Abstract
Hygrometric measurement of gases conditioned by heat and moisture exchangers (HMEs) or heated humidifiers (HH) during mechanical ventilation is mainly used for research. The technique of the visual evaluation of the condensation on the flex tube or on the humidification chamber’s wall is feasible at the patient bedside but has many limitations. Several techniques to measure the moisture of gases exist. The most frequently used are the psychrometric method and the capacitance hygrometers that may be used in patients (during invasive or non-invasive ventilation) or on bench. The gravimetry (used by the standard ISO 9360) has technical limitations with high risk of errors and can only be used on bench. Psychrometry and capacitance hygrometers are generally used for clinical research, whereas the manufacturers of humidification systems often use gravimetry. This may explain the large differences in performance evaluation found for HMEs assessment. It was again observed during the pandemic that the humidity measurements conducted by the manufacturers with the ISO standards overestimated the humidity delivered to patients by their devices. Only independent measurements could discriminate between safe devices that should be used in patients from other devices. The large differences found between the manufacturer’s claim and the measured humidity by the psychrometric method call into question the validity of the ISO standard for detecting underperforming HMEs.
A new method to evaluate humidity delivered by heated wire humidifiers has been described recently. The heater plate temperature is closely correlated to the absolute humidity delivered to patients, and this temperature should be monitored in the case of high ambient temperature (that causes dysfunction of heated wire humidifiers). Heater plate temperature of above 62 °C predicts adequate humidity (above 30 mgH2O/L) in most situations with MR850.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Absolute humidity
- Humidification
- Mechanical ventilation
- Psychrometry
- Gravimetry
- ISO 9360
- Patient safety
- Heater plate temperature
Evaluation of the humidity of the gases delivered to patients has allowed an improvement and a progressive diversification of the humidification devices used during mechanical ventilation. The main techniques to evaluate the performances of the heat and moisture exchangers (HMEs) and of the heated humidifiers (HH) in terms of humidification are mainly used in research. The technique of the visual evaluation of condensation on the flex tube or on the humidification chamber’s wall is feasible at the patient bedside but has several limitations. Many techniques to measure the moisture of gases exist. The most frequently used in the clinical setting are the psychrometric method and the capacitance hygrometers usable on patients (during invasive or non-invasive ventilation) or on benches. The gravimetry (used by the standard ISO 9360) has technical limitations and can be used only on bench. Psychrometry and capacitance hygrometers are generally used for clinical research, whereas the manufacturers of the humidification systems often use the gravimetry. This may explain the differences in performance evaluation found for humidification device assessment [1, 2]. However, the large differences found between the manufacturer’s claim and the measured humidity call into question the validity of the ISO standard for detecting underperforming devices [1, 3].
1 Visual Evaluation of Condensation
1.1 Condensation in the Flex Tube
A simple way to evaluate if the gases administered to the patients are correctly humidified is to visually seek if condensation exists in the flex tube of the endotracheal tube. Indeed, if there is a difference between gas temperature in the circuit and the room temperature, the gas cools along the circuit, involving an increase in the relative humidity and possibly a condensation on the wall if the dew point temperature is reached. This technique was validated by two teams; they showed a good correlation between condensation and the absolute humidity of gases delivered by the tested HME [4, 5]. This simple technique can be used with both HME and HH, but it remains vague and can only give an idea of the level of relative humidity of gases. Under no circumstances, however, it allows to accurately evaluate the gas water contents.
1.2 Condensation on the Humidification Chamber’s Inner Wall
With the heated humidifiers, it is possible to determine indirectly if the gas reaches a high relative humidity by examining condensation on the walls of the humidification chamber. This technique was validated for relatively low room temperatures (between 22 and 24 °C) [6]. Indeed, low room temperatures are required to get a sufficient difference of temperature with the gas circulating in the humidification chamber. While cooling by contact with the wall, the relative humidity of the gas can raise, and condensation on the wall will occur at the dew point. On the contrary, with high room temperature, the delta between ambient and chamber temperature is not enough to lead to condensation. In this case, there is no correlation between condensation on the wall and the level of gas humidification [6] (Fig. 3.1). Consequently, this technique is useless when ambient temperatures are high, conditions that lead to heated wire humidifier dysfunction [6].
