Abstract
Cerebral palsy (CP) is a neurodevelopmental disorder characterized by abnormal movement or posture. CP can have many different causes, but genomic copy number variants are causal in at least 4% of patients with typical CP, and at least 14% have disease-causing single nucleotide variants or indels. Pathogenic genomic lesions of major effect probably account the neurological deficits in more than twice as many patients with atypical CP, i.e., neuromotor dysfunction with additional neurodevelopmental abnormalities or malformations, or with MRI findings and medical history that are not characteristic of a perinatal insult. Disease-causing variants of many different genetic loci can produce a CP-like phenotype, and most genetic changes of major effect that cause CP arise as de novo mutations. The importance of genetic variants of minor effect and of epigenetic modifications in producing a multifactorial predisposition to CP is unclear.
Recognizing the specific cause of CP in an affected individual is essential to providing optimal clinical management. An etiological diagnosis provides families an “enhanced compass” that improves overall well-being, facilitates access to educational and social services, permits accurate genetic counseling, and may make precision therapy that targets the pathophysiology available. Trio exome sequencing with assessment of copy number or trio genome sequencing is indicated in the initial clinical workup of children with CP, especially those with additional malformations or neurodevelopmental abnormalities.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Cerebral palsy
- Atypical cerebral palsy
- Movement disorder
- Copy number variant
- Single nucleotide variant
- Multifactorial
- Exome sequencing
- Genome sequencing
- Twin studies
- Epigenetics
- Therapy
To understand/gain insight into:
-
The type of genetic aberrations underlying cerebral palsy and of the mode(s) of inheritance.
-
The reported yield of genetic investigations (including chromosomal micro-array analysis, exome sequencing) in cerebral palsy.
-
The difference in yield of genetic testing between typical and atypical cerebral palsy patients.
-
The importance of establishing an underlying diagnosis in patients with cerebral palsy.
-
At least 4% of patients with cerebral palsy have disease-causing copy number variants, and at least 14% have disease-causing single nucleotide variants or indels.
-
In patients in whom cerebral palsy-like neuromotor dysfunction occurs with additional malformations or neurodevelopmental abnormalities, the rate of disease-causing genomic lesions is more than twice as high.
-
Aberrations of many different genetic loci can produce a cerebral palsy-like phenotype.
-
Most, but not all, gene or chromosomal mutations that cause cerebral palsy occur de novo.
-
Recognizing the cause of cerebral palsy in an affected patient is essential to providing optimal clinical management, including precision therapy.
-
Genome-wide (exome or genome) sequencing is indicated in the initial work-up of patients with cerebral palsy, especially those who have additional neurodevelopmental abnormalities or malformations.
Introduction
Cerebral palsy (CP) is not a homogeneous disease entity but rather an etiologically diverse group of conditions characterized by abnormal movement or posture with onset early in development [1,2,3,4,3]. It has been known for more than 50 years that some patients with clinical features of cerebral palsy have a genetic syndrome or inherited metabolic disorder [4, 5], but for a long time such cases were considered to be highly exceptional. We now know that they are not — it has become apparent in the past decade that many patients with developmental abnormalities of motor function have an underlying genetic disease of major effect, such as a Mendelian disorder or chromosomal abnormality.
The structural and/or functional central nervous system abnormalities that underlie CP may have their origin at conception, during embryonic or foetal development, during the perinatal period, or in early childhood. A major genetic cause is most likely when the condition has obvious prenatal onset, but the clinical features of CP may not become manifest until later in life in other instances. Non-genetic factors, such as teratogenic exposures, hypoxia, hemorrhage or infections, may also cause CP, and in some other patients the cause is a combination of non-genetic and genetic factors. ‘Genetics’ is definitely plural when referring to CP.
Patients with CP are often classified clinically into spastic, hypotonic, dystonic (also called ‘dyskinetic’), ataxic, and mixed subgroups and by the limbs involved (diplegia, hemiplegia or quadriplegia, and occasionally other patterns) [1,2,3,4,5]. Each of these clinical subgroups and patterns of involvement is also etiologically and genetically heterogeneous, and while certain major genetic forms of CP characteristically produce only one particular kind of involvement, the clinical presentation of other genetic forms of CP is variable [1, 6].
Clinical definitions of CP require that the condition be non-progressive, and developmental abnormalities of movement or posture that become worse with time are sometimes called ‘atypical CP’ or ‘cerebral palsy mimics’ [6, 7]. Distinguishing progressive from non-progressive neuromotor abnormalities is important for clinical management but may present difficulties in genetic analysis of these conditions for several reasons [8]. Firstly, disease progression occurs over time and may not be apparent when a child is initially evaluated. Secondly, the rate of progression may be very slow, and the functional loss may not become apparent until later in life. Thirdly, some patients are very severely involved from birth, and it may not be possible to recognize disease progression clinically. Fourthly, disease progression may not affect motor function but become apparent in other ways, such as intractability of seizures to treatment, loss of vision or speech, or cognitive decline. In addition, genetic diseases that can cause CP are often quite variable in their manifestations and course from patient to patient, so that disease progression may be obvious in some individuals but not in others with the same condition. Finally, specific treatment is available for some diseases that may present as CP [9], and the treatment may prevent progression of the neuromotor symptoms.
In this chapter, we consider the genetics and genomics of both non-progressive and progressive neurodevelopmental movement disorders because almost all reported studies include some patients who have typical CP and others who are atypical or may become so later in their course. The information is organized by study design: twin and other family studies (without genetic testing), association studies, studies of chromosomal abnormalities or genomic copy number variants, studies of Mendelian diseases caused by single nucleotide variants or indels, and epigenetic studies. This organization also generally reflects the time when the studies were done, with genome-wide sequencing and epigenetic studies being most recent, and the others, earlier.
