Abstract
Prenatal exposure to alcohol can lead to harmful developmental outcomes and is the leading known cause of developmental disability in the western world. Fetal Alcohol Spectrum Disorder (FASD) describes the constellation of adverse effects that can result from maternal consumption of alcohol during pregnancy. The cognitive and behavioural symptoms associated with FASD are both debilitating and life-long. The extent and severity of these deficits require a high level of the coordinated management plan that involves service delivery and resource allocations that can be extremely costly to caregivers and the health care system. A timely diagnosis of FASD is the most important factor in the prevention of secondary disabilities, despite the inherent challenges of obtaining one. Unique approaches are needed to mitigate the impact of FASD and prenatal alcohol exposure, thus improving diagnosis, intervention and treatment for affected individuals.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara Learning Objectives-
To identify the range of effects from prenatal alcohol exposure
-
To understand the criteria required for an FASD diagnosis
-
To explore challenged with FASD diagnosis
-
The diagnosis of FASD is complex and requires a highly trained, multidisciplinary team including physicians, psychologists and other allied health care professionals.
-
An FASD diagnosis is based on a combination of factors including central nervous system problems (structural, neurological, and/or functional), facial dysmorphology (smooth philtrum, thin upper lip, and short palpebral fissure) and confirmed prenatal alcohol exposure.
-
There is no safe threshold for alcohol consumption during pregnancy.
-
All pregnant women and women of child-bearing age should be asked periodically about alcohol, tobacco, prescription drug use, and illicit drug use, and those at- risk for problematic substance use should be offered brief interventions and referral to community resources.
-
A disproportionate number of individuals with FASD have mental health comorbidities, such as depression; mood and anxiety disorders; attention deficit /hyperactivity disorder (ADHD); and conduct disorder.
Introduction
Prenatal exposure to alcohol can lead to harmful developmental outcomes and is the leading known cause of developmental disability in the western world. Fetal Alcohol Spectrum Disorder (FASD) describes the constellation of adverse effects that can result from maternal consumption of alcohol during pregnancy. The cognitive and behavioural symptoms associated with FASD are both debilitating and life-long [1]. The extent and severity of these deficits require a high level of coordinated service delivery that is extremely costly to the health care system. FASD is not unique to developed countries and is a growing global health concern worldwide.
The diagnosis of FASD is complex and requires a highly trained, multidisciplinary team including physicians, psychologists and other allied health care professionals. This level of expertise is essential to the accurate diagnosis of FASD-related disabilities and for identifying functions and deficits—especially neurodevelopmental—and for recommending interventions that will not only improve outcomes for affected individuals and their families but also provide access to services.
Diagnosis is based on a combination of factors including central nervous system problems (structural, neurological, and/or functional), facial dysmorphia (smooth philtrum, thin upper lip, and short distance between the inner and outer corners of the eyes) and confirmed prenatal alcohol exposure. The confirmed absence of alcohol during pregnancy rules out a diagnosis of FASD. Diagnostic practices vary depending on the diagnostic schema used; clinical categorization is not standardized [2, 3].
FASD can be diagnosed at birth, but often goes undiagnosed until later in life when behavioural and cognitive effects become more evident [4]. Early diagnosis (e.g., before age 6 years) and intervention are considered critical to improve development and to reduce the likelihood of secondary disabilities [5, 6].
Diagnosis can be extremely complicated and, in an attempt to guide diagnostic teams, a number of approaches have been identified around the world. Fetal Alcohol Spectrum Disorder: Canadian Guidelines for Diagnosis [7] were published by a panel of Canadian experts in 2005 in an attempt to provide simple, but thorough, evidence-based guidelines for diagnoses related to prenatal exposure to alcohol. These Canadian guidelines were updated in 2016 [1]. Additional diagnostic guidelines include those from the Institute of Medicine [8], the FASD 4-Digit Diagnostic Code [9], the Centers for Disease Control and Prevention FAS guidelines [10], the updated Hoyme FASD guidelines [11] and the Mortality and Morbidity Weekly Report Guidelines [12]. Several countries have used these different schemas to inform the developmental of their own diagnostic guidelines, for example, Argentina [13], Netherlands [14] Germany [15], Australia [16], and Scotland [17].
There is consensus among the diagnostic schemas that the facial features associated with prenatal alcohol exposure are unique to FASD; however, they differ in the number of features that must be present to obtain a diagnosis. It is the central nervous system dysfunction that has the most diverse range of potential deficits and variability, which leads to differences in the final diagnosis. A critical implication of this predicament is the inability to combine data from sources that use different diagnostic schemas preventing the creation of large datasets that can be used for research, to calculate prevalence and inform nomenclature.
Coles et al. [18] compared the most common diagnostic schema for FASD and suggested problems in convergent validity among systems, as demonstrated by a lack of reliability in diagnosis, but concluded that the absence of an external standard makes it impossible to determine whether any system is more accurate. Table 24.1 illustrates the differences between systems.
Currently, diagnosis of FASD continues to be problematic depending on a variety of reasons including lack of diagnostic capacity, lack of antenatal history and lack of support. These reasons further highlight the need to create comprehensive diagnostic guidelines that can be implemented easily, with as much objectivity as possible. Clearly, diagnosis has significant implications for incidence, prevalence and surveillance, economic and cost calculations, and supply and demand of services across many sectors. For the purposes of this textbook, the 2016 Canadian Guidelines will be used [1], recognizing that, while using different systems may result in different specific diagnoses, the process of physical and neurodevelopmental assessment is largely the same.
In 2005, Fetal Alcohol Spectrum Disorder (FASD): Canadian Guidelines for Diagnosis [7] was published as a supplement to the Canadian Medical Association Journal. The guidelines were created following widespread consultation with expert practitioners and partners in the field and were the first attempt to provide user-friendly, evidence-based guidelines for diagnostic services related to Fetal Alcohol Spectrum Disorder (FASD) in the Canadian context. Eventually, more experience revealed gaps and inconsistencies in areas that needed improvement and/or clarity (i.e. diagnostic recommendations specific for very young children and adults); and, following widespread consultation with experts from around the world, the Canadian guidelines were updated in 2016 [1].
Epidemiology and Cost of FASD
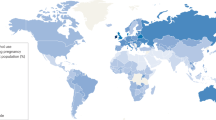
The specific prevalence of FASD is the subject of a number of investigations around the world. Lange et al estimate that the global prevalence of FASD is 7.7 per 1000 population, with some countries being as high as 111 per 1000 [19]. These statistics continue to be difficult to obtain, due to the absence of a centralized database in which diagnostic data could be entered and tracked.
