Abstract
This book chapter highlights the significance of biomaterials in modern medicine and biology. Biomaterials can be used to replace or repair damaged or missing body parts, allowing patients to regain mobility and improve their quality of life. The unique properties of biomaterials make them suitable for a range of medical devices, including implants, prosthetics, cardiovascular devices, drug delivery systems, wound dressings, and tissue engineering. Biocompatibility is a key characteristic of biomaterials, allowing them to interact with living tissue without causing adverse reactions. Mechanical properties and durability, which cause biomaterials to degrade in the body over time, are other crucial characteristics. Biomaterials are classified into natural and synthetic biomaterials. Each class has its unique advantages, making them suitable for various applications in the medical field. For instance, metals and ceramics are commonly used as cardiovascular, orthopaedic, dental implants and vascular stents due to their strength and biocompatibility, while polymers are used in wound dressings, drug delivery systems, and tissue engineering due to their versatility and customization. The unique properties of natural biomaterials make them attractive for various applications in different fields. Some of these applications include medical implants and devices, pharmaceutics, tissue engineering, food packaging, cosmetics, and environmental applications. Ongoing research efforts are focused on developing biomaterials with improved biocompatibility, mechanical strength, and degradation rates, leading to the creation of innovative treatments and devices in medicine. Overall, biomaterials have the potential to revolutionize healthcare by enabling the development of novel treatments and devices that can improve patient outcomes and quality of life. With ongoing research and development, the potential for biomaterials to transform healthcare is vast, offering hope for the future.
Graphical Abstract

Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Natural & synthetic biomaterials
- Biomaterials History
- Biocompatibility
- Medical implants
- Tissue engineering & regeneration
- Drug delivery
- Diagnosis
- Wound healing
1 Introduction
Materials are used to engineer different things all around us. However, engineering is present not only around us, but also within us. The materials used for that purpose are called biomaterials, a special category of materials used for engineering in/on our bodies. The human tissues, organs, or body systems occasionally fail to perform their normal functions, and these disorders are sometimes treated with the medications, i.e., drugs. All disorders, however, cannot be treated with drugs. They require one-of-a-kind biomaterials. In its broadest definition, the term “biomaterial“can refer to all the substances other than food and drugs that are utilized for biomedical purposes, i.e., to treat or diagnose illnesses or to repair, enhance, or replace tissues, organs, or physiological functions. This is from a bandage to an artificial pacemaker or a dental implant. All are biomaterials that have been engineered using a distinct set of materials designed to work well with a human body (Fig. 1).
Humans have been using biomaterials since prehistoric times, and now progress in biomedical research has been steadily accelerating to meet ever-increasing needs in healthcare and medicine practices. The introduction of medical devices made from biomaterials improved the quality of human life; as a result, millions of lives have been saved. Advancements in biomaterials research have solved many medical problems in both therapeutics and diagnostics. Therefore, translation of biomaterials into medical devices is a clinically important aspect clearly dependent on several factors such as biomaterials engineering, clinical realities, in vivo testing on humans and animals, industry involvement in developing suitable biomaterial devices and commercialization, etc. Figure 2 depicts a schematic representation of the path from biomedical advances to clinical use. Thousands of biomedical medical devices and diagnostic products have been used to aid in restoration to normal body functions of human tissues or organs after their deterioration. Currently, over 6000 different types of biomedical devices are listed in the Medical Device Product Classification Database, which is governed by the Food and Drug Administration’s Centre for Medical Devices and Radiological Health [1].
2 Definition of Biomaterials
Biomaterial research is a highly dynamic and ever-changing discipline, with ever-changing definitions of biomaterial. Biomaterials are seen differently at different times due to changes in their application, and numerous attempts have been made to describe them [2, 3].
An agreement was established among a group of biomaterial scientists at a European Society for Biomaterials meeting in 1987, and a contested definition of biomaterials was derived: “A non-viable material utilized in a medical device, designed to interact with biological systems”. However, the definition evolved and the reference to non-viability was later deleted.
In 1999 David F. William defined biomaterials as “a substance intended to interface with biological systems to assess, treat, augment, or replace any tissue, organ, or function of the body” in his Dictionary of Biomaterials.
Taking into account the dynamic developments in the area of biomaterial research and biomaterials definition, William discussed these changes in his recent leading opinion article, “On the nature of biomaterials”, and he redefined the definition of biomaterials as: “A biomaterial is a substance that has been engineered to take a form which, alone or as part of a complex system, is used to direct, by control of interactions with components of living systems, the course of any therapeutic or diagnostic procedure, in human or veterinary medicine”.
Biomaterials are defined by the American National Institute of Health as “any substance or combination of substances, other than drugs, synthetic or natural in origin, that can be used for any period of time, that augments or replaces partially or completely any tissue, organ, or function of the body, in order to maintain or improve the quality of life of the individual”.
Considering all the definitions in a broad sense, a biomaterial can be defined as a material engineered to acquire a form that can affect the course of any therapeutic or diagnostic procedure through interactions with the biological systems. These are all rather narrow definitions, but they will all be elaborated on throughout this book.
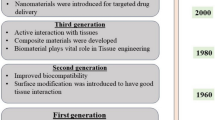
3 History of Biomaterials
Biomaterials are being used by humans either deliberately or unknowingly since prehistoric times. The biomedical implants and prostheses were found in human skeletons and skulls during the excavation of sites attributed to different civilizations of antiquity – Egyptian, Roman, Greek, and Etruscan. A spear point was discovered inserted into the hip of a Kennewick man’s approximately 9000-year-old remains. Even though the spear tip may have been an accidental implant bearing very little relation to the modern biomaterials, it is one of the earliest examples of an exogenous material that has been well tolerated and lodged in the human body. The use of skin grafting utilizing autogenous forehead skin for the restoration of the nose and skin from the cheek for the treatment of damaged earlobes is documented in one of the first surgical manuals from 600 BC. According to ancient Mayan documents from 600 BC people then used seashells as dental implants. It is also widely documented that the Middle Ages Europeans used catgut for suturing. The Ancient Egyptians used linen thread for wound treatment. It is noteworthy that humans have been studying biomaterials for a long time and have had great success despite not having the necessary knowledge of material science, sterilization, or biocompatibility.
Materials of natural origin and other metals were employed in Greece and Rome from the seventh century BC to the fourth century AD for the treatment of wounds and other health issues. During the sixteenth century in Europe, dental repairs were made using metals like gold and silver, and bone fractures were repaired by using the iron threads. The industrial revolution in the nineteenth century saw the development of X-rays and anaesthesia, and surgeries were performed under sterile conditions. The use of metal in internal body repairs was also initiated. After World War II, science and technology combined to develop prostheses, medical devices, or implants, such as heart valves, bone plates, hip joints, and cardiac pacemakers, to repair or replace damaged body parts or tissues. Following that, the progress on biomaterials was nucleated from several scientific communities, and scientific journals were established to collect the progress on biomaterials. Because of the numerous complications caused by implantable biomaterials, scientists coined the term “biocompatibility“for the first time in 1968. Ideally, the developed biomaterials should be biocompatible, meaning they should not be toxic or harmful to the biological system. Currently, biomaterials are used extensively in the medical field for drug delivery, tissue engineering, regenerative medicine, 3D bio printing of the organs, and many more applications [4]. A pictorial summary of the history of biomaterials from prehistoric times to twenty-first century is given in Fig. 3.
4 Biomaterial Characteristics
As stated above, there is no agreement on the definition of biomaterials, and it is constantly evolving. As a result, it is critical to understand the characteristics of biomaterials to aid in determining which materials are biomaterials and which are not. However, the requirements of biomaterials vary and depend on the type of biomedical application. The objective of a biomaterial is to treat, improve, or replace a body tissue or function, thus all the biomaterials must have the following four characteristics (Fig. 4).
4.1 Biocompatibility
Biomaterials that interact directly with the human body require specific design expertise. Biocompatibility is not only a vital characteristic of biomaterials, but it is also what designates something as a biomaterial. Technically, any substance can be used as a biomaterial, but to succeed the material must be biocompatible with which the biological system it intends to interact.
