RO, Judd RM, Kim RJ (2002) Myocardial scarring in asymptomatic or mildly symptomatic patients with hypertrophic cardiomyopathy. J Am Coll Cardiol 40(12):2156–2164
Moon JC, McKenna WJ, McCrohon JA, Elliott PM, Smith GC, Pennell DJ (2003) Toward clinical risk assessment in hypertrophic cardiomyopathy with gadolinium cardiovascular magnetic resonance. J Am Coll Cardiol 41(9):1561–1567
Adabag AS, Maron BJ, Appelbaum E, Harrigan CJ, Buros JL, Gibson CM, Lesser JR, Hanna CA, Udelson JE, Manning WJ, Maron MS (2008) Occurrence and frequency of arrhythmias in hypertrophic cardiomyopathy in relation to delayed enhancement on cardiovascular magnetic resonance. J Am Coll Cardiol 51(14):1369–1374. doi:10.1016/j.jacc.2007.11.071
Maron MS, Appelbaum E, Harrigan CJ, Buros J, Gibson CM, Hanna C, Lesser JR, Udelson JE, Manning WJ, Maron BJ (2008) Clinical profile and significance of delayed enhancement in hypertrophic cardiomyopathy. Circ Heart Fail 1(3):184–191. doi:10.1161/CIRCHEARTFAILURE.108.768119
Maron MS (2012) Clinical utility of cardiovascular magnetic resonance in hypertrophic cardiomyopathy. J Cardiovasc Magn Reson 14:13. doi:10.1186/1532-429X-14-13
Sado DM, White SK, Piechnik SK, Banypersad SM, Treibel T, Captur G, Fontana M, Maestrini V, Flett AS, Robson MD, Lachmann RH, Murphy E, Mehta A, Hughes D, Neubauer S, Elliott PM, Moon JC (2013) Identification and assessment of Anderson-Fabry disease by cardiovascular magnetic resonance noncontrast myocardial T1 mapping. Circ Cardiovasc Imaging 6(3):392–398. doi:10.1161/CIRCIMAGING.112.000070
Rowin EJ, Maron MS, Lesser JR, Maron BJ (2012) CMR with late gadolinium enhancement in genotype positive-phenotype negative hypertrophic cardiomyopathy. JACC Cardiovasc Imaging 5(1):119–122. doi:10.1016/j.jcmg.2011.08.020
Strijack B, Ariyarajah V, Soni R, Jassal DS, Greenberg CR, McGregor R, Morris A (2008) Late gadolinium enhancement cardiovascular magnetic resonance in genotyped hypertrophic cardiomyopathy with normal phenotype. J Cardiovasc Magn Reson 10:58. doi:10.1186/1532-429X-10-58
Funabashi N, Takaoka H, Horie S, Ozawa K, Daimon M, Takahashi M, Yajima R, Saito M, Fujiwara K, Tani A, Kamata T, Uehara M, Kataoka A, Kobayashi Y (2013) Regional peak longitudinal-strain by 2D speckle-tracking TTE provides useful information to distinguish fibrotic from non-fibrotic lesions in LV myocardium on cardiac MR in hypertrophic cardiomyopathy. Int J Cardiol 168(4):4520–4523. doi:10.1016/j.ijcard.2013.06.105
Sugihara H, Taniguchi Y, Ohtsuki K, Umamoto I, Nakazawa T, Shima T, Nakamura T, Azuma A, Kohno Y, Nakagawa M (1993) Assessment of myocardial perfusion abnormalities in patients with apical hypertrophic cardiomyopathy using exercise 201Tl scintigraphy. Kokyu To Junkan 41(11):1089–1093
Taniguchi Y, Sugihara H, Ohtsuki K, Umamoto I, Nakagawa T, Shiga K, Nakamura T, Azuma A, Kohno Y, Nakagawa M et al (1994) Effect of verapamil on myocardial ischemia in patients with hypertrophic cardiomyopathy: evaluation by exercise thallium-201 SPECT. J Cardiol 24(1):45–51
Dilsizian V, Bonow RO, Epstein SE, Fananapazir L (1993) Myocardial ischemia detected by thallium scintigraphy is frequently related to cardiac arrest and syncope in young patients with hypertrophic cardiomyopathy. J Am Coll Cardiol 22(3):796–804
