Abstract
Regional anesthesia plays an important role in the management of pain in trauma patients and may affect outcomes in specific injuries. Trauma is a leading cause of mortality and morbidity in the United States and throughout the world, especially among younger patients. Neuraxial anesthesia and peripheral nerve blockade techniques have become increasingly common in the care of trauma patients, a trend likely to continue as the benefits of regional anesthesia become more valued and opioid-sparing regimens increase in popularity. Pain due to acute injuries is often undertreated as treatment of life-threatening injuries and resuscitation take priority over pain management early in the hospital course. Once patients are stabilized and relevant life-threatening injuries addressed, analgesia should not be unnecessarily delayed. This chapter provides overview of the role of regional anesthesia in trauma, along with several common injuries (burns, rib fractures, etc.), but should not limit the procedural options available to the regional anesthesiologist treating a victim of trauma.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Case StemA 33-year-old male patient arrives in the emergency room after extraction from a motor vehicle crash. The patient was a restrained passenger in a vehicle that struck a tree at approximately 45 mph. He has received 1 L of intravenous fluids during transport, along with an unknown amount of IV morphine. After a negative FAST exam and trauma survey, a thorough evaluation by the ED and trauma staff reveals a head laceration and diffuse tenderness and bruising over the right lateral chest wall. Vital signs are now in the normal range except for a blood pressure of 144/82 and a heart rate of 102. The patient has a GCS of 15 and complains of sharp pain along the right chest. A cervical collar immobilization device is in place. Imaging reveals non-displaced fractures of ribs four through six in the right mid-axillary line. The regional anesthesia service is consulted for assistance with pain management.
FormalPara Questions and Answers-
1.
What is the impact of trauma in the United States?
Among those less than 45 years old, trauma is the leading cause of death. In 2011, inpatient care for trauma patients exceeded $30 billion, and the economic burden of trauma is estimated at $500 billion annually. The most common causes of trauma include falls (47%) and motor vehicle crashes (7%). Trauma due to violent assault is more common in those 18–44 years old. The extremities are disproportionately affected in trauma. With the use of modern military armor, more battlefield participants are surviving with higher rates of extremity injuries. The rate of extremity injury in motor vehicle crash survivors is also high [1].
-
2.
What types of injuries can be treated with regional anesthetic techniques?
Peripheral nerve blocks can be performed for almost any painful extremity injury. These blocks usually spare systemic side effects and are site-specific. Furthermore, there is strong evidence that regional anesthesia may decrease length of stay in the ICU and hospital. For upper extremity injuries, brachial plexus blocks (interscalene, supraclavicular, infraclavicular, and axillary approaches), as well as blockade of individual nerves and digital blocks distally, can be performed. For lower extremity injuries, blockade along the femoral and sciatic nerves and their branches are commonly performed, though other blocks can be useful for select patients. Truncal blocks, such as thoracic epidurals, paravertebral, erector spinae plane, and transversus abdominal plane blocks, and less commonly performed serratus plane, PECS, and intercostal blocks may also be part of the regional anesthesiologist’s toolkit.
-
3.
Why are multimodal regimens that include regional anesthesia techniques often preferred over intravenous opioids?
The most common method of treating pain in trauma patients continues to be intravenous opioids. However, opioids carry a significant adverse effect profile, including: pruritus, immunosuppression, respiratory depression, hypotension, delirium, constipation, nausea and vomiting, and increased length of hospital stay. Opioids may interfere with the ability to perform neurologic assessments, and potentially lead to addiction. Multimodal regimens for pain treatment have several advantages over opioid-based therapy and are becoming standard of care for both surgical and trauma patients. Along with other IV and oral medications, including ketamine, NSAIDs, acetaminophen, dexmedetomidine, and gabapentin, both neuraxial and regional techniques have important roles in reducing trauma pain in appropriate patients. A reduction in opioid use also decreases the need for intensive monitoring, which may confer a cost savings for health systems with high staffing outlays.
-
4.
What patients are candidates for Neuraxial blocks versus Peripheral nerve blocks?