Biocompatibility assessment is intended to confirm the ability of a material to prevent negative responses and correctly carry out the specific biomedical task. However, assessment of biocompatibility is an intricate process, as there is not any specific definition or exact measurement to declare a material as a biomaterial. Usually, biocompatibility is characterized in context of its use for a specific application. Thus, any material performing well for a specific biomedical application cannot be declared biocompatible for all the biomedical applications.
For example, ceramic materials are widely used in dental implants and show good biocompatibility. They can cause incompatibility, however, when used with the vascular system like blood clotting. So, it is important to define biocompatibility specifically for a system like biocompatibility with cardiovascular system or with soft or hard tissues. Biocompatibility may have to be specifically measured for each specific biomedical application. It is also important to take functional evaluation into consideration while determining biocompatibility. For example, teflon (polytetrafluoroethylene) is biologically inert in the context that it does not trigger any adverse biological reaction with the living tissues. However, when teflon is used for the temporomandibular joint replacement, its fragmentation can trigger serious foreign body responses leading to erosion of the adjacent structures. Thus, its biocompatibility can be argued, and it gives us an insight into the importance of functional evaluation of the entire implant system. Biocompatibility of a material is determined by combination of many aspects like its chemical composition, intended use, duration of use, and physical shape. An example is given in the review by T. G. Moizhess, where carcinogenesis not only depends on the chemical composition of the biomaterial but also on shape of the implant system. The tumorigenic polymer system when implanted caused lower carcinogenicity after perforation and showed complete loss of carcinogenicity on fragmentation [5].
Some basic and important principles of biocompatibility are defined by U.S. Food and Drug Administration (FDA). FDA evaluates the biocompatibility of the complete biomaterial device system and not only the component materials of the system. ISO 10993-1 establishes norms for the biological assessment of the medical devices, substantiating that biological assessments must be “performed on the final medical device or representative samples from the final device or materials processed in the same manner as the final medical device (including sterilization, if needed)”.
4.2 Biological Functionality
Over the years, there has been a transition from permissive bio-inert materials to bioactive biomaterials, and biological functionality is an important characteristic of a biomaterial. Biological functionality implies a set of characteristics that a biomaterial must possess or comply with in its intended biological function. For example, an artificial valve has to close and open as per the requirement in its biological functionality. A controlled-release drug delivery system should provide a controlled drug release at a predetermined rate in its biological functionality. A biomaterial is designed with dynamic functionality and anticipated to integrate with the biological complexity and perform the desired functions in the body. So, numerous parameters are tested before a biomaterial is introduced into the market, just like drugs testing.
4.3 Chemical Stability
Chemical stability implies the ability of a biomaterial to maintain its integrity after implantation into its site of application. After surgical implantation, a biomaterial has to bear the attack of the body’s physiological environment. Under these conditions, some biomaterials are oxidized and can produce toxic by-products. Consequently, an implant can degrade and not perform its intended function. For example, one of the major limitations of metallic biomaterial is its chemical instability due to prolonged contact with the biological fluids, leading to corrosion (sum of electrochemical phenomena). So, a biomaterial should be chemically inert and stable to perform its function properly, not causing any harm to the body. It should be resistant to biological ageing for the intended duration of use, or if it is supposed to be used for a limited period, it should be biodegradable with no toxic by-products.
4.4 Machinability
Machinability implies that the material should be mouldable into a biomedical device with the potential to be sterilized by any standard sterilization method (autoclave, UV sterilization, alcohol disinfection, ethylene oxide gas disinfection, etc.). The material should not be impaired after sterilization. A biomaterial should have suitable manufacturability, i.e., the ability to manufacture the biomedical device easily for its anticipated use with high reliability. A biomaterial device should be robust to bear the strain, stress, shear, and mixture of these forces anticipated at their intended site of action in the body. Hardness, yield strength, tensile strength, and elasticity are some of the important characteristics of a biomaterial that should be considered and assessed prior to implantation. For example, for the materials to be used in hard tissue applications, the mechanical properties are of utmost importance. Wear and tear are often the main reasons for the failure of the implants. The device should have suitable mechanical properties appropriate for their intended site use. For example, a bone replacement biomaterial should possess good mechanical properties as it is anticipated to face significant mechanical stress at the implantation site. Similarly, a heart valve has to keep opening and closing many times a day and for a prolonged period of time, so it should be resistant to wear and tear on prolonged duration of use.
To summarize a biomaterial should:
-
Be biocompatible, i.e., non-toxic, non-inflammatory, non-carcinogenic, etc. Its degradation product should not be harmful to the body and excretable.
-
Have desirable chemical and physical and chemical stability.
-
Have suitable processability for the anticipated application.
-
Have suitable mechanical properties to bear the anticipated stress at the site of application for the intended period of use.
-
Carry the anticipated function at its site of implantation.
-
Be easy to process and sterilizable by validated sterilization techniques without any impairment.
-
Be cost-effective and reliable.
5 Classification of Biomaterials
Biomaterials can be classified on the basis of their source or application. Based on the source and material properties, the biomaterials can be classified into natural and synthetic biomaterials. The natural biomaterials are further classified into protein and polysaccharide-based biomaterials. The synthetic biomaterials are classified into metallic, polymeric, and ceramic biomaterials (Fig. 5). All these classes of biomaterials exhibit different physicochemical, mechanical, and biological properties, which help them to enable their function in or on the human body [5].
5.1 Natural Biomaterials
Natural biomaterials are obtained from living species, from either plants or animals [6]. The use of natural biomaterials in biomedical applications is not new; humans have been using them since ancient times. However, natural biomaterials have some drawbacks. The biomaterials themselves have a certain level of variability due to inherent differences between material sources that may make producing high levels of reproducibility difficult. Furthermore, unless the material is extremely pure, these substances may occasionally cause immunological reactions. Natural biomaterials are divided into two types 1) protein origin biomaterials and 2) polysaccharide origin biomaterials.
5.1.1 Protein Origin Biomaterials
Protein origin biomaterials are the primary structural components for many tissues. Proteins are essentially amino acid polymers arranged in a three-dimensional folded form. They are used for the fabrication of sutures, haemostatic agents, tissue scaffolds, and drug delivery systems. Examples of protein origin biomaterials include collagen, silk, fibrin, and gelatin (Fig. 6).
Collagen
Collagen is the most common protein in the human body and is essential for the development of skin and other musculoskeletal tissues. Collagen is a main structural component in the connective tissue. In mammals about 20–35% of whole-body protein content contains collagen. Based on the structure, currently 28 different forms of collagen are identified in the human body. All these structures consist of at least one triple helix. Among them, Type-I collagen is most prevalent and accounts for nearly 90% of collagen in the human body.
Collagen has attracted interest as an appropriate matrix material for tissue engineering, since it is the main component of the extracellular matrix and acts as a natural substrate for cell adhesion, proliferation, and differentiation. Collagen is one of the key initiators of the coagulation cascade because of its high thrombogenicity, which has led to its usage as a haemostatic agent. For a variety of surgical indications, several collagen-based haemostats are currently available or in clinical studies.
Collagen undergoes enzymatic degradation in the presence of collagenases and metalloproteinases and yields amino acids. Because of their enzymatic biodegradability, interesting physicochemical, mechanical, and biological properties, collagen has been processed into different forms such as sheets, tubes, sponges, foams, nanofibrous matrices, powders, fleeces, injectable viscous solutions, and dispersions for biomedical applications. Several forms of collagen derivatives are used as scaffold materials for cardiovascular, musculoskeletal, and nervous tissue engineering applications.
