Abstract
The assessment of intrathecally synthesised immunoglobulin is an important part of routine cerebrospinal fluid (CSF) analysis. Immunoglobulins can be detected in normal CSF and are derived from plasma. The appearance of immunoglobulins in normal CSF is readily explained by size-dependent diffusion across blood-CSF barriers, and their concentrations increase with the general increase in CSF protein concentrations observed in a wide range of neurological diseases. Therefore, methods that take the normal diffusion of immunoglobulins into account are needed for quantitative assessment of intrathecal immunoglobulin synthesis. Intrathecally synthesised immunoglobulins are usually of restricted clonality, and electrophoresis-based methods can be used for detecting this in the form of oligoclonal bands. These methods depend on comparing paired CSF and blood samples. Qualitative analyses for the assessment of intrathecally synthesised oligoclonal bands are more technically demanding, but are more sensitive for the detection of intrathecal immunoglobulin synthesis, and are less susceptible to artefacts induced by blood-CSF barrier disturbances than quantitative methods. The same general principles apply both for the detection of total intrathecal immunoglobulin synthesis and for the detection of specific antibody responses in infectious or autoimmune conditions.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Myelin Basic Protein
- Oligoclonal Band
- Somatic Hypermutation
- Intrathecal Synthesis
- Eosinophilic Meningitis
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
The mammalian immune system has evolved to protect against infections against a plethora of infectious agents and employs a wide range of responses to protect the host against bacterial, viral and parasitic infections. The immune system is also involved in inflammatory responses to tissue damage and in the pathogenesis of autoimmune and autoinflammatory diseases. Basically, the immune system can be divided into an innate and an adaptive part (Paul 2008). The innate immune system comprises granulocytes; mononuclear phagocytes such as monocytes, macrophages and microglia; and dendritic cells which are specialised antigen-presenting cells. These cells express a wide range of molecules including pattern recognition receptors for molecules associated with pathogens (Broz and Monack 2013). In addition, humoral factors, including pentraxins such as the acute-phase proteins C-reactive protein and serum amyloid, complement proteins, and the coagulation and kinin system are part of the innate immune system (Shishido et al. 2012).
The adaptive immune system comprises B cells and T cells, which are lymphocytes developing in the bone marrow and thymus (Paul 2008). Each newly developed B or T cell expresses a unique antigen receptor in the form of an immunoglobulin or a T-cell antigen receptor. The development of unique antigen receptors is the result of genetic recombination combined with stochastic addition of single nucleotides to the receptor-encoding DNA sequence. Developing lymphocytes undergo positive selection processes to ensure that they express functional antigen receptor molecules. This is followed by negative selection, where potentially harmful, autoreactive cells are pruned from the developing lymphocyte repertoire.
Following the activation of an antigen-specific lymphocyte in secondary lymphatic tissue, e.g. lymph node or spleen, it proliferates vigorously. This initial clonal expansion is followed by the differentiation of cells into various effector cell types and memory cells, which are long-living cells that continue to recirculate in the body or remain in peripheral tissues after the initial immune response, thus ensuring a more rapid and efficient immune response upon a second encounter with an infectious agent (Heyzer-Williams and Heyzer-Williams 2005; Sprent and Surh 2011).
2 The Humoral Immune Response
2.1 B-Cell Development and Activation
Humoral immune responses depend on the primary activation of antigen-reactive B cells, which is initiated by the binding of antigen to immunoglobulins on the B-cell surface (Harwood and Batista 2010). This activates a signalling cascade involving protein kinases, the induction of second messenger molecules and gene expression (Kurosaki et al. 2010). In addition, immunoglobulins with their bound antigen are internalised, and the antigen is processed by proteases in endosomes. This is followed by the binding of peptide fragments of the antigen to major histocompatibility class II molecules (human leucocyte antigen or HLA molecules in humans), which are subsequently expressed on the cell surface (Neefjes et al. 2011). This allows interactions between antigen-specific CD4 T cells and antigen-specific B cells, resulting in the activation of CD4 T cells with specificity for the same antigen that initially activated the B cell. A hallmark of the humoral immune response is the development of plasma cells secreting high-affinity antibodies that are class switched from the initial IgM isotype to other isotypes (see below) and the development of a long-living pool of memory B cells. Although T-cell-independent B-cell responses can provide some protection early in the course of an immune response, the development of memory B cells and plasma cells secreting high-affinity antibodies requires T-cell help (Miller et al. 1965; Vos et al. 2000). This reaction takes place in the germinal centres of secondary lymphoid organs, where targeted recombination and somatic hypermutation in the immunoglobulin genes induced by the enzyme activation-induced deaminase result in the selection of B cells producing high-affinity, class-switched antibodies (Nutt and Tarlinton 2011; Victora and Nussenzweig 2012). Based mainly on research in rodents, it was previously thought that T-cell help depends on T-helper type 2 (Th2) cells. It is now, however, widely accepted that help to B cells involves a recently discovered subtype of CD4 T cells termed follicular helper (TFH) cells rather than Th2 cells (Crotty 2011; Tangye et al. 2013).
