Abstract
Brachytherapy (BT) with or without external beam radiotherapy remains the standard of care in the treatment for early-stage and locally advanced gynecological malignancies treated with definitive radiation, where it has demonstrated an overall survival benefit. Stereotactic body radiotherapy (SBRT) has been explored for the treatment of patients who are unable to have brachytherapy procedures, have persistent disease after definitive treatment, develop pelvic or distant recurrences, or present with oligometastatic disease. This chapter explores treatment indications, technique, and management of toxicity and reviews published literature regarding SBRT for gynecologic malignancies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Stereotactic body radiotherapy
- Oligometastasis
- Pelvic recurrence
- Pelvic sidewall
- Severe late toxicity
- Para-aortic lymph node metastasis
Pearls
-
SBRT has been employed in recurrent, oligometastatic, and up-front settings for gynecologic tumors, alone or with EBRT.
-
There are no randomized trials to evaluate the efficacy and toxicity of SBRT in these settings.
-
Local control rate for SBRT re-irradiation of lymph node or distant metastatic sites is ≥65%.
-
Local control of small tumors approaches 100% (Choi et al. 2015; Deodato et al. 2009; Guckenberger et al. 2010).
-
Local control appears dose dependent with doses BED10 > 70 for ovarian cancer and possibly higher for other cancers (Macchia et al. 2020; Seo et al. 2015).
-
Local control rate for SBRT re-irradiation/pelvic sidewall failures is ~40–50% (Dewas et al. 2011; Park et al. 2015).
-
Distant metastasis is the most common failure pattern after SBRT for recurrent tumors with 45–70% 2–4 year distant failure rate.
Treatment Indications
-
For gynecologic malignancies, SBRT may be indicated to treat isolated lateral pelvic or nodal recurrences or oligometastatic disease (Table 9.1).
-
While early studies have explored SBRT techniques to administer a boost dose in definitive radiotherapy for gynecologic malignancies, brachytherapy remains the gold standard for this purpose.
-
SBRT should be cautiously utilized for salvage of central recurrences within the high-dose region of the prior treatment field in patients who have undergone definitive radiation owing to its high potential toxicity.
Workup and Recommended Imaging
-
H&P, including prior radiotherapy, detailed gynecologic history, performance status, pelvic examination.
-
Review of systems:
-
Vaginal bleeding.
-
Pelvic or back pain.
-
Neuropathy associated with sidewall recurrences leading to leg pain or weakness.
-
Bowel or bladder symptoms.
-
-
Labs:
-
CBC, metabolic panel, liver function tests.
-
-
Imaging:
-
MRI within 2 weeks of SBRT.
-
PET/CT or CT with contrast as alternatives for recurrent disease.
-
-
Pathology:
-
FNA or CT-guided biopsy of accessible lesions.
-
Radiosurgical Technique
Simulation and Treatment Planning
-
Supine position, arms on chest or overhead.
-
Immobilization with body frame and/or fiducial monitoring or bone/body tracking.
-
Consider bladder empty or empty and full scan to reproducibly optimize dosimetry to adjacent organs at risk (OARs).
-
Thin-cut CT (≤2.5 mm thickness) recommended.
-
IV and oral contrast to delineate bowel and vessels.
-
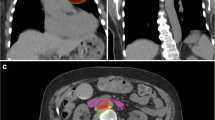
GTV is contoured using fusion of the MRI or PET/CT scan merged into the area of interest on simulation CT scan.
-
PTV = GTV + 3–8 mm (dependent upon site-specific motion considerations).
-
Lower OAR doses can be achieved using a large number of beam angles/arcs and smaller margins.
-
Phantom-based QA on all treatment plans prior to delivery of first fraction.
Dose Prescription
-
Doses are divided into 1–5 fractions usually over 1–2 weeks.
-
SBRT alone in previously unirradiated sites:
-
SBRT alone in previously irradiated fields:
-
SBRT with EBRT 45 Gy for PALN recurrences:
-
5 Gy × 4–5 fractions (Higginson et al. 2011)
-
-
In series where SBRT has substituted for brachytherapy boost during initial treatment of the primary tumor, dose prescriptions mimic commonly accepted brachytherapy schedules:
-
7 Gy × 4 fractions (Albuquerque et al. 2020)
-
-
Dose prescribed to 70–80% IDL.
