Abstract
Spontaneous intracranial hypotension (SIH) is a disorder of low cerebrospinal fluid (CSF) volume secondary to CSF leakage through a dural defect along the neuraxis with an estimated incidence of 5 people per 100,000.
Great debate persists on the optimal treatment of this pathology, and clinical results are often contradictory. SIH may be initially approached via conservative measures, such as bed rest that is often supplemented with hydration, caffeine, and theophylline, which overall relieve symptoms in a small subset of patients at 6 months. Epidural blood patching (EBP) is generally the next consideration in symptom management. It is the most commonly performed intervention for spinal CSF leaks, as the first option or following the failure of conservative treatment. Further procedures may be performed in the case of EBP partial or temporary response and if the spinal CSF leak has been definitively localized (Beck et al., Neurology 87:1220–26, 2016). In those cases, if the CSF leak is well localized, the surgical closure of the spinal CSF leak may be considered.
SIH is a complex but treatable CSF disorder. Despite recent advances in the field of neuroimaging and the different therapeutic options available, the appropriate management remains controversial and should be tailored to the patient.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Spontaneous intracranial hypotension (SIH) is a disorder of low cerebrospinal fluid (CSF) volume secondary to CSF leakage through a dural defect along the neuraxis [1, 2]. The estimated incidence of SIH is 5 people per 100,000 [3], but the true incidence is expected to be higher because it is frequently misdiagnosed initially.
Patients usually present with bilateral subdural hygromas or subdural hematomas (SDHs) and orthostatic headache, which generally starts within 15 min of assuming an upright position, predominantly in the back of the head. This can be explained by the sagging of the brain secondary to the low CSF volume and the resulting tension on the cranial nerves and dura mater, which is especially tension sensitive in the posterior fossa [4]. Other symptoms may include nausea, vomiting, disorientation, memory impairment, diplopia, gait disturbance, cranial nerve palsies, sinus thrombosis, large-vessel strokes, and comas [5,6,7,8,9]. Auditory disturbances such as ringing in the ears, or tinnitus—a pressure sensation in the ear—can seldom coexist, and some patients are initially treated for sudden hearing loss or suspected Ménière disease [10].
Neuroimaging techniques need to be directed toward the brain, to assess the consequences of CSF hypotension, and toward the spinal column, to localize the leakage and possibly guide diagnosis if a targeted treatment is pursued. The best tool to diagnose SIH is magnetic resonance imaging (MRI), which usually shows the triad of diffuse dural thickening/enhancement, the downward displacement of the brain (“slumping” midbrain), and subdural hematomas or hygromas [11,12,13].
Great debate persists on the optimal treatment of this pathology, and clinical results are often contradictory.
Our group recently performed a systematic review and meta-analysis of the literature to evaluate the role of different factors that possibly affect the efficacy of the EBP procedure, by analyzing comparative studies reporting a clear description of patients experiencing good and poor responses to EBP [14].
2 Pathogenesis
SIH is caused by spontaneous CSF leaks from the spinal meningeal diverticula or dural rents along nerve sleeves [15]. Mechanical factors and several connective tissue disorders, such as Marfan syndrome, Ehlers-Danlos syndrome type 2, and autosomal dominant polycystic kidney disease, can determine dural weakness, leading to one or more CSF leaks. Ventral dural tears by disk herniation and CSF–venous fistulas are other possible underlying etiologies.
According to the Monro–Kellie doctrine, the loss of volume secondary to CSF leaks increases blood volume, ultimately leading to the enlargement of dural arteries, the dilatation of cortical/medullary veins, and the dilatation of dural venous sinuses.
Conversely, the neurophysiological hypothesis arises from observing an abnormally low spinal epidural pressure in patients affected by SIH. This would act as an aspiration force applied to the entire dural surface, thus determining a CSF transdural “steal” in predisposed patients, such as those with connective disorders.
3 Diagnosis
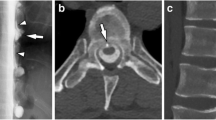
Diagnostic criteria include a CSF pressure < 60 mm H2O and/or radiological evidence of a CSF leak [2]. However, only one-third of SIH patients have low CSF opening pressure; moreover, lumbar puncture is an invasive procedure. Therefore, performing MRIs on the head and the spine is mandatory [16]. Myelography with iodinated contrast followed by the thin-cut computed tomography (CT) of the entire spine (or with gadolinium followed by MRI) has been shown to be the study of choice to accurately define the location and extent of a CSF leak when it is required. The majority of CSF leaks are at the cervicothoracic junction or along the thoracic spine. Multiple simultaneous CSF leaks can coexist.
