Abstract
This study aims at evaluating the efficiency of the National Healthcare Systems (NHS) in a number of southeastern European countries (Albania, Bulgaria, Cyprus, Greece, Hungary, North Macedonia, Montenegro, Romania, Serbia, Slovenia, and Slovakia), for the years before and during the covid-19 pandemic. To achieve this goal, a two-stage data envelopment analysis (DEA) model was constructed, comprised of four input variables (health expenditure per capita, number of physicians, number of nurses, number of hospital beds), one intermediate variable (vaccination rates), and two output variables (life expectancy at birth and mortality rates). In the second stage, the DEA results were regressed against socioeconomic variables (Gini index of income inequality, GDP per capita, ratio of population over 65 years old and “EU age”). The data was extracted from a combination of secondary sources (Eurostat, WHO, OECD, The World Bank, Our Word in Data). The DEA results reveal that Cyprus and Albania have the most efficient NHS, while Serbia and Slovakia have the least. The efficiency of the Greek NHS has significantly improved since 2015. Moreover, the regression analysis shows that GDP does not have a noteworthy impact on NHS efficiency, income inequality has a positive, albeit debatable positive impact, increasing aging ratios put substantial pressure on the health systems and EU membership bears important benefits to the NHS. This study sheds light on the comparative assessment and the determinants of the NHS in South-East Europe and provides useful insights for health professionals, economists, and policymakers.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Health issues gain increasing importance on the global agenda, especially since the covid-19 pandemic onset. Simultaneously, efficiency has become an ultimate goal for both private and public organizations. National health system (NHS) efficiency in particular is of the utmost importance for several reasons (Cylus et al. 2016). The main is that the cost of any healthcare inefficiencies is not only wasted money, but it can be human lives, too. Even in less extreme cases, an inefficient NHS fails to cure patients creating accumulative pressure that generates more inefficiency. This situation generates public frustration and to alleviate it, policymakers often divert resources from other vital sectors, such as education, aggravating social welfare. ΝΗS efficiency is particularly important for southeastern European countries facing financial pressures and concerns over their long-term financial sustainability. A thorough understanding of the NHS efficiency determinants would enable policymakers to make the best possible use of existing resources and provide healthcare funders, such as governments, insurance companies, and individuals, with critical information about how their money is being spent.
This study aims to contribute to a better understanding of the factors affecting NHS efficiency, with a special focus on south-east European (SEE) countries. This area is of particular interest because it is comprised of both developed and developing, EU and non-EU member states, with diverse socioeconomic profiles, which have undergone major financial and organizational transformations during the last two decades, triggered both by the financial crisis (2009–2018) and by the covid-19 pandemic (2020 onwards). To achieve these goals, a two-stage methodology was engaged. First, a DEA model calculates the overall healthcare efficiency of the NHS in Albania, Bulgaria, Cyprus, Greece, Hungary, North Macedonia, Montenegro, Romania, Serbia, Slovenia, and Slovakia, for the years before (2008), during (2015) and after (2019) the financial crisis (and before the pandemic), as well as during the covid-19 pandemic, without and with vaccination (2020 and 2021, respectively). Subsequently, a regression analysis is engaged, aiming at evaluating a number of environmental factors for their contribution to NHS efficiency. The two approaches reveal the (in)efficiencies of the NHSs in the south-east European countries as well as their exogenous determinants and provide useful insights for health professionals, economists, and policymakers.
The structure of the paper is as follows. Section 2 summarizes the situation of the Greek healthcare system. Section 3 describes the study results and Sect. 4 discusses the study conclusions.
2 Literature Review
During the last decades, the SEE countries have engaged in extensive health system transformations, including reforms of primary and secondary healthcare, new governance and funding arrangements, the privatization of healthcare provision, and the introduction of health insurance systems (Bartlett et al. 2012). Especially after the great recession that hit most of the European economies in 2009, additional structural changes took place and efficiency became one of the main concerns of the health sector due to constant pressures on healthcare sources. Amongst these turbulent times, the need for a thorough assessment of the NHS efficiency is indispensable. To this end, Stanculescu and Neculau (2014) conducted a comparative qualitative study on the performance of Public Healthcare Systems in South-East Europe. Among their findings, the researchers conclude that SEE countries lag behind Western European States in terms of living conditions although life expectancy at birth has been increasing since 2000. These nations also display high rates of infant and maternal mortality which may be connected with the existing socioeconomic, ethnic and geographical inequalities in health status. Access to healthcare and social services is much more limited for people with low-income and poor education, for those belonging to minorities (e.g. Roma and migrant populations) and/or who live in rural areas. Additional disparities are generated by the heavy reliance on informal (out-of-pocket) payments for health services, which are substantial in most SEE states.