Sorajja P, Chareonthaitawee P, Ommen SR, Miller TD, Hodge DO, Gibbons RJ (2006) Prognostic utility of single-photon emission computed tomography in adult patients with hypertrophic cardiomyopathy. Am Heart J 151(2):426–435. doi:10.1016/j.ahj.2005.02.050
Kaimoto S, Kawasaki T, Kuribayashi T, Yamano M, Miki S, Kamitani T, Matsubara H (2012) Myocardial perfusion abnormality in the area of ventricular septum-free wall junction and cardiovascular events in nonobstructive hypertrophic cardiomyopathy. Int J Cardiovasc Imaging 28(7):1829–1839. doi:10.1007/s10554-011-9994-z
Lee KH, Jang HJ, Lee SC, Kim YH, Lee EJ, Seo JD, Kim BT (2003) Myocardial thallium defects in apical hypertrophic cardiomyopathy are associated with a benign prognosis. Thallium defects in apical hypertrophy. Int J Cardiovasc Imaging 19(5):381–388
Yamanari H, Kakishita M, Fujimoto Y, Hashimoto K, Kiyooka T, Katayama Y, Otsuka F, Emori T, Uchida S, Ohe T (1997) Effect of regional myocardial perfusion abnormalities on regional myocardial early diastolic function in patients with hypertrophic cardiomyopathy. Heart Vessels 12(4):192–198
Yamada M, Elliott PM, Kaski JC, Prasad K, Gane JN, Lowe CM, Doi Y, McKenna WJ (1998) Dipyridamole stress thallium-201 perfusion abnormalities in patients with hypertrophic cardiomyopathy. Relationship to clinical presentation and outcome. Eur Heart J 19(3):500–507
Takata J, Counihan PJ, Gane JN, Doi Y, Chikamori T, Ozawa T, McKenna WJ (1993) Regional thallium-201 washout and myocardial hypertrophy in hypertrophic cardiomyopathy and its relation to exertional chest pain. Am J Cardiol 72(2):211–217
Cannon RO 3rd, Dilsizian V, O’Gara PT, Udelson JE, Tucker E, Panza JA, Fananapazir L, McIntosh CL, Wallace RB, Bonow RO (1992) Impact of surgical relief of outflow obstruction on thallium perfusion abnormalities in hypertrophic cardiomyopathy. Circulation 85(3):1039–1045
Lerch H, Schafers M, Gietzen F, Schafers K, Kuwert T, Kuhn H, Schober O (1997) Myocardial perfusion and metabolism after transcoronary ablation of septum hypertrophy (TASH) in hypertrophic obstructive cardiomyopathy. Nuklearmedizin 36(6):218–222
Ishida Y, Nagata S, Uehara T, Yasumura Y, Fukuchi K, Miyatake K (2001) Clinical analysis of myocardial perfusion and metabolism in patients with hypertrophic cardiomyopathy by single photon emission tomography and positron emission tomography. J Cardiol 37(Suppl 1):121–128
Ito Y, Hasegawa S, Yamaguchi H, Yoshioka J, Uehara T, Nishimura T (2000) Relation between thallium-201/iodine 123-BMIPP subtraction and fluorine 18 deoxyglucose polar maps in patients with hypertrophic cardiomyopathy. J Nucl Cardiol 7(1):16–22. doi:10.1067/mnc.2000.99188
Shimonagata T, Nishimura T, Uehara T, Hayashida K, Kumita S, Ohno A, Nagata S, Miyatake K (1993) Discrepancies between myocardial perfusion and free fatty acid metabolism in patients with hypertrophic cardiomyopathy. Nucl Med Commun 14(11):1005–1013
