Abstract
Prediction: Retina laser treatment should become the most important and widely used treatment in ophthalmology for the treatment and prevention of virtually all causes of irreversible visual loss.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Prediction: Retina laser treatment should become the most important and widely used treatment in ophthalmology for the treatment and prevention of virtually all causes of irreversible visual loss.
That is, it should become. But will it? The ancient world had the Oracle of Delphi [1]. The closest thing we have had to predict the future in the modern world is The Spectator magazine. The Spectator is a weekly British magazine that has been published continuously since 1828 [2]. Over the years, The Spectator has offered a regular vignette posting predictions 10, 25, 50 years into the future, from prior editions of the magazine. The long publishing history of the Spectator has allowed readers to read and assess those past predictions for accuracy. As it happens, The Spectator’s predictions about the future are virtually never accurate.
This is not because the prognosticators of The Spectator are stupid or foolish. Anything but. The problem with predicting the future is two-fold: First, our only frame of reference is the past. This causes us to imagine the future only in terms of what we know now, or can imagine, based on our experience and current understanding. Thus, the future we tend to imagine is a better now. We expect current trends to continue, debts to be paid, and justice to finally be done. But, in general, our expectations are based on experience, not prescience. The Spectator is no different.
The second reason the future cannot be predicted is that disruptive events occur that are unanticipated by our experience, current thinking, or current technology. It is these unanticipated disruptive changes that will change the future far more profoundly than the incrementalism that dominates our thinking and limits imaginations [3, 4]. We can’t predict the future because the things that will define it do not exist and have likely not even occurred to anyone yet. This is easily confirmed by looking at the things that define our lives today. Who saw google or Tesla coming in 2000? Who even knew how important they would become when they appeared? Few, if any.
My bold prediction for the idea future of medicine also comes from experience, albeit a virtual one. I think Star Trek had it right with Bones’ “Tricorder”. The Tricorder was small hand-held device that he simply waved at a sick or injured person. The device both diagnosed and treated them, just like that. Why Bones had to be a doctor to do this was never clear to me (concerning note to the AMA). But that’s where we’re headed. Maybe an implanted chip instead of a thing we need to hold in our hand…? It’s coming, for sure.
Absent prescience, focus on near-term incrementalism is a safer bet. As we are primarily concerned with the future of retinal laser treatment, it is safe to bet that retinal laser will become more effective, safer, faster, easier, more pleasant, and more useful. The bigger question is whether anyone will care? Will laser be replaced by something we cannot currently envisage? Almost certainly. Nothing lasts forever. But, when, how, and by what, is unclear. Because the best we can do is project incrementally, in the following we will examine the general attributes of currently available laser modes to better understand what they do, and what room for improvement there might be in the future.
Candidate directions for the future of retinal laser therapy: how do they compare? We ask reason to point the way.
Mechanism of Retinal Laser
As discussed in more detail in “Neuroprotection”, all therapeutic retinal laser effects are mediated by RPE cells that are affected by the laser but not killed. Thus, the response to laser damaging to the retina is characterized by the same biologic effects arising from laser treatment sublethal to the retina, with additional effects resulting from tissue destruction, death, debridement, remodeling, and repair [5,6,7]. The effects arising only from laser-induced tissue damage are nontherapeutic and clinically detrimental, as they include principally inflammation, loss of function, and local fibrosis. Thus, the therapeutic effects of laser modes of inherently destructive laser modes such as conventional photocoagulation (CPC) (including the PASCAL), SRT, and 2RT are indirect, with all direct effects being adverse. In contrast, the therapeutic effects of MPL sublethal to the RPE are direct, arising from the area directly exposed to the laser beam, and thus entirely therapeutic and without adverse treatment effects [7,8,9,10]. The implications of this difference are difficult to overstate. The results of the Early Treatment of Diabetic Retinopathy Study (EDTRS) presaged this understanding, finding that increased treatment intensity increased adverse treatment effects, while increased density increased therapeutic effectiveness [11]. A fundamental difference between ETDRS CPC and laser treatment entirely sublethal to the retina, such as SDM MPL, is that increasing density of CPC to improve clinical effectiveness also reduces visual function. The less retina, the less disease. However, like amputation instead of antibiotics, this approach is at odds with clinical goals of sight preservation and vision improvement. For laser sublethal to the RPE, increasing treatment density and area increases the therapeutic effect by maximizing the restorative effects of treatment and improving, rather eliminating retinal and visual function [10]. These principles are reflected in some basic clinical observations: that there are no outcome differences associated with laser wavelength, as retinal destruction by any means is retinal destruction; that the detrimental effects of less damaging laser treatment modalities are differences of degree, and not kind; and that the visual benefits of destructive laser modes are reduced according to the degree of LIRD produced by that particular mode of treatment [7,8,9,10,11,12,13].
The fundamental differences in the effects of current laser modes, CPC, SRT, 2RT and MPL are, as suggested above, evident in their effects on retinal and visual function. These then determine how, when, where, for what, and how often each can be used therapeutically, and how well they achieve clinical goals. These inherent properties also determine the potential for each laser mode going into the future.
Arguably the most important advance needing to be made in ophthalmology is prevention of the major causes of irreversible visual loss. These are, in order of significance, AMD, DR, open angle glaucoma (OAG), and inherited retinal degenerations (IRDs). Some might argue that acquired myopia belongs in that list [14]. It is axiomatic that to slow, stop, or reverse disease progression and reduce the risks of visual loss, any effective treatment must first improve retinal function [15, 16]. Then, such a treatment would either have to be a permanent cure, or if temporarily effective, be renewable without limit to allow the benefits of treatment to be maintained.
There are many studies on the biologic responses to retinal laser treatment that are covered in the chapter on “Neuroprotection” and are relevant to this discussion. However, in this section we will focus on the key end-effects of laser treatment—retinal and visual function—rather than how and why we got there. For the purposes of examining the end-results of retinal laser on retinal function, electrophysiology is a widely available and highly sensitive measure of the retinal physiology that has been used to study the response to various current laser modes. This information should be helpful in suggesting which laser modes may be best suited best to the future job of preventing vison loss.
