Abstract
Traditionally, patients suffering from Alzheimer’s disease (AD) have been diagnosed according to clinical criteria, and a diagnosis has only been made in the dementia stage of the disease. Definite diagnosis required autopsy to confirm the neuropathological findings associated with AD, namely, extracellular depositions of amyloid β (Aβ) protein and intraneuronal neurofibrillary tangles consisting of hyperphosphorylated tau (P-tau) protein, together with gross cortical atrophy caused by neuronal degeneration and loss. These findings are reflected in the cerebrospinal fluid (CSF) of patients with AD. Numerous studies have shown that AD patients have lower levels of Aβ42 and higher levels of P-tau and total tau (T-tau) in CSF than cognitively healthy controls. In the new diagnostic criteria for AD, these CSF biomarkers are included as in vivo evidence of AD neuropathology together with positron emission tomography (PET) measurements of global cortical amyloid load. Further, AD is now divided into several disease stages, namely, preclinical AD and mild cognitive impairment and dementia due to AD. In this chapter, we review CSF biomarker characteristics for the various disease stages for AD and how to use them in the differentiation against other common neurodegenerative disorders. New candidate CSF biomarkers for AD are also presented, as well as a discussion on the standardization of biomarkers and their application in clinical trials.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Mild Cognitive Impairment
- Dementia With Lewy Body
- Mild Cognitive Impairment Patient
- Cerebral Small Vessel Disease
- Stable Mild Cognitive Impairment Patient
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
1.1 How It All Began
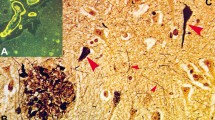
More than a century has passed since Doctor Alois Alzheimer in 1906 was the first to present a case of the disease that later would be named after him: Alzheimer’s disease (AD). The patient was a woman that he had followed over time who displayed progressive memory disturbances and cognitive symptoms, and finally dementia. Upon her death at an age of 51 years, he performed an autopsy and noticed specific findings in her brain, namely, “miliary bodies” (plaques) and “dense bundles of fibrils” (tangles), which now are considered the main neuropathological characteristics of AD (Alzheimer 1987). Except for elucidating that disturbances in the cholinergic neuronal systems are a characteristic of AD, this was what was known on AD pathogenesis during the forthcoming 80 years. However, subsequent research efforts have given detailed knowledge on the molecular pathogenesis linked to these initial discoveries.
1.2 Amyloid Plaques
That the plaques mainly consisted of the 4 kDa β-amyloid (Aβ) peptide was discovered in 1985 (Masters et al. 1985). It is now known that the major isoforms of Aβ in the plaques are Aβ4-42, Aβ1-42, and Aβ1-40 (Portelius et al. 2010). Plaques also contain deformed neurites and are often surrounded by microglia and sometimes astrocytes (Perl 2010).
Aβ originates from the amyloid precursor protein (APP) and is released after enzymatic action of β- and γ-secretase. Mutations in the gene for APP, as well as in the genes for presenilin 1 and 2, which are components of the γ-secretase, lead to altered levels of Aβ and are seen in the rare familial variant of AD (FAD) (Mullan et al. 1992; van Duijn et al. 1991; Chartier-Harlin et al. 1991; Selkoe 2001). This, together with the findings of cerebral Aβ plaque pathology in patients with Down syndrome, who have one extra of the APP containing chromosome 21 (trisomy 21), led to the hypothesis that Aβ is a driving force in the disease process (Hardy and Higgins 1992; Hardy 2009). This hypothesis, called the “amyloid cascade hypothesis,” states that increased levels of Aβ serve as a key initiating event in the disease process that ultimately results in neuronal degeneration and dementia.
1.3 Neurofibrillary Tangles
The neurofibrillary tangles are composed of abnormally phosphorylated tau protein (Grundke-Iqbal et al. 1986). Tau is an axonal protein that in its unphosphorylated state provides stabilizing functions for the microtubules (Goedert et al. 1989). When phosphorylated, however, this ability is disrupted, which leads to tau aggregation, impaired axonal transport, and eventually death of the neuron (Spires-Jones et al. 2009). Loss of neurons is a third feature of AD and can be seen at the gross anatomical levels—patients with AD have a significant thinning of the cerebral cortex compared to healthy controls (Ahn et al. 2011).
1.4 Diagnosis
The gold standard for the diagnosis of AD has since long been to perform an autopsy after the patient has deceased. The pathological hallmarks of plaques and tangles must be present to a certain extent to confer a pathological diagnosis. In 1984, clinical criteria for probable AD were published by a working group established by the National Institute of Neurological and Communicative disorders and Stroke and the Alzheimer’s Disease and Related Disorders Association (McKhann et al. 1984). By these criteria, a diagnosis of AD could only be made when the patient was demented, and the diagnosis was mainly made by excluding other causes of dementia. Revision of these guidelines was made by the National Institute on Aging (NIA) in 2011 (Jack et al. 2011). Now, cerebrospinal fluid (CSF) and imaging biomarkers (magnetic resonance imaging measurements of hippocampal atrophy and positron emission tomography [PET] measurements of amyloid load and cortical glucose metabolism) were implemented for providing in vivo evidence of AD neuropathology. Also, the whole spectrum of the disease was acknowledged, from cognitively healthy individuals to patients experiencing some cognitive deficits (i.e., mild cognitive impairment [MCI]), and ultimately patients with full-blown dementia. According to these NIA 2011 guidelines, a diagnosis of AD could be made irrespective of disease stage, and criteria for preclinical AD, mild cognitive impairment (MCI) due to AD, and dementia due to AD were given (Sperling et al. 2011a; Albert et al. 2011).
1.5 Roles of CSF Biomarkers for AD
Biomarkers are variables (physiological, biochemical, anatomical) that can be measured in vivo and that indicate specific features of disease-related pathological changes (Jack et al. 2010). CSF has been the most successful source for finding fluid biomarkers for AD pathology. Since it surrounds the brain, it is close to the pathologies of interest, which may explain the success rate. As mentioned above, biomarkers are becoming increasingly important in the diagnosis of AD. However, there are also other potential roles.
As of today, the only treatments available for AD are symptomatic, and studies have shown significant but limited effects (Raina et al. 2008). Hence, disease-modifying drugs are needed. Over the past 20 years, there have been a large number of drug candidates, mainly focusing on the amyloid cascade hypothesis, but all have failed in late-stage clinical trials (Karran et al. 2011). This has raised critical voices about this hypothesis, especially since it has not been proven with certainty in late onset AD, which is the most common form. However, drug studies have mainly targeted patients in later stages of AD. Since disease-modifying drugs probably will be most effective in the earlier stages of the disease, before plaque and tangle load and neurodegeneration become too severe, it is possible that the recent drug failures partly may depend on including too severely affected patients (Garcia-Alloza et al. 2009; Das et al. 2001; Levites et al. 2006; Sperling et al. 2011b). A need to find patients early in the disease process, maybe even at a presymptomatic stage, has arisen. Here, CSF biomarkers may have an important role in providing early evidence of ongoing AD pathology. Even though the longitudinal trajectories of the AD biomarkers need to be further elucidated, it is known that biomarker abnormalities can be found before patients experience their first symptoms, reflecting the long asymptomatic phase of the disease (Jack et al. 2010). Further, biomarkers can provide indirect evidence that disease-modifying drugs really affect the central disease process and hallmark neuropathology, which is central together with a beneficial effect on cognition (Siemers 2009). Together, this has created a need for biomarkers corresponding to core element of the disease process for use in diagnostics and to monitor biochemical actions of upcoming drugs. In this chapter, we review the literature of biomarkers related to AD and highlight their diagnostic capability as well as their relation to AD pathology. Figures 20.1 and 20.2 show a summary of the biomarkers reviewed in this chapter.
Table of CSF biomarkers reviewed in this chapter. AD Alzheimer’s disease, ALS amyotrophic lateral sclerosis, BACE1 β-site APP cleaving enzyme 1, CJD Creutzfeldt-Jakob disease, CSF cerebrospinal fluid, DLB dementia with Lewy bodies, FTD frontotemporal dementia, HIV human immunodeficiency virus, sAPP soluble amyloid precursor protein
2 Core CSF AD Biomarkers
The CSF biomarkers for AD that have been most successful reflect the core cerebral pathologies of the disease.
