Abstract
Spinal atypical meningiomas are rare, and those whose main extension is in the epidural space are anecdotal. Here, we report a case of a young woman presenting with sensory disturbances and a radiological diagnosis of a dorsal epidural sleeve-like mass. The surgical resection of the lesion allowed the decompression of the spinal cord and led to the histopathological diagnosis of atypical meningioma. At the 3-month follow-up, her neurological recovery was complete. Because of the gross total removal of the lesion, adjuvant radiotherapy was not performed: At the 2-year follow-up, no recurrence of disease was detected. A comprehensive literature review was performed, and just two more case reports on epidural atypical meningiomas were found in the English literature. Through this case report and literature review, we described a rare manifestation of spinal meningioma that entered into a differential diagnosis for extradural spinal lesions, such as secondary malignancies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Spinal meningiomas (SMs) typically arise into intradural extramedullary space. Rarely, they may originate extradurally, which is more likely the origin site of malignant neoplasms such as metastases or lymphoma [1]. About 10% of all spinal meningiomatous lesions have an extradural extension, while those originating purely extradurally are extremely rare [2]. The occurrence of high-grade epidural SMs is almost anecdotal. Herein, we describe the case of a young woman presenting with sensory disturbances attributable to a sleeve-like epidural thoracic mass. The clinical, intraoperative, and pathological findings of this rare entity are reported. A search of the English literature via PubMed was conducted to find studies on spinal epidural atypical meningiomas.
2 Materials and Methods
The case of an epidural atypical spinal tumor was described through clinical and surgical reports from onset to 24 months after surgery. The main radiological and histopathological features are highlighted to make the case representative.
A search of studies in the English literature was conducted on PubMed to identify previous reports on spinal epidural atypical meningiomas. We used the following keywords alone or a combination of them: “atypical”; “grade II”; “epidural”; “extradural”; and “meningioma.”
3 Results
3.1 Case Report
In January 2020, a 24-year-old woman was admitted to the Neurosurgery of Fondazione Policlinico Agostino Gemelli IRCCS in Rome, Italy, with a 6-month history of dysesthesia and paresthesia in the lower limbs. Her symptoms had progressively exacerbated over time and eventually irradiated to the abdomen. A neurological examination upon admission revealed bilateral tactile hypoesthesia (5/10) and paresthesia below Th4. She presented with exaggerated knee and ankle reflexes, bilaterally. Her extensor plantar response and patellar clonus were elicited on the left side. Her motor function was preserved, as was her control of voluntary sphincters. Her medical history included only therapy with Aldactone for hirsutism related to polycystic ovary syndrome.
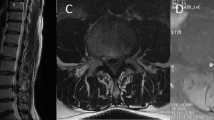
Magnetic resonance imaging (MRI) showed an expansive and infiltrating lesion in the extradural, subarachnoid space at Th4-Th5. The mass extended caudally for approximately 34 mm from the superior end plate of Th4 to the upper half of the Th5 vertebral body. The pathological tissue was located posteriorly with increased thickness on the right side, and it caused the segmental stenosis of the spinal canal, the obliteration of the perimedullary cerebrospinal fluid (CSF) spaces, spinal cord compression, and displacement to the left. On T2-weighted images, the spinal cord showed slight hyperintensity, possibly due to ischemic events. The pathological tissue appeared isointense on T1-weighted images and mildly hyperintense on T2-weighted images, with restricted proton motion on diffusion-weighted images (DWI) and a diffuse and homogenous contrast uptake. Following the injection of the contrast medium, the lesion had a sleeve-like appearance causing spinal cord compression. In addition, the lesion presented an initial extension toward the neural foramina, mainly in the right Th4-Th5 intervertebral foramen. There was no evidence of signal alterations on the adjacent skeletal segments consistent with bone swelling. The pathological tissue was not of unequivocal interpretation, and a lymphoproliferative disorder was included in the differential diagnosis. A coexisting myelopathic area was evident (Fig. 1a).
MRI imaging: (a) preoperative sagittal MRI with contrast showing the contrast-enhancing dorsal spinal epidural lesion; (b) preoperative axial MRI documenting the sleeve-like epidural lesion; (c, d) 2-year follow-up T1-weighted sagittal and axial postoperative MRI with contrast documenting recurrence-free dorsal spinal canal
Surgery was performed with intraoperative neurophysiological monitoring to assess the motor- and somatosensory-evoked potentials of the inferior limbs. Following the exposure of the Th4-Th5 laminae and joints, we performed a bilateral Th4 laminectomy by using the high-speed drill and the bone punches. The dura appeared covered by a gray-reddish, elastic, and hard tissue, tightly adherent to and infiltrating the right anterolateral dural sleeve and the emerging nerve root (Fig. 2).