The rate of FASD in the United States has been estimated at 15 per 1000 live births [20]. Prevalence data for FASD in Canada were reported at 5 per 1000 live births [20], with rates up to 16 times higher among some populations. Of the statistics that are available, it is likely that they are an under-estimate of the actual prevalence in most countries around the world, due in part to delayed diagnosis, misdiagnosis or no diagnosis at all. For example, underestimates of the prevalence of FASD have been reported in communities in Italy [21] and in Western Australia due to limitations in the birth defect registry (birth defects are only recorded for children between 0–1 year of age) [22] Without accurate prevalence data, it is difficult to determine total cost (direct and indirect) associated with FASD. Greenmyer et al. [23] suggest that the mean annual cost for children with FASD is estimated at $22,810 and for adults $24,308, but conclude that the data on the economic burden of FASD are scarce, and the existing estimates likely underestimate the full economic impact on affected individuals, their caregivers, and society.
The economic burden of FASD in Canada, specifically, was reported to total approximately $1.8 billion (from about $1.3 billion as the lower estimate up to $2.3 billion as the upper estimate) in 2013 [24]. The highest contributors to the economic burden were costs associated with productivity losses (due to morbidity and premature mortality), the cost of corrections, and the cost of health care.
Importance of Early Diagnosis
Although a substantial amount of research has been devoted to furthering the understanding of prenatal alcohol pathophysiology, prevention continues to be an ongoing challenge. FASD is among the leading, preventable causes of developmental disability and a major public health concern. The early recognition of at-risk children is critical for initiating the appropriate intervention and treatment strategies. Qualitative data reveals that the “lived” experiences of parenting a child with FASD include a range of concerns, such as societal, educational, health and judicial [25]; all of which can be significantly impacted by the time a diagnosis is made. Women expressed great difficulty in obtaining a diagnosis for their child from a medical professional and frustration with the process, as they felt that they were constantly dealing with barriers and challenges with the system [25].
Infants who were non-dysmorphic at birth were later found to be at the greatest risk for significant behavioural problems as children and adolescents [26]. Without the distinct facial presentation, FASD diagnosis at birth continues to remain elusive; though no less important [27]. The need for a concerted and coordinated effort, to provide the appropriate education to practicing physicians about the phenotypes of FASD, must be made to ensure accurate and timely diagnoses; only then can the most appropriate management plans be put in place [28, 29].
Background and Terminology for the Diagnosis of Fetal Alcohol Spectrum Disorder
In 1968, Lemoine published a seminal paper that first identified the relationship between prenatal alcohol exposure and birth defects [30]. Although his initial observations did not attain international resonance, a few years later several physicians published the first case studies in North America describing the physical findings of babies born to chronic alcoholic mothers [31, 32] and coined the term “Fetal Alcohol Syndrome” (FAS). In 1978, four post-mortem anatomical assessments were conducted and profound neurological malformations stemming from errors in the migration of neuronal and glial elements [33]. Slowly the medical community began to accept that alcohol was a teratogen. Since the first description of FAS, a number of different terminologies have been introduced and revised. Still, FAS continues to be a diagnostic term that is used today and can be recognized on both a national and international scale. Interested readers are referred to Calhoun and Warren’s review for a historical account of the evolution of FAS as a medical diagnosis [34].
Terminology Associated with Diagnosis
Because terminology is tightly associated with diagnostic criteria, several different approaches have been developed along with their own specific nomenclature to describe the different manifestations of prenatal alcohol exposure (Tables 24.1 and 24.2). A number of diagnostic guidelines for FASD have been published; most notably those by the Institute of Medicine (IOM) FASD [8], the FASD 4-Digit Diagnostic Code [9], the Centers for Disease Control and Prevention (CDC) FAS guidelines [10], the Canadian FASD guidelines [1], the Hoyme FASD guidelines [11] and the Mortality and Morbidity Weekly Report Guidelines [12]—all of which share similar diagnostic approaches and in the case of the 4-digit diagnostic code include a number of additions. To date, several comparisons have been made in the literature [18, 35] (Astley et al., 2006; Coles et al., 2016) and the 2005 Canadian guidelines published a harmonization of the 4-digit diagnostic code and IOM [7]. Regardless of the differences in terminology, an important evolution of all diagnostic approaches is the move towards providing services based on an individual’s needs, and not on what caused their diagnosis. Specifically, it is recommended that services should be available for individuals across the full continuum of FASD—for this reason, the 2016 Canadian Guidelines added the “At-Risk” designation in recognition of this need [1]. Regardless, it is critical to remember, while the diagnostic features associated with FASD represent a spectrum of effects, the specific diagnostic terms are not indicative of a continuum of severity of the neurodevelopmental deficits.
The term FASD was originally coined as an umbrella term to encompass the diagnoses and the breadth of disabilities associated with prenatal alcohol exposure. Commonly used terminologies include: Fetal Alcohol Syndrome (FAS), Fetal Alcohol Effects (FAE), Partial Fetal Alcohol Syndrome (pFAS), Alcohol-Related Neurodevelopmental Disorder (ARND), Alcohol-Related Birth Defects (ARBD), the 4-Digit Diagnostic Code nomenclature: Neurodevelopmental Disorder, associated with Prenatal Alcohol Exposure (ND-PAE), Neurobehavioral Disorder—Alcohol Exposed (NB-AE), and Static Encephalopathy—Alcohol Exposed (SE-AE). The terminology can be confusing and the categories overlap in some instances (Table 24.1).
The Canadian Guideline attempted to simplify diagnosis into FASD with or without sentinel facial features and the “at risk” designation [1], and suggests the following, based on experience and expert opinion:
FASD should now be used as a diagnostic term when prenatal alcohol exposure is considered to be a significant contributor to observed deficits that cannot be explained by other etiologies. Because the observed deficits are recognized as being multifactorial in origin, all other known relevant contributors (e.g., trauma, known genetic anomalies) should be documented with the FASD diagnosis as they have significant impact on the functional and neurological challenges of the affected individuals [1].
Diagnosis
A summary of the criteria for diagnosis based on the Canadian Guidelines is shown in Table 24.3 and the pathway for achieving each diagnosis (or for a non-FASD diagnosis) is shown in Fig. 24.1.
Algorithm from Canadian Guideline [With permission from the CMAJ, Reference 1]
The Diagnostic Process
Confirmation of Prenatal Alcohol Exposure
Confirmation of prenatal alcohol exposure (PAE) requires documentation that the biological mother consumed alcohol during the index pregnancy based on: reliable clinical observation; self-report; reports by a reliable source; medical records documenting positive blood alcohol concentrations; alcohol treatment or other social, legal or medical problems related to drinking during the pregnancy [1].
Prenatal Alcohol Exposure and the Developing Fetus
In the absence of facial dysmorphology, confirmed prenatal alcohol exposure is needed to identify FASD. However, in many cases, the antenatal records are unavailable making it impossible to determine the precise dosimetry data for the timing and dose of alcohol in pregnancy. That said, several features of alcohol metabolism are well characterized, have significant implications for the developing fetus, and are important to inform the diagnosis. The typical blood alcohol concentration for prenatal alcohol exposure is assessed using body weight and frequency of drinking [36]. Persistent alcohol use increases tolerance, which can result in very high blood alcohol concentrations for some individuals, without them feeling the effects of alcohol. This can make it difficult to identify the problem of drinking. Another key factor is the effect of drinking on consecutive days, when the second exposure episode begins before the blood alcohol concentration from the previous drinking episode has reached zero. In these situations, a higher blood alcohol concentration for the second episode will result leading to an extended period of exposure for the fetus. Despite many years of investigation, a safe threshold for alcohol consumption during pregnancy has not been identified [37].
