Abstract
In the last years, the entire world has been affected by the SARS-COV-2 pandemic, that represents the etiologic agent of Coronavirus disease 2019 (CoViD-19), which degenerated into a global pandemic in 2020. CoViD-19 has also had a strong impact on cancer patients. Our analysis has been performed at the Department of Oncology of the AORN “Cardarelli” in Naples, collecting data from all patients who had access in 2019–2020. We aim to understand how CoViD-19 affected hospital admissions. The statistical analysis showed that between 2019 and 2020 there was an increase in urgent hospitalizations and a decrease in scheduled hospitalization, probably to decrease the risk of infection, particularly in this category of susceptible patients. Indeed, as recommended by the European Society of Medical Oncology, during the pandemic, it was necessary to reorganize healthcare activities, ensure adequate care for patients infected with CoViD-19. Therefore telemedicine services were implemented and clinic visits were reduced.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
In the last years, the entire world has been affected by the SARS-COV-2 pandemic. This virus belongs to the genus Betacoronavirus (family Coronaviridae) and represents the etiologic agent of Coronavirus disease 2019 (CoViD-19), which degenerated into a global pandemic in 2020 [1].
The pathophysiology of SARS-CoV-2 primarily affects the respiratory tract, but other organs are often involved [2,3,4,5]. Onset symptoms are often fever with dry cough and dyspnea [4]. Headache, vomiting, dyspepsia, diarrhea, muscle pain, joint pain, and fatigue may also be present [6].
Symptoms in SARS-CoV-2 positive patients can be mild or result in acute respiratory distress syndrome (ARDS) with uncontrolled inflammation that can lead to multiple organ failure (MOF).
During the pandemic, it was necessary to reorganize healthcare system to ensure adequate care for both CoViD-19-infected patients and non-CoViD patients by providing essential and not deferrable care. In particular, the European Society of Medical Oncology immediately provided guidance and training to medical oncologists on how to manage cancer patients as the CoViD-19 pandemic progressed. This society recommended whenever possible, strengthening telemedicine services, aiming to diminish clinic visit through an increase of oral therapies [7, 8].
Cancer patients, moreover, often have suppressed immune systems due to cancer treatments such as surgery and chemotherapy, so they are more susceptible to infections [9, 10].
Early studies have shown that, especially in the absence of vaccines, SARS-CoV-2 positive patients, who have an underlying tumor, have an increased risk of death and/or admission to intensive care (ICU admission). In addition, cancer patients, with CoViD-19, who have recently undergone cancer treatment are at greater risk of more severe signs and symptoms and an increased risk of complications [11, 12]. Different data-driven approaches have been proposed to deal with different tasks, showing higher performances [13,14,15,16,17,18,19,20,21].
Our analysis has been performed at the Department of Oncology of the AORN “Cardarelli” in Naples, collecting data from all patients who had access in 2019–2020. To better understand how che CoViD-19 affected hospital admissions in the oncologic area we compared the data of patient discharged during a pre-pandemic period (2019) and a intra-pandemic one (2020).
To achieve this, statistical analyses and logistic regressions have be implemented to compare the two groups consisting of sets of variables that assess departmental performance. In this way, the organizational impact of the pandemic can be quantified, as done in other previous work on other wards of the hospital.
2 Methods
This Study was conducted on patients admitted to the Department of Oncology of the AORN “Cardarelli” of Napoli and discharged in the two years period 2019–2020.
The Dataset was extracted from the QuaniSDO information system software in use in the hospital. This data source has the great advantage to be available without requiring further consent by patients since they already consent to their use during the hospitalization process.
The patients discharged in 2019 were 1437 while in 2020 the admissions were 110. We consider different features extracted from the medical history: biographic (i.e. Gender, Age), discharge mode (1–9 starting from dead to ordinary discharge) and hospitalization type (1–3 starting from scheduled to the one with pre-hospitalization). Statistical analysis am Logistic Regression were implemented using the software IBM SPSS ver. 27.
2.1 Data Analysis
The first step of data analysis was the verification of the normality of the distributions, which is essential to carry out the subsequent multivariate analysis. The normality test of Shapiro-Wilk resulted in a p-value < 0.05, null hypothesis was therefore refused and the non-normality of the distribution confirmed. In the second phase, patients’ data were sorted by the year of discharge and the significance of the changes in the different variables between the two groups evaluated by the one-way analysis of variance (one-way ANOVA) as shown in Table 1.
Multinominal Logistic Regression was then implemented for unveiling relationships between variables. Since Logistic Regression models the probability of one event out of two alternatives, non-dichotomous variables had to be converted to binary values. As such, nominal variable with more than 2 values (i.e. Mode of Discharge) were analyzed through the use of dummy variables. On the other hand, to evaluate the changes in scale variables (i.e. Age, LOS, Weight of DRG) between the two years, it was used as reference the median value of the relative 2019 group.
