Abstract
Outcomes of normal pressure hydrocephalus (NPH) treatment has been under investigation for over 40 years. The first reports disclosed relatively high complication rates, directly related to surgery. Even postoperative improvement rates were incomparably small compared to results nowadays. This is primarily due to advances in shunting devices, a better understanding of the disease pathogenesis, and more precise identification of NPH patients.t is now possible to target the treatment more efficiently and thus achieve better treatment outcomes with minimal surgery-related complications. Selected up-to-date reports show that over 75% of iNPH patients improve after surgery, regardless of the indication criteria and cerebrospinal fluid (CSF) diversion techniques. Despite a lot of effort to sustain initial improvement in clinical outcomes after shunt implantation, the improvement tends to decline with longer follow-ups. Although the understanding of the disease’s pathophysiology has unquestionably improved, and an enormous body of literature dedicated to the investigation of NPH-characteristic parameters (both clinical and radiological) has been published, the main problem of NPH diagnosis remains the same. The frequent occurrence of neurodegenerative diseases and other comorbidities in the elderly is an important factor implicating treatment outcome and prognosis of NPH patients. Surgical candidates are selected according to the expected postoperative improvement of clinical symptoms. If any of the symptoms of the clinical triad do not improve after surgery, it is important to investigate it in more detail, usually referring the patient to another specialist (urologist, neurologist etc.). The results of outcomes vary which may be explained by the frequent occurrence of comorbidities. The proper identification of comorbidities should be included as a central part of NPH management. This chapter is dedicated to both early and long-term results of NPH treatment, where we aim to discuss individual nuances involving treatment outcomes, as well as specific prognosis for NPH patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Normal pressure hydrocephalus treatment prognosis
- NPH prognosis
- NPH diagnosis
- Shunt surgery
- Long-term shunt outcomes
1 Introduction
Clinical outcomes of normal pressure hydrocephalus (NPH) treatment reported in the literature vary. Possible reasons include different indication and improvement criteria, different postoperative follow-up methods, degree of comorbidities, non-discrimination of aetiologies -idiopathic normal pressure hydrocephalus (iNPH) versus secondary normal pressure hydrocephalus (sNPH), different duration or degree of clinical symptoms, different treatment modalities, differences in shunt systems and other factors [1,2,3,4]. On average, over 75% of iNPH patients improve after surgery, regardless of the indication criteria and CSF diversion techniques in the selected studies [5]. Treatment of NPH typically involves implantation of a shunt device which provides a diversion of the cerebrospinal fluid to a different part of the body where the fluid is absorbed. The role of endoscopic third ventriculostomy (ETV), which is routinely used in the treatment of obstructive hydrocephalus, remains controversial in NPH treatment [6]. Mitchell and Mathew introduced ETV in the treatment of iNPH patients in 1999 but 75% of four patients in their cohort ended up with a ventriculoperitoneal (VP) shunt [7]. Since then, several low-quality studies and case series have been published with promising results suggesting that ETV may restore CSF dynamics and pulsatility patterns in NPH. The authors of the retrospective review on ETV in iNPH from 2016 base the effectivity of ETV on ‘modified bulk flow theory’, with the proviso that every hydrocephalus is obstructive, and that ETV would make sense, especially in the case of functional stenosis of the aqueduct [8]. Nevertheless, the evidence for ETV in NPH is low in comparison to shunting and only one very low-quality randomised study comparing ETV with the VP shunt has been published with inconclusive results [6]. Therefore, this chapter will summarise current knowledge about the outcomes and prognosis of shunted NPH patients, and mention the natural course of the disease. ETV outcomes are discussed in its specific chapter (see Chap. 24).
With the current knowledge of the disease pathophysiology, the frequent occurrence of neurodegenerative and other comorbidities in ageing patients, selection of surgical candidates is focused on the expected improvement of clinical symptoms after surgery. Confirmation of NPH diagnosis is definitive only in patients with improvement of the symptoms after shunt implantation. The indication for surgery is usually decided with the help of guidelines and functional test analysis [9,10,11]. It is not certain how to approach patients who do not improve in functional testing, but correspond to NPH both clinically and in terms of findings on imaging examinations. In terms of possible comorbidities (e.g. osteoarthritis of large joints, stress incontinence, benign prostatic hyperplasia, etc.), it is necessary to approach each patient individually. If any of the symptoms of the triad do not improve after surgery, it should be further investigated and it may be necessary for the patient to be referred to another specialist, e.g. urologist to evaluate urinary symptoms more in detail [12]. The reported differences in outcomes may therefore be partly explained by the prevalence of concurrent comorbidities and their proper identification should be included in the central part of NPH management [13].
2 Early and Short-Term Postoperative Outcomes
Until 2002, there was no study comparing the results of a shunt operation with a randomised control group [14]. In the past few years, however, several such studies have been conducted. For example, Kazui et al. [15] showed significantly higher clinical improvement after LP shunt implantation in the immediately operated group (65%) than in the delayed group (5%) 3 months after randomisation (prior to surgery in the control group) defined as an improvement of 1 or more points on Modified Rankin Scale (mRS). Nakajima et al. [16] published the results of a nationwide hospital survey in Japan comparing the results of patients who underwent shunt surgery with non-operated controls (using mRS), and only the operated patients achieved significant improvement at 1-year follow-up control, regardless of the type of shunt surgery. In a prospective European multicentre iNPH study, 69% of patients improved according to mRS (one-point improvement) and 84% improved according to an age-standardised iNPH scale (five-point improvement). Indication for surgery was based on various clinical and radiological criteria, and there was no a randomised control group [17]. The Swedish Hydrocephalus Quality Registry reported that the number needed to treat for improving one patient from unfavourable (mRS 3–5) to favourable (mRS 0–2) was 3.0 [18]. Improvements can be maintained for several years [19], despite possible shunt revisions [20]. A higher percentage of improvement might be achieved with strict diagnostic and treatment protocols [9]—e.g. Poca et al. [14] reported clinical improvement in almost 90% of patients (with an improvement of at least one point on the iNPH scale). However, strict diagnostic criteria might result in under-treatment; therefore, each patient should be evaluated individually.
Different target options for both proximal and distal ends of the shunt system are possible. These include mainly ventriculoperitoneal (VP), lumboperitoneal (LP) and ventriculoatrial (VA) shunts. Outcomes of shunt diversion methods are comparable and approximately 75% of patients improve in the first year after shunting [5]. Although cardiopulmonary and renal complications are serious concerns associated with VA shunt placement, they are uncommon in patients with iNPH [21]. LP shunt outcomes do not significantly differ from VP shunt outcomes [22]. Early and short-term postoperative outcomes are definitely connected with diagnostic accuracy and shunt indication [11] and are possibly most favourable when CSF outflow resistance is increased and global cerebral autoregulation is intact, in combination with arterial normotension [23]. A recent study found that mild preoperative iNPH severity, shorter preoperative symptom duration, good tap test response, and complete DESH were associated with good short-term postoperative outcome at 1 year [24]. Also, it was found that compared to reference individuals, the neuropsychological aspects and quality of life of iNPH patients improved during the first 3 months after surgery, in some parts nearly to normal values [25]. This means that patients with longstanding preoperative symptoms may not receive the same benefits of surgical intervention as patients with a shorter duration of preoperative symptoms. However, with longer follow-up, the patients generally tend to reach the same endpoint [26]. Another study showed that the outcomes of VP-shunt surgery did not significantly differ between 6 months and 2 years post-surgery, indicating that the outcome at 6 months remained stable for up to 24 months. Longer symptom duration and older age should not deter patients with iNPH from undergoing shunt implantation [27].
Despite many efforts to predict shunt response non-invasively, none of them have shown any clinical benefit [28]. The utility of imaging to predict response to shunting is limited, and no imaging feature alone can be used to exclude patients from shunt surgery [29, 30]. The results are closely related to the diagnostic procedures and guideline adherence throughout the centres [9, 11]. Laparoscopic and less invasive implantations have been introduced with the goal to minimise wound-related complications [31]. However, between 2007 and 2017, laparoscopic assistance was only used in 6% of implantations in the USA [32]. Also, there is currently no evidence in the literature to support this approach nor its potential benefits over the traditional surgical technique.
Of note is the recent systematic review and meta-analysis by Giordan et al. [5] which focused on the comparison of different surgical techniques in NPH management. It included 33 studies with a total of 2461 patients. An improvement in postoperative functional outcome was observed in over 75% of patients, regardless of the surgical technique or the CSF diversion units used. In terms of the valves, NPH patients managed by programmable and by fixed valves had similar treatment outcomes. On the other hand, compared to the fixed valves, adjustable devices were associated with a reduction in revisions (12% vs. 32%), along with a lower number of subdural collections (9% vs. 22%). This mirrors the prediction that revision rates are probably going to decrease with increased use of adjustable novel devices. Using neuronavigation may be suggested for guiding the ventricular implantation [33]. A recent study however did not find any clear benefit of its usage [34].
2.1 Complications and Mortality
In a recent service evaluation of early postoperative outcomes in NPH, D’Antona et al. [35] reported 0% mortality, 7% morbidity and no revisions or readmissions to ICU in 88 patients who underwent lumbar drain insertion and/or VP shunt implantation. Seven patients had minor complications, and no moderate or severe complications were reported. No correlation between preoperative morbidity, surgical outcomes and hospital length of stay was found. A large multicentre survey of a privately insured United States healthcare network, however, showed a 7.29% 30-day readmission rate for 974 patients with NPH who underwent ventricular shunting. The perioperative complication rate was 21.15%, and included intracerebral haemorrhage (5.85%) and extra-axial haematoma (subdural or epidural 5.54%) Pre-existing comorbidities such as peripheral vascular disease, cerebral vascular disease, diabetes, paralysis or renal disease, were associated with risks of complication or readmission. Approximately 5.9% of patients needed reoperation within 30-days [36]. Another study reported a 36% complication rate (23% shunt related complication rate) in iNPH patients with a 0% mortality rate. INPH patients had a significantly smaller risk of shunt surgery-related complications than other patient groups treated with shunting [37]. Another study showed 0.5% 30-day mortality rate without a significant difference from controls [38]. Hebb et al. [39] in 2001 reported an overall mean complication rate of 38% after shunt surgery and a shunt revision rate of 22%. However, a more recent systematic review reported a lower pooled complication rate of 10% and a shunt revision rate of 16% [5]. A subsequent meta-analysis also showed the benefit of using adjustable devices. Some of the revisions made in the past would have been e easily solved with adjustments only. Another study showed that approximately 50% of revisions occur in the 1st year after initial shunt surgery and are mainly due to malfunctions [19]. A study comparing the complication rate 3 months after VP shunt insertion in NPH and non-NPH patients found that high Karnofsky Performance Score at admission and NPH as an underlying indication significantly reduced the odds ratio for a complication [37]. Subdural haematomas (SDHs) are common complications of shunt treatment accompanied with overdrainage. Recent study showed that SDHs developed in 10% of patients in 12-month follow-up and 36% of these cases were treated surgically. Significantly lower portions of surgeries were made in patients with adjustable shunts. SDH and treatment do not significantly affect survival in iNPH patients, thus the non-invasive treatment offered by adjustable shunts considerably reduces the level of severity of this common adverse event [40]. Male sex, antiplatelet medication, and a lower opening pressure at surgery were risk factors for SDH [41]. Infections are rarer. A recent study reported an infection rate of 5.9% [42] and another study of 4.76% during the first 3 months [43].
