Abstract
Sedation and analgesia can reduce NIV failure associated with patient discomfort, anxiety, agitation, and pain. The ideal drug does not exist and there is limited data available on efficacy and safety to guide the development of best practice, prevailing local practice patterns. Monitoring sedation is a key point of a successful procedure. Protocols should be implemented in the ICU, including assessment through validated scales.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
The role of noninvasive ventilation (NIV) in intensive care units (ICU) has gained relevance in the past few decades in response to evidence of its benefits as a means of reducing dependence on endotracheal intubation and invasive mechanical ventilation and its associated complications. According to the European Respiratory Society/American Thoracic Society (ERS/ATS) guidelines, published in 2017, in acute settings, NIV is highly recommended for acute exacerbations of chronic obstructive pulmonary disease and severe cardiogenic pulmonary edema. It should be considered in immunocompromised patients with acute respiratory failure (ARF), weaning of hypercapnic patients, prevention of post-extubation failure of high-risk patients, postoperative period, chest trauma patients, and as a palliative treatment [1]. The main purpose of NIV in these settings is to correct gas exchange and decrease work of breathing, but different goals according to severity and end-of-life choices can be applied. NIV can be used to prevent the occurrence of ARF, to prevent further clinical deterioration and the need for endotracheal intubation when ARF is already established, or as “ceiling treatment” or palliative care in do not intubate/do not resuscitate patients [2].
The success of NIV is dependent on patient’s acceptance and compliance, which is affected by the severity of illness, claustrophobia, anxiety, patient–ventilator dyssynchronies, abdominal distension, dryness of upper airways, and interface related problems, such as air leaks, poor mask fitting, mask intolerance, and pain associated with skin lesions. The patient may refuse to continue with uncomfortable support, causing its discontinuation and subsequent requirement for endotracheal intubation. If the patient learns to breathe through the ventilator, and if the support overcomes the respiratory distress, then the need for help and reassurance decreases. The presence of healthcare staff at the bedside during the initial hours of application may help this process. Discomfort, anxiety, agitation, pain, dyspnea, and delirium may be associated with NIV failure and worst outcomes. Application of analgesia and sedation may increase patient comfort and NIV tolerance and success in specific situations, but expert teams and highly monitored settings are required, such as intensive care units. The goal is to achieve sedation to a point where the patients are comfortable and awake/arousable. There is limited data available to guide the development of best practice, prevailing local practice patterns [3].
Low-dose sedatives could be used during NIV in mildly agitated patients [2], but sedation may also delay a necessary intubation. Sedation could be of benefit in situations where NIV is clearly indicated and where careful evaluation identifies anxiety, dyspnea with a high affective dimension, or delirium as barriers to its successful implementation [3]. This rationale for sedation during NIV may be applied to the first hours of adaptation to ventilation, and later when prolonged ventilation is required [4]. The choice of NIV interface and assisted ventilation pattern may influence the need for sedation. Patient acceptance increases with less constricting interfaces (e.g., helmet). Moreover, bilevel positive airway pressure is more often related to need for anxiolytics or sedatives than continuous positive airway pressure [3].
Before considering sedation or analgesia, there are other measures that can be applied to improve tolerance of NIV. For example, an adequate choice of mask type and size, applying a rotation strategy, and using newer algorithms that enhance patient–ventilator synchrony may avoid intolerance. Also, the expertise of the NIV team contributing to appropriate adjustments in equipment and ventilator settings and to a feeling of confidence to the patient can improve the success of NIV [5]. If the patient remains intolerant and uncooperative despite these strategies, administration of analgesia and sedation may be considered to optimize the chances of success during NIV for minimizing the requirement for endotracheal intubation or when NIV is a “ceiling treatment.”
2 Discussion
The goals of sedation for a conscious and cooperative patient in ICU are to provide a good control of anxiety, agitation and discomfort, assure analgesia, preserve day/night cycles, and provide good sleep quality. Sleep quality can be optimized by avoiding factors that cause sleep disturbance such as exposure to sound and light that may disrupt circadian rhythm and cause frequent arousals from sleep. Other goals for sedation include hemodynamic stability, preservation of metabolic homeostasis, muscular relaxation, preservation of diaphragmatic function, and attenuation of the stress/immune response [3]. An ideal drug should accomplish all these goals and additionally have short acting activity, no accumulation in case of renal or liver failure, and no rebound effects when discontinued.