Tadamura E, Kudoh T, Hattori N, Inubushi M, Magata Y, Konishi J, Matsumori A, Nohara R, Sasayama S, Yoshibayashi M, Tamaki N (1998) Impairment of BMIPP uptake precedes abnormalities in oxygen and glucose metabolism in hypertrophic cardiomyopathy. J Nucl Med 39(3):390–396
Nakajima K, Bunko H, Taki J, Shimizu M, Muramori A, Hisada K (1990) Quantitative analysis of 123I-meta-iodobenzylguanidine (MIBG) uptake in hypertrophic cardiomyopathy. Am Heart J 119(6):1329–1337
Shimizu M, Sugihara N, Kita Y, Shimizu K, Horita Y, Nakajima K, Taki J, Takeda R (1992) Long-term course and cardiac sympathetic nerve activity in patients with hypertrophic cardiomyopathy. Br Heart J 67(2):155–160
Zhao C, Shuke N, Yamamoto W, Okizaki A, Sato J, Ishikawa Y, Ohta T, Hasebe N, Kikuchi K, Aburano T (2001) Comparison of cardiac sympathetic nervous function with left ventricular function and perfusion in cardiomyopathies by (123)I-MIBG SPECT and (99 m)Tc-tetrofosmin electrocardiographically gated SPECT. J Nucl Med 42(7):1017–1024
Terai H, Shimizu M, Ino H, Yamaguchi M, Hayashi K, Sakata K, Kiyama M, Hayashi T, Inoue M, Taki J, Mabuchi H (2003) Cardiac sympathetic nerve activity in patients with hypertrophic cardiomyopathy with malignant ventricular tachyarrhythmias. J Nucl Cardiol 10(3):304–310
Grover-McKay M, Schwaiger M, Krivokapich J, Perloff JK, Phelps ME, Schelbert HR (1989) Regional myocardial blood flow and metabolism at rest in mildly symptomatic patients with hypertrophic cardiomyopathy. J Am Coll Cardiol 13(2):317–324
Ishiwata S, Maruno H, Senda M, Toyama H, Nishiyama S, Seki A (1997) Myocardial blood flow and metabolism in patients with hypertrophic cardiomyopathy–a study with carbon-11 acetate and positron emission tomography. Jpn Circ J 61(3):201–210
Perrone-Filardi P, Bacharach SL, Dilsizian V, Panza JA, Maurea S, Bonow RO (1993) Regional systolic function, myocardial blood flow and glucose uptake at rest in hypertrophic cardiomyopathy. Am J Cardiol 72(2):199–204
Kagaya Y, Ishide N, Takeyama D, Kanno Y, Yamane Y, Shirato K, Maruyama Y, Itoh M, Ido T, Matsuzawa T et al (1992) Differences in myocardial fluoro-18 2-deoxyglucose uptake in young versus older patients with hypertrophic cardiomyopathy. Am J Cardiol 69(3):242–246
Camici P, Chiriatti G, Lorenzoni R, Bellina RC, Gistri R, Italiani G, Parodi O, Salvadori PA, Nista N, Papi L et al (1991) Coronary vasodilation is impaired in both hypertrophied and nonhypertrophied myocardium of patients with hypertrophic cardiomyopathy: a study with nitrogen-13 ammonia and positron emission tomography. J Am Coll Cardiol 17(4):879–886
Lorenzoni R, Gistri R, Cecchi F, Olivotto I, Chiriatti G, Elliott P, McKenna WJ, Camici PG (1998) Coronary vasodilator reserve is impaired in patients with hypertrophic cardiomyopathy and left ventricular dysfunction. Am Heart J 136(6):972–981
Cecchi F, Olivotto I, Gistri R, Lorenzoni R, Chiriatti G, Camici PG (2003) Coronary microvascular dysfunction and prognosis in hypertrophic cardiomyopathy. N Engl J Med 349(11):1027–1035. doi:10.1056/NEJMoa025050
Choudhury L, Rosen SD, Patel D, Nihoyannopoulos P, Camici PG (1997) Coronary vasodilator reserve in primary and secondary left ventricular hypertrophy. A study with positron emission tomography. Eur Heart J 18(1):108–116
