Abstract
It is widely accepted that the ideal way for a human infant to be nourished up to the age of 6 months is exclusive breastfeeding. Thereafter, breastfeeding with additional sources of nutrition is suitable up to the first or second birthday, or for even more prolonged periods [1, 2]. Breast milk is the sole food which precisely addresses the developmental requirements of the infant, providing both nutritional elements and bioactive compounds to ensure survival as well as healthy growth [3]. In this chapter, the nutritional and bioactive elements of breast milk are summarised. The latter category includes cells, molecules which target infectious pathogens and dampen down inflammation, growth factors and prebiotics. Breast milk differs from artificial substitutes insofar as the latter is of essentially fixed composition, whereas breast milk varies considerably in its constituents, whether in a single nursing session, over the course of the day or over the whole period of lactation. Human milk composition differs from mother to mother, as it does between populations. There are a number of reasons for this variable composition, including factors related to both the mother and the surrounding environment, as well as to the way milk is expressed and the feeding pattern. Knowledge of the constituents of breast milk is vital, in order to best utilise the opportunities breastfeeding offers, especially for those children who are most vulnerable to adverse outcomes, and to inform discussion about how breast milk can potentially be stored and whether it should be pasteurised. The chapter will also discuss bioactive factors which have been identified as potential prophylactic or therapeutic agents and may be suitable to undergo pharmaceutical development and testing [3–5].
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
It is widely accepted that the ideal way for a human infant to be nourished up to the age of 6 months is exclusive breastfeeding. Thereafter, breastfeeding with additional sources of nutrition is suitable up to the first or second birthday, or for even more prolonged periods [1, 2]. Breast milk is the sole food which precisely addresses the developmental requirements of the infant, providing both nutritional elements and bioactive compounds to ensure survival as well as healthy growth [3]. In this chapter, the nutritional and bioactive elements of breast milk are summarised. The latter category includes cells, molecules which target infectious pathogens and dampen down inflammation, growth factors and prebiotics. Breast milk differs from artificial substitutes insofar as the latter is of essentially fixed composition, whereas breast milk varies considerably in its constituents, whether in a single nursing session, over the course of the day or over the whole period of lactation. Human milk composition differs from mother to mother, as it does between populations. There are a number of reasons for this variable composition, including factors related to both the mother and the surrounding environment, as well as to the way milk is expressed and the feeding pattern. Knowledge of the constituents of breast milk is vital, in order to best utilise the opportunities breastfeeding offers, especially for those children who are most vulnerable to adverse outcomes, and to inform discussion about how breast milk can potentially be stored and whether it should be pasteurised. The chapter will also discuss bioactive factors which have been identified as potential prophylactic or therapeutic agents and may be suitable to undergo pharmaceutical development and testing [3,4,5].
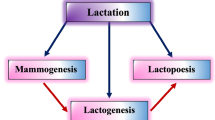
2 Stages of Lactation
The initial milk expressed by the mother postpartum is colostrum, which differs from mature milk in the amount expressed, its appearance and constituents. This early milk is expressed in low volumes over the initial days after delivery and contains abundant immune-related cells and humoral factors, notably secretory IgA, lactoferrin and white blood cells. It also contains factors that direct development, such as epidermal growth factor (EGF) [4,5,6]. The level of lactose in colostrum is low and it appears that this fluid is optimised for immune support and directing growth more than for supplying nutrition. The electrolyte composition of colostrum also differs from transitional or mature milk, being richer in sodium, chloride and magnesium ions, but lower in potassium and calcium [5, 6]. The rising of milk lactose concentration heralds the onset of transitional milk. Within the breast, this reflects a structural change, with the epithelium developing tight junctions between cells. The exact point at which this change occurs varies from mother to mother, however the expression of transitional milk, known as the second stage of lactogenesis, generally begins a few days after delivery. The second stage is considered delayed if it has not started by 72 h postpartum. This delay seems to be associated with neonatal prematurity and maternal obesity. It also correlates with specific metabolic biomarkers [7, 8]. The changes in biochemical composition that confirm the onset of the second stage include sodium concentration, sodium to potassium ratio, as well as citrate and lactose levels [9].