More recently, OECD published a series of country health profiles (OECD 2021a), providing a succinct overview of health systems in the EU/European Economic Area (EEA), highlighting the unique characteristics and challenges of each country. According to this overview, the countries of southeastern Europe spend less on healthcare than most other EU countries and they have an average NHS effectiveness worse than the EU27. They display high rates of both preventable and treatable mortality.Footnote 1 High rates of these two indicators are suggestive of major deficiencies in the health system’s ability to provide appropriate and timely treatment to the population and highlight the need for additional spending on preventive care. Moreover, the SEE countries demonstrate generally low life expectancy rates with significant disparities by both gender and socioeconomic status. Two countries however, namely Greece and Cyprus, show a different pattern (OECD 2021a).
Greece was selected as a focal point for the current study because the NHS of this country underwent tremendous reforms during the last fifteen years to become more efficient. Greece followed a bailout program known as Economic Adjustment Program (EAP), for eight years (2010–2018) which stipulated strict austerity measures and structural adjustments in many sectors (Myloneros and Sakellariou 2021). Especially in healthcare, a combination of ‘macro’ health policy changes (including budget caps) and ‘micro’ structural measures (including gatekeeping, e-prescription and generic drugs) was employed to improve efficiency (Kalavrezou and Jin 2021). Greece completed the Economic Adjustment Program in 2018, however, the shrinkage of healthcare expenditures continued in 2019 (OECD 2021b). The covid-19 pandemic that outbroke in the first months of 2020 led to increased financial support to the NHS, including national and European funding, for emergency medical staff, medical equipment, and the operation of intensive care units (ICUs) (OECD 2021b). The Greek NHS was further strengthened against covid-19, with a vaccination program starting on 27 December 2020 (Greek Government 2022). Nevertheless, the effectiveness of the Greek health system is still threatened, since life expectancy at birth declined by six months in 2020 (OECD 2021b).
Several scholars have assessed the efficiency of the Greek NHS during the economic crisis (Fragkiadakis et al. 2016; Mitropoulos et al. 2018; Flokou et al. 2017; Xenos et al. 2017); however, these studies were limited within national borders and exclusively preoccupied with the public hospital sector. Moreover, technical efficiency focusing primarily on budget control may be inadequate to create an insightful understanding of NHS management. Therefore, a two-stage panel approach was chosen as the most appropriate to examine the NHS efficiency of neighboring countries in different periods. This study focuses on both developed and developing South-East European countries that have undergone significant structural changes during the last two decades. In addition to Greece which underwent significant transformations due to the financial crisis described above, other countries in this region experienced profound economic, political and social changes due to their entrance to the European Union (Cyprus, Hungary, Slovakia and Slovenia joined the EU on 1st January 2004 and Bulgaria and Romania, followed in 2007). The remaining countries of the sample (Albania, the Republic of North Macedonia, Montenegro and Serbia) are EU candidates; therefore, they go through a transition period that also requires structural public administration transformations.
Based on the notion that the NHS of a country may be considered a production system that transforms inputs into outputs (Dhaoui 2019), this study initially uses Data Envelopment Analysis (DEA), which is a popular methodology for assessing technical efficiency in healthcare. Gavurova et al. (2021) adopted an input-oriented Dynamic Network Data Envelopment Analysis (DNDEA) assuming both constant and variable returns to scale (VRS and CRS, respectively), to quantify and compare the efficiency of OECD health systems over three periods (2000, 2008, and 2016). Kozuń-Cieślak (2020) applied three DEA models in 25 OECD countries to examine the relationship between NHS efficiency and economic wealth. She used health expenditure as a percentage of GDP, health expenditure per capita, medical doctors per 1,000 inhabitants, practicing nurses per 1,000 inhabitants, medical equipment per one million inhabitants as inputs and infant mortality per 1,000 live births, as output. Asandului et al. (2014) evaluated the efficiency of the healthcare systems of 30 European countries in 2010, using the number of doctors, the number of hospital beds and public health expenditures as a percentage of GDP as inputs and life expectancy at birth, health adjusted life expectancy and infant mortality rate as outputs in both CRS and VRS DEA models. Ouertani et al. (2018) applied DEA to longitudinal data from Saudi Arabia, using public spending on health as input and life expectancy and 1/infant mortality as outputs.
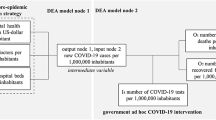
Based on the above literature, the DEA variables used in this study included four inputs (health expenditure per capita, number of physicians, number of nurses, number of hospital beds), one intermediate variable (vaccination rates), and two outputs (life expectancy at birth and mortality rates).