Dose Limitations
-
Dose limitations to OAR should meet accepted brachytherapy standards or those as outlined in TG 101 (see Appendix).
-
In the setting of re-irradiation, composite planning should be employed, with appropriate BED conversion for dose summation.
Dose Delivery
-
Initial verification by kV X-ray or CBCT to visualize the tumor or surrogate markers for positioning.
-
Verification imaging should be repeated at least every 5 min for longer treatments.
Toxicities and Management
-
Grade 3 or higher acute toxicity or severe late toxicity is rare.
-
Common acute toxicities:
-
Fatigue:
-
Usually self-limiting but may last for several weeks to months.
-
-
Urethritis/cystitis:
-
Treatment with phenazopyridine or topical analgesics at the urethral meatus.
-
-
Dermatitis:
-
Skin erythema, hyperpigmentation, dry desquamation.
-
Limited by increased number of beam angles to reduce entrance and exit doses.
-
Treated with supportive care, including moisturizers, low-dose steroid creams, topical analgesics, and antimicrobial salves.
-
-
Diarrhea/proctitis:
-
Managed with low-residue diet and antidiarrheals.
-
-
Nausea:
-
More common with treatment of retroperitoneal nodes leading to bowel dose.
-
Pretreatment with antiemetic 1 h prior to each fraction can limit acute episodes of nausea after treatment.
-
-
-
Moderate or severe late toxicities:
-
Vaginal stenosis:
-
Managed with vaginal dilator every other day.
-
-
Ureteral stricture:
-
Expectant management or dilatation procedure.
-
-
Vesicovaginal or rectovaginal fistula:
-
Surgical management.
-
-
Intestinal obstruction:
-
Managed with bowel rest or surgical management.
-
-
Soft-tissue necrosis has been observed particularly in the re-treatment setting. If symptomatic, this may be treated with hyperbaric oxygen therapy.
-
Recommended Follow-Up
-
Pelvic exam every 3 months for 2 years, then every 6 months for 3 years, then annually.
-
For cervical cancers, Pap smear every 6 months for 5 years and then annually. Pap smear surveillance should start 6 months after treatment due to postradiation changes.
-
PET/CT or CT A/P with contrast 3 months after completion of therapy.
Evidence
SBRT for Oligometastases or as Re-irradiation for Recurrent Tumors
-
Kunos et al. (2012): Prospective phase II study, 50 patients with primary gynecologic site, recurrence in ≤4 metastases. Treatment sites were PALN (38%), pelvis (28%), and other distant sites including abdomen, liver, lung, and bone (34%). Dose was 8 Gy × 3 fractions to 70% IDL with Cyberknife. CTV = PET-avid lesions. PTV = CTV + 3 mm. Thirty-two percent had treatment in previously irradiated field. Median follow-up for surviving patients 15 months. No SBRT-treated lesion progressed. Sixty-four percent recurred elsewhere. Three patients (6%) had grade 3–4 toxicity (one grade 3 diarrhea, one enterovaginal fistula, one grade 4 hyperbilirubinemia) (Kunos et al. 2012).
-
Dewas et al. (2011): Retrospective study of 16 previously irradiated patients (45 Gy median dose) with pelvic sidewall recurrences. Primary tumors were cervix (n = 4), endometrial (n = 1), bladder (n = 1), anal (n = 6), and rectal (n = 4). Treatment was 36 Gy to 80% IDL in 6 fractions over 3 weeks with Cyberknife. Median maximum tumor diameter 3.5 cm. 10.6-month median follow-up. One-year actuarial LC 51%. Median DFS 8.3 months. Four of eight patients with sciatic pain had reduction in pain by the end of treatment, but none were able to discontinue opiates. No grade 3 or higher toxicity (Dewas et al. 2011).
-
Choi et al. (2009): Retrospective study of 28 cervical cancer patients with isolated PALN metastases. Twenty-four had SBRT 33–45 Gy in 3 fractions; 4 had EBRT followed by SBRT boost. PTV = GTV + 2 mm. Rx to 73–87% IDL. Twenty-five patients received cisplatin-based chemotherapy before (n = 2), during (n = 9), or after (n = 14) SBRT. Four-year LC was 68% overall, and 100% if PTV volume ≤17 mL (Choi et al. 2009).