For patients in ICU requiring endotracheal intubation and invasive mechanical ventilation, it has been described that outcomes improve with routine monitoring of the depth of sedation, presence of pain and delirium, prompt and effective pain treatment, and when administration of sedatives is kept to the minimum necessary for the comfort and safety of the patient [6]. However, information on the management of pain, agitation, and delirium in patients undergoing NIV is scarce and there are no guidelines focusing on this subject. The recently published Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption (PADIS) in Adult Patients in the ICU do not include recommendations for patients undergoing NIV [7]. The lack of evidence-based information results in heterogeneous practices in different centers guided by individual clinical experience.
In ICU patients undergoing NIV with a high risk of failure it is important, when using sedation and analgesia, to avoid respiratory drive depression and to guarantee easy arousal with alleviation of NIV-induced discomfort. This permits patients to discharge their secretions and avoid aspiration, ultimately leading to an increase in the rate of adherence to NIV and, hopefully, the chance of success in avoiding endotracheal intubation and invasive mechanical ventilation [4].
In a survey published in 2007 [8] on sedation practices during NIV in North America, Europe and Australia/Asia, physicians reported using sedation in less than 25% of patients. Sedation and analgesia were more commonly used by North Americans than Europeans (41% vs. 24% for sedation, 48% vs. 35% for analgesia) and critical care versus noncritical care physicians (42% vs. 24% for sedation and 50% vs. 34% for analgesia). In North America, benzodiazepine alone was the preferred agent (33%), followed by an opioid alone (29%). Europeans were less likely to use a benzodiazepine alone (25%) but more likely to use an opioid alone (37%). Sedation was usually administered as an intermittent intravenous bolus, outside a protocol, and was assessed by nurses using clinical endpoints rather than a sedation scale. The differences in prescribing patterns suggest that the choice of agent is determined more by familiarity than by evidence-based practice. These results are outdated and probably do not represent current practices.
Muriel et al. published a multicenter observational study, in 2015, based on data collected in 2010, including patients who received at least 2 h of NIV as first-line therapy at ICU admission. They concluded that nearly 20% of patients received sedation or analgesia during NIV. Midazolam and morphine were the most commonly used sedative and analgesic drugs. The use of analgesics or sedatives alone was not associated with outcome but their simultaneous use was associated with NIV failure, ICU mortality and 28-day mortality [9]. Another retrospective study using data from a tertiary referral hospital in Japan, published in 2015, showed that 3.4% of patients receiving NIV due to acute respiratory failure were given sedatives to control agitation [10]. Morphine, dexmedetomidine, propofol, midazolam, and fentanyl were used in 19%, 15%, 13%, 9%, and 9% of the cases, respectively.
Pilot studies have suggested that continuous infusion of a single sedative or analgesic agent may decrease patient discomfort, with no significant deleterious effects on respiratory drive, respiratory pattern or hemodynamics, and with improvement in gas exchanges [11]. There are no robust data to favor any one drug, class of drugs, or protocol over all others [3].
The most traditionally classes of drugs used in continuous infusion to provide analgesia and sedation in ICU patients include γ-aminobutyric acid (GABA) receptor agonists (i.e., propofol and midazolam) and opioids (i.e., morphine and fentanyl). However, both classes of drugs may blunt the output of the respiratory center [5]. Modern drugs with very short half-lives and favorable pharmacokinetic profiles (i.e., remifentanil) or that do not interfere with respiratory drive (i.e., dexmedetomidine) may be of help to start and keep a mild analgosedation level under NIV [2].
2.1 Drugs for Sedation and Analgesia During NIV
Several dugs have been used for analgesia and sedation of patients during NIV. They have distinct pharmacokinetic and pharmacodynamic properties, and different side-effects (Table 63.1) that must be accounted for when choosing the optimal sedation agent for a patient.
Propofol, a widely used drug for sedation in ICU, could have a role for sedation during NIV. It acts as a GABAA agonist, with other effects, including on glutamate and cannabinoid receptors, and has a short-acting activity with a half-life of 30–60 min. Propofol causes vasodilation and negative inotropy, inducing hypotension and bradycardia [6]. Physiological studies on the effects of subhypnotic concentrations of propofol on respiratory mechanics, pharyngeal function, and airway protection have suggested the possibility of carrying out NIV while patients are under sedation [12]. Clouzeau et al. published a small cohort study with 10 patients assessing the feasibility and safety of target-controlled infusion (TCI) of propofol for conscious sedation of patients with NIV failure due to low tolerance [12]. TCI allows rapid and precise adjustment of the propofol concentration according to the clinical response of the patient. This preliminary study showed that in a selected population, TCI of propofol could be safe and effective for the treatment of NIV failure due to low tolerance. However, no further studies have been published and there is still a lack of evidence on the safety and efficacy of propofol for NIV tolerance.