Thorough evaluation of health efficiency is frequently difficult due to external factors, beyond the control of healthcare management. To overcome this limitation, many studies in this area consider the impact of external (environmental) factors by employing regression analysis on the DEA results. Castaldo et al. (2020) engaged a two-stage methodology to assess the efficiency of health expenditure in 30 OECD countries over the period 2005 to 2015. In the first stage, they applied input-oriented DEA to estimate the technical efficiency using public health expenditure as input and a health performance indicator comprised of infant mortality rate, life expectancy at birth and hospital discharge rates as output. In the second stage, they regressed DEA results against a number of non-discretionary variables, such as the Gross Domestic Product (GDP), the rates of vaccination, weather temperature, red tape (slowness of bureaucracy), tobacco consumption and obesity. Dhaoui (2019) used a two-stage performance analysis, to assess the technical efficiency of eighteen NHSs in the Middle East and North Africa (MENA) region for the years 1997, 2005 and 2014. In the first stage, he used both input- and an output-oriented DEA and in the second stage, he analyzed the health efficiency determinants using a Tobit regression with GDP per capita, health expenditure, adult literacy rate, urbanization level and control of corruption as independent variables. Similarly, Gong et al. (2019) applied input-oriented CRS Network DEA to measure the healthcare efficiency in thirty China provinces from 2009 to 2016. Then, they practiced Tobit regression to analyze the factors affecting overall efficiency, using GDP per capita, number of high education enrollment, government health expenditure, social health expenditure, personal health expenditure, number of public hospitals and number of private hospitals, as independent variables. Zarulli et al. (2021) studied the healthcare system efficiency of 140 countries, using DEA analysis with life expectancy as single output and regression analysis in the second stage with education index; infants lacking immunization against DTP3 and measles; current health expenditure as a percentage of GDP; share of the population using at least basic sanitation services; share of unemployed in the labor force; income inequality measured by the Gini coefficient; and the ratio of 65 or older population to those of working age as dependent variables. Finally, Dincă et al. (2020) examined the healthcare efficiency in 17 EU Member states taking into account the year in which each state joined the EU, separating the sample countries into old member states (before 2004) and new member states (after 2004).
Based on the above literature, the Gini index of income inequality, the GDP per capita, the ratio of population over 65 years old and the “EU age” (i.e. the number of years that a country is a member of the European Union), were selected as independent variables for the regression analysis in the current study.
3 Methodology
3.1 Data Envelopment Analysis
DEA is a mathematical linear programming approach used to measure the technical efficiency (TE) of different Decision-Making Units (DMUs), as well as the same DMU over time. In the last case, each DMU is treated as a separate DMU in each period. This procedure enables the comparison of every DMU both to itself over time and to peers allowing us to determine efficiency variations across countries and across time (panel approach).
On these grounds, a DEA for cross-sectional data has been conducted upon five sub-periods: 2008 (before the financial crisis), 2015 (during the financial crisis), 2019 (after the financial crisis, before the pandemic), 2020 (during the pandemic, without covid-19 vaccines) and 2021 (during the pandemic, with covid-19 vaccines). This study aligns with the majority of the DEA studies that use input-oriented models (based on the assumption that the adjustment of inputs cannot significantly increase this output at one time) and both constant and variable returns to scale (CRS and VRS, respectively) assumptions (Cantor and Poh 2018).
The input-oriented model used in this study is described by the following equation (Medarević and Vuković 2021):
where:
-
θ0 is the efficiency score of the NHSs under assessment
-
λi is a vector of positive constraints, indicating the weight of the restrictions
-
\({x}_{si}\) is the quantity of input s used by the i DMU
-
yri is the output value of the r variable produced by the i DMU.
3.2 Regression
In the second stage, the DEA efficiency scores calculated in the first step were used as the dependent variable (\({\widehat{\rho }}_{0}^{*}\)), and regressed on potential exogenous (environmental) variables (zi), according to the following generic equation (Simar and Wilson 2007):
where:
-
α is the regression constant
-
zi are the environmental variables
-
β is the regression coefficient
-
\({\xi }_{i}\) is a statistical noise with distribution limited by \({\xi }_{i }\le 1-a-{z}_{i}\beta \) because DEA efficiency scores are less than or equal to unit.
3.3 Data
The data used in this paper were sourced from various sources, as seen in Table 1. The data for most of the DEA and regression variables were extracted from the World Bank (data last updated 27/4/2022) and were supplemented by the latest data for the years 2020–2021 available from the national statistic institute of each country. Data about covid-19 deaths and vaccination rates in 2021 was derived from Our World in Data. As two output indicators (Y1 and Y2) are de-stimulants (they refer to an undesirable output), they were converted into desirable measures by using them as denominators (i.e. Y1* = 1/Y1 and Y2* = 1/Y2), as applied also by Ouertani et al. (2018).