Due to collagen’s high reactivity, a variety of compounds, such as polyepoxy substances, hexamethylene-diisocyanate, carbodiimides, difunctional or multifunctional aldehydes, and succinimidyl ester polyethylene glycol, can be used to create cross-link collagen. Due to highly favourable interactions of collagen matrix with the proteins, collagen can be used in the protein delivery applications. The applicability of collagen also extends into gene delivery owing to its good Injectability and good protective property from the enzymatic degradation. The composite biomaterials of collagen are also used in different orthopaedic applications. For example, one of the FDA-approved composite “collagrafts” comprised of fibrillar collagen, hydroxyapatite, and tricalcium phosphate is used as a biodegradable synthetic bone graft material.
Silk
Silk is a natural polymeric protein fibre produced by different insect species. The first record of silk use as a biomaterial dates back to Chinese and Indus civilizations around 2500 BC. Silk possesses excellent biocompatibility, self-assembly, mechanical properties, controllable structure formation, and interesting morphology. Such characteristics make silk-based biopolymers valuable candidates in the biomedical field for wound healing and tissue engineering. The silk fibroin forms three-dimensional structures such as sponges, foams, and scaffolds, which are used in tissue engineering, disease models, and implantable devices. Silk is also used in biomedical textiles as wound dressing material due to its good toughness, tensile strength, and ductility. Silk has good mechanical properties, softness, and antibacterial properties, contributing to its use in hygiene and healthcare products including materials used in hospital wards and operating rooms. Silk materials are employed in operating theatres as patient drapes and surgical equipment such as gowns, caps, masks, cover cloths, etc. Silk fibroin-based biomaterials are also used as skin grafts, bone grafts, as well in the preparation of artificial skin. Silk-based biomaterials are also used in other applications such as regenerating ligaments, tendons, and cardiac tissues. Silk is also used as a suture in cardiovascular, ophthalmic, and neurological surgeries, owing to its good knot strength, ease of processing, low propensity to rip through tissue, and good biocompatibility.
Fibrin
Fibrin is a non-globular protein, which is involved in the clotting of blood. Fibrin has been one of the most well-known biomaterials since it was first extensively purified in the 1940s. The application of fibrin as a biomaterial is very diverse in the medical field. For tissue engineering applications, fibrin gels are created by mixing fibrinogen, NaCl, thrombin, and CaCl2. Its key advantages include being highly biocompatible, having the ability to control tissue regeneration, and fast polymerizing reaction. Fibrin-based biomaterials are useful for tissue engineering applications because they can act as a scaffold for tissue healing, and they promote cellular proliferation. Tisseel was the first FDA-approved tissue sealant based on fibrin that is available in the market for clinical applications. Later, other sealant brands such as Beriplast and Biocol entered the market. ARTISSfibrin is another fibrin-based sealant (Baxter International Inc., Deerfield, Illinois, USA) available in the market. It is used to adhere autologous skin grafts in wound healing. Fibrin glue is used in the postoperative process in place of sutures or dressings to enhance healing and lessen scarring.
Gelatin
Gelatin is a molecular derivative of type I collagen. Like collagen, the major structural components in the gelatin include glycine, proline, and hydroxyproline. Gelatin is primarily created when the triple helical structure of collagen is irreversibly hydrolysed by methods like heat and enzymatic denaturation, leaving behind randomly coiled domains. Therefore, gelatin has a very similar molecular composition to collagen, but it is less organized than collagen. Gelatin is a fibrous insoluble protein and is a major component in skin, bone, and connective tissues. Gelatin can be extracted from several sources like cattle bones, fish, pig skins, and some insects. Compared to the extracellular matrix proteins such as collagen, fibronectin, and laminin, gelatin has gained more popularity as a biomaterial in the biomedical field due to the following reasons.
-
(i)
Gelatin is readily available at less cost.
-
(ii)
The solubility of gelatin is much higher when compared to extracellular matrix proteins.
-
(iii)
The molecular structure of gelatin is similar to the structure of collagen and contains important binding sites for cell attachment.
-
(iv)
Gelatin is highly biocompatible, biodegradable, and doesn’t show any toxic effects, and antigenicity to the human cells.
Gelatin is highly useful in cell and tissue culture applications and also used as a plasma expander, wound dressing, adhesive, and absorbent pad for surgical application. Gelatin is used in pharmaceutical products including hard capsules, soft capsules, and tablets. The gelatin film is used in both hard and soft capsules to mask the taste and odour of the medications inside while also shielding them from the outside environment. Gelatin is employed in tablet applications as a natural binding and disintegrating agent as well as an excellent tablet coating that protects the active ingredients against oxidation and light damage. It is frequently found in body care items such as facial creams, suntan lotions, shampoos, and moisturizing creams.
5.1.2 Polysaccharide Origin Biomaterials
Polysaccharides are long-chain polymeric biomaterials composed of monosaccharide units bound together by glycosidic linkages glycosidic linkages.The polysaccharides are abundant in nature, and they can be extracted from different sources such as algae, plants, microorganism, and animals. Examples of polysaccharide biomaterials obtained from algae include alginate, agarose, galactans, and carrageenan. Cellulose, pectin, guar gum, and starch are examples of plant-derived polysaccharides. Similarly, the polysaccharides extracted from the microorganism include xanthan gum, dextran, gellan gum, pullulan, and bacterial cellulose. Hyaluronan, chondroitin, heparin, chitin, and chitosan are polysaccharide biomaterials extracted from animals. Polysaccharides possess different physiochemical and biological properties that depend on their chemical structure, functional groups, charge, etc. Based on the charge, the polysaccharide-based biomaterials are classified into three sub-classes: 1) positively charged polysaccharides; 2) negatively charged polysaccharides; 3) neutral polysaccharides. Examples of positively charged, negatively charged, and neutral polysaccharide biomaterials include chitosan, hyaluronan, and cellulose respectively. In this section, we describe a few commonly employed polysaccharide biomaterials (Fig. 6) for medical applications:
Cellulose
Cellulose (C6H10O5)n is the most prevalent natural polysaccharide with adjustable characteristics. It is used in diverse biomedical applications such as drug delivery and tissue engineering. It is composed of several d-glucose units connected through β-(1–4) glycosidic bonds. The polysaccharide chains in the cellulose are aligned in parallel to form microfibrils with high tensile strength. Cellulose is the structural component for primary cell wall of plants. Cellulose is usually obtained from plants, fungi, algae, animals, and certain species of bacteria (example: acetobacter xylinum). Cellulose is a tasteless and odourless biodegradable neutral polysaccharide.
Depending on the source of origin, cellulose is available in a variety of compositions and morphologies. The high intramolecular hydrogen bonding of cellulose is responsible for its high solution viscosity, strong crystallization propensity, and capacity to form fibrillar threads. Owing to their good biocompatibility, cellulose-based biomaterials are widely used in drug delivery applications, wound healing, and as tablet binders, coating materials, and viscosity modifiers. Cellulose has a wide range of uses in cartilage tissue engineering. It offers a platform for cell growth and development. The microcrystalline cellulose and powdered cellulose derivatives such as E460i and E460ii are widely used as inactive fillers in tablet manufacturing.
Chitosan
Chitosan is a prevalent polysaccharide biomaterial found in nature. It is a liner polysaccharide and is made up of randomly distributed deacetylated unit “β-(1 → 4)-linked D-glucosamine” and acetylated unit “N-acetyl-D-glucosamine”. The free –NH2 and –OH groups in the structure of chitosan enable it to react with a wide variety of chemical entities to form chitosan-based biomaterials. The distinctive properties of chitosan such as biocompatibility, its affinity towards biomolecules, and suitable chemical structure for chemical modifications allow its utility as a prominent material for biomedical applications. Several factors such as crystallinity, molecular weight of the polymer, and degree of deacetylation influence the physiochemical properties of the chitosan. The applicability of chitosan-based biomaterials has been found in tissue engineering, regenerative medicine, drug delivery, and wound dressings.
The chitosan salts with organic acids such as succinic or lactic acid are used as haemostatic agents. Due to its positive charge, protonated chitosan attracts platelets, causing them to quickly clump together and form thrombuses. Chitosan derivatives are used as artificial kidney semi-permeable membranes. The properties of chitosan derivatives such as optical clarity, mechanical stability, sufficient optical correction, gas permeability, wettability, and immunological compatibility make them useful in the development of ocular bandage lenses.
