Abstract
Peroxisome proliferative activated receptors (PPARs) act as ligand-activated transcription factors involved in glucose and lipoprotein metabolism, and in inflammation. binding to specific response elements (PPREs) within the nucleus. Heterodimerization with a retinoid X receptor and interaction with coactivators and corepressors occur after binding of natural or synthetic agonists. The first synthetic agonists in clinical use were fibrates for PPAR alpha and thiazolidinediones for PPAR gamma. Dual α γ agonists, pan α γ δ agonists, partial agonists or selective PPAR modulators (SPPARMs) have been evaluated in clinical development in diabetic people with current stage prior or after marketing authorization tabulated.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
The chapter is divided into five sections:
-
1.
PPAR gene and gene variants, proteins and natural ligands
-
2.
Synthetic ligands: from PPAR activators to PPAR agonists
-
3.
The PPAR machinery with subsections on
-
(a)
Coactivators and corepressors
-
(b)
Metabolic modifications (phosphorylation, ubiquitination and sumoylation, acetylation and methylation)
-
(c)
Partial agonists or selective PPAR modulators (SPPARMs)
-
(a)
-
4.
Effect of PPAR agonists in diabetes
-
(a)
Pharmacology, in particular in the pancreas
-
(b)
Effects in type 1 diabetes
-
(c)
Effects in type 2 diabetes and/or dyslipidemia with products reaching clinical development
-
(a)
-
5.
Conclusions and perspectives
PPAR Gene and Gene Variants, Proteins and Natural Ligands
Peroxisome proliferative activated receptors (PPARs) belong to a subfamily of the nuclear receptors which includes the retinoic acid receptors, the thyroid hormone receptors, and the revErbA-related orphan receptors [1]. The PPAR subfamily contains three isoforms, namely PPAR α (PPARA, NR1C1), PPAR β/δ (NR1C2 identified here as PPAR δ) and PPAR γ (PPARG, NR1C3, PPAR γ1 and PPAR γ2 sub-isoforms) that are encoded by different genes on different chromosomes.
In humans, PPAR α is mapped on chromosome 22 on the regions 22q12-q13.1; 22q13.31 with a linkage group of six genes and genetic markers [2]. The human PPAR γ gene is located on chromosome 3 at position 3p25, close to the retinoic acid receptor beta (RAR β) and the thyroid hormone receptor beta genes [3,4,5]. Two different human PPAR γ transcripts are expressed in hematopoietic cells: a 1.85-kb transcript, which corresponds to the full-length mRNA (PPAR γ1), and a shorter 0.65-kb transcript (PPAR γ2) [5]. PPAR γ2 is mostly expressed in adipose tissue where the PPAR γ2/PPAR γ1 ratio of messenger RNA is directly correlated with body mass index and where a low-calorie diet downregulates PPAR γ2 messenger RNA in subcutaneous fat [6]. Several variants in the PPAR γ gene have been identified, with the Pro12Ala variant having been the most extensively examined in epidemiologic studies. A strong association between PPAR γ 12Ala polymorphism and a reduction in type 2 diabetes risk (odds ratio: 0.86, 95% CI: 0.81–0.90) was recently described in an updated meta-analysis of 60 studies involving 32,849 subjects with type 2 diabetes mellitus (T2DM) and 47,456 controls evaluated by the Human Genome Epidemiology Network [7].
The human PPAR δ, which was cloned from a human osteosarcoma cell library, is located on chromosome 6, at position 6p21.1-p21.2 [8]. In the mouse, where the first PPAR, PPAR α was identified in 1990 by Issemann and Green [9], PPAR α is found on chromosome 15, PPAR γ is located on chromosome 6 at position E3-F1, while PPAR δ is found on chromosome 17 [10]. In both human and mouse, PPAR transcript is encoded by six exons (one in the A/B domain, two in the C domain, one for the hinge region and two for the ligand binding domain).
PPAR isoforms share a common domain structure as shown in the schematic view in Fig. 6.1. Five domains designated A/B, C, D, E and F are distinguishable, and each has a different function. The N-terminal A/B domain contains at least one constitutionally active transactivation region (AF-1) and several autonomous transactivation domains (AD) [1]. The specificity of gene transcription is granted by the isoform-specific sequence of the A/B domain of the receptor [11]. Chimeric proteins generated by fusion with the A/B domains of other receptor proteins attenuate the specificity of target gene activation [11]. The DNA-binding domain (DBD, C domain) is the most conserved region, which contains a short motif responsible for DNA-binding specificity (P-box) on sequences called peroxisome proliferator response elements (PPREs), typically containing the AGGTCA motif.
Structure of PPARs. In the upper panel, the structure of PPARs with their four domains: 1 is the NH2 terminal and 468 the COOH terminal for PPAR α. The bottom panel illustrates the relative activation for PPAR α and PPAR γ for major agonists with fenofibrate and rosiglitazone as behaving as specific activators and saroglitazar or pioglitazone with mixed effects
The D domain, called a hinge, permits the change in shape of PPARs. The C terminal E/F domain contains the ligand binding domain (LBD), a large pocket in the shape of the letter Y of polar character and the AF-2 region for binding co-activators and co-repressors. When activated by ligands, PPARs heterodimerize with another nuclear receptor, the retinoid X receptor, and alter the transcription of target genes after binding to specific PPREs on target genes.
Natural ligands for PPARs are long chain fatty acids, saturated or not, such as EPA: eicosapentaenoic acid, DHA docosahexaenoic acid, and eicosanoids: 8-HETE (hydroxyeicosatetraenoic acid), and to some extent leukotriene B4 (LTB4) for PPAR α, 9- and 13-HODE (hydroxyoctadecadienoic acid), two 15 lipoxygenase metabolites of linoleic acid and 15-deoxy PGJ2, for PPAR γ and prostacyclin (PGI2) for PPAR δ [12,13,14]. However, tissue concentrations are probably too low for them being the active ligands [15]. A new candidate endogenous ligand for PPAR α in the liver is a glycerophosphocholine esterified with palmitic and oleic acids 16:0/18:1-GPC or POPC (1-palmitoyl, 2-oleoyl-sn-glycero-3-phosphocholinehydroxyeicosatetraenoic acid) which was identified in the liver of mice by tandem mass spectrometry [16]. This phosphatidylcholine is displaced from PPAR α by the synthetic agonist Wy14643. Its portal infusion induces dependent gene expression of carnitine palmitoyltransferase 1 (CPT1) in wild-type mice, but not in PPAR α deficient mice. Recently, two other phosphatidylcholines, DLPC and DUPC (1,2-dilauroyl-sn-glycero-3-phosphocholine and 1,2-(cis-cis-9,12-octadecadienoyl)-sn-glycero-3-phosphatidylcholine respectively), have been shown to improve glucose control in two mouse models of insulin resistance [17]; however, they did not affect rosiglitazone binding to PPAR γ, and their effects are linked to stimulation of another nuclear receptor liver receptor homologue (LRH)-1.
Synthetic Ligands: From PPAR Activators to PPAR Agonists
PPAR α was first cloned from a mouse liver cDNA library at ICI, the pharmaceutical company which developed clofibrate, the first fibrate [9], and subsequently in humans [2, 18]. Fibrates, which were in clinical use as lipid-lowering agents for 20 years before this discovery, are weak PPAR α agonists, effective on human PPAR in the micromolar range, explaining the observation that they are given in the range of 100–1200 mg/day. Fibrates, such as fenofibrate, mainly act via activation of PPAR α in the liver to regulate genes involved in fatty acid oxidation [19]. They were then called PPAR α activators and their main laboratory effects are to reduce triglycerides and increase high density lipoprotein (HDL) cholesterol levels. The first potent and selective PPAR α agonist acting in the nanomolar range with clinical data was LY518674, the development of which was stopped in 2007 when phase 2 studies showed no advantage over existing fenofibrate [20].
The link between PPAR γ activation and the thiazolidinedione insulin-sensitizing agents pioglitazone and rosiglitazone was established by researchers at Upjohn and Glaxo in 1994 and 1995, respectively [21, 22]. PPAR γ increases adipocyte differentiation and storage of fat. The short-term marker of PPAR γ activation in plasma is an increase in levels of the adipocytokine named adiponectin, which increases insulin sensitivity in liver and muscle [23, 24]. First animal results with PPAR δ agonists L165041 and GW501516 were reported in 1999 by researchers at Merck and in 2001 at Glaxo [25, 26].