Transitional milk somewhat resembles colostrum, although it involves a considerable step up in milk production as called for by the infant’s rapid development and growth, which impose greater metabolic demands. The usual period during which transitional milk is expressed is from 5 days to 2 weeks after delivery. It is followed by the stage of mature milk. Mature milk contains all the expected elements at around 4–6 weeks after birth. Thereafter, there are only relatively minor adjustments to the constituents contained in breast milk, although compositional variety is always a feature of human milk [10, 11].
3 Studies of Breast Milk Composition
Studies concerning the composition of breast milk, as indexed in Medline, have steadily increased in number over the last half-century. There are still announcements of newly discovered constituents in human milk, and an active global research effort is underway to determine the functions of each constituent. There have been multiple studies examining the composition of breast milk in different groups of mothers. These studies employed a range of methods to collect, store and analyse human milk. The ideal method of sampling is to obtain multiple samples of milk from the same mother at different points during a 24-h period [10, 11]. This sampling technique suffers from the disadvantage that it is costly and may discourage mothers from enrolling in a study. A second technique that allows for standardisation is to take all samples at a particular point during the day, such as in the morning, and to collect the entire milk content of whichever breast has not been used to feed the infant in the preceding 2–3 h. This procedure needs to be repeated several times in the same study participant on different days [12]. The majority of studies in the literature, nonetheless, are based on milk obtained in a non-standardised way from milk banks, where the milk arrives at different times and different points during nursing and is expressed from mothers at different stages of lactation. These studies on the composition of breast milk also lack standardisation in how and for how long milk was stored, how frequently was frozen and defrosted and whether it was pasteurised or not. All these factors may partly explain the heterogeneity in the results obtained.
4 Nutritional Constituents within Breast Milk
There are three sources for the nutritional components of breast milk. The lactocytes synthesise a number of compounds for secretion into milk. The maternal diet supplies other components, whilst others come from the body stores of the mother. In general, breast milk retains its nutritional value despite maternal dietary deficiencies, but there are specific vitamins and fatty acids which must be present in the maternal diet for these compounds to be present in breast milk. This issue is discussed elsewhere in this volume [12,13,14].
4.1 Macronutrients
The level of macronutrients in breast milk does exhibit a degree of variation between individuals and over the whole course of breastfeeding, but there is a notable consistency in macronutrient content in different groups, despite differences in maternal diets. On average, the concentration of protein in mature milk is calculated to lie between 0.9 and 1.2 g/dL, of lipids from 3.2 to 3.6 g/dL and of lactose from 6.7 to 7.8 g/dL. The calorific value of breast milk is estimated at between 65 and 70 kcal/dL and is mostly related to the lipid content. There are differences between milk expressed following a term pregnancy and that seen from mothers of preterm infants. Preterm milk generally contains a higher concentration of protein and lipids. A study undertaken in the Californian city of Davis examined mature milk expressed 4 months after delivery and related its macronutrient composition to specific characteristics of the mother. There were a number of maternal characteristics found to be of significance, in particular body mass index (BMI), dietary protein, parity, whether menses had recommenced and how often the infant was fed. Individual mothers whose milk production was greater generally produced milk that was less rich in lipids and protein but richer in lactose.
Breast milk proteins can be separated into those that aggregate in the whey and those that are in the casein fraction. Each fraction contains a surprisingly varied range of different proteins and peptides [14, 15]. The proteins present at the highest concentration are casein, α-lactalbumin, lactoferrin, secretory immunoglobulin IgA, lysozyme and serum albumin [16, 17]. Around 25% of the nitrogen contained in breast milk is not in protein form, being found as urea, urate, creatine, creatinine, amino acids or nucleotides. There is a significantly higher level of protein in breast milk from mothers of preterm infants. Whatever the stage of pregnancy when delivery occurred, protein content falls in breast milk between the first and fourth to sixth weeks. If a preterm infant is fed by donor milk, the concentration of protein and amino acids is insufficient unless artificially supplemented. This is because most donor milk is of mature type and provided by mothers who delivered a term infant. The level of protein in breast milk does not depend on what the mother eats, but it does rise if the BMI is greater and falls when the volume of milk expressed is very high [10, 18].