2.1 Aβ42
Aβ is produced during normal cell metabolism and is secreted into the CSF (Seubert et al. 1992). The finding that Aβ42 is the most common isoform of Aβ in senile plaques led to development of assays for its quantification (Jarrett et al. 1993). The levels of CSF Aβ1-42 (Aβ42) are approximately 50 % lower in AD patients compared to controls, which has been shown with several different enzyme-linked immunosorbent assay (ELISA) methods (Sunderland et al. 2003; Blennow 2004). The most prevalent explanation for the reduced Aβ42 in CSF is that the sequestration into plaques in the brain leaves less available for diffusion into the CSF. Cerebral plaque load at autopsy correlates inversely with Aβ42 levels in lumbar CSF antemortem and ventricular CSF postmortem (Tapiola et al. 2009; Strozyk et al. 2003). Studies using PET for in vivo amyloid imaging have also found an inverse relationship between amyloid brain load and CSF Aβ42 (Fagan et al. 2006; Forsberg et al. 2008; Tolboom et al. 2009; Grimmer et al. 2009). Similar results have been obtained using the PET ligand 18FFDDNP, which is believed to bind to both plaques and tangles (Tolboom et al. 2009). These findings provide support of the notion that CSF Aβ42 is a measure of fibrillar Aβ42 and cerebral plaque load. Importantly, recent large studies have shown that the agreement between CSF Aβ42 and amyloid PET measurements is very high, with more than 90 % concordance, demonstrating that these methods give similar diagnostic information (Palmqvist et al. 2014).
2.2 P-tau
The amount of P-tau in CSF is commonly measured by ELISAs targeting tau phosphorylated at either threonine 181 or threonine 231 (Kohnken et al. 2000; Vanmechelen et al. 2000). These assays correlate well and show a similar association with AD (Hampel et al. 2004). Patients with AD have increased levels of CSF P-tau, in most studies around 200–300 % of control levels, and the levels in CSF have been shown to correlate with cerebral tangle pathology at autopsy (Blennow 2004; Tapiola et al. 2009; Buerger et al. 2006). In a study where cortical biopsies were taken from living patients with normal pressure hydrocephalus, a correlation between the amount of hyperphosphorylated tau in the biopsies and P-tau levels in CSF was found (Seppala et al. 2012). This supports the hypothesis that CSF P-tau reflects cerebral tangle pathology and the phosphorylation state of tau.
2.3 T-tau
CSF total tau corresponds to the intensity of neuronal and axonal damage and degeneration, which has been demonstrated in several studies. Levels increase after cardiac arrest, stroke, and brain trauma and are associated with amount of damaged tissue as well as clinical outcome (Hesse et al. 2001; Ost et al. 2006; Zetterberg et al. 2006; Rosen et al. 2014). In patients with Creutzfeldt-Jakob disease (CJD), a rapid rate of neurodegeneration is present, which is reflected in CSF by very high levels of T-tau (Otto et al. 1997). There are several isoforms and phosphorylation sites of the tau protein (Portelius et al. 2008). The ELISA assay most frequently used is capable of detecting all isoforms independent of phosphorylation state (Blennow et al. 1995). Studies have consistently shown that patients with AD have increased levels with about 300 % compared with normal controls (Sunderland et al. 2003; Blennow 2004). Also, it has been shown that levels of CSF T-tau antemortem correlate with the load of tangle pathology at autopsy, which indicates that release of tau from tangle-bearing neurons may contribute to levels of T-tau. In line with this, binding of the PET ligand 18FFDDNP has been shown to correlate with CSF T-tau levels (Tolboom et al. 2009).
3 Core Biomarkers in Various Stages of AD
3.1 Preclinical AD
Studies on preclinical AD have either been cross sectional, including patients with FAD, or longitudinal, with healthy elderly cohorts followed over time. The cross-sectional studies have calculated expected age of disease onset, which they relate biomarker levels to. One study showed that mutation carriers had elevated levels of CSF T-tau 15 years before expected symptom onset and reduced levels of CSF Aβ42 10 years before expected symptom onset (Bateman et al. 2012). Another study showed increased CSF Aβ42 in mutation carriers 20 years before estimated MCI onset (Reiman et al. 2012). Other studies that included cognitively normal mutation carriers closer to expected onset of AD have found increased levels of P-tau or T-tau, reduced Aβ42, and reduced Aβ42: Aβ40 ratio in CSF in these individuals compared with controls (Ringman et al. 2012; Moonis et al. 2005; Ringman et al. 2008).
The longitudinal studies have included cognitively healthy individuals, from which baseline biomarker levels have been related to future decrease in cognitive function or development of MCI or AD. CSF levels of Aβ42 alone or in combination with T-tau or P-tau have been associated with impending cognitive impairment (Gustafson et al. 2007; Fagan et al. 2007; Stomrud et al. 2007). Increased rates of brain atrophy have been found in cognitively normal individuals with low levels of CSF Aβ42 (Schott et al. 2010; Fagan et al. 2009; Fjell et al. 2010). Increased ratio of T-tau:Aβ42 or low levels of CSF Aβ42 have been found to predict conversion to MCI in cognitively normal individuals or AD in nondemented elderly individuals, respectively (Li et al. 2007; Skoog et al. 2003). One study found that the predictive ability of CSF Aβ42 for the development of MCI or AD in individuals with subjective complaints was superior to that of P-tau or T-tau (van Harten et al. 2012). However, long-term prospective CSF studies on cognitively normal individuals followed for 10–20 years until development of AD are missing. Also, the longitudinal studies are in fact cross sectional with respect to biomarker measurements, since baseline biomarker data has been correlated with longitudinal clinical outcome. True longitudinal studies with repeated biomarker measurements to determine the longitudinal biomarker trajectories are needed.
3.2 MCI Due to AD
Patients with MCI have a risk for AD over a 4.5-year period that is roughly tripled compared to cognitively normal controls (Bennett et al. 2002). The yearly progression rate from MCI to AD is around 10–15 % (Petersen 2004). Hence, long follow-up periods are required so that late converters are caught. Also, it is important to remember the heterogeneous nature of MCI, since affected individuals may progress to other dementias than AD, including vascular dementia (VaD), frontotemporal dementia (FTD), and dementia with Lewy bodies (DLB), or remain relatively stable in cognition (Petersen 2003). Patients with impending AD can be accurately distinguished from stable MCI patients by the CSF biomarker profile of low levels of Aβ42 in combination with high levels of P-tau and T-tau (Blennow and Hampel 2003). Different combinations of these biomarkers have been used in several studies to successfully predict AD in MCI patients (Hansson et al. 2006; Buchhave et al. 2012; Hertze et al. 2010; Visser et al. 2009; Shaw et al. 2009; Mattsson et al. 2009; Johansson et al. 2011a). CSF T-tau and P-tau levels have been associated with brain atrophy in early stage MCI/AD (Fagan et al. 2009). Also, the levels of these two biomarkers were higher in MCI patients with a more rapid progression to AD, indication that they may be related to disease progress (Buchhave et al. 2012).
3.3 AD with Dementia
The combination of Aβ42, P-tau, and T-tau can accurately distinguish AD patients from controls, with sensitivity and specificity over 80 % (Blennow 2004; Blennow and Hampel 2003). P-tau is the most AD specific of the biomarkers and may therefore be valuable when differentiating against other dementias (Hampel et al. 2010). Increased levels of P-tau have been found in patients with AD compared with patients suffering from FTD and VaD, DLB, and Parkinson disease with dementia (Hampel et al. 2004; Hall et al. 2012a). However, a large study on patients with AD as well as DLB, FTD, and VaD showed that an AD biomarker profile was present in a substantial part of the non-AD patients (Schoonenboom et al. 2012). Potential reasons for this overlap may be misdiagnosis or the presence of mixed dementias. Future autopsy studies will hopefully shed light on this issue. The presence of mixed pathologies increases with age, but the applicability of the core AD CSF biomarkers has been assessed in AD patients in different ages (Mattsson et al. 2012a). It was found that the accuracy decreased with age, but the combination of the biomarkers gave sufficiently strong results for the biomarkers to be used in old patients. Some studies have evaluated the longitudinal alterations of the core biomarkers in AD patients. Levels of Aβ42 and P-tau remain largely unaltered over time, while data concerning T-tau is more inconclusive (Blennow et al. 2007; Zetterberg et al. 2007; Mattsson et al. 2012b; Buchhave et al. 2009; Le Bastard et al. 2013). Some studies have found an increase of T-tau over time, while others have found stable levels. However, high levels of P-tau and T-tau have been associated with a more rapid disease progression (Samgard et al. 2010; Wallin et al. 2010; van Rossum et al. 2012).
3.4 Autopsy-Verified AD
The diagnostic performance of CSF AD biomarkers has been evaluated by performing subsequent autopsy of patients after death. They can with high sensitivity and specificity discriminate AD from cognitively normal elderly as well as patients with other dementias, such as FTD, DLB, and VaD (Sunderland et al. 2003; Shaw et al. 2009; Clark et al. 2003; Bian et al. 2008; Koopman et al. 2009). CSF biomarkers provide similar or better diagnostic accuracy compared with only using clinical criteria for diagnosis.
4 Aβ-Related Biomarkers
4.1 BACE1
The activity of BACE1 has been assessed in AD patients, but the results have not been consistent. Smaller studies have found increased BACE1 activity in CSF from AD patients (Holsinger et al. 2004; Holsinger et al. 2006; Verheijen et al. 2006). One study found that the activity was increased in patients with MCI and dementia due to AD compared with controls (Zetterberg et al. 2008). Another study found elevated levels in MCI patients, but not in AD patients (Mulder et al. 2010; Zhong et al. 2007). Finally, three studies found no differences between AD patients and controls (Mulder et al. 2010; Zhong et al. 2007; Rosén et al. 2012; Perneczky et al. 2014). However, in one of these studies, AD patients were stratified according to disease severity, which revealed that patients with moderate–severe dementia had lower levels of BACE1 activity than patients with mild dementia (Rosén et al. 2012). Although there is no clear-cut role for BACE1 activity in the diagnosis of AD, it may be useful in clinical trials on BACE1-inhibitors to monitor target engagement of the drug.
