Abstract
This chapter is a guide to the diagnosis of secondary headaches that are nonvascular. By necessity, the sections are disparate, but important for diagnostic purposes.
In the first part, consideration is given to the diagnosis of cerebrospinal fluid (CSF)-related abnormalities, such as idiopathic intracranial hypertension (IIH, pseudotumor cerebri) and CSF low-pressure headaches.
The second part of the chapter deals with headaches secondary to tumors. The third part gives guidance on the diagnosis of headaches attributed to infection, such as human immunodeficiency virus (HIV). Headaches attributed to Chiari malformation type 1 constitute the fourth section. Headaches attributed to homeostasis disorders are covered in the fifth section.
The next sections include headaches attributed to substances, cervicogenic headache, and temporomandibular disorders.
The chapter ends with a section on the new International Classification of Headache Disorders, third edition (ICHD-3) classification system for diagnosing trigeminal neuralgia (TN) and painful trigeminal neuropathies, with a part on the other cranial neuralgias as well.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Secondary headache
- Idiopathic intracranial hypertension
- Pseudotumor cerebri
- Low CSF pressure headache
- Brain tumor headache
- HIV headache
- Chiari malformation type 1
- Cervicogenic headache
- Trigeminal neuralgia
- Trigeminal neuropathy
- Cranial neuralgia
Introduction
The second chapter on diagnosis of secondary headaches includes nonvascular disorders .
The organization of the chapter is by unrelated secondary disorders, linked by their propensity to cause headache, and their ICHD-3 classification are listed in Table 7.1 .
Secondary Idiopathic Intracranial Hypertension (Pseudotumor Cerebri)
Normal cerebrospinal fluid (CSF) pressure ranges from 70 to 250 mm of H2O. Elevated intracranial hypertension may be idiopathic or due to secondary causes. Secondary causes for increased intracranial pressure (ICP) are listed in Table 7.2 .
Once secondary causes of raised ICP are excluded, the diagnosis of idiopathic intracranial hypertension (IIH, pseudotumor cerebri) can be made on the basis of headache, documented raised ICP, and headache either developing along with the increased pressure and/or reported improvement of headache with lowering of ICP following removal CSF with lumbar puncture (LP). Although once considered the hallmark of IIH, evidence of papilledema is no longer a necessary criterion, given the fact that cases of IHH without papilledema does infrequently occur. The finding of papilledema on examination still remains strong supporting evidence for the diagnosis.
As noted above, IIH was previously referred to as benign intracranial hypertension as well as pseudotumor cerebri. Diagnostic criteria by the ICHD-3 for IIH are listed in Table 7.3.
The disorder tends to affect obese females (body mass index > 30). Patients most often report a constant, daily, pressure-like headache pain that may be frontal, retro-orbital or diffuse in location, and at least moderate in severity. The headache is aggravated by Valsalva-type maneuvers. Other signs and symptoms include papilledema as well as cranial nerve dysfunction. It is not uncommon for the patient to report visual changes such as blurring or transient visual obscurations (TVOs). Diplopia related to cranial nerve VI palsy and pulsatile tinnitus are additional common complaints. Persistently elevated CSF pressures can lead to permanent visual loss.
The patient should be evaluated with magnetic resonance imaging (MRI) and magnetic resonance venography (MRV) to rule out venous thrombosis, which as noted, is the most common secondary cause other than obesity. Other findings suggestive of IIH can be seen on MRI as listed in Table 7.4. A neuro-ophthalmologic examination, including visual field testing, is required to monitor visual acuity. An LP is necessary to document raised ICP. The diagnosis of IIH cannot be made without an LP performed in the lateral decubitus position! (Table 7.5).
An opening pressure of greater than 250 mm H2O in adults, and greater than 280 mm H2O in children is confirmatory of the diagnosis. The previous ICHD-2 classification allowed for the diagnosis of IIH if the opening pressure was greater than 200 mm H2O in nonobese individuals, but this criterion has been changed in the ICHD-3 criteria of 2013. Patients respond favorably after the withdrawal of CSF, but unfortunately the response is short lasting, and further treatment will be described in Chap. 17.
Low Cerebrospinal Fluid Pressure Headache
Headache caused by low CSF pressure is either the result of a previous LP, a CSF fistula, or idiopathic in etiology. The clinical manifestations are similar despite the etiology of the intracranial hypotension (Table 7.6).