(a and b) Visual evaluation of condensation on the heated humidifier humidification chamber [6]. A close correlation exists between visual evaluation of the condensation (based on a condensation scale; see below) and heated wire humidifier performance (absolute humidity (mg H2O/L) of inspiratory gases) when ambient air is low enough (22 to 24 °C) (a). However, there is no correlation when ambient air is high (28 to 30 °C) (b). Scale for visual evaluation of condensation: the level of condensation on the humidification chamber wall can be assessed by visual inspection as follows: 1, dry; 2, vapor; 3, vapor with a few small droplets; 4, numerous droplets not covering the entire wall; 5, numerous droplets covering the wall almost completely. This scale has been used in several studies [5, 6]
2 Techniques to Measure the Hygrometry of Gases During Mechanical Ventilation
2.1 What Is Hygrometry?
Hygrometry characterizes the quantity of moisture of air, namely, the quantity of water vapor present in the air (or in another gas). It does not take into account the water present in liquid or solid form.
Definition of humidity: humidity or moisture expresses the presence of a mixture of dry air and water vapor in ambient air. In general, moisture refers to the “rate of moisture” expressed in % which refers to the relative humidity. The determination of this measurement is related to conditions, such as the temperature and the pressure. The rate of moisture in a volume of air is generally expressed by one of the following parameters (Fig. 3.2):
-
Absolute humidity (AH) or water content of a gas which defines the quantity of water vapor (i.e., gaseous state or steam) contained within a certain volume of this gas. It is generally expressed in mgH2O/L. The maximum water content of a gas increases with its temperature (Fig. 3.3).
-
Dew point temperature: it is the temperature for which at constant pressure, it is necessary to cool down a mass of humid air to reach the saturation of this steam gas. When the gas is further cooled, condensation appears. Knowing this temperature makes it possible to determine the humidity of air, thanks to the tables and diagrams like the Mollier diagram (Fig. 3.3). A parameter associated with this concept is the absolute humidity at saturation (AHS) (or maximal water content) which corresponds to the absolute humidity or water content, when the gas is saturated. The absolute humidity at saturation depends on the gas temperature (Fig. 3.3) [7].
-
Relative humidity (RH) is defined as the ratio of absolute humidity with the absolute humidity at saturation of this gas: RH = (AH/AHS) × 100.
Schematic representation of relative humidity (RH), absolute humidity (AH), and absolute humidity at saturation (AHS) with different temperatures. At 17 °C, a gas is completely saturated with water vapor; the water content (AH) is equal to AHS. This temperature corresponds to the dew point. By cooling down gas at 10 °C, condensation occurs. By warming up the gas, the water content (AH) remains the same, but since gas can contain more water with a higher temperature, the relative humidity diminishes. The hatched lines represent the quantity of water vapor in comparison with the complete volume of gas. This volume is artificially separated from the rest of the gas (in white) which is a volume of dry gas without water vapor
Presentation of the air water contents (i.e., absolute humidity (in mgH2O/L)) according to its temperature and according to the relative humidity of the air (RH). The curves of 25, 50, and 100% of saturation or relative humidity (RH) are represented. At 100% of relative humidity, the water content corresponds to the maximum water contents (i.e., absolute humidity at saturation (AHS)). At 37 °C, water content of the gas is 44 mgH2O/L with 100% of relative humidity (gas completely saturated with vapor water), and it is 22 mgH2O/L with 50% of RH and 11 mgH2O/L with 25% of RH
A gas containing steam contains a quantity of energy (enthalpy) or latent heat, which will be released at the time of the passage of the gas state to the liquid state (condensation). On the contrary, during the evaporation of gas, energy is required and the temperature of the gas decreases.
2.2 Psychrometry
2.2.1 Working Principles of Psychrometry
The psychrometric method comes from the exploitation of the Mollier diagram. The work of Mollier completed at the nineteenth century highlighted the relation between temperature and humidity relative to a given pressure. The Mollier diagram directly resulting from its research shows this relation. In spite of the limited means of its author at the time of this research, the Mollier diagram remains a reference. In particular, the psychometric method that is used for the majority of hygrometric measurements presented here is based on this work. The diagrams are valid for a given pressure. The influence of the pressure for a clinical application is negligible, because of the low amplitude of the barometric variations. Thus, measurements to be carried out only take into account the temperature as a variable (Fig. 3.4).