Despite a lot of effort to sustain initial improvement in clinical outcomes after shunt insertion in NPH patients, the improvement tends to decline within longer follow-ups. According to a recent meta-analysis [5], over 75% of patients evaluated after 12 months experienced an improvement in their clinical status after shunting. This number subsequently decreased to 73% of patients followed up from 12 to 36 months, and an even more significant decline was observed for patients whose follow-up exceeded 36 months (71%). However, it is important to note, and as it is discussed more in detail below, the overall improvement rate of NPH patients after shunting is notably higher compared to the natural course of the disease [44,45,46].
3 Gait Impairment Outcomes
Gait is the symptom most likely to improve after shunting and typically tends to keep sustained improvement. To give an example, in the series of 50 shunted NPH patients, there was an improvement after shunting which sustained improvement over a median follow-up time of 120.2 ± 2.3 months compared to the initial baseline, as stated by Grasso et al. [18]. Moreover, gait improvement is the one most connected to quality of life. Of note, persistent gait impairment and depression are the strongest predictors of low quality of life after NPH treatment [47]. Following the first reports saying that gait disturbances may be an initial manifestation of NPH, the gait impairment in NPH has since been studied in detail. As a result, some specific features that can to some extent distinguish NPH from other disorders have been identified. NPH gait disorder is sometimes called “magnetic” or “glued to the floor”, with other characteristic patterns such as diminished gait velocity, loss of balance, short stride, so-called en blog turning etc., features that are described in an individual chapter more in detail (see Chap. 9) [48]. A study from 2001 evaluated differences in gait impairment between patients suffering from NPH (n = 11) and those with Parkinson’s disease (n = 10), compared to twelve age-matched healthy controls [49]. Although some reports have reported parkinsonian signs as typical for NPH patients, contraindicatory findings have been published with better clinical profiles and the distinction between probable and possible NPH patients [50,51,52]. Moreover, this differentiated the possible existence of comorbidities that could bias what is and what is not a characteristic pattern for NPH. Additionally, according to the most recent reports, parkinsonian signs are not very common in well-defined NPH, regardless of existing comorbidity [53, 54]. Still, Parkinsonism is a differential diagnosis of NPH of great importance [55]. In the study by Stolze et al. [49], gait velocity increased by approximately 21% following the CSF tap test in NPH patients, compared to the natural gait velocity at the baseline. Also, a coefficient of variation for stride length, step width, and foot angle was calculated. Interestingly, it significantly decreased after the CSF tap test, along with the enlargement of the stride length, but the cadence remained at the same level without any difference. According to these findings, in terms of the gait impairment, gait velocity has been found to be the pattern that tends to improve the most also following the shunt placement [5, 18]. This is particularly useful for predicting shunt responsiveness, considering the high sensitivity of this gait feature to the CSF tap test [56]. If secondary deterioration occurs after surgery, and shunt malfunction is ruled out, the comorbid disease should be suspected.
In 2000, Blomsterwall et al. [57] studied the association between disturbances of balance and gait in NPH patients before and after shunt insertion. Interestingly, 75% of patients improved in gait velocity and 69% in balance, suggesting that improved balance may be to some extent responsible for gait improvement. Similar results were reported in a recent multicentre prospective observational study by Trungu et al. [46]. Out of 181 NPH patients, the mean gait domain was 58.5 ± 14.3 preoperatively, 66.0 ± 12.2 postoperatively and 70.1 ± 13.4. This domain was statistically significantly improved in shunted NPH patients at the 12 monthfollow-up examination. (p < 0.001). A similar trend was observed in the balance domain, the mean values were 66.7 ± 21.5 preoperatively, 72.4 ± 19.2 postoperatively, and 71.7 ± 22.1 at the 12-month follow-up (p = 0.001). Other reports observed that gait improvement was present three years after shunt insertion in 80–83% of shunted NPH patients and in approximately 87% of NPH patients 7 years after shunting [58, 59]. Supported by various studies evaluating the effect of shunt implantation on postoperative outcomes in NPH patients, the gait domain shows the highest improvement along with the impact on overall clinical score postoperatively. This is also true with respect to long-term follow-ups [4, 60, 61].
A recently published study by Sundström et al. [55] evaluated the outcome measure timed up and go (TUG) in a large, nationwide cohort that included 1300 iNPH patients before and after surgery. The authors compared the TUG test to the 10-m walk test (10MWT), the iNPH scale, the mRS, and Mini-Mental State Examination (MMSE). Significant improvements in TUG and 10MWT were observed in both the general group and for the group stratified for sex and age. Interestingly, women tended to perform significantly worse after shunting in both TUG and 10MWT (p < 0.001), but there was no observed difference between males and females in overall postoperative improvement (Fig. 1). Moreover, there was a strong association between TUG and the 10MWT before and after shunt implantation (r = 0.76). However, there was only a moderate relationship between TUG and the iNPH scale (r = 0.34), weak to moderate association with mRS (r = 0.22) and negligible correlation was seen between TUG and MMSE (r = 0.17). These findings, based on a large population of non-selected NPH patients, show that the TUG time and steps are significantly improved regardless of sex and age [55]. NPH patients tend to perform worse in the TUG test compared to healthy elderly controls, in both preoperative and postoperative examinations at 3 months. These higher values of TUG times can be explained by NPH-related gait dysfunction which is to some extent independent of age, and the improvement of gait disturbances typically takes time to normalise. Some gait impairment features are irreversible regardless of shunt insertion [55, 62, 63]. Notably, patients with more severe symptoms preoperatively, that is, those with higher TUG values, benefited from shunting, but their gait amelioration was not significant regardless of clinical improvement. The fact that the improvement of NPH patients after shunting is typically independent of age, in contrast to healthy elderly individuals, is supported by a meta-analysis of 21 studies that investigated the TUG test in healthy elderly subjects. The mean values of TUG times were different among patients’ age groups, 8.1 s (95% CI, 7.1 to 9.0 s) for patients between 60 and 69 years; 9.2 s (95% CI, 8.2 to 10.2 s) for patients 70–79 olds; and finally 11.3 s (95% CI, 10.0 to 12.7 s) for subjects aged between 80 and 99 years [64].
Histogram displaying the number of patients within each TUG time interval pre- and postoperatively for men (n = 744) and women (n = 505). Preoperatively, 175 men and 79 women had TUG time < 13.5 s. Postoperatively, the corresponding numbers were 364 and 186. Above this threshold, the risk of falling is considered to be increased. Sundström et al. [55]. The paper is an Open Access article distributed under the terms of the Creative Commons licensed under CC-BY-4.0 Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited
The mentioned reports are a great example of why early treatment is preferable and why even patients with severe symptoms should not be excluded from surgery. Agerskov et al. [62] outlined that they did not find any association between the severity of symptoms and treatment outcome. Additionally, although Kimura et al. [24] found a negative correlation between these two factors, that is, symptom severity and expected treatment outcome, the benefits of shunt implantation in well-selected NPH patients still substantially exceeds the progression of the disease when left untreated [44,45,46, 55].
3.1 Cognitive Outcomes
As a part of Hakim’s triad, some NPH patients experience a range of neuropsychological alterations, which tend to mimic concurrent neurodegenerative comorbidities and their distinguishment is often challenging. Nevertheless, the ‘typical NPH cognitive profile’ comprises memory, learning and attention impairment, along with disturbances of processing and psychomotor speed or disruptions of executive and other functions. The disruptions of frontal functions are a common part of NPH-related cognitive disturbances since they are based on extended ventricular dilatation and thus on the damage of frontosubcortical projections or subcortical structures [65, 66]. This may be to some extent (although highly dependent on many factors, including the length of such damage, individual patient predisposition, shunt responsiveness etc.) a reversible process when the shunt works properly, and ventricular dilatation is reduced [67, 68]. Memory functions tend to improve following the shunt insertion, as frequently reported [18, 69, 70]. Significant improvements were found for spatial memory and visual recall. NPH patients simultaneously tended to improve in different subtests of the Wechsler Memory Scale. A recent systematic review and meta-analysis [70] calculated differences in neuropsychological tests before and after surgery. Of 23 studies (1059 NPH patients) included in the final meta-analysis, the authors searched for surgical effects on cognitive outcomes evaluated through adequate tests including the MMSE, the Rey Auditory Verbal Learn Testing (RAVLT), trail making tests A and B (TMT-A and TMT-B), delayed verbal recall subjects, backwards digit span and phonemic verbal fluency. There was a statistically significant positive effect of shunting on cognition (p < 0.001) and memory (p < 0.001).ess significant positive effect on executive function (backwards digit span, p < 0.03; phonemic verbal fluency, p = 0.005; TMT-B, p = 0.03) and significant psychomotor speed (TMT-A, p < 0.001). The meta-regression models did not find any statistically significant effects of age, follow-up, or gender on improvement in the MMSE. Nevertheless, the mentioned meta-analysis evaluated studies with short follow-ups (from 3 to 12 months) and therefore could not provide conclusions about the effect of shunting on cognitive improvement in NPH patients after a longer period of follow-up. According to some reports, RAVLT is likely to be highly sensitive to improved cognition in NPH subjects, since a significant correlation between the improvement in RAVLT retention score and in both the total and delayed verbal recall subtests has been observed [71, 72]. Although some studies have shown no change in cognitive performance in the MMSE test [20, 73, 74], there are also contradictory reports finding significant improvements [75,76,77]. Regarding the improvement of executive function after surgery, some studies have reported significant improvement in the backwards digit span test [68, 73, 78, 79], however, others have not shown any changes [20, 80]. Similarly, improvements in the Stroop test have been so far heterogeneous [60, 67, 76]. The reason why executive function usually does not show a significant tendency to improve is probably based on a noteworthy proportion of patients suffering from disproportionately impaired executive function at the baseline clinical examination, therefore supporting the hypothesis that such impairment may reflect irreversible damage to fronto-subcortical connectivity in NPH patients [70, 74, 81]. It is clear that overall, cognitive amelioration after surgery is sometimes limited and mental state is often the first of the symptoms to decline [82, 83].
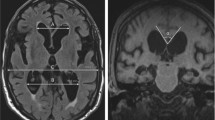
A recent prospective report by Hellström et al. [68] investigated the effects of shunt insertion on the cognitive profile in 47 iNPH patients, compared to 159 age-matched healthy controls. All iNPH patients showed improvement in all neuropsychological tests, except for the Digit Span forward, Digit Span Wechsler Adult Intelligence Scale score and the Simple Reaction Time. The authors observed that more severely impaired functions before surgery tended to improve more following the shunt insertion, compared to milder disturbances. Most patients improved according to the Grooved Pegboard (86–90%) and Stroop (82–91%) testing three months after surgery. On the other hand, the lowest number of patients improved on the Digit Span forward and backward tests (26% and 44%, respectively). Despite positive shunt-related improvement in iNPH patients, most of the cited studies did not evaluate long-term cognitive outcomes and the question of how long neuropsychological improvement lasts has not been answered in larger population studies with longer follow-ups yet. Several studies which examined a small number of patients or with no detailed clinical evaluation of the iNPH diagnosis did not find any significant long-term improvement in cognitive functions after iNPH intervention [60, 84, 85]. Nevertheless, of note is a recent study of 48 iNPH patients which found that the majority of them (77%) were able to improve or maintain cognitive function for at least 2 years after surgery when compared to their baseline cognitive clinical status [86]. There was a statistically significant improvement in the MMSE scale at 3 months (p = 0.0002) and 1 year postoperatively (p = 0.004), compared to patients’ initial baseline scores. However, 2 years following the shunting, the mean MMSE score almost returned to the preoperative level − 12 patients showed an increased MMSE score by ≥ 2 points, 11 patients showed a decline by ≥ 2 points, and almost no change was found in the remaining 25 patients (Fig. 2). The final number of 37 patients (77%) therefore refers to patients with cognitive improvement and no observed change in their neuropsychological testing 2 years after surgery, both compared to their baseline status. To compare the aforementioned results to other studies, improved performance in the MMSE test was significant in the vast majority of reports [75,76,77]. However, other investigations did not find any change in the improvement of iNPH patients in the MMSE after shunt implantation [73, 74, 87]. In a recent study by Hülser et al. [25], there was a significant improvement in the overall test battery during the first 3 months after shunt insertion, including the MMSE testing (p < 0.024). However, despite such an improvement, the iNPH patients were not able to reach the baseline of the healthy age-matched controls, even in early follow-ups after shunt surgery [25]. These findings are suggestive of the fact that even though the postoperative improvement in the MMSE may be statistically significant, the cognitive performance of iNPH patients is worse when compared to healthy controls. Another term that should be mentioned is the so-called “ceiling effect”, characteristic of iNPH patients who perform with around 24 points in the MMSE test, therefore being close to normal values of unaffected individuals [70]. This effect describes the reduced sensitivity of the MMSE test for mild cognitive dysfunction, which challenges the comparison of these changes in cognitive disturbances before and after shunt implantation [70]. Thist may be one of the reasons why there is no significant detection of changes in the MMSE testing, since some mild cognitive dysfunctions may be undetectable through this test [70, 81]. Therefore, additional, and more detailed neurophysiological testing may be appropriate, including the Montreal Cognitive Assessment (MoCA), which showed better diagnostic accuracy than the MMSE itself [70, 88].