Classically, patients report a headache in the upright position with relief of symptoms when recumbent. CSF opening pressure is measured at below 60 mmHg H2O. Studies of the CSF may reveal a normal to slightly elevated protein level and even a mild lymphocytic pleocytosis.
Approximately a third of patients will develop headache following LP. The postdural puncture headache (previously termed postlumbar puncture headache) generally occurs within 5 days after the dural puncture. Spontaneous improvement typically occurs within 2 weeks of the onset of symptoms. In cases without spontaneous improvement, an epidural lumbar blood patch can provide prompt relief.
The symptoms are most likely related to a persistent dural tear caused by the LP needle, resulting in fistula formation. Female gender, younger age (31–50 years), and prior history of postdural puncture headache are risk factors.
Methods to try to reduce the risk of postdural puncture headache include inserting the LP needle bevel parallel to the longitudinal axis of the dural fibers, using a smaller needle size, replacement of the stylet before the needle is withdrawn, and using noncutting needles such as the Sprotte needle. The duration of recumbency following an LP or the recommendation to increase fluids does not seem to influence the occurrence of postdural puncture headache.
Idiopathic low CSF pressure headache or CSF fistula headache also produces symptoms of low-pressure headache, although the response to positional changes is less impressive than with postdural puncture headache. If the headache develops into a chronic condition, the classical features of orthostatic headache often diminish and may even be present in the lying position.
In the case of a CSF fistula, there is sometimes a known trauma or iatrogenic cause such as a neurosurgical procedure. More commonly, fistulas may occur spontaneously without a known precipitating event, as in the case of idiopathic low CSF pressure headache. Spontaneous CSF leaks are most commonly identified in the cervical or thoracic region.
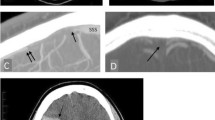
An MRI of the brain with and without gadolinium is often diagnostic of low CSF pressure headache , demonstrating evidence of brain sag and diffuse pachymeningeal enhancement without evidence of leptomeningeal involvement. Other imaging findings are listed in Table 7.7.
Unfortunately, despite the number of diagnostic imaging studies which can be utilized, finding the actual site of the leak is often quite difficult and in some cases impossible. Radioisotope cisternography is no longer recommended given poor sensitivity and more useful modalities such as MRI with fat suppression and computed tomography (CT) myelography. CT myelography may be the most reliable diagnostic approach to utilize.
Headache Attributed to Intracranial Neoplasm
Headache may be the initial presentation in approximately 20 % of patients with brain tumors. The incidence of headache increases to 50–70 % of patients later in the course of their illness.
Most individuals with an underlying brain tumor who present with headache will also have other focal neurologic symptoms such as seizures, confusion, or hemiparesis. Brain tumor headache is characterized as progressive, diffuse, nonpulsating, and associated with nausea and/or vomiting. The headache may be constant or intermittent. The headache worsens with physical activity, Valsalva-type maneuvers, and tends to be most severe in the morning and after napping.
Both mass effect of the tumor and hydrocephalus contribute to the headache, causing local pressure and/or traction on pain-sensitive structures of the brain. Headache is more frequent with infratentorial tumors than supratentorial tumors. Finally, patients with primary headache disorders before developing a brain tumor will often have some features of their preexisting headaches with their brain tumor headache .
Headache Attributed to Infectious Diseases
Any underlying infection may produce a headache or worsen a preexisting primary headache condition. The infection may be systemic or intracranial. Patients with headache related to systemic infection generally have fever, malaise, and diffuse myalgias.
Headache is common in HIV-infected patients at any stage of the illness and has been noted to occur with HIV seroconversion related to primary infection. Later in HIV illness, any presentation of headache or change in pattern of headache should be assumed to be secondary (Table 7.8).
Intracranial infections are most often bacterial or viral, but various opportunistic infections may occur, particularly in immunosuppressed patients . In general, the greatest risk for opportunistic infections is in HIV patients with CD4 counts below 200 cells/mm3, and those with CD4 counts greater than 500 cells/mm3 are not considered to be at risk. Evaluation for intracranial infections should be performed in individuals presenting with new-onset or worsening headache associated with fever, meningismus, altered mentation, or focal neurologic deficits.
