Abstract
Several chronic lung diseases that affect the airways, including chronic obstructive pulmonary disease, obstructive cystic fibrosis, and bronchial asthma, can be defined from a pathophysiological point of view as muco-obstructive diseases. These diseases are characterized by exacerbations that when severe needed hospitalization and intensive care unit admission. The management of bronchial secretions is one of the main problems encountered during the intensive care management of patients with muco-obstructive diseases. The early start of airway clearance techniques is a fundamental part of the management to reduce the negative impact on patients’ prognosis. A wide range of therapeutic options as techniques and devices are present for managing bronchial encumbrance during intensive care unit stay, but up to now, for all airway clearance techniques, there is an insufficient evidence to affirm the superiority of one technique over another. Moreover, data on their use in conjunction with NIV is lacking. A personalized tailored approach for a single patient is mandatory. Rarely is just one single technique used for a given pathological condition. The best approach is to combine the best effect on the clearance of the airways with the lowest possible incidence of side effects. A trained experienced staff is fundamental to achieving successful treatment. Multicenter randomized controlled trials should be well designed and conducted in this setting to try to resolve the many controversies that exist in this area.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Several chronic lung diseases that affect the airways, including chronic obstructive pulmonary disease (COPD), obstructive cystic fibrosis (oCF), and bronchial asthma, can be defined from a pathophysiological point of view as muco-obstructive diseases (MODs) [1]. These diseases are characterized by exacerbations that when severe needed hospitalization and intensive care unit (ICU) admission [2]. MODs being part of all these diseases can be considered to be also characterized by episodic exacerbations, and their pathogenesis is generally correlated with an increase in bronchial secretions with a change in its rheology [3]. In these conditions, mucus in the small airways cannot be cleared by cough and accumulates, forming the nidus for airflow obstruction, infection, and inflammation which have a key role in respiratory failure development that need intensive care assistance [3]. Unfortunately, a large amount of bronchial secretions is a frequent cause of noninvasive mechanical ventilation (NIV) failure [4, 5]. The management of bronchial secretions is one of the main problems encountered during the intensive care management of patients with MODs. The early start of airway clearance techniques (ACTs) is a fundamental part of the management to reduce the negative impact on patients’ prognosis. They aim to reduce airway obstruction induced by increased secretions occupying the airway lumen and so prevent respiratory tract infections and re-expand the collapsed areas of the lung, thus improving gas exchange and decreasing the pro-inflammatory response [6, 7]. A wide range of therapeutic options as techniques and devices are present on the market for managing bronchial encumbrance during ICU stay, but up to now, for all ACTs, there is an insufficient evidence to affirm the superiority of one technique over another [8]. A personalized tailored approach for a single patient is mandatory. Rarely is just one single technique used for a given pathological condition. The best approach is to combine the best effect on the clearance of the airways with the lowest possible incidence of side effects. A trained experienced staff is fundamental to achieving successful treatment.
2 Role of Airway Clearance in MODs
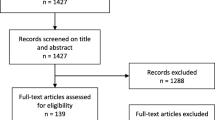
In healthy subjects, mucus secretion, hydration, and clearance play a key role in host defense against lower airway infections. The mucus secretion and hydration in distal airways are regulated by the transport of ions and fluids across the luminal membrane of the lining epithelial cells. In healthy subjects, a well-hydrated mucus layer is transported rapidly at a rate of approximately 50 μm/s from the distal airways toward the trachea [7]. In the MODs like oCF, COPD, and bronchial asthma, the mucus may be retained in the airways due to mucus hyper-concentration (like in oCF or asthma) or defective ciliary function (like in COPD). Retained secretions in the trachea can be expectorated in the form of sputum if there is adequate cough instead of mucus retained in the peripheral airways that cannot be expectorated [9]. MODs are characterized by acute exacerbations involving a vicious circle of airway inflammation, mucin hypersecretion, and mucus retention leading to the formation of mucus plugs. Retained secretions induce airway obstruction with increased airway resistance and thus work of breathing, lung hyperinflation, impaired ventilation/perfusion (V/P) ratio, and lung atelectasis formation, especially in