The typical lipid composition of breast milk involves a high volume of palmitic acid and oleic acid residues attached to triacylglycerides. Palmitic acid is generally attached mid-chain to the glycerol moiety, whereas oleic acid is attached to either of the terminal carbons. The macronutrient category subject to the most variation in breast milk is lipid. The lipid content of hindmilk, the end portion of a feed, potentially contains three-fold more lipid than the initial foremilk [19]. One study which evaluated milk sampled from 71 women over the course of a full day reported that the lipid concentration was highest during the afternoon or evening and this finding was of statistical significance [20]. A different study correlated a quarter of the variation in fat contained in breast milk with variation in maternal protein consumption [10].
The aliphatic acid content of breast milk is affected by maternal dietary consumption, especially consumption of long chain polyunsaturated fatty acids (LCPUFAs). In Western countries, most fatty acids of this type in the diet are omega-6 aliphatic acids, with less consumption of omega-3 acids than is ideal. In North American mothers, breast milk is markedly deficient in docosahexaenoic acid; therefore lactating mothers whose diet lacks this nutrient should be advised to consume supplements to remedy the defect [18, 21, 22].
The main type of sugar within breast milk is lactose, a disaccharide. Lactose varies the least amongst the macronutrients found in breast milk, although it has been noted that women with a high milk volume do secrete greater concentrations of lactose into milk [10]. Oligosaccharides are also a major carbohydrate component in breast milk. They are typically present at a concentration of around 1 g/dL, although this varies according to the stage in breastfeeding and the genetic composition of the mother [23,24,25]. Oligosaccharides in breast milk are not nutritive, but they perform other biological functions, as described later.
Figures representing the mean concentration of macronutrients in breast milk are helpful, but should not be allowed to give the misleading impression that individual samples of milk vary little in their composition. The opposite, in fact, applies, and this variation is especially apparent in lipid and protein concentrations. The total protein concentration in breast milk from mothers who delivered at term ranges from 0.6 to 1.4 g/dL. The range for lipids is from 1.8 to 8.9 g/dL, for lactose from 6.4 to 7.6 g/dL and the calorific value is between 50 and 115 kcal/dL [26]. There are significant differences between milk from mothers who delivered at term and those whose delivery was premature. Accordingly, when a nutritional plan for an infant at high risk is being formulated, the milk available needs to be analysed and fortified as necessary, whilst also monitoring effects on the infant’s growth [27].
4.2 Micronutrients
Breast milk provides the standard to which artificial formula needs to approach to achieve optimal nutritional value. However, there is significant variation in the micronutrient content of breast milk as a result of variation in maternal diet and body stores. This especially applies to vitamins A, B1, B2, B6, B12, D, and iodine. Given the fact that mothers frequently consume a suboptimal diet, mothers can be advised to keep taking multivitamins whilst breastfeeding continues [28, 29]. The level of vitamin K in breast milk is always low, whatever the mother’s dietary intake. This is the reasoning behind the American Academy of Paediatrics’ recommendation that vitamin K should be administered intramuscularly to all neonates to prevent haemorrhagic disease of the newborn [28]. The level of vitamin D in breast milk is also low, especially if the mother has inadequate exposure to sunlight. Due to lifestyle changes, this is now frequently the case all across the globe [30]. Although benefit from supplementing the diet of breastfeeding mothers with vitamin D has not yet been proven experimentally, current guidelines advise supplying additional vitamin D to all new breastfeeding mothers and their offspring. The inability to provide a thorough, detailed review of every micronutrient contained in breast milk is a limitation of this chapter. Interested readers can find several detailed reviews available elsewhere in the literature [28, 29, 31].
5 Bioactive Constituents and Their Sources
One definition of bioactive constituents in the diet considers them as substances which ‘affect biological processes or substrates which hence have an impact on body function or condition and ultimately health’ [32, 33]. The bioactive molecules found in breast milk originate from several different sources. The epithelial cells of breast produce and secrete certain such compounds, whilst cellular components of milk are the source of others. Furthermore, the breast epithelium recognises and actively transports some molecules from the plasma to the milk, by means of specific receptor interactions. The epithelial cells secrete milk fat globules (MFGs), which contain within them various proteins attached to membranes as well as specific lipid components [34]. These different sources all contribute to the abundance of bioactive molecules within breast milk. In women who are breastfeeding, B-lymphocytes are drawn towards the breast, and secretory immunoglobulin produced by these cells is then transferred into the milk ducts via polymeric immunoglobulin receptors (pIgR) [35]. In contrast, vascular endothelial growth factor (VEGF) concentrations are significantly higher in breast milk than in maternal circulation, which suggests that VEGF is manufactured and secreted by the breast itself [36, 37]. A knowledge of where the constituents of breast milk that possess bioactivity originate is helpful in understanding the varying levels of secreted maternal medications in milk.