2.2 Immunoglobulins
Basically, immunoglobulins are composed of two heavy chain and two light chain molecules with a molecular weight of approximately 150,000 kD (Paul 2008). The heavy chains with a molecular weight of 50–70 kD are composed of four immunoglobulin superfamily domains linked by a hinge region, and the light chains with a molecular weight of 23 kD consist of two immunoglobulin superfamily domains (Fig. 10.1). The heavy chains specify the isotype and subclass of the immunoglobulin and are linked by disulphide bonds in the Fc (fraction, crystallisable) part of the molecule. The light chains are either kappa or lambda light chain molecules, which are linked by disulphide bonds to the other end of the heavy chain molecule, forming the Fab part (fragment, antigen binding) of the immunoglobulin. Hypervariable regions of the heavy and light chain molecules (termed complementarity-defining regions, CDR) are flanked by framework regions which together make up the antigen-binding region of the Fab part, which is also known as the paratope (Table 10.1).
Schematic representation of the basic structure of immunoglobulins. Immunoglobulins are composed of two heavy chains, each consisting of one variable (V H , red) and three constant (C H1 -C H3 , blue) immunoglobulin domains and two light chains, each consisting of one variable (V L , orange) and one constant (C L ) immunoglobulin domain (Paul 2008). Internally the immunoglobulin domains are stabilised by disulphide bonds. The light chain and VH and CH1 domains constitute the Fab (fragment, antigen binding) part of an immunoglobulin, and the CH2 and CH3 domains from the two heavy chains form the Fc (fragment, crystallisable) part. The CH2 and CH3 domains are linked by the hinge region (black), and the hinge regions of the two heavy chain molecules are linked by disulphide bonds (red). The Fc parts of the heavy chains are glycosylated (not shown). Membrane-bound immunoglobulins have an additional, short transmembrane amino acid chain. The paratope is the distal, antigen-binding part, which consists of three hypervariable or complementarity-determining regions (CDR1-3) in the VL and VH domains. Variation in the amino acid sequence of the VL and VH chains arises from somatic recombination of V, D and J gene segments in the immunoglobulin heavy locus (IGH) and somatic recombination of V and J gene segments in the immunoglobulin kappa locus (IGK) and immunoglobulin lambda locus (IGL)
2.3 Plasma Cells and Plasmablasts
After activation by binding of cognate antigen to cell surface immunoglobulin, B-cell proliferation is induced, and in the absence of T-cell help, this may be sufficient to induce an antibody response, which is dominated by the secretion of IgM antibodies by plasmablasts. Plasmablasts are B cells that have developed into a phenotype where they retain some B-cell surface markers, but also secrete immunoglobulins (Heyzer-Williams and Heyzer-Williams 2005; Kurosaki et al. 2010). Such T-cell-independent immune responses can be induced by multivalent antigens, e.g. bacterial surface antigens, and elicit initial antibody responses which provide some protection until high-affinity, class-switched T-cell-dependent antibody responses have evolved (Berland and Wortis 2002; Mebius and Kraal 2005).
T-cell-dependent antibody responses develop in germinal centres in secondary lymphatic tissues and involve interactions between antigen-specific TFH cells, B cells and follicular dendritic cells (FDCs) (Victora and Nussenzweig 2012). FDCs are specialised stroma cells that express antigen complexed with complement or immunoglobulins on their surface in the follicular area of secondary lymphoid organs. FDCs are important for the selection of high-affinity, mutated immunoglobulin-expressing B cells (Gonzalez et al. 2011). The interaction between antigen-specific TFH and B cells induces the expression of the enzyme activation-induced deaminase (AID) in B cells. This results in class switch recombination from the initial expression of IgM and IgD to other immunoglobulin isotypes. The precise class switch undertaken is influenced by cytokines present in the environment with, e.g. transforming growth factor-β (TGF-β) inducing class switching to IgA and Th2 cytokines inducing class switching to IgE (Fagarasan et al. 2010). Furthermore, AID induces somatic hypermutation in the variable region of immunoglobulin genes. This stochastic reaction results in the chance generation of B cells expressing immunoglobulin genes, which show increased affinity for antigen (Heyzer-Williams and Heyzer-Williams 2005). Such high-affinity antibody-secreting cells are selected by poorly understood processes and differentiate either to plasma cells or to long-living memory B cells, which are able to generate a swift antibody response upon re-exposure to the same antigen.