The intraoperative frozen-section examination was suggestive of meningioma. During the delicate removal of the anterolateral component of the tumor, a sudden the reduction in the Motor Evoked Potentials (MEPs) and Somatosensory Evoked Potentials (SEPs) occurred, which was treated with the prompt intravenous injection of methylprednisolone, which helped maintain high arterial pressure and prevent ischemia. The corticospinal D wave exhibited a reduction in the amplitude caudal to the lesion. By that point, the dorsal and the lateral right intraforaminal Th4-Th5 portions of the extradural mass had been successfully and completed resected. Given the decreased neurophysiological pattern recorded during surgery and given that the frozen-section examination suggested meningioma, we decided to avoid any further cauterization on the sites of dural infiltration, in particular the ventrolateral side of the spinal cord. The decision was taken to avoid surgically manipulating the spinal cord, which would have been necessary for the excision of the tumoral component anterior to the dural sac.
In the immediate postoperative period, the patient exhibited proprioceptive disturbances and motor deficits on the right inferior limb (3/5), with worse proximal weakness. Sensory functions and sphincter control were not affected. Postoperative MRI confirmed the gross total resection of the tumor and the findings were negative for spinal canal compression (Fig. 1b). Nonetheless, small T2-hyperintense foci located between Th4 and Th5 persisted on the spinal cord. Compared to the preoperative MRI, the hyperintensity’s extension was substantially unmodified, and only minimal signs of swelling, ascribable to a myelopathic lesion, were present. On the fourth postoperative day, the patient was transferred to a rehabilitation clinic in good clinical condition and reported rapid neurological improvement.
4 Histopathology
Histological specimens consisted of meningothelial tumor fragments. The tumor cells were arranged in chords, nest and whorls (Fig. 3a). Scattered psammomatous bodies were present in the tumor tissue (Fig. 3a). The tumor did not show significant nuclear polymorphism nor areas with necrosis or diffuse growth pattern. However, mitotic activity was significantly high (up to 5 mitoses/10 high-power fields (HPFs)), granting the diagnosis of atypical meningioma (World Health Organization (WHO) grade II, WHO 2016). The tumor infiltrated the epidural tissue at its periphery (Fig. 3b). No infiltration of nervous tissue was found.
At the 3-month follow-up, she presented with complete neurologic recovery. Radiologic follow-ups at 6 and 12 months showed no recurrence of the disease. Spinal cord MRI at the 2-year follow-up showed no recurrence of the disease (Fig. 1c).
We methodically reviewed the English literature on spinal epidural atypical meningioma, and we found out that the occurrence of epidural atypical SMs (WHO grade II) was almost anecdotal. Only two cases have been previously reported (Table 1). Rutherford et al. [3] described the case of a 29-year-old man with exacerbating neuropathic pain, dysesthesia, and paresthesia in the coccygeal, buttock, and thigh regions due to a sacral epidural atypical meningioma. Despite the apparent complete resection, the patient presented with a recurrence of the original symptoms 9 months after surgery: the local recurrence of the meningioma was evident on MRI, extending through the S2 foramen into the presacral soft tissues. At 6 months after second surgery, local and systemic recurrence occurred with multiple pulmonary metastases, so the patient was referred to palliative chemotherapy.
Ben Nsir et al. [1] reported the case of a 70-year-old man who presented with lower-limb paresthesia, dysesthesia, and motor deficits, owing to an anterior lateral extradural lesion at the Th5 level revealed by the MRI. The patient underwent a posterolateral approach in emergency, and his histopathology revealed a diagnosis of epidural atypical meningioma. Despite the complete excision and cauterization of invasion sites, followed by adjuvant radiotherapy, local recurrence occurred 7 years after surgery. The patient presented with severe symptoms of spinal cord compression and MRI evidence of anterolateral progression of the tumor, which involved the soma of Th5 and extended into the posterior mediastinum. Thus, the patient was submitted to a second surgical removal of the recurrent lesion and was successively submitted to rehabilitation, following a good recovery. The scarce available literature on cases of epidural atypical meningioma made it hard to draw conclusions on the epidemiology, prognosis, and optimal management of this disease.