Between group comparison of the mean MMSE score prior and after shunt insertion, according to Kambara et al. [86]. The paper is an Open Access article distributed under the terms of the Creative Commons licensed under CC-BY-4.0 Attribution Licence, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited
Moreover, since the severity and patients’ age are likely associated with the prognosis of the neuropsychological profile, early iNPH intervention is desirable to improve cognitive prognosis [86]. During follow-up, the neuropsychological domain tends to deteriorate, especially in patients experiencing other mild neurodegenerative comorbidities, and the consensus on the reversibility of cognition impairment in NPH patients with respect to concurrent disorders has not yet been elucidated [46]. This might be even further supported by findings that show a decrease in the MMSE score by 3 points after the diagnosis of iNPH if left untreated [44]. Such a deterioration was seen in iNPH patients who waited for surgery for at least 6 months (range from 6.8 to 23.8 months, median 13.2 months) compared to early treated iNPH individuals (waiting time for shunt implantation ranged from 0.1 to 2.7 months, median of 0.2 months) [44]. This statement was also verified in various reports, thus supporting the findings that waiting time for surgery influences the outcome in iNPH patients [89].
3.2 Incontinence Outcomes
One of the first reports dedicated to a more detailed evaluation of shunt effectiveness in improving urinary incontinence was published in 1988 by Ahlberg et al. [90]. Of ten patients with possible NPH, a definite diagnosis was confirmed in four cases. All had a positive Bors’ ice water test. Three of them had a history of subarachnoid haemorrhage and one of severe head trauma. After performing the tap test, the Bors’ test remained positive in three cases, but it changed to negative in one case. All four patients underwent VP shunt placement. Three months after surgery, all four patients had a negative Bors’ test and had normal micturition features on urodynamic testing. Moreover, three patients did not suffer from any bladder instability, and the instability in the remaining case was reduced in comparison to the initial manifestation. The guidelines by Relkin et al. [91] describe that urinary impairment in the early stages of the disease is characterised by abnormal frequency and urgency without urinary incontinence itself. As one of the typical features in NPH-related urinary impairment, the term “neurogenic bladder syndrome” has been used to describe hyperactivity of the bladder in some patients with NPH. Along with the progression of the disease, early features of urinary disturbances develop into serious urinary incontinence. To adequately differentiate NPH-related urinary disturbances from primary urinary incontinence unrelated to NPH, attention should be paid to urodynamic studies which play an important role in the detailed evaluation of common comorbid conditions [91]. This is particularly important to bear in mind when determining the improvement of urinary impairment after shunt implantation in NPH patients. As stated in the chapter dedicated to the symptomatology of NPH (see Chap. 11), urinary incontinence is typically the least frequent symptom of the whole triad and the least discussed in the literature [39].
Although the urinary incontinence domain typically shows a lower proportion of improved patients after surgery, a recent multicentre prospective observational study has observed significant improvement of this symptom in 70% of shunted NPH patients [46]. Furthermore, the results of the urinary incontinence domain were significant improvement at the 12-month follow-up (p = 0.002). Similarly, a prospective cohort study of 23 patients by Krzastek et al. [92] showed significant improvement after shunting not only in urinary urgency or urge incontinence, but also in overall quality of life and the ability to perform everyday activities. The most common symptom of an overactive bladder before surgical implantation of the shunt was two times/night nocturia. Interestingly, this symptom did not improve after shunt insertion, in contrast to the following significantly improved symptoms: urinary urgency (p = 0.016), bother from urinary urgency (p = 0.005), and the amount of urge incontinence (p = 0.038). Moreover, significant improvement in urinary dysfunction was seen more commonly in younger patients and women tended to improve in more domains of urinary impairment after surgery, when compared to men [92]. Aforedescribed reports have described early improvement of urinary dysfunction in shunted NPH patients, however, the question is whether the improvement remains the same in longer follow-ups. Similar to the cognitive deterioration in long-term follow-ups, urinary incontinence has also shown a tendency to decline after longer periods of time, despite the initial improvement in early or short-term follow-ups [18].
3.3 Long-Term Prognosis and the Role of Comorbidities
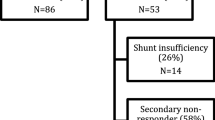
The natural history of untreated patients with NPH is poor, with both increased mortality and morbidity. Shunt insertion can provide long-lasting clinical improvement [93]. However, in some patients, the effect of shunting might be limited over time, or the symptoms might not be well-compensated. If so, evaluation of the shunt function might be reasonable. Kaestner et al. [42] indicated shunt revision for suspected shunt dysfunction in 18% of secondary deteriorations. Immediate improvement was present in 37% of patients. The authors suggested invasive testing if shunt malfunction was suspected. In vivo shunt studies might be used [94]. In iNPH, shunt dysfunction does not often lead to enlargement of ventricles, a surrogate parameter of shunt failure. Nevertheless, the majority of secondary deteriorations were treated conservatively, either by valve adjustments or because of existing connections with concurrent comorbidities [42]. It was also found that favourable outcomes following shunt implantation in patients with NPH did not correlate with decreased ventricular volume one year after surgery [95]. However, the ventricular volume often decreases as well, as there is a little increase in the cortical volume, especially in the regions near the vertex [96]. Another study found that 20% of patients with iNPH were at risk for secondary clinical worsening about 3 years after shunt surgery. About one-fourth of these patients benefited for additional years from pressure level management and/or shunt valve revision [97].
Long-term prognosis is influenced by many factors, not always connected with the disease. If another comorbidity is suspected, specialised consultation might be needed, as well as follow-up by a neurosurgeon and a neurologist. A standardised protocol and a multidisciplinary team dedicated to this disorder is needed to achieve an early and correct diagnosis of NPH [46]. Patients should also adhere to home physical exercises to improve their outcomes but also get a general health benefit [98]. The presence of comorbidities has a fundamental impact on patients’ performance and prognosis following the shunt insertion. Therefore, comorbidities must be considered when evaluating postoperative outcomes, both in early and long-term follow-ups.
Despite the suggestions, the literature dedicated to long-term outcomes of NPH management is still limited. Shorter follow-up studies predominate, and longer-term studies have low numbers of participants. At the beginning of NPH management, the long-term results had not even been paid attention to. The first studies did not provide knowledge until many years later. Greenberg et al. [99] in 1977 reported a 42.8% 3-year shunting success rate. Nowadays, it is no longer imaginable that five patients (6.9%) would die within one month of surgery, or as a direct result of surgical intervention.
Black et al. [100] in 1980 reported longer-term postoperative outcomes of shunting (36.5 months mean follow-up time). Sixty-one percent of patients improved, however, the 35.4% rate of complications, which was comparable to the studies released in the same years, is very high in comparison to recent studies. The change in the progression of the disease, any role of time in terms of clinical symptoms, or any comorbidity factors were not studied. Also, the timing of the evaluation of outcomes was not specified. Interestingly, the ventricle enlargement with little or no sulcal enlargement on CT scan was found to be a predictive factor of postoperative improvement [100]. More than 20 years later in 2001, a questionnaire study by Mori et al. [101] reported an improvement rate of 73.3% at 3 years after shunt surgery, and mortality at 3 years was 2.9%. At 3 months, the improvement rate was 79.2%. Improvement in gait disturbance after the surgery was found in 21 patients (91.3%), improvement in dementia in eight (34.8%), and improvement in urinary incontinence in 14 patients (60.9%). Interestingly, only 18.3% of implanted shunt systems had an anti-siphon device. 74.2% of shunt valves were programmable. The shunt-related complication rate was 18.3% [101]. In 2002, Savolainen et al. [60] reported a 47% gait, 29% incontinence, and 38% mental improvement rate 5 years after the surgery. One year after the shunting, 72% of patients had a good recovery. Following the 5-year follow-up, 11 (65%) of alive patients experienced worsened gait symptoms, while six had no change when compared to their preoperative clinical status. Cognitive problems worsened in 13 patients (77% of alive), while only one patient improved. Worsening of urinary incontinence was present in 10 patients (59%) and six had no change in this sign. Interestingly none of the neuropsychological tests significantly improved after the surgery, and the reported cognitive benefit was subjective. The 16 patients with Alzheimer’s disease did worse after one year than those without pathological changes, but the mortality was not increased. Thus, the role of neurodegenerative comorbidities in the postoperative outcomes had been discussed. Aygok et al. [102] reported a period of 3 months to 3 years after shunting in 50 iNPH patients with only a moderate decline in gait performance (91–75%), retention of memory improvement (80–80%), and improvement in incontinence sustained over time (70–82.5%). Four cases of death were not related to shunting. Even though the risk and fear of falling decreased significantly after shunting, they did not reach the level of risk in controls [103]. However, a significant difference in deaths caused by falls between iNPH patients and controls was not found [104].
