Abstract
An increase in the arousal threshold may predispose critically ill patients with obstructive sleep apnea (OSA) to prolonged apneas and death. In one early study, impaired arousal was hypothesized to have led to prolonged apneas, electroencephalogram (EEG) flattening, and generalized tonic spasms described as “cerebral anoxic attacks” [1]. We present two critically ill patients with OSA, in whom elevated arousal thresholds may have prolonged obstructions, leading to diffuse cerebral hypoxemic EEGs patterns, followed by transient encephalopathy in one subject and death in the other (Figs. 1, 2, and 3; Video 1) [2, 3].
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Obstructive sleep apnea
- Polysomnogram
- Bi-level positive airway pressure therapy
- Cerebral hypoxemia
- Encephalopathic
- Cardiac arrest
- Hypercapnia
- Arousal threshold
- Continuous positive airway pressure therapy
An increase in the arousal threshold may predispose critically ill patients with obstructive sleep apnea (OSA) to prolonged apneas and death. In one early study, impaired arousal was hypothesized to have led to prolonged apneas, electroencephalogram (EEG) flattening, and generalized tonic spasms described as “cerebral anoxic attacks” [1]. We present two critically ill patients with OSA, in whom elevated arousal thresholds may have prolonged obstructions, leading to diffuse cerebral hypoxemic EEGs patterns, followed by transient encephalopathy in one subject and death in the other (Figs. 1, 2, and 3; Video 1) [2, 3].
The patient described in Case 1 suffered a prolonged 90-s obstructive apnea, during which the EEG revealed a sudden change from a classic REM sawtooth pattern (see arrow) to a poorly organized, diffuse delta slow-wave pattern (see closed circle) followed by a general flattening of all activity (see square) that led to attempts to arouse the patient (as evidenced by diffuse movement artifact; see diamond). Nevertheless, persistent obstruction (see triangle) necessitated emergent rescue breathing maneuvers. Persistent EEG flattening followed by slowing and eventual recovery of normal waking patterns was appreciated in subsequent epochs. L left, R right, T temporal, C central, O occipital, CHIN mentalis EMG, L LEG left anterior tibialis EMG, R LEG right anterior tibialis EMG, SNORE snoring microphone, Airflow nasal airflow, CHEST thoracic respiratory effort, ABDOMEN abdominal respiratory effort, SaO2 (%) oxygen saturation. (From Dyken et al. [2]; with permission)
The subject described in Case 2 had a 30-s obstruction that was associated with a SaO2 low of 12%. At that time there was a dramatic change from the preceding stage N3 PSG pattern, with an EEG that showed progressive development of a disorganized, delta/theta slow-wave pattern over a 2.5 min period. LOC left outer canthus, ROC right outer canthus, A1 left ear reference, A2 right ear reference, T temporal, C central, O occipital, EMG electromyogram, LL left leg, RL right leg, NA nasal airflow, CE chest effort, AE abdominal effort, SaO2 oxygen saturation. (From Dyken et al. [3]; with permission)
Following the subject in Case 2’s final series of apneic events, no discernible EEG activity was captured while using a recording sensitivity of 1.0 μV/mm. A prolonged period of asystole (arrow) was followed by cardiac arrest, at which time the patient was declared dead (closed circle). LOC left outer canthus, ROC right outer canthus, A1 left ear reference, A2 right ear reference, T temporal, C central, O occipital, LL left leg, RL right leg, NA nasal airflow, CE chest effort, AE abdominal effort, SaO2 oxygen saturation. (From Dyken et al. [2]; with permission)
1 Case 1
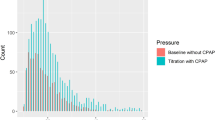
A 52-year-old man, with a history of OSA, pulmonary hypertension, diabetes, and myocardial infarction was admitted to the hospital for a coronary artery bypass. A polysomnogram (PSG) with a bi-level-positive airway pressure (bi-level-PAP) titration was requested as he had persistent snoring with gasping arousals, sleepiness, and morning headaches. During rapid-eye-movement (REM) sleep, there was a 90-s obstructive apnea, with a minimum oxygen saturation (SaO2) level of 31%, followed by diffuse EEG slowing (not compatible with the patient’s normal slow wave pattern of stage N3 [non-rapid eye movement, NREM 3] sleep) suggesting cerebral hypoxemia (Fig. 1 and Video 1). This apnea persisted despite increasing bi-level-PAP to 15/10 centimeters of water pressure (CWP), loud commands, shaking, and sternal rub. After 30-s of unresponsiveness, the initial EEG slowing was immediately followed by a 45-s period of flat/absent EEG activity (using a recording sensitivity of 7 μv/mm). At this time, emergency rescue breathing was initiated, after which he resumed his normal waking breathing pattern and opened his eyes. Within 30-s he responded in a slow/encephalopathic manner and after 19 s his baseline cognitive functioning returned. During this time there was a progressive build-up of diffuse theta slow wave activity that was followed by a mixture of minimal theta with interspersed occipital alpha rhythm. Following full arousal, it took 45-s for the normal baseline EEG to return. Later, bi-level-PAP at 29/25 CWP resolved all obstructions and the patient reported better sleep than usual.