5 Discussion
Meningiomas represent the most common primary spinal tumor in adults, accounting for 39% of all tumors [4]. They are generally well-circumscribed lesions with broad-based dural attachments; the typical dural tail sign is clearly seen in 60–70% of the cases, and sometimes its relationships with the spinal cord and the denticulate ligament cause the so-called ginkgo leaf sign in those meningeal lesions arising laterally or ventrolaterally to the spinal cord [5].
Extradural meningiomas are rare entities, accounting for 2.5–3.5% of all spinal meningiomas and generally involving the thoracic and cervical spine [4, 6]. According to the review by Bettaswamy et al. [2]. Only seven cases of pure extradural spinal meningioma had been reported as of 2016. Due to the rarity of purely extradural meningiomas, these tumors can be misdiagnosed on radiological imaging as spinal metastases [7,8,9] even if radiological features, especially signal intensity on MRI, seem typical of meningiomas. Many authors have highlighted the value of intraoperative histology in adequate surgical management [1, 10].
Epidural meningiomas pose challenges for the surgeon not only because they can be misdiagnosed as other aggressive extramedullary malignancies but also because their surgical management is difficult. Extension over multiple spinal segments, adherence to nerve roots, and dural invasion have been reported in the vast majority of cases [6]. Pathologically, atypical SMs feature elevated mitotic activity (a mitotic index of at least 4 and 20 mitoses/10 HPFs), and/or for atypical SMs, three of the following five histological features are present: spontaneous necrosis, sheeting, prominent nucleoli, high cellularity, and/or small cells [11]. According to some authors SMs’ prognoses are unfavorable because of their invasiveness and vascularization [12,13,14,15]. The gross total resection of the tumor may be difficult to achieve because of bone involvement and/or paraspinal extension. Because of the difficulties in achieving the gross total removal of the tumors, the recurrence rate after surgery seems to be up to four times higher than that in cases of intradural meningiomas [16].
Several pathogenic theories exist: Most likely, epidural SMs arise from the arachnoid tissue lying around the periradicular nerve root sleeve, where spinal leptomeninges merge directly into the dura. As demonstrated by Savardekar et al. [10], this theory provides a rationale to resect the tumor by detaching it from the spinal dura, without needing to excise the dura itself.
These findings refer mostly to a series of WHO grade I epidural SMs, so their value on WHO grade II epidural spinal meningioma is questionable. Indeed, the available knowledge about grade II epidural SMs is very limited because of their rarity. Nevertheless, grade II SMs account for approximately 6% of SMs, mostly intradural lesions. A recent clinical series and literature review [17] focused on atypical meningiomas’ high recurrence risk, ranging from 15% to 61%. Among epidural spinal meningiomas, atypical lesions are very rare. The presented case is the first one diagnosed at our institution, which is a high-volume center for meningiomas in our country. Because of its rarity, it is not yet possible to draw significative conclusions on epidural atypical SMs as nosological entities, but several factors contribute to making them clinical, diagnostic, and surgical dilemmas: They can be preoperatively mistaken for secondary lesions; intraoperative management can be challenging because of the involvement of the surrounding tissues; and gross total resection should be advocated but can be associated with higher morbidity, causing functional deficits, as both in our case and the case described by Ben Nsir et al. [1]. The risk for recurrence seems to be high because of a combination of both their anatomical extension (which often prevents radical excision) and their grading. Furthermore, even without any histological evidence of malignancy, atypical meningioma can metastasize [1]. On the other hand, there’s no evidence that adjuvant radiotherapy is mandatory for the long-term control of the disease [18].
6 Conclusions
Epidural atypical spinal meningiomas are unique owing to a combination of factors. Apart from this case, just two other cases have been previously reported in literature, with relapses and the progression of the disease occurring in both. In our case, gross total resection was achieved, and no signs of local or distant recurrence were observed at the 24-month follow-up. Despite their rarity, epidural atypical meningiomas represent clinicopathological entities that deserve recognition. Further experience is needed to accurately define the prognosis and optimal management of this rare entity.
References
Ben Nsir A, Boughamoura M, Mahmoudi H, Kilani M, Hattab N. Uncommon progression of an extradural spinal meningioma. Case Rep Surg. 2014;2014:630876.