the dependent lung areas. These factors contribute to respiratory failure development [1]. In such cases, the airway clearance techniques (ACTs) are useful in removing secretions from the lower airways of patients suffering from disorders that preclude normal secretion removal. Patients with MODs have both respiratory failure and secretion retention. The use of NIV for respiratory failure may be challenging in patients with retained secretions which necessitates the concurrent use of ACTs. Effective clearance of secretions is also essential for acute and chronic successful treatment with NIV. ACTs include proximal techniques (which help in clearing secretions from central airways) and peripheral techniques (which help in mobilizing secretions from peripheral airways) [8]. The proximal techniques help in augmenting the cough for the removal of secretions from the central airways, and it is generally used when patients have an impaired cough reflex. These are further sub-classified based on whether the inspiratory or expiratory muscles are supported. A mechanical in-exsufflator (MI-E) is the standard approach to treating a patient characterized by impaired cough reflex [10]. Patients with neuromuscular disorders are typical patients with impaired cough reflex that benefit from the use of this treatment [11]. Unfortunately, until now there are poor data about the benefits and risks of utilizing MI-E in patients with MODs because impaired cough reflex levels in this specific population during ICU stay have not been systematically evaluated. Investigating the presence of impaired cough reflex in patients with MODs admitted to ICU is mandatory to early start MI-E to help patients in clearing secretions from the large airways. The main objective is to select the best positive and negative pressure to achieve the best peak expiratory cough flow (PECF). However, only through monitoring ventilator pressure and flow waveform trends, we can achieve the best results [12]. The peripheral techniques assist in the proximal mobilization of the secretions from the small airways using oscillations that can be applied directly to the airways (intrapulmonary percussive ventilation [IPV]) or indirectly transmitted from the body surface (high-frequency chest wall oscillation [HFCWO], manual chest physiotherapy or postural drainage) [8]. A brief description of peripheral airway clearance techniques that can be used alone or in conjunction with NIV in intensive care unit is reported in Table 23.1. In addition, certain pharmacological treatments have been used to change the properties of the mucus to enable easier mobilization. Proper setting of NIV and ACTs is critical, and these represent the real challenges shortly to improve the chances of success and minimize failures and adverse events. The complexity to understand the impact of ACT technologies on NIV is very high. Only poor studies have tried to analyze the best setting [13, 14]. Starting from a respiratory pathophysiology model to understand the impact of secretions retentions on NIV failure is mandatory. Lower airway mucus obstruction induced increased airway resistance which leads to a decrease in peak inspiratory and expiratory flow, while the time required for flow to reach zero during inspiration and expiration tends to increase. These mechanisms mediated a reduction of tidal volume and in MODs can enhance intrinsic positive end-expiratory pressure (iPEEP) that can mediate NIV asynchronies [15]. Another important aspect is to early detect the presence of secretion in the lower airway during NIV. In this case the flow waveform shows characteristic oscillations (Fig. 23.1). The most important determinants during ACTs are to achieve the best peak inspiratory flow (PIF) and peak expiratory flow (PEF) and to follow the best flow waveform changes and the trends in tidal volume variation [12]. Another key element is to know the impact of the NIV interface used (nasal versus oro-facial or total face mask), its internal volume, and the leaks to predict the efficacy of the NIV-ACT combination treatment. A standardized protocol (to correctly select the best frequency, the best time, and the best period) to apply NIV and ACTs in patients with MODs during ICU stay is necessary [16]. It is mandatory to develop a specific clinical model of ACTs in adult and pediatric patients. Now poor data are showing how to incorporate ACTs to improve NIV because the rationale of this approach is to be sure that ACTs are an effective treatment. Today there is a great variability in the clinical practice between countries and health professionals on how to understand and try to resolve the problem of secretion retention [17, 18]. Airway clearance defects impact negatively on NIV and mechanical ventilation success during ICU stay. Multicenter randomized controlled trials should be well designed and conducted in this setting to try to resolve the many controversies that exist in this area. The main ACTs utilized in MODs during the ICU stay, oCF, COPD, and bronchial asthma, are reported below.
