Abstract
Acetabular fractures constitute 18 % of pelvic injuries and most often occur in young adults involved in high-energy motor vehicle collisions or falls from a height. The treatment of acetabular fractures is a complex area of orthopaedics that is continually refined. Patients with acetabular fractures often have multiple injuries, and the initial approach to evaluation should follow ATLS guidelines. CT scan is currently the best diagnosis tool in the acetabular fracture assessment. There are several acetabular fracture classification schemes. However, the most widely used is the Judet-Letournel classification scheme. Nondisplaced fractures or displaced fractures that do not involve the dome of the acetabulum are treated nonsurgically, except posterior wall fractures. Open reduction and internal fixation, as for any other intra-articular fracture, is now a standard treatment for a displaced acetabular fracture. The approach selected depends on pattern and location of the fracture: ilioinguinal or modified Stoppa for anterior fractures and Kocher-Langenbeck for posterior fractures. Both-column fractures may require both an anterior and a posterior approach. Early complications include deep vein thrombosis, post-traumatic nerve palsies (16.4 %), and wound infection (4–5 %). Late complications are as follows: heterotopic ossification (25.6 %), osteoarthritis (26 %), and avascular necrosis (3–53 %). 8.5 % of the patients require total hip arthroplasty 2 years following the initial procedure. The treatment of these fractures sets high demands and needs to be in the hands of experts. In these cases, an excellent or good functional outcome can be expected in between 83 and 89 % of patients with an anatomical reduction.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
6.1 Introduction
The treatment of acetabular fractures is a complex area of orthopaedics that is continually refined. Until the middle of the twentieth century, surgical treatment of pelvic and acetabular fractures was non-existent [1].
In the early 1960s, the management of acetabular fractures was revolutionised by the work of Judet and Letournel. They recognised that the principles applied to the treatment of displaced articular fractures (anatomic reduction, stable fixation, and early movement) should also be applied to the acetabulum. Their studies led them develop news surgical approaches and a classification system which has been tested in time and is currently used all over the world [2]. This approach led to a reduction in the incidence of post-traumatic arthritis and an improvement in the overall outcome.
Acetabular fractures constitute 18 % of pelvic injuries and most often occur in young adults involved in high-energy motor vehicle collisions or falls from a height. As with pelvic fractures, acetabular fractures also can occur in older patients with osteoporotic bone, usually from a low-energy fall.
6.2 Anatomy
The acetabulum can be described as an incomplete hemispherical socket with an inverted horseshoe-shaped articular surface surrounding the nonarticular cotyloid fossa. This articular socket is composed of and supported by two columns of bone, described by Letournel and Judet as an inverted Y [3].
The anterior column is defined as the strut of bone that extends from the sacroiliac joint to the ipsilateral pubic ramus. The anterior column includes the superior pubic ramus, anterior half of the acetabulum, anterosuperior and anteroinferior iliac spines, and anterior iliac crest. The iliopectineal (also called the iliopubic) line on radiographs approximates the anatomic anterior column [4].
The posterior column is the bony strut extending from the posterosuperior iliac spine to the ischial tuberosity. The posterior column includes the portion of the ischium from the ischiopubic junction of the obturator foramen to the greater sciatic notch and posterior half of the acetabulum. The ilioischial line on radiography approximates the anatomic posterior column.
The walls of the acetabulum extend from the corresponding columns, consequently forming the acetabular cup, and stabilise the hip joint. The posterior wall is larger and extends more laterally; the anterior wall is smaller and stabilises the hip joint anteriorly and has been described as extending to the pelvic rim [5].
The neurovascular structures passing through the pelvis are at risk during the original injury and subsequent treatment, and the various surgical approaches are designed around these structures. The sciatic nerve exiting the greater sciatic notch inferior to the piriformis muscle frequently is injured with posterior fractures-dislocations of the hip and fractures with posterior displacement. The superior gluteal artery and nerve exit the greater sciatic notch at its most superior aspect and can be tethered to the bone at this level by variable fascial attachments.
6.3 Clinical Evaluation
Patients with acetabular fractures often have multiple injuries and the initial approach to evaluation should follow ATLS guidelines [5]. Careful assessment of the ipsilateral lower extremity should be taken and performed to rule out fracture or ligamentous injury of the knee. The soft tissues overlying the greater trochanter should be carefully inspected for signs of a Morel-Lavallee lesion , a closed degloving injury resulting in a haematoma and liquefied fat forming between the subcutaneous tissues and the fascial layer. Sciatic nerve function should be carefully assessed in the ipsilateral extremity, especially with fractures involving the posterior wall.