By definition, CPC reduces overall retinal function by destroying the retinal directly where, and near, it is applied. How much the result of testing such as electroretinography (ERG) is affected by the inherently destructive retina laser modes, including CPC, depends primarily on treatment density and retinal area covered. Thus, heavy panretinal photocoagulation (PRP) markedly reduces retinal function by full field electroretinography (ERG), while only a few focal spots of CPC in anywhere in the retina may have little effect on the ERG, despite complete loss of retinal function at the application spots. While there is some recovery after resolution of the acute inflammation and healing that follows CPC, the loss of visual function is permanent and may progress over time due to progressive retinal atrophy resulting from enlargement of the CPC scars [17, 18]. Regarding short-pulse CW laser (PASCAL), a study 104 eyes of 52 patients to undergo panretinal laser for PDR was reported, randomizing patients between conventional panretinal photocoagulation (PRP) and PASCAL peripheral retinal laser. After treatment there was no significant difference in VA between the groups. Full field electroretinography (ERG) and flicker ERG were significantly reduced both groups, with a significantly greater reduction in the PRP group compared to the PASCAL group [19]. In another study, retinal function was assessed in eyes randomized between ranibizumab alone, and PASCAL or conventional CPC peripheral retinal treatment with or without ranibizumab, for proliferative diabetic retinopathy (PDR). At 48 months full-field ERG responses were diminished in all eyes, even in drug-only eyes. However, this reduction in the drug alone eyes was mild compared to the laser-treated eyes. In this study, there was no difference in reduced retinal function by ERG between the eyes treated with CPC and the PASCAL [20]. The PASCAL is designed to photocoagulate the outer retina and photoreceptors, reducing damage to the RPE and overlying neurosensory retina [10]. Thus, it is not surprising that panretinal PASCAL treatment reduces the ERG response, but may preserve retinal function better than CPC [21]. However, the Manchester study showed that PASCAL treatment of sufficient density can reduce retinal function as effectively as conventional suprathreshold photocoagulation [20]. A search of the literature failed to produce studies examining changes in retinal function by electrophysiology in humans following SRT and 2RT.
Regarding MPL, Venkatesh et all reported 46 eyes of 33 patients randomized between 532 nm focal laser and 810 nm “SDM” for DME. These were evaluated with multifocal ERG before and after treatment. With an average follow up of 6 months 18/23 532 nm and 4/23 SDM eyes showed ERG worsening after treatment. Contrast sensitivity, VA and DME reduction were the same between the groups [22]. Jhingan and associates compared CPC PRP and MPL PRP for severe NPDR and low-risk PDR in 20 eyes of 10 patients. At 9 months post treatment, the conventional PRP eyes had worse visual fields, contrast sensitivity, and ERG compared to the MPL eyes, but the difference was not significant [23].
In 2016, 158 eyes of 108 patients with AMD, and 10 eyes of 8 patients with IRDs (rod-cone degeneration (four eyes), cone-rod degeneration (three eyes), and Stargardt's disease (three eyes)) were evaluated before, and 1 month after. panmacular SDM MPL by pattern electroretinography (PERG). Overall VAs were stable, while the PERG responses were improved in both AMD (p = 0.0001) and the IRD groups (p = 0.002). In the AMD eyes, additional testing of contrast acuity (p = 0.006) and microperimetry (p = 0.046) were also improved [15].
In a subsequent study, 26 eyes of 15 pts with retinitis pigmentosa were reported, aged 16–69 (avg. 47) years. Each underwent panmacular SDM MPL. Before, and approximately one month after treatment, each eye was tested by PERG and mesopic visual function testing. All PERG indices improved after treatment, with significant improvements in two signal latency measures (the MagD (µV)/Mag (µV) ratio (P < 0.0001), and the MagD (µV) amplitude (P = 0.0003). All mesopic visual function indices were also significantly improved, (p = 0.02 to p = 0.002), as was average logMAR VA (improving from avg. 0.6 to 0.4) (p = 0.02) [16].
That same year, 2018, 88 eyes of 48 consecutive patients with open angle glaucoma (OAG) were reported [24]. All had glaucomatous optic neuropathy and visual field loss prior to panmacular SDM MPL treatment. Pretreatment, IOPs ranged 6–23 mmHg (average: 13) on 0–3 (average: 1.6) medications. 33 eyes had had prior glaucoma surgery. Snellen visual acuities (VA) ranged 20/15 to count fingers (median 20/60). All were tested by PERG, visually evoked response (VER) and mesopic visual function testing (MVFT) before and approximately one month following SDM MPL treatment. Prior to treatment, both VEPs and MVFTs of all eyes were abnormal. Following SDM, Snellen VA was improved (p = 0.005). IOPs were unchanged. VER P1 amplitudes (p = 0.001), PERG amplitudes (p = 0.05), mesopic VA (p < 0.0001) and mesopic automated perimetry (p < 0.0001) were all significantly improved [24].
Not surprising, visual function tends to parallel retinal function, and thus the effects of the various laser modes on retinal function. CPC for macular disease rarely improves VA, except indirectly, such as treatment relatively distant from the fovea to reduce subretinal fluid from CSR or CNV [25,26,27]. In most applications for MPC, however, the hope is a reduced rate and risk of visual loss, rather than visual improvement.
The visual results of the PASCAL, SRT and 2RT tend to reflect stabilization of visual acuity in most applications. This includes trial for treatment of idiopathic macular telangiectasis, central serous chorioretinopathy (CSR), DME, and PDR for the PASCAL; DME, AMD and CSR for SRT; and DME and AMD for 2RT. For all short-pulse laser modes, treatment of CSR was generally effective, with improved VA. Visual results in DME tended to be stable or slightly improved, but not worsened. Treatment of eyes with intermediate AMD with 2RT reduced drusen, but to no significant effect. However, treatment of advanced dry AMD, characterized by reticular pseudodrusen and/or geographic atrophy, was significantly worsened by both SRT and 2RT (nanosecond laser). [28,29,30,31,32,33,34,35,36,37,38,39,40,41,42]. In all applications of SRT and 2RT, inherently destructive to the RPE and often adjacent structures as well, showed clinically visible laser lesions following treatment. In one study of 577 nm PASCAL for CSR, a titration algorithm (“endpoint management”) was used to try to avoid RPE damage. According to the authors, this technique was successful in avoiding detectable laser lesions by FFA, OCT, and fundus autofluorescence photography (FAF). In these eyes, VA was significantly improved [29].