Hyaluronic Acid
Hyaluronic acid is an example of anionic polysaccharide. It is widely distributed in connective, epithelial, and neural tissues. Hyaluronic acid is a glycosaminoglycan comprised of alternating N-acetyl glucosamine and D-glucuronic acid units connected through β (1–4) and β (1–3) linkages respectively. Hyaluronic acid is a naturally occurring substance found primarily in extracellular matrix, synovial fluid in joints, the umbilical cord, skin, the vitreous humour of the eye, and articular cartilage. Due to the presence of a carboxyl group in its structure, hyaluronic acid is classed as a naturally occurring negatively charged polysaccharide. Hyaluronic acid can absorb a significant amount of water and swell up to 1000 times its original volume. Many researchers use this property to build hyaluronic acid-based drug delivery systems. Additionally, hyaluronic acid is a strong candidate for chemical functionalization due to the availability of free carboxyl and hydroxyl groups. Owing to its properties such as hydrophilicity and biocompatibility, hyaluronic acid has a wide range of uses in biomedical field, particularly in the design of drug delivery systems and tissue engineering. The hyaluronic acid is an FDA-approved biomaterials that frequently is used to treat knee osteoarthritis through intra-articular injection. It is also used in some of the eye formulations to create artificial tears to treat dry eye disease.
Dextran
Dextran is a hydrophilic homopolysaccharide, which is made up of α-1,6-linked D-glucopyranose units with a low percentage of α-1,2-, α-1,3-, or α-1,4-linked side chains. Dextran is a bacterially derived polymer. It is derived from sucrose by the catalytic action with dextransucrase or enzymatic hydrolysis of maltodextrin by dextrinase. Dextran is a water-soluble polysaccharide and is usually stable in mild acidic and basic environments. Due to the high abundance of hydroxylic groups in dextran, it can be derivatized using chemical and physical crosslinking to produce various scaffolds like spheres, tubules, and hydrogels. In the body, dextran is slowly broken down by human enzymes and microbial enzymes present in the gastrointestinal system. The characteristics of dextran such as low toxicity, biocompatibility, biodegradability, and suitability for chemical modifications allow its use in the biomedical field. Dextran is clinically used as an antithrombotic agent, plasma volume expander, viscosity-reducing agent, etc. It is also used to reduce the inflammatory response. Dextran and its derivatives are also used in drug delivery and tissue engineering applications.
Alginate
Alginate is a naturally occurring, anionic, and hydrophilic polysaccharide, which is usually obtained from brown algae (examples: Laminaria hyperborea, Laminaria digitata, Laminaria japonica, etc.). It is a block copolymer of (1–4)-linked β-D-mannuronic acid (M-block) and α-L-guluronic acid (G-Block) monomers. The physicochemical properties of the alginate vary with the length of the block, and the M/G ratio as well as the arrangement of repeating units in its structure. The carboxylic and cis diol groups found in alginate monomers enable the chemical functionalization of this polysaccharide with various moieties such as amino acids, alkyl groups, etc. Because of their biocompatibility, mechanical flexibility, crosslinking activity, and gelling qualities, alginate-based biomaterials are employed in various biomedical applications.
Alginates can form ionic gels in the presence of divalent metal cations like Ca2+, where the high amount of G-clock in the alginate reacts with the Ca2+ and forms an egg-box-like conformational arrangement. Alginates can form hydrogels with a variety of cross-linking agents. The hydrogels of alginate are structurally similar to extracellular matrices of the living tissues. Therefore, the applications of alginate-based hydrogels are extensively found in wound healing, drug delivery, and cell transplantation in tissue engineering. In drug delivery, the controlled release of drugs and other macromolecular proteins from the hydrogel matrix of alginate depends on the cross-linker types used to prepare alginate hydrogel. Moreover, alginate gels can be administered orally or injected into the body in a minimally invasive manner, allowing for a wide range of pharmaceutical applications. Due to their high biocompatibility and low toxicity, the alginate derivatives are also used in the food industry and dentistry.
Pullulan
Pullulan is an exopolysaccharide obtained from yeast-like fungus Aureobasidium pullulans. Chemically, pullulan is comprised of maltotriose repeating units connected by α-(1–6) glycosidic bonds. It is a linear unbranched polysaccharide with a molecular formula of (C6H10O5)n. Pullulans are available with molecular weights in the range of 4.5 × 104 to 6 × 105 Da. The hydroxyl groups present in the structure of pullulans provide an opportunity for chemical modification with a variety of amino acids, alkyl chains, metal nanoparticles, etc. The characteristics of pullulans such as biodegradability, no toxicity, and nonmutagenicity allow their utility in drug delivery and tissue engineering applications.
Chondroitin Sulphate
Chondroitin sulphate (CS) is an anionic heteropolysaccharide, comprised of repeating disaccharide units of β-1,3-linked d-glucuronic acid and β-1,3-linked N-acetyl galactosamine having sulphate groups at various carbon positions. CS is classified into five subgroups based on the position of the sulphate group: chondroitin-4-sulphate; chondroitin-2,4 sulphate/dermatan sulphate; chondroitin-6-sulphate; chondroitin-2,6-sulphate; and chondroitin-4,6-sulphate. The molecular weight of CS varies in the range of 20–25 kDa. The unique characteristics of CS such as biocompatibility, biodegradability, mucoadhesion, and hydrophilicity allow its wide utility in the biomedical field. CS possesses anti-inflammatory, antioxidant, antithrombotic, anticoagulating, and immunomodulatory properties. Hence, CS is used in the biomedical field for managing cardiovascular, cancer, wound healing, and joints-related pathologies. CS is used as a natural supplement for the treatment of osteoarthritis. CS is an FDA-approved biomaterial to use as a skin substitute. CS is also used in the drug delivery applications.
5.2 Synthetic Biomaterials
This class of biomaterials are synthesized in the laboratory for biomedical purposes [7]. The synthetic biomaterials are further subdivided into ceramic, metallic, and polymeric biomaterials. The characteristics, applications, and disadvantageous of these classes of synthetic biomaterials are summarized in Table 1.
5.2.1 Ceramic Biomaterials
Ceramic biomaterials and their composites have received significant importance in the biomedical field due to their properties such as resistance to corrosion, high mechanical strength, high stiffness, hardness, high compression strength, wear resistance, durability, and low density. They can be effective with compressive force, but poor with tension force. Ceramic biomaterials are electric and thermal insulators. They are widely used bioactive inert materials in the human body. Ceramic materials are widely used in orthopaedics and dentistry. Ceramic biomaterials are categorized into three types: 1) ceramic bioactive materials, 2) ceramic bio-inert materials, and 3) ceramic bioresorbable materials.
Bioactive ceramic materials interact with the surrounding bone and soft tissue after being inserted them into the human body. Their implantation into the living bone causes a time-dependent kinetic modification of the surface. Some of the common examples of ceramic bioactive materials include synthetic hydroxyapatite [Ca10(PO4)6(OH)2], glass ceramic, and bioglass.
On the other hand, examples of bio-inert materials include stainless steel, titanium, alumina, partly stabilized zirconia, and ultra-high-molecular-weight polyethylene. These materials have limited interaction with the surrounding tissue once implanted in the human body. In general, a fibrous capsule may grow around bio-inert implants. Therefore, the bio-functionality of bio-inert materials is dependent on tissue integration through the implant. Bio-inert materials that are especially compatible with body parts include silicon nitride (Si3N4), zirconia (ZrO2), alumina (Al2O3), and pyrolytic carbon. They are widely used in hip prostheses, bone scaffolds, spinal fusion implants, hip joint replacement, and dental implants.
