Abstract
This chapter deals on a theoretical level with the importance of interactions between biological and social factors in the epidemic or pandemic spread of infectious diseases. Biosocial interactions are a fundamental factor in the spread of infections, and a more detailed understanding of these interactions is of scientific and practical interest. To be able to describe systematics, it is proposed to link a classic model of infectious disease epidemiology (the epidemiological triad) and a model of the social determinants of health (ecosocial theory). To illustrate the approach, principles of the biology of infectious diseases are examined more closely to identify possible interfaces with social conditions that make it easier or more difficult for the pathogen to spread. This presentation follows the biological process of an infection from exposure to infection and subsequent disease. Step-by-step, it addresses pathogen characteristics and their implications for the interaction with hosts and their social contexts.
Embodiment [is] a concept that refers to how we literally incorporate, biologically, the material and social world in which we live, from in utero to death; a corollary is that no aspect of our biology can be understood absent knowledge of history and individual and societal ways of living
Nancy Krieger, Proximal, distal, and the politics of causation, 2008
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
A pathogen needs the cooperation of its (potential) hosts for an epidemic or even a pandemic to develop. These must either meet in large numbers and become infected in the process or, in the case of indirect transmission, seek contact with the contaminated material in large numbers. This is also the case with infectious diseases that affect humans, which are the focus of this article. It follows that the behaviour of people is a decisive factor in the dynamics of the spread of infectious diseases. However, behaviour is to be understood here in the sociological sense, i.e., not as a purely individual action but as collective, socioculturally shaped patterns of action of larger social groups or entire societies. Of course, a single person who drinks contaminated water, for example, can become infected with cholera. However, a major outbreak will only occur if a large number of people drink from this source and no measures are taken by the group to close or avoid this source. The interactions between pathogens and hosts are, naturally, more complex in reality and depend on both the biological properties of the respective pathogen and the concrete behaviours or reactions of the population affected [1]. A few examples will illustrate this. The transmission properties of a pathogen determine, for example, which social practice increases the probability of infection in the first place. Regarding a respiratory pathogen that is transmitted from person to person via aerosols, different social interactions pose a risk compared with a sexually transmitted disease. Conversely, people at risk of infection react to the characteristics of the pathogen, for example, by deliberately refraining from certain behaviours or by taking organised measures at the social level to specifically combat pathogens or prevent potentially dangerous social situations.
Despite the obvious need to consider pathogen characteristics AND the logic of social practice and social structures when assessing outbreaks, research explicitly addressing the principles of this linkage is comparatively rare [1, 2]. This is understandable, as research in the field of infectious diseases is also primarily disciplinary. Microbiologists, virologists, infectiologists, psychologists, medical sociologists or public health researchers each have their own perspectives on the phenomenon, and even if the contributions of the other disciplines are certainly noticed, genuine interdisciplinary cooperation has been unusual thus far. In addition, the social dimension of the spread of infectious diseases has generally been somewhat out of the focus of research until recently. The social determinants of health (understood as social influences on population health) have been intensively researched, but mainly in relation to noncommunicable diseases, such as diabetes, obesity or cardiovascular disease. Infectious diseases, however, have special characteristics that make it difficult to generalise scientific findings from research on other diseases. Research on social determinants also tends to focus on the social sphere as a source of (causal) influences on health, while the biological processes mediating between social factors and the emergence of a specific disease often play only a secondary role [3]. Of course, there are exceptions in the field of infectious diseases, such as research on the social conditions of the spread of HIV and AIDS, which has revealed, for example, the importance of stigma, the influence of gender norms or the fatal consequences of poverty for diagnosis and treatment [4]. However, little scientific evidence exists for many other infectious diseases, and this applies not only to neglected tropical diseases but also to globally occurring diseases, such as influenza.
Nevertheless, research has made important progress during the coronavirus disease 2019 (COVID-19) pandemic. Within a short period of time, many new empirical studies on different social influences on the course of the pandemic were published [e.g.: 5, 6]. Thus, correlations that were already known could be replicated for COVID-19, and those previously unknown were uncovered. Similarly, there have been initial attempts in connection with COVID-19 to develop further at the theoretical level [e.g. 7]. In addition to new research, the COVID-19 pandemic has also provided ample illustrations of how important it is in the practical management of outbreaks that biological and social processes and their interactions are known to be able to respond in a targeted manner with public health measures. One example is the relatively long-standing uncertainty about the transmission routes (e.g., droplets, airborne, fomite) of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) wild-type and its later variants. This lack of knowledge about the specific sites and circumstances of infection has made it difficult to enact appropriate nonpharmaceutical interventions and protect vulnerable populations at particularly high risk. A lack of knowledge about relevant biosocial contexts thus carried the risk of misdirection (by taking both noneffective or effective measures), which may have had negative consequences for the control of the pandemic as a whole. In response to this experience, there are calls from the scientific community and public health practitioners for a science-based approach to both the biological and social determinants of the COVID-19 outbreak (and future pandemics) to become part of organised global and national pandemic preparedness and response [8].