3 B Cells and Immunoglobulins in the Central Nervous System
3.1 CNS Immunoprivilege and B-Cell Responses
The CNS is conventionally considered an immunoprivileged organ (Carson et al. 2006). The presence of a blood-brain barrier, the lack of a conventional lymphatic drainage system and the sparseness of conventional antigen-presenting cells do, indeed, impose constraints on intrathecal immune responses. B-cell responses are, however, readily induced in the CNS and may be of a similar or even higher magnitude than systemic responses to the same antigen (Gordon et al. 1992). Interestingly, it is possible to induce antibody responses to myelin basic protein (MBP) infused into the CSF, and this results in the subsequent protection against experimental autoimmune encephalomyelitis induced by MBP (Harling-Berg et al. 1991). It appears that the administration of antigen to the CSF is especially immunogenic and the induction of an intrathecal antibody response is associated with the development of a clonally restricted, specific antibody response as assessed by analysis for oligoclonal bands (Harling-Berg et al. 1989; Knopf et al. 1995).
3.2 Quantitative Assessment of Intrathecal Immunoglobulin Synthesis
Normal CSF contains low concentrations of all immunoglobulins. Immunoglobulins in normal CSF derive from passive diffusion across the blood-CSF barriers (Thompson 1988). Diffusion is size-dependent, and the CSF-plasma concentration quotient for various proteins correlates negatively with the size of the individual molecules (Felgenhauer et al. 1976; Felgenhauer and Renner 1977). The CSF-plasma concentration quotient for albumin (Q alb) is commonly used as a measure of barrier integrity and is used to correct for general blood-CSF protein transfer in formulae for the quantitative assessment of intrathecal immunoglobulin synthesis. The size selectivity of the blood-CSF barriers may, however, become disturbed in disease states, leading to erroneous results when the Qalb is used for correction, especially for larger molecules such as IgA and IgM (Thompson 1988).
There is a close relationship between the Q alb and the CSF-plasma concentration quotient for IgG (Q IgG) in control subjects (Delpech and Lichtblau 1972; Ganrot and Laurell 1974). This relationship led to the development of the IgG index, which is Q IgG/Q alb, for the assessment of intrathecal IgG synthesis (Link and Tibbling 1977). The IgG index assumes that there is a linear relationship between the Qalb and the QIgG. This has, however, been questioned by other researchers, who argue that CSF bulk flow is the major determinant of the CSF protein content and that the diffusion theory indicates that the relationship between the Qalb and the QIgG is better explained by a hyperbolic formula (Reiber 1994). Hyperbolic formulae have also been developed for assessing intrathecal synthesis of IgA and IgM (Reiber 1994).
The hyperbolic model is not universally accepted as other researchers have reported that the relationship between the Qalb and the QIgG is linear in a double logarithmic plot and that there is no statistical evidence suggesting that a hyperbolic formula provides a better fit for the data (Öhman 1994). The relationship observed in double logarithmic plots led to the development of the extended IgG index (Öhman et al. 1989) and was later developed into similar extended indices for IgA and IgM (Öhman et al. 1993).
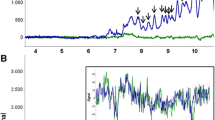
The extended index model is, indeed, the expected model if a linear relationship between the Qalb and the QIgG is assumed, but measuring inaccuracy is also taken into account (Fig. 10.2). If there is no inaccuracy in the measurements, a linear formula such as the IgG index is well suited to establish increased levels of IgG synthesis. Some measuring inaccuracy is, however, unavoidable, and if the same relative measuring inaccuracy applies both for the Qalb and the QIgG at high and low values, this will result in increased variability in the relationship at higher levels. Thus, the linear formula (the IgG index) will tend to give false-positive results at higher Qalb values (Fig. 10.2a), whereas the formulae based on non-linear relationships, i.e. the extended index (Fig. 10.2b) and hyperbolic formula (Fig. 10.2c), are less prone to this error. Indeed, extended immunoglobulin indices and hyperbolic formulae perform better than conventional indices for the quantitative assessment of intrathecal immunoglobulin synthesis (Öhman et al. 1989, 1993; Sellebjerg et al. 1996). None of the formulae are comparable to the detection of oligoclonal bands for the assessment of intrathecal IgG synthesis (Öhman et al. 1992; Sellebjerg et al. 1996). There may, however, be a role for the assessment of intrathecal IgA and IgM synthesis in the diagnosis of infectious diseases in the nervous system (Deisenhammer et al. 2006).