4.2 sAPPα/sAPPβ
The soluble ectodomain of APP (sAPP) is released when the protein is cut by α- or β-secretase. The levels of sAPPα and sAPPβ correlate very well in CSF in both AD patients and controls (Zetterberg et al. 2008). A large number of studies have not shown any differences in levels when comparing AD patients with controls (Hertze et al. 2010; Johansson et al. 2011a; Zetterberg et al. 2008; Perneczky et al. 2014; Rosen et al. 2012; Olsson et al. 2003). Some studies report elevated levels of sAPPβ in MCI patients compared to controls or in MCI patients with impending AD (Olsson et al. 2003; Perneczky et al. 2011). The latter differences were not seen in another study (Hertze et al. 2010). Studies using the core CSF AD biomarkers to characterize patients have found elevated levels of sAPPα and sAPPβ in patients with MCI or dementia that had a biomarker profile indicative of AD pathology, but with large overlaps between diagnostic groups (Lewczuk et al. 2010, 2012; Gabelle et al. 2010). The diagnostic value of sAPP levels appears low, but they may be utilized in clinical trials for studying effects on the APP metabolism, where a dose-dependent decrease in CSF sAPPβ indicates target engagement in clinical trials on BACE1 inhibitors (May et al. 2011).
4.3 Aβ Oligomers
The association between brain amyloid burden and neuronal loss is poor (Gomez-Isla et al. 1997). However, it has been shown that soluble oligomers of Aβ are capable of inhibiting long-term potentiation in vivo and cause abnormal tau phosphorylation and neuritic dystrophy (Walsh et al. 2002; Zempel et al. 2010; Jin et al. 2011; De Felice et al. 2008). Hence, many studies report attempts to measure the CSF levels of Aβ oligomers in patients with AD. This has proven to be difficult and studies have shown that the CSF levels of Aβ oligomers are very low, probably less than 1 % of total Aβ levels, which make reliable quantification challenging. Elevated oligomer levels have been found in the brains and CSF of AD patients (Bruggink et al. 2013; Shankar et al. 2008; Gao et al. 2010; Fukumoto et al. 2010; Georganopoulou et al. 2005; Pitschke et al. 1998). Increased levels were also reported in cognitively normal subjects with a CSF biomarker profile that indicated AD neuropathology (Handoko et al. 2013). Other studies have not been able to find altered levels of Aβ oligomers in CSF from AD patients (Bruggink and Jongbloed 2012; Santos et al. 2012; Yang et al. 2013). Apart from the difficulties of measuring minute amounts of Aβ oligomers in CSF samples, it is also possible that different assays measure different variants of Aβ oligomers, which might explain the divergent results. The studies provide little characterization of what the various assays are measuring.
5 Biomarkers for Other Pathologies
5.1 Blood-Brain Barrier Disturbances
The major biomarker for the integrity of the blood-brain barrier is the ratio between albumin measured in CSF and blood. This albumin ratio is typically normal in AD patients but tends to be elevated in patients with cerebral small vessel disease (Blennow et al. 1990; Wallin et al. 1999). An increased ratio may also be found in Lyme disease (neuroborreliosis), together with findings such as monocytosis and signs of immunoglobulin production in the CSF (Tumani et al. 1995). New potential biomarkers of the blood-brain barrier that need further verification include secretory Ca2+-dependent phospholipase A2 activity and antithrombin III (Chalbot et al. 2010; Zetterberg et al. 2009).
5.2 Neurofilament Light (NFL) Protein
NFL is mainly present in large-caliber myelinated axons, and increased levels are seen in conditions with subcortical axonal degeneration, such as cerebral small vessel disease, FTD, and human immunodeficiency virus (HIV)-associated dementia (Rosengren et al. 1999; Agren-Wilsson et al. 2007; Wallin and Sjogren 2001; de Jong et al. 2007; Landqvist Waldo et al. 2013; Gisslen et al. 2007). It may thus be of value in the differential diagnostics of AD. The simultaneous finding of elevated T-tau and NFL levels in CSF indicates mixed forms of AD and cerebrovascular disease, which appears to be very common in unselected patients undergoing evaluation because of a suspected neurodegenerative disease (Skillback et al. 2013).
5.3 Inflammatory, Glial, and Oxidative Stress Biomarkers
Neuroinflammation is a nonspecific feature of AD, and microglial cells can be found around senile plaques. In the 1990s and early 2000s, several studies reporting alterations in different inflammatory markers in CSF of AD patients (e.g., α1-antichymotrypsin, isoprostane, the interleukins, tumor necrosis factor α, interferon-gamma, complement C1q, and transforming growth factor β) were published (Craig-Schapiro et al. 2009; Zetterberg et al. 2004). The results have though been very inconsistent. A meta-analysis of cytokines in AD in 2010 showed great diversity in the study results (Swardfager et al. 2010). Reasons for discrepancies could include methodological differences (e.g., in the procedures for CSF collection and processing, assay differences, and criteria used for subject ascertainment), prevalence of comorbidities in the studied cohorts, and methods of diagnosis.
A recently described mutation in the microglia-controlling triggering receptor expressed on myeloid cells-2 (TREM2) gene was associated with an increased risk of AD. This has increased the interest of the role of microglia in the development of AD. Microglia are the macrophages of the brain. The enzyme chitotriosidase is secreted by activated macrophages and its levels of which are increased in the lysosomal storage disorder Gaucher disease (Renkema et al. 1998; Hollak et al. 1994). Studies on AD patients have revealed increased levels in CSF, although with overlaps with control groups (Mattsson et al. 2011a; Watabe-Rudolph et al. 2012; Rosén et al. 2014). A glycoprotein that has great homology with chitotriosidase but lacks its enzymatic activity is YKL-40 (Hakala et al. 1993). It is present in both microglial cells and astrocytes, and increased levels have been found in AD patients compared with controls (Rosén et al. 2014; Craig-Schapiro et al. 2010; Perrin et al. 2011; Olsson et al. 2013). One study did not find altered levels in AD patients compared with controls (Mattsson et al. 2011a).
A degree of oxidative stress is present in brains of AD patients and contributes to neuronal damage. Free radicals can cause lipid peroxidation, a feature that may be studied using biomarkers. A compound named isoprostane is produced by free radical-dependent peroxidation of arachidonic acid (Morrow and Roberts 1997). A certain subset, called F2-isoprostane, has been found in increased levels in CSF from AD patients (Montine et al. 1999; Pratico et al. 2000; Montine et al. 2001; Montine et al. 2007). Elevated levels are also reported among MCI patients with impending AD as well as asymptomatic patients with FAD-causing mutations (Ringman et al. 2008; Brys and Pirraglia 2007).
5.4 Synaptic Biomarkers
Loss of synapses correlates with decrease in neurocognitive function in AD patients (Terry et al. 1991). Biomarkers that reflect this pathology would therefore be desirable. Synaptic proteins such as synaptotagmin, growth-associated protein (GAP-43), synaptosomal-associated protein (SNAP-25), rab3a, and neurogranin have been identified in human CSF, and elevated CSF levels of neurogranin have been reported in both MCI and AD (Davidsson et al. 1999; Thorsell et al. 2010). More research is needed to determine the biomarker potential of synaptic proteins in the CSF.
6 Standardization of Biomarkers
The core CSF AD biomarkers have a high diagnostic accuracy for AD, especially in monocenter studies (Andreasen et al. 2001; Tabaraud et al. 2012; Johansson et al. 2011b). However, there is a large variability in measurements between centers and laboratories (Mattsson et al. 2011b). Standardization of pre-analytical and analytical factors is therefore needed before the biomarkers can be implemented in clinical practice. The Alzheimer’s Association has launched a Quality Control Program for CSF biomarkers with the aim of monitoring longitudinal variations and measurements between laboratories (Mattsson et al. 2011b). There are also several other ongoing initiatives, such as the Global Biomarker Standardization Consortium, the CSF-Proteins Working Group of International Federation of Clinical Chemistry and Laboratory Medicine, and the BIOMARKAPD project of the EU Joint Programme in Neurodegenerative Disease Research, that strive towards biomarker standardization (Carrillo et al. 2013). An important step in these standardization efforts is the development of mass spectrometry–based techniques for matrix-independent absolute quantification of Aβ42 in CSF. The first fully validated candidate reference measurement procedure for CSF Aβ42 based on single reaction monitoring (SRM) mass spectrometry has recently been published (Leinenbach et al. 2014). This type of techniques will serve to harmonize different immunoassays with the aim to make uniform cutoff levels across different laboratories.