Twin and Other Family Studies
Hundreds of studies have been published that include twins with CP, but such studies are difficult to interpret with respect to genetic causation because being born of a twin pregnancy is itself strongly associated with the occurrence of CP. Luu and Vohr [10] and Pharoah and Dundar [11] summarized data from CP registry studies and found a substantially greater frequency of CP in twins than in birth registries for the same jurisdictions. CP was reported in 6.3–12.6 per 1000 twins who survived infancy in comparison to 1.0–2.3 per 1000 surviving singleton infants. A population-based study performed through the Medical Birth Registry of Norway found 3649 children who developed CP and 22,558 pairs of twins among 2,036,741 infants born between 1967 and 2002. [12] The prevalence of CP was three times greater among the twins (5.1 per 1000) than among singleton births (1.7 per 1000). After reviewing such data, Briana and Malamitsi-Puchner [13] emphasized the importance of low birth weight and premature delivery, which frequently occur in twin pregnancies, in mediating the development of CP.
Twin studies have been used for almost 150 years to infer genetic causation of familial traits based on recognition that monozygotic twins share all of their genes in common, while dizygotic twins resemble ordinary sibs, sharing about half of their genes [14]. The studies discussed in the previous paragraph comparing the rate of CP in twins to that in singleton pregnancies or the general population ignore zygosity and thus cannot be used to assess the importance of genetic factors in the occurrence of CP.
A study of the population-based Western Australia CP Registry identified 74 sets of twins born between 1956 and 1985 in which one or both members of the pair had CP. [15] The rate of concordance for CP in monozygotic twins was significantly higher than that in dizygotic twins (p = 0.0026). In contrast, concordance for CP was observed in 4 (20%) of 20 monozygotic twin pairs and 10 (40%) of 25 dizygotic twin pairs in a series collected by a single physician over a 21-year period. [16] The fact that concordance was not complete among monozygotic twins is consistent with the known etiological heterogeneity of CP and formally proves that all cases are not caused by major genetic factors.
Very few studies of CP in twins have confirmed zygosity by genetic testing, but monochorionic placentation is strongly associated with the occurrence of CP in twins. [17, 18] Almost all dizygotic pregnancies have dichorionic placentation, and most monozygotic pregnancies are monochorionic, but about 30% of monozygotic pregnancies are dichorionic [19]. Chorionicity is, therefore, an imprecise surrogate for zygosity. The proportion of twin pregnancies that is monozygotic, rather than dizygotic, varies greatly in different populations and has changed in the last few decades as a result of fertility treatments that increase the frequency of pregnancies with two or more genetically distinct foetuses.
The association of monochorionic placentation with CP may largely be attributable to the occurrence of placental vascular anastomoses between the circulatory systems of the twins [20, 21]. Monochorionic placentation is also associated with increased frequencies of intrauterine death of one or both twins, preterm delivery, severe discordance in birth weight between the twins, foetal growth restriction, and congenital anomalies, all of which are also associated with the occurrence of CP [10, 11, 13].
No twin studies have been reported that assess the effect of genetic factors on the occurrence of CP in proven monozygotic versus dizygotic (or monochorionic vs. dichorionic) twins after removing the effects of placental vascular anastomosis, intrauterine death of one twin, preterm delivery, severe birth weight discordance, foetal growth restriction and other congenital anomalies.
Studies that have compared the frequency of CP in co-twins of unknown zygosity to the frequency of CP in sibs of children with CP born of singleton pregnancies have found higher rates of co-occurrence of CP in the twin sibs.
A Norwegian population-based record linkage study [12] found the prevalence of CP to be 79/1000 in the co-twins of children with CP, 15/1000 in the sibs of singleton children with CP, 8.5/1000 in the children of parents with CP, 2.6/1000 in the second-degree relatives of children with CP, and 2.5/1000 in the third degree relatives of children with CP. The prevalence of CP was 1.5/1000, 1.6/1000 and 1.6/1000, respectively in first-, second- and third-degree relatives of individuals without CP in this study. A subsequent publication expanded this investigation by adding four more years of data to include a total of 5707 children with CP and 26,485 twin pairs among 2,297,408 children who survived the neonatal period [22]. In the expanded study, the co-twins of children with CP had a 27-fold greater than expected risk of having CP, and the full sibs of children with CP born of singleton pregnancies had a 6.4-fold greater risk of having CP. The sibs of children with CP born of singleton pregnancies also had higher than expected risks of stillbirth, neonatal death, intellectual disability, autism spectrum disorder, deafness, blindness, epilepsy, attention deficit hyperactivity disorder and schizophrenia. All these risks were even higher among the co-twins of children with CP born of twin pregnancies.
A Swedish population-based record linkage study that included 3997 patients with CP found that the risk of hospitalization for CP was 4.8 times greater than expected among the sibs of individuals with CP born of singleton pregnancies and 29 times greater than expected among the co-twins of individuals with CP born of twin pregnancies. [23]
These data indicate that genetic factors are often important in the aetiology of CP. The studies are compatible with a multifactorial mechanism or with genetic heterogeneity, with some cases resulting from genetic variants of major effect and others having a non-genetic cause. A multifactorial mechanism in some cases, various major genetic factors in other cases, and non-genetic causation in still others seems most likely.
Candidate Gene Association Studies
Association studies are used to identify genetic loci that predispose to or protect against the development of a disease. They are usually based on an assumption that the disease is multifactorial, i.e., caused by a complex combination of many different minor genetic and non-genetic factors.
Association studies of at least 160 different genetic variants in at least 60 candidate genes have been reported in patients with CP and corresponding control groups. Table 35.1 lists the genes and variants (mostly SNPs) that have been assessed in these studies. Most of these genetic loci were chosen for study because of their known involvement in blood clotting, vascular regulation or inflammation, processes that are thought to be important in the pathogenesis of, or physiological response to, perinatal intracranial bleeding [24,25,26]. These studies vary in terms of how the CP was defined, how the patients were ascertained, and what populations the patients represented [26, 27]. Most of the studies are small: the largest candidate gene association study of CP reported to date includes 763 cases [27], but many have fewer than 100 cases.
Although associations with CP have been reported with polymorphic genetic variants near or within a dozen different genes [27,28,29,30,31,32,33,34,35,36,37,38], none of these associations has been replicated in an independent investigation. Many of the reported associations are inverse or ‘protective,’ meaning that patients with the more frequent allele in the population are at higher risk, a counterintuitive observation. Even more associations have been observed in ad hoc subgroups of CP patients, but none of these has been independently replicated, and such observations are suspect for statistical reasons [24,25,26].
