Abstract
Posterior atlantoaxial screw fixation is a widely adopted therapeutic option for C1-C2 instability secondary to fractures or dislocation, degenerative diseases, or tumors at this level. Anterior transarticular screw fixation (ATSF) is an effective alternative to the posterior approaches, presenting several advantages despite being scarcely known and rarely chosen.
In this chapter, we describe the ATSF step by step, illustrating its variations reported in literature, and we critically analyze the several advantages and contraindications of this technique. Moreover, we provide a list of tips and tricks on the surgical procedure, including critical operating room settings—the result of more than 10 years of experience in the field by a senior author.
ATSF is a valid strategy for the treatment of different diseases occurring at the level of the atlantoaxial complex that needs consideration. Given the significant learning curve of this strategy, some hints may be essential to begin introducing this technique in the personal armamentarium of a spine surgeon so that they can perform ATSF safely and effectively.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Atlantoaxial anterior transarticular fixation
- Anterior transarticular screw fixation
- ATSF
- Atlantoaxial instability
1 Introduction
The atlas and the axis represent a unique anatomic and functional segment of the spine.
The complex anatomy of this joint, thanks to its osseous and ligamentous structures, allows the major part of the rotation of the head [1].
Trauma, tumors, and degenerative diseases may cause atlantoaxial instability by lesioning the integrity of bones (C2 dens, rings, or lateral masses of the atlas) or ligaments (transverses or alars). The closed relationship between eloquent anatomical structures, the spinal cord, and vertebral arteries makes the surgical treatments on this segment challenging for every surgeon.
Among the surgical techniques described to treat atlantoaxial instability, the anterior transarticular screw fixation (ATSF) is probably the least known and performed.
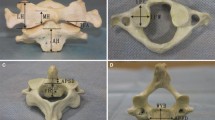
The technique was originally described by Lu on a cadaver [2] (Fig. 1a) and by Reindl on a patient [3]; it has since been modified by Koller in 2006 (Fig. 1b) [4] and later described in multiple cases and technical variations [5,6,7]. The technical difficulty, the inability to decompress neural structures, and the lack of knowledge among most surgeons are the main reasons for the rare choice of this peculiar technique.
Antero-posterior view of classical anterior transarticular screw fixation entry points and the screw’s direction (partially threaded malleolar screws): (a) Lu’s entry point, described in vivo by Reindl, at the lateral edge of the medial third of the C2 articular joint lip; (b) Koller’s technique, with the entry point at the pinafore of the C2 vertebral body
This chapter aims to highlight the advantages and limitations of ATSF, describing technical critical points learned on over a decade of experience with this technique.
2 Discussion
2.1 Indications
Why should we choose this technique over the well-known posterior Goel–Harms one[8, 9]?
First of all, the supine position is safer. The dens tend to adhere to the anterior ring of the atlas in the case of transverse ligament disruption, reducing the risk of cord compression. It is also safer in patients with multiple fractures and in those with cardiorespiratory pathologies [10,11,12].
Compared to cervical posterior approaches, ATSF, as all procedures performed by taking a retropharyngeal approach, implicates no muscle trauma, reducing postoperative pain and hospitalization. It also reduces blood loss, avoiding the surgical exposure and management of the C2 periradicular venous plexus, and reduces the risk of delayed kyphosis secondary to C2 posterior scarification.
2.2 Contraindications
2.2.1 Fixed Rotatory C1-C2 Luxation
Because ATSF is a fluoroscopy-guided procedure, proceed only in the case of having a good visualization of C1-C2 bone limits, especially in the Anterior/Posterior (AP) view. A preoperative open-mouth X-ray can help identify patients without having a clear view, such as those with metal alloys used in dental crowns or with limitations in opening their mouths.
In the case of basilar invagination (BI), the technique of choice should be the posterior one. The distance between the skin incision and the working area is excessive, making the surgical field too deep to also comfortably manage retractors and surgical movements. Furthermore, the X-ray open-mouth AP and lateral views in BI may be confusing for the superimposition of the lateral masses of C1 on occipital and mastoid bones.
Performing ATSF in patients with high-riding vertebral arteries in C2 may expose them to serous risk of vascular damage or stroke. However, this is a relative contraindication because in the technique introduced by Koeller (Fig. 1b), the K-wire and the screws follow a trajectory medial to high in comparison to vertebral artery grooves in C2.
Although some authors have described ways to decompress the spinal cord by taking a retropharyngeal approach at the C1-C2 level, patients requiring decompression should undergo the posterior approach.
3 Step-by-Step Technical Description
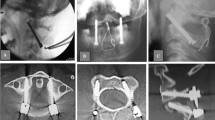
The patient is placed supine on a radiolucent table. The fluoroscopy AP view keeps the mouth open with specific radiolucent distractors or, thinking out of the box, with anything else could do the job, such as shaped corks or gauzes when the patient is toothless (Fig. 2).