7 CSF Biomarkers in Clinical Research
The CSF biomarkers reviewed above play several important roles in clinical research on AD. They may be used as inclusion criteria in clinical trials of disease-modifying anti-AD drug candidates to verify that the included patients have the pathological changes against which the drug is targeted (Blennow et al. 2010). They may also be used as pharmacodynamic markers or markers of target engagement to test if the drug had the desired biochemical effect in patients on active treatment (Hampel et al. 2014). The markers may also be used in longitudinal studies of healthy volunteers and patients in different stages of AD to learn more about the time course of the different pathogenic processes in AD (Blennow et al. 2010). As an example, proteins secreted into the CSF from activated microglia could be used for determining the role of microglial activation in the AD process. If microglial activation is involved in the disease process and precedes neurodegeneration, a prediction would be that patients on route to AD first drop in CSF Aβ42 (as a sign of Aβ buildup in the brain), then increase in markers of microglial activation, which ultimately is followed by cognitive symptoms and rise in CSF tau (as a sign of neurodegeneration). If microglial activation is a phenomenon downstream of neurodegeneration, such biomarker signals would appear after the rise in CSF tau. Finally, biomarkers for AD-related pathophysiological processes have also proven useful as quantitative traits for genetic analyses (Cruchaga et al. 2013; Andreasson et al. 2014).
8 CSF Biomarkers in Other Neurodegenerative Diseases
Pathologies relating to more than one neurodegenerative disorder are not an uncommon finding in postmortem brains. One autopsy study on brains of patients who had a clinical diagnosis of AD found that only 13.6 % of them had pure AD neuropathology, while the others displayed concomitant pathologies such as DLB and TDP (Toledo et al. 2013). This can have an impact in treatment studies targeting a certain pathology, since unknown pathologies may be affecting the outcome. Hence, it is important to find accurate biomarkers relating to pathologies from other diseases than AD.
In the brains of FTD patients, common findings are the neuronal inclusions of tau, TDP-43, or FUS protein (Seelaar et al. 2011). It is a heterogeneous disorder with around one third of the patients having an autosomal dominant variant with mutations in progranulin, microtubule-associated protein tau, or C9orf72. The search for CSF biomarkers for FTD has had limited success. TDP-43 has been measured in the CSF of FTD patients, but appears to originate mainly from blood and be of minor diagnostic importance (Feneberg et al. 2014). Patients with FTD typically have normal or mildly elevated levels of T-tau, but the use of T-tau to distinguish between AD and FTD only gives sensitivity and specificity figures around 80 % (Hampel and Teipel 2004). However, FTD patients have normal levels of P-tau, which can improve the diagnostic separation (Hampel et al. 2004). Further, FTD goes with increased CSF levels of NFL (de Jong et al. 2007).
Patients with DLB and PD belong to a group of diseases called synucleinopathies, based on the findings of α-synuclein in the Lewy bodies that constitute the pathologic hallmark of the diseases. Efforts have been made to quantify α-synuclein in CSF to find a diagnostic biomarker. Lower CSF levels of α-synuclein have been found in patients suffering from α-synucleinopathies (van Dijk et al. 2014; Hong et al. 2010; Mollenhauer et al. 2011; Shi et al. 2011; Hall et al. 2012b; Kasuga et al. 2010), although not in all studies (Spies et al. 2009; Reesink et al. 2010; Noguchi-Shinohara et al. 2009). Altogether, the levels of α-synuclein seem to be reduced in patients with α-synucleinopathies, but with overlap between diagnostic groups. The use of CSF α-synuclein as a biomarker for PD and DLB is also complicated by the finding that α-synuclein seems to reflect neuronal degeneration, with a very marked increase in disorders with marked neuronal loss, such as CJD (Mollenhauer et al. 2008). DLB patients have decreased levels of Aβ42 together with normal or only slightly elevated levels of T-tau in CSF (Parnetti et al. 2008; Zetterberg et al. 2010). Also here, P-tau may be utilized for increased discriminatory power against AD (Parnetti et al. 2008; Vanmechelen et al. 2001).
Due to the heterogenic nature of VaD and also the high degree of uncertainty in the clinical diagnosis of VaD, especially to exclude that a patient fulfilling the clinical criteria for VaD does not have concomitant AD pathology, it is difficult to make definite statements about CSF biomarker changes in patients suffering from this disorder (Roh and Lee 2014). However, findings of an increase in the CSF/serum albumin ratio and an increased CSF NFL level in a patient with a clinical picture suggestive of VaD add support to this diagnosis, while concomitant findings of low CSF Aβ42 and P-tau support a diagnosis of mixed AD/VaD (Blennow et al. 1990; Wallin et al. 1999; Skillback et al. 2013; Sjogren et al. 2001).
As mentioned above, patients with CJD have very high CSF levels of T-tau. As they tend to have normal or slightly elevated CSF levels of P-tau, the ratio of P-tau and T-tau may be used to differentiate CJD from AD (Riemenschneider et al. 2003; Skillback et al. 2014). Indeed, the CJD biomarker profile (T-tau >1,400 ng/L and T-tau/P-tau ratio >25) shows a very high positive likelihood ratio (LR+) for CJD, both in the differential diagnosis against AD (LR + 197) and against other dementias (LR + 109) (Skillback et al. 2014).
9 Summary
Three CSF biomarkers reflect the core pathological features of AD: T-tau (neurodegeneration), P-tau (tau hyperphosphorylation and tangle formation), and Aβ42 (plaque pathology). According to revised clinical criteria, these markers may help diagnosing AD also in pre-dementia stages of the disease. At present, their most obvious utility is in clinical trials of novel disease-modifying treatments against AD. In the future, they may help in selecting the right treatment for individual patients by making it possible to assess what molecular pathology that is most likely to cause the patient’s symptoms. Research is currently identifying and validating biomarkers for additional pathophysiological processes, including microglial activation and synapse loss.
References
Agren-Wilsson A, Lekman A, Sjoberg W et al (2007) CSF biomarkers in the evaluation of idiopathic normal pressure hydrocephalus. Acta Neurol Scand 116(5):333–339
Ahn HJ, Seo SW, Chin J et al (2011) The cortical neuroanatomy of neuropsychological deficits in mild cognitive impairment and Alzheimer's disease: a surface-based morphometric analysis. Neuropsychologia 49(14):3931–3945
Albert MS, DeKosky ST, Dickson D et al (2011) The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7(3):270–279
Alzheimer A (1987) About a peculiar disease of the cerebral cortex. By Alois Alzheimer, 1907 (Translated by L. Jarvik and H. Greenson). Alzheimer Dis Assoc Disord 1(1):3–8
Andreasen N, Minthon L, Davidsson P et al (2001) Evaluation of CSF-tau and CSF-Abeta42 as diagnostic markers for Alzheimer disease in clinical practice. Arch Neurol 58(3):373–379
Andreasson U, Lautner R, Schott JM et al (2014) CSF biomarkers for Alzheimer’s pathology and the effect size of APOE varepsilon4. Mol Psychiatry 19(2):148–149
Bateman RJ, Xiong C, Benzinger TL et al (2012) Clinical and biomarker changes in dominantly inherited Alzheimer’s disease. N Engl J Med 367(9):795–804
Bennett DA, Wilson RS, Schneider JA et al (2002) Natural history of mild cognitive impairment in older persons. Neurology 59(2):198–205
Bian H, Van Swieten JC, Leight S et al (2008) CSF biomarkers in frontotemporal lobar degeneration with known pathology. Neurology 70(19 Pt 2):1827–1835
Blennow K (2004) Cerebrospinal fluid protein biomarkers for Alzheimer’s disease. NeuroRx 1(2):213–225