3 Airway Clearance in Acute Exacerbation of Bronchial Asthma
Asthma is a heterogeneous disease, characterized by chronic airway inflammation. It is defined by the history of respiratory symptoms such as wheeze, shortness of breath, chest tightness, and cough that vary over time and in intensity, together with variable expiratory airflow limitation [19]. Asthma exacerbations can be life-threatening, with 25,000–50,000 such patients per year requiring admission to an ICU in the United States [20]. Mucociliary clearance is altered in asthma, and mucus plugging of proximal and distal lower airways can mainly mediate death in patients during cases of fatal asthma [21]. Moreover, mucus plugging limits aerosol delivery, contributes to airway obstruction, and is one of the main causes of NIV failure. This notion by itself should set mucus hypersecretion among the most relevant therapeutic targets in severe asthma attacks that need ICU admission. Few studies have examined the effect of NIV (either biphasic positive airway pressure [BiPAP] ventilation or continuous positive airway pressure [CPAP]) in patients with life-threatening asthma exacerbation (LTAE). A Cochrane review concluded that the use of NIV with the standard of care may be beneficial but should be used cautiously [22]. Unfortunately, the usefulness of ACTs in LTAE alone or conjunction with NIV or CPAP is generally unknown. No randomized controlled trials are available, but only a few clinical cases report. Firstly Barach and Beck [23] used MI-E in 76 patients with “bronchopulmonary disease,” including asthma, emphysema, and bronchiectasis. When using MI-E with bronchodilator aerosols, they found average vital capacity (VC) increases of 15% in 12 patients with bronchial asthma with reported marked improvement in dyspnea. This exceeded the VC improvements with the bronchodilator alone, but it is unclear whether the improvements were due to better distribution of aerosol during the insufflation phase (and, thus, better, relief of bronchoconstriction), lung recruitment, a reduction of obstructing airway secretions, or all of the above. Importantly, Barach and Beck reported no significant complications in their studies. Successful use of high-frequency percussive ventilation (HFPV) for a status asthmaticus in a patient failing conventional mechanical ventilation was reported in a single-case report, but larger studies are needed to verify its efficacy [24]. Finally, only one randomized, double-masked, controlled clinical trial investigated the role of HFCWO in the treatment of asthma exacerbation [25]. The authors concluded that HFCWO is feasible and may improve dyspnea during asthma exacerbations, but further research is needed to evaluate the role of HFCWO in improving clinical outcomes in this population.
4 Airway Clearance in Acute Exacerbation of Chronic Obstructive Pulmonary Disease (COPD)
Patients hospitalized for severe acute exacerbations of chronic obstructive pulmonary disease (AECOPD) with rapid clinical deterioration should be considered for NIV to prevent further deterioration in gas exchange and respiratory workload as well as the need for endotracheal intubation [26]. Airway inflammation, bronchospasm, and the increase in sputum volume are constant in these patients, and they are responsible for an increase in lower airways resistance and air trapping. In addition, increased secretions can lead to NIV failure and the need for intubation and invasive mechanical ventilation [27]. ACTs aim to remove sputum from the lower airways; however, literature data on their efficacy during AECOPD is unclear. Bellone et al. demonstrated that chest physiotherapy using a positive expiratory pressure mask in patients with mild acidosis requiring NIV with pressure support could produce benefits in sputum clearance and could reduce the amount of time that the patient requires NIV [28]. Several peripheral airway clearance techniques have been studied in AECOPD, but data on their use in conjunction with NIV is lacking [16]. Cough flows have value in predicting successful extubation and mortality rate in patients with COPD [29]. Cough augmentation with MI-E produces a significant increase in peak cough flow (PCF) and facilitates airway secretion clearance in NMDs [11]. Concerning COPD only early publications are available with controversial results [30]. Barach et al. describe some benefits [23], instead of Sivasothy et al. that reported that MI-E decreased PCF and did not induce significantly improvement, suggesting that it may even exacerbate hyperinflation [31]. Winck et al. in a prospective clinical trial demonstrated that MI-E improved oxygenation and breathlessness without a significant improvement in PCF, but also without any deterioration in breathing pattern or pulmonary parameters concluding that MI-E may be a potential complement to NIV, and may help reduce the frequency of pulmonary complications caused by retention of secretions with good tolerance and reduced adverse effects. However, further evaluation is warranted in a larger patient population [30]. IPV should be an interesting ACT to enhance intrabronchial secretion mobilization in conjunction or in association with NIV. A randomized controlled study was aimed to show that the use of IPV could prove effective in avoiding further deterioration in patients with AECOPD with mild respiratory acidosis. Exacerbation worsened in 6 of 17 patients in the control group versus 0 of 16 in the IPV group (p < 0.05). The hospital stay was also