As seen in Table 2, health expenditure as a percentage of GDP (X1) ranges from 9.46 in the EU to 5.42 in Albania, has a tendency to increase over the years and demonstrates a little variation across the countries’ sample. The same is true for the number of physicians per 1,000 people (X2), which ranges from 6.22 in Greece to 1.49 in Albania (4.79 is the EU average). The number of nurses and midwives per 1,000 people (X3) displays more variation, ranging from 12.74 in Slovenia to 3.94 in North Macedonia (9.30 is the EU average). The number of beds per 1,000 people (X4) ranges from 7.29 in Bulgaria to 2.8 in Albania (5.25 is the EU average). Vaccine doses per 1,000 people (X5) have been calculated only for the year 2021 (the covid-19 vaccines were made publicly available in December 2020). The number of doses may be more than 1,000 per 1,000 people since multiple doses apply to a single person. The EU average for 2021 was 1,690.00 and the values of the X5 variable ranged from 1,720.00 in Cyprus to 542.00 in Bulgaria. The mortality per 100,000 people caused by covid-19 (Y1) was calculated for the years 2020 and 2021 and ranged from 276.01 in Bulgaria to 31.66 in Cyprus (142.29 is the EU average). Similarly, total mortality of any cause (covid-19 included) per 100 k (Y2), ranged from 1,647.06 in Bulgaria to 628.13 in Cyprus (972.45 is the EU average). Life expectancy (Y3) ranged from 81.22 in Cyprus to 73.84 in Bulgaria (80.38 is the EU average) and generally declined in the two last years (2020 and 2021) due to the covid-19 pandemic.
Regression variables were selected only for the year 2019 both because this was the most recent year with available data for all countries and all variables and because this was the most “normal” year, on the verge between the financial crisis and the pandemic. As seen in Table 1, GDP per capita varies significantly across the selected countries, ranging from 42,339€ in Cyprus to 13,998€ in Albania (28,780€ was the EU average). The Gini index (GNI) ranges from 40.3 in Bulgaria to 23.2 in Slovenia (30.6 is the EU average). The Gini index measures the extent to which the distribution of income or consumption among individuals or households within an economy deviates from a perfectly equal distribution. A GNI of 0 represents perfect equality, while an index of 100 implies perfect inequality. The proportion of the total population that is older than 65 years ranges from 21.95% in Greece to 14.05% in Cyprus (20.46% is the EU average). Lastly, the sample contains both non-EU members (Albania, North Macedonia, Montenegro, Serbia) and countries that joined the European Union either a long time ago (Greece has been an EU member country for 41 years, since 1 January 1981) or recently (Romania and Bulgaria are the newest EU members, since 2007).
4 Results
4.1 DEA Results
The DEA efficiency scores range between 0 and 1, where one indicates the unit is relatively efficient, and a value <1 indicates inefficiency. For the years studied, all DEA models used two outputs, namely the total mortality of any cause and the life expectancy. An extra DEA model (2021 covid) was run for the year 2021, including vaccination doses as an intermediate input and covid deaths as output (Table 3).
Both CRS and VRS DEA methodologies were applied giving similar results. Due to space limitations, it was chosen to present and discuss only the CRS results.
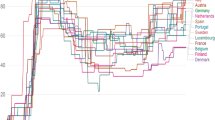
As we can see in Table 3 and Fig. 1, Cyprus and Albania constantly rank in the 1st place in NHS efficiency. Greece reached the efficiency frontier from 2019 onwards. North Macedonia ranks high except for a slight decline in 2020. Romania is perhaps the only country with efficiency decreasing over time, except for a temporary increase in 2020. Hungary had an impressive efficiency improvement between 2015 and 2019 but after 2020 efficiency declined sharply, perhaps due to the challenges that the covid-19 pandemic imposed on the NHS. The same pattern applies to Slovakia and Slovenia, to a smaller extent. The reverse pattern is observed for Montenegro, Serbia and the EU average, the efficiencies of which significantly increased during the pandemic. Another rather controversial observation is that the EU average ranks very low until 2020, well below the average efficiency of the sample countries, which is constantly improving.
Additionally, the examination of the 2021-covid model’s results reveals that there is a significant efficiency gap between Cyprus (and Albania) that lay on the efficiency frontier and the remaining countries whose efficiencies rank from the minimum of 0.143 (Hungary) to the maximum of 0.417 (Serbia), much lower than the efficiency frontier. This finding indicates that, with the exception of the two countries that constantly record high NHS efficiencies, the other countries fell behind in managing the pandemic, even with the support of the available covid-19 vaccine.