Benzodiazepines act as GABAA receptor agonists but have a high risk of delirium and tolerance, and continuous administration should be discouraged. Midazolam is a short-acting benzodiazepine with a half-life of 3–11 h, but active metabolite accumulates with prolonged infusion [6]. Anxiolytic properties may be attractive for patients under NIV, but single bolus administration of the lowest possible dose followed, or not, by another sedative drug should be preferable. Benzodiazepines have been strongly associated with higher incidence of delirium. Studies in mechanically ventilated patients have concluded that benzodiazepines have worst clinical outcomes than other sedatives, and guidelines suggest using either propofol or dexmedetomidine over benzodiazepines [7]. Although there is a lack of trials evaluating benzodiazepines use in NIV, similar results are expected.
Remifentanil is a μ-opioid receptor agonist with pharmacodynamic properties similar to those of other opioids, with potent analgesic and light sedative effect, but with a unique pharmacokinetic profile. It is a potent, short-acting opioid with a half-life of 3–4 min, and does not accumulate with prolonged infusion [6]. Its metabolism is unaffected by hepatic or renal dysfunction, since it is metabolized by plasma esterases into an inactive metabolite. Its main adverse effects include nausea, constipation, respiratory depression, and bradycardia. At low dose, remifentanil increases comfort without decreasing respiratory drive, and because it does not accumulate, there are no concerns about unpredictable or delayed recovery, making its use possible even in NIV. In a pilot study, Constantin et al. showed that remifentanil-based sedation as a continuous infusion in selected patients with NIV failure was effective in increasing NIV tolerance and safety [13]. However, in that study, the required level of sedation was not achieved in 3 of the 13 patients with the maximum allowed dose of remifentanil. To avoid high doses of opioids, which decrease respiratory drive, a combination of propofol and remifentanil was used, but PaCO2 increased.
Dexmedetomidine, a highly selective α2-adrenoreceptor agonist that stimulates receptors in the locus ceruleus to provide sedation and in the spinal cord to enhance analgesia. It also has sympatholytic effects via central and peripheral mechanisms [6]. It has mild sedative, anxiolytic, analgesic, and opioid-sparing effects without causing significant respiratory depression and is suitable for short-term sedation in an intensive care setting. Due to it pharmacologic profile, it has been used as a useful sedative in ICU patients. Also, it offers a qualitatively different type of sedation, when compared to propofol and benzodiazepines, since sedation is obtained when patients are undisturbed, but they can be easily aroused with minimal stimulation [4]. The use of dexmedetomidine is associated with hemodynamic adverse effects, causing hypotension and bradycardia. Other adverse effects include dry mouth and nausea [6].
Given the pathophysiology of NIV failure, dexmedetomidine appears to offer the range of qualities best configured to address these concerns, namely it does not interfere with the patency of the upper airway, does not cause respiratory depression, and improves the affective dimension of dyspnea [3]. In comparison, opioids, propofol, and benzodiazepines may decrease upper airway diameter with possible deleterious risk during NIV. Furthermore, dexmedetomidine produces analgesia, another advantage over propofol and benzodiazepines.
In a recent systematic review and meta-analysis [14], on the safety and efficacy of dexmedetomidine in acutely ill patients requiring NIV, 12 randomized controlled trials were included. The use of dexmedetomidine, compared to other sedation strategies or placebo, reduced the risk of endotracheal intubation and mechanical ventilation [relative risk (RR) 0.54, 95% confidence interval (CI) 0.41–0.71], delirium (RR 0.34, 95% CI 0.22–0.54), ICU length of stay [mean difference −2.40 days, 95% CI −3.51 to −1.29], and risk of developing pneumonia (RR 0.30, 95% CI 0.17–0.52), while increasing the risk of bradycardia (RR 2.80, 95% CI 1.92–4.07) and hypotension (RR 1.98, 95% CI 1.32–2.98). The majority of studies allowed dexmedetomidine dosing that ranged from 0.2–0.7 μg/kg/h. There was no difference in duration of NIV with dexmedetomidine compared to other strategies. The authors concluded that the benefits of dexmedetomidine should be weighed against the probable undesirable effects of hypotension and bradycardia.