significantly shorter in the IPV group [32]. Antonaglia et al. evaluated in a randomized controlled trial the effect of IPV by mouthpiece during NIV with helmet in patients with AECOPD. A benefit in favor of the NIV-helmet plus IPV group was found in terms of reduction of the duration of ventilatory treatment and ICU stay and improvements in gas exchange at intensive care unit discharge. Improvement in gas exchange and other physiologic variables was found after the first IPV session [33]. Further studies are needed to confirm the advantage of adding IPV sessions to the strongly recommended practice of NIV and to improve the selection of the patients likely to benefit from IPV, before being able to adopt a “strength through unity for the noninvasive challenges” [34]. A systematic review evaluated the effect of ACTs in patients experiencing an AECOPD has shown that in patients with respiratory failure, techniques that apply positive pressure to the airways may reduce either the need for or duration of NIV and hospital length of stay [35]. It was notable that all other techniques were applied in the reviewed studies, including breathing exercises, postural drainage (PD), chest wall vibration, coughing, huffing, intermittent positive pressure breathing, positive expiratory pressure (PEP) mask therapy, and IPV, which were applied without any reported adverse effects. HFCWO was investigated in AECOPD with negative results [36]. Some of the issues that could have altered these negative results include that oscillation frequency is influenced by the degree of changes in expiratory flow and expiratory volume changes. Thus, a patient selection must be performed carefully in providing a patient-specific therapy. This is both a practical and physiologically relevant approach, due to variations in lung functions, airway resistance, and compliance among a heterogeneous group of acute COPD patients. It is also known that the frequency of HFCWO application must be personalized and should be set on parameters such as the severity of AECOPD and the extent of airway secretions. Further clinical studies focusing on the patient-specific parameters such as an airway secretion score and intrinsic predictive risk factors associated with AECOPD can be useful in understanding the influence of HFCWO on AECOPD during ICU stay [37]. Growing data show how also high-flow nasal cannula (HFNC) can represent a safe and effective therapeutic option in the management of AECOPD [38]. In addition, this device can provide to administer heated and humidified oxygen preventing oxidative damage and mucus drying. This can suggest the use of HFNC in COPD patient management with mucus hypersecretion/retention and impaired mucociliary clearance mechanism. However, there are no data about HFNC’s effectiveness in preventing and treating muco-obstructive events.
5 Airway Clearance in Acute Exacerbation of Obstructive Cystic Fibrosis Bronchiectasis
Cystic fibrosis (CF), a single-gene disease, is characterized by autosomal recessive mutation (chemical change) in the CF gene-related termed as cystic fibrosis transmembrane conductance regulator (CFTR) protein [39]. The CFTR protein forms a chloride channel that has a key role in efficient mucus transport. Mutations in CFTR induce impaired chloride secretion, sodium reabsorption, and water transport, inducing a hyper mucus concentration and impaired mucociliary clearance [39]. Dehydrated and hyper viscous mucus secretions are correlated to lead endobronchial mucus stagnation and thus lower airway infection with a narrow spectrum of distinctive bacteria inducing a chronic inflammatory response that mediate the development of severe bronchiectasis [39]. Patients can develop acute or chronic respiratory failure that needs long-term oxygen therapy with or without NIV [40]. Literature data show several studies on airway clearance which have specifically recruited patients on long-term NIV instead of little scientific evidence of the role of ACTs alone or in conjunction with NIV during acute exacerbation of oCF [41,42,43]. These studies included patients who were not already on NIV for their management. The addition of NIV to chest physiotherapy in patients with acute exacerbation of oCF has been found to reduce muscle fatigue, dyspnea, and hypoxemia. MI-E has a potentially key role in CF patients with respiratory muscle weakness, especially in the presence of respiratory failure. In this setting, it has an advantage over NIV, as the latter is unable to provide active exsufflation. In a series of two CF patients with acute exacerbation, this approach proved a good profile in terms of safety and efficacy in achieving airway clearance [44]. However, patients must be monitored for dynamic airway compression or wheeze. In patients with cystic fibrosis, ACTs are the mainstay of secretion management. These include breathing manoeuvers (autogenic drainage and active cycle of breathing technique) and positive expiratory pressure devices. The choice of ACTs should be individualized based on the patient’s clinical status, lung function, and local availability and expertise [45]. The use of peripheral ACTs in conjunction with NIV via a nasal mask in patients with both stable or acute exacerbation of cystic fibrosis is associated with reduced respiratory muscle fatigue. The use of ACTs in a combination with NIV may also result in reduced dyspnea and hypoxemia. The use of hydration such as hypertonic saline before ACT may improve patient satisfaction and lung function [16].