There are a great number of moisture sensors, relying on very complex principles (reserved with applications in laboratory) like hygrometer with radioactive isotopes and on very simple principles like the hair hygrometer, based on the principle of lengthening of a hair with moisture [8].
Psychrometer is one of the oldest hygrometers, invented by Regnault, around 1845. Its principle is based on the Mollier diagram and the measure of a difference in temperature between a “dry” temperature sensor and a “wet” temperature sensor.
A psychrometer consists of two temperature probes, wet and dry, placed in the gas for which humidity is assessed. One of the thermometers, called “wet” thermometer, is maintained wet with the help of a cloth soaked with water. The other, called “dry” thermometer, measures the temperature of the gas. Through contact with air, the water of the fabric evaporates if the gas is not already saturated with water, which causes a cooling of the wet thermometer until a balanced temperature. Knowing these two temperatures makes it possible to determine the rate of humidity relative to the abacuses means, derived from the Mollier diagram.
In the medical field which interests us, psychrometry was used in many studies [2, 5, 9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26], and the use of this technique was well described [13, 22].
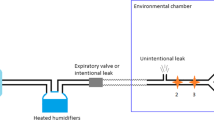
Two temperature sensors – dry and wet – are placed on the inspiratory way (generally in the event of measurement of the inspiratory gas hygrometry) or on the expiratory way (in the event of measurement of the expiratory gas hygrometry). The temperatures must be measured after the steady state is reached, after 15 min to 3 h (in particular when measurements relate to heated humidifiers with compensation system). The psychrometric method is based on the comparison of the dry and wet temperatures. The dry probe is put first (ventilator side), and the humid probe, encircled with a sterile piece of cloth soaked in water, is put about 1 cm ahead of the dry probe (patient side) (Fig. 3.5). The vaporizing of the water on the humid probe depends on the relative humidity of the gas (the more the gas is “dry” or has a low relative humidity, the more vaporization occurs, leading to the cooling of the probe). The gradient of temperature between both probes varies in a converse manner proportional to the relative humidity of gas. There is no gradient of temperature between the dry and humid probe when the gas is saturated with a relative humidity of 100%.
Flow separator used for psychrometric studies. This separator is required due to the low response time of this hygrometer. It allows analyzing only inspiratory (most often) or expiratory gas without mixing of the flows. The additional dead space is minimal as the gases are separated; however, resistive proprieties must be taken into account during the measurements
Relative humidity (RH) is calculated in reference to a psychrometric diagram taking into account differences between the temperatures of the two probes [27].
The absolute humidity at saturation (AHS) is acquired by the following expressions:
where T is the temperature of the dry probe.
Absolute humidity (AH) is acquired by the following formula and by knowing the relative humidity (RH) and absolute humidity at saturation (AHS):
The response time of this psychrometer for a gas at a speed of 1 m/s was measured in 1.25 s for 50% of equilibration and 4.1 s for 90% of equilibration of the temperature. The response time (63% of the equilibrium time) is in the order of 2 s [13]. Considering that the relatively long response time does not allow the separation of inspiration and expiration in normal breathing conditions, a flux separator should be used, allowing separating inspiratory gases from expiratory gases (Fig. 3.5). It allows the non-“pollution” of inspiratory gases with expiratory gases during measurement.
The temperature probes are placed on the inspiratory or expiratory ways, according to the type of measurement. The calibration of this machine is based on the calibration of the temperature probes. Furthermore, before every series of measurements, the measured temperatures by the two temperature probes of the psychrometer (prior to the soaking in water of the humid probe) should be compared with a standard temperature acquired with a high-precision thermometer, placed at the same level as both assessed temperature probes. The value of the highest temperature in the inspiratory canal should be considered in the course of several cycles after equilibrium. Certain teams use the medium inspiratory temperature [13, 22].