In 2007, Kahlon et al. [84] reported 5-year outcomes of shunted patients with a 43% improvement rate in the walk step test, 39% of patients improved in the walk time test, and 39% improved in the reaction time test, whereas only 4% showed improvement in the memory test. 57% reported that they still perceived improvement compared with their preoperative status. However, only 36% of shunted patients were available at the follow-up at 5 years. Between the 6-month and 5-year follow-up periods, 37% out of the initial 75 patients died. The death rates in operated (37%) and not operated (38%) patients were similar. However, the 7.4% annual death rate was higher than 3.2% of the general Swedish population in the same age group. The causes of death were mainly due to cardiovascular disease (32%), and malignancy (25%). The results emphasised the importance of taking comorbidities and older age into account when selecting patients with NPH symptoms for shunt surgery [84]. Chen et al. [105] reported that during the 3 years of follow-up, five of the 28 patients died, the other six were lost to follow-up (including telephone contact), and three patients had progressive clinical deterioration. Pujari et al. [19] reported an overall sustained improvement among all symptoms over a mean follow-up duration of 5.9 ± 2.5 years. Gait showed the highest maintenance of improvement over baseline (83% at 3 years and 87% at the last analysed follow-up of 7 years), cognition showed intermediary improvement (84% and 86%, respectively), and urinary incontinence showed the least improvement (84% and 80%, respectively). However, only 27% of all shunted patients were evaluated at 7 years. The study suggested the role of selection criteria in the high long-term success rates, however, 29 patients (52.7%) required a total of 62 shunt revisions during the follow-up period [19]. Mirzayan et al. [106] reported similar long-term improvement rates with much lower needs for revision surgeries (n = 8). The long-term data were available for 34 of 55 patients only and 29 patients (56.9%) died. The cause of death was a cardiac failure in seven patients (13.9%) and cerebral infarction in 12 patients (23.5%). Gölz et al. [107] reported outcomes in 61 of 141 patients at six years after shunt implantation—59% of patients had an excellent outcome, 15% had a satisfactory benefit, and 26% had unsatisfactory results. The overall complication rate was 13%. Valve revision surgeries were necessary in 8.2% of cases of valve dysfunction, overdrainage, and underdrainage. The abdominal catheter was revised in 2 patients (1.4%) because of dislocation. Interestingly, 47% of patients died during the follow-up but the causes of death were not known in the majority of the patients [107]. The previously mentioned study by Grasso et al. [18] showed a long-term follow-up of 7–10 years. A sustained improvement was observed in 36 patients (76%), no changes were observed in six patients (12%), further deterioration was observed in three patients (6%), and death was observed in 5 patients (10%). The study also showed a worse prognosis in patients beyond a value of 3 Comorbidity index points, while it has been shown that the prognosis becomes worse even if other outcome predictors point to a favourable prognosis [108]. It has been suggested that the worse prognosis with NPH is not the result of the hydrocephalus aetiology itself, but the consequence of a typical accumulation of negative outcome predictors as a consequence of the misinterpretation of normal ageing and delayed adequate treatment [108]. Takeuchi et al. [109] concluded that iNPH symptoms generally improve after shunting. However, the symptoms begin to gradually recur at 3 years postoperatively. This tendency was particularly observed in those aged ≥ 80 years while the frequency of the complicating diseases is in general higher in this age group [109]. A study on LP shunts found that outcomes deteriorated near pre-operation levels after 3 years, indicating that the recovery outcomes of LP shunts for the treatment of iNPH were not sustainable [110]. In a single-centre study by de Oliveira et al. [111], 38% of the patients showed sustained improvement at 8 − 10 years of follow-up while 16 patients were dead (32%) and an additional five (10%) were lost to follow-up. At early follow-up, there were 12 complications in 9 patients (18%) without other complications in the mid-term or long-term evaluations. Table 1 summarises the studies reporting long-term outcomes.
It can be assumed that long-term results will be affected by many factors. Associated diseases, the state and time of hydrocephalus detection and its compensation, the presence of irreversible changes, the share of symptoms in increasing other risks (falls, urinary tract infections), the component of the disease “uncompensated” by shunt therapy could be involved [113].
A recent study comparing iNPH patients with age-matched controls showed that more pronounced symptoms in the preoperative ordinal gait scale and lower Mini-mental State Examination results were the most important predictors of mortality along with the prevalence of heart disease. Patients who improved in both the gait scale and the mRS after shunting had similar survival as aged, sex and habitational municipality matched controls (p = 0.391) indicating that shunt surgery for iNPH, besides of possible clinical improvement, can normalise survival [104]. Over the median follow-up period of 5.9 years, the mortality Hazard Ratio (HR) of iNPH patients was 1.81 when compared to controls and 30-day mortality after shunting was 0.5% [104]. An earlier study by Malm et al. [114] reported 3.3 Relative Risk (RR) of death and 2.4% 30-day mortality for iNPH patients.
Although different statistical methods were used, and the results cannot be directly compared with the same relevance, lower figures were reported. Authors suggest increased awareness and improved knowledge of iNPH in the context of increasing incidence of shunt surgery of iNPH patients [17] as well as surgical and anaesthetic technical improvements to be the contributing factors [104]. If the studies presenting long-term outcomes are divided by the decades of publication, a trend towards higher percentages of clinical improvement with lower prevalence of complications may be observed (Table 2).
Mortality related to shunting in long-term studies is negligible [106]. Moreover, adjustable valves in the recent meta-analysis were associated with a reduction in revisions (12% vs. 32%) and subdural collections (9% vs. 22%) when compared to fixed valves [5]. A single-centre study showed 12% transient morbidity in patients with gravitational valves and 25% in differential pressure valves while patients with gravitational valves showed a more profound improvement in clinical symptoms [115]. With the advance of valve technology and the safety of shunt treatment, the previous reluctance to intervene in patients over 80 years of age should be reconsidered. 80% of patients aged > 80 years experienced an improvement in their mobility and 65.7% (objective or subjective) improvement in cognition following VP shunt insertion [116]. A large analysis of 7696 general, general thoracic, and vascular surgery cases found increasing age to be itself a risk factor of postoperative morbidity and mortality while other risk factors increase with age [117]. However, in a recent study of NPH patients, age did not independently correlate with surgical complication or 30-day readmission rate while the poor outcome was associated with a history of myocardial infarction within 1 year, cerebrovascular and moderate/severe renal failure [36]. Increasing age does not necessarily decrease the chance of shunt succeeding [10] and age alone should be no barrier to the treatment of iNPH [116].
Andrén et al. [118] recently pointed out that shunt implantation should not be postponed, and early shunt implantation prolongs survival, specifically in patients > 75 years of age. The crude four-year mortality was 39.4% in iNPH patients where the implantation was postponed by 6–24 months, compared to 10.1% in early shunted iNPH patients. Previous studies from the same department have already shown that patients who had to wait for shunt surgery had worse treatment outcomes [44, 119]. Also, the patients who improved on the gait scale or in the mRS postoperatively survived longer. In fact, the survival of patients who improved in both these scales was no different than that of the control group. The patients who continued to deteriorate postoperatively had a substantially higher mortality rate than patients with unchanged scores [104]. Together with studies reporting an association between longer duration of iNPH symptoms and decreasing likelihood of response to shunting it may be suggested that the reversibility of symptoms diminishes over time [44, 118,119,120,121] and therefore early diagnosis and operation without delay should be emphasised [118]. Moreover, iNPH patients with more pronounced symptoms preoperatively have shorter survival [104]. Another study reported that patients who survived the follow-up after 5 years showed greater postoperative improvement [106]. However, even though a heavier burden of symptoms is associated with reduced survival, treatment for iNPH is still highly beneficial with an estimated gain of 2.2 life years and 1.7 quality-adjusted life years [122]. Comorbidities significantly influence the clinical outcome of iNPH patients undergoing shunt therapy and should be included in the assessment of the benefits and risks of shunt surgery [58]. Comorbid Alzheimer’s disease (AD) is frequent in iNPH patients. 19% of shunted NPH patients had AD histopathological findings based on cortical brain biopsies performed during placement of CSF shunts with a strong correlation with success after shunting [123]. However, studies that did not find a difference in the outcome of surgery between patients with AD comorbidity predominate [124,125,126,127]. A recent study found that 26% of participants with iNPH had coexisting AD pathology, which did not significantly influence the clinical response to shunt surgery [128]. However, those having moderate to severe dementia are more unlikely to improve after shunting [82]. Another study found that results of RAVLTest, Grooved Pegboard test, Stroop colour-naming test and interference test were predictive of AD or Parkinson’s spectrum disorder comorbidities and were closely related to the outcome of shunting [129]. In terms of Parkinsonism, a study showed that patients with suspected NPH and potentially undiagnosed Parkinson’s syndrome can improve in CSF tap test at the same rate as patients without suspicion of a movement disorder [130]. Nevertheless, longer follow-up of those patients is needed. Another study revealed that comorbid Parkinson’s spectrum disorder deteriorates the clinical course of iNPH. However, shunt surgery is recommended regardless of this comorbidity [131]. A recent meta-analysis revealed significantly increased lumbar CSF Phosphorylated-Tau (−0.55 SMD, p = 0.04) and Total-Tau (−.50 SMD, p = 0.02) in shunt-non-responsive iNPH [132] which may suggest the future role of CSF analysis in shunt prognostication or evaluation of neurodegenerative comorbidities. An analysis by Spangoli et al. [133] showed a trend towards shorter survival in patients with a severe degree of cerebrovascular disease (CVD). However, both patients with and without CVD and/or risk factors for vascular disease presented a significant improvement after shunting. 79% of patients without and 52% of patients with CVD were considered to be improved at the long-term follow-up at a mean of 52 months. Another study also found that the prevalence of lumbar spondylosis, compression fracture, severe periventricular hyperintensity, deep and subcortical white matter hyperintensity, and old cerebral infarcts was significantly higher among the tap test non-responders [134]. Nevertheless, lumbar stenosis should be evaluated if symptoms suspect it. Periventricular hyperintensities may suggest irreversible vascular changes and risk factors should be evaluated. An epidemiological study found a higher frequency of hypertension in iNPH patients than in controls (52 vs. 32%) as well as an overrepresentation of type 2 diabetes mellitus of 22 versus 12% [135]. Raftopoulos et al. [136] reported a lasting improvement in 91% of 23 patients until death or at least 5 years after shunt surgery with cardiovascular or cerebrovascular ischaemia being a main cause of death. Reported main causes of death are related to vascular or particularly cerebrovascular disease and dementia while deaths due to neoplasms are less common [104, 106, 133, 137]. In iNPH, the prevalence of risk factors for cerebrovascular disease is higher than in controls [138, 139] while an overlay of pathophysiological mechanisms underlying the development of iNPH and cerebrovascular disease remains to be elucidated [140]. With reports that patients with vascular comorbidity also improve after shunting for iNPH [104, 133, 141, 142] it could be suggested that the presence of cerebrovascular comorbidity should not itself be an exclusion criterion for shunting and maintenance of a clinical protocol of proper identification of shunt responders should be preferred. However, it should be taken into account that evidence of marked white matter disease in the initial imaging may also inform for worse long-term outcomes [82].
4 Conclusion
NPH is a crucial differential diagnosis for neurodegenerative disorders, especially considering the possible reversibility or improvement of symptoms. Despite the potential risk of complications, shunt malfunction, shunt failure, and surgical revisions, surgical treatment of NPH in the vast majority of cases delivers not only clinical amelioration but also an overall improvement in quality of life. The treatment effect and its importance for the prognosis of NPH patients and the improvement or at least maintenance of their clinical profiles is clear. Gait impairment is the symptom most likely to improve after shunting and it shows the lowest tendency to decline after surgery within longer follow-ups. Conversely, cognitive amelioration and the improvement in urinary functions after shunt implantations are limited and both symptoms are often the first to deteriorate, regardless of the initial improvement in early or short-term follow-ups. To a greater extent, the existence of concurrent comorbidities in NPH patients has a fundamental impact on clinical status, postoperative outcomes, and further prognosis. It is of great importance to meticulously evaluate associated comorbidities in relation to postoperative outcomes, both in early and long-term follow-ups. The benefits of shunt implantation clearly overcome the benefits of the spontaneous natural course of the disease in well-selected NPH patients. Unfortunately, the literature evaluating long-term outcomes of NPH treatment is still limited and lacks larger proportions of participants. Nevertheless, longer duration of symptoms, the severity of symptoms and older age should not be factors that exclude patients with iNPH from undergoing shunt insertion, although they are associated with worse postsurgical improvement.
5 Key Points
-
Outcomes of iNPH treatment are similar between different CSF diversion devices, and over 75% of treated iNPH patients improve as a result of active treatment policy.
-
Benefits, risks, and outcomes of various CSF diversion strategies (ventriculoperitoneal, ventriculoatrial, or lumboperitoneal shunts) are similar and comparable.
-
Gait is the most likely symptom to improve after shunting and typically tends to maintain sustained improvement. Long-term evaluation and monitoring of NPH is needed to clearly outline the extent of improvement.
-
The presence of concurrent comorbidities in NPH patients has a fundamental impact on the treatment outcome as well as patients’ prognosis, both from an early and long-term perspective.