The PPAR Machinery
The PPAR machinery is similar to other nuclear receptors with sequential complexes of coactivators and corepressors with enzymatic activities (for review see Rosenfeld 2006) [27] and a series of metabolic transformations that turn PPARs towards activation or direct them to degradation (Fig. 6.2). The role of these different proteins, their metabolic transformations and the concept of selective PPAR modulator are summarized in the next sections. Without ligand, the transcription of DNA into messenger RNA is usually repressed by the binding of corepressors on the heterodimer PPAR-RXR and chromatin is compacted (Fig. 6.3). With the presence of ligand in the ligand binding domain, the structural changes in the AF-2 region permit to replace corepressors by coactivators, to associate remodelling of chromatin by acetylation of histones, in order for RNA polymerase to access the DNA and initiate transcription (Fig. 6.4). One important aspect common to PPAR activation is transrepression of inflammatory genes under the control of nuclear factor kappa B (NFκB) or activated protein (AP) 1. This transrepression is an indirect effect since there is no PPRE in the promoter. This was shown for PPAR γ on induction of tumour necrosis factor (TNF) α by phorbol myristate acetate in human monocytes/macrophages [28], for PPAR α on human aortic smooth muscle cells and interleukin (IL) 1-induced IL6 expression [29, 30] and for PPAR δ with expression of monocyte chemoattractant protein (MCP)-1 [31]. In human endothelial cells, fenofibrate and L165041, but not rosiglitazone, inhibited TNF α-induced monocyte adhesion, Vascular Cell Adhesion Molecule-1 (VCAM-1) expression, and Monocyte Chemotactic Protein-1 (MCP-1) secretion through inhibition of nuclear P65 translocation, necessary for NFκB activation [32].
PPAR network. Upon activation with ligand, PPAR heterodimerizes with RXR α and activate target genes (transactivation). Phosphorylation has opposite effect transactivation for PPAR α or its inhibition for PPAR γ. Sumoylation of PPAR is associated with transrepression which prevents transcription of NFκB or AP-1 dependent inflammatory genes and with a reduction of degradation in the proteasome. CDK5 cyclin dependent kinase 5, ERK MAPK mitogen activated kinase, PKA PKC AMPK protein kinase A or C and AMP activated kinase, NCoR nuclear corepressor, HDAC3 histone deacetylase 3
Corepressor complex: without ligand, PPAR and RXR α are linked to their PPRE direct repeat (AGGTCA) n AGGTT by the DNA binding domain; the corepressors NCoR and SMRT prevent DNA transcription. AF1 AF2 ligand-independent transactivation domains 1 and 2, DBD DNA binding domain, LBD ligand binding domain, Nco R nuclear corepressor, SMRT silencing mediator for retinoid and thyroid hormone
Coactivator complex: with fixation of ligands, conformational changes in ligand binding domain permit replacement of corepressors by coactivators, of which the enzymatic activities, acetylate, phosphorylate or methylate the chromatin allowing access to DNA of RNA polymerase and initiation of transcription into copies of messenger RNA
PPAR Coactivators and Corepressors
The main PPAR coactivator, or at least the best studied one, is peroxisome proliferator-activated receptor γ coactivator 1α (PGC-1α) [33]. Through a number of transcription factors, including PPARs, PGC-1α modulates numerous metabolic pathways in liver, skeletal and cardiac muscle, and adipose tissue, including gluconeogenesis and glycolysis, fatty acid synthesis and oxidation. Indeed, PGC-1α itself is subject to the same modulations as PPAR (see below through phosphorylation, ubiquitination or sumoylation). Other PPAR coactivators are steroid receptor coactivator1 (SRC1) and cyclic adenosine 5′-monophosphate (cAMP) response element binding protein (CBP/P300) which possess histone acetyl transferase activity, leading to the decondensation of chromatin necessary for gene transcription.
The main PPAR corepressors are named as nuclear receptor corepressor (NCoR) and silencing mediator for retinoid and thyroid hormone (SMRT) which are associated with histone deacetylase activity which maintain chromatin in a compact state. The role of NCoR was studied by specifically knocking out its gene in mouse adipocytes (AKO) or muscle (MKO). MKO mice were able to run longer than normal mice [34]. AKO mice had higher insulin sensitivity in liver, muscle and adipose tissue than normal mice, with limited additional effect of rosiglitazone since PPAR γ target genes were already derepressed by NCoR deletion [35]. The effects of rosiglitazone to cause hemodilution were the same in AKO and normal mice. In MKO mice, exercise capacity and mitochondrial oxidation are enhanced by the loss of a transcriptional cofactor in muscle cells through modulation of transcription factors that includes PPAR δ. SMRT is a protein structurally similar to NCoR, which possesses different receptor interaction domains (RID) for different nuclear receptors, called RID2 for PPAR or RXR or RID1 for retinoid acid receptor [36].
Phosphorylation
Phosphorylation of PPAR γ by mitogen activated kinase (MAPK)-extracellular signal related kinase (ERK) 1 at serine 112 inhibits adipogenesis [37]. Phosphorylation of PPAR α on serine residues in the ligand-independent transactivation domain AF1 in response to insulin increases transcription activity through dissociation of corepressors [38]. HMG CoA reductase inhibitors (‘statins’) have been shown to stimulate PPAR α transcription by reducing its phosphorylation in HepG2 cells, a synergistic effect with fenofibric acid [39]. Transcriptional activation of PPAR α by bezafibrate was dose dependently increased by statins in human kidney 293T cells. In addition, concomitant administration of fenofibric acid and pitavastatin decreased the transactivation of NFκB induced by phorbol myristate acetate (PMA) [40]. Data on PPAR δ phosphorylation are limited to the location of predicted consensus phosphorylation sites and inhibition of PPAR δ activation by kinase inhibitors [41].
It was shown that phosphorylation of PPAR γ at Serine-273 by activated CDK5 leads to a loss of transcription of PPAR γ in adipocytes [42]. The cyclin dependent kinase (CDK) 5, which is present in the cytoplasm and the nucleus, is activated by phosphorylation at tyrosine 15 within a high glucose milieu and IL1β, by TNF α or by high fat diet. This finding permitted the same authors to discover new small molecules binding to PPAR γ blocking CDK5 serine 273 phosphorylation, like thiazolidinediones (TZDs), with potent antidiabetic activity in insulin-resistant mice fed a high fat, high sugar diet, without causing fluid retention and weight gain [43]. However, to date no clinical development has been reported blocking CDK5 pathway.
Ubiquitination
Proteins are degraded in the proteasome after fixation on lysine residues of repeated sequences of a small 76AA polypeptide called ubiquitin. In the absence of their ligands, PPARs are rapidly degraded by this process. The degradation of PPAR γ is increased by different TZD ligands [44]; conversely, ubiquitination of PPAR α is reduced transiently with different fibrate ligands [45] and ubiquitination of PPAR δ is markedly reduced by PPAR δ agonists [46].
Sumoylation
Sumoylation is the attachment of another polypeptide of 101 amino acids called SUMO, for small ubiquitin like modifier. Sumoylation at a lysine in the ligand-binding domain of PPAR γ is the mechanism which converts activation of transcription by rosiglitazone into repression of NFκB or activator protein (AP) 1 in murine macrophages. This prevents ubiquitination of NCoR to maintain repression of inflammatory genes such as inducible NO synthase [47]. In adipose tissue, sumoylation of PPAR γ, which reduces the effect of rosiglitazone, is increased in the absence of the hepatokine fibroblast growth factor (FGF) 21 [48].
Similarly, sumoylation at lysine 185 has been identified in the hinge region of PPAR α [49]. To date, a potential sumoylation site for PPAR δ has also been suggested on lysine 185.
Post-translational regulation of PPARs by different patterns of mono- or polyubiquitination, as well as by mono- or polysumoylation, has been reviewed by Wadosky and Willis [50]. This review also reports that the coreceptor RXR α and the coactivators PGC-1α can be ubiquitinated or sumoylated, adding to the complexity of these regulatory processes.
Acetylation
Acetylation and deacetylation of genes are major procesess affecting gene expression through decondensation and recondensation of chromatin. It also affects proteins. The first nuclear receptors shown to be acetylated were the androgen oestrogen receptors; this has not been shown clearly for PPAR [51]. However, their key coactivator PGC-1α is inactivated by acetylation in high energy states or deacetylated by sirtuin 1 in low energy states [52]. The nicotinamide adenine dinucleotide (NAD)-dependent histone deacetylases or sirtuins by interacting with PPARs and their coactivators thus provide a new level of complexity to the regulation of nuclear receptors [53].
Methylation
Methylation of histones is another prominent histone posttranslational modification in response to environmental and pharmacological factors. The methylation of histone lysine residues is a reversible process with interplay between lysine methylation by methyltransferases (KMTs) and demethylation by lysine demethylases (KDMs).