Graphic representation of the consequence of measuring inaccuracy for the use of intrathecal immunoglobulin synthesis formulae (see text for discussion). (a) models a linear relationship, e.g., (b) a double-logarithmic relatoinship, and (c) a hyperbolic relationship between the CSF-plasma quotient of a reference protein (a) and an immunoglobulin of interest (b)
The passive diffusion of immunoglobulins from plasma into the CSF should also be considered when specific antibodies are investigated in patients with CNS infections. Simply calculating an antibody index by comparing the concentration of the specific antibody in CSF and plasma to the CSF and plasma concentrations of IgG is usually sufficient, and similar methods can be applied for the analysis of specific IgM antibodies (Deisenhammer et al. 2006). The application of antibody indices has been used for many antigens, but the results should be interpreted with caution as some patients with MS also show intrathecal synthesis of several virus-specific antibodies, mostly directed against measles, rubella and varicella-zoster virus, the so-called MRZ reaction (Table 10.2) (Felgenhauer and Reiber 1992).
3.3 Qualitative Assessment of Immunoglobulin Synthesis
The detection of clonally restricted, intrathecally synthesised IgG is a hallmark of multiple sclerosis and is observed in more than 90 % of patients with MS (Freedman et al. 2005). IgG oligoclonal bands can, however, also be observed in other diseases (Kostulas et al. 1987; McLean et al. 1990). An account of the development of oligoclonal band analyses is given in the chapter on the history of the CSF earlier in this book. Briefly, it is recommended that oligoclonal bands are analysed by isoelectric focusing followed by immunochemical detection of IgG (Keir et al. 1990). The simultaneous analysis of the CSF and serum with similar amounts of IgG being analysed is mandatory in order to distinguish between CSF bands resulting from local synthesis and bands derived from plasma (Fig. 10.3).
Isoelectric focusing patterns (immunostaining for IgG) showing 1 normal (polyclonal) serum (S) and CSF (C) (no intrathecal IgG synthesis), 2 normal serum and oligoclonal CSF (intrathecal oligoclonal IgG synthesis present), 3 oligoclonal serum and CSF with additional bands in CSF not present in serum (intrathecal oligoclonal IgG synthesis present), 4 identical oligoclonal bands in serum and CSF (mirror pattern, no intrathecal IgG synthesis), 5 paraprotein (monoclonal) resolving in several adjacent bands with a similar pattern in serum and CSF (no intrathecal oligoclonal IgG synthesis), 6 normal serum and single band in CSF (equivocal pattern not considered to represent intrathecal oligoclonal IgG synthesis) (Figure supplied by Poul Erik Hyldgaard Jensen, Neuroimmunology Laboratory, Danish Multiple Sclerosis Center, Rigshospitalet, University of Copenhagen)
It is generally recommended that five different patterns are distinguished: normal pattern, paraprotein, oligoclonal IgG bands only in the CSF, oligoclonal IgG synthesis with identical bands in the CSF and plasma and systemic IgG synthesis with additional bands only in the CSF (Andersson et al. 1994). The latter two patterns are observed in many infectious and inflammatory diseases, whereas the majority of MS patients have IgG oligoclonal bands only in the CSF.
Isoelectric focusing has also been used for the analysis of other immunoglobulin isoforms and for detection of intrathecal synthesis of free immunoglobulin light chains, but these analyses are not in routine use (Deisenhammer et al. 2006; Freedman et al. 2005).
Isoelectric focusing followed by immunoblotting to membranes coated with antigen from infectious agents can be helpful in the diagnosis of CNS infections, but is technically challenging. Interestingly, using methods that provide an estimate of the affinity of the antibody, it has been suggested that antibodies against viral antigens in MS are of low affinity compared to antibodies to the same antigens in patients with viral encephalitis (Luxton et al. 1995; Luxton and Thompson 1990).
3.4 Intrathecal IgM Synthesis
Monomers of IgM molecules are joined in pentamers by J chains to form secreted IgM but may also exist as IgM monomers. The high molecular weight of pentameric IgM (900,000 kD) means that quantitative assessment of intrathecal IgM synthesis is especially prone to artefacts due to alterations in blood-CSF barriers. Intrathecal IgM synthesis is observed in MS and infectious and other inflammatory diseases (Öhman et al. 1993; Sellebjerg et al. 1996). The analysis of IgM oligoclonal bands is technically challenging but is less prone to artefacts than quantitative analysis, and it has been suggested that the presence of IgM oligoclonal bands in MS associated with disease activity and a poor prognosis (Sharief and Thompson 1991, 1992; Villar et al. 2002, 2003). Interestingly, intrathecally secreted IgM in the CSF is derived from cells carrying somatic hypermutations, suggesting that they may be derived from an intrathecal germinal centre-like reaction (Beltran et al. 2014).