Operating room setting with Medtronic O-Arm2 used as a C-arm fluoroscopy with mechanic automatic rotation; a gauzes’s roll was used as a radiolucent open-mouth dilator (no teeth available for the cork); AP and lateral views can be seen on the screen with a good visualization of the C1 lateral masses and their anatomical relationships
The proper visualization of C1 lateral masses should be checked before fixing the head. Contrary to what we believed necessary at the beginning of our experience with this surgical technique [5], there is no need to fix the head to a radiolucent Mayfield head holder (a very expensive tool not available in every spine center). It is sufficient to tape the head to the table in the desired position.
The procedure is started with a classic Smith–Robinson retropharyngeal approach centered to C4-C5 in order to set up the best trajectory, which is a little divergent from the anterior longitudinal ligament. Once the anterior longitudinal ligament has been exposed, the retropharyngeal space is cranially opened up to the anterior tubercle of C1. The pharynx should be retracted with blunt long retractors by a second surgeon in order to reduce postoperative dysphagia. Once the radiological level has been checked, surgery proceeds depending on the technique chosen.
In Lu’s technique (Fig. 1a), a progressive scarification of the anterior surface of C2 has to be performed in a medial to lateral direction in order to expose at least the medial third of the C1-C2 joints. At this point, the entry level of the K-wire should be identified both radiologically and macroscopically, consisting of a point on the undersurface of the overhanging lip of the lateral mass of C2, 4–5 mm lateral to the base of the odontoid process[2, 3].
Concerning the trajectory, it could be necessary to partially drill the anterior surface of the C2 promontorium in order to gain the correct inclination with the K-wire guide instrument. We believe that the description of the trajectory with craniocaudal and mediolateral angles is useless or misleading. Because this is not a lab procedure but rather a fluoroscopy-guided technique, the trajectory of the K-wire and the length of the screw should be determined on each side according to the bony structure displayed on the screen. The target areas for the K-wire are the superolateral margin of the C1 lateral mass in the AP view, without passing the lateral or superior cortical rims where the vertebral artery is and C0-C1 articulation trauma can occur, and the posterior third of the C1 lateral mass in the lateral view, aiming to avoid passing beyond the posterior cortical rim, where the ipsilateral vertebral artery usually runs.
In the Koeller technique (Fig. 1b), the K-wire and screw entry point lies underneath the pinafore of C2, increasing the screw purchase in the bone of the C2 promontory and improving the stability of the construct. Therefore, the time-consuming and uncomfortable scarification of C1-C2 joint is not needed if joint scarification for fusion is not mandatory.
In Koller’s technique, as well as in dens screwing, the anterior surface of C3 vertebral body and that of the C2-C3 disc need to be drilled away in order to reach the correct angle in the sagittal plane.
Even though ATSF can achieve a solid fixation [13, 14], fusion at this site should be the final target. In the case of traumatic disruption of the C1-C2 articular surfaces or in the case of unilateral degenerative osteoarthritis, fusion can be expected to appear without the need for bone scarification and fusion promotion. In all other cases, the scarification of the articular processes and the injection of bone paste inside the joint could be achieved (not easily) with long curved curettes. ATSF is performed with a standard Smith–Robinson approach, so no blood loss or pain is expected, but mild dysphagia and early discharge are expected. Given the aforementioned bone fusion issue, a temporary cervical collar should be prescribed in the case of high preoperative instability, uncertain bone quality, or screw purchase.
4 Tips and Tricks
-
Always preoperatively check the AP visualization of the lateral masses with an open-mouth X-ray.
-
An intraoperative fluoroscopic clear view is mandatory for the safety of this procedure. Given that precise AP and lateral positions of the fluoroscopy are needed in each step of the K-wire and then of the screw introduction, our advice is to use two fluoroscopic C-arms, or one C-arm with automatic rotation with displayed degrees (an O-arm, Medtronic, Minneapolis, MN, USA could be used this way; see Fig. 2), or find an expert fluoroscopy technician.
-
Use very long and narrow blunt handheld retractors to retract the pharynx.
-
A short neck and a prominent chest could limit instrument usability. Therefore, choose a surgical system with an angulated K-wire holder/guide and cardanic screw drivers, keeping available the malleolar screws’ system for specific further instruments (e.g., cannulated drill and rescue screws).
-
The AP and LL angulations should be well evaluated at the beginning of the K-wire introduction because this procedure often does not allow small variations in direction after the wire is in the bone. Excessive angle variations during K-wire introduction may result in its breakage inside the bone. In this case, a dedicated cannulated drill bit can be helpful to loosen the wire from the surrounding bone and then pull it out after grabbing its caudal extremity.
-
A critical point in Lu’s technique is that the K-wire entry point should be at the lateral border of the medial third of the C2 joint, paying attention to being deep enough to leave sufficient bone on the cortical lip of C2 after the screw introduction, to avoid cortical bone damage and screw loosening (Fig. 3).
