Abstract
In the face of emerging health situations, such as COVID-19, the psychosocial risk factors that lead to professional burnout are exacerbated in general comprehensive medicine (MGI) specialists, as they are the first response personnel to the crisis. This descriptive cross-sectional study was carried out between April and July 2020 at the Elena Fernández Castro Polyclinic in Los Palacios, Pinar del Río, Cuba, to determine the risk factors that influenced professional burnout in MGI specialists working in the offices in the center of the city. A total of 28 specialists completed the Burnout Assessment Inventory (MBI), the 10 Wishes technique, and an in-depth interview. The results showed that 76% of them were affected by professional burnout. Significant associations also appeared with factors such as work overload, lack of perceived control, and community breakdown at work. It is concluded that social and labor-related risk factors associated with burnout affected physicians.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Stress at work has been one of the major concerns of the field of health psychology. Physical conditions, organizational demands, task demands, interpersonal relationships, and individual or personological variables have been identified as some of the underlying organizational factors of it (Zaldívar, 2017). When stress is overwhelming and disrupting, it can lead someone to feel burnout. The Professional Burnout Syndrome (PFS) also known as Professional Exhaustion Syndrome (PAS) “is a response to chronic job stress characterized by demotivation, disinterest, internal discomfort or job dissatisfaction that seems to affect to a greater or lesser extent a significant professional group” (Borda et al., 2007, p. 14).
Some models linked to organizational theory explain burnout on the basis of organizational factors. Leiter et al. (2001), for example, maintain that burnout does not attribute the problem to the individuals themselves, but to the social environment in which they work, since the structure and functioning of the workplace affect the interaction of individuals and the way in which they carry out their work. According to the psychosocial perspective of Maslach et al. (2001), the main parameters that identify the syndrome are emotional fatigue, depersonalization, and lack of personal fulfillment.
PDS is considered by the World Health Organization (WHO) as an occupational hazard. Its incidence is between 43 and 45% in general practitioners and between 22 and 60% in specialists (Puertas et al., 2015). Currently, there is a need to know the factors that affect the wellbeing and occupational health of these professionals (Do Carmo et al., 2010). Some studies have followed a line of research that tries to clarify the causal, modulating, antecedent, and consequent variables of burnout in health professionals (Chacón Roger & Grau, 2004). Some significant antecedents on the subject are the works of Boyle et al. (1991), Chacón Roger (1995), and Gil et al. (1996).
Certain stressful characteristics of working conditions in the medical profession are frequently related to the onset of the syndrome. These include the relationship with patients and their families, daily contact with death and pain, responsibility for the health of others, shift work, pressure of care, workload, social pressure, dealing with emergency situations, mismatch of expectations, and organizational situations such as lack of promotion, inequity in treatment or problems with supervisors. Primary care professionals also face less planning and coordination of teamwork, greater uncertainty about the adequacy of treatments and greater time pressure that moves between the poles of health and illness, life, and death; elements that organizationally also constitute risk factors for professional burnout.
The situation produced by the COVID-19 pandemic in itself constitutes a stressor, especially for medical personnel. Primary health care professionals had a high degree of commitment to providing care and they were responsible for monitoring and surveilling the disease as well. In addition, research work, priority surveillance of risk groups, and the care they must take to avoid becoming infected with the disease compounded their daily workload. All these circumstances caused significant degrees of professional exhaustion by increasing their feelings of anxiety, insecurity, fear, and depression at the possibility of getting sick, and the responsibility of watching over their work area.
Healthcare organizations must prioritize caring for their own teams of professionals because dealing with the psychological, social and/or physical issues of patients on a regular basis increases their potentially vulnerability to chronic stress, emotional exhaustion, and professional burnout. Otherwise, the quality of life of these professionals will suffer and the organizations in which they work will face serious repercussions.
Given this reality, we sought to answer the following question: What were the risk factors that affected the level of professional burnout among physicians specializing in General Integral Medicine (GIM) at the Elena Fernández Castro Polyclinic, in the municipality of Los Palacios in the period April–June 2020, during the COVID-19 pandemic?
Method
Design
A descriptive, non-experimental, cross-sectional, correlational, descriptive correlational study was carried out using a quantitative and qualitative (mixed) methodology based on a phenomenological approach.
Sample
The study population consisted of 33 professionals who provided medical assistance at the Elena Fernández Castro Polyclinic in the municipality of Los Palacios during the period April–June 2020. Professionals who had not graduated as specialists and who had been working at the Polyclinic for less than 6 months were excluded. A probabilistic sample design was used to randomly select 25 physicians.