3.5 Intrathecal IgG Synthesis
The major indication for assessing intrathecal IgG synthesis is for the diagnosis of MS (Deisenhammer et al. 2006; Freedman et al. 2005). Intrathecal IgG synthesis is, however, observed in a wide variety of inflammatory diseases and infections, and the IgG index or IgG oligoclonal band analysis is often used to screen for inflammatory CNS diseases. Due to its higher sensitivity and specificity, oligoclonal band analysis is the preferred method for assessment of intrathecal IgG synthesis. The IgG oligoclonal bands observed in MS are synthesised by local plasmablasts and plasma cells and have accumulated somatic mutations, suggesting that they represent high-affinity antibodies, but the antigenic target of these antibodies is unknown (Obermeier et al. 2008, 2011). Interestingly, similar clones have been observed among circulating B cells in MS patients (Palanichamy et al. 2014).
3.6 Intrathecal IgA Synthesis
IgA is mainly secreted as a dimer, and upon addition of the secretory component, it is excreted from mucosal surfaces where it has an important role in mucosal immune responses (Holmgren and Czerkinsky 2005). The IgA1 subclass accounts for the majority of circulating and secreted IgA (Delacroix et al. 1982). The IgA2 subclass is more prevalent in secreted IgA. IgA can also be produced intrathecally. However, when intrathecally produced, it is not associated with the secretory component (Woo et al. 1993), and monomeric IgA is produced in substantial amounts during an intrathecal antiviral immune response (Öhman et al. 1995). The class switch to IgA production is directed by TGF-β, and mice with selective deficiency of TGF-β in B cells show a complete absence of IgA in plasma (Cazac and Roes 2000; van Vlasselaer et al. 1992). Interestingly, the endogenous production of TGF-β in B cells contributes to class switching to IgA in human B cells (Zan et al. 1998).
Most studies addressing intrathecal synthesis of IgA have used quantitative methods. Intrathecal synthesis of IgA is less prevalent than intrathecal IgG synthesis but has been reported to occur commonly in patients with bacterial meningitis, including neurotuberculosis (Felgenhauer and Schadlich 1987; Lolli et al. 1989; Sellebjerg et al. 1996). Interestingly, two studies have demonstrated that intrathecal IgA synthesis as assessed by extended immunoglobulin indices is associated with a less severe disease course in patients with MS. The first study showed that the quantitatively assessed intrathecal IgA synthesis correlated negatively with the CSF concentration of MBP as biomarker of demyelination (Sellebjerg et al. 1998). The second study found a relationship between intrathecal IgA synthesis and overall mortality (Vrethem et al. 2004). It is tempting to speculate that this might relate to an immunoregulatory effect of the IgA isotype shift factor TGF-β or IgA itself (Fagarasan et al. 2010).
3.7 Intrathecal IgE Synthesis
Only few studies have investigated IgE in the CSF, and at present the assessment of intrathecal IgE synthesis has no role in routine CSF diagnostics. IgE is secreted as a monomer and is involved in the host response against parasitic infections and allergic reactions. The isotype shift to IgE and the IgG4 subclass is associated with Th2 immune responses, and in multiple sclerosis (MS) there is predominantly intrathecal synthesis of the Th1-associated IgG1 subclass, whereas IgE indices are reduced (Greve et al. 2001). Conversely, in patients with eosinophilic meningitis due to infection with the nematode Angiostrongylus cantonensis, intrathecal synthesis of IgE is prominent, consistent with the known role of Th2 immune responses in parasitic infections (Padilla-Docal et al. 2008). Such patients do, however, also show evidence of intrathecal synthesis of other immunoglobulins than IgE (Dorta-Contreras et al. 2005).
3.8 Intrathecal IgD Synthesis
The biological role of IgD in immune responses is poorly understood. IgD is coexpressed with IgM on the surface of naïve B cells, and IgD or IgM signalling is involved in initial B-cell activation (Harwood and Batista 2010). Only a small proportion of B cells do, however, undergo somatic hypermutation and class switching for the development of IgD-secreting plasma cells. IgD may have a role in mucosal immunity in the airways, providing a link between innate and adaptive immune responses by binding to basophilic granulocytes (Chen et al. 2009). In one study using immunoglobulin indices to compare intrathecal synthesis of IgG, IgM, IgA and IgD, increased IgG index values were more commonly increased in MS than in patients with other inflammatory diseases, whereas the latter patient group more commonly showed increased IgA index, IgD index and IgM index values than did patients with MS (Lolli et al. 1989). In other studies, IgD oligoclonal bands were found mainly in patients with demyelinating diseases, infections and tumours (Mavra et al. 1992, 1999).
