Abstract
Background: Bruxism is when a person habitually clenches or grinds their teeth. It is a form of parafunctional activity that occurs during sleep and during periods of alertness. This activity can be heard as a grinding or clicking sound and cause facial and/or jaw pain. Bruxism is classified into two categories: sleep bruxism, which occurs during sleep, and awake bruxism, which occurs during periods of alertness. The exact cause of bruxism is unknown. However, there are many potential contributing factors. STAB is a new tool to diagnose bruxism and evaluate possible comorbidities. It has two Axis. Subjectrelated reports on bruxism conditions and possible outcomes are part of Axis A and include clinical (researcher reports) and instrumental assessments (technical reports). Axis B contains self-reported data (subject-based reports) on variables and conditions that may be causal or ancillary in bruxism. This review aims to evaluate the possible use of STAB in the diagnosis of bruxism; Methods: PubMed, Web of Science and Lilacs were systematically searched until 31/01/2023. In addition, a manual search was performed using the bibliography of selected articles and a Google Scholar search. It was completed, and the papers were read to assess their eligibility. Results: The STAB will assist in gathering data on various elements, conditions, and circumstances presently understudied in bruxism. It is split into two axes for this reason. Conclusion: Subject-based reports on bruxism status and possible consequences are part of Axis A, along with clinical (examiner reports) and instrumental assessments (technology report). Self-reported data (subject-based report) on variables and conditions that may play a causal or concomitant part in bruxism are included in axis B. Building predictive models for use in clinical and research settings will be possible thanks to this complete multidimensional assessment system.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
Bruxism is when a person habitually clenches or grinds their teeth. It is a form of parafunctional activity that occurs during sleep and periods of alertness [1]. This activity can be heard as a grinding or clicking sound and cause facial and/or jaw pain [2,3,4,5]. Bruxism is classified into two categories: sleep bruxism, which occurs during sleep, and awake bruxism, which occurs during periods of alertness. The exact cause of bruxism is unknown. However, there are many potential contributing factors. It is believed to be a combination of physical, psychological, strongly increased due the Covid-19 [6,7,8,9,10], and environmental factors. Some of the physical factors that may contribute to bruxism include malocclusion (improper bite alignment), temporomandibular disorders (TMDs) [11, 12], and certain neurological conditions. Psychological factors such as stress and anxiety may also play a role in developing bruxism [13, 14]. Environmental factors such as caffeine and alcohol consumption and lifestyle choices can also contribute to the onset of bruxism. The symptoms of bruxism can vary depending on the severity of the condition. Common signs and symptoms include jaw pain, headaches, tooth sensitivity, facial pain, wear and tear on teeth, and a clicking or grinding sound while sleeping [15]. Diagnosis of bruxism typically involves a physical exam, medical history, and a dental examination. Treating bruxism focuses on correcting the underlying cause if one can be identified. Treatment may involve lifestyle modifications such as stress management, relaxation techniques, and avoiding caffeine and alcohol. Also, mouth guards or splints may protect the teeth from wear and tear. In more severe cases, more aggressive treatments, such as muscle relaxants, may be necessary [16]. Bruxism is a common condition that can significantly impact the quality of life. It is important to speak to a healthcare provider if bruxism is suspected. Early diagnosis and treatment can help reduce the severity of symptoms and improve the overall quality of life. Numerous therapy options for bruxism occur while you sleep, including pharmacological, psychological, and dental approaches. Pharmacological therapies use a variety of medications, including benzodiazepines, anticonvulsants, beta-blockers, dopaminergic agents, antidepressants, and others. Botulinum toxin types A local injections have been given to patients with significant bruxism to relieve their symptoms. However, little is understood about the drug’s