Methylation of PPAR γ promotor decreases PPAR γ in murine 3T3L1 adipocytes [54].
Partial Agonists or SPPARMs
A partial agonist is a ligand that induces a submaximal response even at full receptor occupancy. It can also reduce the full PPAR γ agonist response. For instance, in comparison with rosiglitazone, troglitazone is a full agonist on murine 3T3L1 adipocytes, but a partial agonist in muscle C2C12 myotubes and HEK293T kidney cells [55]. Olefsky proposed to name selective PPAR modulators (SPPARMs); such products differ from full agonists by differential regulation of target genes [56]. SPPARMs are designed to separate efficacy and adverse effect dose–response curves. This concept was already developed in nuclear receptor pharmacology, with selective oestrogen receptor modulators (SERMs), such as tamoxifen or raloxifene, which recruit corepressors such as NCoR to the AF2 region, whereas oestradiol recruits coactivators such as the glucocorticoid receptor interacting protein 1 (GRIP1) [57] or with selective vitamin D modulators such as paricalcitol with differential recruitment of coactivators than calcitriol, the active form of vitamin D [58].
Pemafibrate has been described as a SPPARM α due to different binding to PPAR α ligand binding domain and recruitment of coactivators/corepressors than fenofibrate [59]. Pemafibrate was first approved in Japan with the same indications than fenofibrate in hyperlipidemia. A large-scale intervention study PROMINENT has recruited 10391 participants with T2DM and dyslipidemia [60] to assess the reduction in cardiovascular events. Results were expected at the end of 2022 but the study was discontinued for futility in April 2022.
Increasing concentrations or doses with full PPAR γ agonists lead to greater efficacy, but greater adverse events, such as weight gain and volume expansion.
PPAR γ partial agonists such as balaglitazone or INT131 displace a full agonist such as rosiglitazone. Metaglidasen, the (−) stereoisomer of halofenate, tested as racemate in the 90s as a lipid lowering agent, is another selective partial PPAR γ modulator and was in clinical development for its uricosuric activity. Partial agonists bind the same pocket as TZDs, which is required to block PPAR γ phosphorylation, but induce different conformational changes in PPAR γ, leading to different recruitment of coactivator/corepressor. As an example, INT131 induces less recruitment of DRIP205 (vitamin D-interacting protein 205), a coactivator involved in lipid accumulation than rosiglitazone or pioglitazone in HEK cells [61]. The same finding was reported with fibrates: gemfibrozil induced less recruitment of DRIP205 than fenofibrate and behaves as a partial agonist to increase apoA-I activation. This translated in a comparative trial in dyslipidemic patients to a larger increase in ApoA-I, a protective apoprotein in HDL, with fenofibrate than with gemfibrozil [62].
Effects of PPAR Agonists in Diabetes
This review is limited to PPAR activators or agonists which are marketed or remain in clinical development in diabetes and/or dyslipidemia (Table 6.1). Several PPAR antagonists were synthesized but they were not developed for the treatment of diabetes [63]. GW6471, a potent PPAR α antagonist, is mostly used as a pharmacological agent to test whether an effect is PPAR dependent or PPAR independent. GW9662 is a PPAR γ antagonist which promotes the recruitment of NCoR. Finally, GSK0660 and GSK3787 are PPAR δ antagonists for pharmacological use which compete with the binding of full agonists. However, GSK0660 when used alone behaves as an inverse agonist activity to inhibit the TNF α-induced expression of multiple chemokines in human retinal microvascular endothelial cells [64, 65].
The organs implicated in glucose control are listed in Table 6.2. With their direct effects on gene expression and their indirect effects on inflammation, and according to their tissue distribution, PPARs affect most of these organs, beyond the liver for PPAR α, the adipose tissue for PPAR γ and the skeletal muscle for PPAR δ. In the kidney, they have different locations: PPAR α is located mainly in the proximal tubule, the medullary thick ascending limb and in the mesangium; PPAR γ in the distal medullary collecting duct and glomeruli; and PPAR δ in a diffuse fashion as in other organs [66]. In the brain, the interplay of PPAR subtypes has been shown in cultures of astrocytes, where the three subtypes are present. PPAR α (fenofibrate), PPAR δ (GW501516) and PPAR γ (rosiglitazone) agonists and their respective antagonists (GW6471, GSK0660 and GW9662) decreased the release of the proinflammatory cytokine, TNF α in rat astrocytes stimulated by lipopolysaccharide (LPS) [67]. Combined application of PPAR γ and PPAR δ activators increased cyclooxygenase 2 expression induced by LPS, whereas the additional application of a PPAR α agonist abolished this effect [68].
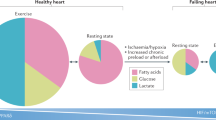
In the pancreas, the three PPARs are expressed in pancreatic β cells. PPAR α modulates fatty acid oxidation, and PPAR γ directs them toward esterification. Although PPAR δ is the most abundant PPAR in the pancreas at the mRNA and the protein level, until recently its effects on fatty acid oxidation have been less well-studied [69]. PPAR δ activation increases fatty acid oxidation and to a larger extent than PPAR α activation. In the pancreas, fatty acids acutely potentiate glucose-stimulated insulin secretion (GSIS) but their chronic exposure elevates basal insulin secretion and alters GSIS, a phenomenon called lipotoxicity.
Discordant results are reported in the literature with PPAR α or PPAR γ agonists. PPAR α was described to potentiate and PPAR γ to attenuate GSIS in INS-1E cells, an immortalized insulinoma rat cell line [70]. On the contrary, in vivo, the PPAR α agonist fenofibrate impaired GSIS in neonatal rats receiving monosodium glutamate to induce obesity, while pioglitazone, a PPAR γ agonist, increased it in db/db mice [71, 72]. This discordance might be explained by the low expression level of PPAR γ in INS-1E cells.
Reduced amounts of sulfatide, 23% of the levels in control participants, in pancreatic islets of individuals with newly diagnosed type 1 diabetes, have been associated with reduced expression of enzymes involved in sphingolipid metabolism. Fenofibrate, which activates sulfatide biosynthesis, completely prevented diabetes in NOD mice [73]. Fenofibrate treatment initiated 7 days after diagnosis eliminated the need for insulin therapy in a 19-year-old girl newly diagnosed type 1 diabetes [74].
Activation of PPAR δ by unsaturated FAs or a synthetic ligand enhanced GSIS in primary rat islets or INS-1E cells without affecting basal insulin secretion [69]. In order to maintain β cell function, PPAR δ would play a role of lipid sensor to adjust the mitochondrial fatty acid oxidation. It was recently suggested that 4-hydroxy-nonenal (4-HNE) was one endogenous activating ligand of PPAR δ [75]. The level of reactive oxygen species (ROS), such as 4-HNE, is essential to β cell function, as low-0level ROS production increases glucose-induced insulin secretion, whereas high levels of ROS can induce β cell apoptosis.
GSIS is also linked to influx of calcium ions to the cytosol induced by depolarization from the voltage-dependent Ca2+ channel. In INS-1 cells, the sarco-endoplasmic reticulum Ca2+ ATPase (SERCA2) pump maintains intracellular Ca2+ homeostasis, in particular a high Ca2+ level in the endoplasmic reticulum. The expression of this pump is decreased in animal models of diabetes and in diabetic human islets. Pioglitazone directly increases expression of SERCA2 through transcription of the gene and indirectly through prevention of CDK5-induced phosphorylation of PPAR γ [76]. This experiment suggests that blocking CDK5 could permit to dissociate positive effects on glucose homeostasis from other effects from PPAR γ agonists.
Effects of PPAR Agonists in Type 1 Diabetes
Clinical studies with PPAR agonists in type 1 diabetes (T1DM) are limited to their effects on lipid or glucose markers. One placebo-controlled randomized study was conducted with fenofibrate in 44 patients with T1DM to assess its effect alone or in combination with vitamin E for 8 weeks on in vitro copper-induced oxidation of LDL and VLDL particles [77]. The lag time of oxidation was significantly prolonged by fenofibrate 200 mg + vitamin E 400 IU. A placebo-controlled randomized study is evaluating the effects of fenofibrate on progression of diabetic retinopathy in 450 adults with T1DM (http://clinicaltrials.gov/ct2/show/NCT01320345) [78].
The lipid-modifying effects of bezafibrate in T1DM were evaluated in earlier placebo-controlled studies [79, 80]. Of note, this fibrate, now considered as an archetype pan-PPAR agonist in transactivation assays, did not improve HbA1c after 3 months of treatment [40, 81].