Instrument
The study used two data collection techniques: inventories and interviews. The Maslach Burnout Inventory (MBI) was administered to identify the presence or absence of Burnout Syndrome. It includes 22 items that measure the three dimensions of the syndrome: Emotional Fatigue (EF), Depersonalization (PD), and Personal Fulfillment (PR). Each item has seven response options, only one of which is answered. Each response option is assigned a value from zero to six, with the score for each dimension being the sum of these values.
In-depth interviews with participants were carried out with the objective of obtaining more extensive information about their experiences and perceptions about professional life and how these could affect their professional burnout during this stage.
Finally, participants were asked to mention 10 wishes, a technique applied in organizational psychology with the aim of identifying more concretely the group’s needs, conflicts, frustrations, as well as future goals and aspirations in the work environment. This helped us to delve deeper into the presence of professional burnout in each participant.
Statistical Analyses
After the scoring of the instruments, a statistical analysis of the levels of Burnout and its dimensions was carried out using the SPSS statistical package for Windows. Subsequently, the results of the instruments were integrated, obtaining information on the presence of professional burnout and descriptions of the relationship of burnout with social and organizational variables.
Results
As shown in Fig. 36.1, most of the specialists consulted showed high (40%) and intermediate (36%) levels of professional burnout. When breaking down the results obtained in each of the three dimensions of the Burnout Assessment Inventory (MBI), it is possible to observe that 68% of the participants were affected by a high level of emotional exhaustion (see Table 36.1).
This result was qualitatively corroborated by the other techniques utilized. In the analysis of the in-depth interviews, content emerged on how agents external to the nature of the work itself were the ones that most frequently led to physical and emotional exhaustion. Factors such as the demands of managers and superiors, and the number of tasks to be performed in addition to care work, which participants often felt insufficient, pressured, overwhelmed, and often hindered their work. Some of the responses were as follows: “They send us to comply with a number of indicators that are very difficult to fully comply with and even more so in a situation like this,” “the number of things you have to do to comply with the established indicators robs us of the time to attend to the patient which is what is really important to me,” “it is necessary to decrease paperwork to work and dedicate more time to people and to the surveillance now added with COVID-19.”
When discussing the feelings experienced by these professionals in the face of work demands, feelings of exhaustion, obstinacy, pressure, tiredness, stress, eagerness, frustration, negativity, pessimism, and discouragement were evoked. Exhaustion and tiredness were the most recurrent within their criteria. The MBI revealed that the most endorsed items were “I feel tired at the end of the workday,” “working all day with many people is an exhausting effort,” and “working with people causes me stress”; with scores at the highest level resulting in a high level of emotional exhaustion. Most of the specialists agreed that it was very stressful to work all day with many people, citing difficult interactions with patients, the number of people seen per day, the lack of resources for the effective treatment of patients, and the demands that patients made on the medical staff.
Emotional fatigue was also identified in this group through physical symptoms and the negative reactions they experienced in relation to their work. During the interview, the physicians consulted said they felt upset, bad-tempered, worried, and tense when dealing with unfulfilled demands after the workday. One of them even reported sleep disorders such as insomnia and the use of psychotropic drugs to help them sleep: “I almost always have to take psychotropic drugs to sleep, the worries of the other day disturb my sleep, so my physical performance for the next day suffers a lot”; others complained of headaches, neck, and joint pain. Some of their answers mentioned: “after finishing the day I feel very stressed, I end up with headache and bad mood,” “when I finish work, I feel very exhausted and with a lot of pain in my neck.”
Depersonalization as a dimension of professional burnout, as can be seen in Table 36.1, was at a low level in our sample, representing 60% of the sample. Going deeper with these professionals in the interview, it was found that their current workload had a negative influence on their work with patients; because when burnout is too much, the behavior and treatment of patients and even colleagues tend to be complex, sometimes causing discomfort and leading to negative feelings and responses towards patients, their superiors, and colleagues. Some said: “in my tiredness and exhaustion I do not attend to the patient as I should and stress levels then increase,” “after finishing my working day I cannot stand society,” “when I feel too burdened by work, I do not want to talk or be talked to.”