Blennow K, Hampel H (2003) CSF markers for incipient Alzheimer’s disease. Lancet Neurol 2(10):605–613
Blennow K, Wallin A, Fredman P, Karlsson I, Gottfries CG, Svennerholm L (1990) Blood-brain barrier disturbance in patients with Alzheimer’s disease is related to vascular factors. Acta Neurol Scand 81(4):323–326
Blennow K, Wallin A, Agren H, Spenger C, Siegfried J, Vanmechelen E (1995) Tau protein in cerebrospinal fluid: a biochemical marker for axonal degeneration in Alzheimer disease? Mol Chem Neuropathol 26(3):231–245
Blennow K, Zetterberg H, Minthon L et al (2007) Longitudinal stability of CSF biomarkers in Alzheimer’s disease. Neurosci Lett 419(1):18–22
Blennow K, Hampel H, Weiner M, Zetterberg H (2010) Cerebrospinal fluid and plasma biomarkers in Alzheimer disease. Nat Rev Neurol 6(3):131–144
Bruggink KA, Jongbloed W, Biemans EA et al (2012) Amyloid-beta oligomer detection by enzyme-linked immunosorbent assay in cerebrospinal fluid and brain tissue. Anal Biochem 433(2):112–120
Bruggink KA, Jongbloed W, Biemans EA et al (2013) Amyloid-beta oligomer detection by ELISA in cerebrospinal fluid and brain tissue. Anal Biochem 433(2):112–120
Brys M, Pirraglia E, Rich K et al (2009) Prediction and longitudinal study of CSF biomarkers in mild cognitive impairment. Neurobiol Aging 30(5):682–690
Buchhave P, Blennow K, Zetterberg H et al (2009) Longitudinal study of CSF biomarkers in patients with Alzheimer’s disease. PLoS One 4(7):e6294
Buchhave P, Minthon L, Zetterberg H, Wallin AK, Blennow K, Hansson O (2012) Cerebrospinal fluid levels of beta-amyloid 1-42, but not of tau, are fully changed already 5 to 10 years before the onset of Alzheimer dementia. Arch Gen Psychiatry 69(1):98–106
Buerger K, Ewers M, Pirttila T et al (2006) CSF phosphorylated tau protein correlates with neocortical neurofibrillary pathology in Alzheimer’s disease. Brain 129(Pt 11):3035–3041
Carrillo MC, Blennow K, Soares H et al (2013) Global standardization measurement of cerebral spinal fluid for Alzheimer’s disease: an update from the Alzheimer’s Association Global Biomarkers Consortium. Alzheimers Dement 9(2):137–140
Chalbot S, Zetterberg H, Blennow K, Fladby T, Grundke-Iqbal I, Iqbal K (2010) Cerebrospinal fluid secretory Ca2+-dependent phospholipase A2 activity: a biomarker of blood-cerebrospinal fluid barrier permeability. Neurosci Lett 478(3):179–183
Chartier-Harlin MC, Crawford F, Houlden H et al (1991) Early-onset alzheimer’s disease caused by mutations at codon 717 of the beta-amyloid precursor protein gene. Nature 353(6347):844–846
Clark CM, Xie S, Chittams J et al (2003) Cerebrospinal fluid tau and beta-amyloid: how well do these biomarkers reflect autopsy-confirmed dementia diagnoses? Arch Neurol 60(12):1696–1702
Craig-Schapiro R, Fagan AM, Holtzman DM (2009) Biomarkers of Alzheimer’s disease. Neurobiol Dis 35(2):128–140
Craig-Schapiro R, Perrin RJ, Roe CM et al (2010) YKL-40: a novel prognostic fluid biomarker for preclinical Alzheimer’s disease. Biol Psychiatry 68(10):903–912
Cruchaga C, Kauwe JS, Harari O et al (2013) GWAS of cerebrospinal fluid tau levels identifies risk variants for Alzheimer’s disease. Neuron 78(2):256–268
Das P, Murphy MP, Younkin LH, Younkin SG, Golde TE (2001) Reduced effectiveness of Abeta1-42 immunization in APP transgenic mice with significant amyloid deposition. Neurobiol Aging 22(5):721–727
Davidsson P, Puchades M, Blennow K (1999) Identification of synaptic vesicle, pre- and postsynaptic proteins in human cerebrospinal fluid using liquid-phase isoelectric focusing. Electrophoresis 20(3):431–437
De Felice FG, Wu D, Lambert MP et al (2008) Alzheimer’s disease-type neuronal tau hyperphosphorylation induced by A beta oligomers. Neurobiol Aging 29(9):1334–1347
de Jong D, Jansen RW, Pijnenburg YA et al (2007) CSF neurofilament proteins in the differential diagnosis of dementia. J Neurol Neurosurg Psychiatry 78(9):936–938
Fagan AM, Mintun MA, Mach RH et al (2006) Inverse relation between in vivo amyloid imaging load and cerebrospinal fluid Abeta42 in humans. Ann Neurol 59(3):512–519
Fagan AM, Roe CM, Xiong C, Mintun MA, Morris JC, Holtzman DM (2007) Cerebrospinal fluid tau/beta-amyloid(42) ratio as a prediction of cognitive decline in nondemented older adults. Arch Neurol 64(3):343–349
Fagan AM, Head D, Shah AR et al (2009) Decreased cerebrospinal fluid Abeta(42) correlates with brain atrophy in cognitively normal elderly. Ann Neurol 65(2):176–183
Feneberg E, Steinacker P, Lehnert S et al (2014) Limited role of free TDP-43 as a diagnostic tool in neurodegenerative diseases. Amyotroph Lateral Scler Frontotemporal Degener 15:351–356
Fjell AM, Walhovd KB, Fennema-Notestine C et al (2010) Brain atrophy in healthy aging Is related to CSF levels of A{beta}1-42. Cereb Cortex 20:2069–2079
Forsberg A, Engler H, Almkvist O et al (2008) PET imaging of amyloid deposition in patients with mild cognitive impairment. Neurobiol Aging 29(10):1456–1465
Fukumoto H, Tokuda T, Kasai T et al (2010) High-molecular-weight beta-amyloid oligomers are elevated in cerebrospinal fluid of Alzheimer patients. FASEB J 24(8):2716–2726
Gabelle A, Roche S, Geny C et al (2010) Correlations between soluble alpha/beta forms of amyloid precursor protein and Abeta38, 40, and 42 in human cerebrospinal fluid. Brain Res 1357:175–183
Gao CM, Yam AY, Wang X et al (2010) Abeta40 oligomers identified as a potential biomarker for the diagnosis of Alzheimer’s disease. PLoS One 5(12):e15725
Garcia-Alloza M, Subramanian M, Thyssen D et al (2009) Existing plaques and neuritic abnormalities in APP:PS1 mice are not affected by administration of the gamma-secretase inhibitor LY-411575. Mol Neurodegener 4:19
Georganopoulou DG, Chang L, Nam JM et al (2005) Nanoparticle-based detection in cerebral spinal fluid of a soluble pathogenic biomarker for Alzheimer’s disease. Proc Natl Acad Sci U S A 102(7):2273–2276
Gisslen M, Hagberg L, Brew BJ, Cinque P, Price RW, Rosengren L (2007) Elevated cerebrospinal fluid neurofilament light protein concentrations predict the development of AIDS dementia complex. J Infect Dis 195(12):1774–1778
Goedert M, Spillantini MG, Potier MC, Ulrich J, Crowther RA (1989) Cloning and sequencing of the cDNA encoding an isoform of microtubule-associated protein tau containing four tandem repeats: differential expression of tau protein mRNAs in human brain. Embo J 8(2):393–399
Gomez-Isla T, Hollister R, West H et al (1997) Neuronal loss correlates with but exceeds neurofibrillary tangles in Alzheimer’s disease. Ann Neurol 41(1):17–24
Grimmer T, Riemenschneider M, Forstl H et al (2009) Beta amyloid in Alzheimer’s disease: increased deposition in brain is reflected in reduced concentration in cerebrospinal fluid. Biol Psychiatry 65(11):927–934
Grundke-Iqbal I, Iqbal K, Tung YC, Quinlan M, Wisniewski HM, Binder LI (1986) Abnormal phosphorylation of the microtubule-associated protein tau (tau) in Alzheimer cytoskeletal pathology. Proc Natl Acad Sci U S A 83(13):4913–4917
Gustafson DR, Skoog I, Rosengren L, Zetterberg H, Blennow K (2007) Cerebrospinal fluid beta-amyloid 1-42 concentration may predict cognitive decline in older women. J Neurol Neurosurg Psychiatry 78(5):461–464
Hakala BE, White C, Recklies AD (1993) Human cartilage gp-39, a major secretory product of articular chondrocytes and synovial cells, is a mammalian member of a chitinase protein family. J Biol Chem 268(34):25803–25810
Hall S, Ohrfelt A, Constantinescu R et al (2012a) Accuracy of a panel of 5 cerebrospinal fluid biomarkers in the differential diagnosis of patients with dementia and/or parkinsonian disorders. Arch Neurol 69(11):1445–1452
Hall S, Ohrfelt A, Constantinescu R et al (2012b) Accuracy of a panel of 5 cerebrospinal fluid biomarkers in the differential diagnosis of patients with dementia and/or parkinsonian disorders. Arch Neurol 69:1445–1452, 1–8
Hampel H, Teipel SJ (2004) Total and phosphorylated tau proteins: evaluation as core biomarker candidates in frontotemporal dementia. Dement Geriatr Cogn Disord 17(4):350–354