As noted previously, the effects of MPL can span the entire range from suprathreshold CPC (inherently destructive to the retina) to SDM (which is reliably sublethal to the RPE) in all eyes, depending upon the laser parameters employed [7,8,9,10, 43]. For the purposes of this discussion, we will focus on SDM as the most different treatment modality when compared to CPC and short-pulse lasers that are inherently damaging to the retina. We continue to place the PASCAL in this group, even though treatment without retinal damage has been reported in one paper of 12 eyes. This is because, despite a titration algorithm, the narrow therapeutic range of CW lasers, of just 0.010 W in breadth in the case of the PASCAL, is simply too small a target to consistently “hit” reliably in a large number of eyes and laser spots, due to the marked susceptibility of such a narrow safety window to eye-specific factors, such as media opacity, fundus pigmentation, and regional differences in retina fundus pigmentation and retinal thickness [7,8,9,10, 29,30,31,32, 43, 31]. There is a substantive difference between treatment than can be retina-sparing, and treatment that is consistently and reliably retina-sparing [10, 30, 32, 43, 31].
In general, the visual results of SDM MPL reflect visual improvement in most applications. These include DME, PDR, dry and wet AMD, CSR, IRDs including retinitis pigmentosa, OAG, BRVO, and post-membrane peeling maculopathy [24, 27, 30, 44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63]. In particular, where head-to-head comparison of visual results of CPC and SDM MPL are reported (all for DME), the visual results of MPL are always superior to CPC [27, 46, 61,62,63,64]. A single trial comparing short-pulse CW laser (PASCAL) to MPL, found MPL visual results better [34]. It is interesting to note that, in DME, VA often improves out of proportion to the decrease in macular thickening, a marked contrast to CPC [61,62,63,64]. In some studies of DME employing the SDM high-density treatment strategy, the visual results of MPL rival intravitreal drug therapy [27, 65].
While retinal and visual function are objective measures, “safety” has been an historically fluid concept. The definition of safe laser treatment has reflected our understanding of treatment, and the available modes of treatment. In the CPC era, the many and significant adverse treatment effects of CPC, sufficiently well known that no list is required here, were considered acceptable because, compared to no treatment for such things and DME, PDR, and extrafoveal CNV, CPC was significantly better than no treatment at all. Since LIRD was presumed to be necessary for a therapeutic effect, efforts to improve safety centered primarily around reducing the severity of the inherent adverse effects, by reducing the intensity of suprathreshold CPC, and breaking treatment, such as CPC PRP, into partial treatments spread over time to reduce treatment-associated inflammation and pain [66]. As CPC intensity gradually declined, “subthreshold” therapy increased in popularity [7, 10]. New approaches to limiting LIRD to reduce the severity of the inherent adverse effects of LIRD, such as the PASCAL, SRT, and 2RT were developed. However, because LIRD was still the goal of treatment as it was universally believed to be necessary for therapeutically effectiveness, the inherent risks and adverse effects of retinal laser persisted [10]. However, a new definition of laser safety gradually emerged, placing into disfavor the dense white suprathreshold full-thickness burns of the ETDRS and MPSG [11,12,13, 66, 67].
It has been clear for nearly 2 decades that LIRD is in fact unnecessary, and even detrimental, to achieving optimal therapeutic effectiveness [51,52,53]. Responsible for all adverse effects of retinal laser treatment and unnecessary, the new standard for treatment safety is complete avoidance of LIRD with treatment that is sublethal to the RPE, and reliably so. Taken to its logical conclusion, this means that safe retinal laser treatment is now defined as treatment that is reliably safe in the fovea, and without any adverse treatment effects [30].
If we sum up the properties of current retinal laser modalities in an attempt to predict an incremental future and thus technical progress, we find:
-
The most important future application of retinal laser is prevention of visual loss from the major chronic progressive retinopathies.
-
To do this, treatment must improve retinal function. Available evidence indicates MPL is the best candidate in this regard.
-
Preventive treatment works best given early. This means prior to symptomatic vision loss and often clinical findings of disease. To treat and retreat asymptomatic patients at low current risk of vision loss, treatment must be extraordinarily safe. This means reliably safe (sublethal to the RPE) in the fovea, whether treated intentionally or inadvertently. Current evidence suggests MPL is the best candidate in this regard.
-
Preventive treatment must therefore preserve or improve vision function and visual acuity, and not for any reason worsen visual acuity. Only MPL has demonstrated this ability in all tested applications, including those without macular edema or fluid.
-
To maintain treatment effects over a lifetime of disease, treatment must be repeatable and renewable over a lifetime. Retinal damaging treatment modalities are not suited to such treatment as they quickly become visually threatening due to the accumulation of LIRD. MPL, employing the SDM paradigm reliably sublethal to the RPE, has been demonstrated to be infinitely repeatable with renewable therapeutic effects. Thus, current evidence suggests MPL is the best candidate in this regard.
-
To maximize treatment safety, preventive laser parameters and treatment should be uniform in all eyes, with minimal reliance on surgeon judgement. Because reliably safe retinal laser treatment is possible, the only remaining risk of treatment is surgeon misjudgment or error. Therefore, treatment should not be influenced by patient- or eye-specific factors that would require adjustment of laser parameters on a per eye basis. Current evidence indicates that MPL is the only treatment modality with a demonstrated facility in this regard.
-
The fact that LIRD is unnecessary and responsible for all adverse effects arising from retinal laser treatment redefines it, from a prerequisite of treatment to serious adverse treatment effect (SAE), or the most serious complication of laser treatment. Possible, or even frequent, avoidance of LIRD is unacceptable when reliably consistent LIRD avoidance is available. It is this level of safety that makes all else noted above possible. Thus, basic medical ethics require use of only treatments that are reliably sublethal to the retina. Current evidence indicates MPL as the best candidate in this regard.
The above conclusions suggest that MPL is the best candidate for the future of retinal laser treatment. It also raises two critical objections to continued use of retina-damaging laser modalities, all conceived and developed at a time when such damage was universally believed to be necessary for effective treatment; a practical objection, and an ethical objection.
From a practical point of view, retinal laser treatment has been shown to improve retinal and visual function in a wide variety of disparate chronic progressive retinopathies, united in their fundamental commonality of representing neurodegenerations. Some of these include IRDs and OAG. Little imagination is needed to see that superimposition of LIRD in these settings can only be detrimental to retinal and visual function. Further, any degree of LIRD markedly limits both application, such as to the fovea, and maintenance treatment over the lifetime of the patient if necessary. A further advantage of treatment sublethal to the RPE is that laser can be applied to the entire retina to address a panretinopathy, such as diabetic retinopathy or retinitis pigmentosa, to maximize therapeutic effects, in much the same way that intravitreal drug therapy treats the entire retina. Such “total retinal treatment” is forbidden to retinal damaging laser modes, due to the inevitable loss of retinal and visual function that would ensue.