efficacy, pharmaceutical safety, and long-term monitoring. Psychological therapy includes psychotherapy, hypnosis, biofeedback, relaxation techniques to manage stress, and behavior therapy focused on good sleep hygiene. Occlusion correction, tooth surface restoration, and orthodontic therapy are all dental therapies for bruxism. Standardized tools are the most accurate and reliable methods for assessing bruxism [17]. This article will discuss standardized tools for assessing bruxism, their reliability and validity in diagnosis, and how they can inform clinical and therapeutic decisions. The Bruxism Activity Rating Scale (BARS) is the most common tool for assessing bruxism. This validated questionnaire asks patients to rate their bruxism activity over the past week on a scale from 0 to 10. It is valid for children and adults and reliable across different cultures and languages. Additionally, the BARS can differentiate between grinding, clenching, and both grinding and clenching [18]. Another tool used to assess bruxism is the Bruxism Severity Index (BSI). This validated questionnaire asks patients to rate the severity of their bruxism symptoms on a scale from 0 to 10. It is reliable across different cultures and languages and valid for children and adults. Additionally, the BSI can differentiate between mild, moderate, and severe levels of bruxism. The Bruxism Symptom Checklist (BSC) is another validated tool for assessing bruxism. It is a self-administered questionnaire asking patients to rate their bruxism symptoms’ frequency and severity on a scale from 0 to 10. It is reliable across different cultures and languages and valid for children and adults. Additionally, the BSC can differentiate between mild, moderate, and severe levels of bruxism. Finally, the Bruxism Impact Questionnaire (BIQ) is a validated tool used to assess the impact of bruxism on quality of life. It is a self-administered questionnaire asking patients to rate their bruxism symptoms’ impact on a scale from 0 to 10 [19]. It is reliable across different cultures and languages and valid for children and adults. Additionally, the BIQ can differentiate between mild, moderate, and severe levels of bruxism. In conclusion, standardized tools are vital for accurately assessing bruxism and informing clinical and therapeutic decisions. According to the available data, bruxism is a behaviour that should not be assessed using the straightforward binary distinction of “present versus missing.” It may be necessary to distinguish between the various motor behaviours that comprise the bruxism continuum (such as clenching versus grinding, with or without teeth contact). This is necessary because the aetiology, comorbidities, and possible outcomes of various motor activities may differ. This review aims to evaluate the possible use of STAB in the diagnosis of bruxism.
1.1 Materials and Methods
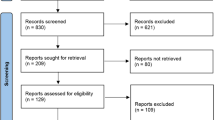
Literature searches of free text and MeSH terms were performed using MedLine (PubMed), Web of Science, and Lilacs. All searches for any relationship between orthodontics and telemedicine were conducted using a combination of subject headings and free-text terms; the final search strategy was determined through several pre-searches. The keywords used in the search strategy were as follows: ”stab” [All Fields] AND (“bruxism” [MeSH Terms] OR “bruxism” [All Fields]) (Table 1). Only papers providing data at the end of the intervention were included. Exclusion criteria were: (1) Studies on patients with lack of multiple dental elements; (2) cross-over study design; (3) studies written in a language different from English; (4) full-text unavailability (i.e., posters and conference abstracts); (5) studies involving animal; 120 (6) review article; (7) case report. Articles regarding the use of STAB for the diagnosis of bruxism were selected as inclusion criteria. The scientific databases were used in the execution of the review (PUBMED, WEB of SCIENCE, LILACS). The electronic search was conducted between January 3, 2000, and February 2023. “stab” and “bruxism” have both been used together with the boolean operator AND.
Two reviewers (R.F. and G.M.) separately extracted data from the included studies using an individualised data extraction on a Microsoft Excel sheet. A third reviewer was used to obtain consensus in cases of disagreement. The following information was taken out: (1) first author; (2) publication year; (3) nationality; (4) results; (5) main findings.