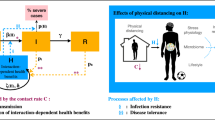
What exactly such pandemic preparedness should look like regarding biosocial interactions is not easy to answer at present. This is because the scientific foundation is incomplete, as explained above. Against this background, this chapter deals on a theoretical level with the significance of the interactions between biological and social factors for the epidemic or pandemic spread of infectious diseases. This biosocial synthesis also serves to describe vulnerability more precisely both as a biological property and as a social property (e.g., belonging to a social group that is frequently exposed to pathogens). The purpose of this chapter is to roughly organise the field of research and to bring together previously known principles or hypotheses in one contribution. I use a classic model of infectious disease epidemiology, namely, the epidemiological triangle (also called the triad), as a theoretical framework. It describes the causation of infectious disease as the product of an interaction between pathogen, host and environment. However, it is precisely the aspect of the interaction of the three factors that has, thus far, only been theoretically differentiated to a limited extent. This also applies to the interaction of the biological characteristics of the pathogen and host and the social environment in which both move. Accordingly, I draw on ecosocial theory, a concept from public health research that describes relationships between people’s social environment and their health. To explore the possibility of linking the models, an exemplary analysis is presented in the second part of this chapter. If focuses on the question of what conclusions can be drawn about relevant social factors from the knowledge of the biological properties of pathogens alone. In other words, the biology of the pathogen is used to look at social factors (biology to social).
2 Conceptual Framework
Following the arguments outlined in the introduction, a theoretical model to describe biosocial relationships should be both disease-specific and integrate notions of biological and social processes. A classic model of the development of infectious diseases that fulfil these conditions is the epidemiological triangle. It goes back to work in plant biology and veterinary epidemiology and postulates that three variables and their interaction are crucial for infectious disease causation: characteristics of the pathogen, the host and the environment [9, 10].
First, I would like to outline the basic characteristics of the pathogen. Only some of the basic characteristics are explained here initially; a more differentiated consideration will follow later in the text. It should be noted that the central feature of the aetiology (development) of infectious diseases is the necessary presence of a specific biological pathogen. These are different forms of organisms, whereby the most important pathogens in human infectious diseases are viruses, bacteria, parasites, fungi and microbes [11]. The relevant pathogens are those that are able to colonise and infect a host—in this case, a human being [12]. While colonisation is superficial, infection is the penetration of the pathogen into the host tissue. For some pathogens, such as many viruses, infection also means that the pathogen manages to replicate initially in the host organism using its resources. When assessing how effectively and efficiently a pathogen spreads (transmission), a third question is crucial: which mode of transmission the pathogen uses to colonise and infect a host? This also includes a consideration of the circumstances under which and the intensity with which a host has contact with the pathogen, i.e., whether it is exposed to it. Once an infection has occurred, the further course of the infection is also pathogen specific. There can be symptom-free courses with complete healing and symptomatic diseases up to chronic or fatal courses. Whether a disease develops from an infection is determined by the pathogen’s individual pathogenicity (the ability of the pathogen to trigger a disease). The severity of the disease, including the risk of a fatal course, is related to the virulence of the pathogen [13].
The second edge in the triangle is the host. First, the host determines through its behaviour (a) whether an exposure occurs at all and (b) if a superficially colonising pathogen leads to an infection, for example, by preventive behaviour, such as hand hygiene. A further host-related factor that is decisive for disease transmission is the so-called susceptibility of the host, which denotes the probability that a host becomes infected if exposed to a pathogen [14]. This is determined by the immune system and the general constitution or resilience of the organism. Both have a genetic component but are also flexible. The immune system, for example, is capable of adapting to certain pathogens and developing immunity through previous infections or external immunisation (i.e., vaccination) to improve its defense against subsequent exposures to the same pathogen [14]. Once infected, immunity and constitution remain important because they also influence the further course of the disease (in interaction with the specific pathogenicity and virulence of the pathogen). People with chronic preconditions, for example, may be particularly vulnerable to developing severe disease if an infection occurs.
The environment, as the third variable, influences both the pathogen and the host and determines how often and under what circumstances the two come into contact with each other. Strictly speaking, it is, thus, less to be understood as part of a triangle but rather as the framework within which host and pathogen exist and interact. The environment was originally understood primarily as the natural environment in the epidemiological triad [10]. Most pathogens need very specific environmental conditions to develop and spread. Important examples are temperatures and their seasonal stability, solar radiation, the presence of certain habitats or biotopes (e.g., stagnant water as a breeding ground for certain mosquitoes) and the presence of host animals in the case of pathogens whose natural reservoir is animals (see below). These conditions are both of current importance for existing pathogen populations and formative in the long term, as they govern the evolutionary adaptation and genetic development of these organisms.
The environment in the epidemiological triangle also includes the social environment [13]. A generally valid and theoretically sound taxonomy of the social factors that are relevant in this context does not yet exist. However, Van Seventer and Hochberg have presented a list of broader categories in their presentation of the principles of infectious diseases that are used here [13]. The categories “land use”, “infrastructure” and “technology and industry” are directly related to the natural environment. Land use covers a wide spectrum of human interactions with nature, from agriculture and forestry to water resource management. Although Seventer and Hochberg do not explicitly mention it, it can also include the built environment, i.e., settlements, cities, industrial areas, etc. Land use is a term that is used to describe a wide range of human activities. The type and intensity of land use not only change the natural environment and thus the living conditions for pathogens but also determine the ecosystems in which people spend time and possibly come into contact with pathogens. Under infrastructure, the authors sum up particularly those technical infrastructures that are connected to pathogen habitats. These can be, for example, defective water pipes on a small scale or systems for water treatment and supply of entire regions on a large scale. Technology and industry also represent a broad category that includes many subcategories from medical technology (e.g., antibiotics, disinfection) to food processing and industrial animal husbandry. Another category is “travel and commerce”, i.e., the movement and encounter of people and goods that are potential reservoirs for pathogens (e.g., import of animals). “Economy” is also listed as a factor, although Van Seventer and Hochberg define it quite narrowly and focus primarily on economic inequality and its consequences for access to hygiene and clean water/food. Closely related to this is the category “war and conflict”. Refugee movements, unhygienic living conditions or a lack of access to clean food are typical consequences of armed conflicts and make it easier for pathogens to spread in the populations affected. “Policy” is also on the list but is somewhat narrowed to policy interventions aimed directly at controlling outbreaks. The final category listed is “social/behavioural” norms and culture. Sociocultural factors shape individuals’ contact or hygiene behavior and, therefore, have a major impact on infection risks [1]. Examples of significant norms are conventions for distance or closeness in everyday encounters, hygiene norms (e.g., regarding hand washing), sexual norms or norms for illness behaviour in the case of a symptomatic illness.