4 Conclusions
The analysis of intrathecal immunoglobulin synthesis is important for the diagnosis of multiple sclerosis and other inflammatory neurological diseases. The analysis of IgG is most widely used, and it is recommended that this is done by isoelectric focusing with specific immunochemical detection of IgG bands. For quantitative analysis, the IgG index is often used, but non-linear formulae such as hyperbolic formulae and extended indices are better suited, especially for the analysis of IgA and IgM and when there is an impairment of the blood-CSF barrier function independent of its cause.
References
Andersson M, Varez-Cermeno J, Bernardi G et al (1994) Cerebrospinal fluid in the diagnosis of multiple sclerosis: a consensus report. J Neurol Neurosurg Psychiatry 57:897–902
Beltran E, Obermeier B, Moser M et al (2014) Intrathecal somatic hypermutation of IgM in multiple sclerosis and neuroinflammation. Brain 137:2703–2714
Berland R, Wortis HH (2002) Origins and functions of B-1 cells with notes on the role of CD5. Annu Rev Immunol 20:253–300
Broz P, Monack DM (2013) Newly described pattern recognition receptors team up against intracellular pathogens. Nat Rev Immunol 13:551–565
Carson MJ, Doose JM, Melchior B et al (2006) CNS immune privilege: hiding in plain sight. Immunol Rev 213:48–65
Cazac BB, Roes J (2000) TGF-beta receptor controls B cell responsiveness and induction of IgA in vivo. Immunity 13:443–451
Chen K, Xu W, Wilson M et al (2009) Immunoglobulin D enhances immune surveillance by activating antimicrobial, proinflammatory and B cell-stimulating programs in basophils. Nat Immunol 10:889–898
Crotty S (2011) Follicular helper CD4 T cells (TFH). Annu Rev Immunol 29:621–663
Deisenhammer F, Bartos A, Egg R et al (2006) Guidelines on routine cerebrospinal fluid analysis. Report from an EFNS task force. Eur J Neurol 13:913–922
Delacroix DL, Dive C, Rambaud JC et al (1982) IgA subclasses in various secretions and in serum. Immunology 47:383–385
Delpech B, Lichtblau E (1972) Immunochemical estimation of IgG and albumin in cerebrospinal fluid. Clin Chim Acta 37:15–23
Dorta-Contreras AJ, Noris-Garcia E, Escobar-Perez X et al (2005) IgG1, IgG2 and IgE intrathecal synthesis in Angiostrongylus cantonensis meningoencephalitis. J Neurol Sci 238:65–70
Fagarasan S, Kawamoto S, Kanagawa O et al (2010) Adaptive immune regulation in the gut: T cell-dependent and T cell-independent IgA synthesis. Annu Rev Immunol 28:243–273
Felgenhauer K, Reiber H (1992) The diagnostic significance of antibody specificity indices in multiple sclerosis and herpes virus induced diseases of the nervous system. Clin Investig 70:28–37
Felgenhauer K, Renner E (1977) Hydrodynamic radii versus molecular weights in clearance studies of urine and cerebrospinal fluid. Ann Clin Biochem 14:100–104
Felgenhauer K, Schadlich HJ (1987) The compartmental IgM and IgA response within the central nervous system. J Neurol Sci 77:125–135
Felgenhauer K, Schliep G, Rapic N (1976) Evaluation of the blood-CSF barrier by protein gradients and the humoral immune response within the central nervous system. J Neurol Sci 30:113–128
Freedman MS, Thompson EJ, Deisenhammer F et al (2005) Recommended standard of cerebrospinal fluid analysis in the diagnosis of multiple sclerosis: a consensus statement. Arch Neurol 62:865–870
Ganrot K, Laurell CB (1974) Measurement of IgG and albumin content of cerebrospinal fluid, and its interpretation. Clin Chem 20:571–573
Gonzalez SF, Degn SE, Pitcher LA et al (2011) Trafficking of B cell antigen in lymph nodes. Annu Rev Immunol 29:215–233
Gordon LB, Knopf PM, Cserr HF (1992) Ovalbumin is more immunogenic when introduced into brain or cerebrospinal fluid than into extracerebral sites. J Neuroimmunol 40:81–87
Greve B, Magnusson CG, Melms A et al (2001) Immunoglobulin isotypes reveal a predominant role of type 1 immunity in multiple sclerosis. J Neuroimmunol 121:120–125