The ethical objection to retina-damaging laser modes is likewise compelling. Past and even current acceptance of the adverse treatment effects inherent to retina-damaging treatment modes (even those described as “non-damaging” despite being photodisruptive to the RPE and outer retina) is a holdover from the CPC era when LIRD was thought to be necessary, and when there were no other, particularly no retina-sparing, treatment options available. Thus, the numerous and often severe adverse effects of CPC were considered acceptable when the benefits of treatment were compared to no treatment at all. Such decades long universally-held attitudes die slowly and persist even to this day, in spite of the advent of effective retina-sparing treatment alternatives.
Without invoking Hippocrates, a brief consideration of retina damaging vs. retina sparing treatment can be instructive. It is axiomatic in medicine that riskier, more invasive treatments should be considered over safer, less invasive treatments only if the added risks and complexity offer enough added benefit to justify the added risks and adverse effects [68]. Therefore, it is appropriate to ask if retina-damaging treatments are superior to sublethal treatments, and if so, are they sufficiently superior to justify the risks and inherent adverse treatment effects?
As described above, rather than superior, and certainly sufficiently superior to justify the risks and inherent adverse effects of treatment, the therapeutic effects of retinal-damaging laser treatments are instead consistently inferior to retina-sparing treatments by virtually all measures, the inferiority of damaging treatments is generally proportional to the severity of treatment associated LIRD. However, the differences are of degree, not kind.
Also axiomatic in medicine is that intervention should begin with the safest, simplest, least expensive, and least invasive treatment likely to be effective [69]. Thus, the inherent adverse effects of CPC have relegated it to rescue therapy behind drug therapy for most indications [70]. SDM MPL, absent any known adverse effects and thus without the adverse effects and risks of intravitreal drug therapy, however, is favorably positioned both practically and ethically as the first-choice treatment for many conditions also amenable to drug therapy [71].
Thus, from both a practical and ethical point of view, retinal laser treatment has a potentially important role to play in the goal of prevention of vision loss from the most important causes of irreversible vision loss, but only if it is reliably sublethal and absolutely non-damaging to the RPE and neurosensory retina.
This is “Modern Retinal Laser Therapy” (MRT) [32, 72, 73]. In short, MRT eschews LIRD in favor of low-intensity treatment reliably sublethal to the RPE. MRT eschews focal, local, and low-density grid treatment required by CPC and other damaging modes of treatment in favor of high-density treatment of large areas of dysfunctional retina, not with the desire to eliminate it, but with the intent to improve and normalize its function and maximize the clinical effects of treatment by maximal recruitment of dysfunctional retina to the therapeutic cause. Current data, although limited, suggests that MRT has the greatest potential of any currently known treatment modality, laser, drug, or other, to prevent vision loss in the future by virtue of its safety, durability, effectiveness, low cost, and breadth of indications [74,75,76].
To do this, more studies are required. This represents the single greatest obstacle to realizing the potential of MRT, because such studies are expensive and thus require sponsorship and support of parties expecting to benefit financially from the study outcomes. Currently, for this reason, the pharmaceutical industry dominates clinical data generation. Despite its potential benefits to society and healthcare, retinal laser treatment lacks such influential benefactors. This will need to change [77,78,79].
All current retinal laser platforms are designed to do treatment damaging to the retina, whether it be conventional CPC or more selective destruction of the outer retina (PASCAL), or RPE (SRT and 2RT). This is because they were all conceived of decades ago when the presumption of necessary LIRD was accepted universally. With time and progress in our understanding of the mechanism of action of retinal laser, some of these systems have been repurposed to perform less or non-damaging treatment by adding MPL capability. However, the design and use of all current systems remains dictated by their original intent and maintained capability of performing treatment intentionally destructive to the retina.
An additional incremental change in design was the introduction of application of pre-programmed patterned laser applications by the PASCAL. This facility has now been adopted by all currently retinal laser manufactures. A further incremental improvement in a number of retinal laser platforms is the added option of increasing the density of grid treatments by moving the spots closer together to reduce untreated retina and increase treatment density. Again, this is achieved by repurposing the underlying CPC laser delivery platform. The purported advantage of using such pattern applications is to improve treatment speed. However, as discussed elsewhere, once one considers the programming and treatment design time, the time savings seems to be minimal, if not taking longer to perform, than simple treatment aided by the standard laser repeat mode [80].
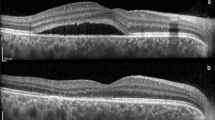
It has been well established that LIRD is contraindicated as neither directly nor independently contributing therapeutic effectiveness. Further, we now have MPL laser parameters that have proven to be safe in effective I all eyes, without regard for eye-specific variations in media opacity, retinal thickness, or pigmentation. Thus, titration of laser parameters, necessary for damaging laser modes such as CPC and SRT, is not only unnecessary, but increases the risk of LIRD and jeopardizes treatment safety if it leads to departure from known safe parameters [9, 10, 30,31,32]. Thus, the only risk of MRT is surgeon error, either by accidental or intentional use of parameters destructive to the retina. Because all current laser platforms are fundamentally designed to do damaging treatment, generally CPC, this risk remains an inherent property of all. (Figs. 19.1 and 19.2).
Fundus photograph and OCT of an eye three days following 577 nm MPL (5% duty cycle) for a branch retinal vein occlusion. A titration algorithm was employed in an attempt to adjust treatment to be subthreshold and sublethal to the RPE. After treatment the patient reported visual loss and multiple central scotomata. Note multiple threshold and suprathreshold retinal burns in a low-density grid pattern. From: Chang DB, Luttrull JK. Comparison of subthreshold 577 nm and 810 nm micropulse laser effects on heat-shock protein activation kinetics: Implications for treatment efficacy and safety. Transl Vis Sci Tecnol. 2020 Apr 28;9(5):23. doi: 10.1167/tvst.9.5.23. eCollection 2020 Apr.