6.4 Radiographic Evaluation
Acetabular fracture classification by Judet and Letournel requires oblique radiographs of the pelvis. A standard radiograph series consists of an anteroposterior view and left and right Judet views. Judet views are right posterior oblique (also known as right iliac oblique or left obturator oblique) and left posterior oblique (also known as left iliac oblique or right obturator oblique) views of the pelvis. Appropriate positioning of the obliquity is confirmed by ensuring that the coccyx projects over the ipsilateral femoral head: In the right posterior oblique projection, the coccyx should project over the right femoral head.
The obturator oblique view splays open the contralateral iliac wing and allows visualisation of the ipsilateral iliopectineal line and posterior wall. For example, with a right obturator oblique view, the right iliopectineal line, left iliac wing, and right posterior wall are best visualised.
An iliac oblique view shows the ipsilateral ilioischial line and the anterior wall. Thus, the right iliac oblique view will show the entire right ilium en face, the right anterior wall, and the left posterior wall. These views are critical to orthopaedists because they are the intraoperative views used to judge reduction.
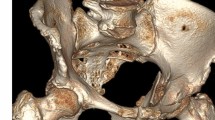
CT scan better defines acetabular fractures, particularly in identifying the location and displacement of fractures and loose fragments in the hip joint. CT also helps with preoperative planning. Furthermore, CT offers better soft tissue assessment for rapid evaluation of visceral structures in the multitrauma patient [6] (Figs. 6.1 and 6.2).
6.5 Classification
There are several acetabular fracture classification schemes, with the most widely used classification scheme being the Judet-Letournel classification scheme.
In the Judet-Letournel classification system, acetabular fractures are classified into two broad categories: elementary and associated fractures. The associated fracture patterns are composed of a combination of at least two of the elementary fracture patterns. The importance of this classification system lies in the fact that different acetabular fractures are repaired by different surgical approaches and techniques [7].
Elementary fractures include wall, column, and transverse fractures. These fracture types can easily be remembered by recalling the basic functional anatomy of the acetabulum: Elementary fractures involve a single wall, a single column, or are purely transverse. The simplest elementary fractures are two-part fractures. It is important to note that the term “transverse fracture” should be reserved to describe a diagnostic type of acetabular fracture, whereas the term “transverse” should be avoided when describing the orientation of a fracture because it may quickly become confusing as to which type of fracture is present.
Associated fracture patterns have at least three major fracture fragments and include a posterior column fracture with a posterior wall fracture, a transverse fracture with a posterior wall fracture, an anterior column fracture with a posterior hemi-transverse fracture, a T-type transverse fracture, and associated both-column fractures.
Although there are ten fracture patterns , 90 % of acetabular fractures that occur are one of five types: associated both-column, T-type, transverse, transverse with posterior wall, and elementary posterior wall fractures [8]. Some investigators have advocated concentrating only on these common fractures; however, commonly acetabular fractures do not fit perfectly in one of the fracture patterns in the classification scheme.
The most frequent type of fracture involved the posterior wall, accounting for 23.9 % of all injuries. Fractures involving both columns were seen in 22 %, those described as transverse and involving the posterior wall accounted for 17.7 %, while other fracture types were less common and were seen in less than 10 %.
The AO group has developed an alphanumeric classification system for acetabular fractures based on the severity of the fracture: Type A fractures include fractures of a single wall or column, type B fractures involve both anterior and posterior columns (both transverse or T-type fractures), and type C fractures involve both anterior and posterior columns, but all articular segments, including the roof, are detached from the remaining segment of the intact ilium. Type C fractures are those designated both-column fractures in the Letournel and Judet classification. Each type has subtypes 1, 2, and 3, depending on the characteristics of the fracture (Figs. 6.3, 6.4, and 6.5).
6.6 Treatment
6.6.1 Nonsurgical Treatment
In the past few decades, indications for conservative management have been reduced to a minimum, and it is currently used mostly in circumstances preventing surgery [9].
Nondisplaced fractures or displaced fractures that do not involve the dome of the acetabulum are treated nonsurgically. The dome of the acetabulum has been defined by Matta et al. [10] as the area within the 45° roof arc or the superior 10 mm on a CT scan. An exception to this rule is posterior wall fractures, which may not involve the dome but nevertheless can result in hip instability if a large fragment is involved.