Three placebo-controlled randomized studies have been reported with TZDs in T1DM patients on insulin therapy, with modest insulin-sparing effects as compared to those observed in type 2 diabetes mellitus (T2DM). In 50 overweight adults with T1DM, an 8-month intervention to achieve glycated haemoglobin level of 7.0% required an 11% increase in the daily dose of insulin in the placebo group, but no change in the rosiglitazone group [82]. In 36 T1DM adolescents aged 10–18 years, the dose of insulin was increased 9% with placebo and reduced by 6% with rosiglitazone after 6 months of treatment, with HbA1c remaining stable around 8.5% [83]. In 60 lean T1DM patients aged 14 years or more, 6 months treatment with pioglitazone was associated with a significant decrease in HbA1c (0.2%) and in postprandial glucose levels (0.7 mmol/L) in the intervention group only, with no changes in insulin doses [84]. In patients with slowly progressive T1DM, diagnosed by the presence of glutamic acid decarboxylase (GAD) antibodies, an insulin-requiring state defined by HbA1c and post glucose C-peptide levels was reached at 4 years in 4/4 subjects randomized to pioglitazone as compared to 1/5 subjects randomized to metformin [85]. Thus, the effects of TZDs in T1DM sharply differ from those reported for T2DM prevention with troglitazone in TRIPOD [86], rosiglitazone in DREAM [87], and pioglitazone in ACT-NOW where development of T2DM in patients with impaired glucose tolerance over 2.4 years decreased from 19.7% with placebo to 7.0% with pioglitazone [88].
Effects of PPAR Agonists in Type 2 Diabetes and Dyslipidemia
For the treatment of T2DM, the first TZD PPAR γ agonist troglitazone was introduced in the US in October 1997 and was withdrawn in March 2000 for hepatic toxicity. Rosiglitazone and pioglitazone were introduced in the US in 1999 and in Europe in 2000. In Japan, pioglitazone was introduced in 1999 and rosiglitazone in 2003. The effects of pioglitazone on macrovascular events in 5238 T2DM patients were reported in 2005 [89]. Although the study primary endpoint was not reached, there was a significant 16% reduction in the main secondary endpoint, which included death from any cause, acute non-fatal myocardial infarction or stroke. The effect of TZDs on diabetes control and the controversy about their hazard on cardiovascular events have been the subjects of numerous reviews in the early 2010s [90,91,92].
The first PPAR α/γ dual agonist muraglitazar was submitted for treatment of diabetes to the Food and Drug Administration (FDA) for registration but the file was withdrawn in May 2006 after a combined analysis of clinical studies indicated an increased cardiovascular risk [93]. Such an increase in cardiovascular risk led to the suspension of registration of rosiglitazone in Europe in September 2010 and severe limitations to its use in the US. Finally, in June 2011, pioglitazone was withdrawn from some European markets due to increased risk of bladder tumours, a decision not endorsed by the European Medicines Agency.
Discontinuation of the development of PPAR agonists occurred for multiple reasons: toxicity of the compound (vascular or bladder tumours in rodents with MK767 or ragaglitazar, respectively), long duration of development, clinical adverse events, expectation not to be better than existing drugs, and stopping development efforts in the cardiometabolic domain. In particular, the FDA requested in July 2004 that 2-year rodent carcinogenicity studies be completed and reviewed before proceeding to phase 3 studies of more than 6-months duration. This decision was made after the evaluation of carcinogenicity in rodents for 11 PPAR agonists, with the observation of haemangioma/haemangiocarcinoma with 8/11 compounds and urinary bladder/renal pelvic transitional cell carcinomas with 5/6 PPAR α/γ dual agonists and pioglitazone (www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM071624.pdf) [94]. In addition, the FDA requested in December 2008 that new antidiabetic agents had to demonstrate through randomized, prospective clinical trials that they do not increase risk for cardiovascular events (www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM071627.pdf) [95]. The thiazolidinedione intervention with vitamin D evaluation (TIDE) study, a large intervention study to assess the effect of the existing TZDs pioglitazone and rosiglitazone on cardiovascular events, planned in 16000 T2DM patients at risk of CVD events was initiated in 2009 but stopped by the FDA 1 year later leaving uncertainty about the risks and benefits from TZDs (TIDE 2012) [96]. The authors stated that, had this study been initiated earlier, it would have provided clear evidence regarding the efficacy and safety of rosiglitazone and pioglitazone. Evaluation of pioglitazone was continued in T2DM patients on metformin in comparison with sulfonylureas (TOSCA-IT) [97] and in insulin resistant patients after a stroke or transient ischemic attack (IRIS) [98]. To date, pioglitazone remains a unique agent to improve insulin sensitivity.
Currently the number of PPAR agonists in phase 2 or phase 3 of clinical development in diabetes and/or dyslipidemia has been markedly reduced as compared to the mid-2010s (Table 6.3).
Two PPAR α agonists have reached the market for treatment of dyslipidemia: pemafibrate K877 from Kowa in Japan and saroglitazar ZYH1 from Zydus in India, the later having a PPAR γ component [103]. The PPAR γ SPPARMs balaglitazone, now discontinued in development, and INT131 appear to be as effective as pioglitazone on HbA1c levels but caused less weight gain in 6-month trials [99, 104]. Indeed, glitazones are chiral drugs marketed as racemates where the S stereoisomer possesses the PPAR γ activity and the R stereoisomer inhibits mitochondrial pyruvate transport while maintaining insulin sensitizing properties. Two PPAR γ derivatives from pioglitazone, R pioglitazone deuterated (PXL065) [105] and azemiglitazone (MSDC0602) [106], described as mitochondrial membrane transport protein modulators, reproduce part of the effect of pioglitazone without its adverse effects. Hydroxypioglitazone (leriglitazone MIN102) has increased brain entry which could be of benefit to improve mitochondrial function in neurodegenerative diseases [107].
Clinical studies with the first PPAR δ activators have been limited to short-term mechanistic studies. In moderately obese volunteer subjects with dyslipidemia, GW501516 10 mg once daily (od) for 2 weeks reduced fasting and postprandial TG levels by 30%, liver fat measured by magnetic resonance imaging by 20%, and urinary isoprostane levels, a marker of oxidative stress, by 30%. In a skeletal muscle biopsy of the thigh, the expression of carnitine palmitoyltransferase 1b, which permits fatty acid to enter the mitochondria, was increased suggesting increased fat oxidation [108]. In a randomized, placebo-controlled, cross-over trial 13 obese dyslipidemic subjects received GW501516 2.5 mg od for 6 weeks. The GW501516 reduced apo CIII production, increased VLDL-apoB catabolism, and increased apoA-II production and HDL-C levels [109]. MBX8025, another specific PPAR δ agonist, was recently reported to reduce TG and increase HDL-C levels alone or in combination with a statin in 181 dyslipidemic patients treated for 8 weeks [100].
Initially, the most studied PPAR dual agonist was aleglitazar, an α/γ agonist with a large intervention study ALECARDIO in 7226 T2DM patients after a recent acute coronary syndrome randomized to aleglitazar 150μg or placebo [110]. The study was terminated after a median 2 years of follow-up for lack of efficacy on the primary endpoint combining cardiovascular death, non-fatal myocardial infarction and non-fatal stroke and increased risk of hospitalization for heart failure. However, this risk was only present in those treated with the antiplatelet agent clopidogrel due to previously unknown pharmacokinetic interaction [111]. In addition, aleglitazar compared with placebo caused a larger reduction in HbA1c and haemoglobin and a larger increase in serum creatinine and adiponectin in patients who were concomitantly using clopidogrel versus patients who were not. Another PPAR α/γ dual agonist, lobeglitazone or CKD-501, has been marketed in Korea with a 6-month comparative trial with pioglitazone [112].
The first pan-PPAR agonist advanced to phase 2 was GW677954 or sodelglitazar which was discontinued from clinical development due to safety concerns. Chiglitazar is another pan-PPAR agonist with full gamma and partial alpha and delta agonist activities in preregistration in China [102]. Lanifibranor is described as a moderately potent and well-balanced modulator of the three PPARs isoforms with partial PPAR γ agonist activity [113, 114].
The development of these new agents, initially evaluated in T2DM or dyslipidemia, has moved recently after the results obtained in a pilot study with pioglitazone in patients with impaired glucose tolerance or T2DM and liver biopsy-confirmed nonalcoholic steatohepatitis (NASH) [115]. The presence of T2DM in patients with metabolic-associated fatty liver disease increases the risk of disease progression to NASH and advanced fibrosis.