-
The length of preoperative symptoms is a fundamental predictor of shunt effectiveness and clinical improvement.
-
Surgery-related complication and revision rates following the NPH management are likely to decrease prospectively, mainly due to the usage of advanced adjustable devices and advances in the understanding of the disease.
-
Increasing age does not automatically decrease the chance of successful shunt implantation and age alone should be no barrier to the treatment of iNPH.
Abbreviations
- 10MWT:
-
10M walk test
- AD:
-
Alzheimer’s disease
- CI:
-
Confidence interval
- CSF:
-
Cerebrospinal fluid
- CT:
-
Computed tomography
- CVD:
-
Cerebrovascular disease
- ETV:
-
Endoscopic third ventriculostomy
- LP:
-
Lumboperitoneal
- MMSE:
-
Mini-Mental State Examination
- MoCA:
-
Montreal Cognitive Assessment
- mRS:
-
Modified Rankin Scale
- NPH:
-
Normal pressure hydrocephalus
- iNPH:
-
Idiopathic normal pressure hydrocephalus
- RAVLT:
-
Rey Auditory Verbal Learn Testing
- SDH:
-
Subdural haematoma
- SMD:
-
Standardised mean difference
- sNPH:
-
Secondary normal pressure hydrocephalus
- TMT:
-
Trail Making Test
- TUG:
-
Timed up and go
- VA:
-
Ventriculoatrial
- VP:
-
Ventriculoperitoneal
References
Shaw R, Everingham E, Mahant N, Jacobson E, Owler B. Clinical outcomes in the surgical treatment of idiopathic normal pressure hydrocephalus. J Clin Neurosci 2016;29:81–86. https://doi.org/10.1016/j.jocn.2015.10.044.
Esmonde T, Cooke S. Shunting for normal pressure hydrocephalus (NPH). Cochrane Database Syst Rev 2002;Cd003157. https://doi.org/10.1002/14651858.Cd003157.
Kameda M, Yamada S, Atsuchi M, Kimura T, Kazui H, Miyajima M, Mori E, Ishikawa M, Date I. Cost-effectiveness analysis of shunt surgery for idiopathic normal pressure hydrocephalus based on the SINPHONI and SINPHONI-2 trials. Acta Neurochir (Wien) 2017;159:995–1003. https://doi.org/10.1007/s00701-017-3115-2.
Klinge P, Hellström P, Tans J, Wikkelsø C. One-year outcome in the European multicentre study on iNPH. Acta Neurol Scand. 2012;126:145–153. https://doi.org/10.1111/j.1600-0404.2012.01676.x.
Giordan E, Palandri G, Lanzino G, Murad MH, Elder BD. Outcomes and complications of different surgical treatments for idiopathic normal pressure hydrocephalus: a systematic review and meta-analysis. J Neurosurg. 2018;1–13. https://doi.org/10.3171/2018.5.Jns1875.
Tudor KI, Tudor M, McCleery J, Car J. Endoscopic third ventriculostomy (ETV) for idiopathic normal pressure hydrocephalus (iNPH). Cochrane Database Syst Rev. 2015;Cd010033. https://doi.org/10.1002/14651858.CD010033.pub2.
Mitchell P, Mathew B. Third ventriculostomy in normal pressure hydrocephalus. Br J Neurosurg. 1999;13:382–385. https://doi.org/10.1080/02688699943484.
Tasiou A, Brotis AG, Esposito F, Paterakis KN. Endoscopic third ventriculostomy in the treatment of idiopathic normal pressure hydrocephalus: a review study. Neurosurg Rev. 2016;39:557–563. https://doi.org/10.1007/s10143-015-0685-4.
Nakajima M, Yamada S, Miyajima M, Ishii K, Kuriyama N, Kazui H, Kanemoto H, Suehiro T, Yoshiyama K, Kameda M, et al. Guidelines for Management of Idiopathic normal pressure hydrocephalus (third edition): endorsed by the Japanese society of normal pressure hydrocephalus. Neurol Med Chir (Tokyo). 2021;61:63–97. https://doi.org/10.2176/nmc.st.2020-0292.
Halperin JJ, Kurlan R, Schwalb JM, Cusimano MD, Gronseth G, Gloss D. Practice guideline: idiopathic normal pressure hydrocephalus: response to shunting and predictors of response: report of the guideline development, dissemination, and implementation subcommittee of the American academy of neurology. Neurology. 2015;85:2063–2071. https://doi.org/10.1212/wnl.0000000000002193.
Skalický P, Mládek A, Vlasák A, De Lacy P, Beneš V, Bradáč O. Normal pressure hydrocephalus-an overview of pathophysiological mechanisms and diagnostic procedures. Neurosurg Rev. 2020;43:1451–1464. https://doi.org/10.1007/s10143-019-01201-5.
Kogan MI, Zachoval R, Ozyurt C, Schäfer T, Christensen N. Epidemiology and impact of urinary incontinence, overactive bladder, and other lower urinary tract symptoms: results of the EPIC survey in Russia, Czech Republic, and Turkey. Curr Med Res Opin. 2014;30:2119–2130. https://doi.org/10.1185/03007995.2014.934794.
Malm J, Graff-Radford NR, Ishikawa M, Kristensen B, Leinonen V, Mori E, Owler BK, Tullberg M, Williams MA, Relkin NR. Influence of comorbidities in idiopathic normal pressure hydrocephalus - research and clinical care. A report of the ISHCSF task force on comorbidities in INPH. Fluids Barriers CNS. 2013;10:22. https://doi.org/10.1186/2045-8118-10-22.
Poca MA, Solana E, Martínez-Ricarte FR, Romero M, Gándara D, Sahuquillo J. Idiopathic normal pressure hydrocephalus: results of a prospective cohort of 236 shunted patients. Acta Neurochir Suppl. 2012;114:247–253. https://doi.org/10.1007/978-3-7091-0956-4_49.
Kazui H, Miyajima M, Mori E, Ishikawa M. Lumboperitoneal shunt surgery for idiopathic normal pressure hydrocephalus (SINPHONI-2): an open-label randomised trial. Lancet Neurol. 2015;14:585–594. https://doi.org/10.1016/s1474-4422(15)00046-0.
Nakajima M, Miyajima M, Ogino I, Akiba C, Kawamura K, Kurosawa M, Kuriyama N, Watanabe Y, Fukushima W, Mori E, et al. Shunt intervention for possible idiopathic normal pressure hydrocephalus improves patient outcomes: a nationwide hospital-based survey in Japan. Front Neurol. 2018;9:421. https://doi.org/10.3389/fneur.2018.00421.
Sundström N, Malm J, Laurell K, Lundin F, Kahlon B, Cesarini KG, Leijon G, Wikkelsö C. Incidence and outcome of surgery for adult hydrocephalus patients in Sweden. Br J Neurosurg. 2017;31:21–27. https://doi.org/10.1080/02688697.2016.1229749.
Grasso G, Torregrossa F, Leone L, Frisella A, Landi A. Long-Term efficacy of shunt therapy in idiopathic normal pressure hydrocephalus. World Neurosurg. 2019;129:e458–63. https://doi.org/10.1016/j.wneu.2019.05.183.
Pujari S, Kharkar S, Metellus P, Shuck J, Williams MA, Rigamonti D. Normal pressure hydrocephalus: long-term outcome after shunt surgery. J Neurol Neurosurg Psychiatry. 2008;79:1282–1286. https://doi.org/10.1136/jnnp.2007.123620.
Poca MA, Mataró M, Matarín M, Arikan F, Junqué C, Sahuquillo J. Good outcome in patients with normal-pressure hydrocephalus and factors indicating poor prognosis. J Neurosurg. 2005;103:455–463. https://doi.org/10.3171/jns.2005.103.3.0455.
Hung AL, Vivas-Buitrago T, Adam A, Lu J, Robison J, Elder BD, Goodwin CR, Jusué-Torres I, Rigamonti D. Ventriculoatrial versus ventriculoperitoneal shunt complications in idiopathic normal pressure hydrocephalus. Clin Neurol Neurosurg. 2017;157:1–6. https://doi.org/10.1016/j.clineuro.2017.03.014.
Miyajima M, Kazui H, Mori E, Ishikawa M. One-year outcome in patients with idiopathic normal-pressure hydrocephalus: comparison of lumboperitoneal shunt to ventriculoperitoneal shunt. J Neurosurg. 2016;125:1483–1492. https://doi.org/10.3171/2015.10.Jns151894.
Lalou AD, Czosnyka M, Donnelly J, Pickard JD, Nabbanja E, Keong NC, Garnett M, Czosnyka ZH. Cerebral autoregulation, cerebrospinal fluid outflow resistance, and outcome following cerebrospinal fluid diversion in normal pressure hydrocephalus. J Neurosurg. 2018;130:154–162. https://doi.org/10.3171/2017.7.Jns17216.
Kimura T, Yamada S, Sugimura T, Seki T, Miyano M, Fukuda S, Takeuchi S, Miyata S, Tucker A, Fujita T, et al. Preoperative predictive factors of short-term outcome in idiopathic normal pressure hydrocephalus. World Neurosurg. 2021;151:e399–406. https://doi.org/10.1016/j.wneu.2021.04.055.
Hülser M, Spielmann H, Oertel J, Sippl C. Motor skills, cognitive impairment, and quality of life in normal pressure hydrocephalus: early effects of shunt placement. Acta Neurochir (Wien). 2022. https://doi.org/10.1007/s00701-022-05149-2.
Vakili S, Moran D, Hung A, Elder BD, Jeon L, Fialho H, Sankey EW, Jusué-Torres I, Goodwin CR, Lu J, et al. Timing of surgical treatment for idiopathic normal pressure hydrocephalus: association between treatment delay and reduced short-term benefit. Neurosurg Focus. 2016;41:E2. https://doi.org/10.3171/2016.6.Focus16146.
Popal AM, Zhu Z, Guo X, Zheng Z, Cai C, Jiang H, Zhang J, Shao A, Zhu J. Outcomes of ventriculoperitoneal shunt in patients with idiopathic normal-pressure hydrocephalus 2 years after surgery. Front Surg. 2021;8:641561. https://doi.org/10.3389/fsurg.2021.641561.
Vlasák A, Skalický P, Mládek A, Vrána J, Beneš V, Bradáč O. Structural volumetry in NPH diagnostics and treatment—future or dead end? Neurosurg Rev. 2021;44:503–14. https://doi.org/10.1007/s10143-020-01245-y.
Subramanian HE, Fadel SA, Matouk CC, Zohrabian VM, Mahajan A. The utility of imaging parameters in predicting long-term clinical improvement after shunt surgery in patients with idiopathic normal pressure hydrocephalus. World Neurosurg. 2021;149:e1–10. https://doi.org/10.1016/j.wneu.2021.02.108.
Park HY, Park CR, Suh CH, Kim MJ, Shim WH, Kim SJ. Prognostic utility of disproportionately enlarged subarachnoid space hydrocephalus in idiopathic normal pressure hydrocephalus treated with ventriculoperitoneal shunt surgery: a systematic review and meta-analysis. AJNR Am J Neuroradiol. 2021;42:1429–1436. https://doi.org/10.3174/ajnr.A7168.
Karasin B, Eskuchen L, Hardinge T, Watkinson J, Grzelak M, Boyce M. Laparoscopic-Assisted ventriculoperitoneal shunt placement: a less invasive approach to treating hydrocephalus. Aorn J. 2021;114:133–146. https://doi.org/10.1002/aorn.13467.