Hampel H, Buerger K, Zinkowski R et al (2004) Measurement of phosphorylated tau epitopes in the differential diagnosis of Alzheimer disease: a comparative cerebrospinal fluid study. Arch Gen Psychiatry 61(1):95–102
Hampel H, Blennow K, Shaw LM, Hoessler YC, Zetterberg H, Trojanowski JQ (2010) Total and phosphorylated tau protein as biological markers of Alzheimer’s disease. Exp Gerontol 45(1):30–40
Hampel H, Lista S, Teipel SJ et al (2014) Perspective on future role of biological markers in clinical therapy trials of Alzheimer’s disease: a long-range point of view beyond 2020. Biochem Pharmacol 88(4):426–449
Handoko M, Grant M, Kuskowski M et al (2013) Correlation of specific amyloid-beta oligomers with tau in cerebrospinal fluid from cognitively normal older adults. JAMA Neurol 1–6
Hansson O, Zetterberg H, Buchhave P, Londos E, Blennow K, Minthon L (2006) Association between CSF biomarkers and incipient Alzheimer’s disease in patients with mild cognitive impairment: a follow-up study. Lancet Neurol 5(3):228–234
Hardy J (2009) The amyloid hypothesis for Alzheimer’s disease: a critical reappraisal. J Neurochem 110(4):1129–1134
Hardy JA, Higgins GA (1992) Alzheimer’s disease: the amyloid cascade hypothesis. Science 256(5054):184–185
Hertze J, Minthon L, Zetterberg H, Vanmechelen E, Blennow K, Hansson O (2010) Evaluation of CSF biomarkers as predictors of Alzheimer’s disease: a clinical follow-up study of 4.7 years. J Alzheimers Dis 21(4):1119–1128
Hesse C, Rosengren L, Andreasen N et al (2001) Transient increase in total tau but not phospho-tau in human cerebrospinal fluid after acute stroke. Neurosci Lett 297(3):187–190
Hollak CE, van Weely S, van Oers MH, Aerts JM (1994) Marked elevation of plasma chitotriosidase activity. A novel hallmark of Gaucher disease. J clin invest 93(3):1288–1292
Holsinger RM, McLean CA, Collins SJ, Masters CL, Evin G (2004) Increased beta-secretase activity in cerebrospinal fluid of Alzheimer’s disease subjects. Ann Neurol 55(6):898–899
Holsinger RM, Lee JS, Boyd A, Masters CL, Collins SJ (2006) CSF BACE1 activity is increased in CJD and Alzheimer disease versus [corrected] other dementias. Neurology 67(4):710–712
Hong Z, Shi M, Chung KA et al (2010) DJ-1 and alpha-synuclein in human cerebrospinal fluid as biomarkers of Parkinson’s disease. Brain 133(Pt 3):713–726
Jack CR Jr, Knopman DS, Jagust WJ et al (2010) Hypothetical model of dynamic biomarkers of the Alzheimer’s pathological cascade. Lancet Neurol 9(1):119–128
Jack CR Jr, Albert MS, Knopman DS et al (2011) Introduction to the recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7(3):257–262
Jarrett JT, Berger EP, Lansbury PT Jr (1993) The carboxy terminus of the beta amyloid protein is critical for the seeding of amyloid formation: implications for the pathogenesis of Alzheimer’s disease. Biochemistry 32(18):4693–4697
Jin M, Shepardson N, Yang T, Chen G, Walsh D, Selkoe DJ (2011) Soluble amyloid beta-protein dimers isolated from Alzheimer cortex directly induce Tau hyperphosphorylation and neuritic degeneration. Proc Natl Acad Sci U S A 108(14):5819–5824
Johansson P, Mattsson N, Hansson O et al (2011a) Cerebrospinal fluid biomarkers for Alzheimer’s disease: diagnostic performance in a homogeneous mono-center population. J Alzheimers Dis 24(3):537–546
Johansson P, Johansson JO, Labrie F et al (2011b) Mild dementia is associated with increased adrenal secretion of cortisol and precursor sex steroids in women. Clin Endocrinol (Oxf) 75(3):301–308
Karran E, Mercken M, De Strooper B (2011) The amyloid cascade hypothesis for Alzheimer’s disease: an appraisal for the development of therapeutics. Nat Rev Drug Discov 10(9):698–712
Kasuga K, Tokutake T, Ishikawa A et al (2010) Differential levels of alpha-synuclein, beta-amyloid42 and tau in CSF between patients with dementia with Lewy bodies and Alzheimer’s disease. J Neurol Neurosurg Psychiatry 81(6):608–610
Kohnken R, Buerger K, Zinkowski R et al (2000) Detection of tau phosphorylated at threonine 231 in cerebrospinal fluid of Alzheimer’s disease patients. Neurosci Lett 287(3):187–190
Koopman K, Le Bastard N, Martin JJ, Nagels G, De Deyn PP, Engelborghs S (2009) Improved discrimination of autopsy-confirmed Alzheimer’s disease (AD) from non-AD dementias using CSF P-tau(181P). Neurochem Int 55(4):214–218
Landqvist Waldo M, Frizell Santillo A, Passant U et al (2013) Cerebrospinal fluid neurofilament light chain protein levels in subtypes of frontotemporal dementia. BMC Neurol 13:54
Le Bastard N, Aerts L, Sleegers K et al (2013) Longitudinal stability of cerebrospinal fluid biomarker levels: fulfilled requirement for pharmacodynamic markers in Alzheimer’s disease. J Alzheimers Dis 33(3):807–822
Leinenbach A, Pannee J, Dülffer T et al (2014) Mass spectrometry-based candidate reference measurement procedure for quantification of Aβ42 in cerebrospinal fluid. Clin Chem 60:987–994
Levites Y, Das P, Price RW et al (2006) Anti-Abeta42- and anti-Abeta40-specific mAbs attenuate amyloid deposition in an Alzheimer disease mouse model. J Clin Invest 116(1):193–201
Lewczuk P, Kamrowski-Kruck H, Peters O et al (2010) Soluble amyloid precursor proteins in the cerebrospinal fluid as novel potential biomarkers of Alzheimer’s disease: a multicenter study. Mol Psychiatry 15(2):138–145
Lewczuk P, Popp J, Lelental N et al (2012) Cerebrospinal fluid soluble amyloid-beta protein precursor as a potential novel biomarkers of Alzheimer’s disease. J Alzheimers Dis 28(1):119–125
Li G, Sokal I, Quinn JF et al (2007) CSF tau/Abeta42 ratio for increased risk of mild cognitive impairment: a follow-up study. Neurology 69(7):631–639
Masters CL, Simms G, Weinman NA, Multhaup G, McDonald BL, Beyreuther K (1985) Amyloid plaque core protein in Alzheimer disease and down syndrome. Proc Natl Acad Sci U S A 82(12):4245–4249
Mattsson N, Zetterberg H, Hansson O et al (2009) CSF biomarkers and incipient Alzheimer disease in patients with mild cognitive impairment. JAMA 302(4):385–393
Mattsson N, Tabatabaei S, Johansson P et al (2011a) Cerebrospinal fluid microglial markers in Alzheimer’s disease: elevated chitotriosidase activity but lack of diagnostic utility. Neuromolecular Med 13(2):151–159
Mattsson N, Andreasson U, Persson S et al (2011b) The Alzheimer’s Association external quality control program for cerebrospinal fluid biomarkers. Alzheimers Dement 7(4):386–95 e6
Mattsson N, Rosen E, Hansson O et al (2012a) Age and diagnostic performance of Alzheimer disease CSF biomarkers. Neurology 78(7):468–476
Mattsson N, Portelius E, Rolstad S et al (2012b) Longitudinal cerebrospinal fluid biomarkers over four years in mild cognitive impairment. J Alzheimers Dis 30(4):767–778
May PC, Dean RA, Lowe SL et al (2011) Robust central reduction of amyloid-beta in humans with an orally available, non-peptidic beta-secretase inhibitor. J neurosci 31(46):16507–16516
McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM (1984) Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology 34(7):939–944
Mollenhauer B, Cullen V, Kahn I et al (2008) Direct quantification of CSF alpha-synuclein by ELISA and first cross-sectional study in patients with neurodegeneration. Exp Neurol 213(2):315–325
Mollenhauer B, Locascio JJ, Schulz-Schaeffer W, Sixel-Doring F, Trenkwalder C, Schlossmacher MG (2011) alpha-Synuclein and tau concentrations in cerebrospinal fluid of patients presenting with parkinsonism: a cohort study. Lancet Neurol 10(3):230–240
Montine TJ, Beal MF, Cudkowicz ME et al (1999) Increased CSF F2-isoprostane concentration in probable AD. Neurology 52(3):562–565
Montine TJ, Kaye JA, Montine KS, McFarland L, Morrow JD, Quinn JF (2001) Cerebrospinal fluid abeta42, tau, and f2-isoprostane concentrations in patients with Alzheimer disease, other dementias, and in age-matched controls. Arch Pathol Lab Med 125(4):510–512
Montine TJ, Quinn J, Kaye J, Morrow JD (2007) F(2)-isoprostanes as biomarkers of late-onset alzheimer’s disease. J Mol Neurosci 33(1):114–119