-
Higginson et al. (2011): Retrospective study of 16 patients treated with SBRT (9 recurrences, 5 SBRT boost, 2 oligometastatic). SBRT doses were 12–54 Gy in 3–5 fractions. Eleven patients had additional EBRT 30–54 Gy. Eleven-month median follow-up. LC 79%. Distant failure 43% (Higginson et al. 2011).
-
Guckenberger et al. (2010): Retrospective study of 19 patients with isolated pelvic recurrence after primary surgical treatment (12 cervix, 7 endometrial primaries). Sixteen previously unirradiated cases had 50 Gy EBRT followed by SBRT boost; 3 patients with prior RT had SBRT alone. Patients were selected for SBRT over brachytherapy due to size (>4.5 cm) and/or peripheral location. Dose for SBRT boost was 5 Gy × 3 fractions to median 65% IDL; SBRT only 10 Gy × 3 fractions or 7 Gy × 4 fractions to the 65% IDL. Three-year LC 81%. Median time to systemic progression 16 months. Sixteen percent severe complication rate (2 intestino-vaginal fistulas and one small bowel ileus). Two of the patients with severe complications had prior pelvic RT ± brachytherapy and had bowel maximum point dose of EQD2 >80 Gy (Guckenberger et al. 2010).
-
Deodato et al. (2009): Retrospective study of 11 patients, dose escalation with 5 daily SBRT fractions up to 6 Gy per fraction, in previously irradiated (n = 6) or previously unirradiated (n = 5) patients with recurrent gynecologic tumors. Two-year local PFS 82%. Two-year DMFS 54%. No grade 3–4 toxicity (Deodato et al. 2009).
-
Seo et al. (2015): Retrospective review of 88 patients with para-aortic recurrences treated with SBRT, of which 52 were from primary gynecological sites and 36 were from other sites. BED10 ≥ 95 Gy (p = 0.011) and gross tumor volume (GTV) ≤ 15 cm3 (p = 0.002) were associated with better local control (Seo et al. 2015).
-
Park et al. (2015): Retrospective multi-institutional (KROG 14–11) cohort of 85 patients and 100 lesions treated with SBRT for recurrent or oligometastatic uterine cancer. Predominantly (89%) lymph node metastases, with 59 within the prior radiation field, treated to a median dose of 39 Gy in 3 fractions (BED10 90 Gy). Overall, 2 and 5-year LC rates were 82.5% and 78.8%, with OS at 2 and 5 years of 57.5% and 32.9%, respectively, and only 5 incidence of grade 3+ toxicity. 2-Year local control was worse for lesions within a previously irradiated field (60.2% vs. 92.8%, p < 0.01) and tended to marginally become better for lesions treated with BED10 ≥ 69.3 Gy (87.7% vs. 66.1% p < 0.59) of which previously irradiated tumors had lower marginal doses (Park et al. 2015).
-
Macchia et al. (2020): Retrospective multi-institution (MITO RT-01) study of 261 ovarian cancer patients with metastatic, recurrent, or persistent disease treated with SBRT. Inclusive of any anatomic site, median BED10 of 50.7 Gy (range: 7.5–262.5) with a median of 1 lesion (range: 1–7) treated. At a median follow-up of 22 months, 2-year LC was 81.9%, with 95.1% late toxicity-free survival at 2 years. On MVA, patient age ≤60 years (OR 1.6), PTV volume ≤18 cm3 (OR 1.9), lymph node treatment site (OR 2.9), and BED10 > 70 Gy (OR 2.0) were associated with improved rates of complete response (Macchia et al. 2020).
-
Yegya-Raman et al. (2020): Meta-analysis of 17 studies and 667 patients with 1071 metastatic lesions from gynecologic malignancies. Predominantly ovarian (57.6%), cervical (27.1%), and uterine (11.1%), with most patients having a single metastatic site (65.4%). Response rate ranged from 49 to 97%, with most (7/8 studies) reporting >75% response. Crude local control ranged from 71 to 100% with most (14/16 studies) demonstrating a local control of >80%. Grade ≥3 toxicities were not observed in 10/16 studies. Those studies reporting grade ≥3 toxicity observed this in 2.6–10% of patients. SBRT was well tolerated with high rates of efficacy, with disease progression most commonly being reported at a distant site (79–100%) (Yegya-Raman et al. 2020).