A Intravenous fundus fluorescein angiogram of 56 year-old Asian woman with proliferative diabetic retinopathy and center-involving macular edema. B Infrared autofluorescence fundus photography (FAF) on prior to treatment. C FAF one week following 810 nm panmacular SDM MPL for center-involving DME. The patient reported that 3 days following treatment her vision worsened and a central scotoma appeared. Note the macular laser burns. Visual acuity before treatment 20/50; one week post treatment 20/400. D FAF two weeks later, three weeks following treatment. Note shrinkage of laser lesion. VA 20/200. The cause of the macular laser damage appeared to most likely be due to inadvertent use of a 15% duty cycle rather than the intended 5% duty cycle
Thus, retinal laser technology has not caught up with our current understanding and approach to retinal laser treatment, best exemplified by SDM MLT MRT. Because MRT applies treatment safely, geographically, and in high density, there is no need for precise targeting. The capacity to perform retina-damaging treatment can now be eliminated from laser platforms—at least those dedicated to treating macular disease and chronic progressive retinopathies (CPC will still be required for retinal cautery/retinopexy of retinal breaks)—also eliminating associated risks of treatment. Finally, substantial work has been done to understand how to optimize laser parameters for both safety and efficacy (Chang DB, Luttrull JK, unpublished data). All of these considerations suggest ample room for improvement in the safety and efficacy of retinal laser treatment, if MRT concepts are applied, via automation. Stay tuned for further developments.
References
Fairbanks A. Herodotus and the oracle of delphi. Class J. 1906;1(2):37–48.
The Spectator magazine. Press Holdings, London. ISSN: 0038-6952.
Reza FM (1994) [1961]. An introduction to information theory. Dover Publications, Inc., New York. ISBN: 0-486-68210-2.
Christiansen C. The innovator’s dilemma. 1st ed. Boston, USA: Harvard Business Review Press; May 1, 1997. ISBN-10: 0875845851; ISBN-13: 978-0875845852.
Richert E, Papenkort J, von der Burchard C, Klettner A, Arnold P, Lucius R, Brinkmann R, Framme C, Roider J, Tode J. Selective retina therapy and thermal stimulation of the retina: different regenerative properties—implications for AMD therapy. BMC Ophthalmol. 2021;21(1):412. https://doi.org/10.1186/s12886-021-02188-8. PMID: 34847865; PMCID: PMC8630886.
Tackenberg MA, Tucker BA, Swift JS, Jiang C, Redenti S, Greenberg KP, Flannery JG, Reichenbach A, Young MJ. Müller cell activation, proliferation and migration following laser injury. Mol Vis. 2009;15:1886–96. PMID: 19768129; PMCID: PMC2746266.
Luttrull JK, Dorin G. Subthreshold diode micropulse photocoagulation as invisible retinal phototherapy for diabetic macular edema A review. Curr Diabetes Rev. 2012;8:274–84.
Luttrull JK, Sramek C, Palanker D, Spink CJ, Musch DC. Long-term safety, high-resolution imaging, and tissue temperature modeling of subvisible diode micropulse photocoagulation for retinovascular macular edema. Retina. 2012;32(2):375–86.
Chang DB, Luttrell JK. Comparison of subthreshold 577nm and 810nm micropulse laser effects on heat-shock protein activation kinetics: Implications for treatment efficacy and safety. Transl Vis Sci Tecnol. 2020 Apr 28;9(5):23. Doi: 10.1167/tvst.9.5.23. eCollection 2020 Apr
Chhablani J, Roh YJ, Jobling AI, Fletcher EL, Lek JJ, Bansal P, Guymer R, Luttrull JK. Restorative retinal laser therapy: present state and future directions. Surv Ophthalmol. 2018;63(3):307–28.
Photocoagulation for diabetic macular edema. Early Treatment Diabetic Retinopathy Study report number 1. Early Treatment Diabetic Retinopathy Study research group. Arch Ophthalmol. 1985;103(12):1796–806. PMID: 2866759.
Atmaca LS, Ozmert E, Gündüz K. Comparisons of photocoagulation treatment in exudative age-related macular degeneration with the blue-green argon, green argon and red krypton laser wavelengths. Ophthalmologica. 1993;207(1):46–54. https://doi.org/10.1159/000310405. PMID: 7506402.
Evaluation of argon green vs krypton red laser for photocoagulation of subfoveal choroidal neovascularization in the macular photocoagulation study. Macular Photocoagulation Study (MPS) Group. Arch Ophthalmol. 1994;112(9):1176–84. https://doi.org/10.1001/archopht.1994.01090210060017. PMID: 7522004.
GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health. 2021;9(2):e144–60. https://doi.org/10.1016/S2214-109X(20)30489-7. Epub 2020 Dec 1. Erratum in: Lancet Glob Health. 2021 Apr;9(4):e408. PMID: 33275949; PMCID: PMC7820391.
Luttrull JK, Margolis BWL. Functionally guided retinal protective therapy as prophylaxis for age-related and inherited retinal degenerations. A pilot study. Invest Ophthalmol Vis Sci. 2016;5 7(1):265–75. https://doi.org/10.1167/iovs.15-18163.
Luttrull JK. Improved retinal and visual function following subthreshold diode micropulse laser (SDM) for retinitis pigmentosa. Eye (London) Feb 2018 PAP open access. https://doi.org/10.1038/s41433-018-0017-3.
Messias A, Ramos Filho JA, Messias K, Almeida FP, Costa RA, Scott IU, Gekeler F, Jorge R. Electroretinographic findings associated with panretinal photocoagulation (PRP) versus PRP plus intravitreal ranibizumab treatment for high-risk proliferative diabetic retinopathy. Doc Ophthalmol. 2012;124(3):225–36. https://doi.org/10.1007/s10633-012-9322-5. Epub 2012 Mar 29. PMID: 22457045
Morgan CM, Schatz H. Atrophic creep of the retinal pigment epithelium after focal macular photocoagulation. Ophthalmology. 1989;96:96e103.
Ye H, Yu M, Lu L, Jin C, Luo G. Electroretinogram evaluation for the treatment of proliferative diabetic retinopathy by short-pulse pattern scanning laser panretinal photocoagulation. Lasers Med Sci. 2018 Jul;33(5):1095–102. https://doi.org/10.1007/s10103-018-2474-0. Epub 2018 Mar 15. Erratum in: Lasers Med Sci. 2018 Apr 28; PMID: 29542045.