Alvi MA, Brown D, Yolcu Y, Zreik J, Javeed S, Bydon M, Cutsforth-Gregory JK, Graff-Radford J, Jones DT, Graff-Radford NR, et al. Prevalence and trends in management of idiopathic normal pressure hydrocephalus in the United States: insights from the national inpatient sample. World Neurosurg. 2021;145:e38–52. https://doi.org/10.1016/j.wneu.2020.09.012.
Yamada S, Ishikawa M, Nakajima M, Nozaki K. Reconsidering ventriculoperitoneal shunt surgery and postoperative shunt valve pressure adjustment: our approaches learned from past challenges and failures. Front Neurol. 2021;12:798488. https://doi.org/10.3389/fneur.2021.798488.
Jin MC, Wu A, Azad TD, Feng A, Prolo LM, Veeravagu A, Grant GA, Ratliff J, Li G. Evaluating shunt survival following ventriculoperitoneal shunting with and without stereotactic navigation in previously shunt-naïve patients. World Neurosurg. 2020;136:e671–82. https://doi.org/10.1016/j.wneu.2020.01.138.
D'Antona L, Blamey SC, Craven CL, Sewell D, Manohara S, Leemans M, Worby S, Thompson SD, Golahmadi AK, Funnell JP, et al. Early postoperative outcomes of normal pressure hydrocephalus: results of a service evaluation. J Neurosurg Anesthesiol. 2021;33:247–253. https://doi.org/10.1097/ana.0000000000000668.
Nadel JL, Wilkinson DA, Linzey JR, Maher CO, Kotagal V, Heth JA. Thirty-Day hospital readmission and surgical complication rates for shunting in normal pressure hydrocephalus: a large national database analysis. Neurosurgery. 2020;86:843–850. https://doi.org/10.1093/neuros/nyz299.
Schenker P, Stieglitz LH, Sick B, Stienen MN, Regli L, Sarnthein J. Patients with a normal pressure hydrocephalus shunt have fewer complications than do patients with other shunts. World Neurosurg. 2018;110:e249–57. https://doi.org/10.1016/j.wneu.2017.10.151.
Andrén K, Wikkelsø C, Hellström P, Tullberg M, Jaraj D. Response to the Letter to the Editor regarding the article entitled ‘Early shunt surgery improves survival in idiopathic normal pressure hydrocephalus’. Eur J Neurol 2021, 28:e90 https://doi.org/10.1111/ene.14804.
Hebb AO, Cusimano MD. Idiopathic normal pressure hydrocephalus: a systematic review of diagnosis and outcome. Neurosurgery. 2001;49:1166–1184; discussion 1184–1166. https://doi.org/10.1097/00006123-200111000-00028.
Sundström N, Lagebrant M, Eklund A, Koskinen LD, Malm J. Subdural hematomas in 1846 patients with shunted idiopathic normal pressure hydrocephalus: treatment and long-term survival. J Neurosurg. 2018;129:797–804. https://doi.org/10.3171/2017.5.Jns17481.
Gasslander J, Sundström N, Eklund A, Koskinen LD, Malm J. Risk factors for developing subdural hematoma: a registry-based study in 1457 patients with shunted idiopathic normal pressure hydrocephalus. J Neurosurg. 2020;1–10. https://doi.org/10.3171/2019.10.Jns191223.
Kaestner S, Behrends R, Roth C, Graf K, Deinsberger W. Treatment for secondary deterioration in idiopathic normal pressure hydrocephalus in the later course of the disease: a retrospective analysis. Acta Neurochir (Wien). 2020;162:2431–2439. https://doi.org/10.1007/s00701-020-04475-7.
Skalický P, Mládek A, Vlasák A, Whitley H, Bradáč O. First experiences with Miethke M.blue® valve in iNPH patients. J Clin Neurosci. 2022;98:127–132. https://doi.org/10.1016/j.jocn.2022.02.004.
Andrén K, Wikkelsø C, Tisell M, Hellström P. Natural course of idiopathic normal pressure hydrocephalus. J Neurol Neurosurg Psychiatry. 2014;85:806–810. https://doi.org/10.1136/jnnp-2013-306117.
Kiefer M, Unterberg A. The differential diagnosis and treatment of normal-pressure hydrocephalus. Deutsches Aerzteblatt Online. 2012. https://doi.org/10.3238/arztebl.2012.0015.
Trungu S, Scollato A, Ricciardi L, Forcato S, Polli FM, Miscusi M, Raco A. Clinical outcomes of shunting in normal pressure hydrocephalus: a multicenter prospective observational study. J Clin Med. 2022;11:1286. https://doi.org/10.3390/jcm11051286.
Israelsson H, Eklund A, Malm J. Cerebrospinal fluid shunting improves long-term quality of life in idiopathic normal pressure hydrocephalus. Neurosurgery. 2020;86:574–582. https://doi.org/10.1093/neuros/nyz297.
Gallia GL, Rigamonti D, Williams MA. The diagnosis and treatment of idiopathic normal pressure hydrocephalus. Nat Clin Pract Neurol. 2006;2:375–381. https://doi.org/10.1038/ncpneuro0237.
Stolze H. Comparative analysis of the gait disorder of normal pressure hydrocephalus and Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2001;70:289–97. https://doi.org/10.1136/jnnp.70.3.289.
Ahn BJ, Lee M, Ju H, Im K, Kwon KY. An elderly man with normal pressure hydrocephalus presenting with asymmetric parkinsonism in the upper and lower extremities. Geriatr Gerontol Int. 2020;20:791–792. https://doi.org/10.1111/ggi.13940.
Akiguchi I, Ishii M, Watanabe Y, Watanabe T, Kawasaki T, Yagi H, Shiino A, Shirakashi Y, Kawamoto Y. Shunt-responsive parkinsonism and reversible white matter lesions in patients with idiopathic NPH. J Neurol. 2008;255:1392–1399. https://doi.org/10.1007/s00415-008-0928-1.
Blomsterwall E, Bilting M, Stephensen H, Wikkelsö C. Gait abnormality is not the only motor disturbance in normal pressure hydrocephalus. Scand J Rehabil Med. 1995;27:205–9.
Bugalho P, Guimarães J. Gait disturbance in normal pressure hydrocephalus: a clinical study. Parkinsonism Relat Disord. 2007;13:434–437. https://doi.org/10.1016/j.parkreldis.2006.08.007.
Gallagher R, Marquez J, Osmotherly P. Clinimetric properties and minimal clinically important differences for a battery of gait, balance, and cognitive examinations for the tap test in idiopathic normal pressure hydrocephalus. Neurosurgery. 2019;84:E378-e384. https://doi.org/10.1093/neuros/nyy286.
Sundström N, Rydja J, Virhammar J, Kollén L, Lundin F, Tullberg M. The timed up and go test in idiopathic normal pressure hydrocephalus: a nationwide study of 1300 patients. Fluids Barriers CNS. 2022;19:4. https://doi.org/10.1186/s12987-021-00298-5.
Agostini V, Lanotte M, Carlone M, Campagnoli M, Azzolin I, Scarafia R, Massazza G, Knaflitz M. Instrumented gait analysis for an objective pre-/postassessment of tap test in normal pressure hydrocephalus. Arch Phys Med Rehabil. 2015;96:1235–1241. https://doi.org/10.1016/j.apmr.2015.02.014.
Blomsterwall E, Svantesson U, Carlsson U, Tullberg M, Wikkelsö C. Postural disturbance in patients with normal pressure hydrocephalus. Acta Neurol Scand 2000;102:284–291. https://doi.org/10.1034/j.1600-0404.2000.102005284.x.
Lemcke J, Meier U. Idiopathic normal pressure hydrocephalus (iNPH) and co-morbidity: an outcome analysis of 134 patients. Acta Neurochir Suppl. 2012;114:255–259. https://doi.org/10.1007/978-3-7091-0956-4_50.
Deopujari CE, Karmarkar VS, Shah N, Vashu R, Patil R, Mohanty C, Shaikh S. Combined endoscopic approach in the management of suprasellar craniopharyngioma. Childs Nerv Syst. 2018;34:871–876. https://doi.org/10.1007/s00381-018-3735-8.
Savolainen S, Hurskainen H, Paljärvi L, Alafuzoff I, Vapalahti M. Five-year outcome of normal pressure hydrocephalus with or without a shunt: predictive value of the clinical signs, neuropsychological evaluation and infusion test. Acta Neurochir (Wien). 2002;144:515–523; discussion 523. https://doi.org/10.1007/s00701-002-0936-3.
Giannini G, Palandri G, Ferrari A, Oppi F, Milletti D, Albini-Riccioli L, Mantovani P, Magnoni S, Chiari L, Cortelli P, et al. A prospective evaluation of clinical and instrumental features before and after ventriculo-peritoneal shunt in patients with idiopathic Normal pressure hydrocephalus: the Bologna PRO-Hydro study. Parkinsonism Relat Disord. 2019;66:117–124. https://doi.org/10.1016/j.parkreldis.2019.07.021.
Agerskov S, Hellström P, Andrén K, Kollén L, Wikkelsö C, Tullberg M. The phenotype of idiopathic normal pressure hydrocephalus-a single center study of 429 patients. J Neurol Sci. 2018;391:54–60. https://doi.org/10.1016/j.jns.2018.05.022.
Yamada S, Ishikawa M, Miyajima M, Nakajima M, Atsuchi M, Kimura T, Tokuda T, Kazui H, Mori E. Timed up and go test at tap test and shunt surgery in idiopathic normal pressure hydrocephalus. Neurol Clin Pract. 2017;7:98–108. https://doi.org/10.1212/cpj.0000000000000334.
Bohannon RW. Reference values for the timed up and go test: a descriptive meta-analysis. J Geriatr Phys Ther. 2006;29:64–68. https://doi.org/10.1519/00139143-200608000-00004.
Chiaravalloti A, Filippi L, Bagni O, Schillaci O, Czosnyka Z, Czosnyka M, de Pandis MF, Federici G, Galli M, Pompucci A, et al. Cortical metabolic changes and clinical outcome in normal pressure hydrocephalus after ventriculoperitoneal shunt: our preliminary results. Rev Esp Med Nucl Imagen Mol (Engl Ed). 2020;39:367–374. https://doi.org/10.1016/j.remn.2020.01.005.
Kito Y, Kazui H, Kubo Y, Yoshida T, Takaya M, Wada T, Nomura K, Hashimoto M, Ohkawa S, Miyake H, et al. Neuropsychiatric symptoms in patients with idiopathic normal pressure hydrocephalus. Behav Neurol. 200921:165–174. https://doi.org/10.3233/ben-2009-0233.
Hellström P, Edsbagge M, Archer T, Tisell M, Tullberg M, Wikkelsø C. The neuropsychology of patients with clinically diagnosed idiopathic normal pressure hydrocephalus. Neurosurgery. 2007;61:1219–1226; discussion 1227–1218. https://doi.org/10.1227/01.neu.0000306100.83882.81.
Hellström P, Edsbagge M, Blomsterwall E, Archer T, Tisell M, Tullberg M, Wikkelsø C. Neuropsychological effects of shunt treatment in idiopathic normal pressure hydrocephalus. Neurosurgery. 2008;63:527–535; discussion 535–526. https://doi.org/10.1227/01.Neu.0000325258.16934.Bb.
Peterson KA, Housden CR, Killikelly C, DeVito EE, Keong NC, Savulich G, Czosnyka Z, Pickard JD, Sahakian BJ. Apathy, ventriculomegaly and neurocognitive improvement following shunt surgery in normal pressure hydrocephalus. Br J Neurosurg 2016;30:38–42. https://doi.org/10.3109/02688697.2015.1029429.