Often, a thoracic or lumbar epidural, or single-injection spinal can provide effective analgesia for proximal traumatic injuries. In fact, a thoracic epidural is considered the gold standard for chest and abdominal analgesia. However, there are several limitations to neuraxial procedures. An infrequent but catastrophic complication of neuraxial anesthesia is spinal hematoma. Many trauma patients are coagulopathic due to blood loss, hypothermia, sepsis, or liver injuries. Perioperative thromboprophylaxis and widespread use of anticoagulation agents further complicate neuraxial patient selection and procedural timing. Current guidelines are readily available and suggest avoiding neuraxial procedures, including epidural catheter removal, when the INR exceeds 1.4. Epidurals are generally avoided in patients with significant head or spine injuries as neurologic evaluation can be complicated. Finally, neuraxial local anesthetics often cause sympatholysis and hypotension. Patients who are under-resuscitated or hypotensive at baseline may not be ideal candidates for neuraxial analgesia, although vasopressors can be utilized to counteract these effects to an extent. Peripheral nerve blocks offer an option to provide excellent analgesia for trauma patients when neuraxial anesthesia is contraindicated.
-
5.
Who should receive a continuous catheter versus a single-injection block?
Pain associated with trauma is often severe and longstanding, and development of chronic pain is common after trauma caused by musculoskeletal injury. Whereas ropivacaine or bupivacaine single-injection blocks often provide 16–24 h of analgesia, continuous nerve block catheters can substantially prolong the duration of pain relief. While nerve block catheters are typically removed within 5–7 days due to the risk of infection, some have been left in for weeks. Patients who require repeated procedures, such as skin grafting, debridements, or serial fracture repairs, and those with more complex injuries, are likely to benefit from continuous nerve block catheters. Studies have consistently demonstrated a catheter-specific complication rate under 5% at 8 days, and catheter infection rates of 0–3%. When multiple catheters are utilized in polytrauma patients, care must be taken to ensure that local anesthetics in the plasma do not reach toxic levels. While continuous infusion catheters have several advantages for analgesia, many patients, such as those expected to be discharged quickly, those with sepsis or an active infection in the vicinity of the block, or those unable to tolerate a catheter, are better suited for single-injection blocks [2].
-
6.
Can peripheral nerve blocks be performed in the field or Emergency Department (ED)?
While anesthesiologists are the most qualified physicians to perform nerve blocks, they are rarely able to attend to patients in the emergency department. However, studies have shown that regional anesthesia performed in the ED decreases length of stay and improves clinical flows [3]. Some blocks, such as fascia iliaca blockade for hip fractures, can be relatively safely performed without ultrasound guidance. Digital blocks, sciatic, interscalene, and others have been successfully performed in the field for pain control prior to arrival at a hospital. New technologies, such as handheld ultrasonography, may also increase trauma patient access to timely regional anesthetics.
-
7.
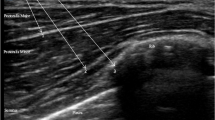
What blocks are appropriate for shoulder reduction?
Dislocated shoulders are common in trauma patients, and shoulder reductions are often performed in the emergency department. IV sedation is routinely employed to provide muscular relaxation, but carries risks of gastric aspiration, respiratory depression, hypotension. An interscalene approach to the brachial plexus block effectively anesthetizes the superior trunk and offers an excellent alternative to sedation. The pulmonary status of the patient must be understood, as an interscalene block often affects the phenic nerve resulting in ipsilateral diaphragmatic paralysis. Nonetheless, the risks of hypotension, aspiration, and apnea are minimized with this approach. Monitoring costs and emergency room length of stay are reduced when an interscalene block is employed compared to procedural sedation [4].
-
8.
What blocks are appropriate for digital amputation or replantation?
Amputation injuries can be classified as guillotine (clean cut), crush, avulsion, and surgical. Clean cut amputations carry the best prognosis for functional recovery. Surgical amputations are often performed when distal tissues have no chance of survival (due to ischemia, temperature injuries, infection, etc.). When multiple digits are to be replanted, the thumb is given first priority as it is responsible for 40% of hand function. Warm ischemia permitted time for digits is approximately 12 h, while icing can increase this time to beyond 30 h.