Confirming Maternal Alcohol Exposure
The first step of the diagnostic process is confirming prenatal alcohol exposure. Thus, one of the most difficult issues related to FASD diagnosis is the lack of accurate antenatal records with documented prenatal alcohol exposure. Compounding the problem is the fact the majority of the individuals with FASD do not have the three identifying facial features [38, 39]. In these cases, a diagnosis is even more challenging when the brain injury is mild and the majority of the behavioural and intellectual deficits do not present until the child is school-age. Due to denial, embarrassment, and litigious fears, maternal reports of gestational drinking are often inaccurate or not available [40].
Based on the literature and clinical experience, it is evident that substantial differences exist in the screening and referral processes used for alcohol, including during pregnancy. The Society of Obstetricians and Gynaecologists of Canada recommends that all pregnant women and women of child-bearing age should be asked periodically about alcohol, tobacco, prescription drug use, and illicit drug use, and that pregnant women at-risk for problematic substance use should be offered brief interventions and referral to community resources for further psychosocial support [41]. The American College of Obstetricians and Gynecologists have similar recommendations [42]. In a review of the prenatal record forms in Canada, most lacked the appropriate prompts to encourage providers to intervene or refer pregnant patients with high-risk drinking behaviours to seek appropriate treatment [43]. Additionally, it was speculated that the level of ‘at-risk’ drinking during pregnancy was underestimated across Canada, as less than half of the prenatal record forms included the use of validated screening tools (i.e., T-ACE, TWEAK). Of the records that included prenatal screening tools, questions related to the amount(s) and type(s) of alcoholic drinks consumed, the pattern of drinking and the frequency were not included. Failure to identify at-risk alcohol consumption during pregnancy, or to appropriately intervene, may increase the likelihood of an alcohol-exposed fetus. Currently, the evidence-based recommendations related to the prevention and diagnosis of FASD have not been consistently integrated into prenatal record forms.
Health care providers are often uncomfortable discussing sensitive topics such as alcohol consumption with their pregnant patients and do not possess a good understanding of the effects of alcohol on the developing fetus or are unaware of the appropriate interventions once alcohol use has been confirmed [44]. Documentation and maternal history of substance use are both important components for identifying an individual with prenatal alcohol exposure, which is critical for a diagnosis in situations where there are no physical features.
For patients, who were adopted or in foster care, obtaining confirmation of prenatal alcohol exposure can be another challenge for diagnosis [45, 46]. Without a record of antenatal history, FASD diagnoses are near impossible. Documented antenatal records are difficult to obtain for many children in care; a problem that is compounded when the adoption is International [45, 47]. Risk factors such as “a history of alcoholism”, “multiparous” and “age” (i.e., older at the time of an affected pregnancy) can all be used when considering an FASD diagnosis. It is imperative that nurses, physicians, and other health care providers become comfortable with obtaining a history of prenatal alcohol use and training to provide the appropriate follow-up care and guidance.
Biomarkers
Biomarkers have been under investigation to assist with obtaining confirmation of prenatal alcohol exposure. The most common clinical tool is maternal self-reporting. However, a more objective approach is the use of biomarkers from biological specimens alone or in combination with maternal self-reporting [48]. It has been reported that the biomarkers fatty acid ethyl esters, ethyl glucuronide, ethyl sulfate, and phosphatidyl ethanol may be promising indicators for the detection of prenatal alcohol exposure [48]. Other potential biomarkers include ultrasound measurements of the fetal corpus callosum [49] and deficits involving the visual system [50,51,52,53,54].
The discussion and development of potential biomarkers for prenatal alcohol exposure are not without significant ethical implications. Biomarkers for FASD pose several unique challenges due to the nature of the information obtained and the implications. Positive screens include a greater element of social risk for parents, particularly mothers (i.e., public exposure of their substance use, the potential for child welfare involvement, apprehensions, and legal consequences). Moreover, there are many risks related to introducing a technology before the ethical ramifications have been thoroughly considered, especially the role and rights of the parent, physician and state [55]. The key ethical issues have been summarized as follows: targeting populations for prenatal alcohol exposure screening; consent and respect for persons; stigma and participation rates; the cost-benefit of a screening program; the sensitivity, specificity and associated outcomes of a screen; confidentiality and appropriate follow-up to positive screen results; and the use of screen results for criminal prosecution [56]. Interestingly, it is the stakeholder perspectives (e.g., parents, health care providers) that have been absent in most of the reviews of the ethical issues surrounding a prenatal alcohol exposure screen. These perspectives are needed to provide appropriate insight into the potential impact and implications of biomarkers.
The Physical Examination and Differential Diagnosis
The diagnostic process should include a comprehensive social and medical history, and a complete physical examination [1]. The dysmorphology assessment is used to differentiate the specific physical features associated with prenatal alcohol exposure from those that arise due to other causes. Specific facial abnormalities have been described for the FASD population [31].
Facial Features
The revised Canadian diagnostic guidelines recommend the following criteria:
-
Simultaneous presentation of 3 sentinel facial features (short palpebral fissures, smooth philtrum and thin upper lip)
-
In all cases, any signs of other congenital anomalies should be recorded, including microcephaly.
The classic triad of facial features associated with FASD includes short palpebral fissures, smooth or flattened philtrum and a thin vermilion border of the upper lip [1]. However, the presence of fewer than 3 facial features in individuals with FASD is more common, with 39% of individuals in a large Canadian database having no sentinel features, 24% having one, 15% with two and 14% with all three [39]. The presence of facial features continues to play an important role in the assessment for FASD, where prenatal also exposure cannot be confirmed, although differences in facial variation in human subjects and the reliability of alcohol intake information pose significant challenges for establishing dose-response relationships. Animal models; however, enable the study of facial alterations related to specific timing and dose of alcohol. In the mouse model of FASD, facial morphometric analysis in parallel to anthropometry was used to successfully identify pups exposed to prenatal ethanol following a specific dose and time of alcohol exposure [59]; illustrating the utility of experimental mouse models to better define risk factors (e.g., dose, timing, frequency) that contribute to the facial phenotype in FASD. The implications for the clinical situation are unknown, but in future, it may be possible to determine alcohol dosimetry from the severity of a given facial feature.
Advancements have also been made to the tools that are used to collect information about facial dysmorphology. Using a unique set of facial regions and features, 2 and 3D facial scanned images were used to develop an automated technique that could accurately discriminate subjects with FAS from controls, without human intervention [6, 60]. As well, a stereo-photogrammetric tool for the diagnosis of FAS in infants has proven highly precise and reliable [61], which is promising given that, with early intervention, the prognosis of FASD improves substantially and development of secondary disabilities decreases [62].