Bioresorbable refers to a substance that, when introduced into the human body, begins to disintegrate and is gradually replaced by a new tissue. This class of ceramics is comprised mainly of calcium. Some of the examples of bioresorbable ceramic materials include calcium phosphate, aluminium calcium phosphate, tricalcium phosphate, calcium aluminates, zinc sulphate calcium phosphate, zinc calcium phosphorous oxide, and ferric calcium phosphorous oxide. These compounds undergo hydrolytic breakdown in the body at their implantation site. The degraded products produced from the process are absorbed by the body and eliminated through the standard metabolic process. They are highly useful as dental restorative products as well as in orthopaedic applications. They are used as artificial bones, teeth, knees, hips, tendons, and ligaments.
In order to apply ceramic biomaterials to medical applications they must possess a certain set of characteristics including non-allergic, bio-functional, bio-compatible, non-carcinogenic, non-toxic, and non-inflammatory. The applicability of ceramic materials has also been well explored in the dental field because of their high inertness to the biological fluid like saliva, aesthetically favourable appearance, and excellent compressive strength. Their utility is also explored in drug delivery applications. The black pyrolytic carbon ceramic materials are easy to make and have good biocompatibility. They are widely used in cardiovascular implants. Owing to their good strength, they are also used in composite implant materials supporting components for tensile loading applications, e.g., loading of artificial ligaments and tendons.
5.2.2 Metallic Biomaterials
Metallic biomaterials have been given significant importance in the biomedical field because of their excellent thermal, electrical, and mechanical properties. They have been widely used in the preparation of artificial heart valves, pacemaker leads, and vascular stents. They are also used in load-bearing implants such as hip and knee replacements. Metallic biomaterials are also used as electrodes due to their high conductivity. However, there are certain drawbacks to the metallic biomaterials such as high modulus, cytotoxicity, easy corrosion, and metal ion sensitivity that reduce their utility as implant materials.
The physicochemical and mechanical properties of metallic biomaterials can be fine-tuned by incorporating multi-metal functionality. This can be achieved by surface modification, such as surface structuring or coating with bioactive ceramic materials and polymer thin films. The resultant chemically modified biomaterials obtained from this method are called “bio-metallic alloys”, which are highly inert to the biological system; hence, they possess high corrosion resistance, long-term stability, and reliable mechanical strength. In addition, they also possess excellent tensile strength, fracture toughness, and fatigue stress. These characteristics allow them to be used in orthopaedics (used as artificial joints, plates, and screws), orthodontics (used as braces, and dental implants), cardiovascular implants (used in artificial hearts, and stents), neurosurgical devices, etc. The first metal alloy implant, “Sherman Vanadium Steel”, was developed to manufacture bone fracture plates and screws. Some of the other commonly used metallic biomaterials include pure Ti, Ti-6Al-4 V, Co-Cr alloys, stainless steel, noble metal alloys, and shape memory alloys.
The metallic biomaterials are majorly classified into three major groups: Ti-alloys, stainless steel, and Co-Cr alloys (Fig. 7).
Stainless Steel
Stainless steel is resistant to rust and corrosion and is an alloy of iron. It contains chromium along with carbon, other non-metals, and metals to produce desirable characteristics. The corrosion resistance of stainless steel is attributable to chromium, which forms a passive layer that protects the material and self-heal in the presence of oxygen and water. Reducing the Ni-content in the stainless steel offers improved protection from corrosion. Due to characteristics such as good toughness, biocompatibility, and easily producible with low cost, stainless steel is widely used in biomedical applications. Different types of stainless steel are produced by industries, among them austenitic stainless steel is most widely used for the orthopaedic applications in the forms of screws, plates, and hip-nails apparatus.
Co-Cr Alloys
Cobalt-based alloys were initially utilized as medical implants in the 1930s. They are one of the hardest and biocompatible alloys. They possess high wear and corrosion resistance properties and are used as orthopaedic implants. Cobalt-based alloys were the first alloys to be used in dental implants. Their applications also extend to joint and fracture fixing. There are a variety of biocompatible Co-based composites available, including CoCrMo, CoCr, and Ni-free CoCrW alloys. Cobalt-chromium alloys are generally classified into two types: (i) Co-Cr-Mo alloy and (ii) Co-Cr-Ni-Mo alloy. Bearing good corrosion protection, high loading capacity, stronger fatigue and elastic-modulus, Co-Cr-Mo alloys have been used for many years in dentistry, and recently in orthopaedic treatment, especially for joint reconstructions. Co-Cr-Ni-Mo’s are used in the high loading prosthesis for joint rebuilding of knee and hip problems in biomedical treatment. Co-based alloys are extremely resistant to corrosion.
Titanium Alloys
Ti and its alloys have received interest in the biomedical field especially in the orthopaedic and dental applications because of their good mechanical properties, corrosion resistance, and good biocompatibility. Commercially, pure titanium and the alloy of Ti-6Al-4 V are frequently used metallic biomaterials applied for dental and orthopaedic applications. However, the long-term use of Ti-6Al-4 V implants causes an allergic reaction in human tissue due to leaching of aluminium and vanadium. As a result, new alloys free from cytotoxic components are now being developed.
Recently magnesium (Mg), iron (Fe), tantalum (Ta), and zinc (Zn) alloys have received significant interest as biodegradable metallic alloys. Among them, Mg is essential for human metabolism, and it possesses enough tensile strength, and resistance to the fracture. It is a lightweight element; therefore, Mg-based alloys are used to support the load-bearing applications, particularly applied in stents and small fracture repairs. Mg is well known to provide stimulatory effects on the generation of new bone tissues. The biodegradability of the Mg-based metallic scaffolds and implants is fine-tuned by changing the ratio and type of the alloying metals. However, the performance of biodegradable metallic implants is significantly undermined by characteristics such as the risk of infection and inflammation. This phenomenon significantly leads to the loss of tissues or cells in the proximity of the implant. Another challenge associated with metallic biomaterials is their biodegradation that leads to premature loss of the mechanical strength of the implant system.
5.2.3 Polymeric Biomaterials
Polymers are long-chain macromolecules comprised of covalently bonded repeating monomer units. Polymers constitute the largest class of diverse biomaterials. Depending on their origin, they are classified as synthetic or natural polymeric biomaterials. Owing to their unique properties such as biocompatibility, controlled biodegradability, non-toxicity, and remodelling, polymeric biomaterials have attracted considerable interest in the biomedical field. In this section, we provide a brief summary and applications of the synthetic-derived polymeric biomaterials. The natural polymeric biomaterials are already summarized in the Sect. 2.1. Natural biomaterials.
Based on degradation behaviour, synthetic polymers are classified into two classes: 1) synthetic degradable polymeric biomaterials and 2) synthetic non-degradable polymeric biomaterials.
5.2.3.1 Synthetic Degradable Polymeric Biomaterials
This class of biodegradable polymers has gained significant interest in the medical field, because of their interesting physicochemical properties and biodegradability [8]. The first example of a synthetic biodegradable polymer produced is poly(glycolic acid) (PGA) in 1954. Some other examples for synthetic biomaterials include polylactic acid (PLA), polyethylene glycol (PEG), poly (lactic-co-glycolic acid) (PLGA), polycaprolactone (PCL), and polydioxanone (PDS). These synthetic biodegradable polymeric materials are alternatives to the natural biodegradable polymers. They undergo controlled degradation into small monomer species under in vivo conditions due to hydrolysis or enzymatic actions occurring in the body. The degraded products of polymeric biomaterials are non-toxic, which do not show any inflammatory reactions in the body. The degraded products are easily metabolizable and are excretable. For example, PLGA undergoes hydrolytic cleavage into biocompatible monomers glycolic acid and lactic acid. The biodegradation of the polymeric structures is affected by its molecular weight, hydrophilicity, hydrophobicity, etc. Examples of some of the most used synthetic polymer for biomedical applications are summarized below (Fig. 8):
Polylactic Acid (PLA)
PLA is a thermoplastic polymer obtained from the condensation reaction of lactic acid or ring-opening polymerization of lactide in the presence of an organometal catalyst like stannous octate. It is one of the largely consumed polymeric bioplastics. PLA occurs in the form of L-PLA, D-PLA, and in the mixture of D,L-PLA. PLA undergoes hydrolytic degradation through a desertification process and leads to the formation of lactic acid monomer as a by-product. Lactic acid is biocompatible and can be easily eliminated from the body through a natural biochemical pathway. Therefore, PLA and PLA-based derivatives are often used in the biomedical implants in the form of screws, anchors, pins, plates, rods, and as a mesh. The average biodegradation time of PLA varies from 6 months to 2 years based on its structure and molecular weight. Due to good control over the biodegradation rate of PLA and its derivatives, they are widely used for the fabrication of different drug delivery systems. The composite materials of PLA are also extended for different biomedical applications. For instance, the composite of PLA/tricalcium phosphate is used as a scaffold for bone engineering. PLA derivatives are also used in the 3D printing technology to print artificial biological structures.