Ketamine is a short-acting drug with sedative, analgesic, anti-inflammatory, and antidepressant effects properties that are mainly attributed to its activity as an inhibitor of the N-methyl-d-aspartate (NMDA) receptor [15]. It exhibits dissociative effects by perpetuating a dream-like detachment from the environment and has potential for abuse and adverse neuropsychiatric reactions. Ketamine typically exhibits a rapid onset of action; the elimination half-life is approximately 2–3 h and depends on hepatic and renal function. Ketamine does not cause respiratory depression at doses given for analgesia or procedural sedation [3], but has the capacity of causing bronchodilation by increasing circulating catecholamines, inhibiting vagal outflow, and relaxing airway smooth muscle, which could be useful for some types of patients needing NIV. Complications associated with ketamine administration include fatigue, dizziness, nausea, feelings of unreality, hemodynamic effects (increases blood pressure and heart rate), arrhythmias, hypersalivation, emergence reactions, and laryngospasm [15]. There is a relatively abundant literature concerning the use of ketamine for procedural sedation, but experience for sedation during NIV is limited [3].
2.2 Monitoring Sedation and Pain During NIV
Although sedation can play a role in preventing intolerance to NIV, it is also potentially dangerous because of the risk of oversedation, need for intubation and undesired side effects. For that reason their use should be carefully considered. The depressant effects of sedation and analgesia on respiratory function vary between individuals depending on the choice and dose of the drug, its sedative or analgesic effects, and sensitivity and metabolic capabilities of the patient [5]. The incidence and severity of sedative-related complications in patients admitted in ICU are variable and depend on the dosage, type of drug, severity or ARF and expertise of the team [4]. Monitoring sedation during NIV is a key point of a successful procedure. Sedation and analgesia should be administered by experienced staff, with continuous monitoring of cardiorespiratory and ventilator parameters, and prompt capacity of endotracheal intubation if NIV fails. Several scales are available that may be helpful in ensuring a minimal level of sedation for NIV tolerance, which also requires trained staff to be applied [5].
As for all ICU patients, evaluation of sedation and pain should be performed by trained personnel according to a scale. Moreover, sedation for NIV should be included in a sedation protocol in each ICU that includes the recommended scales for evaluation and measures to be applied accordingly to the evaluation. Besides sedation and pain, delirium should also be assessed.
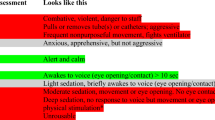
For sedation assessment, the most commonly used scores are Richmond Agitation-Sedation Scale (RASS) and Ramsay Sedation Score (RAS). There is a lack of data comparing the different scales. At least one clinical tool should be used to assess the neurological status of patients under NIV with the aim of obtaining the desired neurological sedative effect for the delivered dose of the chosen drug [4]. In the study of Matsumoto et al., patients were most often managed between −2 and 0 on the RASS during sedation [10].
A patient’s self-report of pain is the reference standard for pain assessment in patients who can communicate reliably [7]. Among critically ill adults who are able to self-report pain, the 0–10 Numeric Rating Scale (NRS) administered either verbally or visually is a valid and feasible pain scale. A descriptive pain scale like the Verbal Descriptor Scale (VDS) should be considered for ICU patients unable to use a numerically formatted scale such as the 0–10 NRS. Among critically ill adults unable to self-report pain and in whom behaviors are observable, the Behavioral Pain Scale in intubated (BPS) and nonintubated (BPS-NI) patients and the Critical-Care Pain Observation Tool (CPOT) demonstrate the greatest validity and reliability for monitoring pain [7]. The BPS-NI was developed for patients with delirium and/or an impaired vigilance status unable to communicate, contains three domains (i.e., facial expressions, movements of upper limbs, vocalization), and each domain contains four descriptors rated on a 1 to 4 scale [16]. Although it was not validated in patients under NIV, it may be useful for patients with this type of respiratory support and unable to self-report.
3 Conclusion
Sedation and analgesia can reduce NIV failure and so decrease morbidity in selected patients. This practice must be performed in an ICU setting with trained individuals and close monitoring. The ideal drug does not exist, but dexmedetomidine and ketamine may be interesting alternatives in experienced units due to their pharmacological profiles. Propofol and opioids (such as remifentanil) are in an intermediate position. The continuous administration of benzodiazepines should be discouraged, but the anxiolytic properties of these drugs may be used in a single-shot administration. A sedation protocol must be implemented in the ICU and scales should be used for assessment.
Key Major Recommendations
-
Sedation and analgesia can reduce NIV failure to avoid endotracheal intubation or when NIV is a “ceiling treatment.”