2.3 Comparison of Psychrometry with Other Techniques
2.3.1 Studies Using the Psychrometry
The psychrometric technique was used by numerous teams [2, 5, 9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26]. The first measurements which we acquired with the psychrometric method showed a very good reproducibility of measurements compared with data beforehand published for identical systems of humidification. For instance, the hygrometric performance evaluation of the Hygrobac DAR HME made by different teams found data very close [5, 22, 28]. Also, within our laboratory, the reproducibility of measurements accomplished for the same system was very good with weak standard deviations (usually lower in 1 mgH2O/L) [1, 6, 29,30,31].
By comparing the psychrometric measurements provided in the literature with other techniques to measure hygrometry, it appears a good correlation between measurements accomplished with psychrometry and those performed with other techniques. The most frequent alternative techniques to measure the performances of the humidification systems are the gravimetry (bench studies only) and the capacitance hygrometer which also allows making measurements in mechanically ventilated patients.
2.3.2 Studies Using the Gravimetry
Gravimetry is one of the techniques used for the evaluation of the humidification systems. A method was developed and recommended by the norm ISO 9360 [32]. It is based on weight difference of a semi-closed system over a given period (normally of 2 h) and assesses the loss of water in the system which consists of a lung, the humidification system to be tested [26, 33,34,35,36,37,38], and a model simulating a patient with a saturated expiratory gas (Fig. 3.6). Results are normally expressed in mgH2O/L of water loss/hour. Knowing the value of exhaled humidity and minute ventilation, it is possible to determine the absolute humidity of the delivered gas.
Gravimetric method to measure hygrometry according to the norm ISO 9360 [33]
This method is used mainly by the manufacturers to test the humidification systems on bench. The major limitation of this technology is that it cannot be directly used with patients. The other limitation is that it requires high-precision equipment for the weighing of the system and for the measurements of inspired and expired volumes at different levels of temperature and humidity. The study of Branson and Davis is the most exhaustive among those having used this technology [33]. These authors assessed the performances of 21 HMEs with the gravimetric method according to norm ISO 9360. It is possible to make the comparison with our bench study [1] for four HMEs tested in the same conditions of ventilation (tidal volume of 500 mL, respiratory rate of 20 breaths/min) (Table 3.1). Most of the other HMEs were different or with a reference that did not allow making identification with certainty.
The most important difference in measurements was with Hygroster (−7.5%) but remains weak. For other HMEs, the difference is minimal: Hygrobac (−2.5%), Hygrobac S (+4.2%), and Portex 1200 (+0.2%). When used by the companies, the differences between psychrometry and gravimetry are very high as shown in several studies [1, 3].
The main advantage of the psychrometry is that it can be used on patients as well as on bench, allowing a clinical validation of the model.
2.3.3 Studies Using Capacitance Hygrometer
This hygrometer was described for this usage for humidification system evaluation in 1983 by Tilling [39]. The sensor is a fine polymeric film with electrodes positioned on each side. According to relative humidity, the water steam is absorbed on the polymeric film, which changes its capacitance. These hygrometers are usually not expensive. Their main flaw is to have a significant drift, which often requires frequent calibrations. Moreover, considering that the response time is very quick, the given values (maximum, minimum, and medium value) make the analysis of results very difficult.
This hygrometer was used by several teams [19, 40,41,42,43], but results are difficult to compare with other hygrometers considering the quick response time of this hygrometer, the values of absolute humidity being given in maximum, minimum, or average (Table 3.2). It seems that the medium value is the one which gets closer to most psychrometric data, except in the case of Pall Ultipor used in the study of Martin et al. [19].
2.4 Limitations of the Psychrometric Method
The psychrometric method has nevertheless some limitations which are necessary to know. It is possible that the ambient temperature has an influence on measurement. Indeed, at the level of the separator of flux, there can be thermal exchanges between the gas passing in this piece and surrounding air, particularly when the difference in temperature between these gases is important. To restrict this phenomenon, it is possible to use an isothermic foam around the separator of flux. The use of the medium rather than maximum temperature could also restrict this phenomenon. Another problem linked to the piece which separates inspiratory gases from expiratory gases is the high resistance, especially in the inspiratory way. Inspiratory resistance was measured at 19.6 cmH2O for 1 L/s and expiratory ones at 4.8 cmH2O for 1 L/s. Due to the inspiratory resistance, in patients ventilated with assist-control ventilation in volume, the peak pressures increase and in patients ventilated with a pressure mode, the volumes delivered by the ventilator are reduced with the presence of the flow separator. In the first case, it is necessary to increase the high pressure alarms, and in the second event, it is necessary to increase the level of assistance to about 5–10 cmH2O to obtain an equivalent tidal volume. Due to the expiratory resistances, there can be a risk of expiratory flow limitation. Usually, the duration of the measurements does not exceed 15 min to attain the steady state, which limits this potential issue. In practice, we did not have problem of poor tolerance in the course of numerous measurements, probably due to the selection of the patients. The patients included had to have a relative respiratory stability (FiO2 ≤ 80%) as well as hemodynamic stability (epi- or norepinephrine ≤2 mg/h).