6 Conclusions
MODs like obstructive CF, COPD, and bronchial asthma are characterized by exacerbations that when severe needed hospitalization and intensive care unit (ICU) admission. The management of bronchial hypersecretion is one of the main problems encountered during the intensive care management and a frequent cause of noninvasive mechanical ventilation (NIV) failure. The early start of airway clearance techniques (ACTs) is a fundamental part of the management to reduce the negative impact on patients’ prognosis. Data on their use in conjunction with NIV is lacking. A personalized tailored approach for a single patient is mandatory. Rarely is just one single technique used for a given pathological condition. The best approach is to combine the best effect on the clearance of the airways with the lowest possible incidence of side effects. It is mandatory to develop a specific clinical model of ACTs alone and in conjunction with NIV in adult and pediatric patients with MODs.
Key Messages
-
Chronic lung diseases such as COPD, bronchial asthma, and CF are characterized during acute exacerbation by mucus hypersecretion/retention and impaired mucociliary clearance that can negatively impact patients’ prognosis during ICU stay.
-
The management of bronchial hypersecretion is one of the main problems encountered during intensive care management and a frequent cause of NIV failure.
-
The early start of airway clearance techniques (ACTs) is a fundamental part of the management of these patients.
-
The best approach is to combine the best effect on the clearance of the airways with the lowest possible incidence of side effects. It is mandatory to develop a specific clinical model of ACTs alone and in conjunction with NIV in adult and pediatric patients with MODs.
-
Proper setting of NIV and ACTs is critical, and these represent the real challenges shortly to improve the chances of success and minimize failures and adverse events.
-
Multicenter randomized controlled trials should be well designed and conducted in this setting to try to resolve the many controversies that exist in this area.
Abbreviations
- ACTs:
-
Airway clearance techniques
- AECOPD:
-
Acute exacerbations of chronic obstructive pulmonary disease
- BiPAP:
-
Biphasic positive airway pressure
- CF:
-
Cystic fibrosis
- CFTR:
-
Cystic fibrosis transmembrane conductance regulator
- COPD:
-
Chronic obstructive pulmonary disease
- CPAP:
-
Continuous positive airway pressure
- HFCWO:
-
High-frequency chest wall oscillation
- HFNC:
-
High-flow nasal cannula
- ICU:
-
Intensive care unit
- iPEEP:
-
Intrinsic positive end-expiratory pressure
- IPV:
-
Intrapulmonary percussive ventilation
- LTAE:
-
Life-threatening asthma exacerbation
- MCC:
-
Mucociliary clearance
- MI-E:
-
Mechanical in-exsufflator
- MODs:
-
Muco-obstructive diseases
- NIV:
-
Noninvasive mechanical ventilation
- oCF:
-
Obstructive cystic fibrosis
- PECF:
-
Peak expiratory cough flow
- PEF:
-
Peak expiratory flow
- PEP:
-
Positive expiratory pressure
- PIF:
-
Peak inspiratory flow
- PD:
-
Postural drainage
- VC:
-
Vital capacity
References
Boucher RC. Muco-obstructive lung diseases. N Engl J Med. 2019;380(20):1941–53. https://doi.org/10.1056/NEJMra1813799.
Scala R. Respiratory high-dependency care units for the burden of acute respiratory failure. Eur J Intern Med. 2012;23(4):302–8. https://doi.org/10.1016/j.ejim.2011.11.002.