2 Results
STAB has two planes. Subject-related reports on bruxism conditions and possible outcomes are part of Axis A and include clinical (researcher reports) and instrumental assessments (technical reports). Axis B contains self-reported data (subjectbased reports) on variables and conditions that may be causal or ancillary in bruxism. Axis B has self-reported data (subject-based reports) on variables and conditions that may be causal or ancillary in bruxism. In addition, two additional instruments are being developed for STAB. A toolkit version of STAB (STAB Toolkit) is available to enhance assessing a specific factor or condition using a dedicated and complete questionnaire/instrument. A bruxism screener instrument (BruxScreen) is available to enhance understanding and clarity. It has been used experimentally for its efficacy. Inside is a thematic list of articles selected for inclusion in the full version of STAB. They provide an explanatory manual on specific points in my special writing paper. Based on current knowledge, stackable rating classifications do not make sense as the bruxism landscape is increasingly complex. The most effective way to develop a multidimensional bruxism assessment system is to collect as much information as possible about the bruxism condition index, potential aetiology and comorbid factors, integrated assessment of the condition, and clinical outcomes. Was [20]. The items currently included in the full version of STAB are listed within the context of this assumption. Articles related to bruxism conditions dominate the STAB. A screening tool was created to find individuals who might benefit from undergoing a total STAB. A negative bruxism test does not require the lengthy STAB complete form. Clinical evaluation should begin there if a patient presents to the clinic with a particular phenotype (such as pain or tooth wear). Different factors shaped by the central nervous system and associated with comorbidities affect the phenotype. Clinicians zoom out from the symptoms to perform a thorough assessment, including symptoms, signs, and comorbidities related to diagnosis and aetiology [21]. Assessments are a combination of patient self-reports collected through questionnaires, oral interviews, and clinical assessments, including required phenotype-related items. Again, this clinical assessment can complement instrumental assessment using techniques relevant to the patient’s phenotype. Combining these different assessment levels can provide personalized precision medicine targeting specific phenotypes. In a patient whose bruxism is part of the above evaluation, her STAB in full can be considered. For example, it is a possible aetiology of pain and tooth wear. Potential STAB processes can also be determined based on this. If bruxism is suspected, the patient can be tested with a bruxism screening device. The prevailing theory is that status confirmation requires approval of certain things. Therefore, if BruxScreen raises suspicion of bruxism, the physician must verify that one or more of her selected STAB items are positive to confirm the bruxism status. Progression from doubt to fame can be seen along this path. A thorough evaluation of comorbidities, contributing factors, and clinical outcomes are required when the status is reviewed, and complete STAB administration is required. The next stage of STAB refinement was a total’ entry point’ to the STAB: suspected signs and symptoms of bruxism. Additionally, research can be conducted using cross-sectional and, particularly, longitudinal designs to address important questions like “In which cases is bruxism linked with certain consequences and in which cases it is not?” and “In which circumstances—i.e., secondary bruxism—is bruxism linked with a known aetiology?” With enough time, extracting data using artificial intelligence techniques will be possible. Defining and assessing bruxism status is essential when using the STAB for clinical and research reasons. By using quantitative (such as bruxism time index and bruxism work index) and qualitative assessment, the ultimate objective is to phenotype bruxism status (e.g. for sleep bruxism: arousal-related events, isolated short-lasting events, elevated background activity, prolonged tonic activity; for awake bruxism: long tonic activity, short-lasting events). The crucial additional point is that the STAB project’s efforts will give doctors tools for their clinics and referral, which will better collaborate with them to assess, prevent, and treat bruxism [22].
3 Discussion
The Bruxism Activity Rating Scale, Bruxism Severity Index, Bruxism Symptom Checklist, and Bruxism Impact Questionnaire are all validated tools that are reliable and effective for children and adults of different cultures and languages [23]. Is. These tools can distinguish crunches, crunches, and crunches, mild, moderate and severe bruxism. The device will help gather information on several bruxism-related conditions, aspects, and currently understudied variables. Instead of using stackable or dichotomous (yes/no) ratings, we created a complete multidimensional rating system to develop predictive models for clinical and research settings. Another group of international experts recently released an overview manuscript to outline the general design of a Standardized Tool for the Assessment of Bruxism. (STAB) [24]. The STAB project’s goal is to collect as much information as possible regarding the potential risk, comorbidity, and associated factors for bruxism, as well as the state of bruxism and its clinical effects. Specific domains will be formatted for data taken from the participant, gathered during a clinical evaluation, and recorded with instruments. Currently, the STAB is being revised by a group of invited reviewers, not expert council members. The final iteration will also be tested in the field to see if it can be improved. In brief, the STAB seeks to pinpoint pertinent elements linked to the causes, prevalence, and effects of bruxism. This information can be applied to several things in clinical and research contexts. Clinical algorithms can be developed based on known variables along the aetiology-status-consequences trajectory to forecast the presence of bruxism, its causes, and its effects [25]. An instrument on bruxism should be able to connect the various areas for clinicians. The objectives of this phase will be (a) a definitive identification of bruxism status based on MMA levels during wakefulness or sleep as well as the frequency of behaviour during wakefulness and (b) an evaluation of the correlation of such status with the subject-based and clinically based assessment domains as well as with the various Axis B categories. Based on their availability to conduct fieldwork, chosen research groups and co-authors will be added to the core expert panel for all primary investigations. The connections between the areas will be established after the second phase, including those between aetiology and concurrent conditions (Axis B), bruxism status (Axis A—IBA), and subjective and/or clinical markers (Axis A—SBA/CBA). A third and final step will involve the extraction of the volume of data gathered through a preliminary study using artificial intelligence techniques. The amount of collected data may increase to an unmanageable level, necessitating the development of new analysis techniques. (e.g. big data, artificial intelligence). It is possible to set scoring standards for each sub-axis to create a graphical representation of the bruxism assessment [26]. Models could be developed to forecast the causes of additive bruxism in the presence of certain subjective or clinical factors and vice versa. We’ll define various usage strategies for study, clinical, and customized management at the individual level.