Polyglycolic Acid (PGA)
Like PLA, PGA is also a thermoplastic polymer obtained from the condensation of glycolic acid or ring opening polymerization from glycolide in the presence of an organometal catalyst such as stannous octate. PGA is a linear polymeric biomaterial used as implants in vascular and orthopaedic surgeries. Both PLA and PGA are FDA-approved synthetic polymers used to produce resorbable stitches. The degraded products of PGA are water soluble and are easily eliminated from the body completely between 2 to 3 months. Medically, PGA is used to produce implantable medical devices such as anastomosis rings, pins, rods, plates, and screws. Its application also extends to tissue engineering and drug delivery. Owing to its properties such as high tensile strength, easy handling, and excellent knotting ability, PGA is used in subcutaneous sutures, intracutaneous closures, and abdominal and thoracic surgeries. Copolymers of PGA such as poly(lactic-co-glycolic acid), poly(glycolide-co-caprolactone), and poly(glycolide-co-trimethylene carbonate) are widely used in the preparation of surgical sutures.
Poly(Lactide-Co-Glycolide) (PLGA)
PLGA is a copolymer of the lactide and glycolide and is obtained from the ring-opening polymerization of these two monomers in the presence of stannous octate catalyst. PLGA is an FDA-approved polymer used in a variety of biomedical devices such as grafts, sutures, implants, prosthetic devices, and surgical sealant films. The physicochemical properties such as crystallinity, glass transition temperature, solubility, and degradation properties of PLGA can be varied by changing the molar ratio of the lactide and glycolide content in the polymer. For example, increasing glycolic acid content in the copolymer leads to faster degradation of the PLGA and is vice versa when it contains high content of lactide in the structure. PLGA undergoes hydrolytic degradation in the presence of water and breaks to non-toxic by-products, lactic acid, and glycolic acid. These products are easily eliminated from the body. The glass transition temperature of PLGA varies from 40 to 60 °C. Because of the controlled biodegradability, biocompatibility, and suitable glass transition temperature, PLGA is widely used in various drug delivery applications. PLGA is also used as scaffolds for bone, skin, cartilage, and nerve regeneration applications.
Polydioxanone (PDS)
PDS is one the ether-ester-linked synthetic biodegradable polymers obtained from the ring opening polymerization of p-dioxanone in the presence of an organometallic catalyst like zirconium acetylacetone or zinc L-lactate. The glass transition temperature of PDS varies in the range of −10°C to 0°C. Due to the low glass transition temperature, PDS is not thermally stable as are other biodegradable synthetic polymers such as PLA and PLGA. Therefore, polymer processing for medical applications is usually kept under as much as low possible temperatures to avoid depolymerization of PDS. The characteristics of PDS such as high biocompatibility, and mechanical flexibility, enable its utility in the biomedical field for the preparation of surgical sutures. The applicability of PDS also extends to several other biomedical fields including tissue engineering, orthopaedics, drug delivery, maxillofacial surgery, plastic surgery, and cardiovascular applications.
Polycaprolactone (PCL)
PCL is an aliphatic biodegradable polyester obtained from the ring-opening polymerization of ε-caprolactone in the presence of a metal-based catalyst like Stannous (II) octoate. It is a hydrophobic, semi-crystalline, and thermoplastic polymer. It undergoes slow ester hydrolysis under physiological conditions over a variable period of time that depends on the PCL molecular weight, degree of crystallinity, and degradation conditions. Therefore, PCL is widely used in controlled drug delivery applications. It is used for a variety of medical applications including sutures, wound dressing, cardiovascular tissue engineering, nerve regeneration, and bone tissue engineering. Few PCL-based drug delivery devices and sutures are FDA approved. However, PCL has some limitations such as slow degradation rate, poor mechanical properties, and low cell adhesion properties that shorten its utility in the biomedical field, particularly in tissue engineering. Preparation of composite biomaterials with PCL leads to remarkably improved mechanical properties, controllable degradation rates, and enhanced bioactivity that are suitable for a variety of biomedical applications.
Polyvinyl Alcohol (PVA)
PVA is 1,3-diol linkage synthetic biodegradable polymer, which is usually obtained from the hydrolysis of polyvinyl acetate. PVA is a crystalline material soluble in the water. PVA forms strong and ultrapure hydrogels without any cross-linking agents. It also exhibits good biocompatibility with low protein adhesion tendency. Owing to these properties, PVA is widely used for the fabrication of vascular stents, cartilages, contact lenses, drug delivery carriers, etc.
Recently, some other classes of synthetic biodegradable polymers such as polyanhydrides, polyphosphazenes, block copolymers with PEG, and poly-(alkylcyanoacrylates) have received importance for a variety of biomedical applications. Among them, research on polyanhydride biodegradable polymers is currently a popular topic of research due to their controlled surface erosion, and shorter average half-lives properties. Polyanhydrides shows controlled drug release property for a variety of drugs, hence they are extensively used as a drug delivery carrier. Poly(sebacic acid-co-1,3- bis(p-carboxyphenoxy)propane) is an example of a polyanhydride used for the fabrication of FDA-approved Gliadel wafers used for the localized brain delivery of 1,3- bis(2-chloroethyl)-N-nitrosourea against brain cancer. Polyanhydride copolymers of erucic acid dimer and sebacic acid are used for the fabrication of septacin implants for the controlled delivery of gentamicin sulphate in the treatment of osteomyelitis.
5.2.3.2 Synthetic Non-degradable Polymeric Biomaterials
This class of polymers does not undergo biodegradation; however, because of their prominent physicochemical properties, these polymers are widely used in the biomedical field. Some of the common non-degradable polymeric biomaterials used for the medical purpose are summarized as follows (Fig. 8):
Poly-Methyl-Methacrylate (PMMA)
PMMA is obtained by the free radical polymerisation of methyl methacrylate monomers. PMMA is lightweight, transparent, and it possess good mechanical properties. PMMA is used in orthopaedic applications. PMMAs possess good biocompatibility, hence they are widely used for the preparation of intraocular lenses. PMMA is also used in the cosmetic surgeries and in dentistry for the fabrication of dental prosthetics, artificial teeth, and orthodontic appliances.
Polyurethanes (PUs)
PUs are alternating polymers obtained from the reaction between diisocyanates (hard segments) and polyols (soft segments) in the presence of light or catalyst (example: dibutyltin dilaurate, DABCO, etc.). In 1937, Otto Bayer and his co-workers developed the first PUs. By changing the ratio of hard and soft segments during the synthesis of polymer, variety of PU derivatives are designed for biomedical applications such as rubber, fibres, films, paints, coatings, elastomers, foams, gels, etc. For many decades, PU derivatives have been used in the biomedical field due to their prominent physicochemical characteristics such as high tensile strength, good durability, fatigue resistance, and excellent biocompatibility. PU derivatives are used as scaffolds in tissue engineering, shape memory devices, nontoxic implants, various cardiovascular implants, wound healing, and bone regeneration.