Another limitation shared by most of the hygrometric measurements is the inability to assess systems producing nebulizations. Indeed, psychrometry measures the vapor of water contained in a gas, while nebulization draws away micro-droplets under liquid form. These droplets make the dry probe wet, which distorts measurements. This limitation also exists with other methods using sensors (hygrometer with capacitance, dew point hygrometers).
2.5 Limitations of the Gravimetric Method (and ISO 9360)
Manufacturers usually state the humidity output of their devices based on ISO 9360 method. Thiery et al. suggested that independent hygrometric measurements are required to evaluate humidification devices [2]. The authors found markedly lower performances with psychrometric measurements in patients with Hygroster than those specified by the manufacturer: 27.3 ± 2.2 mgH2O/L vs. 33.4 mgH2O/L, respectively. Lellouche et al. evaluated on bench 48 HMEs and filters and compared the humidity performances claimed by the manufacturers using the ISO 9360 method and humidity measured by the psychrometric method [1]. The authors found large differences between humidity performances specified by manufacturers using the ISO 9360 method and the humidity measured on bench by the psychrometric method. The mean difference in absolute humidity between the two methods was 3.0 ± 2.7 mgH2O/L, with 36% of the device having a difference greater than 4 mgH2O/L, and the maximum difference was 8.9 mgH2O/L. Recently, we compared manufacturer’s claim (based on ISO 9360 method) and psychrometric measurements of HME responsible for endotracheal tube occlusions in patients mechanically ventilated for COVID-19 [3]. We measured unacceptably low humidity output (mean 25.8 ± 0.9 mgH2O/L) despite the fact that manufacturers reported a reassuring humidity of 32.8 ± 1.6 mgH2O/L. The mean difference between claimed and measured humidity in this small series was 6.4 ± 1.4 mgH2O/L. None of the HME involved in endotracheal tube occlusion had a humidity delivered above 30 mgH2O/L with psychrometric measurements, while they all passed the test with the ISO 9360. In other words, the ISO standard fails to protect patients from an underperforming HME.
3 Benches for Measurements of Hygrometry (for HME, “Active” HME, and Heated Humidifiers)
The bench evaluation of HME and “active” HME requires simulating a physiological model that provides saturated exhaled gas as for a patient with a normal core temperature. According to the literature data, exhaled gases are saturated with vapor water at 32 °C in the endotracheal tube at the teeth level [44, 45], which corresponds to a water content of 34 mgH2O/L (Fig. 3.7). These values of absolute expiratory humidity are concordant with those found in the study assessing expiratory humidity in patients with hypothermia and normal core temperatures [30]. The simulation of saturated expiration can be performed with a heated humidifier (Fig. 3.8).
Expiratory gas temperature in ten patients during anesthesia. In dotted lines is the gas temperature in the endotracheal tube at the level of the teeth. (Adapted from Dery et al. [45])
Hygrometric bench test apparatus used to measure the humidification performances of HMEs and antibacterial filters. A driving ventilator delivered controlled cycles (respiratory rate set at 20 breaths/min with a tidal volume of 500 mL and a positive end-expiratory pressure of 5 cmH2O). A heated humidifier (MR730) was connected to the expiratory limb of the model and was set to deliver gases with a water content of 35 mgH2O/L at the Y-piece. A circuit with heated wire was used after the humidification chamber. The (ambient) temperature should be maintained constant between 24.5 °C and 25.5 °C. The system can be installed in a space isolated (like an incubator) to keep this constant temperature. Ideally, an isothermic insulating foam should surround the separator of flow to avoid the variations of heat on this level and condensation in the part of hygroscopy. For all the studies on bench, the number of measurements carried out for each studied condition must be preset (between three and six measurements). This bench can be used for the study of the filter humidifiers and the active filters [1, 29]
Several studies are published using a model with simulation of expiratory saturated gases going from 32 to 37 °C, which corresponds to gas absolute humidity between 34 and 44 mgH2O/L [26, 33,34,35,36,37,38, 46,47,48,49]. We performed a bench study to compare different filters and HME in stable and controlled situations [1] (Fig. 3.8).