3 Results
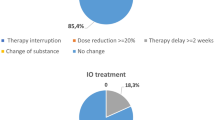
Data were collected for 2447 patients admitted by the Department of Oncology of the AORN “A. Cardarelli” of Naples between 2019 and 2020, Table 1 shows the characteristics of the population sorted by year of discharge. The results show a significant change in the type of hospitalization and patients’ age between the two years, with an increase in “2. Urgent Hospitalization” (from 73.5% to 76.7%) and the median age (from 63 to 64 years). No other significant variation has been highlighted.
The output of Logistic regression is shown in Table 2. In Logistic Regression OR indicates the ratio of probabilities of an event to occur over the possibilities of it not occurring, based on the effect of a variable. In our models we studied the effect of the Year of Discharge on the other variables. For example, an OR = 1.33 (CI 1.082–1.635) in the Type of Hospitalization 2 (Urgent Hospitalization) states that a patient admitted in 2020 has the probability to have been hospitalized urgently of about 55% (CI 50%-60%) over the other possible outcomes (1. Scheduled Hospitalization) [22].
Table 2 confirm the significance of the shift both in Age and Type of Hospitalization shown in Table 1.
4 Discussions and Conclusions
The aim of the study is to evaluate how a pandemic, such as CoViD-19, affects Department of Onclology activities. Data of the 2019 are used as a reference of the normal activity of the Department.
Our analysis has been performed at the Department of Oncology of the AORN “Cardarelli” in Naples, collecting data from 1437 patients who were discharged in 2019 and 1010 who were, instead, discharged in 2020. Amoung the avaible variables on the QuaniSDO hospital information system, the ones specifically collected (i.e. gender, age, relative DRG weight, admission mode and discharge mode) were chosen because of major interest and more easily influenced by the pandemic [23].
Logistic Regression was chosen statistical mode because it is commonly used to estimate the association of one or more predictors (independent variables) with a binary outcome (dependent variable). The relationship between each predictor and the dichotomous outcome can then be studied while holding constant the values of the other independent variables. This is particularly useful not only to understand the independent relationship of each variable with the outcome, but also, adjust the estimates for the effects of confounding variables in observational research.
A reason for its popularity among medical researchers is that the exponentiated logistic regression slope coefficient can be conveniently interpreted as an odds ratio. The odds ratio indicates how much the odds of a particular outcome change for a 1-unit increase in the independent variable (for continuous independent variables) or versus a reference category (for categorical variables) [24].
The analysis shows a decrease in the total number of hospital admissions from 2019 to 2020, and, in particular, an increase of urgent hospitalization and a decrease of scheduled hospitalization. These results show how the AORN Cardarelli appears to follow the already cited national and international guidelines to decrease hospital admissions, except for cases of real clinical emergency, especially in this category of patients, who are more exposed to Healthcare Associated Infections (HCAI). Patients were admitted to the hospital only when truly necessary by making appropriate use of hospital care resources.
This study has some limitations: it does not include, indeed, the effect of the reduction on the access to cancer screening during the pandemic. This aspect, along with the short period of observation, does not allow to correctly evaluate the impact of these modifications on the outcomes, because in cancers cases they have to be assessed on a long term period.
A future development of this study would be, on the one hand, the inclusion of screening and the extension of the period of observation and on the other hand, the evaluation of effectiveness, efficiency and performance of the healthcare processes, using several tools such as: Machine Learning [25,26,27], news processing techniques [28,29,30,31], Lean Six Sigma [32, 33], other decision support tools [34,35,36] and statistical analysis [37,38,39,40,41,42].