Olivotto I, Cecchi F, Gistri R, Lorenzoni R, Chiriatti G, Girolami F, Torricelli F, Camici PG (2006) Relevance of coronary microvascular flow impairment to long-term remodeling and systolic dysfunction in hypertrophic cardiomyopathy. J Am Coll Cardiol 47(5):1043–1048. doi:10.1016/j.jacc.2005.10.050
Knaapen P, van Dockum WG, Gotte MJ, Broeze KA, Kuijer JP, Zwanenburg JJ, Marcus JT, Kok WE, van Rossum AC, Lammertsma AA, Visser FC (2006) Regional heterogeneity of resting perfusion in hypertrophic cardiomyopathy is related to delayed contrast enhancement but not to systolic function: a PET and MRI study. J Nucl Cardiol 13(5):660–667. doi:10.1016/j.nuclcard.2006.05.018
Bravo PE, Zimmerman SL, Luo HC, Pozios I, Rajaram M, Pinheiro A, Steenbergen C, Kamel IR, Wahl RL, Bluemke DA, Bengel FM, Abraham MR, Abraham TP (2013) Relationship of delayed enhancement by magnetic resonance to myocardial perfusion by positron emission tomography in hypertrophic cardiomyopathy. Circ Cardiovasc Imaging 6(2):210–217. doi:10.1161/CIRCIMAGING.112.000110
Lefroy DC, de Silva R, Choudhury L, Uren NG, Crake T, Rhodes CG, Lammertsma AA, Boyd H, Patsalos PN, Nihoyannopoulos P et al (1993) Diffuse reduction of myocardial beta-adrenoceptors in hypertrophic cardiomyopathy: a study with positron emission tomography. J Am Coll Cardiol 22(6):1653–1660
Schafers M, Dutka D, Rhodes CG, Lammertsma AA, Hermansen F, Schober O, Camici PG (1998) Myocardial presynaptic and postsynaptic autonomic dysfunction in hypertrophic cardiomyopathy. Circ Res 82(1):57–62
Choudhury L, Guzzetti S, Lefroy DC, Nihoyannopoulos P, McKenna WJ, Oakley CM, Camici PG (1996) Myocardial beta adrenoceptors and left ventricular function in hypertrophic cardiomyopathy. Heart 75(1):50–54
Orakzai SH, Orakzai RH, Nasir K, Budoff MJ (2006) Assessment of cardiac function using multidetector row computed tomography. J Comput Assist Tomogr 30(4):555–563
Dewey M, Muller M, Eddicks S, Schnapauff D, Teige F, Rutsch W, Borges AC, Hamm B (2006) Evaluation of global and regional left ventricular function with 16-slice computed tomography, biplane cineventriculography, and two-dimensional transthoracic echocardiography: comparison with magnetic resonance imaging. J Am Coll Cardiol 48(10):2034–2044. doi:10.1016/j.jacc.2006.04.104
Mangalat D, Kalogeropoulos A, Georgiopoulou V, Stillman A, Butler J (2009) Value of cardiac CT in patients with heart failure. Curr Cardiovasc Imaging Rep 2(6):410–417. doi:10.1007/s12410-009-0052-3
Mao S, Budoff MJ, Oudiz RJ, Bakhsheshi H, Wang S, Brundage BH (1999) Effect of exercise on left and right ventricular ejection fraction and wall motion. Int J Cardiol 71(1):23–31
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Finocchiaro, G., Vitrella, G., Pinamonti, B. (2014). Other Imaging Techniques in Hypertrophic Cardiomyopathy. In: Pinamonti, B., Sinagra, G. (eds) Clinical Echocardiography and Other Imaging Techniques in Cardiomyopathies. Springer, Cham. https://doi.org/10.1007/978-3-319-06019-4_12
Download citation
DOI: https://doi.org/10.1007/978-3-319-06019-4_12
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-06018-7
Online ISBN: 978-3-319-06019-4
eBook Packages: MedicineMedicine (R0)