Fahy JV, Dickey BF. Airway mucus function and dysfunction. N Engl J Med. 2010;363(23):2233–47. https://doi.org/10.1056/NEJMra0910061.
Carlucci A, Richard JC, Wysocki M, Lepage E, Brochard L, Ventilation SCGoM. Noninvasive versus conventional mechanical ventilation. An epidemiologic survey. Am J Respir Crit Care Med. 2001;163(4):874–80. https://doi.org/10.1164/ajrccm.163.4.2006027.
Volsko TA. Airway clearance therapy: finding the evidence. Respir Care. 2013;58(10):1669–78. https://doi.org/10.4187/respcare.02590.
Randell SH, Boucher RC, University of North Carolina Virtual Lung G. Effective mucus clearance is essential for respiratory health. Am J Respir Cell Mol Biol. 2006;35(1):20–8. https://doi.org/10.1165/rcmb.2006-0082SF.
Wanner A, Salathe M, O'Riordan TG. Mucociliary clearance in the airways. Am J Respir Crit Care Med. 1996;154(6):1868–902. https://doi.org/10.1164/ajrccm.154.6.8970383.
Belli S, Prince I, Savio G, Paracchini E, Cattaneo D, Bianchi M, et al. Airway clearance techniques: the right choice for the right patient. Front Med. 2021;8:544826. https://doi.org/10.3389/fmed.2021.544826.
Button B, Goodell HP, Atieh E, Chen YC, Williams R, Shenoy S, et al. Roles of mucus adhesion and cohesion in cough clearance. Proc Natl Acad Sci U S A. 2018;115(49):12501–6. https://doi.org/10.1073/pnas.1811787115.
Homnick DN. Mechanical insufflation-exsufflation for airway mucus clearance. Respir Care. 2007;52(10):1296–305; discussion 306-7.
Auger C, Hernando V, Galmiche H. Use of mechanical insufflation-exsufflation devices for airway clearance in subjects with neuromuscular disease. Respir Care. 2017;62(2):236–45. https://doi.org/10.4187/respcare.04877.
Volpe MS, Guimaraes FS, Morais CC. Airway clearance techniques for mechanically ventilated patients: insights for optimization. Respir Care. 2020;65(8):1174–88. https://doi.org/10.4187/respcare.07904.
Nicolini A, Grecchi B, Ferrari-Bravo M, Barlascini C. Safety and effectiveness of the high-frequency chest wall oscillation vs intrapulmonary percussive ventilation in patients with severe COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:617–25. https://doi.org/10.2147/COPD.S145440.
Longhini F, Bruni A, Garofalo E, Ronco C, Gusmano A, Cammarota G, et al. Chest physiotherapy improves lung aeration in hypersecretive critically ill patients: a pilot randomized physiological study. Crit Care. 2020;24(1):479. https://doi.org/10.1186/s13054-020-03198-6.
Vignaux L, Vargas F, Roeseler J, Tassaux D, Thille AW, Kossowsky MP, et al. Patient-ventilator asynchrony during non-invasive ventilation for acute respiratory failure: a multicenter study. Intensive Care Med. 2009;35(5):840–6. https://doi.org/10.1007/s00134-009-1416-5.
Hadda V, Suri TM, Pahuja S, El-Khatib M, Ciobanu LD, Cabrita B, et al. Secretion management in patients with ineffective airway clearance with non-invasive mechanical ventilation use: expert guidance for clinical practice. Monaldi Arch Chest Dis. 2021;91(4):1499. https://doi.org/10.4081/monaldi.2021.1499.
Ntoumenopoulos G, Hammond N, Watts NR, Thompson K, Hanlon G, Paratz JD, et al. Secretion clearance strategies in Australian and New Zealand intensive care units. Aust Crit Care. 2018;31(4):191–6. https://doi.org/10.1016/j.aucc.2017.06.002.
Connolly B, Barclay M, Blackwood B, Bradley J, Anand R, Borthwick M, et al. Airway clearance techniques and use of mucoactive agents for adult critically ill patients with acute respiratory failure: a qualitative study exploring UK physiotherapy practice. Physiotherapy. 2020;108:78–87. https://doi.org/10.1016/j.physio.2020.06.003.