There are a number of ways in which research into the bioactive breast milk compounds can impact clinical practice. A key concept that both patients and the wider public need to grasp is that the research so far clearly shows that breast milk is more sophisticated than just another type of food. Indeed, breast milk provides infants with a number of compounds which enhance both survival and healthy growth. Accordingly, for infants at risk and where the mother cannot supply her own milk, donor breast milk is vital, provided it is safe to use. Proteomic studies reveal that the types of proteins present differ according to the stage of breastfeeding, in addition to differences associated with whether delivery occurred at term or prematurely [14, 15]. Thus, wherever the possibility exists, donor milk should be from a donor whose own infant is at the same stage of development as the patient. In actual clinical practice, this precise matching may not be achievable. Recognition of the role of bioactive compounds in breast milk has led to a rethink in how donor milk is collected, stored and pasteurised. Retaining bioactivity has become the goal. Furthermore, the mechanisms by which bioactive milk constituents enhance infant health offer new targets for future pharmaceutical or other therapeutic interventions [36, 37].
This chapter does not aim to comprehensively review the entire spectrum of bioactivity in breast milk. Instead, the objective is to examine a subset of bioactive factors in breast milk and relate their changing levels to the developmental requirements of the infant. The patterns of secretion associated with term and premature delivery are described, as well as the variations associated with the stage of lactation. In many cases, the bioactive factors function in a synergistic manner, which means that replacement or supplementation of individual bioactive molecules or sets thereof is generally less efficacious than supplying complete breast milk [38].
6 Growth Factors
Multiple different growth factors have been identified in breast milk. These molecules act on various infant organs, such as the gut, circulatory, nervous and endocrine systems [36,37,38].
6.1 Epidermal Growth Factor (EGF): Development and Repair of the Intestinal System
EGF plays a vital role in healthy development and repair of the gut lining. It is detectable in breast milk as well as amniotic fluid [38,39,40]. EGF remains intact even in the highly acidic gastric interior, and is not degraded by digestive enzymes. Within the intestines it has a stimulatory effect upon the gut lining, promoting the synthesis of DNA and cellular replication. It also increases water and glucose uptake by the gut and promotes protein manufacture [41, 42]. EGF also performs several protective roles within the infant gut, such as preventing excessive apoptosis and opposing the action of tumour necrosis factor-alpha (TNF-α). The latter promotes inflammation and alters the tight junctions between different enterocytes and between hepatocytes [43]. Heparin-binding growth factor also belongs to the same family of related proteins. This is the principal signalling molecule involved in resolving hypoxic injury, ischaemic-reperfusion damage, shock secondary to haemorrhage, resuscitation injury and necrotising enterocolitis [44]. The highest concentration of EGF occurs at the beginning of the lactation period, decreasing as lactation continues [45, 46]. The mean concentration of EGF in colostrum exceeds the mother’s circulating level by 2000 times. In mature milk, EGF is 100 times more abundant than in maternal circulation [41]. Additionally, the level in breast milk of mothers who delivered prematurely is higher than in cases where delivery occurred at term [45, 46].
6.2 Neuronal Growth Factors: Normal Maturation
The intestinal system of infants is immature in several different ways, including the development of the enteric nervous system, which depends for proper maturation on the presence of brain-derived neurotrophic factor (BDNF) and glial cell-line-derived neurotrophic factor (GDNF). Peristaltic intestinal motion is often dysfunctional in premature infants. This function improves in the presence of BDNF. Rodent models exhibit severe deficiency of neurones in the gut of animals without GDNF. Ciliary neurotrophic factor (CNF) is a protein with similarities to BDNF and GDNF. All three molecules are present in breast milk for a period lasting 90 days after delivery. When neurones were exposed to GDNF isolated from human milk, cellular survival improved and the cells developed new projections [30, 31].