Headaches associated with infection can be caused by meningitis, encephalitis, brain abscess, or subdural empyema. Antibiotic therapy should be initiated immediately if there is concern for intracranial infection, after which the clinician can proceed with diagnostic testing with urgent CT, LP, and MRI.
The headache attributed to infection should resolve within 3 months of successful treatment. A persistent headache pattern may develop in up to 1/3 of patients following a past episode of meningitis despite adequate treatment. Another subset, chronic headache attributed to infection, refers to headaches lasting for more than 3 months when the underlying infection remains active.
Headache Attributed to Chiari Malformation Type I
Chiari malformation type 1 (CM1) is most often congenital although acquired cases may occur, most commonly as a result of intracranial hypotension, excessive CSF drainage or injury. CM1 is diagnosed on MRI if there is greater than a 5-mm inferior displacement of the cerebellar tonsils below the foramen magnum; only 3 mm is required if there is associated crowding of the subarachnoid space at the craniocervical junction as evidenced by obstruction of CSF flow seen on MRI CINE flow studies.
Patients with CM1 commonly report headache along with a number of other symptoms related to compression of the cerebellum, brainstem, and cervical cord (Tables 7.9 and 7.10). It is important to remember that not all patients with evidence of CM1 on imaging are symptomatic.
Commonly associated with this condition are tethered cord, IIH , syringomyelia, and scoliosis. The headache is located occipitally and is brief in duration, lasting less than 5 min. It is often triggered by Valsalva-type maneuvers. This secondary cough headache is further discussed with primary cough headache in Chapter 3. Although a patient’s symptoms can be effectively treated with various medications, especially indomethacin, suboccipital decompression surgery may be indicated for those with headache with significant neurological signs and symptoms .
Headaches Associated with Disorders of Homeostasis
There are a number of systemic disorders and metabolic conditions frequently associated with headache (Table 7.11). The patient will exhibit signs and symptoms related to the underlying condition in addition to the headache. Diagnostic testing is required to confirm the diagnosis. Upon treatment of the underlying condition, the headache will resolve.
Toxic Headaches
A number of substances may produce headache either due to exposure or withdrawal (Table 7.12). Typically, once the exposure ends, the headache resolves. Headache is a commonly listed adverse effect of multiple medications. Therefore, a review of the patient’s list of medications noting their start date can be helpful in pinpointing any correlation with the headache.
Cervicogenic Headache
Headache may be a referred pain originating from the neck. This type of headache must be distinguished clinically from those patients with neck pain as an associated symptom of a primary headache disorder.
Patients at risk for cervicogenic headache include those with a history of arthritis with known cervical spondylosis and degenerative disc disease, or those with a history of neck trauma, particularly whiplash-type injuries. An examination may reveal tenderness, muscle spasm of the cervical paraspinal and neck muscles, and limitations in cervical range of motion.
Cervical myofascial pain alone without evidence of degenerative changes in the cervical spine should be diagnosed as tension-type headache. Degenerative change in the spine is a very common finding in individuals without symptoms of headache and neck pain, and therefore this finding in isolation cannot be used for definitive diagnosis of cervicogenic headache .
The pain is most often unilateral, typically starts in the occipital region, and radiates frontally. The unilaterality must be stressed as a key clinical symptom, along with the primary neck pain complaint, and the report that neck movement precipitates or aggravates the pain. Even when pain is reported bilaterally, there tends to be a one-sided predominance.
Relief after cervical anesthetic blockade can confirm the diagnosis. The head pain likely originates from stimulation of the upper cervical roots leading to the activation of the trigeminal nucleus caudalis located within the upper segment of the cervical spinal cord.
The ICHD-3 criteria for cervicogenic headache are somewhat limited in utility. They are included in Table 7.13, but clinically useful pearls follow in Table 7.14.
Temporomandibular Disorder
Temporomandibular joint (TMJ) dysfunction is a fairly common problem. Patients may present with headache which is localized to the preauricular region, mandible, masseter, and temporal region. In addition to frontotemporal headache, patients often complain of otalgia, tinnitus, and dizziness. Clinical history may elicit symptoms of bruxism during sleep and reported jaw locking or popping. Limited jaw opening and tenderness of the masticatory muscles may be noted during examination. TMJ dysfunction leads to myofascial pain contributing to the symptoms of headache. Symptoms are often self-limited, but in persistent cases, referral to a TMJ specialist may help to correct the problem.