Reduction in fibrosis score with pioglitazone 4 mg compared with placebo was shown in a 18-month study in 101 patients with prediabetes or T2DM and biopsy-proven NASH [116]. Phase II studies with pioglitazone derivatives are underway with pioglitazone deuterated PXL065 (NCT04321343) or completed with azemiglitazone in NASH patients with or without diabetes [105]. The expected endpoint in long-term phase III, reduction in NASH score without worsening of fibrosis, is felt more likely to occur in diabetic patients in the azemiglitazone study in the planning stage in 1800 patients (NCT03970031). Elafibranor (GFT505) is a PPAR α/δ agonist with an initial 3-month study in T2DM [101]. After positive results in phase II studies with elafibranor, the dual PPAR α/δ agonist [117], in the interim analysis of the phase III RESOLVE-IT, the response rate in the 717 patients enrolled on study drug was 19.2% for patients who received elafibranor 120 mg compared to 14.7% for patients in the placebo arm. With the pan PPAR agonist lanifibranor, the primary endpoint of the phase II trial NATIVE was reduced in the combined inflammation and ballooning score, with no worsening of fibrosis after 6 months in 247 participants with similar effects in those with and without T2DM [118].
Conclusion and Perspectives
The pharmacology of PPARs, one family of nuclear receptors, is extremely complex as it regulates energy stores in major organs through modulation of genes in lipid and carbohydrate metabolism as well as adaptation to stress, fasting and feeding. The natural ligands for PPARs are fatty acids and prostaglandins. Their first synthetic ligands are fibrates for PPAR α, thiazolidinediones for PPAR γ, few PPAR δ agonists and then dual and pan-PPAR agonists. Most of these well-designed products have been discontinued from clinical development for various reasons from animal toxicity, clinical safety, to no advantage over existing drugs or hurdles to substantiate it. When compared with the initial version of this chapter in 2014 only three products have been marketed. Currently, the most advanced new PPAR agonist is pemafibrate, a PPAR α agonist, which is being evaluated for the prevention of cardiovascular events in people with type 2 diabetes and dyslipidemia. The prevention and treatment of microvascular events such as diabetic retinopathy, as shown with fenofibrate, now in clinical use for almost 50 years, should represent another area of research for new products. The anti-inflammatory effects of PPAR agonists have been well documented in animal experiments, although their potential in human disease is yet to be demonstrated. Dual PPAR α/γ and pan PPAR agonists may offer additional protection in diabetes and metabolic-associated fatty liver disease such as NASH. The search for natural PPAR ligands has been encouraged by the discovery that phosphatidylcholine derivatives can activate PPAR α and should continue for other.
References
Desvergne B, Wahli W. Peroxisome proliferator-activated receptors: nuclear control of metabolism. Endocr Rev. 1999;20:649–88.
Sher T, Yi HF, McBride OW, Gonzalez FJ. cDNA cloning, chromosomal mapping and functional characterization of the human peroxisome proliferator activated receptor. Biochemistry. 1993;32:5598–604.
Lazar MA, Chin WW. Nuclear thyroid hormone receptors. J Clin Invest. 1990;86:1777–82.
Mattei MG, Rivière M, Krust A, Ingvarsson S, Vennström B, Islam MQ, et al. Chromosomal assignment of retinoic acid receptor (RAR) genes in the human, mouse, and rat genomes. Genomics. 1991;10:1061–9.
Greene ME, Blumberg B, McBride OW, Yi HF, Kronquist K, Kwan K, Hsieh L, Greene G, Nimer SD. Isolation of the human peroxisome proliferator activated receptor gamma cDNA: expression in hematopoietic cells and chromosomal mapping. Gene Expr. 1995;4:281–99.
Vidal-Puig AJ, Considine RV, Jimenez-Linan M, Werman A, Pories WJ, Caro JF, Flier JS. Peroxisome proliferator-activated receptor gene expression in human tissues. J Clin Invest. 1997;99:2416–22.
Gouda HN, Sagoo GS, Harding AH, Yates J, Sandhu MS, Higgins JP. The association between the peroxisome proliferator-activated receptor-gamma2 (PPARG2) Pro12Ala gene variant and type 2 diabetes mellitus: a HuGE review and meta-analysis. Am J Epidemiol. 2010;171:645–55.
Schmidt A, Endo N, Rutledge SJ, Vogel R, Shinar D, Rodan GA. Identification of a new member of the steroid hormone receptor superfamily that is activated by a peroxisome proliferator and fatty acids. Mol Endocrinol. 1992;6:1634–41.
Issemann I, Green S. Activation of a member of the steroid hormone receptor superfamily by peroxisome proliferators. Nature. 1990;347:645–50.
Youssef J, Badr M. Role of peroxisome proliferator-activated receptors in inflammation control. J Biomed Biotechnol. 2004;3:156–66.
Hummasti S, Tontonoz P. The peroxisome proliferator-activated receptor N-terminal domain controls isotype-selective gene expression and adipogenesis. Mol Endocrinol. 2006;20:1261–75.
Devchand P, Keller H, Peters H, Vasquze M, Gonzalez F, Wahli W. The PPAR alpha-leukotriene B4 pathway to inflammation control. Nature. 1996;384:39–43.
Kliewer SA, Sundseth SS, Jones SA, Brown PJ, Wisely GB, Koble CS. Fatty acids and eicosanoids regulate gene expression through direct interactions with peroxisome proliferator-activated receptors α and γ. Proc Natl Acad Sci U S A. 1997;94:4318–23.
Forman BM, Chen J, Evans RM. Hypolipidemic drugs, polyunsaturated fatty acids, and eicosanoids are ligands for peroxisome proliferator-activated receptors α and δ. Proc Natl Acad Sci U S A. 1997;94:4312–7.
Willson TM, Brown PJ, Sternbach DD, Henke BR. The PPARs: from orphan receptors to drug discovery. J Med Chem. 2000;43:527–50.
Chakravarthy MV, Lodhi IJ, Yin L, Malapaka RV, Xu HE, Turk J, Semenkovich CF. Identification of a physiologically relevant endogenous ligand for PPAR α in liver. Cell. 2009;138:476–88.
Lee JM, Lee YK, Mamrosh JL, Busby SA, Griffin PR, Pathak MC, et al. A nuclear-receptor-dependent phosphatidylcholine pathway with antidiabetic effects. Nature. 2011;474:506–12.
Mukherjee R, Jow L, Noonan D, McDonnell DP. Human and rat peroxisome proliferator activated receptors (PPARs) demonstrate similar tissue distribution but different responsiveness to PPAR activators. J Steroid Biochem Mol Biol. 1994;51:157–66.
Schoonjans K, Staels B, Auwerx J. The peroxisome proliferator activated receptors (PPARs) and their effects on lipid metabolism and adipocyte differentiation. Biochim Biophys Acta. 1996;1302:93–109.
Nissen SE, Nicholls SJ, Wolski K, Howey DC, McErlean E, Wang MD, et al. Effects of a potent and selective PPAR-alpha agonist in patients with atherogenic dyslipidemia or hypercholesterolemia: two randomized controlled trials. JAMA. 2007;297:1362–73.
Harris PK, Kletzien RF. Localization of a pioglitazone response element in the adipocyte fatty acid-binding protein gene. Mol Pharmacol. 1994;45:439–45.
Lehmann JM, Moore LB, Smith-Oliver TA, Wilkison WO, Willson TM, Kliewer SA. An antidiabetic thiazolidinedione is a high affinity ligand for peroxisome proliferator-activated receptor gamma (PPAR gamma). J Biol Chem. 1995;270:12953–6.
Matsuzawa Y, Funahashi T, Nakamura T. Molecular mechanism of metabolic syndrome X: contribution of adipocytokines adipocytes-derived bioactive substances. Ann N Y Acad Sci. 1999;892:146–54.
Wagner JA, Wright EC, Ennis MM, Prince M, Kochan J, Nunez DJ, et al. Utility of adiponectin as a biomarker predictive of glycemic efficacy is demonstrated by collaborative pooling of data from clinical trials conducted by multiple sponsors. Clin Pharmacol Ther. 2009;86:619–25.
Berger J, Leibowitz MD, Doebber TW, Elbrecht A, Zhang B, Zhou G, et al. Novel peroxisome proliferator-activated receptor (PPAR) γ and PPAR δ ligands produce distinct biological effects. J Biol Chem. 1999;274:6718–25.
Oliver WR, Shenk JL, Snaith MR, Russell CS, Plunket KD, Bodkin NL, et al. A selective peroxisome proliferator-activated receptor δ agonist promotes reverse cholesterol transport. Proc Natl Acad Sci U S A. 2001;98:5306–11.
Rosenfeld MG, Lunyak VV, Glass CK. Sensors and signals: a coactivator/corepressor/epigenetic code for integrating signal-dependent programs of transcriptional response. Genes Dev. 2006;20:1405–28.