This categorisation of social influences on infectious diseases is not complete. The health care system, for example, and its effectiveness in preventing and treating disease is missing. However, Seventer and Hochberg do not claim to be exhaustive. Their aim is rather to illustrate the importance of social structures and practices and identify important problem areas. Naming individual social factors of influence, however plausible their significance may be in individual cases, can only be a first step. These are not disjunctive categories but, instead, highly interdependent variables. Policy, for instance, influences almost all other categories but is itself also influenced by them (e.g., technical progress can make regulatory action necessary). Furthermore, it is necessary to define and specify idiosyncratic interactions with the other two angles of the triangle, i.e. pathogen and host, for the various social categories.
To grasp the complexity of the social environment and biosocial interactions within the epidemiological triangle better, it might be useful to make references to general theoretical ideas on the social determinants of human health. Nancy Krieger’s ecosocial model [15, 16] is of particular interest in the case of infectious diseases. It builds on more general models of the social determinants of health and extends them by including ecological, epidemiological and medical-sociological ideas of disease causation. First, it postulates that influences on health can manifest themselves on different social levels, from the micro level of social actors to the meso level of social networks and social environments (e.g., households, neighbourhoods, work, consumption/markets, education) to the macro level of social structures and systems (e.g., economic, political, health and legal system). Although the levels are interdependent, they can each be conceptualised as specific environments that influence people’s health-related behaviour in a characteristic way, as well as containing material and psychosocial risks and resources for health. Another important element of the model is the assumption that there is a modification of influences of the social environment by the political economy of a society. This refers to systems of an unequal distribution of resources (e.g., health, power, access to cultural capital, distribution of income and wealth), which are linked particularly to the characteristics of gender, race/ethnicity and social class. Structural distributional inequalities lead to health inequalities in the next step, as socially disadvantaged individuals are more often exposed to potentially harmful environments than better-off people. This structural element is highly significant, as almost all diseases, including infectious diseases, more often affect disadvantaged populations than more privileged populations (health inequalities) [17].
What distinguishes the ecosocial model from related models on the social determinants of health is the explicit consideration of the biosocial processes that link influences of the social environment and human health. According to Krieger, confrontation with the social environment leads to a so-called embodiment—understood as a translation of environmental influences into pathogenic processes. In this context, Krieger speaks of “pathways of embodiment […], that involve exposure, susceptibility, and resistance (as both social and biological phenomena)” [16, p. 225]. Embodiment can thus be understood as the interface between biology and the social environment and is therefore of paramount importance for understanding the genesis of diseases. If these processes are understood, it is possible to assess which social factors can be considered influences in the first place and which biological factors make people particularly susceptible to social influences. If embodiment is interpreted in this way, however, it is necessary to look at this interface in a disease-specific way, since, as is well known, every disease has its own pathology.
However, the ecosocial model has not yet been adapted for the specifics of infectious diseases—even though direct references to the epidemiological triad can be seen in the concept of “pathways to embodiment”. In contrast to chronic degenerative diseases, where exogenous risk factors that arise in the social environment (e.g., noise pollution in a noisy workplace) have an effect on the person and influence their health, in the case of infectious diseases, the pathogen and its peculiarities must be considered an “actor”, so to speak. The social environment is then no longer just something that affects a person via mediators (i.e., risk factors) but can also be, for example, the physical habitat for the pathogen. Exemplarily, a virus that is transmitted directly from person to person spreads particularly effectively in social contexts in which as many people as possible come together physically, be it in large gatherings or through the contacts of mobile populations distributed over a large area. If it succeeds in infecting a large number of people, it becomes part of the social environment itself and can, in turn, infect other, previously unaffected people. At the same time, the social environment shapes the resilience of the members of a community, for example, via the influence that living and working conditions have on the general state of health or the targeted build-up of immunity to pathogens through socially organised vaccination campaigns. Thus, a continuous and dynamic interaction between pathogens, hosts and the social contexts in which they are embedded can be assumed [1, 18]. This idea of interaction is also taken up by Merrill Singer and colleagues in their syndemic concept [19]. They focus on explaining the phenomenon that certain diseases tend to occur together (clustering). However, Singer and colleagues explicitly state that interactions between diseases occur because “contextual and social factors create the conditions in which two (or more) diseases or health conditions cluster” [19, p. 942].
In sum, linking the epidemiological triangle with ecosocial theory could provide a suitable theoretical framework to hypothesise specific roles of social factors in the spread of infectious diseases. As mentioned, the model needs to be adapted to the specificities of infectious diseases. This is not possible in its entirety here due to the complexity of the interactions indicated. Instead, the following section will take a first step by taking a closer look at the process of embodiment in infectious diseases and drawing consequences for the analysis of social environments.