-
Sedation and analgesia should be administered by experienced staff with close monitoring, and using the minimum doses to avoid oversedation and adverse side effects.
-
Dexmedetomidine appears to offer the best range of qualities, but the benefits should be weighed against the probable undesirable effects of hypotension and bradycardia.
-
Ketamine may be an interesting alternative, but there is a lack of information on efficacy and safety for sedation during NIV.
-
A sedation protocol must be implemented in the ICU and scales should be used for assessment.
Abbreviations
- ARF:
-
Acute respiratory failure
- BPS:
-
Behavioral Pain Scale
- BPS-NI:
-
Behavioral Pain Scale in nonintubated
- CI:
-
Confidence interval
- CPOT:
-
Critical-Care Pain Observation Tool
- ERS/ATS:
-
European Respiratory Society/American Thoracic Society
- GABA:
-
γ-aminobutyric acid
- ICU:
-
Intensive Care Unit
- NIV:
-
Noninvasive ventilation
- NRS:
-
Numeric Rating Scale
- RR:
-
Relative risk
- TCI:
-
Target-controlled infusion
- VDS:
-
Verbal Descriptor Scale
References
Rochwerg B, Brochard L, Elliott MW, et al. Members of the Task Force. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50:1602426.
Scala R, Pisani L. Noninvasive ventilation in acute respiratory failure: which recipe for success? Eur Respir Rev. 2018;27:180029.
Longrois D, Conti G, Mantz J, et al. Sedation in non-invasive ventilation: do we know what to do (and why)? Multidiscip Respir Med. 2014;9:56.
Scala R. Sedation during non-invasive ventilation to treat acute respiratory failure. Shortness Breath. 2013;2(1):35–43.
Conti G, Hill NS, Nava S. Is sedation safe and beneficial in patients receiving NIV? No. Intensive Care Med. 2015;41:1692–5.
Reade MC, Finfer S. Sedation and delirium in the intensive care unit. N Engl J Med. 2014;370(5):444–54.
Devlin JW, Skrobik Y, Gélinas C, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2018;46(9):e825–73.
Devlin JW, Nava S, Fong JJ, et al. Survey of sedation practices during noninvasive positive-pressure ventilation to treat acute respiratory failure. Crit Care Med. 2007;35:2298–302.
Muriel A, Peñuelas O, Frutos-Vivar F, et al. Impact of sedation and analgesia during non-invasive positive pressure ventilation on outcome: a marginal structural model causal analysis. Intensive Care Med. 2015;41(9):1586–600.
Matsumoto T, Tomii K, Tachikawa R. Role of sedation for agitated patients undergoing noninvasive ventilation: clinical practice in a tertiary referral hospital. BMC Pulm Med. 2015;15:71.
Hilbert G, Navalesi P, Girault C. Is sedation safe and beneficial in patients receiving NIV? Yes. Intensive Care Med. 2015;41:1688–91.
Clouzeau B, Bui HN, Vargas F, et al. Target-controlled infusion of propofol for sedation in patients with non-invasive ventilation failure due to low tolerance: a preliminary study. Intensive Care Med. 2010;36(10):1675–80.
Constantin JM, Schneider E, Cayot-Constantin S, et al. Remifentanil-based sedation to treat noninvasive ventilation failure: a preliminary study. Intensive Care Med. 2007;33:82–7.
Lewis K, Piticaru J, Chaudhuri D, et al. Safety and efficacy of dexmedetomidine in acutely ill adults requiring non-invasive ventilation: a systematic review and meta-analysis of randomized trials. Chest. 2021;159(6):2274–88.
Hurth KP, Thomas KB, Rudoni MA. The reemergence of ketamine for treatment in critically ill adults. Crit Care Med. 2020;48(6):899–911.
Chanques G, Payen JF, Mercier G, et al. Assessing pain in non-intubated critically ill patients unable to self report: an adaptation of the behavioral pain scale. Intensive Care Med. 2009;35(12):2060–7.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Silva, C.M. (2023). Sedation and Analgesia During Noninvasive Ventilation in Intensive Care. In: Esquinas, A.M. (eds) Noninvasive Mechanical Ventilation. Springer, Cham. https://doi.org/10.1007/978-3-031-28963-7_63
Download citation
DOI: https://doi.org/10.1007/978-3-031-28963-7_63
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-28962-0
Online ISBN: 978-3-031-28963-7
eBook Packages: MedicineMedicine (R0)