Messias K, Barroso RM, Jorge R, Messias A. Retinal function in eyes with proliferative diabetic retinopathy treated with intravitreal ranibizumab and multispot laser panretinal photocoagulation. Doc Ophthalmol. 2018;137(2):121–9. https://doi.org/10.1007/s10633-018-9655-9. Epub 2018 Sep 12. PMID: 30209775.
Kriechbaum K, Bolz M, Deak GG, Prager S, Scholda C, Schmidt-Erfurth U. High-resolution imaging of the human retina in vivo after scatter photocoagulation treatment using a semiautomated laser system. Ophthalmology. 2010;117(3):545–51. https://doi.org/10.1016/j.ophtha.2009.07.031. Epub 2010 Jan 19. PMID: 20031226.
Venkatesh P, Ramanjulu R, Azad R, Vohra R, Garg S. Subthreshold micropulse diode laser and double frequency neodymium: YAG laser in treatment of diabetic macular edema: a prospective, randomized study using multifocal electroretinography. Photomed Laser Surg. 2011;29(11):727–33. https://doi.org/10.1089/pho.2010.2830. Epub 2011 May 25. PMID: 21612513.
Jhingan M, Goud A, Peguda HK, Khodani M, Luttrull JK, Chhablani J. Subthreshold microsecond laser for proliferative diabe tic retinopathy: a randomized pilot study. Clin Ophthalmol. 2018;12:141–5. https://doi.org/10.2147/OPTH.S143206. PMID: 29391774; PMCID: PMC5774491.
Luttrull JK, Samples JR, Kent D, Lum BJ: Panmacular subthreshold diode micropulse laser (SDM) as neuroprotective therapy in primary open-angle glaucoma. Glaucoma Research 2018–2020, pp. 281–294 Edited by: John R. Samples and Paul A. Knepper © 2018 Kugler Publications, Amsterdam, The Netherlands.
Diabetic Retinopathy Clinical Research Network (2009). The course of response to focal/grid photocoagulation for diabetic macular edema. Retina (Philadelphia, Pa.), 29(10):1436–43. https://doi.org/10.1097/IAE.0b013e3181bcef6b.
Bressler SB, Almukhtar T, Aiello LP, Bressler NM, Ferris FL, 3rd, Glassman AR, Greven CM. Diabetic retinopathy clinical research Network. Green or yellow laser treatment for diabetic macular edema: exploratory assessment within the Diabetic Retinopathy Clinical Research Network. Retina (Philadelphia, Pa.) 33(10):2080–8. https://doi.org/10.1097/IAE.0b013e318295f744.
Lavinsky D, Cardillo JA, Melo LA Jr, Dare A, Farah ME, Belfort R Jr. Randomized clinical trial evaluating mETDRS versus normal or high-density micropulse photocoagulation for diabetic macular edema. Invest Ophthalmol Vis Sci. 2011;52(7):4314–23. https://doi.org/10.1167/iovs.10-6828. PMID: 21345996.
Lavinsky D, Silva MOD, Chaves AE, Schneider WFM, Lavinsky F, Palanker D. Functional and structural effects of nondamaging retinal laser therapy for macular telangiectasia type 2: a randomized sham-controlled clinical trial. Retina. 2021;41(3):487–94. https://doi.org/10.1097/IAE.0000000000002882. PMID: 33370517.
Lavinsky D, Palanker D. Nondamaging photothermal therapy for the retina: initial clinical experience with chronic central serous retinopathy. Retina. 2015;35(2):213–22. https://doi.org/10.1097/IAE.0000000000000340. PMID: 25158944.
Luttrull JK, Sinclair SD. Safety of transfoveal subthreshold diode micropulse laser for intra-foveal diabetic macular edema in eyes with good visual acuity. Retina. 2014;34(10):2010–20.
Lavinsky D, Sramek C, Wang J, Huie P, Dalal R, Mandel Y, Palanker D. Subvisible retinal laser therapy: titration algorithm and tissue response. Retina. 2014;34(1):87–97. https://doi.org/10.1097/IAE.0b013e3182993edc. PMID: 23873164.
Keunen JEE, Battaglia-Parodi M, Vujosevic S, Luttrull JK. International Retinal Laser Society Guidelines for Subthreshold Laser Treatment. Transl Vis Sci Technol. 2020;9(9):15. https://doi.org/10.1167/tvst.9.9.15. eCollection 2020 Aug.PMID: 32879771.
Roisman L, Magalhães FP, Lavinsky D, Moraes N, Hirai FE, Cardillo JA, Farah ME. Micropulse diode laser treatment for chronic central serous chorioretinopathy: a randomized pilot trial. Ophthalmic Surg Lasers Imaging Retina. 2013;44(5):465–70. https://doi.org/10.3928/23258160-20130909-08. PMID: 24044709.
Al-Barki A, Al-Hijji L, High R, Schatz P, Do D, Nguyen QD, Luttrull JK, Kozak I. Comparison of short-pulse subthreshold (532 nm) and infrared micropulse (810 nm) macular laser for diabetic macular edema. Sci Rep. 2021;11(1):14. https://doi.org/10.1038/s41598-020-79699-9. PMID: 33420100; PMCID: PMC7794500.
Jain A, Collen J, Kaines A, Hubschman JP, Schwartz S. Short-duration focal pattern grid macular photocoagulation for diabetic macular edema: four-month outcomes. Retina. 2010;30(10):1622–6. https://doi.org/10.1097/IAE.0b013e3181e095d8. PMID: 21060272.
Yasui A, Yamamoto M, Hirayama K, Shiraki K, Theisen-Kunde D, Brinkmann R, Miura Y, Kohno T. Retinal sensitivity after selective retina therapy (SRT) on patients with central serous chorioretinopathy. Graefes Arch Clin Exp Ophthalmol. 2017;255(2):243–54. https://doi.org/10.1007/s00417-016-3441-8. Epub 2016 Aug 6. PMID: 27497611.
Roider J, Liew SH, Klatt C, Elsner H, Poerksen E, Hillenkamp J, Brinkmann R, Birngruber R. Selective retina therapy (SRT) for clinically significant diabetic macular edema. Graefes Arch Clin Exp Ophthalmol. 2010;248(9):1263–72. https://doi.org/10.1007/s00417-010-1356-3. PMID: 20393742.