The inability to replicate candidate gene association studies is a common observation in complex diseases [39, 40]. Independent replication is essential because candidate disease association studies are often confounded by issues related to disease definition, patient ascertainment, population stratification, publication bias and statistical analysis. More recent genetic association studies of many complex diseases address these problems through genome-wide testing of tens of thousands or more SNPs in homogenous groups of thousands to tens of thousands of patients. We are not aware of any published genome-wide association studies of patients with CP [41], and it seems unlikely that this approach would be informative unless the known aetiological and pathogenetic heterogeneity of CP were taken into account in patient selection and data analysis.
Studies of Chromosomal Abnormalities and Genomic Copy Number Variants
Major genetic factors are those that are both necessary and sufficient to cause a particular disease in a patient. Clinically, major genetic causes of disease include inherited or de novo Mendelian disorders and chromosomal abnormalities. At a molecular level, the changes that cause genetic disease of major effect are alterations of nucleotide sequence, genomic copy number or genomic structure, alone or in combination. Most mutations that cause inherited or de novo Mendelian diseases are alterations of nucleotide sequence, usually single nucleotide variants. Alterations of genomic copy number or structure are conventionally called ‘chromosomal abnormalities’ because microscopic (cytogenetic) analysis has been used to identify them for more than 60 years. However, most disease-causing genomic alterations are too small to be visualized under the light microscope and require molecular techniques such as chromosomal microarray analysis or genome sequencing for detection.
Anecdotal reports of patients with CP and various chromosomal abnormalities have occasionally appeared in the medical literature [42,43,44,45], and a few patients with segmental gain or loss of genomic material large enough to be seen cytogenetically and a ‘cerebral palsy’ phenotype are reported in the DECIPHER or ClinVar databases (Table 35.2). However, we are not aware of any study describing the results of routine cytogenetic testing in a large series of patients with CP.
In a study of data from eleven European CP registries, 13 (0.3%) of 4584 children with CP born between 1976 and 1996 were reported to have chromosomal abnormalities detected by cytogenetic analysis [46]. This must be a minimal estimate because the techniques available for identifying genomic imbalance were much less sensitive at that time than they are today and because cytogenetic analysis was infrequently done on children with CP, which was usually assumed to have been caused by perinatal anoxia or intracranial bleeding.
Segmental gains or losses of genomic material are usually called ‘deletions’ or ‘duplications’ if they can be demonstrated under the microscope and ‘copy number variants’ (CNVs) if they are smaller (generally <10 Mb) and require the use of molecular techniques, such as chromosomal microarray analysis (CMA) or exome sequencing, to be detected. Much smaller (1–50 bp) genomic gains or losses that can only be identified by sequencing are called ‘indels’.
Variability is a normal feature of the human genome. The nucleotides of two unrelated people differ by about 1% of their total nucleotide sequence or content and by more than 20,000 CNVs, on average [47]. Most of these variants occur as polymorphisms in the general population and are inherited from one parent or the other, and most are thought to be unrelated to the occurrence of CP or any other disease. A small fraction of the genomic variants in each of us arise de novo as a result of new mutations.
There are two critical steps in identifying disease-causing CNVs in patients with CP. The first is recognition of the genomic variant, which is usually done by CMA or DNA sequencing, and the second is determining that the variant is, in fact, capable of causing disease. Rare CNVs that are both necessary and sufficient to cause a genetic disease are classified as ‘pathogenic’ or ‘likely pathogenic’ according to standard laboratory criteria [48]. Most CNVs that are unrelated to the occurrence of a genetic disease can be classified as ‘benign’ or ‘likely benign’. We are unable to determine whether some other CNVs have an effect on the phenotype – such variants are classified as being of ‘uncertain significance’.
A few individual patients with CP and other neurodevelopmental abnormalities who were found to have apparently disease-causing CNVs have been described in the medical literature [49,50,51], but it is impossible to determine if the co-occurrence of CP and the CNV in these anecdotal cases reflects a causal or coincidental relationship. Dozens of patients with various pathogenic or likely pathogenic CNVs and CP are listed in the ClinVar [52] or DECIPHER [53] databases (Table 35.2). Almost all of these patients have other neurodevelopmental conditions in addition to CP, and a few are reported also to have malformations of other organ systems or dysmorphic features. Most of the CNVs seen in these patients are unique; very few are recurrent copy number changes that are recognized causes of specific genetic syndromes (Table 35.2).
In one remarkable family, nine individuals with spastic quadriplegia and intellectual disability where found by molecular techniques to carry a 225 kb copy number loss of chromosome 9p24.3 that includes the KANK1 (ANKRD15) gene [54]. This CNV, which was transmitted through at least four generations, is incompletely penetrant but appears to have caused the CP in affected family members. Individuals with various KANK1 copy number losses from other families do not usually have CP [55].
DECIPHER provides a list of 66 genetic syndromes that are caused by CNVs [56]. None of these conditions includes CP as a cardinal feature. However, some children with the Phalen-McDermid (22q13 deletion) syndrome are diagnosed with cerebral palsy because they have neonatal hypotonia, delayed walking and unsteady gait [57].
Seven patient series have determined the frequency of CNVs among individuals with CP (Table 35.3). Most of these studies found that relatively few (0–6%) of the CP patients had disease-causing CNVs. One exception was a series of 52 patients with disabling non-progressive pyramidal and/or extra pyramidal signs beginning before 3 years of age and no periventricular leukomalacia or spinal cord lesions and no history of hypoxic ischemic encephalopathy, brain infarction, encephalitis or head trauma [58]. Sixteen pathogenic or likely pathogenic CNVs were found in 16 (31%) of these atypical CP patients. Patients in the other series who had disease-causing CNVs often had other neurodevelopmental disorders such as intellectual disability, autism or epilepsy, and some had structural malformations of the brain or other organ systems. Unfortunately, however, the clinical descriptions, apart from their CP, reported for patients in these series are limited.
Most disease-causing CNVs in CP patients occur de novo, rather than being inherited from one of the parents. This is true of disease-causing CNVs in other neurodevelopmental disorders as well [59, 60].