Headache attributed to TMJ disorder should have pain in conjunction with the development of the disorder and should remit as the problem is treated. If this is still uncertain, provocative maneuvers including active or passive movement of the jaw should be able to provoke the headache. ICHD-3 beta points out that there is an overlap between this disorder and tension-type headache, and when there is uncertainty about TMJ dysfunction as a cause, coding should lean toward the diagnosis of tension-type headache.
Trigeminal Neuralgia
Trigeminal neuralgia (TN) is a disorder involving one or more of the sensory divisions of the trigeminal nerve that often produces brief but severe lancinating pain. The disorder was previously referred to tic douloureux and typically affects older individuals in its classical form.
TN used to be divided into classical or symptomatic subtypes. The 2013 ICHD-3 beta dropped the symptomatic form, and TN is divided into two broad categories, classical TN and what is really not TN and is now called painful trigeminal neuropathy (PTN; see Table 7.15).
Classical TN is further subdivided into a purely paroxysmal form, with lightning-like, electric shock-like pains lasting seconds, and a form with concomitant persistent facial pain of moderate intensity in the same affected area, usually the second and third division of the trigeminal nerve (V2, 3). Classical TN is often related to neurovascular compression of the trigeminal nerve root near the dorsal root entry zone, usually by the superior cerebellar artery.
PTN encompasses the trigeminal neuropathic pain syndromes caused by other disorders such as multiple sclerosis, postherpetic neuralgia, trauma, and that caused by a tumor or lesion. Thus, all TN is really secondary.
Diagnosis of Classical Trigeminal Neuralgia
The diagnosis of TN requires recognition of the well-described, excruciating lightning-like paroxysms of pain in one or more of the divisions of the trigeminal nerve, with triggers, without radiation, without autonomic features, and with latency periods. Pain is brief but tends to have successive recurrences, with refractory periods .
The location of TN is in V2 and V3; < 5 % of TN is located in V1. Bilateral cases are rare, except for PTN related to multiple sclerosis.
Chewing, talking, or touching the face may trigger pain, although paroxysms can occur spontaneously as well. The triggers are characteristically described as innocuous, often occurring in a stereotypical location, and are sometimes so severe that patients stop eating and lose weight. After repeated triggering, there is often a refractory period of relief in TN.
The ICHD-3 criteria for the diagnosis of TN overall are listed in Table 7.16.
From a diagnostic standpoint, the differential will be between TN and primary stabbing headaches, as well as the shorter trigeminal autonomic cephalalgias (TACs), such as paroxysmal hemicrania (PH) and short-lasting unilateral neuralgiform headache attacks (SUNHAs). Table 7.17 lists the major clinical features of TN and Table 7.18 some pearls on distinguishing TN from the short-lasting TACs and primary stabbing headaches. Rarely, the short-lasting TACs and TN can occur in the same individual, requiring separate concomitant treatments .
As noted, classical TN comes in two forms, a purely paroxysmal form and a form with the shock-like paroxysms, but a persistent moderate facial pain in between the stabs. The ICHD-3 criteria for these two forms, simply distinguished by the absence or presence of the continuous facial pain, are listed in Table 7.19.
PTN , formerly called symptomatic TN, is the result of an underlying structural lesion (Table 7.20). Common secondary causes include herpes zoster, multiple sclerosis, aneurysms, syringomyelia, post medullary infarction, sarcoidosis, and various tumors including meningiomas, schwannomas/acoustic neuromas, cholesteatomas, epidermoids, and metastases. PTN can also be posttraumatic. The ICHD-3 types of PTN are listed in Table 7.21.
Clinical features of PTN are listed in Table 7.22 and clinical pearls on diagnosing classical TN versus PTN are listed in Table 7.23. Patients should undergo an MRI/MRA of the brain with and without gadolinium to determine if they have a lesion where repair or treatment could lead to cure.
Other Facial Neuralgias
There are a number of other facial pain syndromes and neuralgias which are listed in Table 7.24. Many of these neuralgias have very specific diagnostic features, such as the swallowing trigger of glossopharyngeal neuralgia and the deep ear pain location for nervus intermedius neuralgia. A careful imaging workup for these rare neuralgias looking for secondary causes such as neoplasm is always mandatory.