2 Case 2
An 80-year-old man with Alzheimer’s disease was admitted with an exacerbation of severe chronic obstructive pulmonary disease and congestive heart failure with atrial fibrillation/flutter, under a do-not-resuscitate/do-not-intubate status. His wife gave written consent for a portable PSG to be performed as part of an IRB approved research study, with the understanding that no heroic measures to sustain life were to be instituted, including the use of PAP devices. He had significant OSA with a respiratory disturbance index of 37 events per hour, a minimum SaO2 value (prior to his final series of apneic events) of 80%, with a baseline SaO2 of 96–98%. Following a 30-s obstructive apnea during stage N3 sleep, while the SaO2 decreased to 12%, the EEG assumed an irregular, disorganized, delta slow-wave pattern for 150 s, followed by electrocerebral silence when using a recording sensitivity of 1.0 μv/mm (Figs. 2 and 3). No discernible EEG activity was appreciated despite noxious stimulation. This obstruction preceded a mixture of obstructive and new-onset central apneas that were followed by complete respiratory arrest. Simultaneously, the heart rate decreased from 148 beats per minutes (bpm) to 40 bpm. Subsequently, 29 min of relative bradycardia (defined as a heart rate < 60 bpm) was followed by cardiac arrest (Fig. 3).
3 Discussion
A sleep apneic event typically ends with an arousal or “micro-arousal” (of which the patient is usually not aware) [4]. This is an important protective reflex that allows relief of the upper airway obstruction, with an increase in tidal volume and respiratory frequency, without which it is unlikely that the apnea would terminate.
During apnea several stimuli can induce arousal, including hypercapnia, hypoxia and increased airway resistance. Arousal to CO2 is mediated by serotonin neurons in the raphe nuclei of the brainstem, probably in the midbrain, which are in close association with large branches of the basilar artery [5,6,7]. They sense variations in arterial PCO2, responding indirectly to changes in intracellular pH by increasing their excitatory drive to other neurons that mediate arousal, possibly including those in the hypothalamus, thalamus, and cortex [5]. Genetic deletion of 5-HT neurons leads to profound loss of hypercapnic arousal. At the same time, serotonin neurons next to large arteries in the medulla sense arterial PCO2 using the same mechanisms, but project to and stimulate respiratory neurons to increase ventilation [5, 8, 9].
Hypoxia alone can induce arousal without hypercapnia [10]. Reductions in arterial PO2 are sensed by the peripheral arterial chemoreceptors in the carotid and aortic bodies. Afferent information is carried to the medulla via the glossopharyngeal and vagal nerves, respectively. Although central mechanisms of hypoxemic arousal are not clear, they do not rely on serotonergic neurons, but may involve other neurons in the raphe and solitary tract nuclei [6, 11]. At the same time, afferent information from peripheral chemoreceptors stimulates respiratory neurons to increase ventilation and restore O2 levels back to normal.
Arousal can also be induced by increased work of breathing in response to airway occlusion [12]. Nevertheless, as arousal does not occur during early airway obstruction (at apnea onset), it is implicit that the development of hypercapnia and hypoxia is critical in arousal with OSA.
Berry et al. have shown that OSA, in and of itself, increases the arousal threshold, possibly due to sleep fragmentation and hypoxemia [13]. White et al. showed the arousal threshold to hypoxia and hypercapnia can be increased by short-term sleep deprivation [14]. As sleep deprivation is common in acutely ill patients, they could only “speculate—as to the clinical significance of these findings as they apply to the patient with a precarious respiratory status.” In addition, Issa and Sullivan showed that an immediate effect of the initial use of continuous positive airway pressure therapy (CPAP) is to further increase the arousal threshold [15]. Sullivan and Grunstein hypothesized that this “rebound” sleep is responsible for a “marked depression of the patient’s arousability” and leaves them “vulnerable to potential life-threatening hypoxemia” [16]. They went on to state “This phenomenon can occur in patients usually with severe sleep apnea and carbon dioxide retention when a subcritical level of CPAP is selected, resulting in partial upper airway obstruction during these abnormally long episodes of REM sleep.” These and other case reports support the hypothesis that an increase in the arousal threshold in critically ill patients with OSA may predispose them to death from sustained hypoxemia and hypercapnia [17, 18].
References
Cirignotta F, Zucconi M, Mondini S, et al. Cerebral anoxic attacks in sleep apnea syndrome. Sleep. 1989;12:400–4.