Harling-Berg C, Knopf PM, Merriam J et al (1989) Role of cervical lymph nodes in the systemic humoral immune response to human serum albumin microinfused into rat cerebrospinal fluid. J Neuroimmunol 25:185–193
Harling-Berg CJ, Knopf PM, Cserr HF (1991) Myelin basic protein infused into cerebrospinal fluid suppresses experimental autoimmune encephalomyelitis. J Neuroimmunol 35:45–51
Harwood NE, Batista FD (2010) Early events in B cell activation. Annu Rev Immunol 28:185–210
Heyzer-Williams LJ, Heyzer-Williams MG (2005) Antigen-specific memory B cell development. Annu Rev Immunol 23:487–513
Holmgren J, Czerkinsky C (2005) Mucosal immunity and vaccines. Nat Med 11:S45–S53
Keir G, Luxton RW, Thompson EJ (1990) Isoelectric focusing of cerebrospinal fluid immunoglobulin G: an annotated update. Ann Clin Biochem 27(Pt 5):436–443
Knopf PM, Cserr HF, Nolan SC et al (1995) Physiology and immunology of lymphatic drainage of interstitial and cerebrospinal fluid from the brain. Neuropathol Appl Neurobiol 21:175–180
Kostulas VK, Link H, Lefvert AK (1987) Oligoclonal IgG bands in cerebrospinal fluid. Principles for demonstration and interpretation based on findings in 1114 neurological patients. Arch Neurol 44:1041–1044
Kurosaki T, Shinohara H, Baba Y (2010) B cell signaling and fate decision. Annu Rev Immunol 28:21–55
Link H, Tibbling G (1977) Principles of albumin and IgG analyses in neurological disorders. III. Evaluation of IgG synthesis within the central nervous system in multiple sclerosis. Scand J Clin Lab Invest 37:397–401
Lolli F, Halawa I, Link H (1989) Intrathecal synthesis of IgG, IgA, IgM and IgD in untreated multiple sclerosis and controls. Acta Neurol Scand 80:238–247
Luxton RW, Thompson EJ (1990) Affinity distributions of antigen-specific IgG in patients with multiple sclerosis and in patients with viral encephalitis. J Immunol Methods 131:277–282
Luxton RW, Zeman A, Holzel H et al (1995) Affinity of antigen-specific IgG distinguishes multiple sclerosis from encephalitis. J Neurol Sci 132:11–19
Mavra M, Luxton R, Keir G et al (1992) Oligoclonal immunoglobulin D in the cerebrospinal fluid of neurologic patients. Neurology 42:1244–1245
Mavra M, Drulovic J, Levic Z et al (1999) CNS tumours: oligoclonal immunoglobulin D in cerebrospinal fluid and serum. Acta Neurol Scand 100:117–118
McLean BN, Luxton RW, Thompson EJ (1990) A study of immunoglobulin G in the cerebrospinal fluid of 1007 patients with suspected neurological disease using isoelectric focusing and the Log IgG-Index. A comparison and diagnostic applications. Brain 113(Pt 5):1269–1289
Mebius RE, Kraal G (2005) Structure and function of the spleen. Nat Rev Immunol 5:606–616
Miller JF, De Burgh PM, Grant GA (1965) Thymus and the production of antibody-plaque-forming cells. Nature 208:1332–1334
Neefjes J, Jongsma ML, Paul P et al (2011) Towards a systems understanding of MHC class I and MHC class II antigen presentation. Nat Rev Immunol 11:823–836
Nutt SL, Tarlinton DM (2011) Germinal center B and follicular helper T cells: siblings, cousins or just good friends? Nat Immunol 12:472–477
Obermeier B, Mentele R, Malotka J et al (2008) Matching of oligoclonal immunoglobulin transcriptomes and proteomes of cerebrospinal fluid in multiple sclerosis. Nat Med 14:688–693
Obermeier B, Lovato L, Mentele R et al (2011) Related B cell clones that populate the CSF and CNS of patients with multiple sclerosis produce CSF immunoglobulin. J Neuroimmunol 233:245–248
Öhman S (1994) Points of view concerning the diffusion theory for blood-CSF barrier function and dysfunction. J Neurol Sci 126:240–245
Öhman S, Forsberg P, Nelson N et al (1989) An improved formula for the judgement of intrathecally produced IgG in the presence of blood brain barrier damage. Clin Chim Acta 181:265–272
Öhman S, Ernerudh J, Forsberg P et al (1992) Comparison of seven formulae and isoelectrofocusing for determination of intrathecally produced IgG in neurological diseases. Ann Clin Biochem 29(Pt 4):405–410
Öhman S, Ernerudh J, Forsberg P et al (1993) Improved formulae for the judgement of intrathecally produced IgA and IgM in the presence of blood CSF barrier damage. Ann Clin Biochem 30(Pt 5):454–462