The pathogenic/likely pathogenic CNVs reported in these CP patient series involved many different chromosomal regions. This observation is consistent with the heterogeneous genetic aetiology of CP discussed above. However, it is interesting that some specific CNVs were reported in patients in two different series: del(22)(p11.21), dup(22)(p11.21), and duplication of the entire X chromosome in males (Table 35.3). The clinical syndromes associated with these CNVs (velocardiofacial/Di George syndrome, 22q11 duplication syndrome and Klinefelter syndrome, respectively) are well characterized, but cerebral palsy is not a usual feature of any of them.
Studies of Single Nucleotide Variants and Indels
Each of us has 4,000,000 to 5,000,000 single nucleotide variants (SNVs) and 700,000 to 800,000 indels (insertions or deletions of 1 to 50 nucleotides) in comparison to the reference human genome sequence [47]. Such ‘small’ alterations of nucleotide sequence are more frequent major causes of genetic disease than larger changes such as chromosomal abnormalities or genomic CNVs. Although small sequence variants can cause Mendelian diseases, most SNVs and indels are simply genomic differences that are transmitted from generation to generation without any apparent effect on the phenotype. SNVs and indels also arise by new mutation in every person. Most of these de novo changes, like the majority of inherited variants, occur outside of the genes and have no effect on the phenotype. However, if a mutation affects a gene, the change may abrogate or alter the gene’s normal function.
Although many different technologies were used to identify disease-causing SNVs and indels in the past, the advent of accurate, rapid, and increasingly cost-effective ‘next-generation’ or ‘second-generation’ DNA sequencing has made it routinely possible to test panels of hundreds or thousands of genes, all protein-coding segments of every gene (the ‘whole exome’), or all of a person’s DNA (the ‘whole genome’) at once. Rare SNVs or indels that are both necessary and sufficient to cause a genetic disease are conventionally classified as ‘pathogenic’ or ‘likely pathogenic’ variants according to standard laboratory criteria [61]. Most SNVs or indels have no influence on the phenotype and can be classified as ‘benign’ or ‘likely benign’, but some variants cannot easily be interpreted and must be classified as variants of uncertain significance. Recognizing the one or two genomic variants that cause a Mendelian disease in an affected person’s exome or genome sequence data requires sophisticated bioinformatics and clinical analysis of the results.
OMIM [62], an online catalogue of human genes and genetic phenotypes, lists 58 genetic diseases that may present as cerebral palsy (Table 35.4). These Mendelian disorders are caused by alterations of 54 different genes. It is important to note that other neurodevelopmental abnormalities occur in all of these diseases and some have multisystem manifestations. Some are progressive and can be recognized as being different from typical CP once this becomes apparent clinically.
The results of exome sequencing have been reported in more than 350 CP or atypical CP patients (Table 35.5). The largest published series, which was recently reported by Jin and associates [63], includes 250 patients with CP defined by standard clinical criteria. This study was performed to explore genetically mediated disease mechanisms in CP, and SNVs and indels were assessed using case-control analyses of patient groups rather than by classification of variants for pathogenicity in each individual patient, as is done when exome sequencing is used clinically. On the basis of their analysis, Jin and associates [63] estimated that CP can be attributed to disease-causing SNVs or indels in at least 14% of patients. This clearly is a minimal estimate of the rate of disease-causing small nucleotide sequence changes among patients with conventionally defined CP [63]. Substantially higher proportions of patients with disease-causing SNVs or indels were observed in the patient series reported by Schnekenberg et al. [64], Takezawa et al. [65], Matthews et al. [66] or Rosello et al. [67], but all of these studies are much smaller and many of the patients included have an atypical form of CP (Table 35.5).
Disease-causing SNVs or indels reported in patients with CP or atypical CP involve 54 different genes (Table 35.6). The diseases caused by genetic alterations at some of these genetic loci are recognized as being associated with clinical features of CP, but 42 (78%) of the genes are not included in the list of genetic conditions that may present as CP (Table 35.4). The clinical features of most of these conditions in Table 35.6 are known to overlap with those of CP, but this is not true for a few of them (marked with an asterisk in Table 35.6). Whether the observation of apparently disease-causing variants of these genetic loci among patients with CP or atypical CP represents an expansion of our knowledge about the phenotypic spectrum of these rare genetic diseases or is simply coincidental is currently uncertain. It is noteworthy, however, that all of the genetic conditions in which a CP-like phenotype occurs also include other neurological abnormalities, and often non-neurological anomalies as well (Tables 35.4 and 35.6). Jin et al. [63] also demonstrated substantial overlap among the genes associated with CP and those associated with intellectual disability, autism or epilepsy.
Epigenetic Studies
Epigenetic mechanisms regulate the transfer of information from the genome, allowing different cell types, organs, body systems and the individual to develop from an undifferentiated zygote and to function throughout life. Although this concept is easy to understand, defining epigenetics in a precise scientific fashion has been surprisingly controversial [68]. Key aspects of epigenetic mechanisms are their dependence on features of the chromatin outside of the DNA sequence itself and the stable, but not invariably fixed, transmission of the epigenetic state of a cell through mitosis and over time. Epigenetic mechanisms also provide a means by which the environment can influence genomic function [69].
Laboratory animal studies have clearly established the importance of epigenetic mechanisms in neurodevelopment and adult neurological function, and many observational investigations are consistent with similar roles in humans [70]. The best-studied epigenetic systems are methylation of DNA and acetylation of histone proteins, but other covalent DNA or histone modifications, non-coding RNAs, and four-dimensional alterations of chromatin structure and its relationship to the nuclear membrane may also act in epigenetic regulation. Moreover, epigenetic changes of one kind can affect other kinds of epigenetic alterations in a multidimensional regulatory network [70].
Crowgey and her associates [71] performed genome sequencing of white blood cell DNA from 16 adolescents with spastic CP and 16 control subjects. Sequencing reads from 1.5 million CpG methylation sites throughout the genome were selected bioinformatically, and the degree of methylation at each site was quantified. Comparison of the CP and control groups found significantly increased or decreased methylation at 0.4% of the CpG sites assessed. Because the study was performed in adolescents, it was not possible to determine whether the methylation differences found reflected the presence of spastic CP (or its treatment) or were markers of the processes that caused the CP in these patients.