Jiang C, Ting AT, Seed B. PPAR-γ agonists inhibit production of monocyte inflammatory cytokines. Nature. 1998;391:82–6.
Staels B, Koenig W, Habib A, Merval R, Lebret M, Torra IP, et al. Activation of human aortic smooth-muscle cells is inhibited by PPARalpha but not by PPAR gamma activators. Nature. 1998;393:790–3.
Delerive P, De Bosscher K, Besnard S, Vanden Berghe W, Peters JM, Gonzalez FJ, et al. Peroxisome proliferator-activated receptor alpha negatively regulates the vascular inflammatory gene response by negative cross-talk with transcription factors NF-kappa B and AP-1. J Biol Chem. 1999;274:32048–54.
Lee C-H, Chawla A, Urbiztondo N, Liao D, Boisvert WA, Evans RM. Transcriptional repression of atherogenic inflammation: modulation by PPAR delta. Science. 2003;302:453–7.
Rival Y, Benéteau N, Taillandier T, Pezet M, Dupont-Passelaigue E, Patoiseau JF, et al. PPARalpha and PPARdelta activators inhibit cytokine-induced nuclear translocation of NF-kappaB and expression of VCAM-1 in EAhy926 endothelial cells. Eur J Pharmacol. 2002;435:143–51.
Fernandez-Marcos PJ, Auwerx J. Regulation of PGC-1α, a nodal regulator of mitochondrial biogenesis. Am J Clin Nutr. 2011;93:884S–90.
Yamamoto H, Williams EG, Mouchiroud L, Cantó C, Fan W, Downes M, et al. NCoR1 is a conserved physiological modulator of muscle mass and oxidative function. Cell. 2011;147:827–39.
Li P, Fan W, Xu J, Lu M, Yamamoto H, Auwerx J. Adipocyte NCoR knockout decreases PPARγ phosphorylation and enhances PPARγ activity and insulin sensitivity. Cell. 2011;147:815–26.
Reilly SM, Bhargava P, Liu S, Gangl MR, Gorgun C, Nofsinger RR, et al. Nuclear receptor corepressor SMRT regulates mitochondrial oxidative metabolism and mediates aging-related metabolic deterioration. Cell Metab. 2010;12:643–53.
Hu E, Kim JB, Sarraf P, Spiegelman BM. Inhibition of adipogenesis through MAP kinase-mediated phosphorylation of PPAR gamma. Science. 1996;274:2100–3.
Juge-Aubry CE, Hammar E, Siegrist-Kaiser C, Pernin A, Takeshita A, Chin WW, et al. Regulation of the transcriptional activity of the peroxisome proliferator-activated receptor alpha by phosphorylation of a ligand-independent trans-activating domain. J Biol Chem. 1999;274:10505–10.
Martin G, Duez H, Blanquart C, Berezowski V, Poulain P, Fruchart JC, et al. Statin-induced inhibition of the Rho-signaling pathway activates PPARalpha and induces HDL apoA-I. J Clin Invest. 2001;107:1423–32.
Inoue I, Itoh F, Aoyagi S, Tazawa S, Kusama H, Akahane M, Mastunaga T, et al. Fibrate and statin synergistically increase the transcriptional activities of PPARα/RXRα and decrease the transactivation of NFκB. Biochem Biophys Res Commun. 2002;290:131–9.
Burns KA, Vanden Heuvel JP. Modulation of PPAR activity via phosphorylation. Biochim Biophys Acta. 2007;1771:952–60.
Choi JH, Banks AS, Estall J, Kajimura S, Bostrom P, Laznik D, et al. Anti-diabetic drugs inhibit obesity-linked phosphorylation of PPARγ by Cdk5. Nature. 2010;466:451–7.
Choi JH, Banks AS, Kamenecka TM, Busby SA, Chalmers MJ, Kumar N, et al. Antidiabetic actions of a non-agonist PPARγ ligand blocking Cdk5-mediated phosphorylation. Nature. 2011;477:477–81.
Hauser S, Adelmant G, Sarraf P, Wright HM, Mueller E, Spiegelman BM. Degradation of the peroxisome proliferator-activated receptor gamma is linked to ligand-dependent activation. J Biol Chem. 2000;275:18527–33.
Blanquart C, Barbier O, Fruchart JC, Staels B, Glineur C. Peroxisome proliferator-activated receptor alpha (PPARalpha) turnover by the ubiquitin-proteasome system controls the ligand-induced expression level of its target genes. J Biol Chem. 2002;277:37254–9.
Genini D, Catapano CV. Block of nuclear receptor ubiquitination. A mechanism of ligand-dependent control of peroxisome proliferator-activated receptor δ activity. J Biol Chem. 2007;282:11776–85.
Pascual G, Fong AL, Ogawa S, Gamliel A, Li AC, Perissi V, et al. A SUMOylation-dependent pathway mediates transrepression of inflammatory response genes by PPAR-gamma. Nature. 2005;437:759–63.
Dutchak PA, Katafuchi T, Bookout AL, Choi JL, Yu RT, Mangelsdorf DJ, Kliewer SA. Fibroblast growth factor-21 regulates PPAR γ activity and the antidiabetic actions of thiazolidinediones. Cell. 2012;148:556–67.
Pourcet B, Pineda-Torra I, Derudas B, Staels B, Glineur C. SUMOylation of human peroxisome proliferator-activated receptor alpha inhibits its trans-activity through the recruitment of the nuclear corepressor NCoR. J Biol Chem. 2010;285:5983–92.
Wadosky KM, Willis MS. The story so far: post translational regulation of peroxisome proliferator-activated receptors by ubiquitination and SUMOylation. Am J Physiol Heart Circ Physiol. 2011;302:H515–26.
Wang C, Powell MJ, Popov VM, Pestell RG. Acetylation in nuclear receptor signalling and the role of sirtuins. Mol Endocrinol. 2008;22:539–45.
Lerin C, Rodgers JT, Kalume DE, Kim SH, Pandey A, Puigserver P. GCN5 acetyltransferase complex controls glucose metabolism through transcriptional repression of PGC-1alpha. Cell Metab. 2006;3:429–38.
Finkel T, Deng CX, Mostoslavsy P. Recent progress in the biology and physiology of sirtuins. Nature. 2009;460:587–91.
Fujiki K, Kano F, Shiota K, Murata M. Expression of the peroxisome proliferator activated receptor γ gene is repressed by DNA methylation in visceral adipose tissue of mouse models of diabetes. BMC Biol. 2009;7:38.
Camp HS, Li O, Wise SC, Hong YH, Frankowski CL, Shen X, et al. Differential activation of peroxisome proliferator-activated receptor-[gamma] by troglitazone and rosiglitazone. Diabetes. 2000;49:539–47.
Olefsky JM. Treatment of insulin resistance with peroxisome proliferator-activated receptor gamma agonists. J Clin Invest. 2000;106:467–72.
Shang Y, Hu X, DiRenzo J, Lazar MA, Brow M. Cofactor dynamics and sufficiency in estrogen receptor-regulated transcription. Cell. 2000;103:843–52.
Issa LL, Leong GM, Sutherland RL, Eisman JA. Vitamin D analogue-specific recruitment of vitamin D receptor coactivators. J Bone Miner Res. 2002;17:879–90.
Kawasaki M, Kambe A, Yamamoto Y, Arulmozhiraja S, Ito S, Nakagawa Y, Tokiwa H, Nakano S, Shimano H. Elucidation of molecular mechanism of a selective PPARα modulator, pemafibrate, through combinational approaches of X-ray crystallography, thermodynamic analysis, and first-principle calculations. Int J Mol Sci. 2020;21:361.
Pradhan AD, Paynter NP, Everett BM, Glynn RJ, Amarenco P, Eam M, Ginsberg H, Hiatt WR, Ishibashi S, Koenig W, Nordestgaard BG, Fruchart JC, Libby P, Ridker PM. Rationale and design of the pemafibrate to reduce cardiovascular outcomes by reducing triglycerides in patients with diabetes (PROMINENT) study. Am Heart J. 2018;206:80–93.
Higgins LS, Mantzoros CS. The development of INT131 as a selective PPAR γ modulator: approach to a safer insulin sensitizer. PPAR Res. 2008;2008:936906.
Duez H, Lefebvre B, Poulain P, Pineda Torra I, Percevault F, Luc G, et al. Regulation of human ApoA-I by gemfibrozil and fenofibrate through selective peroxisome proliferator-activated receptor α modulation. Arterioscler Thromb Vasc Biol. 2005;25:1–7.
Pirat C, Farce A, Lebegue N, Renault N, Furman C, Millet R, et al. Targeting peroxisome proliferator-activated receptors (PPARs): development of modulators. J Med Chem. 2012;55:4027–61.