Öhman S, Ernerudh J, Roberg M et al (1995) Determination of total and herpes simplex virus specific monomeric and dimeric IgA in serum and cerebrospinal fluid by ultracentrifugation. Ann Clin Biochem 32(Pt 6):550–556
Padilla-Docal B, Dorta-Contreras AJ, Bu-Coifiu-Fanego R et al (2008) Intrathecal synthesis of IgE in children with eosinophilic meningoencephalitis caused by Angiostrongylus cantonensis. Cerebrospinal Fluid Res 5:18
Palanichamy A, Apeltsin L, Kuo TC et al (2014) Immunoglobulin class-switched B cells form an active immune axis between CNS and periphery in multiple sclerosis. Sci Transl Med 6:248ra106
Paul WE (2008) Fundamental immunology. Lippincott, Williams & Wilkins, Philadelphia
Reiber H (1994) Flow rate of cerebrospinal fluid (CSF)–a concept common to normal blood-CSF barrier function and to dysfunction in neurological diseases. J Neurol Sci 122:189–203
Sellebjerg F, Christiansen M, Rasmussen LS et al (1996) The cerebrospinal fluid in multiple sclerosis. Quantitative assessment of intrathecal immunoglobulin synthesis by empirical formulae. Eur J Neurol 3:548–559
Sellebjerg F, Christiansen M, Nielsen PM et al (1998) Cerebrospinal fluid measures of disease activity in patients with multiple sclerosis. Mult Scler 4:475–479
Sharief MK, Thompson EJ (1991) Intrathecal immunoglobulin M synthesis in multiple sclerosis. Relationship with clinical and cerebrospinal fluid parameters. Brain 114(Pt 1A):181–195
Sharief MK, Thompson EJ (1992) Distribution of cerebrospinal fluid oligoclonal IgM bands in neurological diseases: a comparison between agarose electrophoresis and isoelectric focusing. J Neurol Sci 109:83–87
Shishido SN, Varahan S, Yuan K et al (2012) Humoral innate immune response and disease. Clin Immunol 144:142–158
Sprent J, Surh CD (2011) Normal T cell homeostasis: the conversion of naive cells into memory-phenotype cells. Nat Immunol 12:478–484
Tangye SG, Ma CS, Brink R et al (2013) The good, the bad and the ugly – TFH cells in human health and disease. Nat Rev Immunol 13:412–426
Thompson EJ (1988) The CSF proteins: a biochemical approach. Elsevier, Amsterdam
van Vlasselaer P, Punnonen J, de Vries JE (1992) Transforming growth factor-beta directs IgA switching in human B cells. J Immunol 148:2062–2067
Victora GD, Nussenzweig MC (2012) Germinal centers. Annu Rev Immunol 30:429–457
Villar LM, Masjuan J, Gonzalez-Porque P et al (2002) Intrathecal IgM synthesis predicts the onset of new relapses and a worse disease course in MS. Neurology 59:555–559
Villar LM, Masjuan J, Gonzalez-Porque P et al (2003) Intrathecal IgM synthesis is a prognostic factor in multiple sclerosis. Ann Neurol 53:222–226
Vos Q, Lees A, Wu ZQ et al (2000) B-cell activation by T-cell-independent type 2 antigens as an integral part of the humoral immune response to pathogenic microorganisms. Immunol Rev 176:154–170
Vrethem M, Fernlund I, Ernerudh J et al (2004) Prognostic value of cerebrospinal fluid IgA and IgG in multiple sclerosis. Mult Scler 10:469–471
Woo AH, Cserr HF, Knopf PM (1993) Elevated cerebrospinal fluid IgA in humans and rats is not associated with secretory component. J Neuroimmunol 44:129–135
Zan H, Cerutti A, Dramitinos P et al (1998) CD40 engagement triggers switching to IgA1 and IgA2 in human B cells through induction of endogenous TGF-beta: evidence for TGF-beta but not IL-10-dependent direct S mu → S alpha and sequential S mu → S gamma, S gamma → S alpha DNA recombination. J Immunol 161:5217–5225
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Sellebjerg, F. (2015). Immunoglobulins in Cerebrospinal Fluid. In: Deisenhammer, F., Sellebjerg, F., Teunissen, C., Tumani, H. (eds) Cerebrospinal Fluid in Clinical Neurology. Springer, Cham. https://doi.org/10.1007/978-3-319-01225-4_10
Download citation
DOI: https://doi.org/10.1007/978-3-319-01225-4_10
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-01224-7
Online ISBN: 978-3-319-01225-4
eBook Packages: MedicineMedicine (R0)