This issue was not a concern in a study performed on DNA obtained from archived newborn blood spots of 23 children with various forms of CP and 21 unaffected controls [72]. Using a standard microarray assay of 450,000 variably methylated genomic loci, this study found significantly different methylation of 0.05% of the loci tested. The authors suggest that differential methylation at these loci might predict the development of CP in a child, but, given the probable aetiological heterogeneity of the patients studied, it is unlikely that these differences provide any insight into underlying genetic factors.
Monozygotic twins, who are identical genetically but are discordant with respect to CP, provide an opportunity to assess the effect of non-genetic factors on methylation patterns. Mohandas and her colleagues [73] used a standard 450,000 locus methylation microarray to test archived newborn blood spots from 15 monozygotic pairs in which one twin developed CP and the other did not. No probes were found that exhibited statistically significant differential methylation between the twins with CP and the unaffected co-twins after adjusting for multiple testing, but top-ranked differentially methylated probes below the statistical cutoff involved genes that were associated with immunity and inflammation or with epileptic encephalopathy.
The findings were different in a study of four pairs of monozygotic twins who were discordant for CP and in whom genome-wide methylation was assayed by reduced representation bisulphite genome sequencing [74]. One hundred ninety differentially methylated genes were identified among the discordant twins. Enrichment analysis showed associations with genes involved in cerebral atrophy, and pathway analysis suggested involvement in the biosynthesis of antibiotics, glycolysis/gluconeogenesis and propanoate metabolism.
The Genetics and Genomics of Cerebral Palsy
Building on earlier family and twin studies, recent genomic investigations have clearly demonstrated that genetic factors of major effect cause CP in many patients. Most CNVs and small alterations of nucleotide sequence that have been found to cause CP or atypical CP arise as a result of de novo mutations, so studies that depend on the recurrence frequency within families substantially underestimate genetic contributions to the aetiology of CP.
Studies of series of patients with typical CP suggest that at least 4% have disease-causing CNVs [75,76,77] (Table 35.3) and at least 14% have disease-causing SNVs or indels [63] (Table 35.5). The rates of disease-causing genomic lesions are substantially higher among patients with atypical CP (Tables 35.3 and 35.5). Mutations of many different genetic loci can produce a CP-like phenotype (Tables 35.2, 35.3, 35.4, and 35.6). It seems likely that additional major genetic causes of CP will be recognized as more patients are tested, more sensitive tests (e.g. sequencing of the entire genome) are used, and bioinformatics and clinical interpretation of genomic data improve.
The importance of genetic variants of minor effect and of epigenetic modifications in producing a multifactorial predisposition to CP is less clear. These factors are likely to exist on theoretical grounds, but their involvement has been difficult to demonstrate convincingly. This is probably because of the variety and complexity of such multifactorial predispositions and of the interactions among them in different combinations.
Recognizing the specific cause of CP in a patient is essential to providing optimal clinical management for each affected individual. The financial, emotional and social costs for patients and families affected with CP are great, and obtaining a precise diagnosis provides families an ‘enhanced compass’ that improves overall well-being [78, 79]. Recognizing a specific genetic cause may also facilitate access to educational and social services beyond those that are related to the patient’s physical disability. In addition, treatment targeting pathophysiology is available for a subset of atypical CPs, namely those caused by inherited metabolic diseases [80]. Examples include congenital neuro-transmitter defects and inherited disorders of amino acid metabolism. Early recognition and initiation of therapy (e.g. medical diet, vitamin supplementation, liver transplantation or medication) is essential before irreversible damage is done in patients suffering a treatable Mendelian inherited metabolic disease. Time is brain!
Patients who receive genetic diagnoses and their families benefit by obtaining knowledge of the cause and projected natural history of their condition, and a precise genetic diagnosis is essential for accurate genetic counselling about recurrence in a family. Finally, obtaining a genetic diagnosis ends an expensive, time-consuming and emotionally draining ‘diagnostic odyssey’ for many families.
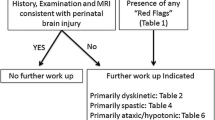
In a substantial fraction of patients with CP, and especially in those whose CP is atypical, an underlying genetic disease is responsible for the neuro-developmental abnormalities. Trio exome sequencing and chromosomal microarray analysis or trio genome sequencing with bioinformatics analysis for CNVs as well as SNVs and indels are clinically indicated in the initial workup of CP patients.
References
Gupta R, Appleton RE. Cerebral palsy: not always what it seems. Arch Dis Childh. 2001;85(5):356–60.
Michael-Asalu A, Taylor G, Campbell H, Lelea L, Kirby RS. Cerebral palsy: diagnosis, epidemiology, genetics, and clinical update. Adv Pediatr. 2019;66:189–208.
Sadowska M, Sarecka-Hujar B, Kopyta I. Cerebral palsy: current opinions on definition, epidemiology, risk factors, classification and treatment options. Neuropsychiatr Dis Treat. 2020;16:1505–18.
Sjogren T, Larsson T. Oligophrenia in combination with congenital ichthyosis and spastic disorders; a clinical and genetic study. Acta Psychiatr Neurol Scand Suppl. 1957;113:1–112.
Lesch M, Nyhan WL. A familial disorder of uric acid metabolism and central nervous system function. Am J Med. 1964;36(4):561–70.
Pearson TS, Pons R, Ghaoui R, Sue CM. Genetic mimics of cerebral palsy. Mov Disord. 2019;34(5):625–36.
MacLennan AH, Lewis S, Moreno-De-Luca A, et al. Genetic or other causation should not change the clinical diagnosis of cerebral palsy. J Child Neurol. 2019;34(8):472–6.
Smithers-Sheedy H, Badawi N, Blair E, et al. What constitutes cerebral palsy in the twenty-first century? Dev Med Child Neurol. 2014;56(4):323–8.
Leach EL, Shevell M, Bowden K, Stockler-Ipsiroglu S, van Karnebeek CDM. Treatable inborn errors of metabolism presenting as cerebral palsy mimics: systematic literature review. Orphanet J Rare Dis. 2014;9(1):197.