Savage SR, McCollum GW, Yang R, Penn JS. RNA-seq identifies a role for the PPAR beta/delta inverse agonist GSK0660 in the regulation of TNFalpha-induced cytokine signaling in retinal endothelial cells. Mol Vis. 2015;21:568–76.
Capozzi ME, Savage SR, McCollum GW, Hammer SS, Ramos CJ, Yang R, Bretz CA, Penn JS. The peroxisome proliferator-activated receptor-β/δ antagonist GSK0660 mitigates retinal cell inflammation and leukostasis. Exp Eye Res. 2020;190:107885.
Guan Y, Breyer MD. Peroxisome proliferator-activated receptors (PPARs): novel therapeutic target in renal disease. Kidney Int. 2001;60:14–30.
Chistyakov DV, Astakhova AA, Goriainov SV, Sergeeva MG. Comparison of PPAR ligands as modulators of resolution of inflammation, via their influence on cytokines and oxylipins release in astrocytes. Int J Mol Sci. 2020;21:9577.
Aleshin S, Grabeklis S, Hanck T, Sergeeva M, Reiser G. Peroxisome proliferator-activated receptor (PPAR)-gamma positively controls and PPAR-alpha negatively controls cyclooxygenase-2 expression in rat brain astrocytes through a convergence on PPAR beta/delta via mutual control of PPAR expression levels. Mol Pharmacol. 2009;76:414–24.
Ravnskjaer K, Frigerio F, Boergesen M, Nielsen T, Maechler P, Mandrup S. PPAR delta is a fatty acid sensor that enhances mitochondrial oxidation in insulin-secreting cells and protects against fatty acid-induced dysfunction. J Lipid Res. 2010;51:1370–9.
Ravnskjaer K, Boergesen M, Rubi B, Larsen JK, Nielsen T, Fridriksson J, et al. Peroxisome proliferator-activated receptor α (PPARα) potentiates, whereas PPAR γ attenuates, glucose-stimulated insulin secretion in pancreatic β cells. Endocrinology. 2005;146:3266–76.
Liu S, Lui Q, Li L, Huan Y, Sun S, Shen Z. Long-term fenofibrate treatment impaired glucose-stimulated insulin secretion and up-regulated pancreatic NF-kappa B and iNOS expression in monosodium glutamate-induced obese rats: is it a latent disadvantage? J Transl Med. 2011;9:176.
Yajima K, Hirose H, Fujita H, Seto Y, Fujita H, Ukeda K, et al. Combination therapy with PPAR γ and PPAR α agonists increases glucose-stimulated insulin secretion in db/db mice. Am J Physiol Endocrinol Metab. 2003;284:E966–71.
Holm LJ, Krogvold L, Hasselby JP, Kaur S, Claessens LA, Russell MA, Mathews CE, Hanssen KF, Morgan NG, Koeleman BPC, Roep BO, Gerling IC, Pociot F, Dahl-Jørgensen K, Buschard K. Abnormal islet sphingolipid metabolism in type 1 diabetes. Diabetologia. 2018;61:1650–61.
Buschard K, Holm LJ, Feldt-Rasmussen U. Insulin independence in newly diagnosed type 1 diabetes patient following fenofibrate treatment. Case Rep Med. 2020;2020:6865190.
Cohen G, Riahi Y, Shamni O, Guichardant M, Chatgilialoglu C, Ferreri C, et al. Role of lipid peroxidation and PPAR-δ in amplifying glucose-stimulated insulin secretion. Diabetes. 2011;60:2830–42.
Kono T, Ahn G, Moss DR, Gann L, Zarain-Herzberg A, Nishiki Y, et al. PPAR γ activation restores pancreatic islet SERCA2 levels and prevents β-cell dysfunction under conditions of hyperglycaemic and cytokine stress. Mol Endocrinol. 2012;26:257–71.
Engelen W, Manuel-y-Keenoy B, Vertommen J, De Leeuw I, Van Gaal L. Effects of micronized fenofibrate and vitamin E on invitro oxidation of lipoproteins in patients with type 1 diabetes mellitus. Diabetes Metab. 2005;31:197–204.
A trial in adults with type 1 diabetes mellitus evaluating the effects of fenofibrate versus placebo on macular thickness and volume (FAME 1 EYE). Available from http://clinicaltrials.gov/ct2/show/NCT01320345. Last accessed 13 Apr 2021.
Winocour PH, Durrington PN, Bhatagnar D, Ishola M, Arrol S, Lahor BC, Anderson DC. Double-blind placebo-controlled study of the effects of bezafibrate on blood lipids, lipoproteins and fibrinogen in hypercholipidaemic type 1 diabetes. Diabet Med. 1990;7:736–43.
Winocour PH, Durrington PN, Bhatagnar D, Ishola M, Mackness M, Arrol S, Anderson DC. The effect of bezafibrate on very low density lipoprotein (VLDL), intermediate density lipoprotein (IDL), and low density lipoprotein (LDL) composition in type 1 diabetes associated with hypercholesterolaemia or combined hyperlipidaemia. Atherosclerosis. 1992;93:83–94.
Tenenbaum A, Motro M, Fisman EZ. Dual and pan-peroxisome proliferator-activated receptors (PPAR) co-agonism: the bezafibrate lessons. Cardiovasc Diabetol. 2005;4:14. https://doi.org/10.1186/475-2840-4-14.
Strowig SM, Raskin P. The effect of rosiglitazone on overweight subjects with type 1 diabetes. Diabetes Care. 2005;28:1562–7.
Stone ML, Walker JL, Chisholm D, Craig ME, Donaghue KC, Crock P, et al. The addition of rosiglitazone to insulin in adolescents with type 1 diabetes and poor glycaemic control: a randomized-controlled trial. Pediatr Diabetes. 2008;9(part 1):326–34.
Bhat R, Bhansali A, Bhadada S, Sialy R. Effect of pioglitazone therapy in lean type 1 diabetes mellitus. Diabetes Res Clin Pract. 2007;78:349–54.
Shimada A, Shigihara T, Okubo Y, Katsuki T, Yamada Y, Oikawa Y. Pioglitazone may accelerate disease course of slowly progressive type 1 diabetes. Diabetes Metab Res Rev. 2011;27:951–3.
Buchanan TA, Xiang AH, Peters RK, Kjos SL, Marroquin A, Goico J, et al. Preservation of pancreatic beta-cell function and prevention of type 2 diabetes by pharmacological treatment of insulin resistance in high-risk Hispanic women. Diabetes. 2002;51:2796–803.
Gerstein HC, Yusuf S, Bosch J, Pogue J, Sheridan P, Dinccag N, et al. Effect of rosiglitazone on the frequency of diabetes in patients with impaired glucose tolerance or impaired fasting glucose. Lancet. 2006;368:1096–105.
Defronzo RA, Tripathy D, Schwenke DC, Banerji M, Bray GA, Buchanan TA, Clement SC, Gastaldelli A, Henry RR, Kitabchi AE, Mudaliar S, Ratner RE, Stentz FB, Musi N, Reaven PD, ACT NOW Study. Prevention of diabetes with pioglitazone in ACT NOW: physiologic correlates. Diabetes. 2013;62:3920–6.
Dormandy JA, Charbonnel B, Eckland DJ, Erdmann E, Massi-Benedetti M, Moules IK, et al. Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial. Lancet. 2005;366:1279–89.
Derosa G. Efficacy and tolerability of pioglitazone in patients with type 2 diabetes mellitus: comparison with other oral antihyperglycaemic agents. Drugs. 2010;70:1945–61.
Krentz AJ. Rosiglitazone: trials, tribulations and termination. Drugs. 2011;71:123–30.
Friedland SN, Leong A, Filion KB, Genest J, Lega IC, Mottillo S, et al. The cardiovascular effects of peroxisome proliferator-activated receptor agonists. Am J Med. 2012;125:126–33.
Nissen SE, Wolski K, Topol EJ. Effect of muraglitazar on death and major adverse cardiovascular events in patients with type 2 diabetes mellitus. JAMA. 2005;294:2581–6.
FDA guidance for the industry. Diabetes mellitus. Developing drugs and therapeutic biologics for treatment and prevention. www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM071624.pdf.
FDA guidance for industry. Diabetes Mellitus. Evaluating cardiovascular risk in new antidiabetic therapies to treat type 2 diabetes. www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM071627.pdf.
The TIDE Trial Investigators. Design, history and results of the thiazolidinedione intervention with vitamin D evaluation (TIDE) randomised controlled trial. Diabetologia. 2012;55:36–45.