Moonis M, Swearer JM, Dayaw MP et al (2005) Familial Alzheimer disease: decreases in CSF Abeta42 levels precede cognitive decline. Neurology 65(2):323–325
Morrow JD, Roberts LJ (1997) The isoprostanes: unique bioactive products of lipid peroxidation. Prog Lipid Res 36(1):1–21
Mulder SD, van der Flier WM, Verheijen JH et al (2010) BACE1 activity in cerebrospinal fluid and its relation to markers of AD pathology. J Alzheimers Dis 20(1):253–260
Mullan M, Crawford F, Axelman K et al (1992) A pathogenic mutation for probable Alzheimer’s disease in the APP gene at the N-terminus of beta-amyloid. Nat Genet 1(5):345–347
Noguchi-Shinohara M, Tokuda T, Yoshita M et al (2009) CSF alpha-synuclein levels in dementia with Lewy bodies and Alzheimer’s disease. Brain Res 1251:1–6
Olsson A, Hoglund K, Sjogren M et al (2003) Measurement of alpha- and beta-secretase cleaved amyloid precursor protein in cerebrospinal fluid from Alzheimer patients. Exp Neurol 183(1):74–80
Olsson B, Hertze J, Lautner R et al (2013) Microglial markers are elevated in the prodromal phase of Alzheimer’s disease and vascular dementia. J Alzheimers Dis 33(1):45–53
Ost M, Nylen K, Csajbok L et al (2006) Initial CSF total tau correlates with 1-year outcome in patients with traumatic brain injury. Neurology 67(9):1600–1604
Otto M, Wiltfang J, Tumani H et al (1997) Elevated levels of tau-protein in cerebrospinal fluid of patients with Creutzfeldt-Jakob disease. Neurosci Lett 225(3):210–212
Palmqvist S, Zetterberg H, Blennow K et al (2014) Accuracy of brain amyloid detection in clinical practice using cerebrospinal fluid Aβ42: a cross-validation study against amyloid PET in non-demented individuals. JAMA Neurol 71:1282–1289
Parnetti L, Tiraboschi P, Lanari A et al (2008) Cerebrospinal fluid biomarkers in Parkinson’s disease with dementia and dementia with Lewy bodies. Biol Psychiatry 64(10):850–855
Perl DP (2010) Neuropathology of Alzheimer’s disease. Mt Sinai J Med 77(1):32–42
Perneczky R, Tsolakidou A, Arnold A et al (2011) CSF soluble amyloid precursor proteins in the diagnosis of incipient Alzheimer disease. Neurology 77(1):35–38
Perneczky R, Alexopoulos P, Alzheimer’s Disease Neuroimaging Initiative (2014) Cerebrospinal fluid BACE1 activity and markers of amyloid precursor protein metabolism and axonal degeneration in Alzheimer’s disease. Alzheimers Dement 10:S425–S429
Perrin RJ, Craig-Schapiro R, Malone JP et al (2011) Identification and validation of novel cerebrospinal fluid biomarkers for staging early Alzheimer’s disease. PLoS One 6(1):e16032
Petersen RC (2003) Mild cognitive impairment: aging to Alzheimer’s disease. Oxford University Press, New York
Petersen RC (2004) Mild cognitive impairment as a diagnostic entity. J Intern Med 256(3):183–194
Pitschke M, Prior R, Haupt M, Riesner D (1998) Detection of single amyloid beta-protein aggregates in the cerebrospinal fluid of Alzheimer’s patients by fluorescence correlation spectroscopy. Nat Med 4(7):832–834
Portelius E, Hansson SF, Tran AJ et al (2008) Characterization of tau in cerebrospinal fluid using mass spectrometry. J Proteome Res 7(5):2114–2120
Portelius E, Bogdanovic N, Gustavsson MK et al (2010) Mass spectrometric characterization of brain amyloid beta isoform signatures in familial and sporadic Alzheimer’s disease. Acta Neuropathol 120(2):185–193
Pratico D, Clark CM, Lee VM, Trojanowski JQ, Rokach J, FitzGerald GA (2000) Increased 8,12-iso-iPF2alpha-VI in Alzheimer’s disease: correlation of a noninvasive index of lipid peroxidation with disease severity. Ann Neurol 48(5):809–812
Raina P, Santaguida P, Ismaila A et al (2008) Effectiveness of cholinesterase inhibitors and memantine for treating dementia: evidence review for a clinical practice guideline. Ann Intern Med 148(5):379–397
Reesink FE, Lemstra AW, van Dijk KD et al (2010) CSF alpha-synuclein does not discriminate dementia with Lewy bodies from Alzheimer’s disease. J Alzheimers Dis 22(1):87–95
Reiman EM, Quiroz YT, Fleisher AS et al (2012) Brain imaging and fluid biomarker analysis in young adults at genetic risk for autosomal dominant Alzheimer’s disease in the presenilin 1 E280A kindred: a case-control study. Lancet Neurol 11(12):1048–1056
Renkema GH, Boot RG, Au FL et al (1998) Chitotriosidase, a chitinase, and the 39-kDa human cartilage glycoprotein, a chitin-binding lectin, are homologues of family 18 glycosyl hydrolases secreted by human macrophages. Eur J Biochem 251(1–2):504–509
Riemenschneider M, Wagenpfeil S, Vanderstichele H et al (2003) Phospho-tau/total tau ratio in cerebrospinal fluid discriminates Creutzfeldt-Jakob disease from other dementias. Mol Psychiatry 8(3):343–347
Ringman JM, Younkin SG, Pratico D et al (2008) Biochemical markers in persons with preclinical familial Alzheimer disease. Neurology 71(2):85–92
Ringman JM, Coppola G, Elashoff D et al (2012) Cerebrospinal fluid biomarkers and proximity to diagnosis in preclinical familial Alzheimer’s disease. Dement Geriatr Cogn Disord 33(1):1–5
Roh JH, Lee JH (2014) Recent updates on subcortical ischemic vascular dementia. J stroke 16(1):18–26
Rosén C, Andreasson U, Mattsson N et al (2012) Cerebrospinal fluid profiles of amyloid β-related biomarkers in Alzheimer’s disease. Neuromolecular Med 14(1):65–73
Rosen C, Andreasson U, Mattsson N et al (2012) Cerebrospinal fluid profiles of amyloid beta-related biomarkers in Alzheimer’s disease. Neuromolecular Med 14(1):65–73
Rosen C, Rosen H, Andreasson U et al (2014) Cerebrospinal fluid biomarkers in cardiac arrest survivors. Resuscitation 85(2):227–232
Rosén C, Andersson C, Andreasson U et al (2014) Increased levels of chitotriosidase and YKL-40 in CSF from patients with Alzheimer’s disease. Dement Geriatr Cogn Dis Extra 4:297–304
Rosengren LE, Karlsson JE, Sjogren M, Blennow K, Wallin A (1999) Neurofilament protein levels in CSF are increased in dementia. Neurology 52(5):1090–1093
Samgard K, Zetterberg H, Blennow K, Hansson O, Minthon L, Londos E (2010) Cerebrospinal fluid total tau as a marker of Alzheimer’s disease intensity. Int J Geriatr Psychiatry 25(4):403–410
Santos AN, Ewers M, Minthon L et al (2012) Amyloid-beta oligomers in cerebrospinal fluid are associated with cognitive decline in patients with Alzheimer’s disease. J Alzheimers Dis 29(1):171–176
Schoonenboom NS, Reesink FE, Verwey NA et al (2012) Cerebrospinal fluid markers for differential dementia diagnosis in a large memory clinic cohort. Neurology 78(1):47–54
Schott JM, Bartlett JW, Fox NC, Barnes J, Alzheimer’s Disease Neuroimaging Initiative Initiative (2010) Increased brain atrophy rates in cognitively normal older adults with low cerebrospinal fluid Abeta1-42. Ann Neurol 68(6):825–834
Seelaar H, Rohrer JD, Pijnenburg YA, Fox NC, van Swieten JC (2011) Clinical, genetic and pathological heterogeneity of frontotemporal dementia: a review. J Neurol Neurosurg Psychiatry 82(5):476–486
Selkoe DJ (2001) Alzheimer’s disease: genes, proteins, and therapy. Physiol Rev 81(2):741–766
Seppala TT, Nerg O, Koivisto AM et al (2012) CSF biomarkers for Alzheimer disease correlate with cortical brain biopsy findings. Neurology 78(20):1568–1575
Seubert P, Vigo-Pelfrey C, Esch F et al (1992) Isolation and quantification of soluble Alzheimer’s beta-peptide from biological fluids. Nature 359(6393):325–327
Shankar GM, Li S, Mehta TH et al (2008) Amyloid-beta protein dimers isolated directly from Alzheimer’s brains impair synaptic plasticity and memory. Nat Med 14(8):837–842
Shaw LM, Vanderstichele H, Knapik-Czajka M et al (2009) Cerebrospinal fluid biomarker signature in Alzheimer’s disease neuroimaging initiative subjects. Ann Neurol 65(4):403–413
Shi M, Bradner J, Hancock AM et al (2011) Cerebrospinal fluid biomarkers for Parkinson disease diagnosis and progression. Ann Neurol 69(3):570–580
Siemers ER (2009) How can we recognize “disease modification” effects? J Nutr Health Aging 13(4):341–343
Sjogren M, Blomberg M, Jonsson M et al (2001) Neurofilament protein in cerebrospinal fluid: a marker of white matter changes. J Neurosci Res 66(3):510–516