Luu TM, Vohr B. Twinning on the brain: the effect on neurodevelopmental outcomes. Am J Med Genet Part C Seminars Med Genet. 2009;151C(2):142–7.
Pharoah POD, Dundar Y. Monozygotic twinning, cerebral palsy and congenital anomalies. Hum Reprod Update. 2009;15(6):639–48.
Tollånes MC, Wilcox AJ, Lie RT, Moster D. Familial risk of cerebral palsy: population based cohort study. Br Med J. 2014;349(2):g4294.
Briana DD, Malamitsi-Puchner A. Twins and neurodevelopmental outcomes: the effect of IVF, fetal growth restriction, and preterm birth. J Matern-Fetal Neonatal Med. 2019;32(13):2256–61.
Burbridge D. Francis galton on twins, heredity and social class. Br J Hist Sci. 2001;34(3):323–40.
Petterson B, Stanley F, Henderson D. Cerebral palsy in multiple births in western australia: genetic aspects. Am J Med Genet. 1990;37(3):346–51.
Laplaza FJ, Root L, Tassanawipas A, Cervera P. Cerebral palsy in twins. Dev Med Child Neurol. 1992;34(12):1053–63.
Burguet A, Monnet E, Pauchard JY, et al. Some risk factors for cerebral palsy in very premature infants: importance of premature rupture of membranes and monochorionic twin placentation. Biol Neonate. 1999;75:177–86.
Adegbite AL, Castille S, Ward S, Bajoria R. Neuromorbidity in preterm twins in relation to chorionicity and discordant birth weight. Am J Obstet Gynecol. 2004;190(1):156–63.
Hall JG. Twinning. Lancet. 2003;362(9385):735–43.
Ortibus E, Lopriore E, Deprest J, et al. The pregnancy and long-term neurodevelopmental outcome of monochorionic diamniotic twin gestations: a multicenter prospective cohort study from the first trimester onward. Am J Obstet Gynecol. 2009;200(5):494.e1–8.
Hack KEA, Koopman-Esseboom C, Derks JB, et al. Long-term neurodevelopmental outcome of monochorionic and matched dichorionic twins. PLoS ONE. 2009;4(8)
Tollånes MC, Wilcox AJ, Stoltenberg C, Lie RT, Moster D. Neurodevelopmental disorders or early death in siblings of children with cerebral palsy. Pediatrics (Evanston). 2016;138(2):e20160269.
Hemminki K, Li X, Sundquist K, Sundquist J. High familial risks for cerebral palsy implicate partial heritable aetiology. Paediatr Perinat Epidemiol. 2007;21(3):235–41.
Wu D, Zou Y, Xu X, et al. The association of genetic polymorphisms with cerebral palsy: a meta-analysis. Dev Med Child Neurol. 2011;53(3):217–25.
Fahey MC, Maclennan AH, Kretzschmar D, Gecz J, Kruer MC. The genetic basis of cerebral palsy. Dev Med Child Neurol. 2017;59(5):462–9.
van Eyk CL, Corbett MA, Maclennan AH. The emerging genetic landscape of cerebral palsy, vol. 147. Netherlands: Elsevier; 2018. p. 331–42.
Sun L, Xia L, Wang M, et al. Variants of the OLIG2 gene are associated with cerebral palsy in chinese han infants with Hypoxic–Ischemic encephalopathy. Neuromol Med. 2018;21(1):75–84.
Djukic M, Gibson CS, MacLennan AH, et al. Genetic susceptibility to viral exposure may increase the risk of cerebral palsy. Aust N Z J Obstet Gynaecol. 2009;49(3):247–53.
Wu YW, Croen LA, Torres AR, Van De Water J, Grether JK, Hsu NN. Interleukin-6 genotype and risk for cerebral palsy in term and near-term infants. Ann Neurol. 2009;66(5):663–70.
Kapitanović Vidak H, Catela Ivković T, Jokić M, Spaventi R, Kapitanović S. The association between proinflammatory cytokine polymorphisms and cerebral palsy in very preterm infants. Cytokine. 2012;58(1):57–64.
Kallankari H, Huusko JM, Kaukola T, et al. Cerebral palsy and polymorphism of the chemokine CCL18 in very preterm children. Neonatology. 2015;108(2):124–9.
Bi D, Wang H, Shang Q, et al. Association of COL4A1 gene polymorphisms with cerebral palsy in a chinese han population. Clin Genet. 2016;90(2):149–55.
Shang Q, Zhou C, Liu D, et al. Association between osteopontin gene polymorphisms and cerebral palsy in a chinese population. Neuromol Med. 2016;18(2):232–8.
Xu J, Xia L, Shang Q, et al. A variant of the autophagy-related 5 gene is associated with child cerebral palsy. Front Cell Neurosci. 2017;11:407.
Xia L, Chen M, Bi D, et al. Combined analysis of interleukin-10 gene polymorphisms and protein expression in children with cerebral palsy. Front Neurol. 2018;9:182.
Torres-Merino S, Moreno-Sandoval HN, Thompson-Bonilla MR, et al. Association between rs3833912/rs16944 SNPs and risk for cerebral palsy in mexican children. Mol Neurobiol. 2018;56(3):1800–11.
Xia L, Xu J, Song J, et al. Autophagy-related gene 7 polymorphisms and cerebral palsy in chinese infants. Front Cell Neurosci. 2019;13:494.
Xu Y, Wang H, Sun Y, et al. The association of apolipoprotein E gene polymorphisms with cerebral palsy in chinese infants. Mol Genet Genomics. 2014;289(3):411–6.
Hirschhorn JN, Lohmueller K, Byrne E, Hirschhorn K. A comprehensive review of genetic association studies. Genet Med. 2002;4(2):45–61.
Siontis KCM, Patsopoulos NA, Ioannidis JPA. Replication of past candidate loci for common diseases and phenotypes in 100 genome-wide association studies. Eur J Hum Genet. 2010;18(7):832–7.
GWAS catalog. <https://www.ebi.ac.uk/gwas/search?query=cerebral%20palsy.>
Jagiello GM. Familial 13–15 translocation abnormality (Denver classification) associated with one case of cerebral palsy. New Engl J Med. 1963;269(2):66–9.
