Abstract
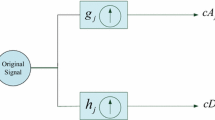
The main goal of this study is to precisely determine the optimum anesthetic dosage required for surgical procedures by evaluating the degree of deep sedation in patients. Anesthesiologists can control the right dose of sedative to guarantee patient comfort and safety during a medical treatment by being aware of the brain waves connected to deep sedation. The electroencephalogram, or EEG, is used as a tool to assess brain activity to identify the deep phase of sedation. The detection method involves analyzing EEG signals imported from an open database in order to extract significant features, followed by preprocessing to remove artifacts related to internal and external factors that can disturb the signal, such as muscle movement, heartbeat, etc., by using Butterworth bandpass filters, the filtered signal is then divided into four separate frequency bands (beta, alpha, theta, and delta). The FFT approach is used to identify the dominating band as the last stage, enabling researchers to extract pertinent information and choose appropriate sedative levels. These procedures are carried out with the aid of LabVIEW software, which has a dedicated Toolkit for the biomedical industry and enables the visualization of the results on a practical and effective graphical interface. In addition, the use of LabVIEW as a processing tool emphasizes the significance of the field of physiological signal processing and demonstrates its potential to streamline and enhance research methodologies in related studies. The outcomes of this study demonstrated that the delta wave, which represents the profound state of sedation, dominates the other waves with a dominance rate of 98.59%. These findings may help to develop sedation monitoring methods in clinical settings. Healthcare providers can improve the dose of a sedative lowering the risk of under- or over-sedation, and enhancing the patient's experience during surgical procedures by precisely detecting the deep phase of sedation using EEG analysis.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Abdolrazaghnejad, A., Banaie, M.: Fentanyl-midazolam vs. midazolam-ketamine regarding patient sedation analgesia for emergency orthopedic procedures. Bangladesh J. Pharmacol. 12(2) (2017). https://doi.org/10.3329/bjp.v12i2.30381
Dobson, G., et al.: Procedural sedation: a position paper of the Canadian Anesthesiologists’ Society. Can. J. Anesth/J. Can Anesth. 65, 1372–1384 (2018). https://doi.org/10.1007/s12630-018-1230-z
Gill, K., Voils, S., Chenault, G., Brophy, G.: Perceived versus actual sedation practices in adult intensive care unit patients receiving mechanical ventilation. Ann. Pharmacother. 46, 1331–1339 (2012). https://doi.org/10.1345/aph.1R037
Moore, K.R.: Critical Care Nursing Interventions and Incidence of Ventilator Associated Pneumonia in the Trauma Population
Bowens, C.D., Thompson, J.A., Thompson, M.T., Breitzka, R.L., Thompson, D.G., Sheeran, P.W.: A trial of methadone tapering schedules in pediatric intensive care unit patients exposed to prolonged sedative infusions. Pediatr. Crit. Care Med. 12, 504–511 (2011). https://doi.org/10.1097/PCC.0b013e3181fe38f5
Li, X., Zhang, L., Gong, F., Ai, Y.: Incidence and risk factors for delirium in older patients following intensive care unit admission: a prospective observational study. J. Nurs. Res. 28, e101 (2020). https://doi.org/10.1097/jnr.0000000000000384
Storrs, C.: Hidden dangers of going under. Sci. Am. 310, 34–35 (2014). https://doi.org/10.1038/scientificamerican0414-34
Pediatric Sedation Outside of the Operating Room
Jacquens, A., Simony, M., Besnard, A., Dupont, J., Degos, V.: Vigilancia de la profundidad de la anestesia general. EMC - Anestesia-Reanimación 49, 1–18 (2023). https://doi.org/10.1016/S1280-4703(22)47393-2
Ramele, R., Villar, A.J., Santos, J.M.: EEG waveform analysis of P300 ERP with applications to brain computer interfaces. Brain Sci. 8, 199 (2018). https://doi.org/10.3390/brainsci8110199
Gerasimov, S., Glushnev, V., Panov, M.: Applications of digital signal processing methods in ultrasonic flowmeters. In: 2018 IV International Conference on Information Technologies in Engineering Education (Inforino), pp. 1–6 (2018)
Potluri, C., et al.: sEMG based real-time embedded force control strategy for a prosthetic hand prototype. In: 2011 IEEE International Conference on Electro/Information Technology, pp. 1–6 (2011)
Cavaliere, F., Cavaliere, C.: Monitoring the depth of anesthesia. In: Chiumello, D. (ed.) Practical Trends in Anesthesia and Intensive Care 2019, pp. 193–205. Springer, Cham (2020). https://doi.org/10.1007/978-3-030-43873-9_13
Shahbazi, F., Ewald, A., Nolte, G.: Univariate normalization of bispectrum using Hölder’s inequality. J. Neurosci. Methods 233, 177–186 (2014). https://doi.org/10.1016/j.jneumeth.2014.05.030
Anier, A., et al.: Relationship between approximate entropy and visual inspection of irregularity in the EEG signal, a comparison with spectral entropy. Br. J. Anaesth. 109, 928–934 (2012). https://doi.org/10.1093/bja/aes312
Liu, Q., Chen, Y.-F., Fan, S.-Z., Abbod, M.F., Shieh, J.-S.: A comparison of five different algorithms for EEG signal analysis in artifacts rejection for monitoring depth of anesthesia. Biomed. Signal Process. Control 25, 24–34 (2016). https://doi.org/10.1016/j.bspc.2015.10.010
Seo, K.H., Kim, K., Lee, S., Cho, J., Hong, J.H.: Changes in electroencephalographic power and bicoherence spectra according to depth of dexmedetomidine sedation in patients undergoing spinal anesthesia. Int. J. Med. Sci. 18, 2117–2127 (2021). https://doi.org/10.7150/ijms.54677
Bob Kemp: Sleep-EDF Database Expanded v1.0.0. https://www.physionet.org/content/sleep-edfx/1.0.0/
el Hadiri, A., Bahatti, L., El Magri, A., Lajouad, R.: Brain signals analysis for sleep stages detection using virtual instrumentation platform. Indon. J. Electric. Eng. Comput. Sci. 29, 761 (2023). https://doi.org/10.11591/ijeecs.v29.i2.pp761-771
Kartika delimayanti, M., et al.: Classification of brainwaves for sleep stages by high-dimensional FFT features from EEG signals. Appl. Sci. 10 (2020). https://doi.org/10.3390/app10051797
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2024 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this paper
Cite this paper
EL Hadiri, A., Bahatti, L., El Magri, A., Lajouad, R. (2024). Profound Sedation Detection Based on Brain Waves Analysis. In: Ezziyyani, M., Kacprzyk, J., Balas, V.E. (eds) International Conference on Advanced Intelligent Systems for Sustainable Development (AI2SD’2023). AI2SD 2023. Lecture Notes in Networks and Systems, vol 905. Springer, Cham. https://doi.org/10.1007/978-3-031-52385-4_1
Download citation
DOI: https://doi.org/10.1007/978-3-031-52385-4_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-52384-7
Online ISBN: 978-3-031-52385-4
eBook Packages: Intelligent Technologies and RoboticsIntelligent Technologies and Robotics (R0)