There are a number of studies exploring possibilities for using technology to help in the diagnosis of FASD, especially related to facial features. For example, heat maps and morphing visualizations of face signatures are being explored and may help clinicians detect facial dysmorphism across the fetal alcohol spectrum in the future. Face signature graphs show potential for identifying non-syndromal, heavily-exposed children, who lack the classic facial phenotype, but have cognitive impairments [2].
Craniofacial development is intimately linked to the development of the brain; though, the relationship between facial directional asymmetry (associated with prenatal alcohol exposure) and structural asymmetry of the brain remains to be determined. It is likely that a range of developmental processes, and their disruption, can lead to associations between the structure and function of the brain, and facial shape and symmetry. This continues to be investigated.
Foroud et al related anthropometric and cognitive measurements in children at 5 and 8 years of age with and without FASD to determine if the face predicts brain (dys)function [63]. Several anatomical features were predictive of group membership (FASD or control), such asmeasures of craniofacial width (minimal frontal), orbital width (palpebral fissure width), and ear and mandibular measures (ear length and lower facial depth). Additionally, facial width, length, and depth measurement were highly sensitive and specific for differentiating children with FASD from controls. Sensitivity and specificity were also high for discriminating children FASD from the heavily-exposed children, who did not meet criteria for FASD. These results provide further insight into the complex relationship between the face and the neuropsychological deficits that occur following prenatal exposure to alcohol and may, in the future, inform new diagnostic tools.
The Neurobehavioural Assessment
Diagnostic Criteria from the Canadian Guidelines
-
Evidence of impairment in 3 or more of the following central nervous system (CNS) domains:
-
Motor Skills
-
Neuroanatomy /Neurophysiology
-
Cognition
-
Language
-
Academic Achievement
-
Memory
-
Attention
-
Executive Function, including Impulse Control
-
Affect Regulation
-
Adaptive Behaviour, Social Skills or Social Communication
-
A severe impairment is defined as a global score or a major subdomain score on a standardized neurodevelopmental measure that is ≥2 standard deviations below the mean, with appropriate allowance for test error. In some domains, large discrepancies among subdomain scores may be considered when a difference of this size occurs with a very low base rate in the population (≤3% of the population). Clinical assessment with converging evidence from multiple sources and DSM-5 diagnostic criteria for certain disorders may also be considered in specific domains which are not easily assessed by standardized tests (for example, in the affect regulation domain the following diagnoses may be taken as an indication of severe impairment: Major Depressive Disorder (with recurrent episodes), Persistent Depressive Disorder, Disruptive Mood Dysregulation Disorder (DMDD), Separation Anxiety Disorder, Selective Mutism, Social Anxiety Disorder, Panic Disorder, Agoraphobia, or Generalized Anxiety Disorder).
The neurobehavioural deficits associated with FASD are multifaceted and vary from mild to severe depending on the situation. In particular, executive functions (those requiring higher levels of cognitive processing) and working memory are typically considered hallmark features of FASD [64,65,66]. Mental health comorbidities are prevalent among individuals with FASD, and they are also at risk for suicide and addiction [67, 68]. Importantly, both the executive function deficits and mental health issues can occur in the absence of facial dysmorphology, making the neurobehavioural assessment critical to the diagnostic process.
FASD and Mental Health
A disproportionate number of individuals with FASD have mental health comorbidities [5, 67, 69]. These problems are often present in childhood and adolescence and persist into adulthood, where mental health problems are considered the most severe characteristics of FASD [70]. The most prevalent mental health issues for individuals with FASD are depression, mood and anxiety disorders, attention-deficit/hyperactivity disorder (ADHD) and conduct disorder (CD). For a comprehensive review of FASD and mental health, please refer to Easey et al. [67] and Pei et al. [68].) Individuals with FASD are also at risk for high rates of suicide [71] and addiction [72]. A systematic review revealed that there were 15 comorbid mental health disorders associated with FASD; ADHD occurred in 50% of all FASD cases (10 times the expected rate) and intellectual disability occurred at 23 times the expected rate. In 5 of the 12 comorbidities, rates in the FASD population significantly exceeded expected rates by 10% to 45% [73].
Others have also shown that ADHD is one of the most common comorbidities in patients with FASD [68, 74, 75]. Several human studies have contrasted cognitive abilities using standardized psychometric tests to characterize the differences in performance between the two clinical populations. Interestingly, although both groups demonstrate neurodevelopmental deficits, the nature and/or mechanisms for the deficits differ, as revealed on tests of spatial working memory [76], adaptive behaviour [77, 78], verbal learning and memory [79], executive function [80] and arithmetic [81]. These data suggest a unique mechanism for the effects of prenatal alcohol exposure on specific neurodevelopmental outcomes.
In a study of children and adolescents (age 8–16 years), with and without prenatal alcohol exposure and ADHD, an elevated risk of psychiatric disorders and behavioural problems were associated with both ADHD and prenatal alcohol, compared to controls [82]. Findings revealed that an ADHD diagnosis elevated the children’s risk of psychiatric diagnoses, regardless of prenatal alcohol exposure. However, co-occurrence of ADHD and prenatal alcohol exposure exacerbated the occurrence of conduct disorders and externalizing behaviours. Furthermore, there was a poor behavioural prognosis for alcohol-exposed children with ADHD, suggesting the potential for more than one neurobehavioural profile for individuals with FASD [82]. These observations are important for mental health care providers, who should routinely consider the possible contribution of prenatal alcohol exposure in the diagnosis and management of mental illness and developmental disorders. Because of the potential neurological (functional and structural) effects resulting from prenatal alcohol exposure, unique screening and intervention approaches may be required for individuals with FASD.
Imaging as a Diagnostic Tool
Imaging and brain metabolism techniques provide unique opportunities to evaluate brain function in vivo. Several excellent reviews describe and summarize the major advancements in understanding the relationship between neural activation and the behavioural outcomes associated with FASD [83, 84]. Data reveal that there are specific differences between those with FASD and those with other disorders, including ADHD [83]. Morphological differences in the brain, and how these differences relate to cognitive deficits and facial dysmorphology, have also been described. New technologies have provided valuable insight into the relationship between white matter microstructure and behaviour, atypical neuromaturation across childhood and adolescence, and differences in neural activation patterns underlying sensory processing, cognition and behavioural deficits associated with FASD, including reductions in global network efficiency [84]. Microcephaly and disproportionate reductions in the size of the parietal lobe, cerebellar vermis, corpus callosum and caudate nucleus, have all been associated with prenatal alcohol exposure [85, 86]. Despite these advancements, there are still many unknowns about the impact of prenatal alcohol exposure on the brain, and continued research efforts are essential to understanding the complex mechanisms underlying the resultant neurodevelopmental deficits.