Warkany J, Weinstein ED, Soukup SW, Rubinstein JH, Curless MC. Chromosome analyses in a children’s hospital: selection of patients and results of studies. Pediatrrics. 1964;33:290–305.
Dumars K, Fialko G, Larson E. E trisomy phenotype associated with small metacentric chromosome and a familial Y-22 translocation. Birth Defects Orig Artic Ser. 1976;12(5):97–104.
Menkes JH, Flores-Sarnat L. Cerebral palsy due to chromosomal anomalies and continuous gene syndromes. Clin Perinatol. 2006;33(2):481–501.
Garne E, Dolk H, Krägeloh-Mann I, Holst Ravn S, Cans C. Cerebral palsy and congenital malformations. Eur J Paediatr Neurol. 2008;12(2):82–8.
Eichler EE. Genetic variation, comparative genomics, and the diagnosis of disease. New Engl J Med. 2019;381(1):64–74.
Riggs ER, Andersen EF, Cherry AM, et al. Technical standards for the interpretation and reporting of constitutional copy-number variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics (ACMG) and the Clinical Genome Resource (ClinGen). Genet Med. 2020;22(2):245–57.
Lee RW, Poretti A, Cohen JS, et al. A diagnostic approach for cerebral palsy in the genomic era. NeuroMolecular Medicine. 2014;16(4):821–44.
Zarrei M, Merico D, Kellam B, et al. A de novo deletion in a boy with cerebral palsy suggests a refined critical region for the 4q21.22 microdeletion syndrome. Am J Med Genet Part A. 2017;173(5):1287–93.
Wiszniewski W, Gawlinski P, Gambin T, et al. Comprehensive genomic analysis of patients with disorders of cerebral cortical development. Eur J Hum Genet. 2018;26(8):1121–31.
Landrum MJ, Lee JM, Benson M, et al. ClinVar: improving access to variant interpretations and supporting evidence. Nucleic Acids Res. 2018;46(D1):D1062–7.
Firth HV, Richards SM, Bevan AP, et al. DECIPHER: database of chromosomal imbalance and phenotype in humans using ensembl resources. Am J Hum Genet. 2009;84(4):524–33.
Lerer I, Sagi M, Meiner V, Cohen T, Zlotogora J, Abeliovich D. Deletion of the ANKRD15 gene at 9p24.3 causes parent-of-origin-dependent inheritance of familial cerebral palsy. Hum Mol Genet. 2005;14(24):3911–20.
Vanzo RJ, Twede H, Ho KS, et al. Clinical significance of copy number variants involving KANK1 in patients with neurodevelopmental disorders. Eur J Med Genet. 2019;62(1):15–20.
DECIPHER CNV syndrome list. <http://decipher.sanger.ac.uk>.
Phelan K, Rogers RC, Boccuto L. Phelan-McDermid syndrome. GeneReviews® Web site. http://www.ncbi.nlm.nih.gov/books/NBK1198/. Updated 2018. Accessed Dec 30, 2020.
Segel R, Ben-Pazi H, Zeligson S, et al. Copy number variations in cryptogenic cerebral palsy. Neurology. 2015;84(16):1660–8.
Grayton HM, Fernandes C, Rujescu D, Collier DA. Copy number variations in neurodevelopmental disorders. Prog Neurobiol. 2012;99(1):81–91.
Wilfert AB, Sulovari A, Turner TN, Coe BP, Eichler EE. Recurrent de novo mutations in neurodevelopmental disorders: properties and clinical implications. Genome Med. 2017:9.
Richards S, Aziz N, Bale S, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the american college of medical genetics and genomics and the association for molecular pathology. Genet Med. 2015;17(5):405–24.
OMIM: Online Mendelian Inheritance In Man. <https://www.omim.org/>.
Jin SC, Lewis SA, Bakhtiari S, et al. Mutations disrupting neuritogenesis genes confer risk for cerebral palsy. Nat Genet. 2020;52(10):1046–5.
Parolin Schnekenberg R, Perkins EM, Miller JW, et al. De novo point mutations in patients diagnosed with ataxic cerebral palsy. Brain. 2015;138(7):1817–32.
Takezawa Y, Kikuchi A, Haginoya K, et al. Genomic analysis identifies masqueraders of full-term cerebral palsy. Ann Clin Transl Neurol. 2018;5(5):538–51.
Matthews AM, Blydt-Hansen I, Al-Jabri B, et al. Atypical cerebral palsy: genomics analysis enables precision medicine. Genet Med. 2019;21(7):1621–8.
Rosello M, Caro-Llopis A, Orellana C, et al. Hidden etiology of cerebral palsy: genetic and clinical heterogeneity and efficient diagnosis by next-generation sequencing. Pediatr Res. 2020; https://doi.org/10.1038/s41390-020-01250-3.
Deans C, Maggert KA. What do you mean, “Epigenetic”? Genetics (Austin). 2015;199(4):887–96.
Romanowska J, Joshi A. From genotype to phenotype: through chromatin. Genes. 2019;10(2):76.
Radford EJ. An introduction to epigenetic mechanisms. In: Progress in molecular biology and translational science, vol. 158. Elsevier B.V; 2018. p. 29–48.
Crowgey E, Marsh A, Robinson K, Yeager S, Akins R. Epigenetic machine learning: utilizing DNA methylation patterns to predict spastic cerebral palsy. BMC Bioinform. 2018;19:225.
Bahado-Singh RO, Vishweswaraiah S, Aydas B, Mishra NK, Guda C, Radhakrishna U. Deep learning/artificial intelligence and blood-based DNA epigenomic prediction of cerebral palsy. Int J Mol Sci. 2019;20(9):2075.
Mohandas N, Bass-Stringer S, Maksimovic J, et al. Epigenome-wide analysis in newborn blood spots from monozygotic twins discordant for cerebral palsy reveals consistent regional differences in DNA methylation. Clin Epigenetics. 2018;10(1):25.
Jiao Z, Jiang Z, Wang J, et al. Whole-genome scale identification of methylation markers specific for cerebral palsy in monozygotic discordant twins. Mol Med Rep. 2017;16(6):9423–30.