Peterson KA, Savulich G, Jackson D, Killikelly C, Pickard JD, Sahakian BJ. The effect of shunt surgery on neuropsychological performance in normal pressure hydrocephalus: a systematic review and meta-analysis. J Neurol. 2016;263:1669–1677. https://doi.org/10.1007/s00415-016-8097-0.
Duinkerke A, Williams MA, Rigamonti D, Hillis AE. Cognitive recovery in idiopathic normal pressure hydrocephalus after shunt. Cogn Behav Neurol. 2004;17:179–184. https://doi.org/10.1097/01.wnn.0000124916.16017.6a.
Chaudhry P, Kharkar S, Heidler-Gary J, Hillis AE, Newhart M, Kleinman JT, Davis C, Rigamonti D, Wang P, Irani DN, et al. Characteristics and reversibility of dementia in Normal Pressure Hydrocephalus. Behav Neurol. 2007;18:149–158 https://doi.org/10.1155/2007/456281.
Gleichgerrcht E, Cervio A, Salvat J, Loffredo AR, Vita L, Roca M, Torralva T, Manes F. Executive function improvement in normal pressure hydrocephalus following shunt surgery. Behav Neurol. 2009;21:181–185. https://doi.org/10.3233/ben-2009-0249.
Saito M, Nishio Y, Kanno S, Uchiyama M, Hayashi A, Takagi M, Kikuchi H, Yamasaki H, Shimomura T, Iizuka O, et al. Cognitive profile of idiopathic normal pressure hydrocephalus. Dement Geriatr Cogn Dis Extra. 2011;1:202–211. https://doi.org/10.1159/000328924.
Thomas G, McGirt MJ, Woodworth G, Heidler J, Rigamonti D, Hillis AE, Williams MA. Baseline neuropsychological profile and cognitive response to cerebrospinal fluid shunting for idiopathic normal pressure hydrocephalus. Dement Geriatr Cogn Disord 2005;20:163–168. https://doi.org/10.1159/000087092.
Mataró M, Matarín M, Poca MA, Pueyo R, Sahuquillo J, Barrios M, Junqué C. Functional and magnetic resonance imaging correlates of corpus callosum in normal pressure hydrocephalus before and after shunting. J Neurol Neurosurg Psychiatry, 2007;78:395–398. https://doi.org/10.1136/jnnp.2006.096164.
Yamamoto D, Kazui H, Wada T, Nomura K, Sugiyama H, Shimizu Y, Yoshiyama K, Yoshida T, Kishima H, Yamashita F, et al. Association between milder brain deformation before a shunt operation and improvement in cognition and gait in idiopathic normal pressure hydrocephalus. Dement Geriatr Cogn Disord. 2013;35:197–207. https://doi.org/10.1159/000347147.
Solana E, Sahuquillo J, Junqué C, Quintana M, Poca MA. Cognitive disturbances and neuropsychological changes after surgical treatment in a cohort of 185 patients with idiopathic normal pressure hydrocephalus. Arch Clin Neuropsychol. 2012;27:304–317. https://doi.org/10.1093/arclin/acs002.
Poca MA, Mataró M, Sahuquillo J, Catalán R, Ibañez J, Galard R. Shunt related changes in somatostatin, neuropeptide Y, and corticotropin releasing factor concentrations in patients with normal pressure hydrocephalus. J Neurol Neurosurg Psychiatry. 2001;70:298–304. https://doi.org/10.1136/jnnp.70.3.298.
Mataró M, Poca MA, Del Mar Matarín M, Catalan R, Sahuquillo J, Galard R. CSF galanin and cognition after shunt surgery in normal pressure hydrocephalus. J Neurol Neurosurg Psychiatry. 2003;74:1272–1277. https://doi.org/10.1136/jnnp.74.9.1272.
Iddon JL, Pickard JD, Cross JJ, Griffiths PD, Czosnyka M, Sahakian BJ. Specific patterns of cognitive impairment in patients with idiopathic normal pressure hydrocephalus and Alzheimer’s disease: a pilot study. J Neurol Neurosurg Psychiatry. 1999;67:723–732. https://doi.org/10.1136/jnnp.67.6.723.
Ghosh S, Lippa C. Diagnosis and prognosis in idiopathic normal pressure hydrocephalus. Am J Alzheimers Dis Other Demen. 2014;29:583–589. https://doi.org/10.1177/1533317514523485.
Klassen BT, Ahlskog JE. Normal pressure hydrocephalus: how often does the diagnosis hold water? Neurology. 2011;77:1119–1125. https://doi.org/10.1212/WNL.0b013e31822f02f5.
Kahlon B, Sjunnesson J, Rehncrona S. Long-term outcome in patients with suspected normal pressure hydrocephalus. Neurosurgery. 2007;60:327–332; discussion 332. https://doi.org/10.1227/01.Neu.0000249273.41569.6e.
McGirt MJ, Woodworth G, Coon AL, Thomas G, Williams MA, Rigamonti D. Diagnosis, treatment, and analysis of long-term outcomes in idiopathic normal-pressure hydrocephalus. Neurosurgery. 2008;62(Suppl 2):670–7. https://doi.org/10.1227/01.neu.0000316271.90090.b9.
Kambara A, Kajimoto Y, Yagi R, Ikeda N, Furuse M, Nonoguchi N, Kawabata S, Kuroiwa T, Kuroda K, Tsuji S, et al. Long-Term prognosis of cognitive function in patients with idiopathic normal pressure hydrocephalus after shunt surgery. Front Aging Neurosci 2020;12:617150. https://doi.org/10.3389/fnagi.2020.617150.
Poca MA, Mataró M, Del Mar Matarín M, Arikan F, Junqué C, Sahuquillo J. Is the placement of shunts in patients with idiopathic normal-pressure hydrocephalus worth the risk? Results of a study based on continuous monitoring of intracranial pressure. J Neurosurg. 2004;100:855–866. https://doi.org/10.3171/jns.2004.100.5.0855.
Pinto TCC, Machado L, Bulgacov TM, Rodrigues-Júnior AL, Costa MLG, Ximenes RCC, Sougey EB. Is the montreal cognitive assessment (MoCA) screening superior to the mini-mental state examination (MMSE) in the detection of mild cognitive impairment (MCI) and alzheimer’s disease (AD) in the elderly? Int Psychogeriatr. 2019;31:491–504. https://doi.org/10.1017/s1041610218001370.
Chidiac C, Sundström N, Tullberg M, Arvidsson L, Olivecrona M. Waiting time for surgery influences the outcome in idiopathic normal pressure hydrocephalus—a population-based study. Acta Neurochirurgica. 2022;164:469–478. https://doi.org/10.1007/s00701-021-05085-7.
Ahlberg J, Norlén L, Blomstrand C, Wikkelsö C. Outcome of shunt operation on urinary incontinence in normal pressure hydrocephalus predicted by lumbar puncture. J Neurol Neurosurg Psychiatry. 1988;51:105–108. https://doi.org/10.1136/jnnp.51.1.105.
Relkin N, Marmarou A, Klinge P, Bergsneider M, Black PM. Diagnosing idiopathic normal-pressure hydrocephalus. Neurosurgery. 2005;57:S4–16; discussion ii–v. https://doi.org/10.1227/01.neu.0000168185.29659.c5.
Krzastek SC, Robinson SP, Young HF, Klausner AP. Improvement in lower urinary tract symptoms across multiple domains following ventriculoperitoneal shunting for idiopathic normal pressure hydrocephalus. Neurourol Urodyn. 2017;36:2056–2063. https://doi.org/10.1002/nau.23235.
Isaacs AM, Hamilton M. Natural history, treatment outcomes and quality of life in idiopathic normal pressure hydrocephalus (iNPH). Neurol India. 2021;69:S561-S568. https://doi.org/10.4103/0028-3886.332281.
Czosnyka ZH, Sinha R, Morgan JA, Wawrzynski JR, Price SJ, Garnett M, Pickard JD, Czosnyka M. Shunt testing in vivo: observational study of problems with ventricular catheter. Acta Neurochir Suppl. 2016;122:353–356. https://doi.org/10.1007/978-3-319-22533-3_69.
Meier U, Paris S, Gräwe A, Stockheim D, Hajdukova A, Mutze S. Is decreased ventricular volume a correlate of positive clinical outcome following shunt placement in cases of normal pressure hydrocephalus? Acta Neurochir Suppl. 2003;86:533–537. https://doi.org/10.1007/978-3-7091-0651-8_109.
Cogswell PM, Murphy MC, Senjem ML, Botha H, Gunter JL, Elder BD, Graff-Radford J, Jones DT, Cutsforth-Gregory JK, Schwarz CG, et al. Changes in ventricular and cortical volumes following shunt placement in patients with idiopathic normal pressure hydrocephalus. AJNR Am J Neuroradiol. 2021;42:2165–2171. https://doi.org/10.3174/ajnr.A7323.
Gutowski P, Rot S, Fritsch M, Meier U, Gölz L, Lemcke J. Secondary deterioration in patients with normal pressure hydrocephalus after ventriculoperitoneal shunt placement: a proposed algorithm of treatment. Fluids Barriers CNS. 2020;17:18. https://doi.org/10.1186/s12987-020-00180-w.
Modesto PC, Pinto FCG. Home physical exercise program: analysis of the impact on the clinical evolution of patients with normal pressure hydrocephalus. Arq Neuropsiquiatr. 2019;77:860–870. https://doi.org/10.1590/0004-282x20190183.
Greenberg JO, Shenkin HA, Adam R. Idiopathic normal pressure hydrocephalus—a report of 73 patients. J Neurol Neurosurg Psychiatry. 1977;40:336–341. https://doi.org/10.1136/jnnp.40.4.336.
Black PM. Idiopathic normal-pressure hydrocephalus. Results of shunting in 62 patients. J Neurosurg. 1980;52:371–377. https://doi.org/10.3171/jns.1980.52.3.0371.
Mori K. Management of idiopathic normal-pressure hydrocephalus: a multiinstitutional study conducted in Japan. J Neurosurg. 2001;95:970–973. https://doi.org/10.3171/jns.2001.95.6.0970.
Aygok G, Marmarou A, Young HF. Three-year outcome of shunted idiopathic NPH patients. Acta Neurochir Suppl. 2005;95:241–245. https://doi.org/10.1007/3-211-32318-x_49.
Larsson J, Israelsson H, Eklund A, Lundin-Olsson L, Malm J. Falls and fear of falling in shunted idiopathic normal pressure hydrocephalus-the idiopathic normal pressure hydrocephalus comorbidity and risk factors associated with hydrocephalus study. Neurosurgery. 2021;89:122–128. https://doi.org/10.1093/neuros/nyab094.
Andrén K, Wikkelsø C, Sundström N, Israelsson H, Agerskov S, Laurell K, Hellström P, Tullberg M. Survival in treated idiopathic normal pressure hydrocephalus. J Neurol. 2020;267:640–648. https://doi.org/10.1007/s00415-019-09598-1.
Chen YF, Wang YH, Hsiao JK, Lai DM, Liao CC, Tu YK, Liu HM. Normal pressure hydrocephalus: cerebral hemodynamic, metabolism measurement, discharge score, and long-term outcome. Surg Neurol. 2008;70 Suppl 1:S1:69–77; discussion S61:77. https://doi.org/10.1016/j.surneu.2008.08.079.
Mirzayan MJ, Luetjens G, Borremans JJ, Regel JP, Krauss JK. Extended long-term (> 5 years) outcome of cerebrospinal fluid shunting in idiopathic normal pressure hydrocephalus. Neurosurgery. 2010;67:295–301. https://doi.org/10.1227/01.Neu.0000371972.74630.Ec.
Gölz L, Ruppert FH, Meier U, Lemcke J. Outcome of modern shunt therapy in patients with idiopathic normal pressure hydrocephalus 6 years postoperatively. J Neurosurg. 2014;121:771–775. https://doi.org/10.3171/2014.6.Jns131211.