6.3 The Insulin-like Growth Factor (IGF) Superfamily and Its Effects on Tissues
Breast milk contains several IGF-related proteins, notably IGF-I and II, as well as IGF-binding proteins and proteases with specificity for IGF. These molecules are most abundant in colostrum, but their levels steadily fall as lactation proceeds. Preterm and term milk do not importantly differ in their level of IGF apart from IGF-binding protein-2 being more abundant in preterm samples. Rodents exposed to surgical stress and fed by total parenteral nutrition exhibited higher levels of tissue growth and lower levels of gut atrophy when administered IGF-I. This effect has not been demonstrated in human subjects so far [1, 2]. IGF-I potentially also increases cellular survival when the gut is exposed to oxidative injury. Breastfeeding increases the concentration of IGF-I in the circulation. IGF absorbed through the gut retains its bioactivity and can enter the vascular circulation. Exactly how IGF taken up by this route functions so far remains unknown, however it has been shown that IGF-I administered by an enteral route at physiological concentrations increases red cell synthesis and raises the haematocrit [32, 33].
6.4 Vascular Endothelial Growth Factor (VEGF): Regulating Vascular Development
The development of new blood vessels is mostly regulated by the balance between VEGF and molecules which antagonise its effect. Colostrum contains the greatest level of VEGF amongst different types of breast milk. Term milk has a greater concentration of VEGF than preterm milk [34, 35]. The pathogenesis of retinopathy of prematurity is believed to arise from a combination of immaturity of the lungs, therapeutic oxygen administration and down-regulation of VEGF. This then causes the retina to grow blood vessels in a disorganised fashion [36, 37]. It is possible that breast milk, which contains VEGF, may be beneficial in mitigating the severity of this condition.
6.5 Erythropoietin: Promoting Development of the Gut and Preventing Anaemia
Erythropoietin is the principal hormone which stimulates erythrocyte synthesis. Haemorrhage, disease of the gut and under-developed haematopoiesis are factors contributing to the anaemia which may affect premature infants. This condition then severely harms normal growth and development [36,37,38,39,40,41]. It has been proposed that exogenous administration of erythropoietin may be beneficial in the prevention of anaemia of prematurity, however results of this practice have produced unclear benefit [38]. Nonetheless, it has been demonstrated that where erythropoietin and iron are co-administered, a potential increase in haemoglobin and haematocrit occurs [39]. A trial involving low numbers of premature infants who were administered erythropoietin enterally found increased numbers of reticulocytes in the circulation. Furthermore, erythropoietin has significant trophic effects and leads to tighter integration of the enterocytic junctions. It appears that exogenous erythropoietin may partially prevent vertical transmission of HIV and may lower the incidence of necrotising enterocolitis [36,37,38,39,40,41].
6.6 Calcitonin and Somatostatin: Regulation of Growth
There are high concentrations of both calcitonin and the precursor molecule, procalcitonin, in breast milk [40]. The calcitonin receptor is present on cells of the intestines from the latter stages of pregnancy into the first year of life, as demonstrated by immunochemical methods. In normal circumstances, somatostatin undergoes swift degradation within the jejunum. It is not absorbed via the gut lining. When this hormone is delivered in breast milk, however, degradation does not occur and it remains bioactive in the intestines. The usual physiological role of somatostatin is inhibition of the action of growth factors. Its exact functions in breast milk is, however, still not fully elucidated [41, 42].
6.7 Adiponectin and Related Hormones: The Regulation of Metabolism and How the Body Is Composed
Adiponectin has a high molecular weight and possesses multiple endocrine functions, in particular the regulation of metabolism and inhibition of inflammatory responses. It is present at high concentration in breast milk and traverses the gut lining, after which it has an apparent regulatory function in metabolism in the infant. There is an inverse correlation between the concentration of breast milk adiponectin and both the infant body mass and BMI in exclusively breastfed infants. It has been hypothesised that adiponectin in breast milk may help to prevent individuals becoming obese or overweight at a later stage in life, but this has not yet been proven to occur. There are several other hormones with a regulatory role in metabolism that can be detected in breast milk. This group includes leptin, resistin and ghrelin, all of which significantly influence energy production and the relative proportions of fat and muscle, as well as orexigenesis [1, 42, 43].