3 Characteristics of Infectious Diseases: Pathways to Embodiment
There are a number of characteristics that distinguish infectious diseases from noncommunicable ones. Knowledge of these is relevant in that the biological characteristics help determine which social influences may be important at different stages of the disease process. In this section, some principles of the biology of infectious diseases are listed to identify possible interfaces with social conditions that make it easier or more difficult for the pathogen to spread. I follow the biological process from exposure to infection to disease and, step-by-step, address pathogen characteristics and their implications for interaction with hosts and social contexts. The explanations are general, make no claim to completeness and are not related to a specific pathogen. To make connections clear, however, COVID-19 is repeatedly used as an example.
4 Transmission: Modes of Transmission
The process begins with the colonisation and infection of a host by the pathogen. The pathway by which this occurs is highly interesting regarding the analysis of social influences, as it is usually directly associated with host behaviour. There are two basic mechanisms: direct transmission of the active pathogen from host to host and indirect transmission of the pathogen via the intermediate step of colonisation or infection of a vehicle [20]. Many pathogens are able to transmit via both routes simultaneously, but the efficiency of transmission may differ depending on the respective route [21].
The two routes can be differentiated further, which will be done here, first, for direct transmission. In this case, there are various modes of transmission, which are generally based on an infected person releasing contaminated material via a portal of exit (e.g., respiratory tract) and this being taken up by another person via a portal of entry [20]. Carriers are primarily body fluids, such as droplets or aerosols, which are released with the respiratory air, blood, breast milk, tear fluid, sweat, semen, vaginal secretions, urine or stool. Which carrier plays a role depends on the pathogen. According to current knowledge, SARS-CoV-2, for example, spreads primarily via secretions that are released with the breath [22, 23]. Droplets, i.e., larger particles of salivary secretion that contain active virus material, are of particular importance. They are produced in larger quantities primarily when speaking (or singing), coughing or sneezing. Due to their size, however, they sink to the ground relatively close to the infected person within a radius of only a few feet [23]. This is important for transmission because infection or initial colonisation by the virus occurs primarily in the upper respiratory tract of the new host. In this respect, a certain physical proximity of one to two metres to the infected subject is necessary to inhale droplets. However, smaller particles (aerosols), which can remain airborne for longer periods and over longer distances, also contain virus material and could initiate infections, especially in closed rooms [24]. In addition, other modes of transmission are also discussed, for example, contact infection through active viruses in stool or urine, which, however, only seem to play a minor role overall [23].
If the transmission properties of the pathogen are known, conclusions can be drawn about social situations that make exposure to a pathogen likely. In the case of SARS-CoV-2, for example, situations in which people come together without much distance and hold conversations or sing/play music together, as well as long stays in unventilated rooms, would be risky. These general considerations allow the identification of concrete social situations in which the risk of transmission is presumably increased. In the case of COVID-19, these would be, for example, visits to concerts with large audiences in confined spaces, working in open-plan offices, meetings in confined spaces and school lessons in crowded classrooms without ventilation. Thus, knowledge of the biological mechanisms involved in the transmission of a pathogen alone allows hypotheses to be made about social contexts with exposure potential. Many public health interventions to control infections are based on such hypotheses. The discussions about nonpharmaceutical interventions must be seen against this background, especially at the beginning of the pandemic when it was still relatively unclear which modes of transmission were important and there was, therefore, a great deal of uncertainty about which measures should be taken [25].
In indirect transmission, on the other hand, the pathogen spreads from one host to another via a so-called vehicle. There are many possible vehicles of transmission. Some pathogens are transmitted through another organism (so-called vector-borne transmission), while others use all possible forms of inanimate matter (e.g., water-borne, airborne, food-borne, object-borne) [21]. Examples are the vector-borne transmission of plasmodia via mosquitoes (Anopheles gambiae) in the case of malaria or the water-borne transmission of the bacterium Vibrio cholerae via contaminated water in the case of cholera [14]. It should be noted that such transmission routes are not always “true” indirect transmissions in the form of a host-vehicle-host chain. There are also pathogens (such as certain bacteria) that permanently colonise inanimate matter and, from there, colonise one host after another. [20] Another variant is that the original host is a vector per se. This applies, for example, to zoonoses, i.e., infectious diseases that can be transmitted from animals to humans. As in the case of direct transmission, knowledge of the vehicles or possible intermediate steps in the infection chain allows general conclusions to be drawn about potentially risky social situations and practices. In the case of vectors, i.e., animals as the source of infection, the characteristics and behaviour of the respective vector become a further relevant factor of transmission in addition to the pathogen properties. In the case of the malaria mosquito mentioned already, staying outdoors or in open spaces during the vector’s active times and without mosquito protection are risky. Zoonoses also affect the relationship between animals and humans, such as the forms and intensity of animal husbandry in agriculture or the conditions under which pets are kept. In the case of transmission via the environment, on the other hand, all of the human everyday behaviour around nutrition and hygiene (e.g., personal hygiene, cleaning of surfaces) potentially plays a role.