Dyken ME, Yamada T, Glenn CL, et al. Obstructive sleep apnea associated with cerebral hypoxemia and death. Neurology. 2004;62:491–3.
Dyken ME, Afifi AK, Im KB. Stroke in sleep. In: Chokroverty S, Sahota P, editors. Acute and emergent events in sleep disorders. New York: Oxford University Press; 2011. p. 328–48.
Martin SE, Engleman HM, Kingshott RN, et al. Microarousals in patients with sleep apnoea/hypopnoea syndrome. J Sleep Res. 1997;6:276–80.
Richerson GB. Serotonergic neurons as carbon dioxide sensors that maintain pH homeostasis. Nat Rev Neurosci. 2004;5:449–61.
Buchanan GF, Richerson GB. Central serotonin neurons are required for arousal to CO2. Proc Natl Acad Sci U S A. 2010;107:16354–9.
Severson CA, Wang W, Pieribone VA, et al. Midbrain serotonergic neurons are central pH chemoreceptors. Nat Neurosci. 2003;6:1139–40.
Bradley SR, Pieribone VA, Wang W, et al. Chemosensitive serotonergic neurons are closely associated with large medullary arteries. Nat Neurosci. 2002;5(5):401–2.
Ptak K, Yamanishi T, Aungst J, et al. Raphé neurons stimulate circuit activity by multiple mechanisms via endogenously released serotonin and substance P. J Neurosci. 2009;29(12):3720–37.
Berthon-Jones M, Sullivan CE. Ventilatory and arousal responses to hypoxia in sleeping humans. Am Rev Respir Dis. 1982;125:632–9.
Darnall RA, Schneider RW, Tobia CM, et al. Arousal from sleep in response to intermittent hypoxia in infant rodents is modulated by medullary raphe GABAergic mechanisms. Am J Physiol Regul Integr Comp Physiol. 2012;302:R551–60.
Issa FG, Sullivan CE. Arousal and breathing responses to airway occlusion in healthy sleeping adults. J Appl Physiol. 1983;55:1113–9.
Berry RB, Kouchi KG, Der DE, et al. Sleep apnea impairs the arousal response to airway occlusion. Chest. 1996;109:1490–6.
White DP, Douglas NJ, Pickett CK, et al. Sleep deprivation and the control of ventilation. Am Rev Respir Dis. 1983;198:984–6.
Issa FG, Sullivan CE. The immediate effects of nasal continuous positive airway pressure treatment on sleep pattern in patients with obstructive sleep apnea syndrome. Electroencephalogr Clin Neurophysiol. 1986;63:10–7.
Sullivan CE, Grunstein RR. Continuous positive airways pressure in sleep-disordered breathing. In: Kryger MH, Roth T, Dement WC, editors. Principles and practice of sleep medicine. Philadelphia: W.B. Saunders Company; 1989. p. 559–70.
Gami AS, Olson EJ, Shen WK, Wright RS, Ballman KV, Hodge DO, Herges RM, Howard DE, Somers VK. Obstructive sleep apnea and the risk of sudden cardiac death: a longitudinal study of 10,701 adults. J Am Coll Cardiol. 2013;62(7):610–6.
Pearce S, Saunders P. Obstructive sleep apnoea can directly cause death. Thorax. 2003;58(4):369.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
1 Electronic Supplementary Material
The polysomnogram (PSG) of a 52-year-old man, with a history of OSA, pulmonary hypertension, diabetes, and myocardial infarction shows during rapid-eye-movement (REM) sleep a 90-s obstructive apnea, with a minimum oxygen saturation (SaO2) level of 31%, followed by diffuse EEG slowing (not compatible with the patient’s normal slow wave pattern of stage N3 [NREM 3] sleep) suggesting cerebral hypoxemia. This apnea persists despite increasing bi-level-PAP to 15/10 centimeters of water pressure (CWP), loud commands, shaking and sternal rub. After 30-s of unresponsiveness, the initial EEG slowing is immediately followed by a 45-s period of flat/absent EEG activity (using a recording sensitivity of 7 μv/mm). At this time emergency rescue breathing was initiated, after which the patient resumes his normal waking breathing pattern and opens his eyes (MOV 44307 kb)
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Dyken, M.E., Glenn, C.L., Richerson, G.B. (2023). Obstructive Sleep Apnea Associated with Cerebral Hypoxemia. In: Thomas, R.J., Bhat, S., Chokroverty, S. (eds) Atlas of Sleep Medicine. Springer, Cham. https://doi.org/10.1007/978-3-031-34625-5_41
Download citation
DOI: https://doi.org/10.1007/978-3-031-34625-5_41
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-34624-8
Online ISBN: 978-3-031-34625-5
eBook Packages: MedicineMedicine (R0)