Reddel HK, Bacharier LB, Bateman ED, Brightling CE, Brusselle GG, Buhl R, et al. Global initiative for asthma strategy 2021: executive summary and rationale for key changes. Eur Respir J. 2022;59(1):2102730. https://doi.org/10.1183/13993003.02730-2021.
Garner O, Ramey JS, Hanania NA. Management of life-threatening asthma: severe asthma series. Chest. 2022. https://doi.org/10.1016/j.chest.2022.02.029.
Kuyper LM, Pare PD, Hogg JC, Lambert RK, Ionescu D, Woods R, et al. Characterization of airway plugging in fatal asthma. Am J Med. 2003;115(1):6–11. https://doi.org/10.1016/s0002-9343(03)00241-9.
Ram FS, Wellington S, Rowe BH, Wedzicha JA. Non-invasive positive pressure ventilation for treatment of respiratory failure due to severe acute exacerbations of asthma. Cochrane Database Syst Rev. 2005;1:CD004360. https://doi.org/10.1002/14651858.CD004360.pub2.
Barach AL, Beck GJ. Exsufflation with negative pressure; physiologic and clinical studies in poliomyelitis, bronchial asthma, pulmonary emphysema, and bronchiectasis. AMA Arch Intern Med. 1954;93(6):825–41. https://doi.org/10.1001/archinte.1954.00240300019003.
Albecker D, Glen Bouder T, Franklin LB. High frequency percussive ventilation as a rescue mode for refractory status asthmaticus - a case study. J Asthma. 2021;58(3):340–3. https://doi.org/10.1080/02770903.2019.1687714.
Krishnan JS, Bilderback AL, Diette GB. Feasibility of high frequency chest wall oscillation (HFCWO) for treatment of asthma exacerbations. Chest. 2004;126:721. https://doi.org/10.1378/chest.126.4_MeetingAbstracts.721S-b.
American Thoracic Society. International consensus conferences in intensive care medicine: noninvasive positive pressure ventilation in acute respiratory failure. Am J Respir Crit Care Med. 2001;163(1):283–91. https://doi.org/10.1164/ajrccm.163.1.ats1000.
Plant PK, Owen JL, Elliott MW. Non-invasive ventilation in acute exacerbations of chronic obstructive pulmonary disease: long term survival and predictors of in-hospital outcome. Thorax. 2001;56(9):708–12. https://doi.org/10.1136/thorax.56.9.708.
Bellone A, Spagnolatti L, Massobrio M, Bellei E, Vinciguerra R, Barbieri A, et al. Short-term effects of expiration under positive pressure in patients with acute exacerbation of chronic obstructive pulmonary disease and mild acidosis requiring non-invasive positive pressure ventilation. Intensive Care Med. 2002;28(5):581–5. https://doi.org/10.1007/s00134-002-1210-0.
Bach JR, Saporito LR. Criteria for extubation and tracheostomy tube removal for patients with ventilatory failure. A different approach to weaning. Chest. 1996;110(6):1566–71. https://doi.org/10.1378/chest.110.6.1566.
Winck JC, Goncalves MR, Lourenco C, Viana P, Almeida J, Bach JR. Effects of mechanical insufflation-exsufflation on respiratory parameters for patients with chronic airway secretion encumbrance. Chest. 2004;126(3):774–80. https://doi.org/10.1378/chest.126.3.774.
Sivasothy P, Brown L, Smith IE, Shneerson JM. Effect of manually assisted cough and mechanical insufflation on cough flow of normal subjects, patients with chronic obstructive pulmonary disease (COPD), and patients with respiratory muscle weakness. Thorax. 2001;56(6):438–44. https://doi.org/10.1136/thorax.56.6.438.
Vargas FB, Boyer A, Salmi LR, Gbikpi-Benissan G, Guenard H, Gruson D, Hilbert G. Intrapulmonary percussive ventilation in acute exacerbations of COPD patients with mild respiratory acidosis: a randomized controlled trial. Crit Care Med. 2005;9(4):382–9. https://doi.org/10.1186/cc3724.