5 Transmission: The Natural Environment
Transmission must be seen in the context of the natural environment and its diverse physical and biological phenomena. The pathogens, their vectors and the hosts move within this environment. Pathogens are generally dependent on certain environmental conditions for their spread or are only able to survive under certain conditions. This applies both to their modes of transmission and their general ability to reproduce, for example, in a preferred vehicle. Which ecosystems pathogens prefer is highly individual. There are those that occur exclusively in small ecological niches (often parasites, such as the guinea worm), while other pathogens can potentially exist in very many ecosystems [14]. There is a dependence on environmental characteristics in both direct and indirect transmission. However, for pathogens that primarily transmit indirectly, there is also dependence on the presence of their preferred vehicle [26]. Therefore, the relationships of this vehicle to the environment and its preferred habitats and biotopes must also be considered here. A certain dependence on climatic conditions and their seasonal changes is also typical. The activity, for example, of many pathogens fluctuates along seasonal variations in temperature, rainfall and solar radiation [27, 28]. There are several reasons for this, for example, the availability of vehicles changes with local weather conditions (e.g., standing puddles as breeding sites for mosquitoes) [29]. In addition, the survivability of the pathogen outside of a host can also be influenced by factors such as solar radiation or heat. However, people’s behaviour also changes with seasonal weather, which is important for both direct and indirect transmission: they consume certain foods seasonally, stay outdoors for shorter or longer periods of time, or change their mobility and contact behaviour depending on the environmental conditions. Exemplarily, more encounters take place indoors when it is cold than during periods of high temperatures. On the one hand, this makes the direct transmission of pathogens transmitted via droplets or aerosols more likely; on the other hand, it reduces the probability of infection by a vector whose habitat is outdoors (e.g., ticks).
It is not possible here to begin to comprehensively describe the complex connection between pathogens and the natural environment. The few aspects listed above must therefore suffice to make clear that the embedding of the pathogen in its environment also has consequences for its interaction with the social environment. the questions in which concrete habitats pathogen and host meet and which moderating influence environmental conditions have on the probability of exposure and infection are essential points. These considerations must also be seen in the context of the massive anthropogenic changes that have affected the entire planet since industrialisation and its fossil economy. Not only global climate change and a general change in land use but also socioeconomic change, for example, related to mobility or income distribution, are expressions of this [26]. This also changes the living conditions for pathogens, and it is assumed that there will be more infectious diseases in the future [30]. There are many reasons for this, such as global warming, which makes new geographical zones accessible to certain pathogens (e.g., malaria, dengue fever), or the increase in zoonoses due to the intrusion of immune-naive humans into previously untouched biotopes or through intensified animal husbandry [26, 29]. SARS-CoV-2 is also suspected to be a zoonosis, and the natural environment of the pathogen is in wildlife populations [31]. Only the intrusion of humans into these unspoiled habitats and the capture and sale of creatures for food purposes would subsequently have promoted the spill over.
6 Transmission: Timing
The last aspect to be addressed in the context of transmission is the time period in the course of the stages of infection and disease during which an infected host (source) can infect another host [13, 20]. This is particularly important in the case of direct human-to-human transmission. Once the source is infected, the pathogen usually needs some time to replicate and colonise a new host. The time it takes for an infected person to become infectious and pass on the pathogen is the latent period. This is followed by the period during which the person remains infectious (infectious period). Another variable is the incubation period, i.e., the time between infection and the appearance of the first symptoms of a disease. This is then followed by the period of clinical disease. The ratio of the respective times varies between pathogens and has a strong influence on the effectiveness of transmission. The time interval between the latent and incubation period and the overlap between the infectious period and the duration of a symptomatic disease are of particular importance. Asymptomatic carriers (the latency period is shorter than the incubation period or the infectious period is longer than the clinical period) are especially very efficient in passing on the pathogen. The reason is an interaction with social practices. The appearance of symptoms is an external sign of disease, causing infected people to reduce social contact either independently or at the instigation of third parties (e.g., quarantine rules, inpatient hospitalisation). Asymptomatic carriers, on the other hand, have no reason to avoid social contact and thus cannot actively prevent the possible infection of others. Knowledge of the latency and incubation periods is therefore essential for dealing with outbreaks in society. Only then is it possible to develop appropriate strategies. If, for example, it is known that transmission occurs primarily via asymptomatic carriers, it is imperative to react at the societal level, for example, by carrying out screening tests or imposing contact restrictions for entire populations at risk. In the case of pathogens where the infectious period overlaps strongly with the clinical illness, on the other hand, it is important to educate people to avoid social contact when symptoms appear. In addition, in such a scenario, special attention must be paid to the protection of those who care for the sick.
7 Infectivity and Immunity
As indicated above, an additional distinction must be made between exposure, colonisation and infection. The exposure and subsequent colonisation do not necessarily mean that the pathogen also succeeds in infecting the person affected. This is determined by an interplay between the characteristics of both the pathogen and host. First, pathogens differ in terms of their infectivity, i.e., their general ability to infiltrate the organism of the host. Both the biological mechanism of infiltration and the dose of exposure required to enable the pathogen to infiltrate are decisive. SARS-CoV-2, for example, has high infectivity according to current knowledge. The virus, especially in its later variants (Delta, Omicron), infiltrates cells highly effectively by docking with its spike protein to cell receptors (i.e., angiotensin-converting enzyme 2 receptor: ACE2) and subsequently use the protein production of the cell to replicate and establish itself in the body of the new host [32]. However, the success of an infection also depends on the viral load to which the person is exposed [33]. This means that an infection becomes more likely if a high amount of virus is ingested in contact with infected people who excrete high amounts of virus (e.g., during particularly infectious stages of the disease or in the case of “superspreaders” who excrete an above-average viral load) [23].