Cluster analysis (Fig. 2) reveals three separate efficiency clusters in the countries under study. Cluster 1 is comprised of the two countries (Albania and Cyprus) located on the efficiency frontier. Cluster 2 contains four countries (Bulgaria, Greece, North Macedonia and Romania) with average efficiency scores between 0.87 and 0.97. Cluster 3 contains five countries (Hungary, Montenegro, Slovakia, Serbia and Slovenia, with the last two displaying the least NHS efficiencies during the years studied).
The above results call for a closer examination of the observed differences. Regression analysis was engaged to test for external factors that may affect NHS efficiency.
4.2 Regression Results
The regression results suggest that our model has a good explanatory value and it is statistically significant (R2 = 0.797, p < 0.05). According to the regression results (Table 4), GDP does not have a significant impact on NHS efficiency. On the contrary, GNI has a relatively significant positive impact. This was also obvious from the DEA results, since Bulgaria which has the highest Gini index in the sample scored better than Slovenia, which has the lowest Gini index and the lowest efficiency score, too. Furthermore, human age over 65 has a significant negative impact, while the EU age (the time elapsed since a country joined the EU) has a significant positive impact on NHS efficiency.
5 Discussion and Conclusions
This study evaluated the NHS efficiency in eleven SEE countries, engaging a two-stage analysis. In the first stage, the technical efficiency of the healthcare systems was calculated, using a Data Envelopment Analysis. In the second stage, the DEA scores were regressed against socioeconomic variables to examine their impact on NHS efficiency.
According to the DEA results, Cyprus and Albania are the two countries with the highest NHS efficiency over the years. The Cypriot population enjoys good health overall, with one of the highest life expectancies in the EU (OECD 2019). The Cypriot healthcare system has undergone several major transformations since the induction of the Republic of Cyprus into the European Union in 2004 intensified by the bailout agreement with the International Monetary Fund, the European Commission and the European Central Bank (known as the Troika) which prevented Cyprus bankruptcy in 2011 (Petrou 2021). Apart from the structural changes, the progressive rise in life expectancy reflects the urbanization of the Cypriot population's lifestyle, the improvement of the diagnostic approach, and easier access to health services (Agathokleous et al. 2016).
Albania has struggled with sustained periods of economic and political isolation within Europe as a former Communist group of countries, leading to great challenges to reforming the country’s economic and social establishments, including healthcare. Despite these obstacles, the Albanian government has conducted many reform cycles over the last three decades. Albania made economic progress during this time, reducing national poverty and gaining upper-middle-income status (Saric et al. 2021). In 2015, the World Bank announced €32.1 million in financing for the Health System Improvement Project in Albania. The project would support improving the efficiency of care in selected hospitals in Albania, improving the management of information in the health system, and increasing financial access to health services (World Bank 2015). A recent study (Saric et al. 2021) observed a significant improvement in the quality of primary healthcare in Albania, between 2015 and 2018.
Greece scored the biggest efficiency improvement between 2015 and 2019, something that has also been measured by other scholars (Gavurova et al. 2021) and can be partially explained by the major transformations that Greek NHS has undergone since 2010 when the country entered the Economic Adjustment Programs. Another factor that may play a positive role is that Greece is an old EU member (since 1981), therefore the country has a good knowledge of the EU supporting mechanisms and may leverage them to its benefit. However, a point of concern is the high percentage of elderly people that may jeopardize the efficiency progress made by the Greek NHS.
On the other hand, among the countries with the lowest efficiency, we can see Serbia and Slovenia. Serbia has made significant gains in terms of life expectancy and basic health indicators but remains far below the EU average, and significant differences are visible across the country's districts and population groups. There is also a large variation in productivity within and across types of hospitals (World Bank 2017; Medarević and Vuković 2021). Serbia’s healthcare system is relatively costly. The total health expenditure as a share of gross domestic product (GDP) gradually increased from 6.5% in the mid-1990s to around 10% in 2010, almost twice the health spending of Albania. Moreover, private spending on health services (out-of-pocket money) remains high, amounting to 42.4% of total health expenditure in 2017 (Bjegovic-Mikanovic et al. 2019). Nevertheless, even though the average NHS efficiency in Serbia is low, it has significantly improved since 2015.
Healthcare reforms in Slovenia have been delayed or failed in recent years as a result of rejected proposals to eliminate complementary health insurance and health financing. This difficulty in reaching a consensus is especially concerning given the fiscal sustainability challenges that Slovenia faces if no policy changes are implemented (OECD 2017). Though population health has improved in recent decades, health disparities due to gender, social and economic factors, and geography continue to pose significant challenges. Outdated facilities are another issue that must be addressed to ensure the long-term sustainability and resiliency of the Slovenian NHS (Albreht et al. 2016).