Single-injection blocks are highly beneficial for surgical amputations, which are often short procedures. Digital replantations are often time-consuming, often taking up to 18 h for multiple replants. This limits the utility of single-injection nerve blockade for replantation procedures. However, it is well-established that regional anesthesia will reduce the surgical stress response and decrease the likelihood of vasospasm and thrombosis in the affected digits. For this reason, a general anesthetic combined with a continuous nerve block catheter is often the best option. For upper extremity digital replantations, a brachial plexus or forearm catheter not only improves pain control, but also establishes a chemical sympathectomy, which inhibits neurogenic vasospasm. While catheters placed anywhere along the brachial plexus can produce hand analgesia, interscalene blocks often fail to anesthetize the inferior trunk, and catheters at the axilla are prone to dislodging. Thus, supraclavicular or infraclavicular catheters are often placed. Finally, patients undergoing a digital replantation are usually subsequently anticoagulated for several days. Placing perineural catheters in anticoagulated patients remains somewhat controversial but is no longer contraindicated.
-
9.
What are some regional anesthetic considerations for patients with burns?
Depending on the location and depth of the burn, burn injury pain can be highly variable. When peripheral nociceptors are destroyed, pain transmission is blunted. However, nociceptors that are not destroyed transmit the painful stimulus immediately and can stimulate a secondary hyperalgesia. Furthermore, burn patients often undergo multiple rounds of procedures, including debridement, dressing changes, and skin grafting. Peripheral nerve blocks are effective for treating burn-related superficial pain, when used correctly. They can reduce opioid consumption and decrease exposure to repetitive general anesthetics. However, there are numerous challenges to utilizing regional anesthesia in these patients. Burn patients are susceptible to infections due to an altered immune response and skin compromise. The placement of a nerve block catheter through burned skin is contraindicated. For deep burns likely to require multiple procedures, single-injection techniques are of little benefit. Continuous nerve block catheters are often a better choice, as local anesthetic boluses can be administered prior to anticipated painful procedures.
Approximately 10% of burn patients also have other traumatic injuries, and many present with burns at multiple anatomic locations [5]. Placement of multiple peripheral nerve catheters is not uncommon. In these cases, care must be taken to avoid systemic toxicity from the local anesthetics.
-
10.
What blocks are appropriate for patients with acute hip fractures?
Acute hip fractures are associated with severe pain, reduced quality of life, and long-term functional impairment. Perioperative delirium is also common in elderly hip fracture patients. It is prudent to minimize opioid use in these patients. Several studies have been published suggesting that regional anesthesia should be initiated as soon as possible in these patients. Femoral nerve blocks or fascial iliaca blocks will cover the majority of the pain at this site but are insufficient for complete surgical analgesia. Even a lumbar plexus block will spare the articular branches from the sacral plexus and input from the sciatic nerve. Thus, open reduction internal fixation of hip fractures are most commonly performed with neuraxial anesthesia, but there are several advantages to also placing a continuous catheter at a proximal femoral nerve location for postoperative pain control [6].
-
11.
What blocks are appropriate for patients with rib fractures?
Rib fractures are a common source of trauma-related pain, and account for more than 10% of trauma-related hospital admissions. Although pneumothorax and lung contusion are often associated with rib fractures and are independent causes of morbidity, significant pain worsens pulmonary status by limiting patients’ ability to breathe adequately. Even in rib fracture patients without an oxygen requirement, shallow tidal breathing can lead to subsequent atelectasis and increase the risk of pneumonia [7]. In most rib fracture patients, operative fixation is not necessary and deferred.
There are several options for effective analgesia involving regional anesthesia. Thoracic epidurals are highly effective, especially when the fractures are bilateral. Other regional anesthesia techniques that can be utilized for rib fractures include paravertebral catheters, erector spinae plane catheters, or serratus anterior catheters.
-
12.
What peripheral nerve blocks are appropriate for patients with chest tubes?