However, the pathogen’s ability to infect now comes up against the host’s defense, which, in the context of infectious diseases, is referred to as susceptibility, i.e., the individual probability of becoming infected when exposed to the pathogen. [14] On a biological level, susceptibility is determined primarily by the immune system (although other factors also play a role, but this would go too far here). The human immune system is highly complex and can only be described here in a general way. What is important is that it has both a general, innate component and a variable, adaptive component. The innate immune system is not very specialised and operates against all pathogens it can recognise. Numerous processes are involved, such as the initiation of inflammation or the destruction of infected body cells by natural killer cells. The second component is the adaptive immune system, which is capable of learning and developing specific responses for individual pathogens. Immune memory is built up by previous infections with this pathogen or external immunisation (i.e., vaccination). If contact occurs again, the pathogen can be recognised, and an immune response tailored to it can be initiated, for example, by killer T cells [14]. Nevertheless, there is marked variance between hosts regarding the effectiveness of both the innate and adaptive immune responses, which means that some people are more susceptible than others. The variance may be the result of normal genetic diversity, but often the effectiveness of the immune system is associated with other characteristics. One key factor is age. The adaptive immune system, for example, must first be trained; thus, newborns or infants naturally have weaker defences against pathogens. The functionality of the immune system in older age then decreases again as a result of ageing processes, which also tends to make older people more susceptible. In addition, the immune systems of men and women differ slightly, which can lead to a different susceptibility of the biological sexes depending on the pathogen. Such a difference has been observed with SARS-CoV-2. The T-cell response of women to the virus seems to be more robust than that of men; consequently, the infection rates of men are higher than those of women [34]. However, the immune system is not only determined by biological characteristics but also influenced by external social factors. One of these, chronic stress, has been shown to affect the immune system negatively [35, 36]. Since chronic stress is predominantly a product of social stressors, such as confrontation with aggressive behaviour, the experience of poverty and exclusion or poor working conditions, there are direct social influences on immunity here. Indirect immunisation through vaccination is also genuinely socially mediated, since vaccinations have to be developed by scientific institutions and made accessible by both the political and health systems.
Furthermore, the immune system is also influenced by the general constitution or resistance of the organism. Preexisting conditions such as metabolic disorders (e.g., diabetes) can weaken the immune system. The same applies to patients with diseases that are treated by specifically reducing the immune system with medication. Immunosuppressants, for example, are used in the treatment of various tumours, resulting in cancer patients becoming susceptible to infections. It should be noted that the general constitution is also determined to a great extent by social living and working conditions. Most widespread chronic diseases have a multicausal aetiology, and their development usually involves numerous social factors, such as socioculturally shaped lifestyles, stress or material disadvantage.
8 Pathogenicity and Virulence
If an infection occurs, immunity and constitution remain important, as they also influence the course of the infectious disease. Two characteristics of the pathogen are decisive here. Pathogenicity refers to the probability that an infection will also result in a symptomatic disease, while virulence refers to the severity or danger of a disease [20]. There is a high variance between different pathogens for both factors. Some of them rarely cause clinical disease, while others almost always lead to symptoms when infected. The dangerousness also differs. The most drastic indicator is the probability of a fatal course (case fatality). This is very low for pathogens such as normal cold viruses (e.g., rhinoviruses), while other pathogens, such as Ebola, have very high lethality.
Influences on the resistance of the hosts and the role of social factors have already been discussed in the previous section. However, at this stage of the disease, there are further interactions with the social environment. The pathogenicity of a pathogen is important in several respects for the social reactions to a disease. First, it determines how the social life of an affected society changes. If the pathogenicity is high and, simultaneously, the number of people infected is considerable, a large number of people will fall ill at the same time during an outbreak. On the one hand, this increases the need for medical care and, thus, the pressure on the health system. On the other hand, these infected people can no longer pursue their normal social roles for the duration of their illness. This can have consequences in many areas of society, especially if employees are absent in large numbers and economic life is disrupted as a result, or if care work is no longer performed and has to be compensated for in some other way. During the COVID-19 pandemic, for example, essential workers were temporarily affected by staff shortages. These were not only particularly health professionals but also employees in the transport sector and the food industry [37, 38]. Such outages can threaten the security of supply and health care and have further negative consequences for the health of the population. The lethality of a disease is also a pathogen characteristic that determines societal responses. It is obvious that the willingness to implement far-reaching measures to protect against infection will be significantly stronger in the case of a particularly lethal disease than an infection with only low lethality.
9 Conclusions
Biosocial interactions between the biological characteristics of pathogens or infectious diseases and social factors have been discussed in this chapter. However, the theoretical study of the biosocial basis of the spread of infectious diseases is not an end in itself. The COVID-19 pandemic has clearly shown that measures taken to prevent and control pandemics work, above all, if they interrupt chains of infection precisely and reduce susceptibility and vulnerability. The selection of such measures depends on the precise knowledge of both the biological properties of the pathogen and the social framework of embodiment. In preparation for future pandemics, it may therefore be useful to further develop the theoretical framework and test it empirically in a targeted manner.
The proposal was made here to fall back on a classic model of infectious disease causation but to combine it with a model of social determinants to be able to describe the interface between the biological properties of pathogens and hosts and the social environment in a conceptually better way. In my opinion, the theoretical analysis shows that Nancy Krieger’s ecosocial theory is quite compatible with the assumptions of the epidemiological triangle. In this respect, it could be worthwhile in the future to develop an ecosocial model specifically for infectious diseases. This was only possible here as an example, and numerous possible systematics could just be hinted at. It would be desirable, for example, to further develop the taxonomy of relevant social contexts or of individual social factors on the occurrence of infections. To date, only general, incomplete category lists are available. In addition, the modes of action of the respective context factors and their different significance depending on certain pathogen characteristics still need to be understood better and systematically described.