Guilt or dissatisfaction at work was an important aspect that sometimes overlapped with defensive and negative attitudes experienced by these professionals, which led to emotional hardening at work. Problems caused by such feelings usually accelerate the process towards burnout, even affecting the professional’s self-esteem and effectiveness at work. The feeling of being blamed by others for their problems became an important aspect within the group, as well as the undisciplined behavior of patients and their companions, and their overestimated expectations of the physicians’ ability to work. Many of them were blamed by companions and relatives for the negative evolution of cases, as well as for factors beyond their power, such as lack of transportation (ambulance), out-of-date equipment, lack of resources and medicines to treat certain pathologies. This generated a feeling of discomfort, stress, dissatisfaction at work, low esteem for their work and the profession in general, which is a symptom directly related to the personal fulfillment of these professionals, which is of vital interest for our study.
Some data exemplified the above, such as: “patients were sometimes very undisciplined and came to question your work as a professional and even offend you without taking into account that as a professional you are doing the best you can and this eventually affects how you work with patients,” “some patients held us responsible for the shortages that exist in the country, of medicines, equipment, and even transportation to the hospital and that made us feel very bad,” “others lied about their symptoms for fear of being admitted to quarantine and that made the work more complex.”
Lack of personal fulfillment was a dimension that was also found to be affected in this group. Although the majority (60%) reported low levels in this area, as shown in Table 36.1, 40% had medium and high levels that contributed to the presence of professional burnout. Lack of personal fulfillment leads to negative responses and evaluations of oneself and one’s own work, as well as to low morale, frustration at work, rejection, and avoidance of interpersonal relationships in the workplace.
The most significant items in this dimension according to the MBI were: “I feel stimulated after working with people,” “I have achieved many useful things in my profession,” “I feel very active.” When interviewing the participants in depth, they said they did not feel very stimulated after working with people, associated with the number of patients they see in a day and the overload of work they experienced.
The need for recognition emerged as one of the fundamental needs for this group, alleging that their daily work went unnoticed by the managers, who, as spokespersons for labor demands and then for compliance, usually forget the human resource. They said that there was no space to stimulate or recognize physicians, instead they get demands, reprimands, and more work; for example, some participants stated: “more than material stimuli, which are nonexistent in our system, it is necessary that, just as we are demanded, we are also recognized for the effort of the work that becomes so complex every day,” “however you work, the only thing that matters is the fulfillment of the indicators, there is no time to show the good results, but there are plenty of meetings to show what is not going well.”
Working conditions were another of the factors that most threatened personal fulfillment. The lack of transportation for medical personnel, as well as the lack of instruments for the exercise of the profession, including the physical conditions of some offices: “if there is no equipment, sometimes you cannot perform procedures,” and the conditions for on-call physicians, especially in terms of food. Feelings of incapacity and of not being able to fulfill all the tasks that are demanded of them are other frustrations experienced by this group and some came to believe that the profession was beyond them: “yes, I have thought about not being able to comply and quit; it is too much of a burden and the stress it generates.” They also added the lack of opportunities for improvement, as well as the lack of ethics, and respect for the medical staff on the part of the managers.
Discussion
The present study was carried out to identify and understand the risk factors that influenced the levels of burnout in physicians specializing in General Comprehensive Medicine who worked in the offices of the Elena Fernández Castro Polyclinic during the COVID-19 pandemic, between April and June of 2020, in the municipality of Los Palacios.
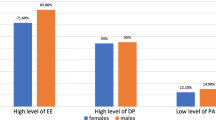
Our findings revealed that 76% of the physicians studied showed medium and high levels of professional burnout. When analyzing the dimensions of professional burnout, the results obtained showed that 68% of the participants had a high level of emotional exhaustion and 60% had a low level of personal fulfillment. Additionally, 16% showed a high level of depersonalization.
The high score obtained in the emotional exhaustion subscale by 68% of the sample was qualitatively corroborated by the other techniques used in the study. Recent research on triggering factors of burnout syndrome (García et al., 2016) found that 82% of the respondents showed a high level of emotional exhaustion. These results were similar to those obtained by us.
Lack of personal fulfillment was another dimension that was also found to be quite affected in this group. With 60% of the sample scoring at a low level of personal fulfillment, this finding coincides with those obtained by Sanjuan et al. (2014) in their research on burnout in nurses working in oncology services, as well as those found in the study by Gutiérrez et al. (2018) where 70% of the sample possessed low levels of personal fulfillment.
This unsatisfied need for self-improvement, together with the overwork experienced, plus the feeling that they did not always achieve the expected results, confirms the results of the burnout assessment inventory on the low personal fulfillment or, in other words, lack of personal fulfillment of these professionals.