7 Oligosaccharides: Selection of Optimal Gut Microbial Flora
Human milk oligosaccharides (HMO) are unique to humans and consist of chains of sugars between 3 and 32 residues in length [23, 24]. Despite their non-nutritional function, these sugars form a strikingly large component within breast milk, at a level similar to that of proteins overall. The synthesis of HMO depends on the action of glycosyltransferases, a group of enzymes which participate in the synthesis of other carbohydrates. HMO function as prebiotics, i.e. they assist the growth of a beneficial (probiotic) intestinal flora. Many pathogens remain in the gut by attachment to oligosaccharides attached to the enterocytic membrane. The HMO and conjugated proteins within the lumen act as alternative binding sites for pathogens, thus acting as a decoy and preventing their adhering to the intestinal lining. There is a variety in the particular HMO secreted by different mothers, the so-called lactotype, which bears comparison with blood groups [23,24,25]. However, there is no aspect of the lactotype corresponding to donor–recipient incompatibility, as occurs with blood transfusions. Thus, an infant may consume milk from any non-related mother. The different lactotypes have probably evolved because of varying binding affinities amongst pathogens. Certain patterns of HMO secretion are able to prevent diarrhoea secondary to infection by specific pathogens, and to inhibit HIV transmission. There is a need for more detailed research focusing on the secretion patterns for HMO and lactose in preterm milk [44, 45].
The traditional medical belief that breast milk is normally sterile has been overturned, and it now appears that breast milk has its own associated microbiota. There are various maternal factors that alter the composition of this microbiota. It also varies as breastfeeding progresses [46, 47]. The specific HMO in milk affect which microbial species colonise the gut and may partly determine which bacteria are present in breast milk.
8 Conclusion
Breast milk is a fluid which is dynamic in composition and acts in numerous different ways to promote the healthy development of the infant. It has both a nutritive and bioactive function. The constituents differ at different stages of breastfeeding and between term and preterm milk samples. Despite the numerous investigations into how breast milk is composed, research continues to identify previously unrecognised constituents. There is a pressing requirement for a study examining in a standard way breast milk samples from multiple populations. This will then allow a thorough, detailed and complete reference for the nutritive and bioactive factors in human milk to be compiled. At present, we are still at the discovery stage in understanding how breast milk contributes to the healthy development of human infants [1, 2, 48].
References
Ballard O, Morrow AL. Human Milk composition: nutrients and bioactive factors. Pediatr Clin N Am. 2013;60(1):49–74. https://doi.org/10.1016/j.pcl.2012.10.002.
Breastfeeding and the use of human milk. Pediatrics. 2012;129(3):e827–41.
Oftedal OT. The evolution of milk secretion and its ancient origins. Animal. 2012;6(3):355–68.
Castellote C, Casillas R, Ramirez-Santana C, Perez-Cano FJ, Castell M, Moretones MG, Lopez- Sabater MC, Franch A. Premature delivery influences the immunological composition of colostrum and transitional and mature human milk. J Nutr. 2011;141(6):1181–7.
Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia. 2007;12(4):211–21.
Kulski JK, Hartmann PE. Changes in human milk composition during the initiation of lactation. Aust J Exp Biol Med Sci. 1981;59(1):101–14.
Henderson JJ, Hartmann PE, Newnham JP, Simmer K. Effect of preterm birth and antenatal corticosteroid treatment on lactogenesis II in women. Pediatrics. 2008;121(1):e92–100.
Nommsen-Rivers LA, Dolan LM, Huang B. Timing of stage II lactogenesis is predicted by antenatal metabolic health in a cohort of primiparas. Breastfeed Med. 2012;7(1):43–9.
Cregan MD, De Mello TR, Kershaw D, McDougall K, Hartmann PE. Initiation of lactation in women after preterm delivery. Acta Obstet Gynecol Scand. 2002;81(9):870–7.
Nommsen LA, Lovelady CA, Heinig MJ, Lonnerdal B, Dewey KG. Determinants of energy, protein, lipid, and lactose concentrations in human milk during the first 12 mo of lactation: the DARLING study. Am J Clin Nutr. 1991;53(2):457–65.