Treatment and Follow-Up
Clinically, a major problem for FASD diagnosticians is follow-up. Depending on where patients obtain their diagnosis will often dictate the type of follow-up services and supports they will receive. In some cases, the diagnosticians do not know where to refer their patients after a confirmed diagnosis is made, making management extremely complex. To further complicate the issue, many individuals with FASD also present with significant comorbidities that must be considered in devising appropriate treatment strategies. Comorbidities substantially increase the difficulty of management over time; underscoring the need for longitudinal assessments from infancy to adulthood [75]. A primary goal when working with the FASD population is to provide anticipatory guidance about future developmental abnormalities and to provide appropriate therapeutic interventions when they present and when feasible. A 10-year management plan has been implemented by some clinics to provide individuals with the opportunity to review their current situation and anticipate upcoming problems. The three common goals to management include (1) prevent multiple foster home placements (i.e., the uprooting and re-assimilation), which are extremely detrimental for optimal development; (2) maximize parent or caretaker understanding of the age-related changes in behaviour and age-related risks; and (3) anticipate future development of age-related impairments common in FASD [75].
Individuals with FASD can present with a wide variety of complex mental health and behavioural problems that require a multifaceted approach to treatment and management. The heterogeneity of the FASD population is further impacted by differences in additional pre- and post-natal insults and adverse events. Unfortunately, with respect to treatment, the demand far exceeds the supply, and many patients are unable to obtain the appropriate services and support due to limitations in availability and accessibility.
The complexity and persistence of FASD-associated problems require a long-term plan for management, especially as the individual matures. Eleven primary intervention categories and subcategories were identified in a retrospective analysis to identify the types and frequencies of supports, services, and referrals recommended by an interdisciplinary diagnostic team for children and youths with FASD [87]. Educational and medical needs were the most common recommendations for individuals with FASD. Comprehensive psychoeducational or neuropsychological assessments; special education programs, services, or eligibility; and advocacy to enhance or modify existing educational programs or services were the most frequent recommendations in the education category. For medical referrals, psychiatric care and/or medication management; vision and/or hearing screening; and neurological consultation or treatment were most common. Interestingly, the recommendations were relatively comparable across diagnostic sub-groups; though differences did emerge when stratified by age. Children in the birth-2 year cohort received more recommendations for family support and social service-child welfare interventions, while for children in the older group, recommendations were predominantly for mental health services and community resources.
Community home-based attachment interventions, such as Circle of Security® (COS), have been beneficial for preschool children affected by FASD [88]. Recent data from Canada’s National FASD Database report that a large breadth of supports and services are recommended to individuals and families as part of the diagnostic process [39]. Zarnegar et al. suggest that using neurodevelopmentally-informed assessment strategies to sequence interventions for young children with diverse neurodevelopmental insults is a promising intervention approach that improves outcomes [89].
Specific Populations
FASD Diagnosis in Infants
For many reasons, diagnosis of FASD at the time of birth is a major challenge; however, there is potential to provide an assessment to newborns, who are at-risk, during infancy (0–18 months). Several interesting studies have evaluated infants, who were affected by prenatal alcohol exposure, to identify the emerging neuropsychological profile and specific risk factors that may be assessed during early physical examinations. Prenatal alcohol exposure has been associated with infant temperament problems [90], difficultness [91], problems with crying, sleeping and eating [92], blunted pain responses [93], poor visual acuity [94], general developmental delays [95], and in one case report, severe gastroesophageal reflux [96]. Prenatal alcohol exposure has also been associated with smaller corpus callosum in newborn MRI scans [97]. Infant symbolic play (i.e., ability of children to use objects, actions or ideas to represent other objects, actions, or ideas as play) has also been evaluated as a potential predictor of FASD [98], though more research is required to identify additional diagnostic tests that can be effective in infants and small children.
FASD Diagnosis in Adults
Based on the available epidemiological data, it is suspected that there is a large population of adults with FASD; however, there are significant limitations in the availability of diagnostic and treatment services. For adults, the impairments predominantly involve social adaptive skills and executive functions, and there is a high degree of psychopathology. These situations represent the cases where a diagnosis has been obtained; though, it is suspected that many adults do not receive the appropriate medical diagnosis and subsequent treatment. These latter cases are enigmatic. With the development and implementation of better screening and diagnostic tools geared towards adults, a more accurate indication of the situation and the specific needs for adults with FASD will emerge. [Please see the following review for a description of the challenges associated with diagnosing FASD in adults [99]].
To date, a large proportion of the information pertaining to FASD in the adult population and the mechanisms by which prenatal alcohol exposure leads to dysfunction (neurological, behavioural and physical) have been obtained from the animal literature. For example, the long-term effects of neonatal alcohol exposure have been associated with impairments in circadian rhythm [100], impairments in sleep-wake behaviour [101] and auditory brainstem response abnormalities (i.e., the indication of hearing and neurological function) [102] in animal models of FASD. As well, prenatal exposure to alcohol may alter responsiveness to stress in the adult offspring [103]. In human studies, structural and physical abnormalities associated with prenatal alcohol exposure include cardiovascular arterial stiffness [104] and reproductive issues [105], including male infertility [106].
Several imaging studies have also revealed insight into the adult FASD brain. Using diffusion tensor imaging—which provides a visual representation of the connections in the brain—changes in white matter integrity of the corpus callosum was revealed in young adults with FASD compared to controls [107]. In future, this could serve as a potential marker for prenatal alcohol exposure. Brain metabolic alterations have also been revealed using magnetic resonance spectroscopy in adults with FASD [108, 109].
Studies describing the adult FASD phenotype reveal that the deficits associated with prenatal alcohol exposure are persistent and debilitating [see review [110]]. Social deficits persist across the lifespan and may worsen with age, independent of IQ and dysmorphology [111] and occupational difficulties that are characterized by disruption, failure and severe social problems [112].
Conclusion
In conclusion, diagnosing any individual with FASD continues to be a major clinical challenge that is compounded by a lack of resources and inconsistencies in diagnostic procedures and follow-up care. Management and treatment plans vary dramatically based on the clinic, the services available and the diagnostic approaches used. Despite this, there have been significant achievements in the efforts to move FASD to the forefront of public awareness and policy campaigns. Research is ongoing and continues to reveal novel discoveries that will help improve the technologies that are available for screening, diagnostics and treatment. This is an exciting time for FASD innovation, with the anticipated evolution of evidence-based, international guidelines and definitions. This will not only improve the understanding of FASD diagnoses but also define prevalence around the world.
References
Cook JL, Green CR, Lilley CM, Anderson SM, Baldwin ME, Chudley AE, et al. Fetal alcohol spectrum disorder: a guideline for diagnosis across the lifespan. CMAJ: Canadian Medical Association Journal. 2016;188(3):191–7. Epub 2015/12/17. https://doi.org/10.1503/cmaj.141593.