Some both-column fractures have extensive comminution, but the fragments remain minimally displaced around the femoral head. This so-called secondary congruence also allows for nonsurgical management. Other contraindications to open reduction and internal fixation include the following: associated medical conditions that prevent surgery; advanced osteoporosis or degenerative joint disease, making hip arthroplasty the better option; and local or systemic sepsis. In all those cases, the treatment consists in mobilisation out of bed with toe-touch weight bearing for 10–12 weeks.
6.6.2 Surgical Treatment
Open reduction and internal fixation, as for any other intra-articular fracture, is now a standard treatment for a displaced acetabular fracture . In a comparative study, nonoperative treatment of the displaced acetabular fracture has been shown to give far inferior results compared to operative treatment (30 % good results versus 86 % good results). The goal of treatment of a displaced acetabular fracture is to achieve anatomical reduction of the articular surface with rigid internal fixation to allow early joint motion, but the choice of surgical approach remains controversial [11].
6.6.2.1 Indications for Operative Treatment and Selection of Approach
Indications include fractures involving the dome of the acetabulum with at least 2 mm of displacement, fractures that result in instability of the hip joint, and fractures with trapped intra-articular fragments. The approach selected depends on pattern and location of the fracture. Fractures involving a single column or wall can be approached through a single approach (ilioinguinal or modified Stoppa for anterior fractures and Kocher-Langenbeck for posterior fractures).
The Kocher-Langenbeck approach is used most frequently in the operative treatment of acetabular fractures. It gives access to the retroacetabular surface of the innominate bone from the ischium to the greater sciatic notch. Access to the quadrilateral surface is possible by palpation through the greater and lesser sciatic notches, allowing assessment after the reduction of fractures involving the quadrilateral plate and anterior column. The greater sciatic notch also provides a window for the placement of clamps to manipulate and reduce these fractures. The superior gluteal neurovascular bundle limits access to the superior iliac wing in this approach.
The ilioinguinal approach offers a direct view of the iliac wing, the anterior sacroiliac joint, the entire anterior column, and the pubic symphysis.
Both-column fractures may require both an anterior and a posterior approach or an extensile approach such as the extended iliofemoral. This is an anatomical approach and follows an internervous plane, reflecting anteriorly the femoral nerve-innervated muscles and posteriorly the muscles innervated by the superior and inferior gluteal nerves. The posterior flap is mobilised as a unit without damaging its neurovascular bundles.
This approach provides direct exposure of the whole outer aspect of the ilium, the posterior column down to the ischium, and the hip joint. With further retraction of the iliopsoas and abdominal muscles medially, exposure of the internal aspect of the ilium is also possible.
6.6.2.2 Fracture Osteosynthesis
Posterior wall fractures are the commonest type of acetabular fracture. Fractures of the posterior wall of the acetabulum as well as fractures of the posterior column, fractures of the posterior column and wall, transverse fractures, and transverse posterior wall T-shaped fractures can be managed with the operative technique described below [12].
Displaced posterior column fractures can be reduced using either a bone hook or a reduction forceps. Rotational deformities can be corrected by inserting a Schanz screw into the ischial tuberosity, thus allowing manipulation of the deformity.
In an isolated posterior wall fracture, the fragment is reduced anatomically and held with the aid of K-wires. Lag screws can then be inserted from the wall to the posterior column. A depth gauge is usually used to determine the screw length and 3.5 mm screws are used from the posterior wall to the posterior column. The overall fixation is then neutralised by the application of 3.5 plate appropriately contoured to accommodate the shape of the posterior column. The plate must be contoured adequately to include coverage of the posterior wall fracture. Where there is a transverse facture, a screw can be inserted from the posterior to the anterior column.
Isolated anterior column and anterior wall fractures account for only 6.3 % of acetabular fractures. Their outcome is often analysed with other associated fracture patterns, particularly hemi-transverse or bicolumnar fractures, thereby masking their true prognosis. In spite of extensive literature on the management of acetabular fractures in general, information on outcome following open reduction and internal fixation (ORIF) of anterior column and anterior wall fractures is scarce [13]. Depending on the displacement and stability of the fracture fragments, either closed reduction and percutaneous fixation or ORIF through an ilioinguinal approach can be performed (Figs. 6.6, 6.7, and 6.8).
6.7 Outcomes and Complications
Following stable fixation, patients should be mobilised as soon as possible. Weight bearing on the injured side is limited to touch down for 10–12 weeks. With stable fractures or solid fixation, active and active-assist range of motion of the affected extremity is begun as soon as symptoms allow. Isometric quadriceps exercises and straight leg raises are begun early to minimise thigh atrophy. Full weight bearing is delayed for 10–12 weeks, at which point progressive strengthening exercises are added.