SBRT Boost in Initial Definitive Radiotherapy
-
Kemmerer et al. (2013): Retrospective study of 11 patients with stage I–III endometrial cancer. Definitive EBRT 45 Gy followed by SBRT boost to the high-risk CTV (1 cm around endometrium and any gross disease after EBRT). Dose: 30 Gy/5 fractions in nine patients, 20–24 Gy/4 fractions in two patients, and two fractions/week. IMRT-based treatment with daily kV CBCT. Ten-month median follow-up. One-year FFP of 68% for all patients, 2-year FFP 100% for grade 1 or stage IA tumors. Eighty percent of failures were in endometrium. One grade 3 toxicity (diarrhea) (Kemmerer et al. 2013).
-
Mollà et al. (2005): Retrospective study of 16 patients with endometrial (n = 9) or cervical (n = 7) cancer treated with SBRT boost, 7 Gy × 2 (post-op, n = 12) or 4 Gy × 5 (no surgery, n = 4), two SBRT fractions per week. PTV = CTV + 6–10 mm. Median follow-up 12.6 months. Dynamic arc therapy or IMRT was used. Only 1 failure in a cervix cancer patient. One patient had grade 3 rectal toxicity (persistent rectal bleeding) and was treated previously with pelvic RT with HDR boost (Mollà et al. 2005).
-
Marnitz et al. (2013): Retrospective review of 11 patients with cervical cancer treated with SBRT boost 6 Gy × 5 fractions to 60–70% IDL QOD. PTV coverage was 93–99% to meet constraints. No grade 3 toxicity reported (Marnitz et al. 2013).
-
Mantz et al. (2016): Prospective phase II trial of curative-intent SBRT boost for patients with uterine or cervical cancer unable or unwilling to undergo surgery or brachytherapy boost. Excluded patients with GTV >125 cc. Primary definitive treatment to the pelvis of 45 Gy in 25-fraction EBRT followed by boost to the GTV of 40 Gy in 5-fraction EOD. Target was tumor plus PTV margin, and delineation of the GTV was aided by co-registration of FDG-PET imaging to the CT planning image set. Overall, 40 patients were enrolled with a median follow-up of 51 months, 33/40 (82.5%) had negative post-SBRT biopsy for invasive malignancy, and 2-year post-SBRT FDG-PET showed complete response at the primary site of disease in 77.5% of patients. No reported incidence of grade ≥3 toxicity was noted (Mantz et al. 2015).
-
Albuquerque et al. (2020): Single-arm prospective phase II trial of SBRT boost for FIGO 2009 stage IB2–IVB cervical cancer, medically unfit to undergo brachytherapy boost, treated with SBRT to 28 Gy in 4 fractions >36 h apart. CTV volume was larger than prior reports, including T2-MR gross tumor, cervix, at least 2 cm of the normal uterine canal with PTV margin 0.3 cm axial and 0.5 cm longitudinal. Overall, 15 patients accrued (53% stage III–IV), with a median follow-up of 19 months. Median SBRT boost volume was 139 cc (range: 51–268), 2-year local control 70.1%, PFS 46.7%, and OS 53.3%, all lower than expected. Smaller PTV boost in patients without grade ≥3 (95 cc versus 225 cc). Patients experiencing grade 3 toxicity were 26.7%, and dosimetric analysis demonstrated that the percentage of rectal circumference receiving 15 Gy was associated with V15 Gy (p = 0.04) with volumes >62.7% being the strongest predictor of toxicity (AUC, 0.93; sensitivity, 100%; specificity, 90%) (Albuquerque et al. 2020).
References
Albuquerque K, Tumati V, Lea J, Ahn C, Richardson D, Miller D, et al. A phase II trial of stereotactic ablative radiation therapy as a boost for locally advanced cervical cancer. Int J Radiat Oncol Biol Phys. 2020;106(3):464–71.
Choi CW, Cho CK, Yoo SY, Kim MS, Yang KM, Yoo HJ, et al. Image-guided stereotactic body radiation therapy in patients with isolated Para-aortic lymph node metastases from uterine cervical and corpus cancer. Int J Radiat Oncol Biol Phys. 2009;74(1):147–53.
Choi JW, Im YS, Kong DS, Seol HJ, Nam DH, Il LJ. Effectiveness of postoperative gamma knife radiosurgery to the tumor bed after resection of brain metastases. World Neurosurg. 2015;84(6):1752–7.