4 Therapeutic Options
SIH may be initially approached via conservative measures, such as bed rest often supplemented with hydration, caffeine, and theophylline [17], which overall relieve symptoms in a small subset of patients at 6 months [18].
Epidural blood patching (EBP) is generally the next consideration in management. It is the most commonly performed intervention for spinal CSF leaks, as the first option or following a failure of conservative treatment [9, 19]. EBP consists of the injection of a variable volume of autologous blood in the epidural space (ranging from 10 to 55 mL) [20, 21], where the patient lies supine in the postprocedural setting to help with epidural blood redistribution along the neuraxis.
There is no consensus on how to perform a blood patch (“loss of resistance,” fluoroscopy guided, CT guided, blood, or fibrin glue). Controversy exists regarding the optimal site of EBP delivery, which can be targeted to the site of the CSF leak on imaging when aiming to seal it, or it can be blindly delivered into the lumbar region, thus raising the pressure in the epidural space. To date, no prospective randomized trials have demonstrated the superiority of one technique over the other. IN more detail, Yoon et al. and Choi et al. [22, 23] compared the results of blind and targeted EBP in responders and nonresponders: however, significant differences between the two groups have not been demonstrated. Some other authors have reported better results following targeted EBP when comparing results with those of nontargeted patching [23, 24], but this finding was not confirmed by our recently performed meta-analysis on this topic. Apart from the chosen technique, the ideal volume of injected blood is still a matter of debate. Higher volumes are correlated with better therapeutic outcomes [21].
The response rate to initial EBP significantly varies among investigations, ranging from 36% to 90% [5, 9, 25]. A patient is generally defined as a good responder if a persistent reduction in a VAS score of at least 50% for at least 6 months is achieved within 48 hours of the EBP [20].
Further procedures may be performed in the case of a partial or temporary response to EBP and if the spinal CSF leak has been definitively localized [26]. In those cases, if the CSF leak is well localized, the surgical closure of the spinal CSF leak may be considered. Surgical procedures may include clipping the leaking root sleeve (for leaks associated with nerve root sleeve diverticula), epidural packing, or primary dural repair, which may prove technically challenging if the leak is ventrally located [10].
Lateral meningeal diverticulae at the nerve root, CSF–venous fistulas, and laterally and ventrally located dural tears can be reached through a dorsal approach and closed safely and with minimal invasiveness through an interlaminar fenestration or a hemilaminectomy [10, 26]. Ventral dural tears require a transdural approach that detaches the denticulate ligaments so that the spinal cord can be mobilized under intraoperative neuromonitoring.
A therapeutic algorithm is schematized in Fig. 1.
5 Conclusion
SIH is a complex but treatable CSF disorder. Despite recent advances in the field of neuroimaging and the various therapeutic options available, the most-appropriate management remains controversial and should be tailored to the patient.
References
Schievink WI, Meyer FB, Atkinson JLD, Mokri B. Spontaneous spinal cerebrospinal fluid leaks and intracranial hypotension. J Neurosurg. 1996;84:598–605.
Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders. Cephalalgia. 2018;38:1–211.
Kranz PG, Gray L, Amrhein TJ. Spontaneous intracranial hypotension: 10 myths and misperceptions. Headache. 2018;58(7):948–59. https://doi.org/10.1111/head.13328. Epub 2018 May 24.
Schievink WI. Misdiagnosis of spontaneous intracranial hypotension. Arch Neurol. 2003;60:1713–8.
Ferrante E, Savino A, Sances G, Nappi G. Spontaneous intracranial hypotension syndrome: report of twelve cases. Headache. 2004;44:615–22.
Loya JJ, Mindea SA, Yu H, Venkatasubramanian C, Chang SD, Burns TC. Intracranial hypotension producing reversible coma: a systematic review, including three new cases. J Neurosurg. 2012;117(3):615–28. https://doi.org/10.3171/2012.4.JNS112030.
Nowak DA, Rodiek SO, Zinner J, Guhlmann A, Topka H. Broadening the clinical spectrum: unusual presentation of spontaneous cerebrospinal fluid hypovolemia. Case report. J Neurosurg. 2003;98:903–7.
Pakiam AS, Lee C, Lang AE. Intracranial hypotension with parkinsonism, ataxia, and bulbar weakness. Arch Neurol. 1999;56:869–72.
Paldino M, Mogilner AY, Tenner MS. Intracranial hypotension syndrome: a comprehensive review. Neurosurg Focus. 2003;15(6):1. ECP2 Published 2003 Dec 15.
Luetzen N, Dovi-Akue P, Fung C, Beck J, Urbach H. Spontaneous intracranial hypotension: diagnostic and therapeutic workup. Neuroradiology. 2021;63(11):1765–72. https://doi.org/10.1007/s00234-021-02766-z. Epub 2021 Jul 23. PMID: 34297176; PMCID: PMC8528761.