The bench evaluation of the heated humidifier performances is easier. The heated humidifier to test is installed on a ventilator with different settings (Fig. 3.9). The circuit of the ventilator is connected to a test lung (at Y-piece), the latter being changed regularly to avoid the accumulation of water. Different temperatures are measured (ambient temperature, ventilator output temperature, inlet chamber temperature) by a high-precision thermometer, and temperatures measured by the humidifier are also recorded (heater plate temperature, outlet chamber temperature, temperature at the Y-piece) [6].
4 Use of the Heated Humidifier Heater Plate Temperature
It was previously demonstrated that humidity delivered to the patient was reduced when the temperature entering in the HH humidification chamber was high (mainly due to high ambient air or high outlet ventilator temperature) [6]. This can be explained by the regulation of HH that maintains a constant outlet chamber temperature (frequently around 37 °C in most heated wire humidifiers). This can be achieved by decreasing the heated plate energy, leading to reduced temperature in the humidification chamber when the inlet chamber temperature is high. We recently evaluated if heater plate temperature could be used as an accurate surrogate of humidity delivered with MR850 humidifier [50]. It turned out that there is a very strong correlation between the heater plate temperature and absolute humidity delivered at the Y-piece, which means that a precise hygrometer is integrated in the heated humidifier. This relationship is not affected by the ambient air temperature but is slightly modified by the minute ventilation. In this study, we found that monitoring of this parameter could be helpful to detect low humidification, especially when ambient temperature is high. Heater plate (HP) temperature above 62 °C could predict a humidity delivered above 30 mgH2O/L with a good sensibility and specificity up to 12.5 L/min. Above this minute ventilation, heater plate temperature above 65 °C should be targeted. When HP temperature is below the target, specific settings should be used (increasing of chamber temperature by 1 to 3 °C or utilization of automated compensation function).
The heated humidifiers usually display the humidification chamber outlet temperature. However, this monitoring is useless and does not inform on humidity delivered [50]. Unfortunately, HP temperature is “hidden” and available only by accessing to the sub-menu as shown in the following video: https://www.youtube.com/watch?v=HImPXoIxLJw
The utilization of heater plate temperature monitoring was implemented in an ICU during the COVID-19 pandemic to avoid endotracheal tube occlusions [51]. After ICU rooms were equipped with negative pressure devices, the ambient temperature rose up to 28–30 °C leading to three episodes of ETO within few weeks, while humidification of the gases delivered to mechanically ventilated patients was performed with heated wire humidifiers. After implementation of measures to avoid under-humidification, including heater plate temperature monitoring, no more ETOs occurred [51]. This method has recently been described more in detail and confirms that when heater plate temperature is above 62 °C for minute ventilation below 12.5 L/min, the humidity delivered to the patients is above 30 mgH2O/L [50].
Let us assume that a gas has a temperature of 25 °C with relative humidity of 80% (point A on the diagram). If the temperature is cooled down to 20 °C, the relative humidity will increase and attain the dew point (100% of relative humidity) (point B). Between points A and B, only relative humidity varies, while absolute humidity is constant. If the gas is further cooled, condensation appears: the relative humidity remains at 100%, but absolute humidity will be reduced (passage from point B toward point C).
References
Lellouche F, et al. Humidification performance of 48 passive airway humidifiers: comparison with manufacturer data. Chest. 2009;135(2):276–86.
Thiery G, et al. Heat and moisture exchangers in mechanically ventilated intensive care unit patients: a plea for an independent assessment of their performance. Crit Care Med. 2003;31(3):699–704.
Lellouche F, et al. How to avoid an epidemic of endotracheal tube occlusion. Lancet Respir Med. 2021;9(11):1215–6.