Antonaglia V, Lucangelo U, Zin WA, Peratoner A, De Simoni L, Capitanio G, et al. Intrapulmonary percussive ventilation improves the outcome of patients with acute exacerbation of chronic obstructive pulmonary disease using a helmet. Crit Care Med. 2006;34(12):2940–5. https://doi.org/10.1097/01.CCM.0000248725.15189.7D.
Vargas F, Hilbert G. Intrapulmonary percussive ventilation and noninvasive positive pressure ventilation in patients with chronic obstructive pulmonary disease: “strength through unity”? Crit Care Med. 2006;34(12):3043–5. https://doi.org/10.1097/01.CCM.0000248523.61864.D5.
Hill K, Patman S, Brooks D. Effect of airway clearance techniques in patients experiencing an acute exacerbation of chronic obstructive pulmonary disease: a systematic review. Chron Respir Dis. 2010;7(1):9–17. https://doi.org/10.1177/1479972309348659.
Goktalay T, Akdemir SE, Alpaydin AO, Coskun AS, Celik P, Yorgancioglu A. Does high-frequency chest wall oscillation therapy have any impact on the infective exacerbations of chronic obstructive pulmonary disease? A randomized controlled single-blind study. Clin Rehabil. 2013;27(8):710–8. https://doi.org/10.1177/0269215513478226.
Esquina AM, Patel B, Pravinkumar E. High-frequency chest wall oscillation in infective exacerbation of COPD: is airway secretion clearance the cornerstone? Clin Rehabil. 2014;28(2):206–7. https://doi.org/10.1177/0269215513508685.
Bruni A, Garofalo E, Procopio D, Corrado S, Caroleo A, Biamonte E, et al. Current practice of high flow through nasal cannula in exacerbated COPD patients. Healthcare. 2022;10(3):536. https://doi.org/10.3390/healthcare10030536.
Stoltz DA, Meyerholz DK, Welsh MJ. Origins of cystic fibrosis lung disease. N Engl J Med. 2015;372(4):351–62. https://doi.org/10.1056/NEJMra1300109.
Moran F, Bradley JM, Piper AJ. Non-invasive ventilation for cystic fibrosis. Cochrane Database Syst Rev. 2017;2:CD002769. https://doi.org/10.1002/14651858.CD002769.pub5.
Holland AE, Denehy L, Ntoumenopoulos G, Naughton MT, Wilson JW. Non-invasive ventilation assists chest physiotherapy in adults with acute exacerbations of cystic fibrosis. Thorax. 2003;58(10):880–4. https://doi.org/10.1136/thorax.58.10.880.
Placidi G, Cornacchia M, Polese G, Zanolla L, Assael BM, Braggion C. Chest physiotherapy with positive airway pressure: a pilot study of short-term effects on sputum clearance in patients with cystic fibrosis and severe airway obstruction. Respir Care. 2006;51(10):1145–53.
Dwyer TJ, Robbins L, Kelly P, Piper AJ, Bell SC, Bye PT. Non-invasive ventilation used as an adjunct to airway clearance treatments improves lung function during an acute exacerbation of cystic fibrosis: a randomised trial. J Physiother. 2015;61(3):142–7. https://doi.org/10.1016/j.jphys.2015.05.019.
Gaynor M, Wood J. Mechanical insufflation-exsufflation for airway clearance in adults with cystic fibrosis. Respirol Case Rep. 2018;6(4):e00307. https://doi.org/10.1002/rcr2.307.
Chaudary N, Balasa G. Airway clearance therapy in cystic fibrosis patients insights from a clinician providing cystic fibrosis care. Int J Gen Med. 2021;14:2513–21. https://doi.org/10.2147/IJGM.S274196.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Ruggeri, P., Profazio, C., Nucera, F. (2023). Airway Clearance in Chronic Respiratory Disorders: Obstructive CF, COPD, and Asthma. In: Esquinas, A.M. (eds) Humidification in the Intensive Care Unit. Springer, Cham. https://doi.org/10.1007/978-3-031-23953-3_23
Download citation
DOI: https://doi.org/10.1007/978-3-031-23953-3_23
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-23952-6
Online ISBN: 978-3-031-23953-3
eBook Packages: MedicineMedicine (R0)