Suttie M, Foroud T, Wetherill L, Jacobson JL, Molteno CD, Meintjes EM, et al. Facial dysmorphism across the fetal alcohol spectrum. Pediatrics. 2013;131(3):e779–88. Epub 2013/02/27. https://doi.org/10.1542/peds.2012-1371.
Burd L, Klug MG, Li Q, Kerbeshian J, Martsolf JT. Diagnosis of fetal alcohol spectrum disorders: a validity study of the fetal alcohol syndrome checklist. Alcohol. 2010;44(7–8):605–14. Epub 2010/01/08. https://doi.org/10.1016/j.alcohol.2009.08.010.
Montag AC, Hull AD, Yevtushok L, Zymak-Zakutnya N, Sosyniuk Z, Dolhov V, et al. Second-Trimester Ultrasound as a Tool for Early Detection of Fetal Alcohol Spectrum Disorders. Alcoholism, clinical and experimental research. 2016;40(11):2418–25. Epub 2016/10/21. https://doi.org/10.1111/acer.13232.
Streissguth AP, Bookstein FL, Barr HM, Sampson PD, O'Malley K, Young JK. Risk factors for adverse life outcomes in fetal alcohol syndrome and fetal alcohol effects. J Dev Behav Pediatr. 2004;25(4):228–38.
Fang S, McLaughlin J, Fang J, Huang J, Autti-Ramo I, Fagerlund A, et al. Automated diagnosis of fetal alcohol syndrome using 3D facial image analysis. Orthod Craniofac Res. 2008;11(3):162–71.
Chudley AE, Conry J, Cook JL, Loock C, Rosales T, LeBlanc N. Fetal alcohol spectrum disorder: Canadian guidelines for diagnosis. CMAJ. 2005;172(5 Suppl):S1–S21.
Stratton K, Howe C, Battaglia. Fetal alcohol syndrome: diagnosis, epidemiology, Prevention, and treatment. In: Institute of Medicine (IOM). National Academy Press; 1996.
Astley SJ, Clarren SK. Diagnosing the full spectrum of fetal alcohol-exposed individuals: introducing the 4-digit diagnostic code. Alcohol Alcohol. 2000;35(4):400–10.
Centers for Disease C, Prevention. Fetal alcohol spectrum disorders: guidelines for referral and diagnosis. Ctr Dis Control Prev. 2004;
Hoyme HE, Kalberg WO, Elliott AJ, Blankenship J, Buckley D, Marais AS, et al. Updated clinical guidelines for diagnosing fetal alcohol spectrum disorders. Pediatrics. 2016;(138, 2) Epub 2016/07/29 https://doi.org/10.1542/peds.2015-4256.
Bertrand J, Floyd LL, Weber MK, Fetal Alcohol Syndrome Prevention Team DoBD, Developmental Disabilities NCoBD, Developmental Disabilities CfDC, et al. Guidelines for identifying and referring persons with fetal alcohol syndrome. MMWR recommendations and reports: morbidity and mortality weekly report recommendations and reports. Centers for Disease Control. 2005;54(RR-11):1–14.
Evrard SG. Diagnostic criteria for fetal alcohol syndrome and fetal alcohol spectrum disorders. Arch Argent Pediatr. 2010;108(1):61–7. Epub 2010/03/06. https://doi.org/10.1590/S0325-00752010000100011.
van Wieringen H, Letteboer TG, Pereira RR, de Ruiter S, Balemans WA, Lindhout D. Diagnosis of fetal alcohol spectrum disorders. Ned Tijdschr Geneeskd. 2010;154:A331.
Landgraf MN, Nothacker M, Heinen F. Diagnosis of fetal alcohol syndrome (FAS): German guideline version 2013. Eur J Paediatr Neurol. 2013;17(5):437–46. https://doi.org/10.1016/j.ejpn.2013.03.008.
Watkins RE, Elliott EJ, Mutch RC, Payne JM, Jones HM, Latimer J, et al. Consensus diagnostic criteria for fetal alcohol spectrum disorders in Australia: a modified Delphi study. BMJ Open. 2012;2(5):e001918. https://doi.org/10.1136/bmjopen-2012-001918.
Wise J. Guidance on fetal alcohol syndrome aims to improve diagnosis and treatment in Scotland. BMJ. 2019;364:l396. Epub 2019/01/27. https://doi.org/10.1136/bmj.l396.
Coles CD, Gailey AR, Mulle JG, Kable JA, Lynch ME, Jones KL. A comparison among 5 methods for the clinical diagnosis of fetal alcohol spectrum disorders. Alcohol Clin Exp Res. 2016;40(5):1000–9.
Lange S, Probst C, Gmel G, Rehm J, Burd L, Popova S. Global prevalence of fetal alcohol spectrum disorder among children and youth: a systematic review and meta-analysis. JAMA Pediatr. 2017;171(10):948–56. Epub 2017/08/23. https://doi.org/10.1001/jamapediatrics.2017.1919.
Popova S, Lange S, Probst C, Parunashvili N, Rehm J. Prevalence of alcohol consumption during pregnancy and fetal alcohol Spectrum disorders among the general and aboriginal populations in Canada and the United States. Eur J Med Genet. 2017;60(1):32–48. Epub 2016/09/18. https://doi.org/10.1016/j.ejmg.2016.09.010.
May PA, Fiorentino D, Coriale G, Kalberg WO, Hoyme HE, Aragon AS, et al. Prevalence of children with severe fetal alcohol spectrum disorders in communities near Rome, Italy: new estimated rates are higher than previous estimates. Int J Environ Res Public Health. 2011;8(6):2331–51. Epub 2011/07/22. https://doi.org/10.3390/ijerph8062331.
Bower C, Rudy E, Callaghan A, Quick J, Nassar N. Age at diagnosis of birth defects. Birth Defects Res A Clin Mol Teratol. 2010;88(4):251–5. Epub 2010/03/10. https://doi.org/10.1002/bdra.20658.
Greenmyer JR, Klug MG, Kambeitz C, Popova S, Burd L. A multicountry updated assessment of the economic impact of fetal alcohol Spectrum disorder: costs for children and adults. J Addict Med. 2018;12(6):466–73. Epub 2018/11/02. https://doi.org/10.1097/ADM.0000000000000438.
Popova S, Lange S, Burd L, Rehm J. The economic Burden of fetal alcohol Spectrum disorder in Canada in 2013. Alcohol Alcohol. 2016;51(3):367–75. Epub 2015/10/24. https://doi.org/10.1093/alcalc/agv117.
Salmon J. Fetal alcohol spectrum disorder: New Zealand birth mothers’ experiences. J Can Pharmacol Clin. 2008;15(2):e191–213. Epub 2008/06/03
Fagerlund A, Autti-Ramo I, Hoyme HE, Mattson SN, Korkman M. Risk factors for behavioural problems in foetal alcohol spectrum disorders. Acta Paediatr. 2011;100(11):1481–8. Epub 2011/05/18. https://doi.org/10.1111/j.1651-2227.2011.02354.x.