Park YG, Kim JR, Kang S, Seifert E, Theisen-Kunde D, Brinkmann R, Roh YJ. Safety and efficacy of selective retina therapy (SRT) for the treatment of diabetic macular edema in Korean patients. Graefes Arch Clin Exp Ophthalmol. 2016;254(9):1703–13. https://doi.org/10.1007/s00417-015-3262-1. Epub 2016 Jan 23. PMID: 26803489. No signif change VA or CFT.
Pelosini L, Hamilton R, Mohamed M, Hamilton AM, Marshall J. Retina rejuvenation therapy for diabetic macular edema: a pilot study. Retina. 2013;33(3):548–58. https://doi.org/10.1097/IAE.0b013e3182670fea. PMID: 23023529.
Prahs P, Walter A, Regler R, Theisen-Kunde D, Birngruber R, Brinkmann R, Framme C. Selective retina therapy (SRT) in patients with geographic atrophy due to age-related macular degeneration. Graefes Arch Clin Exp Ophthalmol. 2010;248(5):651–8. https://doi.org/10.1007/s00417-009-1208-1. Epub 2009 Dec 22. PMID: 20024687
Guymer RH, Wu Z, Hodgson LAB, Caruso E, Brassington KH, Tindill N, Aung KZ, McGuinness MB, Fletcher EL, Chen FK, Chakravarthy U, Arnold JJ, Heriot WJ, Durkin SR, Lek JJ, Harper CA, Wickremasinghe SS, Sandhu SS, Baglin EK, Sharangan P, Braat S, Luu CD; Laser Intervention in Early Stages of Age-Related Macular Degeneration Study Group. Subthreshold Nanosecond Laser Intervention in Age-Related Macular Degeneration: The LEAD Randomized Controlled Clinical Trial. Ophthalmology. 2019 Jun;126(6):829–38. https://doi.org/10.1016/j.ophtha.2018.09.015. Epub 2018 Sep 20. PMID: 30244144.
Wu Z, Luu CD, Hodgson LAB, Caruso E, Brassington KH, Tindill N, Aung KZ, Harper CA, Wickremasinghe SS, Sandhu SS, McGuinness MB, Chen FK, Chakravarthy U, Arnold JJ, Heriot WJ, Durkin SR, Wintergerst MWM, Gorgi Zadeh S, Schultz T, Finger RP, Cohn AC, Baglin EK, Sharangan P, Guymer RH; LEAD Study Group. Secondary and Exploratory Outcomes of the Subthreshold Nanosecond Laser Intervention Randomized Trial in Age-Related Macular Degeneration: A LEAD Study Report. Ophthalmol Retina. 2019 Dec;3(12):1026–1034. https://doi.org/10.1016/j.oret.2019.07.008. Epub 2019 Jul 22. PMID: 31582304.
Dorin G. Subthreshold and micropulse diode laser photocoagulation. Semin Ophthalmol. 2003;18(3):147–53. https://doi.org/10.1076/soph.18.3.147.29812. PMID: 15513476.
Frizziero L, Calciati A, Torresin T, Midena G, Parrozzani R, Pilotto E, Midena E. Diabetic Macular Edema Treated with 577-nm Subthreshold Micropulse Laser: A Real-Life, Long-Term Study. J Pers Med. 2021;11(5):405. https://doi.org/10.3390/jpm11050405. PMID: 34067994; PMCID: PMC8152245
Parodi MB, Spasse S, Iacono P, Di Stephano G, Canziani T, Ravalico G. Subthreshold grid laser treatment of macular edema secondary to branch retinal vein occlusion with micropulse infrared (810 nano meter) diode laser. Ophthalmology. 2006;113(12):2237e42.
Vujosevic S, Bottega E, Casciano M, Pilotto E, Convento E, Midena E. Microperimetry and fundus autofluorescence in diabetic macular edema: subthreshold micropulse diode laser versus modified early treatment diabetic retinopathy study laser photocoagulation. Retina. 2010;30(6):908–16. https://doi.org/10.1097/IAE.0b013e3181c96986. PMID: 20168272.
Vujosevic S, Martini F, Longhin E, Convento E, Cavarzeran F, Midena E. Subthreshold micropulse yellow laser versus subthreshold micropulse infrared laser in center-involving diabetic macular edema: morphologic and functional safety. Retina. 2015;35(8):1594–603. https://doi.org/10.1097/IAE.0000000000000521. PMID: 25719988.
Luttrull JK, Chang DB, Margolis BWL, Dorin G, Luttrull DK. Laser re-sensitization of medically unresponsive neovascular age-related macular degeneration: efficacy and implications. Retina. 2015;35(6):1184–94.
Luttrull JK. Low-intensity/high-density subthreshold diode micropulse laser (SDM) for central serous chorioretinopathy. Retina. 2016;36(9):1658–63.
Luttrull JK, Sinclair SH, Elmann S, Glaser BM. Low incidence of choroidal neovascularization following subthreshold diode micropulse laser (SDM) for high-risk AMD. PLoS ONE. 2018;13(8): e0202097. https://doi.org/10.1371/journal.pone.0202097.
Luttrull JK, Musch MC, Mainster MA. Subthreshold diode micropulse photocoagulation for the treatment of clinically significant diabetic macular edema. Br J Ophthalmol. 2005;89(1):74–80.
Luttrull JK, Spink CJ: Serial optical coherence tomography of subthreshold diode laser micropulse photocoagulation for diabetic macular edema. Ophthalmic Surg, Lasers Imaging. 2006;37:370–7.
Luttrull JK, Spink CJ, Musch DA. Subthreshold diode micropulse panretinal photocoagulation for proliferative diabetic retinopathy. Eye. 2008;22(5):607–12.
Luttrull JK. Subthreshold diode micropulse laser (SDM) for persistent macular thickening and limited visual acuity after epiretinal membrane peeling. Clin Ophthalmol. 2020;14:1177–88.
Luttrull JK, Sinclair SH, Elmann S, Chang DB, Kent D. Slowed progression of age-related geographic atrophy following subthreshold laser. Clin Ophthalmol. 2020;14:2983–2993.
Luttrull JK, Gray G. Prevention of neovascular AMD: Real world efficacy of program of panmacular laser for vision protection. Researchgate.net (2021). https://www.researchgate.net/publication/349952308_Prevention_of_neovascular_AMD_Real_world_efficacy_of_program_of_panmacular_laser_for_vision_protection.