Kiefer M, Eymann R, Steudel WI. Outcome predictors for normal-pressure hydrocephalus. Acta Neurochir Suppl. 2006;96:364–367. https://doi.org/10.1007/3-211-30714-1_75.
Takeuchi T, Yajima K. Long-term 4 years follow-up study of 482 patients who underwent shunting for idiopathic normal pressure hydrocephalus -course of symptoms and shunt efficacy rates compared by age group. Neurol Med Chir (Tokyo). 2019;59:281–286. https://doi.org/10.2176/nmc.oa.2018-0318.
Liu JT, Su PH. The efficacy and limitation of lumboperitoneal shunt in normal pressure hydrocephalus. Clin Neurol Neurosurg. 2020;193:105748. https://doi.org/10.1016/j.clineuro.2020.105748.
de Oliveira MF, Sorte AAB, Jr., Emerenciano DL, Rotta JM, Mendes GAS, Pinto FCG. Long term follow-up of shunted idiopathic normal pressure hydrocephalus patients: a single center experience. Acta Neurol Belg. 2021;121:1799–1806. https://doi.org/10.1007/s13760-020-01538-5.
Eide PK, Sorteberg W. Outcome of surgery for idiopathic normal pressure hydrocephalus: role of preoperative static and pulsatile intracranial pressure. World Neurosurg. 2016;86:186-193.e181. https://doi.org/10.1016/j.wneu.2015.09.067.
Kiefer M, Meier U, Eymann R. Does idiopathic normal pressure hydrocephalus always mean a poor prognosis? Acta Neurochir Suppl. 2010;106:101–106. https://doi.org/10.1007/978-3-211-98811-4_17.
Malm J, Kristensen B, Stegmayr B, Fagerlund M, Koskinen LO. Three-year survival and functional outcome of patients with idiopathic adult hydrocephalus syndrome. Neurology. 2000;55:576–578. https://doi.org/10.1212/wnl.55.4.576.
Suchorska B, Kunz M, Schniepp R, Jahn K, Goetz C, Tonn JC, Peraud A. Optimized surgical treatment for normal pressure hydrocephalus: comparison between gravitational and differential pressure valves. Acta Neurochir (Wien). 2015;157:703–709. https://doi.org/10.1007/s00701-015-2345-4.
Thompson SD, Shand Smith JD, Khan AA, Luoma AMV, Toma AK, Watkins LD. Shunting of the over 80s in normal pressure hydrocephalus. Acta Neurochir (Wien). 2017;159:987–994. https://doi.org/10.1007/s00701-017-3171-7.
Turrentine FE, Wang H, Simpson VB, Jones RS. Surgical risk factors, morbidity, and mortality in elderly patients. J Am Coll Surg. 2006;203:865–877. https://doi.org/10.1016/j.jamcollsurg.2006.08.026.
Andrén K, Wikkelsø C, Hellström P, Tullberg M, Jaraj D. Early shunt surgery improves survival in idiopathic normal pressure hydrocephalus. Eur J Neurol. 2021;28:1153–1159. https://doi.org/10.1111/ene.14671.
Andrén K, Wikkelso C, Hellstrom P, Tullberg M, Jaraj D. Early treatment with CSF diversion reduces mortality in normal pressure hydrocephalus (P3.081). Neurology. 2017;88:P3.081.
McGirt MJ, Woodworth G, Coon AL, Thomas G, Williams MA, Rigamonti D. Diagnosis, treatment, and analysis of long-term outcomes in idiopathic normal-pressure hydrocephalus. Neurosurgery. 2005;57:699–705; discussion 699–705. https://doi.org/10.1093/neurosurgery/57.4.699.
Caruso R, Cervoni L, Vitale AM, Salvati M. Idiopathic normal-pressure hydrocephalus in adults: result of shunting correlated with clinical findings in 18 patients and review of the literature. Neurosurg Rev. 1997;20:104–107. https://doi.org/10.1007/bf01138192.
Tullberg M, Persson J, Petersen J, Hellström P, Wikkelsø C, Lundgren-Nilsson Å. Shunt surgery in idiopathic normal pressure hydrocephalus is cost-effective-a cost utility analysis. Acta Neurochir (Wien). 2018;160:509–518. https://doi.org/10.1007/s00701-017-3394-7.
Pomeraniec IJ, Bond AE, Lopes MB, Jane JA, Sr. Concurrent Alzheimer’s pathology in patients with clinical normal pressure hydrocephalus: correlation of high-volume lumbar puncture results, cortical brain biopsies, and outcomes. J Neurosurg. 2016;124:382–388. https://doi.org/10.3171/2015.2.Jns142318.
Leinonen V, Koivisto AM, Alafuzoff I, Pyykkö OT, Rummukainen J, von Und Zu Fraunberg M, Jääskeläinen JE, Soininen H, Rinne J, Savolainen S. Cortical brain biopsy in long-term prognostication of 468 patients with possible normal pressure hydrocephalus. Neurodegener Dis. 2012;10:166–169. https://doi.org/10.1159/000335155.
Bech-Azeddine R, Hogh P, Juhler M, Gjerris F, Waldemar G. Idiopathic normal-pressure hydrocephalus: clinical comorbidity correlated with cerebral biopsy findings and outcome of cerebrospinal fluid shunting. J Neurol Neurosurg Psychiatry. 2007;78:157–61. https://doi.org/10.1136/jnnp.2006.095117.
Cabral D, Beach TG, Vedders L, Sue LI, Jacobson S, Myers K, Sabbagh MN. Frequency of Alzheimer’s disease pathology at autopsy in patients with clinical normal pressure hydrocephalus. Alzheimers Dement. 2011;7:509–513. https://doi.org/10.1016/j.jalz.2010.12.008.
Golomb J, Wisoff J, Miller DC, Boksay I, Kluger A, Weiner H, Salton J, Graves W. Alzheimer’s disease comorbidity in normal pressure hydrocephalus: prevalence and shunt response. J Neurol Neurosurg Psychiatry. 2000;68:778–781. https://doi.org/10.1136/jnnp.68.6.778.
Yasar S, Jusue-Torres I, Lu J, Robison J, Patel MA, Crain B, Carson KA, Hoffberger J, Batra S, Sankey E, et al. Alzheimer’s disease pathology and shunt surgery outcome in normal pressure hydrocephalus. PLoS One. 2017;12:e0182288. https://doi.org/10.1371/journal.pone.0182288.
Kamohara C, Nakajima M, Kawamura K, Akiba C, Ogino I, Xu H, Karagiozov K, Arai H, Miyajima M. Neuropsychological tests are useful for predicting comorbidities of idiopathic normal pressure hydrocephalus. Acta Neurol Scand. 2020;142:623–631. https://doi.org/10.1111/ane.13306.
Davis A, Gulyani S, Manthripragada L, Luciano M, Moghekar A, Yasar S. Evaluation of the effect comorbid Parkinson syndrome on normal pressure hydrocephalus assessment. Clin Neurol Neurosurg. 2021;207:106810. https://doi.org/10.1016/j.clineuro.2021.106810.
Sakurai A, Tsunemi T, Shimada T, Kawamura K, Nakajima M, Miyajima M, Hattori N. Effect of comorbid Parkinson’s disease and Parkinson’s disease dementia on the course of idiopathic normal pressure hydrocephalus. J Neurosurg. 2022:1–8. https://doi.org/10.3171/2022.1.Jns212282.
Thavarajasingam SG, El-Khatib M, Vemulapalli KV, Iradukunda HAS, Laleye J, Russo S, Eichhorn C, Eide PK. Cerebrospinal fluid and venous biomarkers of shunt-responsive idiopathic normal pressure hydrocephalus: a systematic review and meta-analysis. Acta Neurochir (Wien). 2022. https://doi.org/10.1007/s00701-022-05154-5.
Spagnoli D, Innocenti L, Bello L, Pluderi M, Bacigaluppi S, Tomei G, Gaini SM. Impact of cerebrovascular disease on the surgical treatment of idiopathic normal pressure hydrocephalus. Neurosurgery. 2006;59:545–552; discussion 545–552. https://doi.org/10.1227/01.Neu.0000230259.49167.95.
Naito H, Sugimoto T, Kimoto K, Abe T, Kawano T, Matsuoka C, Ohno N, Giga M, Kono T, Ueno H, et al. Clinical comorbidities correlated with a response to the cerebrospinal fluid tap test in idiopathic normal-pressure hydrocephalus. J Neurol Sci. 2021;430:120024. https://doi.org/10.1016/j.jns.2021.120024.
Pyykkö OT, Nerg O, Niskasaari HM, Niskasaari T, Koivisto AM, Hiltunen M, Pihlajamäki J, Rauramaa T, Kojoukhova M, Alafuzoff I, et al. Incidence, comorbidities, and mortality in idiopathic normal pressure hydrocephalus. World Neurosurg. 2018;112:e624–31. https://doi.org/10.1016/j.wneu.2018.01.107.
Raftopoulos C, Massager N, Balériaux D, Deleval J, Clarysse S, Brotchi J. Prospective analysis by computed tomography and long-term outcome of 23 adult patients with chronic idiopathic hydrocephalus. Neurosurgery. 1996;38:51–59. https://doi.org/10.1097/00006123-199601000-00014.
Junkkari A, Sintonen H, Danner N, Jyrkkänen HK, Rauramaa T, Luikku AJ, Koivisto AM, Roine RP, Viinamäki H, Soininen H, et al. 5-Year health-related quality of life outcome in patients with idiopathic normal pressure hydrocephalus. J Neurol. 2021;268:3283–3293. https://doi.org/10.1007/s00415-021-10477-x.
Jaraj D, Agerskov S, Rabiei K, Marlow T, Jensen C, Guo X, Kern S, Wikkelsø C, Skoog I. Vascular factors in suspected normal pressure hydrocephalus: a population-based study. Neurology 2016;86:592–599. https://doi.org/10.1212/wnl.0000000000002369.
Israelsson H, Carlberg B, Wikkelsö C, Laurell K, Kahlon B, Leijon G, Eklund A, Malm J. Vascular risk factors in INPH: A prospective case-control study (the INPH-CRasH study). Neurology. 2017;88:577–585. https://doi.org/10.1212/wnl.0000000000003583.
Graff-Radford NR. Is normal pressure hydrocephalus becoming less idiopathic? Neurology. 2016;86:588–589. https://doi.org/10.1212/wnl.0000000000002377.
Andrén K, Wikkelsö C, Sundström N, Agerskov S, Israelsson H, Laurell K, Hellström P, Tullberg M. Long-term effects of complications and vascular comorbidity in idiopathic normal pressure hydrocephalus: a quality registry study. J Neurol. 2018;265:178–186. https://doi.org/10.1007/s00415-017-8680-z.
Tullberg M, Jensen C, Ekholm S, Wikkelsø C. Normal pressure hydrocephalus: vascular white matter changes on MR images must not exclude patients from shunt surgery. AJNR Am J Neuroradiol. 2001;22:1665–73.
Funding
This chapter was supported by the Ministry of Health of the Czech Republic institutional grant no. NU23-04-00551.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Skalický, P., Bubeníková, A., Vlasák, A., Bradáč, O. (2023). Prognosis and Outcomes. In: Bradac, O. (eds) Normal Pressure Hydrocephalus. Springer, Cham. https://doi.org/10.1007/978-3-031-36522-5_28
Download citation
DOI: https://doi.org/10.1007/978-3-031-36522-5_28
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-36521-8
Online ISBN: 978-3-031-36522-5
eBook Packages: MedicineMedicine (R0)