Beydon L, et al. Correlation between simple clinical parameters and the in vitro humidification characteristics of filter heat and moisture exchangers. Groupe de travail Sur les Respirateurs. Chest. 1997;112(3):739–44.
Ricard JD, et al. Bedside evaluation of efficient airway humidification during mechanical ventilation of the critically ill. Chest. 1999;115(6):1646–52.
Lellouche L, et al. Influence of ambient air and ventilator output temperature on performances of heated-wire humidifiers. Am J Respir Crit Care Med. 2004;170:1073–9.
Williams RB. The effects of excessive humidity. Respir Care Clin N Am. 1998;4(2):215–28.
Saussure H-BD. BARDE, editor. Défense de l'hygromètre à cheveu, pour servir de suite aux essais sur l'hygrométrie. Genève: MANGET. p. 1788.
Ingelstedt S. Studies on the conditioning of air in the respiratory tract. Acta Otolaryngol Suppl. 1956;131:1–80.
Sara C, Currie T. Humidification by nebulization. Med J Aust. 1965;191:174–9.
Sottiaux T, et al. Comparative evaluation of three heat and moisture exchangers during short-term postoperative mechanical ventilation. Chest. 1993;104(1):220–4.
Tsubota K, Harada J, Goto Y. Efficacy of nine heat and moisture exchangers for intraoperative airway heat conservation. J Aerosol Med. 1991;4(2):117–25.
Jackson C, Webb AR. An evaluation of the heat and moisture exchange performance of four ventilator circuit filters. Intensive Care Med. 1992;18(5):264–8.
Markowicz P, et al. Safety, efficacy, and cost-effectiveness of mechanical ventilation with humidifying filters changed every 48 hours: a prospective, randomized study. Crit Care Med. 2000;28(3):665–71.
Vanderbroucke-Grauls CM, et al. Bacterial and viral removal efficiency, heat and moisture exchange properties of four filtration devices. J Hosp Infect. 1995;29(1):45–56.
Chiumello D, et al. In vitro and in vivo evaluation of a new active heat moisture exchanger. Crit Care. 2004;8(5):R281–8.
Croci M, Elena A, Solca M. Performance of a hydrophobic heat and moisture exchanger at different ambient temperatures. Intensive Care Med. 1993;19(6):351–2.
Martin C, et al. Performance evaluation of three vaporizing humidifiers and two heat and moisture exchangers in patients with minute ventilation >10 L/min. Chest. 1992;102(5):1347–50.
Martin C, et al. Preservation of humidity and heat of respiratory gases in patients with a minute ventilation greater than 10 L/min. Crit Care Med. 1994;22(11):1871–6.
Martin C, et al. Comparing two heat and moisture exchangers with one vaporizing humidifier in patients with minute ventilation greater than 10 L/min. Chest. 1995;107(5):1411–5.
Miyao H, et al. Relative humidity, not absolute humidity, is of great importance when using a humidifier with a heating wire. Crit Care Med. 1992;20(5):674–9.
Ricard JD, et al. Efficiency and safety of mechanical ventilation with a heat and moisture exchanger changed only once a week. Am J Respir Crit Care Med. 2000;161(1):104–9.
Christiansen S, et al. Measurement of the humidity of inspired air in ventilated patients with various humidifier systems. Anasthesiol Intensivmed Notfallmed Schmerzther. 1998;33(5):300–5.
Fassassi M, et al. Airway humidification with a heat and moisture exchanger in mechanically ventilated neonates: a preliminary evaluation. Intensive Care Med. 2007;33(2):336–43.
Tontschev G, Lueder M, Bensow C. The efficiency of various humidifiers for respired gas. Resuscitation. 1980;8(3):167–79.
Walker AK, Bethune DW. A comparative study of condenser humidifiers. Anaesthesia. 1976;31(8):1086–93.
Condon E, Handbook of physics. New York. NY: Churchill Livingstone; 1967.
Lellouche F, Brochard L. Advanced closed loops during mechanical ventilation (PAV, NAVA, ASV, SmartCare). Best Pract Res Clin Anaesthesiol. 2009;23(1):81–93.
Lellouche F, et al. Impact of ambient air temperature on a new active HME and on standard HMES: bench evaluation. Intensive Care Med. 2003;29:S169.