The outcome following acetabular fracture may be influenced by various factors. Those beyond the surgeon’s control include the mechanism of the injury, damage to the femoral head, sciatic nerve injury, dislocation, fracture pattern, associated injuries, the patient’s age, and comorbidities. Crucial yet controllable factors include the timing of surgery, surgical selection, and quality of reduction and fixation. Restoration of articular congruity with stable fixation is the most significant predictive factor of post-traumatic osteoarthritis [14]. Complex associated fractures need to be fixed within the first 5 days, but more simple fractures can be adequately managed up to 15 days after the injury. Beyond this time, results become less satisfactory.
Mears et al. [15] showed in his study of 424 fractures treated by operation that simple fractures were reduced anatomically in 87 % of patients, whereas associated fractures could be reduced anatomically in only 59 %. Matta [16] had similar results, achieving anatomical reduction in 96 % of simple fractures and only 64 % of associated fractures. Both agree that both-column and T-type fractures showed the least accuracy of reduction.
6.7.1 Early Complications
Deep vein thrombosis (DVT) is a major concern for patients with acetabular fractures. Prevention includes use of pneumatic compression boots and chemical prophylaxis.
Iatrogenic nerve or vessel injury can result from surgical treatment. Maintaining the knee in flexion and the hip in extension during the Kocher-Langenbeck approach helps to decrease the tension on the sciatic nerve. Self-retaining retractors should be used with caution. There is an overall incidence of post-traumatic nerve palsies associated with acetabular fractures of 16.4 %. This rises to more than 40 % in fractures involving a posterior dislocation of the hip. The incidence of infection is between 4 and 5 %.
6.7.2 Late Complications
Heterotopic ossifications are most common with the extended iliofemoral and Kocher-Langenbeck approaches and least common with the ilioinguinal approach. A meta-analysis by Giannoudis et al. [17] showed an incidence of 25.6 % of HO following operation for acetabular fractures. However, only 5.7 % of patients will develop HO grade III or IV according to the Brooker classification. Several clinical studies have shown that either local radiation or oral administration of indometacin provided effective prophylaxis against HO following the surgical treatment of acetabular fractures.
The overall incidence of osteoarthritis (OA) following operatively treated acetabular fractures is around 26 %. Higher rates can be reached, especially in anterior column/posterior hemi-transverse, T-shaped, and posterior wall/posterior column fractures. Further risk factors for the development of post-traumatic OA include associated chondral or osseous lesions of the femoral head and the quality of reduction.
The incidence of avascular necrosis (AVN) described in published papers varies from 3 to 53 %. Recent reports show that it may be grossly overestimated and that most of the observed changes in the head of the femur are probably due to OA. However, in patients sustaining a posterior fracture dislocation of the hip, the incidence of AVN increased up to 9.2 % [18].
8.5 % of patients with fractures treated by operation needed an arthroplasty at an average of 2 years following the initial procedure. Anyway, long-term results are influenced by numerous factors. The type of fracture and the quality of the reduction are the main influences on functional outcome. The quality of reduction is a crucial but controllable factor. An excellent or good functional outcome can be expected in between 83 and 89 % of patients with an anatomical reduction [19].
The treatment of these fractures sets high demands and needs to be in the hands of experts. Tertiary referrals should be undertaken as early as possible, since the timing is of utmost importance. It is important, at operation, to obtain the most accurate reduction of the fracture, which is possible, with a minimal surgical approach. Both, anatomical reduction and minimal approach, influence the outcome.
6.8 Conclusions
Acetabular fractures constitute 18 % of pelvic injuries, and most often occur in young adults involved in high-energy motor vehicle collisions or falls from a height. The treatment of acetabular fractures is a complex area of orthopaedics that is continually refined. Patients with acetabular fractures often have multiple injuries and the initial approach to evaluation should follow ATLS guidelines. CT scan is currently the best diagnosis tool in the acetabular fracture assessment. There are several acetabular fracture classification schemes. However, the most widely used is the Judet-Letournel classification scheme. Nondisplaced fractures or displaced fractures that do not involve the dome of the acetabulum are treated nonsurgically, except posterior wall fractures.