Bauer J, Gerss J. Longitudinal analysis of macronutrients and minerals in human milk produced by mothers of preterm infants. Clin Nutr (Edinburgh, Scotland). 2011;30(2):215–20.
Geraghty SR, Davidson BS, Warner BB, Sapsford AL, Ballard JL, List BA, Akers R, Morrow AL. The development of a research human milk bank. J Hum Lact. 2005;21(1):59–66.
Prentice A. Regional variations in the composition of human milk. In: Jensen RG, editor. Handbook of milk composition. San Diego, CA: Academic Press, Inc.; 1995. p. 919.
Liao Y, Alvarado R, Phinney B, Lonnerdal B. Proteomic characterization of human milk whey proteins during a twelve-month lactation period. J Proteome Res. 2011;10(4):1746–54.
Gao X, McMahon RJ, Woo JG, Davidson BS, Morrow AL, Zhang Q. Temporal changes in milk proteomes reveal developing milk functions. J Proteome Res. 2012;11(7):3897–907.
Lonnerdal B. Human milk proteins: key components for the biological activity of human milk. Adv Exp Med Biol. 2004;554:11–25.
Jensen RG. Handbook of milk composition. San Diego, CA: Academic Press, Inc.; 1995. Pediatr Clin North Am. Author manuscript; available in PMC 2014 February 01.
Valentine CJ, Morrow G, Fernandez S, Gulati P, Bartholomew D, Long D, Welty SE, Morrow AL, Rogers LK. Docosahexaenoic acid and amino acid contents in pasteurized donor Milk are low for preterm infants. J Pediatr. 2010;157(6):906–10.
Saarela T, Kokkonen J, Koivisto M. Macronutrient and energy contents of human milk fractions during the first six months of lactation. Acta Paediatr. 2005;94(9):1176–81.
Kent JC, Mitoulas LR, Cregan MD, Ramsay DT, Doherty DA, Hartmann PE. Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006;117(3):e387–95.
Valentine CJ, Morrow G, Pennell M, Morrow AL, Hodge A, Haban-Bartz A, Collins K, Rogers LK. Randomized controlled trial of docosahexaenoic acid supplementation in midwestern U.S. human milk donors. Breastfeed Med. 2012; https://doi.org/10.1089/bfm.2011.0126.
Martin MA, Lassek WD, Gaulin SJ, Evans RW, Woo JG, Geraghty SR, Davidson BS, Morrow AL, Kaplan HS, Gurven MD. Fatty acid composition in the mature milk of Bolivian forager- horticulturalists: controlled comparisons with a US sample. Matern Child Nutr. 2012;8(3):404–18.
Newburg DS, Ruiz-Palacios GM, Morrow AL. Human milk glycans protect infants against enteric pathogens. Annu Rev Nutr. 2005;25:37–58.
Morrow AL, Ruiz-Palacios GM, Jiang X, Newburg DS. Human-milk glycans that inhibit pathogen binding protect breast-feeding infants against infectious diarrhea. J Nutr. 2005;135(5):1304–7.
Gabrielli O, Zampini L, Galeazzi T, Padella L, Santoro L, Peila C, Giuliani F, Bertino E, Fabris C, Coppa GV. Preterm milk oligosaccharides during the first month of lactation. Pediatrics. 2011;128(6):e1520–31.
Michaelsen KF, Skafte L, Badsberg JH, Jorgensen M. Variation in macronutrients in human bank milk: influencing factors and implications for human milk banking. J Pediatr Gastroenterol Nutr. 1990;11(2):229–39.
Arslanoglu S, Moro GE, Ziegler EE. The Wapm Working Group on nutrition. Optimization of human milk fortification for preterm infants: new concepts and recommendations. J Perinat Med. 2010;38(3):233–8.
Greer FR. Do breastfed infants need supplemental vitamins? Pediatr Clin N Am. 2001;48(2):415–23.
Allen LH. B vitamins in breast milk: relative importance of maternal status and intake, and effects on infant status and function. Adv Nutr. 2012;3(3):362–9.
Dawodu A, Zalla L, Woo JG, Herbers PM, Davidson BS, Heubi JE, Morrow AL. Heightened attention to supplementation is needed to improve the vitamin D status of breastfeeding mothers and infants when sunshine exposure is restricted. Matern Child Nutr. 2012;10:383.