Lellouche F, et al. Under-humidification and over-humidification during moderate induced hypothermia with usual devices. Intensive Care Med. 2006;32(7):1014–21.
Lellouche L, et al. Advantages and drawbacks of a heated humidifier with compensation of under-humidification. Am J Respir Crit Care Med. 2003;167(7):A909.
Standardization, I.O.f., Anesthetic and respiratory equipment. Heat and moisture exchangers for use in humidifying gases in humans 1st ed. ISO International Standard 9360, 1992.
Branson R, Davis J. Evaluation of 21 passive humidifiers according to the ISO 9360 standard: moisture output, dead space, and flow resistance. Respir Care. 1996;41:736–43.
Eckerbom B, Lindholm CE. Performance evaluation of six heat and moisture exchangers according to the draft international standard (ISO/DIS 9360). Acta Anaesthesiol Scand. 1990;34(5):404–9.
Mebius C. A comparative evaluation of disposable humidifiers. Acta Anaesthesiol Scand. 1983;27(5):403–9.
Mebius C. Heat and moisture exchangers with bacterial filters: a laboratory evaluation. Acta Anaesthesiol Scand. 1992;36(6):572–6.
Ogino M, Kopotic R, Mannino FL. Moisture-conserving efficiency of condenser humidifiers. Anaesthesia. 1985;40(10):990–5.
Shelly M, Bethune DW, Latimer RD. A comparison of five heat and moisture exchangers. Anaesthesia. 1986;41(5):527–32.
Tilling SE, Hancox AJ, Hayes B. An accurate method of measuring medical humidifier output. Clin Phys Physiol Meas. 1983;4(2):197–209.
Boisson C, et al. Changing a hydrophobic heat and moisture exchanger after 48 hours rather than 24 hours: a clinical and microbiological evaluation. Intensive Care Med. 1999;25(11):1237–43.
Davis K Jr, et al. Prolonged use of heat and moisture exchangers does not affect device efficiency or frequency rate of nosocomial pneumonia. Crit Care Med. 2000;28(5):1412–8.
Thomachot L, et al. Changing heat and moisture exchangers after 96 hours rather than after 24 hours: a clinical and microbiological evaluation. Crit Care Med. 2000;28(3):714–20.
Thomachot L, et al. Efficacy of heat and moisture exchangers after changing every 48 hours rather than 24 hours. Crit Care Med. 1998;26(3):477–81.
Dery R. Humidity in anesthesiology III. Heat and moisture patterns in the respiratory tract during anesthesia with the semi-closed system. Can Anaesth Soc J. 1967;14:287–98.
Dery R. The evolution of heat and moisture in the respiratory tract during anesthesia with a nonrebreathing system. Can Anaesth Soc J. 1973;20:296–309.
Chalon J, et al. The pall ultipor breathing circuit filter--an efficient heat and moisture exchanger. Anesth Analg. 1984;63(6):566–70.
Cigada M, et al. The efficiency of twelve heat and moisture exchangers: an in vitro evaluation. Int Care World. 1990;7:98–101.
Gedeon A, Mebius C. The hygroscopic condenser humidifier. A new device for general use in anaesthesia and intensive care. Anaesthesia. 1979;34(10):1043–7.
Unal N, et al. An experimental set-up to test heat-moisture exchangers. Intensive Care Med. 1995;21(2):142–8.
Lellouche F, Simard S, Bouchard PA. Monitoring of heated wire humidifier MR850 hygrometric performances with heater plate temperature. Respir Care. 2022;67(9):1147–53.
Lavoie-Berard CA, et al. Impact of airway humidification strategy in the mechanically ventilated COVID-19 patients. Respir Care. 2021;67(2):157–66.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Lellouche, F. (2023). Main Techniques for Evaluating the Performances of Humidification Devices Used for Mechanical Ventilation. In: Esquinas, A.M. (eds) Humidification in the Intensive Care Unit. Springer, Cham. https://doi.org/10.1007/978-3-031-23953-3_3
Download citation
DOI: https://doi.org/10.1007/978-3-031-23953-3_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-23952-6
Online ISBN: 978-3-031-23953-3
eBook Packages: MedicineMedicine (R0)