Vaccaro O, Masulli M, Nicolucci A, Bonora E, Del Prato S, Maggioni AP, TOSCA.IT Study Group, et al. Effects on the incidence of cardiovascular events of the addition of pioglitazone versus sulfonylureas in patients with type 2 diabetes inadequately controlled with metformin (TOSCA.IT): a randomised, multicentre trial. Lancet Diabetes Endocrinol. 2017;5:887–97.
Kernan WN, Viscoli CM, Furie KL, Young LH, Inzucchi SE, Gorman M, Guarino PD, Lovejoy AM, Peduzzi PN, Conwit R, Brass LM, Schwartz GG, Adams HP Jr, Berger L, Carolei A, Clark W, Coull B, Ford GA, Kleindorfer D, O’Leary JR, Parsons MW, Ringleb P, Sen S, Spence JD, Tanne D, Wang D, Winder TR, IRIS Trial Investigators. Pioglitazone after ischemic stroke or transient ischemic attack. N Engl J Med. 2016;374:1321–31.
De Paoli AM, Higgins LS, Henry RR, Mantzoros C, Dunn FL, INT131-007 Study Group. Can a selective PPARγ modulator improve glycemic control in patients with type 2 diabetes with fewer side effects compared with pioglitazone? Diabetes Care. 2014;37:1918–23.
Bays HE, Schwartz S, Littlejohn T 3rd, Kerzner B, Krauss RM, Karpf DB. MBX-8025, a novel peroxisome proliferator receptor-delta agonist: lipid and other metabolic effects in dyslipidemic overweight patients treated with and without atorvastatin. J Clin Endocrinol Metab. 2011;96:2889–97.
Cariou B, Zaïr Y, Staels B, Bruckert E. Effects of the new dual PPAR α/δ agonist GFT505 on lipid and glucose homeostasis in abdominally obese patients with combined dyslipidemia or impaired glucose metabolism. Diabetologia. 2011;34:2008–14.
Lu X, Ning Z, Cao H, Yao H, Pan D. 2020. Pooled analysis of a novel peroxisome proliferators-activated receptor pan receptor chiglitazar in patients with type 2 diabetes in China from two phase III trials. European Association for the study of diabetes virtual congress 2020 abstract.
Krishnappa M, Patil K, Parmar K, Trivedi P, Mody N, Shah C, Faldu K, Maroo S, PRESS XII Study Group, Parmar D. Effect of saroglitazar 2 mg and 4 mg on glycemic control, lipid profile and cardiovascular disease risk in patients with type 2 diabetes mellitus: a 56-week, randomized, double blind, phase 3 study (PRESS XII study). Cardiovasc Diabetol. 2020;19:93.
Henriksen K, Byrjalsen I, Qvist P, Beck-Nielsen H, Hansen G, Riis BJ. Efficacy and safety of the PPARγ partial agonist balaglitazone compared with pioglitazone and placebo: a phase III, randomized, parallel-group study in patients with type 2 diabetes on stable insulin therapy. Diabetes Metab Res Rev. 2011;27:392–401.
DeWitt S, Czarnik AW, Jacques V. Deuterium-enabled chiral switching (DECS) yields chirally pure drugs from chemically interconverting racemates. ACS Med Chem Lett. 2020;11:1789–92.
Harrison SA, Alkhouri N, Davison BA, Sanyal A, Edwards C, Colca JR, et al. Insulin sensitizer MSDC-0602K in non-alcoholic steatohepatitis: a randomized, double blind, placebo-controlled phase IIb study. J Hepatol. 2020;72:613–26.
Rodríguez-Pascau L, Britti E, Calap-Quintana P, Na Dong Y, Vergara C, Delaspre F, Medina-Carbonero M, Tamarit J, Pallardo FV, Gonzalez-Cabo P, Ros J, Lynch DR, Martinell M, Pizcueta P. PPAR gamma agonist leriglitazone improves frataxin-loss impairments in cellular and animal models of Friedreich Ataxia. Neurobiol Dis. 2021;148:105162.
Risérus U, Sprecher D, Johnson T, Olson E, Hirschberg S, Liu A, et al. Activation of peroxisome proliferator-activated receptor (PPAR) delta promotes reversal of multiple metabolic abnormalities, reduces oxidative stress, and increases fatty acid oxidation in moderately obese men. Diabetes. 2008;57:332–9.
Ooi EM, Watts GF, Sprecher DL, Chan DC, Barrett PH. Mechanism of action of a peroxisome proliferator-activated receptor (PPAR)-delta agonist on lipoprotein metabolism in dyslipidemic subjects with central obesity. J Clin Endocrinol Metab. 2011;96:E1568–76.
Lincoff AM, Tardif JC, Schwartz GG, et al. Effect of aleglitazar on cardiovascular outcomes after acute coronary syndrome in patients with type 2 diabetes mellitus: the AleCardio randomized clinical trial. JAMA. 2014;311:1515–25.
Koomen JV, Heerspink HJL, Schrieks IC, Schwartz GG, Lincoff AM, Nicholls SJ, Svensson A, Wedel H, Weichert A, Grobbee DE, Stevens J. Exposure and response analysis of aleglitazar on cardiovascular risk markers and safety outcomes: an analysis of the AleCardio trial. Diabetes Obes Metab. 2020;22:30–8.
Kim KS, Hong S, Ahn HY, Park CY. Comparative efficacy of lobeglitazone versus pioglitazone on albuminuria in patients with type 2 diabetes mellitus. Diabetes Ther. 2021;12:171–81.
Boubia B, Poupardin O, Barth M, Binet J, Peralba P, Mounier L, Jacquier E, Gauthier E, Lepais V, Chatar M, Ferry S, Thourigny A, Guillier F, Llacer J, Amaudrut J, Dodey P, Lacombe O, Masson P, Montalbetti C, Wettstein G, Luccarini JM, Legendre C, Junien JL, Broqua P. Design, synthesis, and evaluation of a novel series of indole sulfonamide peroxisome proliferator activated receptor (PPAR) α/γ/δ triple activators: discovery of Lanifibranor, a new antifibrotic clinical candidate. J Med Chem. 2018;61:2246–65.
Lefere S, Puengel T, Hundertmark J, Penners C, Frank AK, Guillot A, de Muynck K, Heymann F, Adarbes V, Defrêne E, Estivalet C, Geerts A, Devisscher L, Wettstein G, Tacke F. Differential effects of selective- and pan-PPAR agonists on experimental steatohepatitis and hepatic macrophages. J Hepatol. 2020;73:757–70.
Belfort R, Harrison SA, Brown K, Darland C, Finch J, Hardies J, Balas B, Gastaldelli A, Tio F, Pulcini J, Berria R, Ma JZ, Dwivedi S, Havranek R, Fincke C, DeFronzo R, Bannayan GA, Schenker S, Cusi K. A placebo-controlled trial of pioglitazone in subjects with nonalcoholic steatohepatitis. N Engl J Med. 2006;355:2297–307.
Cusi K, Orsak B, Bril F, Lomonaco R, Hecht J, Ortiz-Lopez C, Tio F, Hardies J, Darland C, Musi N, Webb A, Portillo-Sanchez P. Long-term pioglitazone treatment for patients with nonalcoholic steatohepatitis and prediabetes or type 2 diabetes mellitus: a randomized trial. Ann Intern Med. 2016;165:305–15.
Ratziu V, Harrison SA, Francque S, Bedossa P, Lehert P, Serfaty L, Romero-Gomez M, Boursier J, Abdelmalek M, Caldwell S, Drenth J, Anstee QM, Hum D, Hanf R, Roudot A, Megnien S, Staels B, Sanyal A, On behalf of the GOLDEN-505 Investigator Study Group. Elafibranor, an agonist of the peroxisome proliferator activated receptor alpha and beta, induces resolution of nonalcoholic steatohepatitis without fibrosis worsening. Gastroenterology. 2016;150:1147–59.
Francque S, et al. The pan PPAR agonist lanifibranor induces both resolution of NASH and regression of fibrosis after 24 weeks of treatment in non-cirrhotic NASH: results of the NATIVE Phase IIb trial American Association for the study of liver disease. Hepatology. 2020;72:9A–11A.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ansquer, J.C. (2023). The PPAR System in Diabetes. In: Jenkins, A.J., Toth, P.P. (eds) Lipoproteins in Diabetes Mellitus. Contemporary Diabetes. Humana, Cham. https://doi.org/10.1007/978-3-031-26681-2_6
Download citation
DOI: https://doi.org/10.1007/978-3-031-26681-2_6
Published:
Publisher Name: Humana, Cham
Print ISBN: 978-3-031-26680-5
Online ISBN: 978-3-031-26681-2
eBook Packages: MedicineMedicine (R0)