Rather controversially, the EU average efficiency is much lower than the sample’s average score, which may further support that NHS efficiency is not a direct outcome of health expenditure since EU has the highest health spending and Albania has the lowest. Besides, Slovenia constantly ranks low in efficiency although it has one of the highest scores in healthcare public spending, something that may be the result of decreasing returns of scale, as already reported by Asandului et al. (2014), meaning that adding more inputs may have an adverse result on the outputs. This also was the case for Greece until 2015, when health spending was significantly shrunk due to structural measures, allowing for constant RTS from then on.
Overall, the DEA results align with previous studies. Asandului et al. (2014) also found that in 2010, Cyprus was on the efficiency frontier and Greece scored higher than Hungary. Medarević and Vuković (2021) who applied DEA in Serbian hospitals from 2015 to 2019, found that they operated at a low-efficiency level, compared to most European peers. However, when comparing the findings, we must bear in mind that the year of the study, the peers compared, and the mix of inputs and outputs selected have an impact on the DEA results (Cantor and Poh 2018).
In the regression analysis, GDP is found not to have a significant impact, indicating that the NHS efficiency cannot be attributed to a single factor, even though this is a significant financial feature, such as the national health expenditure or GDP per capita. This finding is consistent with Gong et al. (2019) who also found that the effect of GDP per capita on the efficiency of the healthcare system in China provinces is not statistically significant. Dhaoui (2019) has also observed that low-income countries can be a reference in terms of health efficiency. Moreover, Asandului et al. (2014) reported that Romania and Bulgaria were among the most efficient NHS, although these countries’ general economic performances are poor. Kozuń-Cieślak (2020) who examined the Bismarckian and Beveridgean-style healthcare systems in 25 OECD countries to identify the relationship between the efficiency of the country’s NHS and its economic wealth, found that more developed economies are technically less efficient, supporting the view that technical efficiency is only one of many factors influencing the superiority of the healthcare system and patient satisfaction. Similarly, Ouertani et al. (2018) claim that increasing public spending does not necessarily result in improving healthcare efficiency, since an NHS is a complex system and other factors (i.e. primary healthcare quality) may interfere with the final results.
GNI has a positive impact which is relatively significant. This finding is rather controversial, given that in most of the studies examining the relationship between income inequality and health levels, it is observed that the population health levels are lower in societies with greater income inequality (Wilkinson and Pickett 2006). However, some scholars have produced evidence that the Gini index has no significant effect on health outcomes (Lorgelly and Lindley 2008; Mackenbach 2002). Other authors claim that the evidence linking income inequality with health levels is inconsistent and insufficient (Lynch et al. 2004). Deaton and Paxson (2004) concluded that inequity itself is not a direct determinant of health levels, but possible correlations between the Gini index and health efficiency may refer to broader notions of inequality and inequity that are most likely important for health. Finally, since income inequalities are reduced in developed economies that enjoy a longer life expectancy and have a great proportion of the elderly population, this observation can be an indicator of the complex interrelations between the socioeconomic determinants having an impact on the NHS outcomes. Lastly, Cornia and Court (2001) came to the conclusion that a Gini coefficient value between 0.25 and 0.40 has a growth-promoting effect. Given that the countries of our sample display a GNI between 23.2 and 40.3, it is possible that this GNI range enables health efficiency growth, too.
Population aging has an adverse impact on NHS efficiency. Medarević and Vuković (2021) have also observed that the efficiency of the Serbian hospitals was negatively associated with the proportion of elderly in the hospital catchment area. This finding is unsurprising since Dincă et al. (2020) mention that healthcare costs increase exponentially for elderly people. Additionally, after the age of 65, people often have more complicated and long-term healthcare needs due to functional deterioration, a decline in mental abilities, physical illness, and psychosocial needs, that demand a great amount of health resources (Kim et al. 2018). This is of particular importance not only for Greece (which has the highest proportion of the elderly population in the sample) but also for the entire Europe, which is an ‘aging society’, and, given the expected extension of life expectancy, will be a ‘post-aged society’ in the near future (Zlotkin 2017). The effects of the expected ‘silver tsunami’ due to population aging are well documented, underlining the fiscal and political difficulties that many countries’ health and social protection systems are projected to encounter in the next decades. Age > 65.