-
A critical point in Koller’s technique is that the normal anatomy of the anterior surface of the axis seldomly permits enough space for two divergent screws. The risk is that an in-out-in trajectory may cause the malpositioning of the K-wire or of the screw (Fig. 4). Moreover, once a screw is in place, there is no sufficient bone volume to extract and reposition one or two screws, eventually leading to difficult and extreme surgical solutions (Fig. 5).
Multiplanar-reconstructed CT: axial image of a patient submitted to ATSF with Koller’s technique, where in this case, the space for the ipsilateral screw was too narrow to be placed side by side with the contralateral, so a modification of the technique was carried out with the two screws crossing inside the C2-body
5 Conclusions
Anterior atlantoaxial screw fixation is a complex surgical technique with a steep learning curve, but it allows for achieving the solid stabilization of this segment with a minimally invasive technique. Every spine surgeon dealing with craniocervical junction instability should have it in their surgical armamentarium, being aware of all the pros and cons of this special technique.
References
Steinmetz MP, Mroz TE, Benzel EC. Craniovertebral junction: biomechanical considerations. Neurosurgery. 2010;66(3 Suppl):7–12. https://doi.org/10.1227/01.NEU.0000366109.85796.42. PMID: 20173531.
Lu J, Ebraheim NA, Yang H, Heck BE, Yeasting RA. Anatomic considerations of anterior transarticular screw fixation for atlantoaxial instability. Spine. 1998;23:1229–35; discussion 1236.
Reindl R, Sen M, Aebi M. Anterior instrumentation for traumatic C1-C2 instability. Spine. 2003;28:E329–33.
Koller H, Kammermeier V, Ulbricht D, Assuncao A, Karolus S, van den Berg B, et al. Anterior retropharyngeal fixation C1-2 for stabilization of atlantoaxial instabilities: study of feasibility, technical description and preliminary results. Eur Spine J. 2006;15:1326–38.
Polli FM, Miscusi M, Forcato S, Raco A. Atlantoaxial anterior transarticular screw fixation: a case series and reappraisal of the technique. Spine J. 2015;15(1):185–93. https://doi.org/10.1016/j.spinee.2014.09.019. Epub 2014 Sep 26. PMID: 25264177.
Ricciardi L, Sturiale CL, Izzo A, Pucci R, Valentini V, Montano N, Polli FM, Visocchi M, Vivas-Buitrago T, Chaichana KL, Quinones-Hinojosa A, Olivi A, Chen S. Submandibular approach for single-stage craniovertebral junction ventral decompression and stabilization: a preliminary cadaveric study of technical feasibility. World Neurosurg. 2019;127:206–12. https://doi.org/10.1016/j.wneu.2019.04.038. Epub 2019 Apr 10. PMID: 30980973.
Gembruch O, Ahmadipour Y, Lemonas E, Müller O. The anterior transarticular fixation of C1/C2 in the elderly with dens fractures. Int J Spine Surg. 2020;14(2):162–9. https://doi.org/10.14444/7031. PMID: 32355621; PMCID: PMC7188103.
Goel A, Laheri V. Plate and screw fixation for atlanto-axial subluxation. Acta Neurochir (Wien). 1994;129:47–53.
Harms J, Melcher RP. Posterior C1-C2 fusion with polyaxial screw and rod fixation. Spine. 2001;26:2467–71.
Kaneko K, Milic-Emily J, Dolovich MB, et al. Regional distribution of ventilation and perfusion as a function of body position. J Appl Physiol. 1966;21:767–77.
Stone JG, Khambatta HJ. Pulmonary shunts in the prone position. Anaesthesia. 1978;33:512–7.
Palmon SC, Kirsch JR, Depper JA, et al. The effect of the prone position on pulmonary mechanics is frame-dependent. Anesth Analg. 1998;87:1175–80.
Sen MK, Steffen T, Beckman L, Tsantrizos A, Reindl R, Aebi M. Atlantoaxial fusion using anterior transarticular screw fixation of C1-C2: technical innovation and biomechanical study. Eur Spine J. 2005;14:512–8.
Lapsiwala SB, Anderson PA, Oza A, Resnick DK. Biomechanical comparison of four C1 to C2 rigid fixative techniques: anterior transarticular, posterior transarticular, C1 to C2 pedicle, and C1 to C2 intralaminar screws. Neurosurgery. 2006;58:516–21; discussion 516–21.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Ethics declarations
The authors declare no conflicts of interest concerning the materials or methods used in this study or the findings specified in this chapter.
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Polli, F.M. et al. (2023). Atlantoaxial Anterior Transarticular Screw Fixation: Indications and Surgical Technique. In: Visocchi, M. (eds) The Funnel: From the Skull Base to the Sacrum. Acta Neurochirurgica Supplement, vol 135. Springer, Cham. https://doi.org/10.1007/978-3-031-36084-8_42
Download citation
DOI: https://doi.org/10.1007/978-3-031-36084-8_42
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-36083-1
Online ISBN: 978-3-031-36084-8
eBook Packages: MedicineMedicine (R0)