4 Conclusion
Despite being a hot topic in the most recent dental and sleep medicine literature, bruxism has never been the subject of standardized assessment standards. The first step toward creating a set of standards for a standardized tool for assessing bruxism is described in this research. (STAB). A Bruxism Evaluation System (BES), suggested by the expert panel, is currently being developed.
References
Qazi, N., Pawar, M., Padhly, P.P. et al.: Teledentistry: evaluation of Instagram posts related to Bruxism. Technol. Health Care, 1–12 (2023).https://doi.org/10.3233/THC-220910
Réus, J.C., Polmann, H., Mendes Souza, B.D. et al.: Association between primary headache and bruxism: an updated systematic review. J. Oral. Facial Pain Headache 35, 129–138. https://doi.org/10.11607/ofph.2745
Quinzi, V., Paskay, L.C., Manenti, R.J., et al.: Telemedicine for a multidisciplinary assessment of orofacial pain in a patient affected by eagle’s syndrome: a clinical case report. Open Dentistry J. 15, 102–110 (2021). https://doi.org/10.2174/1874210602115010102
Ahci, S., Bal, B., Benbir-Senel, G., et al.: Polysomnographic characteristics of sleep-related bruxism: what are the determinant factors for temporomandibular disorders? Cranio J. Craniomandibular Sleep Pract. 40, 544–550 (2022). https://doi.org/10.1080/08869634.2021.2014167
Crescente, G., Minervini, G., Spagnuolo, C., Moccia, S.: Cannabis bioactive compoundbased formulations: new perspectives for the management of orofacial pain. Molecules 28, 106 (2022). https://doi.org/10.3390/molecules28010106
Vozzo, L.M., Azevedo, L., Fernandes, J.C.H., Fonseca, P., Araújo, F., Teixeira, W., Fernandes, G.V.O., Correia, A.: The success and complications of complete-arch implant-supported fixed monolithic zirconia restorations: a systematic review. Prosthesis 5, 425–436 (2023). https://doi.org/10.3390/prosthesis5020029
Spirito, F., Amato, A., Scelza, G. et al.: Education during the COVID-19 pandemic: the perception of Italian dental and medical students. Minerva Dental Oral Sci. 71, 277–286 (2022). https://doi.org/10.23736/S2724-6329.22.04712-X
Badnjević, A., Pokvić, L.G., Džemić, Z., Bečić, F.: Risks of emergency use authorizations for medical products during outbreak situations: a COVID-19 case study. Biomed. Eng. Online, 19 (2020).https://doi.org/10.1186/s12938-020-00820-0
Sycinska-Dziarnowska, M., Maglitto, M., Woźniak, K., Spagnuolo, G.: Oral health and teledentistry interest during the COVID-19 pandemic. J. Clin. Med. 10, 3532 (2021). https://doi.org/10.3390/jcm10163532
Chakraborty, T., Jamal, R.F., Battineni, G., et al.: A review of prolonged Post-COVID-19 symptoms and their implications on dental management. Int. J. Environ. Res. Public Health 18, 5131 (2021). https://doi.org/10.3390/ijerph18105131
Di Francesco, F., Lanza, A., Di Blasio, M., et al.: Application of botulinum toxin in temporomandibular disorders: a systematic review of randomized controlled trials (RCTs). Appl. Sci. 12, 12409 (2022). https://doi.org/10.3390/app122312409
Minervini, G., D’amico, C., Cicciù, M., Fiorillo, L.: Temporomandibular joint disk displacement: etiology, diagnosis, imaging, and therapeutic approaches. J. Craniofacial Surg, 10–1097 (2022). https://doi.org/10.1097/SCS.0000000000009103
Dadnam, D., Dadnam, C., Al-Saffar, H.: Pandemic bruxism. Br. Dent. J. 230, 271 (2021). https://doi.org/10.1038/s41415-021-2788-3