Jorge EC, Jorge EN, Botelho M, Farat JG, Virgili G, El Dib R. Monotherapy laser photocoagulation for diabetic macular oedema. Cochrane Database Syst Rev. 2018;10(10):CD010859. https://doi.org/10.1002/14651858.CD010859.pub2.
Gawęcki M, Jaszczuk-Maciejewska A, Jurska-Jaśko A, Grzybowski A. Functional and morphological outcome in patients with chronic central serous chorioretinopathy treated by subthreshold micropulse laser. Graefes Arch Clin Exp Ophthalmol. 2017;255(12):2299–306.
Gawęcki M, Jaszczuk-Maciejewska A, Jusrka-Jaśko A, Kneba M, Grzybowski A. Transfoveal micropulse laser treatment of central serous chorioretinopathy within six months of disease onset. J Clin Med. 2019. https://doi.org/10.3390/jcm8091398.
Malik KJ, Sampat KM, Mansouri A, Mansouri A, Steiner JN, Glaser BM. Low-intensity/high density subthreshold micropulse diode laser for chronic central serous chorioretinopathy. Retina. 2015;35:532–6.
Brader HS, Young LH. Subthreshold diode micropulse laser: a review. Semin Ophthalmol. 2016;31(1–2):30–9. https://doi.org/10.3109/08820538.2015.1114837. PMID: 26959127.
Scholz P, Altay L, Fauser S. A review of subthreshold micropulse laser for treatment of macular disorders. Adv Ther. 2017 Jul;34(7):1528–55. https://doi.org/10.1007/s12325-017-0559-y. Epub 2017 May 24. PMID: 28540655; PMCID: PMC5504253.
Sivaprasad S, Dorin G. Subthreshold diode laser micropulse photocoagulation for the treatment of diabetic macular edema. Expert Rev Med Devices. 2012;9(2):189–97. https://doi.org/10.1586/erd.12.1. PMID: 22404779.
Chen G, Tzekov R, Li W, Jiang F, Mao S, Tong Y. Subthreshold micropulse diode laser versus conventional laser photocoagulation for diabetic macular edema: a meta-analysis of randomized controlled trials. Retina. 2016;36(11):2059–65. https://doi.org/10.1097/IAE.0000000000001053. PMID: 27096529.
Frizziero L, Calciati A, Torresin T, Midena G, Parrozzani R, Pilotto E, Midena E. Diabetic macular edema treated with 577-nm subthreshold micropulse laser: a real-life, long-term study. J Pers Med. 2021;11(5):405. https://doi.org/10.3390/jpm11050405.PMID:34067994;PMCID:PMC8152245.
Mainster MA. Decreasing retinal photocoagulation damage: principles and techniques. Semin Ophthalmol. 1999; 14:200e9.
Akduman L, Olk RJ. Subthreshold (invisible) modified grid diode laser photocoagulation in diffuse diabetic macular edema (DDME). Ophthalmic Surg Lasers. 1999;30(9):706–14. PMID: 10574491.
Edelstein L. The Hippocratic oath: text, translation and interpretation. 1943. p. 56. ISBN 978-0-8018-0184-6.
Varkey B. Principles of clinical ethics and their application to practice. Med Princ Pract. 2021;30:17–28. https://doi.org/10.1159/000509119.
Glassman AR, Wells JA 3RD, Josic K, Maguire MG, Antoszyk AN, Baker C, Beaulieu WT, Elman MJ, Jampol LM, Sun JK, for the diabetic retinopathy clinical research network. Five-year outcomes after initial aflibercept, bevacizumab, or ranibizumab treatment for diabetic macular edema (protocol t extension study). Ophthalmol. 2020;127(9):1201–10.
Luttrull JK. Laser is the first-choice treatment for diabetic retinopathy. Amsterdam Retina Debate. Annual meeting of the European Society of Retina Specialists (Euretina) 2017; Sept 8, Barcelona, Spain.
Kozak I, Luttrull JK. Modern retinal laser therapy. Saudi J Ophthalmol 2015;29(2):137–46.
Dennett D. Darwin’s dangerous idea and the meanings of life. New York, New York; Simon and Shuster; 1995. ISBN 978-0-684-80290-9.
Halawa OA, Lin JB, Miller JW, Vavvas DG. A review of completed and ongoing complement inhibitor trials for geographic atrophy secondary to age-related macular degeneration. J Clin Med. 2021;10(12):2580. https://doi.org/10.3390/jcm10122580.
Hall J, Matos S, Gold S, Severino LS. The paradox of sustainable innovation: The ‘Eroom’ effect (Moore’s law backwards). J Clean Prod. 2018;172:3487–97. https://doi.org/10.1016/j.jclepro.2017.07.162.ISSN0959-6526.
Lin A, Giuliano CJ, Palladino A, John KM, Abramowicz C, Yuan ML, Sausville EL, Lukow DA, Chait AR, Galluzzo ZC, Tucker C, Sheltzer JM. Off-target toxicity is a common mechanism of cancer drugs undergoing clinical trials. Sci Transl Med. 2019;11(509):eaaw8412. https://doi.org/10.1126/scitranslmed.aaw8412.
Lundh A, Lexchin J, Mintzes B, Schroll JB, Bero L. Industry sponsorship and research outcome. Cochrane Database Syst Rev. 2017;(2). Art. No.: MR000033. https://doi.org/10.1002/14651858.MR000033.pub3.
Anglemyer A, Horvath HT, Bero L. Healthcare outcomes assessed with observational study designs compared with those assessed in randomized trials. Cochrane Database Syst Rev. 2014;(4). Art. No.: MR000034. https://doi.org/10.1002/14651858.MR000034.pub2.
Dal Bó E. Regulatory capture: a review. Oxf Rev Econ Policy. 2006;22(2):203–25. https://doi.org/10.1093/oxrep/grj013.
Chhablani J, Luttrull JK. Retina debate: Is navigated laser the answer for DME? Retinal Physician. 2020:22–5.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Luttrull, J.K. (2023). The Future for Retinal Laser Treatment. Is There One?. In: Grzybowski, A., Luttrull, J.K., Kozak, I. (eds) Retina Lasers in Ophthalmology. Springer, Cham. https://doi.org/10.1007/978-3-031-25779-7_19
Download citation
DOI: https://doi.org/10.1007/978-3-031-25779-7_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-25778-0
Online ISBN: 978-3-031-25779-7
eBook Packages: MedicineMedicine (R0)