Pediatrics, AAo. Pediatric nutrition handbook. 6th ed. Elk Gove Village, IL: American Academy of Pediatrics; 2009.
Korhonen H, Marnila P, Gill HS. Milk immunoglobulins and complement factors. Br J Nutr. 2000 Nov;84 Suppl 1:S75–80.
Garofalo R. Cytokines in human milk. J Pediatr. 2010;156(2 Suppl):S36–40.
Cavaletto M, Giuffrida MG, Conti A. The proteomic approach to analysis of human milk fat globule membrane. Clin Chim Acta. 2004;347(1–2):41–8.
Van de Perre P. Transfer of antibody via mother’s milk. Vaccine. 2003;21(24):3374–6.
Kobata R, Tsukahara H, Ohshima Y, Ohta N, Tokuriki S, Tamura S, Mayumi M. High levels of growth factors in human breast milk. Early Hum Dev. 2008;84(1):67–9.
Patki S, Patki U, Patil R, Indumathi S, Kaingade P, Bulbule A, Nikam A, Pishte A. Comparison of the levels of the growth factors in umbilical cord serum and human milk and its clinical significance. Cytokine. 2012;59(2):305–8.
Hirai C, Ichiba H, Saito M, Shintaku H, Yamano T, Kusuda S. Trophic effect of multiple growth factors in amniotic fluid or human milk on cultured human fetal small intestinal cells. JPGN. 2002;34:524–8.
Chailler P, Menard D. Ontogeny of EGF receptors in the human gut. Front Biosci. 1999;4:87–101.
Wagner CL, Taylor SN, Johnson D. Host factors in amniotic fluid and breast milk that contribute to gut maturation. Clinic Rev Allerg Immunol. 2008;34:191–204.
Read LC, Upton FM, Francis GL, Wallace JC, Dahlenberg GW, Ballad FJ. Changes in the growth- promoting activity of human milk during lactation. Pediatr Res. 1984;18(2):133–9.
Chang C-Y, Chao JC-J. Effect of human milk and epidermal growth factor on growth of human intestinal caco-2 cells. JPGN. 2002;34:394–401.
Khailova L, Dvorak K, Arganbright KM, Williams CS, Halpern MD, Dvorak B. Changes in hepatic cell junctions structure during experimental necrotizing enterocolitis: effect of EGF treatment. Pediatr Res. 2009;66(2):140–4.
Radulescu A, Zhang H-Y, Chen C-L, Chen Y, Zhou Y, Yu X, Otabor I, Olson JK, Besner GE. Heparin-binding EGF-like growth factor promotes intestinal anastomotic healing. J Surg Res. 2011;171:540–50.
Dvorak B, Fituch CC, Williams CS, Hurst NM, Schanler RJ. Increased epidermal growth factor levels in human milk of mothers with extremely premature infants. Pediatr Res. 2003;54(1):15–9.
Dvorak B, Fituch CC, Williams CS, Hurst NM, Schanler RJ. Concentrations of epidermal growth factor and transforming growth factor-alpha in preterm milk. In: Pickering LK, et al., editors. Protecting infants through human milk. Kluwer Academic/Plenum Publishers; 2004. p. 407–9.
Rodrigues D, Li A, Nair D, Blennerhassett M. Glial cell line-derived neurotrophic factor is a key neurotrophin in the postnatal enteric nervous system. Neurogastroenterol Motil. 2011;23:e44–56.
Boesmans W, Gomes P, Janssens J, Tack J, Berghe PV. Brain-derived neurotrophic factor amplifies neurotransmitter responses and promotes synaptic communication in the enteric nervous system. Gut. 2008;57:314–22.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Özdemir, S.A., Şahin, Ö.N., Briana, D.D. (2023). Human Milk Composition: Nutrients and Bioactive Factors. In: Şahin, Ö.N., Briana, D.D., Di Renzo, G.C. (eds) Breastfeeding and Metabolic Programming. Springer, Cham. https://doi.org/10.1007/978-3-031-33278-4_1
Download citation
DOI: https://doi.org/10.1007/978-3-031-33278-4_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-33277-7
Online ISBN: 978-3-031-33278-4
eBook Packages: MedicineMedicine (R0)