References
Lu, R., Zhao, X., et al.: Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet 395(10224), 565–574 (2020). https://doi.org/10.1016/S0140-6736(20)30251-8
Fehr, A.R., Perlman, S.: Coronaviruses: an overview of their replication and pathogenesis. In: Maier, H.J., Bickerton, E., Britton, P. (eds.) Coronaviruses. MMB, vol. 1282, pp. 1–23. Springer, New York (2015). https://doi.org/10.1007/978-1-4939-2438-7_1
Guan, W., Ni, Z., et al.: Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 382(18), 1708–1720 (2020). https://doi.org/10.1056/NEJMoa2002032
Huang, C., Wang, Y., et al.: Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China Lancet 395(10223), 497–506 (2020). https://doi.org/10.1016/S0140-6736(20)30183-5
Chen, N., Zhou, M., et al.: Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 395(10223), 507–513 (2020). https://doi.org/10.1016/S0140-6736(20)30211-7
Shi, H., et al.: Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect. Dis. 20(4), 425–434 (2020). https://doi.org/10.1016/S1473-3099(20)30086-4
Raymond, E., Thieblemont, C., Alran, S., Faivre, S.: Impact of the COVID-19 Outbreak on the management of patients with cancer. Target Oncol. 15(3), 249–259 (2020). https://doi.org/10.1007/s11523-020-00721-1
Pentheroudakis G.: CoViD-19 and Cancer - ESMO. https://www.esmo.org/covid-19-and-cancer/q-a-on-covid-19
Kamboj, M., Sepkowitz, K.A.: Nosocomial infections in patients with cancer. Lancet Oncol. 10(6), 589–597 (2009). https://doi.org/10.1016/S1470-2045(09)70069-5
Longbottom, E.R., et al.: Features of postoperative immune suppression are reversible with interferon gamma and independent of interleukin-6 pathways. Ann. Surg. 264(2), 370–377 (2016). https://doi.org/10.1097/SLA.0000000000001484
Liang, W., et al.: Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 21(3), 335–337 (2020). https://doi.org/10.1016/S1470-2045(20)30096-6
Zhang, L., Zhu, F., et al.: Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan. China Ann. Oncol. 31(7), 894–901 (2020). https://doi.org/10.1016/j.annonc.2020.03.296
Esposito, C., Moscato, V., Sperlí, G.: Trustworthiness assessment of users in social reviewing systems. IEEE Trans. Syst. Man Cybern.: Syst. 52(1), 151–165 (2022). https://doi.org/10.1109/TSMC.2020.3049082
Sperlí, G.: A deep learning based chatbot for cultural heritage. In: Proceedings of the 35th Annual ACM Symposium on Applied Computing, pp. 935–937 (2020). https://doi.org/10.1145/3341105.3374129
Ianni, M., Masciari, E., Sperlí, G.: A survey of big data dimensions vs social networks analysis. J. Intell. Inf. Syst. 57(1), 73–100 (2020). https://doi.org/10.1007/s10844-020-00629-2
Sperlí, G.: A cultural heritage framework using a deep learning based chatbot for supporting tourist journey. Expert Syst. Appl. 183, 115277 (2021). https://doi.org/10.1016/j.eswa.2021.115277
Han, Q., Molinaro, C., Picariello, A., Sperli, G., Subrahmanian, V.S., Xiong, Y.: Generating fake documents using probabilistic logic graphs. IEEE Trans. Dependable Secure Comput. (2021). https://doi.org/10.1109/TDSC.2021.3058994
Di Girolamo, R., Esposito, C., Moscato, V., Sperlí, G.: Evolutionary game theoretical on-line event detection over tweet streams. Knowl.-Based Syst. 211, 106563 (2021). https://doi.org/10.1016/j.knosys.2020.106563
Albanese, M., et al.: Recognizing unexplained behavior in network traffic. In: Network Science and Cybersecurity, pp. 39–62. Springer, New York (2014). https://doi.org/10.1007/978-1-4614-7597-2_3
Petrillo, A., Picariello, A., Santini, S., Scarciello, B., Sperli, G.: Model-based vehicular prognostics framework using big data architecture. Comput. Ind. 115, 103177 (2020). https://doi.org/10.1016/j.compind.2019.103177
Sperlí, G.: A deep learning based community detection approach. In: Proceedings of the 34th ACM/SIGAPP Symposium on Applied Computing, pp. 1107–1110 (2019). https://doi.org/10.1145/3297280.3297574
Hall, G.H., Round, A.P.: Logistic regression–explanation and use. J. Roy. Coll. Phys. London 28(3), 242–246 (1994)
Trunfio, T.A., et al.: Multiple regression model to analyze the total LOS for patients undergoing laparoscopic appendectomy. BMC Med. Inf. Decis. Making 22(1), 1–8 (2022)
Schober, P., Vetter, T.R.: Logistic regression in medical research. Anesth. Analg. 132(2), 365–366 (2021). https://doi.org/10.1213/ANE.0000000000005247
Dhillon, A., Singh, A.: Machine learning in healthcare data analysis: a survey. J. Biol. Today’s World 8(6), 1–10 (2019)
Colella, Y., et al.: Studying variables affecting the length of stay in patients with lower limb fractures by means of Machine Learning. In: 2021 5th International Conference on Medical and Health Informatics, pp. 39–43 (2021).https://doi.org/10.1145/3472813.3472821