Furthermore, it could be useful to continue the research on the biosocial basis of pathogen transmission and thus to work out the pathways to embodiment more clearly. From the knowledge of the biological properties of pathogens, it is possible, in principle, to deduce which social practices, situations and structures are associated with the probability of exposure, susceptibility and vulnerability to critical courses. If it is possible to determine generalisable principles of biosocial interactions as a function of the biological properties of pathogens, this could make it easier in the future to estimate which spreading dynamics can be expected when a specific pathogen encounters certain social conditions. It would be, for instance, conceivable to draw up a kind of checklist of individual pathogens or pathogen groups properties that could provide orientation in the assessment of a current outbreak. This could also provide lessons for the early identification of social groups that are particularly vulnerable in terms of risk of infection and/or severe courses. During the COVID-19 pandemic, for example, socially disadvantaged people had a higher than average burden of disease because their specific living and working conditions made protective behaviours difficult and exposure to the virus more likely (e.g., cramped housing, need to use public transport). Although this health inequality was uncovered by empirical studies relatively early in the pandemic, it was initially little noticed by the public in many countries; consequently, only sporadic policy measures were taken to protect these particularly vulnerable groups [8]. Therefore, systematic preparation for pandemics, which is also oriented towards the biosocial basis of the spread of infections, seems necessary to prevent such inequalities in the future.
Core Messages
-
In the spread of infectious diseases, specific interactions between the biological properties of the pathogen and the host, as well as the social context in which this interaction takes place, play an important role.
-
In order to describe biosocial interactions theoretically, classical concepts of epidemiology can be linked with public health theories. Plausible connections arise, for example, between the epidemiological triangle model and the ecosocial theory.
-
Vulnerabilities can be both biological (e.g. an increased biological susceptibility of a person to become infected with a specific pathogen) and socially based (e.g. social disadvantage). As both aspects interact, a multidimensional conception of vulnerability seems to be necessary.
A continuous and dynamic interaction between pathogens, hosts and the social contexts in which they are embedded can be assumed.
Nico Dragano.
References
Arthur RF, Gurley ES, Salje H et al. (2017) Contact structure, mobility, environmental impact and behaviour: the importance of social forces to infectious disease dynamics and disease ecology. Philos Trans R Soc Lond B Biol Sci 372. https://doi.org/10.1098/rstb.2016.0454
Butler-Jones D, Wong T (2016) Infectious disease, social determinants and the need for intersectoral action. Can Commun Dis Rep 42:S118-S120. https://doi.org/10.14745/ccdr.v42is1a04
Kelly-Irving M, Delpierre C (2021) Framework for understanding health inequalities over the life course: the embodiment dynamic and biological mechanisms of exogenous and endogenous origin. J Epidemiol Community Health 75:1181–1186. https://doi.org/10.1136/jech-2021-216430
Kerrigan D, Donastorg Y, Barrington C et al (2020) Assessing and addressing social determinants of HIV among female sex workers in the Dominican Republic and Tanzania through community empowerment-based responses. Curr HIV/AIDS Rep 17:88–96. https://doi.org/10.1007/s11904-020-00485-3
Benita F, Rebollar-Ruelas L, Gaytán-Alfaro ED (2022) What have we learned about socioeconomic inequalities in the spread of COVID-19? A systematic review. Sustain Cities Soc 86:104158. https://doi.org/10.1016/j.scs.2022.104158
McGowan VJ, Bambra C (2022) COVID-19 mortality and deprivation: pandemic, syndemic, and endemic health inequalities. Lancet Public Heal 7:e966–e975. https://doi.org/10.1016/S2468-2667(22)00223-7
Bambra C (2022) Pandemic inequalities: emerging infectious diseases and health equity. Int J Equity Health 21:6. https://doi.org/10.1186/s12939-021-01611-2
Sirleaf EJ, Clark H (2021) Report of the independent panel for pandemic preparedness and response: making COVID-19 the last pandemic. The Lancet. https://doi.org/10.1016/S0140-6736(21)01095-3
Snieszko SF (1974) The effects of environmental stress on outbreaks of infectious diseases of fishes. J Fish Biology 6:197–208. https://doi.org/10.1111/j.1095-8649.1974.tb04537.x
Scholthof K-BG (2007) The disease triangle: pathogens, the environment and society. Nat Rev Microbiol 5:152–156. https://doi.org/10.1038/nrmicro1596
Alberts B, Johnson A, Lewis J et al (2002) Molecular biology of the cell, 4th edn. Garland Science Taylor & Francis Group, New York
Fox MW, Gower EW (2021) Infecious disease epidemiology. In: Lash TL, VanderWeele TJ, Haneuse S et al. (eds) Modern epidemiology, 4th edn. Wolters Kluwer, Philadelphia, Baltimore, New York, Buenos Aires, Hong Kong, Sydney, Tokyo, pp 805–843