Janczewska I, Wierzba J, Cichon-Kotek M, Janczewska A. Fetal alcohol spectrum disorders–diagnostic difficulties in the neonatal period and new diagnostic approaches. Dev Period Med. 2019;23(1):60–6. Epub 2019/04/08
Floyd RL, O'Connor MJ, Bertrand J, Sokol R. Reducing adverse outcomes from prenatal alcohol exposure: a clinical plan of action. Alcohol Clin Exp Res. 2006;30(8):1271–5. Epub 2006/08/11. https://doi.org/10.1111/j.1530-0277.2006.00175.x.
Manning MA, Hoyme EH. Fetal alcohol spectrum disorders: a practical clinical approach to diagnosis. Neurosci Biobehav Rev. 2007;31(2):230–8.
Lemoine P, Harousseau H, Borteyru JP, Menuet JC. Les enfants de parents alcoolique. Ouest Med. 1968;21:476–82.
Jones KL, Smith DW. Recognition of the fetal alcohol syndrome in early infancy. Lancet. 1973;302(7836):999–1001.
Jones KL, Smith DW, Ulleland CN, Streissguth P. Pattern of malformation in offspring of chronic alcoholic mothers. Lancet. 1973;1(7815):1267–71.
Clarren SK, Alvord EC Jr, Sumi SM, Streissguth AP, Smith DW. Brain malformations related to prenatal exposure to ethanol. J Pediatr. 1978;92(1):64–7. Epub 1978/01/01. https://doi.org/10.1016/s0022-3476(78)80072-9.
Calhoun F, Warren K. Fetal alcohol syndrome: historical perspectives. Neurosci Biobehav Rev. 2007;31(2):168–71. Epub 2007/01/17. https://doi.org/10.1016/j.neubiorev.2006.06.023.
Astley SJ. Comparison of the 4-digit diagnostic code and the Hoyme diagnostic guidelines for fetal alcohol spectrum disorders. Pediatrics. 2006;118(4):1532–45.
Paintner A, Williams AD, Burd L. Fetal alcohol spectrum disorders–implications for child neurology, part 1: prenatal exposure and dosimetry. J Child Neurol. 2012;27(2):258–63.
Comasco E, Rangmar J, Eriksson UJ, Oreland L. Neurological and neuropsychological effects of low and moderate prenatal alcohol exposure. Acta Physiol (Oxf). 2018;222(1) Epub 2017/05/05 https://doi.org/10.1111/apha.12892.
Del Campo M, Jones KL. A review of the physical features of the fetal alcohol spectrum disorders. Eur J Med Genet. 2017;60(1):55–64. Epub 2016/10/13. https://doi.org/10.1016/j.ejmg.2016.10.004.
Cook JL, Unsworth KL, Flannigan K. Exploring the profile of individual with fetal alcohol Spectrum disorder in Canada with the national FASD database. CMAJ Open–Under Review.
Russell M, Martier SS, Sokol RJ, Mudar P, Jacobson S, Jacobson J. Detecting risk drinking during pregnancy: a comparison of four screening questionnaires. American journal of public health. 1996;86(10):1435–9. Epub 1996/10/01. https://doi.org/10.2105/ajph.86.10.1435.
Ordean A, Wong S, Graves L. No. 349-Substance use in pregnancy. J Obstetr Gynaecol Canada. 2017;39(10):922–37 e2. Epub 2017/09/25. https://doi.org/10.1016/j.jogc.2017.04.028.
American College of O, Gynecologists Committee on Health Care for Undeserved W. ACOG Committee Opinion No. 343: psychosocial risk factors: perinatal screening and intervention. Obstet Gynecol. 2006;108(2):469–77. Epub 2006/08/02. https://doi.org/10.1097/00006250-200608000-00046.
Premji SS, Semenic S. Do Canadian prenatal record forms integrate evidence-based guidelines for the diagnosis of a FASD? Can J Public Health. 2009;100(4):274–80. Epub 2009/09/03
Sword W, Akhtar-Danesh N, McDonald SD, Kaminsky K, Roberts N, et al. Screening and intervention practices for alcohol use by pregnant women and women of childbearing age: results of a canadian survey. J Obstetr Gynaecol Canada. 2020; In Press.
Chasnoff IJ, Wells AM, King L. Misdiagnosis and missed diagnoses in foster and adopted children with prenatal alcohol exposure. Pediatrics. 2015;135(2):264–70. Epub 2015/01/15. https://doi.org/10.1542/peds.2014-2171.
Tenenbaum A, Hertz P, Dor T, Castiel Y, Sapir A, Wexler ID. Fetal alcohol spectrum disorder in Israel: increased prevalence in an at-risk population. Isr Med Assoc J. 2011;13(12):725–9. Epub 2012/02/16
Davies JK, Bledsoe JM. Prenatal alcohol and drug exposures in adoption. Pediatr Clin N Am. 2005;52(5):1369–93 vii, Epub 2005/09/13. https://doi.org/10.1016/j.pcl.2005.06.015.
Bager H, Christensen LP, Husby S, Bjerregaard L. Biomarkers for the detection of prenatal alcohol exposure: a review. Alcohol Clin Exp Res. 2017;41(2):251–61. Epub 2017/01/19. https://doi.org/10.1111/acer.13309.
Bookstein FL, Connor PD, Covell KD, Barr HM, Gleason CA, Sze RW, et al. Preliminary evidence that prenatal alcohol damage may be visible in averaged ultrasound images of the neonatal human corpus callosum. Alcohol. 2005;36(3):151–60. Epub 2005/12/27. https://doi.org/10.1016/j.alcohol.2005.07.007.
Vernescu RM, Adams RJ, Courage ML. Children with fetal alcohol spectrum disorder show an amblyopia-like pattern of vision deficit. Dev Med Child Neurol. 2012;54(6):557–62. Epub 2012/05/12. https://doi.org/10.1111/j.1469-8749.2012.04254.x.
Coffman BA, Kodituwakku P, Kodituwakku EL, Romero L, Sharadamma NM, Stone D, et al. Primary visual response (M100) delays in adolescents with FASD as measured with MEG. Hum Brain Mapp. 2013;34(11):2852–62. Epub 2012/06/08. https://doi.org/10.1002/hbm.22110.
Jacobson SW, Stanton ME, Molteno CD, Burden MJ, Fuller DS, Hoyme HE, et al. Impaired eyeblink conditioning in children with fetal alcohol syndrome. Alcohol Clin Exp Res. 2008;32(2):365–72. Epub 2007/12/29. https://doi.org/10.1111/j.1530-0277.2007.00585.x.
Green CR, Mihic AM, Brien DC, Armstrong IT, Nikkel SM, Stade BC, et al. Oculomotor control in children with fetal alcohol spectrum disorders assessed using a mobile eye-tracking laboratory. Eur J Neurosci. 2009;29(6):1302–9. Epub 2009/03/24. https://doi.org/10.1111/j.1460-9568.2009.06668.x.