Trunfio, T.A., Borrelli, A., Improta, G.: Is It Possible to Predict the Length of Stay of Patients Undergoing Hip-Replacement Surgery? Int. J. Environ. Res. Publ. Health 19(10), 6219 (2022)
Ponsiglione, A.M., Cesarelli, G., Amato, F., Romano, M.: Optimization of an artificial neural network to study accelerations of foetal heart rhythm. In: 2021 IEEE 6th International Forum on Research and Technology for Society and Industry (RTSI), pp.159–164 (2021). https://doi.org/10.1109/RTSI50628.2021.9597213
Ponsiglione, A.M., Romano, M., Amato, F.: A finite-state machine approach to study patients dropout from medical examinations.In: 2021 IEEE 6th International Forum on Research and Technology for Society and Industry (RTSI), pp. 289–294 (2021). https://doi.org/10.1109/RTSI50628.2021.9597264
Romano, M., et al.: Symbolic dynamics in cardiotocographic monitoring. In: 2013 E-Health and Bioengineering Conference (EHB). IEEE (2013)
Cesarelli, M., et al.: Prognostic decision support using symbolic dynamics in CTG monitoring. EFMI-STC 186, 140–144 (2013)
Improta, G., Borrelli, A., Triassi, M.: Machine learning and lean six sigma to assess how COVID-19 has changed the patient management of the complex operative unit of neurology and stroke unit: a single center study. Int. J. Environ. Res. Public Health 19(9), 5215 (2022)
Cesarelli, G., Montella, E., Scala, A., Raiola, E., Triassi, M., Improta, G.: DMAIC approach for the reduction of healthcare-associated infections in the neonatal intensive care unit of the university hospital of naples ‘federico ii.’ In: Jarm, T., Cvetkoska, A., Mahnič-Kalamiza, S., Miklavcic, D. (eds.) EMBEC 2020. IP, vol. 80, pp. 414–423. Springer, Cham (2021). https://doi.org/10.1007/978-3-030-64610-3_48
di Laura, D., et al.: Efficiency measures of emergency departments: an Italian systematic literature review. BMJ Open Qual. 10(3), e001058 (2021). https://doi.org/10.1136/bmjoq-2020-001058
LeBlanc, V.R., Manser, T., Weinger, M.B., Musson, D., Kutzin, J., Howard, S.K.: The study of factors affecting human and systems performance in healthcare using simulation. Simul. Healthc.: J. Soc. Simul. Healthc. 6(7), S24–S29 (2011). https://doi.org/10.1097/SIH.0b013e318229f5c8
Vázquez-Serrano, J.I., Peimbert-García, R.E., Cárdenas-Barrón, L.E.: Discrete-event simulation modeling in healthcare: a comprehensive review. Int. J. Environ. Res. Publ. Health 18(22), 12262 (2021). https://doi.org/10.3390/ijerph182212262
Guarino, F., Improta, G., Triassi, M., Castiglione, S., Cicatelli, A.: Air quality biomonitoring through Olea europaea L.: the study case of “land of pyres.” Chemosphere, 282, 131052 (2021). https://doi.org/10.1016/j.chemosphere.2021.131052
Guarino, F., Improta, G., Triassi, M., Cicatelli, A., Castiglione, S.: Effects of zinc pollution and compost amendment on the root microbiome of a metal tolerant poplar clone. Front. Microbiol. 11, 1677 (2020). https://doi.org/10.3389/fmicb.2020.01677
Guarino, F., et al.: Genetic characterization, micropropagation, and potential use for arsenic phytoremediation of dittrichia viscosa (L.) Greuter. Ecotoxicol. Environ. Saf. 148, 675–683 (2018). https://doi.org/10.1016/j.ecoenv.2017.11.010
Guarino F., Cicatelli, A., Brundu, G., Improta, G., Triassi, M., Castiglione, S.: The use of MSAP reveals epigenetic diversity of the invasive clonal populations of Arundo donax L. PLoS One 14 (2019). https://doi.org/10.1371/journal.pone.0215096
De Agostini, A., et al.: Heavy metal tolerance of orchid populations growing on abandoned mine tailings: a case study in Sardinia Island (Italy). Ecotoxicol. Environ. Saf. 189, 110018 (2020). https://doi.org/10.1016/j.ecoenv.2019.110018
Moccia, E., et al.: Use of zea mays L. in phytoremediation of trichloroethylene. Environ. Sci. Pollut. Res. 24, 11053–11060 (2017). https://doi.org/10.1007/s11356-016-7570-8
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this paper
Cite this paper
Montella, E. et al. (2023). The Effect of CoViD-19 Pandemic on the Hospitalization of a Department of Oncology of an Italian Hospital. In: Wen, S., Yang, C. (eds) Biomedical and Computational Biology. BECB 2022. Lecture Notes in Computer Science(), vol 13637. Springer, Cham. https://doi.org/10.1007/978-3-031-25191-7_28
Download citation
DOI: https://doi.org/10.1007/978-3-031-25191-7_28
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-25190-0
Online ISBN: 978-3-031-25191-7
eBook Packages: Computer ScienceComputer Science (R0)