As noted above, the literature indicates that organizational variables best predict the occurrence of the syndrome. Our study included a series of organizational aspects that allowed us to conclude that there were occupational risk factors associated with burnout that affected the health of the physicians, especially in times such as those that occurred in the early stage of the COVID-19 pandemic (Figs. 36.1 and 36.2).
References
Borda, M., Navarro, E., Aun, E., Berdejo, H., Racedo, K., & Ruiz, J. (2007). Síndrome de Burnout en estudiantes de internado del Hospital Universidad del Norte. Salud Uninorte, 23(1), 43–51. https://rcientificas.uninorte.edu.co/index.php/salud/article/view/4054
Boyle, A., Grap, M., & Younger, J. (1991). Personality hardiness, ways of coping, social support, and burnout in critical care nurses. Journal of Advanced Nursing, 16(7), 850–857. https://doi.org/10.1111/j.1365-2648.1991.tb01767.x
Chacón Roger, M. (1995). El Burnout en personal de enfermería. Congreso Internacional de Dolor y Cuidados paliativos.
Chacón Roger, R., & Grau, J. A. (2004). Burnout y variables personales moduladoras en enfermeros que trabajan en hospitales oncológicos (INOR). Psicología y Salud, 14(1), 67–78. https://doi.org/10.25009/pys.v14i1.867
Do Carmo, M., Chaves, M., Marchi, R., Almeida, L., Oliveira, A., & Pedrão, L. (2010). Exceso de trabajo y agravios mentales a los trabajadores de la salud. Revista Cubana de Enfermería, 26(1), 52–64. http://scielo.sld.cu/pdf/enf/v26n1/enf09110.pdf
García, P. E., Gatica, M. L., Cruz, E. R., Luis, K., Vargas, R., Hernández, J., Ramos, V. A., & Macías, D. M. (2016). Factores que detonan el Síndrome de Burnout. Revista Iberoamericana de Contaduría, Economía y Administración, 5(9) https://www.ricea.org.mx/index.php/ricea/article/view/56
Gil, P. R., Peiró, J. M., & Valcárcel, P. (1996). Influencia de las variables de carácter sociodemográfico sobre el síndrome de Burnout: Un estudio en una muestra de profesionales de enfermería. Psicología Social Aplicada, 6(2), 37–57.
Gutiérrez, O., Loboa, N., & Martínez, J. (2018). Prevalencia del Síndrome de Burnout en profesionales de enfermería de la Orinoquia colombiana, 2016. Universidad y Salud, 20(1), 37–43. https://doi.org/10.22267/rus.182001.107
Leiter, M. P., Harvie, P., & Churchill, L. (2001). Abusive interactions and burnout: Examining occupation, gender, and the mediating role of community. Psychology and Health, 16, 547–563. https://doi.org/10.1080/08870440108405526
Maslach, C., Schaufeli, W. B., & Leiter, M. P. (2001). Job Burnout. Annual Review of Psychology, 52, 397–422. https://doi.org/10.1146/annurev.psych.52.1.397
Puertas, A., García, J., & Rosete, V. (2015). Síndrome de burnout (quemado) en médicos residentes adscritos a hospitales del Grupo Ángeles: HA Clínica Londres, HA Lomas, HA Metropolitano, HA México, HA Mocel y HA Pedregal. Acta Médica Grupo Ángeles, 13(2), 69–81.
Sanjuan, E., Arrazola, L., García, O., & Loreto, M. (2014). Prevalencia del Síndrome del Burnout en el personal de enfermería del Servicio de Cardiología, Neumología y Neurología del Hospital San Jorge de Huesca. Enfermería Global, 36(253), 253–264.
Zaldívar, D. (2017). Estrés en el ámbito laboral. Trabajadores.. http://www.trabajadores.cu/20170312/estres-ambito-laboral
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Díaz Sánchez, L.L., Gutiérrez Iglesias, D. (2023). Professional Burnout Risk Factors for Medical Personnel Working in Primary Health Care in Cuba During the COVID-19 Pandemic. In: Portillo, N., Morgan, M.L., Gallegos, M. (eds) Psychology and Covid-19 in the Americas. Springer, Cham. https://doi.org/10.1007/978-3-031-38502-5_36
Download citation
DOI: https://doi.org/10.1007/978-3-031-38502-5_36
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-38501-8
Online ISBN: 978-3-031-38502-5
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)