Kaya, D.I., Ataoglu, H.: Botulinum toxin treatment of temporomandibular joint pain in patients with bruxism: a prospective and randomized clinical study. Niger. J. Clin. Pract. 24, 412–417 (2021). https://doi.org/10.4103/njcp.njcp_251_20
Soegiantho, P., Suryawinata, P.G., Tran, W., Kujan, O., Koyi, B., Khzam, N., Algarves Miranda, L.: Survival of single immediate implants and reasons for loss: a systematic review. Prosthesis 5, 378–424 (2023).https://doi.org/10.3390/prosthesis5020028
de Baat, C., Verhoeff, M., Ahlberg, J., et al.: Medications and addictive substances potentially inducing or attenuating sleep bruxism and/or awake bruxism. J. Oral Rehabil. 48, 343–354 (2021). https://doi.org/10.1111/joor.13061
Amorim, C.S.M., Espirito Santo, A.S., Sommer, M., Marques, A.P.: Effect of physical therapy in bruxism treatment: a systematic review. J. Manipulative Physiol. Ther. 41, 389–404 (2018). https://doi.org/10.1016/j.jmpt.2017.10.014
Goldstein, R.E., Auclair Clark, W.: The clinical management of awake bruxism. J. Am. Dent. Assoc. 148, 387–391 (2017). https://doi.org/10.1016/j.adaj.2017.03.005
Lobbezoo, F., Ahlberg, J., Raphael, K.G., et al.: International consensus on the assessment of bruxism: report of a work in progress. J. Oral Rehabil. 45, 837–844 (2018). https://doi.org/10.1111/joor.12663
Manfredini, D., Ahlberg, J., Aarab, G. et al.: The development of the standardised tool for the assessment of Bruxism (STAB): an international road map. J. Oral Rehabil. (2022).https://doi.org/10.1111/joor.13380
Manfredini, D., Ahlberg, J., Aarab, G., et al.: Towards a standardized tool for the assessment of bruxism (STAB)-overview and general remarks of a multidimensional bruxism evaluation system. J. Oral Rehabil. 47, 549–556 (2020). https://doi.org/10.1111/joor.12938
Manfredini, D., Ahlberg, J., Aarab. G. et al.: Standardised tool for the assessment of Bruxism. J. Oral. Rehabil. (2023).https://doi.org/10.1111/joor.13411
Lavigne, G.J., Khoury, S., Abe, S., et al.: Bruxism physiology and pathology: an overview for clinicians. J. Oral Rehabil. 35, 476–494 (2008). https://doi.org/10.1111/j.1365-2842.2008.01881.x
Lobbezoo, F., Ahlberg, J., Verhoeff, M.C. et al.: The bruxism screener (BruxScreen): Development, pilot testing and face validity. J. Oral. Rehabil. (2023).https://doi.org/10.1111/joor.13442
Manfredini, D., Ahlberg, J., Lobbezoo, F.: Bruxism definition: past, present, and future—what should a prosthodontist know? J. Prosthet. Dent. 128, 905–912 (2022). https://doi.org/10.1016/j.prosdent.2021.01.026
Manfredini, D., Landi, N., Fantoni, F., et al.: Anxiety symptoms in clinically diagnosed bruxers. J. Oral Rehabil. 32, 584–588 (2005). https://doi.org/10.1111/j.1365-2842.2005.01462.x
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2024 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this paper
Cite this paper
Minervini, G., Franco, R., Capogreco, M., Ronsivalle, V., Cicciù, M. (2024). Standardized Tool for the Assessment of Bruxism (STAB): A New Method to Assess the Temporomandibular Disorder Patients. In: Badnjević, A., Gurbeta Pokvić, L. (eds) MEDICON’23 and CMBEBIH’23. MEDICON CMBEBIH 2023 2023. IFMBE Proceedings, vol 94. Springer, Cham. https://doi.org/10.1007/978-3-031-49068-2_73
Download citation
DOI: https://doi.org/10.1007/978-3-031-49068-2_73
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-49067-5
Online ISBN: 978-3-031-49068-2
eBook Packages: EngineeringEngineering (R0)