Atkinson JL, Weinshenker BG, Miller GM, et al. Acquired Chiari I malformation secondary to spontaneous spinal cerebrospinal fluid leakage and chronic intracranial hypotension syndrome in seven cases. J Neurosurg. 1998;88:237–42.
Chiapparini L, Ciceri E, Nappini S, Castellani MR, Mea E, LeoneM B, Savoiardo M. Headache and intracranial hypotension: neuroradiological findings. Neurol Sci. 2004;25(Suppl 3):S138–41.
Schick U, Musahl C, Papke K. Diagnostics and treatment of spontaneous intracranial hypotension. Minim Invasive Neurosurg. 2010;53:15–20.
Signorelli F, Caccavella VM, Giordano M, Ioannoni E, Caricato A, Polli FM, Olivi A, Montano N. A systematic review and meta-analysis of factors affecting the outcome of the epidural blood patching in spontaneous intracranial hypotension. Neurosurg Rev. 2021;44(6):3079–85.
Hyun SH, Lee KH, Lee SJ, Cho YS, Lee EJ, Choi JY, Kim BT. Potential value of radionuclide cisternography in diagnosis and management planning of spontaneous intracranial hypotension. Clin Neurol Neurosurg. 2008;110(7):657–61. https://doi.org/10.1016/j.clineuro.2008.03.014. Epub 2008 May 23. PMID: 18457913..
Kranz PG, Tanpitukpongse TP, Choudhury KR, Amrhein TJ, Gray L. How common is normal cerebrospinal fluid pressure in spontaneous intracranial hypotension? Cephalalgia. 2016;36:1209–17.
Kong DS, Park K, Nam DH, Lee JI, Kim JS, Eoh W, Kim JH. Clinical features and long-term results of spontaneous intracranial hypotension. Neurosurgery. 2005;57:91–6.
Davidson B, Nassiri F, Mansouri A, Badhiwala JH, Witiw CD, Shamji MF, Peng PW, Farb RI, Bernstein M. Spontaneous intracranial hypotension: a review and introduction of an algorithm for management. World Neurosurg. 2017;101:343–9.
Kranz PG, Gray L, Malinzak MD, Amrhein TJ. Spontaneous intracranial hypotension: pathogenesis, diagnosis, and treatment. Neuroimaging Clin N Am. 2019;29(4):581–94.
Levi V, Di Laurenzio NE, Franzini A, et al. Lumbar epidural blood patch: effectiveness on orthostatic headache and MRI predictive factors in 101 consecutive patients affected by spontaneous intracranial hypotension. J Neurosurg. 2019;8:1–9.
Wu JW, Hseu SS, Fuh JL, Lirng JF, Wang YF, ChenWT CSP, Wang SJ. Factors predicting response to the first epidural blood patch in spontaneous intracranial hypotension. Brain. 2017;140(2):344–52.
Yoon SH, Chung YS, Yoon BW, Kim JE, Paek SH, Kim DG. Clinical experiences with spontaneous intracranial hypotension: a proposal of a diagnostic approach and treatment. Clin Neurol Neurosurg. 2011;113(5):373–9.
Choi H, Lee MJ, Choi HA, Cha J, Chung CS. Intracranial structural alteration predicts treatment outcome in patients with spontaneous intracranial hypotension. Cephalalgia. 2018;38(2):323–31.
Cho KI, Moon HS, Jeon HJ, Park K, Kong DS. Spontaneous intracranial hypotension: efficacy of radiologic targeting vs blind blood patch. Neurology. 2011;76:1139–44.
Sencakova D, Mokri B, McClelland RL. The efficacy of epidural blood patch in spontaneous CSF leaks. Neurology. 2001;57(10):1921–3.
Beck J, Ulrich CT, Fung C, Fichtner J, Seidel K, Fiechter M, Hsieh K, Murek M, Bervini D, Meier N, Mono ML, Mordasini P, Hewer E, Z’Graggen WJ, Gralla J, Raabe A. Diskogenic microspurs as a major cause of intractable spontaneous intracranial hypotension. Neurology. 2016;87:1220–6.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Signorelli, F., Visocchi, M. (2023). Spontaneous Intracranial Hypotension: Controversies in Treatment. In: Visocchi, M. (eds) The Funnel: From the Skull Base to the Sacrum. Acta Neurochirurgica Supplement, vol 135. Springer, Cham. https://doi.org/10.1007/978-3-031-36084-8_32
Download citation
DOI: https://doi.org/10.1007/978-3-031-36084-8_32
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-36083-1
Online ISBN: 978-3-031-36084-8
eBook Packages: MedicineMedicine (R0)