Patients who do not fit a typical pattern of TN and for whom no secondary causes could be found were previously referred to as having atypical facial pain and are now said to have persistent idiopathic facial pain. They tend to describe the pain as being more diffuse, often bilateral, and more constant in nature.
These individuals tend to be younger in age and often were believed to have underlying psychiatric illness due to the fact that stress can exacerbate the condition. Atypical facial pain may also be part of a more diffuse chronic pain syndrome that involves other parts of the body.
Conclusions on Secondary Nonvascular Headaches
-
IIH is often a disease of obese women, aged 20–50
-
The diagnosis of IIH cannot be made without an LP
-
Any presentation of headache or change in pattern of headache in HIV-positive patients should be assumed to be secondary
-
Low CSF pressure headache is confirmed with an MRI without and with contrast that shows pachymeningeal enhancement, sometimes with brain sag
-
Classic TN is a disease of the elderly and generally due to a vascular anomaly; PTN is a disease of younger patients and often due to MS
Suggested Reading
Bigal ME, Lipton RB. The differential diagnosis of chronic daily headaches: an algorithm-based approach. J Headache Pain. 2007;8:263–72.
Edlow JA and the American College of Emergency Physicians Clinical Policies Subcommittee. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with acute headache. Ann Emerg Med. 2008;52:407–36.
Forsyth PA, Posner JB. Headaches in patients with brain tumors: a study of 111 patients. Neurology. 1993;43:1678–8.
Frishberg BM, Rosenberg JH, Matchar DB, et al. Evidence-Based Guidelines in the Primary Care Setting: Neuroimaging in Patients with Nonacute Headache. Available at http://www.aan.com/professionals/practice/pdfs/gl0088.pdf. Accessed July 9, 2013.
Goddeau RP, Alhazzani A. Headache in stroke: A review. Headache. 2013;53:1019–22.
Green MW. Secondary headaches. Continuum Lifelong Learning Neurol. 2012;18:783–95.
Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorder, 3rd edition, Beta Version. Cephalalgia 2013;33:629–808.
Ju, YE. Abrupt onset of severe headache. Seminars in Neurology. 2010;30:192–200.
Lipton RB, Feraru ER, Weiss G, Chhabria M, Harris C, Aronow H, Newman LC, Solomon S. Headache in HIV-1-related disorders. Headache .1991;31:518–22.
Locker T, Thompson C, Rylance J, Mason S. The Utility of Clinical Features in Patients Presenting With Nontraumatic Headache: An Investigation of Adult Patients Attending an Emergency Department. Headache. 2006;46:954–61.
Mokri B. Low cerebrospinal fluid pressure syndromes. Neurol Clin. 2004;22:55–74.
Obermann M, Holle D, Naegel S, Diener HC. Headche attributable nonvascular intracranial disorders. Curr Pain Headache Rep. 2011;15:314–23.
Pereira Monteiro JMP, Tepper S, Shapiro RE. Headache Associated with Acute Substance Use or Exposure, in Olesen J, Goadsby P, Ramadan N, Tfelt-Hansen P, Welch MA, Editors, The Headaches, 3rd Ed. Philadelphia: Lippincott Williams and Wilkins, 2006, pp 959–69.
Schiffman ES, Ohrbach R, List T, et al. Diagnostic criteria for headache attributed to temporomandibular disorders (TMD). Cephalalgia. 2012;32:683–92.
Tepper DE, Tepper SJ, Sheftell FD, Bigal ME. Headache Attributed to Hypothyroidism. Current Pain and Headache Reports. 2007;11:304–9.
Vincent MB. Headache and neck. Curr Pain Headache Rep. 2011;15:324–31.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Mays, M., Tepper, D., Tepper, S. (2014). Diagnosis of Major Secondary Headaches, Nonvascular Disorders. In: Tepper, S., Tepper, D. (eds) The Cleveland Clinic Manual of Headache Therapy. Springer, Cham. https://doi.org/10.1007/978-3-319-04072-1_7
Download citation
DOI: https://doi.org/10.1007/978-3-319-04072-1_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-04071-4
Online ISBN: 978-3-319-04072-1
eBook Packages: MedicineMedicine (R0)