Open reduction and internal fixation, as for any other intra-articular fracture, is now a standard treatment for a displaced acetabular fracture. The approach selected depends on pattern and location of the fracture: ilioinguinal or modified Stoppa for anterior fractures and Kocher-Langenbeck for posterior fractures. Both-column fractures may require both an anterior and a posterior approach. Early complications include deep vein thrombosis, post-traumatic nerve palsies (16.4 %), and wound infection (4–5 %). Late complications are as follows: heterotopic ossification (25.6 %), osteoarthritis (26 %), and avascular necrosis (3–53 %). 8.5 % of the patients require total hip arthroplasty 2 years following the initial procedure. The treatment of these fractures sets high demands and needs to be in the hands of experts. In these cases, an excellent or good functional outcome can be expected in between 83 and 89 % of patients with an anatomical reduction.
References
Giannoudis PV, Bircher M, Pohlemann T (2007) Advances in pelvic and acetabular surgery. Injury 38:395–396
Judet R, Judet J, Leturnel E (1964) Fractures of the acetabulum. Classification and surgical approaches for open reduction. J Bone Joint Surg Am 46:1615–1636
Lawrence DA, Menn K, Baumgaertner M, Haims AH (2013) Acetabular fractures: anatomic and clinical considerations. AJR Am J Roentgenol 201:W425–W436
Lenarz CJ, Moed BR (2007) A typical anterior wall fracture of the acetabulum: case series of anterior acetabular rim fracture without involvement of the pelvic brim. J Orthop Trauma 21:515–522
Alonso JE, Volgas DA, Giordano V, Stannard JP (2000) A review of the treatment of hip dislocation associated with acetabular fractures. Clin Orthop Relat Res 377:32–43
O’Toole RV, Cox G, Shanmuganathan K et al (2010) Evaluation of computed tomography for determining the diagnosis of acetabular fractures. J Orthop Trauma 24:284–290
Potok PS, Hopper KD, Umlauf MJ (1995) Fractures of the acetabulum: imaging, classification, and understanding. Radiographics 15:7–23
Durkee NJ, Jacobson J, Jamadar D, Karunakar MA, Morag Y, Hayes C (2006) Classification of common acetabular fractures: radiographic and CT appearances. AJR Am J Roentgenol 187:915–925
Sen RK, Veerappa LA (2009) Long-term outcome of conservatively managed displaced acetabular fractures. J Trauma 67:155–159
Matta JM, Anderson LM, Epstein HC, Hendricks P (1986) Fractures of the acetabulum: a retrospective analysis. Clin Orthop Relat Res 205:230–241
Kumar A, Shah NA, Kershaw SA, Clayson AD (2005) Operative management of acetabular fractures. A review of 73 fractures. Injury 36:605–612
Giannoudis PV, Nikolaou VS (2008) Surgical techniques–How do I do it? Open reduction and internal fixation of posterior wall fractures of the acetabulum. Injury 39:1113–1118
Giannoudis PV, Kanakaris NK, Dimitriou R, Mallina R, Smith RM (2011) The surgical treatment of anterior column and anterior wall acetabular fractures. J Bone Joint Surg Br 93:970–974
Briffa N, Pearce R, Hill AM, Bircher M (2011) Outcomes of acetabular fracture fixation with ten years’ follow-up. J Bone Joint Surg Br 93:229–236
Mears DC, Velyvis JH, Chang CP (2003) Displaced acetabular fractures managed operatively: indicators of outcome. Clin Orthop Relat Res 407:173–186
Matta JM (1996) Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am 78:1632–1645
Giannoudis PV, Grotz MRW, Papakostidis C, Dinopoulos H (2005) Operative treatment of displaced fractures of the acetabulum. A meta-analysis. J Bone Joint Surg Br 87:2–9
Moed BR, Willson Carr SE, Watson JT (2002) Results of operative treatment of fractures of the posterior wall of the acetabulum. J Bone Joint Surg Am 84:752–758
Murphy D, Kaliszer M, Rice J, McElwain JP (2003) Outcome after acetabular fracture: prognostic factors and their inter-relationships. Injury 34:512–517
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Zamora-Carrera, E., Rubio-Suárez, J.C. (2014). Complex Fractures of the Acetabulum. In: Rodríguez-Merchán, E., Rubio-Suárez, J. (eds) Complex Fractures of the Limbs. Springer, Cham. https://doi.org/10.1007/978-3-319-04441-5_6
Download citation
DOI: https://doi.org/10.1007/978-3-319-04441-5_6
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-04440-8
Online ISBN: 978-3-319-04441-5
eBook Packages: MedicineMedicine (R0)