EU age has a significant positive impact on NHS efficiency. This finding is in line with Dincă et al. (2020) who also observed that the old EU members displayed high-efficiency scores, their general sustainable economic performance being proof that they obtained good results with respect to healthcare efficiency. It is possible therefore that a country that belongs to the EU family can benefit from financial support from the European Structural and Investment Funds and the European Regional Development Fund to move its NHS to a higher level. Lomba (2019) reports that EU membership brings significant benefits to the EU citizens, economies and health policy, through the following mechanisms: economies of scale (joint action, procurement and funding), free movement of persons (patient access to healthcare in different EU member states and harmonized patient rights), reduction of cross-border threats (synchronized responses to pandemics/epidemics), promotion of best practices (extensive databases and diffusion of standards), networking (of scientists and national authorities), benchmarking for decision-making, unlocking pharmaceutical and treatment innovation potential and implementing health EU legislation ensuring a safe and well-functioning internal market and the protection of public health.
Overall, the results of this study are useful to governments, regulators, healthcare providers and funders, and the general public. Policymakers aim to achieve both technical efficiency, i.e. maximizing the outputs for the amount of given inputs and allocative efficiency, i.e. directing the limited resources towards the most productive sectors and using the optimal mix of inputs to achieve the productivity goals. Healthcare funders including governments, insurance organizations, households and the general public are interested in knowing which systems, providers and treatments contribute the largest health gains in relation to the level of resources they devour. Our results indicate that more efficient use of resources can help countries to improve their life expectancy even without increasing health expenditure.
This study also has some limitations. The DEA results should be treated with caution, because different countries, different input/output mix, and different years could produce different outcomes. Moreover, both DEA and regression results are sensitive to the data used, which is often unavailable especially when examining current phenomena. In this case, the use of proxies is unavoidable, therefore a re-examination of the same situation in a few years may produce dissimilar results.
Future research can attempt a more detailed examination of the NHS efficiency, by extending the list of DEA inputs and outputs, examining additional socioeconomic factors in the regression analysis, including data from the private healthcare sector and using a larger sample of countries. Furthermore, NHS efficiencies could be assessed with alternative methodologies, either non-parametric (e.g., FDH) and/or parametric (e.g., SFA) or, using a mix of quantitative and qualitative methods, to gain a more comprehensive understanding of the multifaceted factors that affect healthcare systems’ performance.
Notes
- 1.
Preventable mortality can be attributed to risk factors including smoking, alcohol consumption and unhealthy diets and can be avoided through public health and primary prevention interventions. Treatable mortality refers to deaths that can be mainly avoided through healthcare interventions.
References
Agathokleous MN et al (2016) Estimating life expectancy of the population in Cyprus with the use of life tables. Hippokratia 20(2):99
Albreht T et al (2016) Slovenia: health system review. Health Syst Transit 23(1):1–183
Asandului L et al (2014) The efficiency of healthcare systems in Europe: a data envelopment analysis approach. Procedia Econ Finance 10:261–268
Bartlett W, Bozikov J, Rechel B (eds) (2012) Health reforms in south-east Europe. Springer
Bjegovic-Mikanovic V et al (2019) Serbia: health system review. Health Syst Transit 21(3):i-211
Cantor VJM, Poh KL (2018) Integrated analysis of healthcare efficiency: a systematic review. J Med Syst 42(1):1–23
Castaldo A et al (2020) Determinants of health sector efficiency: evidence from a two-step analysis on 30 OECD countries. Econ Bull 40(2):1651–1666
Cornia GA, Court J (2001) Inequality, growth and poverty in the era of liberalization and globalization. In: Policy Brief 4 of the UNU world institute for development economics research (UNU/WIDER), The United Nations University, Helsinki
Cylus J, Papanicolas I, Smith PC, World Health Organization (2016) Health system efficiency: how to make measurement matter for policy and management. World Health Organization, Regional Office for Europe
Deaton A, Paxson C (2004) Mortality, income, and income inequality over time in Britain and the United States. In: Perspectives on the economics of aging, pp 247–286
Dhaoui I (2019) Healthcare system efficiency and its determinants: a two-stage data envelopment analysis (DEA) from MENA countries. Economic Research Forum (ERF), Giza, Egypt
Dincă G et al (2020) The efficiency of the healthcare systems in EU countries–a DEA analysis. Acta Oeconomica 70(1):19–36