Similar to the treatment of rib fracture pain, the anesthesiologist has many options for treating pain arising due to chest tubes, which can be debilitating. Chest tubes are often placed following chest injuries or surgeries in the thoracic cavity to facilitate healing and prevent pneumothorax. Thoracic epidurals, paravertebral blocks, erector spinae plane blocks, serratus anterior plane blocks, intercostal blocks, and intrapleural blocks have all been successfully utilized for treating chest tube pain. When not contraindicated, thoracic epidural analgesia can be highly effective when bilateral chest tubes are placed in trauma or post-surgical patients. Thoracotomy and chest tube-related pain has a high incidence of evolving into chronic pain [8]. Regional anesthesia techniques can decrease the probability of developing chronic pain following incisions or injuries to the chest wall [9].
-
13.
What peripheral nerve blocks are appropriate for penetrating abdominal trauma?
Penetrating abdominal traumas are common and often require a surgical laparotomy after transport to a medical center. The anterior rami of T7 through L1 innervate the abdominal wall. These sensory fibers travel between the second and third muscle layers in the chest and abdomen (between the internal oblique and transversus abdominis muscles) and ultimately terminate at the midline. Although the thoracic epidural has been considered the gold-standard block for the abdomen, more recently, paravertebral, erector spinae plane, transversus abdominis plane, and rectus sheath blocks have increased in popularity due to their improved safety profiles. Abdominal compartment syndrome is intra-abdominal hypertension leading to organ dysfunction. Truncal regional anesthesia can improve the prognosis in abdominal compartment syndrome by increasing abdominal wall compliance [10].
-
14.
Should peripheral nerve blocks be performed on patients with concern for compartment syndrome?
Acute compartment syndrome (ACS) is excessive pressure within a closed compartment which impedes circulation and tissue function within the affected space. Trauma is a leading cause of ACS, with fractures of the tibia and forearm (areas packed with muscles) representing common injuries associated with ACS. Higher risk categories for compartment syndrome include tibial plateau fractures, crush injuries, and prolonged extrication. An emergent fasciotomy is the definitive treatment, as ischemia, myonecrosis, hyperkalemia, and even death can result if not performed within 3–6 h.
ACS has traditionally been diagnosed on the basis of paresthesia with pain out of proportion to the injury. This had spurred fears among both surgeons and anesthesiologists of regional techniques masking ACS pain and delaying the diagnosis of ACS. The vast majority of case reports to date have suggested that ACS after nerve blockade leads to breakthrough pain, which may aid the early diagnosis of ACS [11]. Furthermore, compartment pressure monitoring can routinely be performed for high-risk trauma patients. One consideration when performing regional blocks in trauma patients at risk for ACS may be the use of dilute local anesthetic solutions to allow for breakthrough pain. Although large scale studies are still needed, continuous nerve block catheters are now considered safe and effective in patients at risk for ACS. Catheters can be adjusted, left dry, stopped, or bolused as appropriate for the clinical setting [12].
1 Summary
In addition to enhancing the comfort of trauma patients, techniques employed by the regional anesthesiologist reduce opioid requirements, shorten ED and hospital stays, reduce costs, and improve patient satisfaction with the healthcare system. Often, there are numerous modality options for treating a trauma patient’s pain, and it is up to the regional anesthesiologist to determine the optimal regimen. Ultimately, the decision of whether to utilize a regional anesthetic is made in a multidisciplinary approach after a complete assessment of patient factors and the nature of the injury, in consultation with other providers. Table 1 summarizes the most common regional treatment modalities based on the location of injury.
Common Pitfalls
-
Local anesthetic systemic toxicity (LAST) occurs when plasma levels of local anesthetics reach a toxic concentration. Care should always be taken to avoid exceeding the maximum safe dose of regional anesthetic, especially when performing two or more blocks on the same patient, administering bolus doses, and/or using high infusion rates of concentrated drugs. Blocks associated with high risk of LAST include: paravertebral, intercostal, intrapleural, epidural, and brachial plexus blocks. The clinical manifestation of LAST classically involves seizures, loss of consciousness, and cardiovascular complications (most commonly bradycardia). When suspected, treatment involves cessation of local anesthetic injection, circulatory support (with avoidance of vasopressors other than low-dose epinephrine), and lipid emulsion therapy.