Polysiloxanes
Polysiloxanes are prepared by the hydrolysis of alkyl silicon or polysilicon halides. Polysiloxanes are comprised of a Si-O backbone and with functional groups such as methyl are typically attached to the Si atom. Changing the −Si − O− chain lengths, side groups, and different cross-linking agents produces a variety of polysiloxane-based derivatives with interesting physicochemical characteristics. Poly(dimethylsiloxane) (PDMS) is one of the common examples of this class of polymers, which is frequently used as an implantable device for a long time in the biomedical field. Polysiloxanes are used in the fabrication of elastomers, gels, lubricants, foams, and adhesives. Polysiloxanes are hydrophobic and possess good biocompatibility, electrical insulation, and bio-durability characteristics. The applications of polysiloxanes and its derivatives include finger and toes joints, heart valve prostheses, blood oxygenation membranes, breast implants, artificial ventricles, wound dressings, plastic surgery, penile prostheses, intraocular lenses, vitreous humour, etc. They are used in orthopaedics as hand and foot joint implants material. They are also extensively used in cosmetic implants for aesthetic and reconstructive plastic surgeries.
Poly(Ethylene), Poly(Propylene), and Poly(Styrene)
Poly(ethylene) (PE), poly(propylene) (PP), and poly(styrene) (PS) are common synthetic non-biodegradable polymers used for medical applications. They are thermoplastic polymers. PE, PP and PS are obtained by the radical or metal-mediated polymerization of their corresponding monomers, i.e., ethylene, propylene, and styrene respectively. High-density PE possesses strong intermolecular forces and tensile strength due to a low degree of branching; hence it is widely used in the fabrication of highly durable hip and knee prostheses. Moreover, high-density PE is also used to construct implants that have been used for facial and cranial reconstruction. The copolymers of PE, i.e., poly(ethylene-co-vinyl acetate) is an FDA-approved biomaterial that has been widely used in the fabrication of drug delivery systems. Ocusert and progestasert are some examples of poly(ethylene-co-vinyl acetate)-based drug delivery systems. The applications PP are well known and found in syringe bodies. Due to their hard and brittle nature, the PS is widely used for the fabrication of tissue culture flasks and dishes. The copolymerization of PS with butadiene allows the fabrication of catheters and medical devices for perfusion and dialysis with improved elasticity.
Poly(Ethylene Glycol)
Poly(ethylene glycol) or poly(ethylene oxide) is an ether-linked hydrophilic polymer. PEG is obtained by the polymerization of ethylene oxide in the presence of an acidic or basic catalyst. The high molecular weight PEG can form hydrogels. PEG possesses high hydrophilicity, bio inertness, and outstanding biocompatibility, which allow its utility as a suitable candidate for biomedical applications. PEG-based copolymers are widely used for the delivery of a variety of drugs. They are also used as tissue engineering scaffolds, medical devices, and implants. A variety of PEG-based block copolymers are used for the fabrication of injectable drug delivery carriers. One example is pluronics or poloxamers, which is a triblock copolymer, composed of two hydrophilic PEG blocks and one hydrophobic poly (propylene oxide). Poloxamers are extensively studied as a non-biodegradable carrier for the delivery of a wide variety of drugs. PEG is also used as an inactive ingredient in the pharmaceutical industry as a plasticizer, surfactant, ointment, suppository base, capsule lubricant, and so on. Other applications of PEG include bio-sensing, imaging, bone, and tissue engineering.
6 Applications
Today biomaterials are used in every sphere of biomedical science whether it be diagnostic application, or tissue replacement to tissue regeneration. They have expanded their applications especially over the last few decades, from medical equipments to therapeutic medications and emerging regenerative technologies, and it is continuing to expand more [9]. Five major applications of biomaterials are discussed here to clarify the important ideas (Fig. 9).
6.1 Tissue Engineering
Tissue engineering is one of the most prominent applications of biomaterials, i.e., to repair or replace (partially or completely) a tissue/organ in the body to maintain and restore or improve a body function. Tissue engineering is defined by Langer and Vacanti as “a field that applies the principles of biology and engineering to the development of functional substitutes for damaged tissue”. Examples of tissue engineering applications are as follows:
6.1.1 Applications in Orthodontics
Biomaterials are used in dentistry for a long time as dental implants. The metallic materials are most widely used biomaterials for dental prosthesis in which the metallic biomaterial is integrated into the dental structure by the process called osseointegration. Zirconia, resin composites, titanium alloys, etc. are other widely used biomaterials for dental implants. Calcium hydroxide is another widely used biomaterial with application in root canal treatment.
6.1.2 Cardiovascular System Applications
Use of biomaterials in cardiovascular system is one of the most widely used applications of biomaterials. Biomaterial implants are used for a long time to treat blocked arteries, failure of cardiac valves, etc. Pathological changes in heart valves obstruct their proper opening and closing function that is usually treated by replacing the malfunctioned valve with an artificial one. A prosthetic heart valve can be either mechanical or biological. Some examples of biomaterials used for the mechanical prosthetic heart valves are silicone, stainless steel, titanium, and pyrolytic carbon. Biological prosthetic heart valves can be comprised of both biological (e.g., heart valve from pig and other human donor) and synthetic components like dacron and polytetrafluoroethylene (PTFE).
Similarly, pathological changes in the architecture of an artery can cause obstruction with the flow of blood that is treated by the use of a stent. Corrosion-resistant metals like nitinol, chromium-cobalt alloy, and stainless steel are widely used materials for the grafting of an artificial stent. Cardiopulmonary bypass systems, pacemakers, vascular grafts, and entire artificial hearts are other important examples of biomaterials applications in a cardiovascular system.
6.1.3 Ophthalmic Applications
Biomaterials are widely used for ophthalmic applications. One of the most important uses of biomaterials in ophthalmic is cataract surgery, i.e., replacement of an opacified eye lens with a prosthetic intraocular lens. Silicone and acrylic are commonly used biomaterials for the fabrication of the intraocular lenses. Other examples of biomaterials application in ophthalmic include artificial tears, contact lenses, and vitreous substitutions.
6.1.4 Orthopaedic Applications
Biomaterials have long been used in orthopaedics. One of the most important uses of biomaterials in orthopaedics is for joint prosthesis to repair or replace the joints of knee, hip, elbow, and shoulder. Zirconium oxide and aluminium oxide are the ceramic biomaterials widely used as bonding and bearing material for joint replacement. Polyacetal and polytetrafluorethylene are important biodegradable and bioresorbable materials used for bone plate applications. Polymeric biomaterials like polylactic acid, polydioxanone, and polyglycolic acid are widely used for the fabrication of screws, plates, and pins for bone fixation. Calcium salts such as phosphate and sulphates are another example of widely used biomaterials as bone substitutes to fill up bone defects.
6.2 Applications in Drug Delivery Systems
Today biomaterials are playing important roles in the medicines for the targeted and controlled drug delivery. Many drug moieties have very poor aqueous solubility or poor bioavailability. Rendering them unsuitable for a dosage form. In such cases, biomaterials like polymers and lipids are used to fabricate a drug delivery system that can circumvent these challenges. Examples of biomaterial applications in medicines include micro and nanoformulations for the controlled drug delivery in the context of releasing drug at a desired rate at their intended site of action. Liposomes, nanoparticles, drug-coated vascular stents, and wafer implants are important examples of biomaterial application in drug delivery.
6.3 Diagnosis
Diagnosis of a disease plays a crucial role in the final outcome of disease treatment. Biomaterials are also used for the diagnosis or biosensing, i.e., to detect and report the presence of specific biomolecules in the body. Biomaterials can be used to recognize and label a target biomolecule. Carbon nanomaterials are widely used as biosensor materials due to their good biocompatibility and optical and electronic properties. Transducers as sensors for brain activity and blood glucose monitoring devices are two important examples of biomaterial applications as a biosensor.
6.4 Wound Healing
Dressings, clips, sutures, bandages, and staples for wound closure are a commonly used application of biomaterials. Polyester copolymers, nylon, silk, bovine tissues, and teflon are examples of biomaterials used for wound healing.