Flokou A et al (2017) A window-DEA based efficiency evaluation of the public hospital sector in Greece during the 5-year economic crisis. PLoS ONE 12(5):e0177946
Fragkiadakis G et al (2016) Operational and economic efficiency analysis of public hospitals in Greece. Ann Oper Res 247(2):787–806
Gavurova B et al (2021) Health system efficiency in OECD countries: dynamic network DEA approach. Heal Econ Rev 11(1):1–25
Gong G et al (2019) Has the efficiency of china’s healthcare system improved after healthcare reform? A network data envelopment analysis and tobit regression approach. Int J Environ Res Public Health 16(23):4847
Greek Government (2022) COVID-19 vaccination statistics. https://www.data.gov.gr/datasets/mdg_emvolio/. Accessed 2 May 2022
Kalavrezou N, Jin H (2021) Healthcare reform in Greece: progress and reform priorities. IMF Working Papers 2021(189)
Kim YS et al (2018) Unmet healthcare needs of elderly people in Korea. BMC Geriatr 18(1):1–9
Kozuń-Cieślak G (2020) Is the efficiency of the healthcare system linked to the country’s economic performance? Beveridgeans versus Bismarckians. Acta Oeconomica 70(1):1–17
Lomba N (2019) The benefit of EU action in health policy: the record to date: European added value in action. European Added Value Unit. PE 631.729
Lorgelly PK, Lindley J (2008) What is the relationship between income inequality and health? Evidence from the BHPS? Health Econ 17(2):249–265
Lynch J et al (2004) Is income inequality a determinant of population health? Part 1. A systematic review. Milbank Q 82(1):5–99
Mackenbach JP (2002) Income inequality and population health: evidence favouring a negative correlation between income inequality and life expectancy has disappeared. BMJ 324(7328):1–2
Medarević A, Vuković D (2021) Efficiency and productivity of public hospitals in Serbia Using DEA-Malmquist model and tobit regression model, 2015–2019. Int J Environ Res Public Health 18(23):12475
Mitropoulos P et al (2018) The impact of economic crisis on the Greek hospitals’ productivity. Int J Health Plann Manage 33(1):171–184
Myloneros T, Sakellariou D (2021) The effectiveness of primary health care reforms in Greece towards achieving universal health coverage: a scoping review. BMC Health Serv Res 21(1):1–12
OECD/European Observatory on Health Systems and Policies (2017) Slovenia: Country Health Profile 2017, State of Health in the EU, OECD Publishing, Paris/European Observatory on Health Systems and Policies, Brussels
OECD/European Observatory on Health Systems and Policies (2019) Cyprus: Country Health Profile 2019, State of Health in the EU, OECD Publishing, Paris/European Observatory on Health Systems and Policies, Brussels
OECD/European Observatory on Health Systems and Policies (2021a) Country Health Profiles 2021. https://www.oecd.org/health/country-health-profiles-eu.htm
OECD/European Observatory on Health Systems and Policies (2021b) Greece: Country Health Profile 2021, State of Health in the EU, OECD Publishing, Paris/European Observatory on Health Systems and Policies, Brussels
Ouertani MN et al (2018) Assessing government spending efficiency and explaining inefficiency scores: DEA-bootstrap analysis in the case of Saudi Arabia. Cogent Econ Finance 6(1):1493666
Petrou P (2021) The 2019 introduction of the new national healthcare system in Cyprus. Health Policy 125(3):284–289
Saric J et al (2021) Assessing the quality of care at primary health care level in two pilot regions of Albania. Front Public Health 9
Simar L, Wilson P (2007) Estimation and inference in two-stage, semi-parametric models of production processes. J Econom 136(1):31–64
Stanculescu MS, Neculau G (2014) The performance of public health-care systems in South-East Europe: a comparative qualitative study. Friedrich-Ebert-Stiftung, Belgrade
Wilkinson RG, Pickett KE (2006) Income inequality and population health: a review and explanation of the evidence. Soc Sci Med 62(7):1768–1784
Word Bank (2015) Press release: world bank to help improve quality, access, and efficiency of Albania’s health care system. https://www.worldbank.org/en/news/press-release/2015/02/27/world-bank-to-help-improve-quality-access-and-efficiency-of-albanias-health-care-system
World Bank (2017) Delivering health services efficiently for Serbian’s. World Bank, Washington, DC
Xenos P et al (2017) Efficiency and productivity assessment of public hospitals in Greece during the crisis period 2009–2012. Cost Eff Resource Alloc 15(1):1–12
Zarulli V et al (2021) Health care system efficiency and life expectancy: a 140-country study. PLoS ONE 16(7):e0253450
Zlotkin (2017) World population prospects: the 2017 revision. United Nations. https://www.un.org/development/desa/publications/world-population-prospects-the-2017-revision.html
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Paraschi, E.P. (2023). Healthcare Efficiency Assessment in the Southeastern European Countries Using Two-Stage DEA Analysis. In: Persiani, N., Vannini, I.E., Romiti, A., Karasavvoglou, A., Polychronidou, P. (eds) Challenges of Healthcare Systems in the Era of COVID-19. Contributions to Management Science. Springer, Cham. https://doi.org/10.1007/978-3-031-43114-2_13
Download citation
DOI: https://doi.org/10.1007/978-3-031-43114-2_13
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-43113-5
Online ISBN: 978-3-031-43114-2
eBook Packages: Business and ManagementBusiness and Management (R0)