Skillback T, Zetterberg H, Blennow K, Mattsson N (2013) Cerebrospinal fluid biomarkers for Alzheimer disease and subcortical axonal damage in 5,542 clinical samples. Alzheimers Res Ther 5(5):47
Skillback T, Rosen C, Asztely F, Mattsson N, Blennow K, Zetterberg H (2014) Diagnostic performance of cerebrospinal fluid total tau and phosphorylated tau in Creutzfeldt-Jakob disease: results from the Swedish Mortality Registry. JAMA Neuro 71(4):476–483
Skoog I, Davidsson P, Aevarsson O, Vanderstichele H, Vanmechelen E, Blennow K (2003) Cerebrospinal fluid beta-amyloid 42 is reduced before the onset of sporadic dementia: a population-based study in 85-year-olds. Dement Geriatr Cogn Disord 15(3):169–176
Sperling RA, Aisen PS, Beckett LA et al (2011a) Toward defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 7(3):280–292
Sperling RA, Jack CR Jr, Aisen PS (2011b) Testing the right target and right drug at the right stage. Sci transl med 3(111):111cm33
Spies PE, Melis RJ, Sjogren MJ, Rikkert MG, Verbeek MM (2009) Cerebrospinal fluid alpha-synuclein does not discriminate between dementia disorders. J Alzheimers Dis 16(2):363–369
Spires-Jones TL, Stoothoff WH, de Calignon A, Jones PB, Hyman BT (2009) Tau pathophysiology in neurodegeneration: a tangled issue. Trends Neurosci 32(3):150–159
Stomrud E, Hansson O, Blennow K, Minthon L, Londos E (2007) Cerebrospinal fluid biomarkers predict decline in subjective cognitive function over 3 years in healthy elderly. Dement Geriatr Cogn Disord 24(2):118–124
Strozyk D, Blennow K, White LR, Launer LJ (2003) CSF Abeta 42 levels correlate with amyloid-neuropathology in a population-based autopsy study. Neurology 60(4):652–656
Sunderland T, Linker G, Mirza N et al (2003) Decreased beta-amyloid1-42 and increased tau levels in cerebrospinal fluid of patients with Alzheimer disease. Jama 289(16):2094–2103
Swardfager W, Lanctot K, Rothenburg L, Wong A, Cappell J, Herrmann N (2010) A meta-analysis of cytokines in Alzheimer’s disease. Biol Psychiatry 68(10):930–941
Tabaraud F, Leman JP, Milor AM et al (2012) Alzheimer CSF biomarkers in routine clinical setting. Acta Neurol Scand 125(6):416–423
Tapiola T, Alafuzoff I, Herukka SK et al (2009) Cerebrospinal fluid {beta}-amyloid 42 and tau proteins as biomarkers of Alzheimer-type pathologic changes in the brain. Arch Neurol 66(3):382–389
Terry RD, Masliah E, Salmon DP et al (1991) Physical basis of cognitive alterations in Alzheimer’s disease: synapse loss is the major correlate of cognitive impairment. Ann Neurol 30(4):572–580
Thorsell A, Bjerke M, Gobom J et al (2010) Neurogranin in cerebrospinal fluid as a marker of synaptic degeneration in Alzheimer’s disease. Brain Res 1362:13–22
Tolboom N, van der Flier WM, Yaqub M et al (2009) Relationship of cerebrospinal fluid markers to 11C-PiB and 18F-FDDNP binding. J nucl med 50(9):1464–1470
Toledo JB, Cairns NJ, Da X et al (2013) Clinical and multimodal biomarker correlates of ADNI neuropathological findings. Acta neuropathol Commun 1(1):65
Tumani H, Nolker G, Reiber H (1995) Relevance of cerebrospinal fluid variables for early diagnosis of neuroborreliosis. Neurology 45(9):1663–1670
van Dijk KD, Bidinosti M, Weiss A, Raijmakers P, Berendse HW, van de Berg WD (2014) Reduced alpha-synuclein levels in cerebrospinal fluid in Parkinson’s disease are unrelated to clinical and imaging measures of disease severity. Eur J Neurol 21(3):388–394
van Duijn CM, Hendriks L, Cruts M, Hardy JA, Hofman A, Van Broeckhoven C (1991) Amyloid precursor protein gene mutation in early-onset alzheimer’s disease. Lancet 337(8747):978
van Harten AC, Visser PJ, Pijnenburg YA et al (2013) Cerebrospinal fluid Abeta42 is the best predictor of clinical progression in patients with subjective complaints. Alzheimers Dement 9(5):481–487
van Rossum IA, Vos SJ, Burns L et al (2012) Injury markers predict time to dementia in subjects with MCI and amyloid pathology. Neurology 79(17):1809–1816
Vanmechelen E, Vanderstichele H, Davidsson P et al (2000) Quantification of tau phosphorylated at threonine 181 in human cerebrospinal fluid: a sandwich ELISA with a synthetic phosphopeptide for standardization. Neurosci Lett 285(1):49–52
Vanmechelen E, Van Kerschaver E, Blennow K, et al (2001) CSF-phospho-tau (181P) as a promising marker for discriminating Alzheimer’s disease from dementia with Lewy bodies, in alzheimer’s disease: advances in etiology, pathogenesis and therapeutics. John Wiley and Sons, England. pp 285–291
Verheijen JH, Huisman LG, van Lent N et al (2006) Detection of a soluble form of BACE-1 in human cerebrospinal fluid by a sensitive activity assay. Clin Chem 52(6):1168–1174
Visser PJ, Verhey F, Knol DL et al (2009) Prevalence and prognostic value of CSF markers of Alzheimer’s disease pathology in patients with subjective cognitive impairment or mild cognitive impairment in the DESCRIPA study: a prospective cohort study. Lancet Neurol 8(7):619–627
Wallin A, Sjogren M (2001) Cerebrospinal fluid cytoskeleton proteins in patients with subcortical white-matter dementia. Mech Ageing Dev 122(16):1937–1949
Wallin A, Blennow K, Rosengren L (1999) Cerebrospinal fluid markers of pathogenetic processes in vascular dementia, with special reference to the subcortical subtype. Alzheimer Dis Assoc Disord 13(Suppl 3):S102–S105
Wallin AK, Blennow K, Zetterberg H, Londos E, Minthon L, Hansson O (2010) CSF biomarkers predict a more malignant outcome in Alzheimer disease. Neurology 74(19):1531–1537
Walsh DM, Klyubin I, Fadeeva JV et al (2002) Naturally secreted oligomers of amyloid beta protein potently inhibit hippocampal long-term potentiation in vivo. Nature 416(6880):535–539
Watabe-Rudolph M, Song Z, Lausser L et al (2012) Chitinase enzyme activity in CSF is a powerful biomarker of Alzheimer disease. Neurology 78(8):569–577
Yang T, Hong S, O’Malley T, Sperling RA, Walsh DM, Selkoe DJ (2013) New ELISAs with high specificity for soluble oligomers of amyloid beta-protein detect natural Abeta oligomers in human brain but not CSF. Alzheimers Dement 9(2):99–112
Zempel H, Thies E, Mandelkow E, Mandelkow EM (2010) Abeta oligomers cause localized Ca(2+) elevation, missorting of endogenous Tau into dendrites, Tau phosphorylation, and destruction of microtubules and spines. J neurosci 30(36):11938–11950
Zetterberg H, Andreasen N, Blennow K (2004) Increased cerebrospinal fluid levels of transforming growth factor-beta1 in Alzheimer’s disease. Neurosci Lett 367(2):194–196
Zetterberg H, Hietala MA, Jonsson M et al (2006) Neurochemical aftermath of amateur boxing. Arch Neurol 63(9):1277–1280
Zetterberg H, Pedersen M, Lind K et al (2007) Intra-individual stability of CSF biomarkers for Alzheimer’s disease over two years. J Alzheimers Dis 12(3):255–260
Zetterberg H, Andreasson U, Hansson O et al (2008) Elevated cerebrospinal fluid BACE1 activity in incipient Alzheimer disease. Arch Neurol 65(8):1102–1107
Zetterberg H, Andreasson U, Blennow K (2009) CSF antithrombin III and disruption of the blood-brain barrier. J Clin Oncol 27(13):2302–2303; author reply 3–4
Zetterberg H, Mattsson N, Blennow K (2010) Cerebrospinal fluid analysis should be considered in patients with cognitive problems. Int J Alzheimers Dis 2010:163065
Zhong Z, Ewers M, Teipel S et al (2007) Levels of beta-secretase (BACE1) in cerebrospinal fluid as a predictor of risk in mild cognitive impairment. Arch Gen Psychiatry 64(6):718–726
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Rosén, C., Zetterberg, H., Blennow, K. (2015). Alzheimer’s Disease and Other Neurodegenerative Disorders. In: Deisenhammer, F., Sellebjerg, F., Teunissen, C., Tumani, H. (eds) Cerebrospinal Fluid in Clinical Neurology. Springer, Cham. https://doi.org/10.1007/978-3-319-01225-4_20
Download citation
DOI: https://doi.org/10.1007/978-3-319-01225-4_20
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-01224-7
Online ISBN: 978-3-319-01225-4
eBook Packages: MedicineMedicine (R0)