6.5 Tissue Regeneration
Initially, biomaterials were conceived to repair or substitute an impaired biological function or tissue. Over recent years, however, biomaterial science has made great leaps, and it has moved from tissue engineering to tissue regeneration. Polymers and ceramics are widely used as scaffold material for tissue regeneration applications. For example, tri-calcium phosphate and hydroxyapatite are used as scaffold material for bone regeneration owing to their excellent biomechanical and biochemical compatibility with bone tissues. Polymers and copolymers of PGA, PLA, PCL, and PEG are studied as scaffold material for soft tissue regeneration. Recently, biomaterials are being used in tissue regeneration as biomaterials functionalized with extracellular vesicles. Biomaterials are being used as scaffold material seeded with living cells to regenerate or restore a missing biological tissue. Biomaterials are being used and studied as a platform to carry and deliver the mesenchymal stem cell exosomes to promote wound healing and skin regeneration.
7 Conclusion
Biomaterials are an incredibly powerful tool that is changing our lives daily. Biomaterials have expanded their applications especially over the last few decades, from tissue engineering to diagnostics, medical equipment to the therapeutic medications, and emerging regenerative technologies. The wide meaning has changed over time based on research and usage, and it may continue to expand with exciting advancements in the correspondingly emerging branches of biotechnology and medical science. Biomaterials are amongst the most multidisciplinary fields of all the sciences touching almost every sphere of the biomedical science. This chapter presents a broad picture of biomaterials and their applications that will be further elaborated throughout this book. This chapter guides the readers on how to proceed with the further chapters in this book and comprehend this intricate field of science.
References
Stanciu L, Diaz-Amaya S (2022) Introductory biomaterials an overview of key concepts
Williams DF (1999) The Williams Dictionary of Biomaterials. Liverpool University Press. https://doi.org/10.5949/upo9781846314438
Williams DF (2009) On the nature of biomaterials. Biomaterials 30:5897–5909
Ratner BD et al (2020) Introduction to biomaterials science. Biomaterials science. Elsevier. https://doi.org/10.1016/b978-0-12-816137-1.00001-5
Moizhess TG (2008) Carcinogenesis induced by foreign bodies. Biochemist 73:763–775
Joyce K, Fabra GT, Bozkurt Y, Pandit A (2021) Bioactive potential of natural biomaterials: identification, retention and assessment of biological properties. Signal Transduct Target Ther 61(6):1–28
Langer R, Tirrell DA (2004) Designing materials for biology and medicine. Nat 428:487–492
Domb AJ, Kost J, Wiseman D (1998) Handbook of biodegradable polymers. CRC press
Todros S, Todesco M, Bagno A (2021) Biomaterials and their biomedical applications: from replacement to regeneration. PRO 9
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Quiz/Multiple Answer Questions
Quiz/Multiple Answer Questions
-
1.
Which of the Following Is Not a Biomaterial :
-
(a) Dental Implants (b) Antibiotics (c) Prosthetic Limbs (d) Heart Pacemaker
-
-
Answer: (b) antibiotics.
-
Explanation: Antibiotics are drugs, which do not belong to the category of biomaterials.
-
2.
Biomaterials can be:
-
(a) Natural (b) Synthetic material (c) Both a and b (d) None of the above.
-
-
Answer: (c) Both a and b.
-
3.
What is the most important characteristic of a biomaterial :
-
(a) Biocompatibility (b) Biological functionality (c) Chemical stability (d) All.
-
-
Answer: (d) All.
-
4.
Which of the following is not the application of biomaterials :
-
(a) Drug delivery (b) Tissue replacement (c) Nutrition (d) Orthodontics.
-
-
Answer: (c) Nutrition.
-
5.
Among the following which is not a natural biomaterial :
-
(a) Polylactic acid (b) Collagen (c) Silk (d) Gelatin.
-
-
Answer: (a) Polylactic acid.
-
Explanation: Collagen, silk and gelatine and natural biomaterials are obtained from the biological source. Perhaps, the polylactic acid is a synthetic polymer which is obtained from the polymerization of lactic acid monomer (D,L-Lactide).
-
6.
Among the following which biomaterial belongs to the class of synthetic non-degradable polymers:
-
(a) poly(methyl methacrylate) (b) polyurethanes (c) both a and b (d) poly(lactide-co-glycolide)
-
-
Answer: (c) both a and b.
-
Explanation: poly(lactide-co-glycolide) consisting ester linkage in the polymer chain, which can undergo hydrolysis in aqueous environment. While the poly(methyl methacrylate) and polyurethanes are non-biodegradable and do not have any ester linkage to undergo hydrolysis.
-
7.
Among the following statements which one is incorrect for polyanhydrides biomaterials :
-
(a)
polyanhydrides are synthetic polymeric biomaterials.
-
(b)
polyanhydrides belong to the class of natural synthetic polymers.
-
(c)
polyanhydrides are biodegradable.
-
(d)
Both A and C.
-
(a)
-
Answer: (d) Both A and C.
-
Explanation: Polyanhydrides are synthetic polymer biomaterials, which are biodegradable.
-
8.
Biomaterial are not used as.
-
(a) Drugs (b) Drug delivery carrier (c) Medical implants (d) Diagnostics.
-
-
Answer: (a) Drugs.
-
9.
Among the following which is not belong to the class of metallic biomaterials:
-
Stainless steel (b) Co-Cr alloys (c) Hydroxyapatite (d) Ti and its alloys.
-
-
Answer: (c) Hydroxyapatite.
-
Explanation: Hydroxyapatite is an example for ceramic biomaterials. While the stainless steel, Co-Cr alloys and Ti and its alloys belong to the class of metallic biomaterials.
-
10.
Which of the following is a natural biomaterial?
-
A) Silicone B) Stainless steel C) Collagen D) Polyethylene.
-
-
Answer: C) Collagen.
-
Explanation: Collagen is a naturally occurring protein that is found in connective tissue and is commonly used as a biomaterial in various medical applications.
-
11.
Which of the following is not a biomaterial ?
-
a) Titanium b) Silicone c) Glass d) Polyester.
-
-
Answer: c) Glass.
-
Explanation: Glass is not considered a biomaterial because it is not naturally occurring in the body and does not interact with biological systems in the same way as other biomaterials.
-
12.
What is the primary purpose of biomaterials ?
-
(a)
To replace damaged or diseased tissue.
-
(b)
To stimulate tissue regeneration.
-
(c)
To enhance tissue function.
-
(d)
All of the above.
-
(a)
-
Answer: d) All of the above.
-
Explanation: Biomaterials can be used for a variety of purposes, including replacing damaged or diseased tissue, stimulating tissue regeneration, and enhancing tissue function.
-
13.
Which of the following is a disadvantage of using metallic biomaterials ?
-
(a)
Poor biocompatibility.
-
(b)
Limited mechanical properties.
-
(c)
High cost.
-
(d)
Susceptibility to corrosion.
-
(a)
-
Answer: d) Susceptibility to corrosion.
-
Explanation: Metallic biomaterials can corrode over time, leading to device failure or release of toxic ions into the surrounding tissue.
-
14.
What is the primary advantage of using biodegradable biomaterials ?
-
(a)
They are more biocompatible than non-biodegradable materials.
-
(b)
They reduce the risk of long-term complications.
-
(c)
They eliminate the need for removal surgery.
-
(d)
They are more cost-effective than non-biodegradable materials.
-
(a)
-
Answer: (b) They reduce the risk of long-term complications.
-
Explanation: Biodegradable biomaterials can be broken down and absorbed by the body over time, reducing the risk of long-term complications or the need for removal surgery.
Rights and permissions
Copyright information
© 2023 American Association of Pharmaceutical Scientists
About this chapter
Cite this chapter
Reddy, P.G., Saklani, R., Mandal, M.K., Domb, A.J. (2023). Introduction to Biomaterials. In: Domb, A., Mizrahi, B., Farah, S. (eds) Biomaterials and Biopolymers . AAPS Introductions in the Pharmaceutical Sciences, vol 7. Springer, Cham. https://doi.org/10.1007/978-3-031-36135-7_1
Download citation
DOI: https://doi.org/10.1007/978-3-031-36135-7_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-36134-0
Online ISBN: 978-3-031-36135-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)