Deodato F, Macchia G, Grimaldi L, Ferrandina G, Lorusso D, Salutari V, et al. Stereotactic radiotherapy in recurrent gynecological cancer: a case series. Oncol Rep. 2009;22(2):415–9.
Dewas S, Bibault JE, Mirabel X, Nickers P, Castelain B, Lacornerie T, et al. Robotic image-guided reirradiation of lateral pelvic recurrences: preliminary results. Radiat Oncol. 2011;6(1):77.
Guckenberger M, Bachmann J, Wulf J, Mueller G, Krieger T, Baier K, et al. Stereotactic body radiotherapy for local boost irradiation in unfavourable locally recurrent gynaecological cancer. Radiother Oncol. 2010;94(1):53–9.
Higginson DS, Morris DE, Jones EL, Clarke-Pearson D, Varia MA. Stereotactic body radiotherapy (SBRT): technological innovation and application in gynecologic oncology. Gynecol Oncol. 2011;120(3):404–12.
Kemmerer E, Hernandez E, Ferriss JS, Valakh V, Miyamoto C, Li S, et al. Use of image-guided stereotactic body radiation therapy in lieu of intracavitary brachytherapy for the treatment of inoperable endometrial neoplasia. Int J Radiat Oncol Biol Phys. 2013;85(1):129–35.
Kunos CA, Brindle J, Waggoner S, Zanotti K, Resnick K, Fusco N, et al. Phase II clinical trial of robotic stereotactic body radiosurgery for metastatic gynecologic malignancies. Front. Oncologia. 2012;2:2.
Macchia G, Lazzari R, Colombo N, Laliscia C, Capelli G, D’Agostino GR, et al. A large, multicenter, retrospective study on efficacy and safety of stereotactic body radiotherapy (SBRT) in Oligometastatic ovarian cancer (MITO RT1 study): a collaboration of MITO, AIRO GYN, and MaNGO groups. Oncologist. 2020;25(2):e311–20.
Mantz CA, Shahin FA, Sandadi S, Orr J. Stereotactic body radiation therapy as a boost alternative to brachytherapy for primary gynecologic cancer: disease control and quality of life outcomes from a phase II trial. Int J Radiat Oncol. 2015;93(3):S202.
Marnitz S, Kohler C, Budach V, Neumann O, Kluge A, Wlodarczyk W, Jhan U, Debauer B, Kufeld M. Brachytherapy-emulating robotic radiosurgery in patients with cervical carcinoma. Radiat Oncol. 2013;8:109.
Mollà M, Escude L, Nouet P, Popowski Y, Hidalgo A, Rouzaud M, et al. Fractionated stereotactic radiotherapy boost for gynecologic tumors: an alternative to brachytherapy? Int J Radiat Oncol Biol Phys. 2005;62(1):118–24.
Park HJ, Chang AR, Seo Y, Cho CK, Il JW, Kim MS, et al. Stereotactic body radiotherapy for recurrent or oligometastatic uterine cervix cancer: a cooperative study of the Korean radiation oncology group (KROG 14-11). Anticancer Res. 2015;35(9):5103–10.
Seo YS, Kim MS, Cho CK, Yoo HH, Jang WI, Kim KB, Lee DH, Moon SM, Lee HR. Stereotactic body radiotherapy for oligometastases confined to the Para-aortic region: clinical outcomes and the significance of radiotherapy field and dose. Cancer Investig. 2015;33(5):18–7.
Yegya-Raman N, Cao CD, Hathout L, Girda E, Richard SD, Rosenblum NG, et al. Stereotactic body radiation therapy for oligometastatic gynecologic malignancies: a systematic review. Gynecol Oncol. 2020;159:573–80.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Susko, M.S., Sethi, R.A., Seymour, Z.A., Hsu, IC.J. (2023). Gynecologic Sites. In: Sethi, R.A., Barani, I.J., Larson, D.A., Roach III, M. (eds) Handbook of Evidence-Based Stereotactic Radiosurgery and Stereotactic Body Radiotherapy. Springer, Cham. https://doi.org/10.1007/978-3-031-33156-5_9
Download citation
DOI: https://doi.org/10.1007/978-3-031-33156-5_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-33155-8
Online ISBN: 978-3-031-33156-5
eBook Packages: MedicineMedicine (R0)