Bettaswamy G, Ambesh P, Das KK, Sahu R, Srivastava A, Mehrotra A, Behari S. Extradural spinal meningioma: revisiting a rare entity. J Craniovertebral Junction Spine. 2016;7(1):65.
Rutherford SA, Linton KM, Durnian JM, Cowie RA. Epidural meningioma of the sacral canal: case report. J Neurosurg Spine. 2006;4(1):71–4.
Pant I, Gautam VKS, Kumari R, Chaturvedi S. Spinal tumour: primary cervical extradural meningioma at an unusual location. J Spine Surg. 2017;3(3):509.
Yamaguchi S, Takeda M, Takahashi T, Yamahata H, Mitsuhara T, Niiro T, Kurisu K. Ginkgo leaf sign: a highly predictive imaging feature of spinal meningioma. J Neurosurg Spine. 2015;23(5):642–6.
Zhang LH, Yuan HS. Imaging appearances and pathologic characteristics of spinal epidural meningioma. Am J Neuroradiol. 2018;39(1):199–204.
Ito K, Imagama S, Ando K, Kobayashi K, Hida T, Tsushima M, Matsumoto A, Morozumi M, Tanaka S, Nishida Y, Ishiguro N. Discrimination between spinal extradural meningioma and both intra and extradural meningioma: case report. Nagoya J Med Sci. 2017;79(1):115–21.
Wu L, Yang T, Deng X, Yang C, Zhao L, Yao N, Xu Y. Spinal extradural en plaque meningiomas: clinical features and long-term outcomes of 12 cases. J Neurosurg Spine. 2014;21(6):892–8.
Zevgaridis D, Thomé C. Purely epidural spinal meningioma mimicking metastatic tumor: case report and review of the literature. Spine. 2002;27(18):E403–5.
Savardekar A, Chatterjee D, Chatterjee D, Dhandapani S, Mohindra S, Salunke P. Totally extradural spinal en plaque meningiomas–diagnostic dilemmas and treatment strategies. Surg Neurol Int. 2014;5(7):S291.
Louis DN, Perry A, Reifenberger G, Von Deimling A, Figarella-Branger D, Cavenee WK, Ellison DW. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. 2016;131(6):803–20.
Cohen-Gadol AA, Zikel OM, Koch CA, Scheithauer BW, Krauss WE. Spinal meningiomas in patients younger than 50 years of age: a 21-year experience. J Neurosurg. 2003;98(3):258–63.
Cramer P, Thomale UW, Okuducu AF, Lemke AJ, Stockhammer F, Woiciechowsky C. An atypical spinal meningioma with CSF metastasis: fatal progression despite aggressive treatment. Case report. J Neurosurg Spine. 2005;3:153–8.
Maiti TK, Bir SC, Patra DP, Kalakoti P, Guthikonda B, Nanda A. Spinal meningiomas: clinicoradiological factors predicting recurrence and functional outcome. Neurosurg Focus. 2016;41:E6.
Noh SH, Kim KH, Shin DA, et al. Treatment outcomes of 17 patients with atypical spinal meningioma, including 4 with metastases: a retrospective observational study. Spine J. 2018;19(2):276–84.
Klekamp J, Samii M. Surgical results for spinal meningiomas. Surg Neurol. 1999;52(6):552–62.
Han B, Zhang L, Jia W, Yang J. Clinical features and surgical outcomes of high-grade spinal meningiomas: report of 19 cases and literature review. J Clin Neurosci. 2020;72:264–9.
Sun SQ, Cai C, Ravindra VM, Gamble P, Yarbrough CK, Dacey RG, Ray WZ. Simpson grade I-III resection of spinal atypical (World Health Organization Grade II) meningiomas is associated with symptom resolution and low recurrence. Neurosurgery. 2015;76(6):739–46.
Conflicts of Interest
The authors whose names are listed certify that they have no affiliations with or involvement in any organization or entity with any financial interest or nonfinancial interest in the subject matter or materials discussed in this manuscript.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
di Bonaventura, R. et al. (2023). Spinal Epidural Atypical Meningioma: Case Report and Review of the Literature. In: Visocchi, M. (eds) The Funnel: From the Skull Base to the Sacrum. Acta Neurochirurgica Supplement, vol 135. Springer, Cham. https://doi.org/10.1007/978-3-031-36084-8_56
Download citation
DOI: https://doi.org/10.1007/978-3-031-36084-8_56
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-36083-1
Online ISBN: 978-3-031-36084-8
eBook Packages: MedicineMedicine (R0)