McMichael G, Girirajan S, Moreno-De-Luca A, et al. Rare copy number variation in cerebral palsy. Eur J Hum Genet. 2014;22(1):40–5.
Oskoui M, Gazzellone MJ, Thiruvahindrapuram B, et al. Clinically relevant copy number variations detected in cerebral palsy. Nat Commun. 2015;6(1):7949.
van Eyk CL, Corbett MA, Maclennan AH. The emerging genetic landscape of cerebral palsy. In: Handbook of clinical neurology, vol. 147. Elsevier B.V; 2018. p. 331–42.
Makela NL, Birch PH, Friedman JM, Marra CA. Parental perceived value of a diagnosis for intellectual disability (ID): a qualitative comparison of families with and without a diagnosis for their child’s ID. Am J Med Genet A. 2009;149A(11):2393–402.
Berrios C, Koertje C, Noel-MacDonnell J, Soden S, Lantos J. Parents of newborns in the NICU enrolled in genome sequencing research: hopeful, but not naïve. Genet Med. 2020;22(2):416–22.
Leach EL, Shevell M, Bowden K, Stockler-Ipsiroglu S, van Karnebeek CDM. Treatable inborn errors of metabolism presenting as cerebral palsy mimics: systematic literature review. Orphanet J Rare Dis. 2014;9:197. Accessed Jan 6, 2021
Cheng X, Li T, Wang H, et al. Methylenetetrahydrofolate reductase gene polymorphisms and cerebral palsy in chinese infants. J Hum Genet. 2011;56(1):17–21.
Lin S, Li T, Zhu D, et al. The association between GAD1 gene polymorphisms and cerebral palsy in chinese infants. Tsitol Genet. 2013;47(5):22–7.
O’Callaghan ME, MacLennan AH, Gibson CS, et al. Genetic and clinical contributions to cerebral palsy: a multi-variable analysis. J Paediatr Child Health. 2013;49(7):575–81.
Khankhanian P, Baranzini SE, Johnson BA, et al. Sequencing of the IL6 gene in a case-control study of cerebral palsy in children. BMC Med Genet. 2013;14(1)
Bi D, Chen M, Zhang X, et al. The association between sex-related interleukin-6 gene polymorphisms and the risk for cerebral palsy. J Neuroinflammation. 2014;11(1):100.
He X, Peng Q, Chen Y, et al. Candidate single-nucleotide polymorphisms and cerebral palsy: a case-control study. Biomedical Reports. 2015;3(6):849–52.
Clark EAS, Weiner SJ, Rouse DJ, et al. Genetic variation, magnesium sulfate exposure, and adverse neurodevelopmental outcomes following preterm birth. J Perinatol. 2018;35:1012–22.
Yu T, Xia L, Bi D, et al. Association of NOS1 gene polymorphisms with cerebral palsy in a Han Chinese population: a case-control study. BMC Med Genomics. 2018;11(1):56.
Zarrei M, Fehlings DL, Mawjee K, et al. De novo and rare inherited copy-number variations in the hemiplegic form of cerebral palsy. Genet Med. 2018;20(2):172–80.
Zhu Q, Ni Y, Wang J, et al. Identification of pathways and genes associated with cerebral palsy. Genes Genomics. 2018;40(12):1339–49.
van Eyk CL, Corbett MA, Frank MSB, et al. Targeted resequencing identifies genes with recurrent variation in cerebral palsy. NPJ Genomic Med. 2019;4(1):1–11.
McMichael G, Bainbridge MN, Haan E, et al. Whole-exome sequencing points to considerable genetic heterogeneity of cerebral palsy. Mol Psychiatry. 2015;20(2):176–82.
Acknowledgements
We gratefully acknowledge Peter van Essen, MSc (Radboudumc, The Netherlands) for the literature search and data extraction. This study makes use of data generated by the DECIPHER community. A full list of centres which contributed to the generation of the data is available from https://decipher.sanger.ac.uk/about/stats and via email from decipher@sanger.ac.uk. Funding for the DECIPHER project was provided by Wellcome. Those who carried out the original analyses and data collection bear no responsibility for the further analysis or interpretation of the data.
Multiple Choice Questions
-
1.
The mode of inheritance in the majority of cerebral palsy patients is:
-
(a)
X-linked dominant (de novo)
-
(b)
Autosomal recessive
-
(c)
Autosomal dominant (de novo)
-
(d)
None of the above
-
(a)
-
2.
Establishing a diagnosis in cerebral palsy has implications for
-
(a)
Supportive care
-
(b)
Prognosis and counselling
-
(c)
Prevention and treatment
-
(d)
All of the above
-
(a)
-
3.
In patients with cerebral palsy, genetic aberrations occur with the following frequencies
-
(a)
disease-causing copy number variants: 4%, and single nucleotide variants or indels: 14%
-
(b)
disease-causing copy number variants: 4% and epigenetic signatures: 21%
-
(c)
single nucleotide variants or indels: 14% and epigenetic signatures: 21%
-
(d)
structural and numeric chromosomal abnormalities: 13% and single nucleotide variants or indels: 14%
-
(a)
-
4.
The yield of genetic/genomic testing increases if the following features are present:
-
(a)
positive family history for cerebral palsy, periventricular leukomalacia on neuro-imaging, progressive disease course
-
(b)
progressive disease course, multi-organ involvement, affected siblings
-
(c)
unexplained death in the family, progressive disease course, normal neuro-imaging
-
(d)
abnormalities on prenatal sonogram, normal newborn screening, behavioural problems
-
(a)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Friedman, J., van Karnebeek, C. (2023). Genetics and Genomics of Cerebral Palsy. In: Eisenstat, D.D., Goldowitz, D., Oberlander, T.F., Yager, J.Y. (eds) Neurodevelopmental Pediatrics. Springer, Cham. https://doi.org/10.1007/978-3-031-20792-1_35
Download citation
DOI: https://doi.org/10.1007/978-3-031-20792-1_35
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-20791-4
Online ISBN: 978-3-031-20792-1
eBook Packages: MedicineMedicine (R0)