-
Failure to consider a patient’s coagulation status or anticoagulant medications prior to performing a neuraxial block significantly increases the risk of epidural or spinal hematoma and serious complications. Strict guidelines are readily available and periodically revised. In general, neuraxial blockade is contraindicated with an INR >1.4.
Clinical Pearls
-
Trauma is a leading cause of hospitalization and death in the United States
-
Pain is often underappreciated and undertreated in trauma patients as life and limb-saving treatments are prioritized over pain management.
-
Regional anesthetic techniques, including neuraxial analgesia and peripheral nerve blocks, can decrease opioid requirements, minimize opioid-related side effects, and decrease overall morbidity.
-
Well-established guidelines exist to identify candidates for neuraxial blocks. When neuraxial or other deep blocks are contraindicated, there are often reasonable alternative blocks to consider. For patients not suitable for, or amenable to, regional techniques, multimodal regimens are often advantageous to opioid-based therapy.
-
Effective regional anesthesia for digital reimplantation may improve graft success rates.
-
There are many special considerations in burn victims. Continuous nerve block catheters are especially beneficial in this population.
-
Regional analgesic methods for treating rib fracture pain directly improve respiratory status, decrease opioid-related respiratory depression, and reduce the risk of pulmonary complications.
-
Peripheral nerve blocks may reduce the incidence of delirium, chronic post-traumatic pain, and post-traumatic stress disorder (PTSD), although more research is needed.
-
With modern diagnostic and monitoring tools, peripheral nerve blocks are safe and effective for patients at risk for acute compartment syndrome.
References
DiMaggio C, et al. Traumatic injury in the United States: in-patient epidemiology 2000-2011. Injury. 2016;47:1393–403.
Morin AM, Kerwat KM, Klotz M, et al. Risk factors for bacterial catheter colonization in regional anesthesia. BMC Anesthesiol. 2005;5(1):1.
Grabinsky A, Sharar SR. Regional anesthesia for acute traumatic injuries in the emergency room. Expert Rev Neurother. 2009;9(11):1677–90.
Blaivas M, Adhikari S, Lander L. A prospective comparison of procedural sedation and ultrasound-guided interscalene nerve block for shoulder reduction in the emergency department. Acad Emerg Med. 2011;18:922–7.
Hadzic A. Hadzic’s textbook of regional anesthesia and acute pain management. 2nd ed. New York: McGraw-Hill Education; 2017. p. 977–85.
Slade IR, Samet RE. Regional anesthesia and analgesia for acute trauma patients. Anesthesiol Clin. 2018;36(3):431–54.
Karmakar MK, Ho AM-H. Acute pain management of patients with multiple fractured ribs. J Trauma. 2003;54(3):615–25.
Fleming I, Egeler C. Regional anaesthesia for trauma: an update. Contin Educ Anaesth Crit Care Pain. 2014;14(3):136–41.
Davies RG, Myles PS, Graham JM. A comparison of the analgesic efficacy and side-effects of paravertebral vs epidural blockade for thoracotomy—a systematic review and meta-analysis of randomized trials. Br J Anaesth. 2006;96(4):418–26.
Gadsden J. Regional anesthesia in trauma: a case-based approach. Cambridge: Cambridge University Press; 2012.
Mar GJ, Barrington MJ, McGuirk BR. Acute compartment syndrome of the lower limb and the effect of postoperative analgesia on diagnosis. Br J Anaesth. 2009;102:3–11.
Walker BJ, Noonan KJ, Bosenberg AT. Evolving compartment syndrome not masked by a continuous nerve block: evidence-based case management. Reg Anesth Pain Med. 2012;37:393–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Simmons, B., Hollis, N. (2023). Must-Known Special Considerations for Acute Pain Management in Trauma and Non-OR Patients. In: Li, J., Jiang, W., Vadivelu, N. (eds) First Aid Perioperative Ultrasound. Springer, Cham. https://doi.org/10.1007/978-3-031-21291-8_37
Download citation
DOI: https://doi.org/10.1007/978-3-031-21291-8_37
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-21290-1
Online ISBN: 978-3-031-21291-8
eBook Packages: MedicineMedicine (R0)