van Seventer JM, Hochberg NS (2017) Principles of infectious diseases: transmission, diagnosis, prevention, and control. Int Encyclo Public Health, pp 22–39. https://doi.org/10.1016/B978-0-12-803678-5.00516-6
Abubakar I, Stagg HR, Cohen T et al (eds) (2016) Infectious disease epidemiology, 1st edn. Oxford specialist handbooks in infectious diseases. Oxford University Press, Oxford
Krieger N (2001) Theories for social epidemiology in the 21st century: an ecosocial perspective. Int J Epidemiol 30:668–677. https://doi.org/10.1093/ije/30.4.668
Krieger N (2008) Proximal, distal, and the politics of causation: what’s level got to do with it? Am J Public Health 98:221–230. https://doi.org/10.2105/AJPH.2007.111278
Bartley M (2017) Health inequality: an introduction to concepts, theories and methods, 2nd edn. Polity, Cambridge, UK, Malden, MA, USA
Bonds MH, Keenan DC, Rohani P et al (2010) Poverty trap formed by the ecology of infectious diseases. Proc Biol Sci 277:1185–1192. https://doi.org/10.1098/rspb.2009.1778
Singer M, Bulled N, Ostrach B et al (2017) Syndemics and the biosocial conception of health. The Lancet 389:941–950. https://doi.org/10.1016/S0140-6736(17)30003-X
Krämer A, Akmatov M, Kretzschmar M (2010) Principles of infectious disease epidemiology. In: Krämer A, Kretzschmar M, Krickeberg K (eds) Modern infectious disease epidemiology: concepts, methods, mathematical models, and public health. Springer, New York, pp 85–99
Giesecke J (2017) Modern infectious disease epidemiology, 3rd edn. CRC Press, Boca Raton
Handiso TB, Jifar MS, Nuriye Hagisso S (2022) Coronavirus's (SARS-CoV-2) airborne transmission. SAGE Open Med 10. https://doi.org/10.1177/20503121221094185
Meyerowitz EA, Richterman A, Gandhi RT et al (2021) Transmission of SARS-CoV-2: a review of viral, host, and environmental factors. Ann Intern Med 174:69–79. https://doi.org/10.7326/M20-5008
Baselga M, Güemes A, Alba JJ et al. (2022) SARS-CoV-2 droplet and airborne transmission heterogeneity. J Clin Med 11. https://doi.org/10.3390/jcm11092607
Leclerc QJ, Fuller NM, Knight LE et al (2020) What settings have been linked to SARS-CoV-2 transmission clusters? Welcome Open Res 5:83 https://doi.org/10.12688/wellcomeopenres.15889.2
Hassell JM, Newbold T, Dobson AP et al (2021) Towards an ecosystem model of infectious disease. Nat Ecol Evol 5:907–918. https://doi.org/10.1038/s41559-021-01454-8
Grassly NC, Fraser C (2006) Seasonal infectious disease epidemiology. Proc Biol Sci 273:2541–2550. https://doi.org/10.1098/rspb.2006.3604
Rohr JR, Cohen JM (2020) Understanding how temperature shifts could impact infectious disease. PLoS Biol 18:e3000938. https://doi.org/10.1371/journal.pbio.3000938
Rossati A (2017) Global warming and its health impact. Int J Occup Environ Med 8:7–20 https://doi.org/10.15171/ijoem.2017.963
Watts N, Amann M, Ayeb-Karlsson S et al (2018) The Lancet Countdown on health and climate change: from 25 years of inaction to a global transformation for public health. The Lancet 391:581–630. https://doi.org/10.1016/S0140-6736(17)32464-9
Holmes EC, Goldstein SA, Rasmussen AL et al (2021) The origins of SARS-CoV-2: a critical review. Cell 184:4848–4856. https://doi.org/10.1016/j.cell.2021.08.017
Da Silva SJR, Kohl A, Pena L et al (2023) Recent insights into SARS-CoV-2 omicron variant. Rev Med Virol 33:e2373. https://doi.org/10.1002/rmv.2373
Barreto ML, Teixeira MG, Carmo EH (2006) Infectious diseases epidemiology. J Epidemiol Community Health 60:192–195. https://doi.org/10.1136/jech.2003.011593
Takahashi T, Ellingson MK, Wong P et al (2020) Sex differences in immune responses that underlie COVID-19 disease outcomes. Nature 588:315–320. https://doi.org/10.1038/s41586-020-2700-3
Austin MK, Chen E, Ross KM et al (2018) Early-life socioeconomic disadvantage, not current, predicts accelerated epigenetic aging of monocytes. Psychoneuroendocrinology 97:131–134
Marques AH, Bjørke-Monsen A-L, Teixeira AL et al (2015) Maternal stress, nutrition and physical activity: impact on immune function, CNS development and psychopathology. Brain Res 1617:28–46. https://doi.org/10.1016/j.brainres.2014.10.051
Lyttelton T, Zang E (2022) Occupations and sickness-related absences during the COVID-19 pandemic. J Health Soc Behav 63:19–36. https://doi.org/10.1177/00221465211053615
Reuter M, Rigó M, Formazin M et al (2022) Occupation and SARS-CoV-2 infection risk among 108 960 workers during the first pandemic wave in Germany. Scand J Work Environ Health 48:446–456. https://doi.org/10.5271/sjweh.4037
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Dragano, N. (2023). A Biosocial Perspective on (COVID-19) Pandemic Outbreaks: Interfaces of Biology and Social Determinants. In: Achella, S., Marazia, C. (eds) Vulnerabilities. Integrated Science, vol 18. Springer, Cham. https://doi.org/10.1007/978-3-031-39378-5_5
Download citation
DOI: https://doi.org/10.1007/978-3-031-39378-5_5
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-39377-8
Online ISBN: 978-3-031-39378-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)