Green CR, Munoz DP, Nikkel SM, Reynolds JN. Deficits in eye movement control in children with fetal alcohol spectrum disorders. Alcohol Clin Exp Res. 2007;31(3):500–11. Epub 2007/02/14. https://doi.org/10.1111/j.1530-0277.2006.00335.x.
Marcellus L. Is meconium screening appropriate for universal use? Science and ethics say no. Adv Neonatal Care. 2007;7(4):207–14. Epub 2007/08/19. https://doi.org/10.1097/01.ANC.0000286338.90799.99.
Zizzo N, Di Pietro N, Green C, Reynolds J, Bell E, Racine E. Comments and reflections on ethics in screening for biomarkers of prenatal alcohol exposure. Alcohol Clin Exp Res. 2013;37(9):1451–5. Epub 2013/04/05. https://doi.org/10.1111/acer.12115.
Astley SJ, Clarren SK. A case definition and photographic screening tool for the facial phenotype of fetal alcohol syndrome. J Pediatr. 1996;129(1):33–41.
Astley S, Clarren SK. Diagnostic guide for fetal alcohol syndrome and related conditions: the 4-digit diagnostic code. 2nd ed. Seattle.: Publication services: University of Washington; 1999.
Anthony B, Vinci-Booher S, Wetherill L, Ward R, Goodlett C, Zhou FC. Alcohol-induced facial dysmorphology in C57BL/6 mouse models of fetal alcohol spectrum disorder. Alcohol. 2010;44(7–8):659–71. Epub 2010/06/24. https://doi.org/10.1016/j.alcohol.2010.04.002.
Valentine M, Bihm DCJ, Wolf L, Hoyme HE, May PA, Buckley D, et al. Computer-aided recognition of facial attributes for fetal alcohol spectrum disorders. Pediatrics. 2017;140(6) Epub 2017/12/01 https://doi.org/10.1542/peds.2016-2028.
Mutsvangwa TE, Smit J, Hoyme HE, Kalberg W, Viljoen DL, Meintjes EM, et al. Design, construction, and testing of a stereo-photogrammetric tool for the diagnosis of fetal alcohol syndrome in infants. IEEE Trans Med Imaging. 2009;28(9):1448–58. Epub 2009/04/02. https://doi.org/10.1109/TMI.2009.2017375.
Coles CD, Kable JA, Drews-Botsch C, Falek A. Early identification of risk for effects of prenatal alcohol exposure. J Stud Alcohol. 2000;61(4):607–16. Epub 2000/08/06. https://doi.org/10.15288/jsa.2000.61.607.
Foroud T, Wetherill L, Vinci-Booher S, Moore ES, Ward RE, Hoyme HE, et al. Relation over time between facial measurements and cognitive outcomes in fetal alcohol-exposed children. Alcohol Clin Exp Res. 2012;36(9):1634–46.
Rasmussen C. Executive functioning and working memory in fetal alcohol spectrum disorder. Alcohol Clin Exp Res. 2005;29(8):1359–67.
Pei J, Job J, Kully-Martens K, Rasmussen C. Executive function and memory in children with fetal alcohol Spectrum disorder. Child Neuropsychol. 2011;17(3):290–309. Epub 2011/07/02. https://doi.org/10.1080/09297049.2010.544650.
Doyle LR, Moore EM, Coles CD, Kable JA, Sowell ER, Wozniak JR, et al. Executive functioning correlates with communication ability in youth with histories of heavy prenatal alcohol exposure. J Int Neuropsychol Soc. 2018;24(10):1026–37. Epub 2018/10/17. https://doi.org/10.1017/S1355617718000772.
Easey KE, Dyer ML, Timpson NJ, Munafo MR. Prenatal alcohol exposure and offspring mental health: a systematic review. Drug and alcohol dependence. 2019;197:344–53. Epub 2019/03/05. https://doi.org/10.1016/j.drugalcdep.2019.01.007.
Pei J, Denys K, Hughes J, Rasmussen C. Mental health issues in fetal alcohol spectrum disorder. J Ment Health. 2011;20(5):438–48.
Streissguth AP, Barr HM, Bookstein FL, Sampson PD, Olson HC. The long-term neurocognitive consequences of prenatal alcohol exposure: a 14-year study. Psychol Sci. 1999;10:186–90.
Lemoine P, Harousseau H, Borteyru JP, Menuet JC. Children of alcoholic parents--observed anomalies: discussion of 127 cases. Ther Drug Monit. 2003;25(2):132–6.
O'Connor MJ, Portnoff LC, Lebsack-Coleman M, Dipple KM. Suicide risk in adolescents with fetal alcohol spectrum disorders. Birth Defects Res. 2019;111(12):822–8. Epub 2019/01/25. https://doi.org/10.1002/bdr2.1465.
Goldschmidt L, Richardson GA, De Genna NM, Cornelius MD, Day NL. Prenatal alcohol exposure and offspring alcohol use and misuse at 22years of age: a prospective longitudinal study. Neurotoxicology and teratology. 2019;71:1–5. Epub 2018/11/07. https://doi.org/10.1016/j.ntt.2018.11.001.
Weyrauch D, Schwartz M, Hart B, Klug MG, Burd L. Comorbid mental disorders in fetal alcohol Spectrum disorders: a systematic review. J Develop Behav Pediatr: JDBP. 2017;38(4):283–91. Epub 2017/05/02. https://doi.org/10.1097/DBP.0000000000000440.
Astley SJ. Profile of the first 1,400 patients receiving diagnostic evaluations for fetal alcohol spectrum disorder at the Washington state fetal alcohol syndrome diagnostic & prevention network. J Can Pharmacol Clin. 2010;17(1):e132–e64.
Paintner A, Williams AD, Burd L. Fetal alcohol spectrum disorders–implications for child neurology, part 2: diagnosis and management. J Child Neurol. 2012;27(3):355–62.
Malisza KL, Buss JL, Bolster RB, de Gervai PD, Woods-Frohlich L, Summers R, et al. Comparison of spatial working memory in children with prenatal alcohol exposure and those diagnosed with ADHD; a functional magnetic resonance imaging study. J Neurodev Disord. 2012;4(1):12. https://doi.org/10.1186/1866-1955-4-12.
Crocker N, Vaurio L, Riley EP, Mattson SN. Comparison of adaptive behavior in children with heavy prenatal alcohol exposure or attention-deficit/hyperactivity disorder. Alcoholism, clinical and experimental research. 2009;33(11):2015–23. Epub 2009/09/02. https://doi.org/10.1111/j.1530-0277.2009.01040.x.
Ware AL, Crocker N, O'Brien JW, Deweese BN, Roesch SC, Coles CD, et al. Executive function predicts adaptive behavior in children with histories of heavy prenatal alcohol exposure and attention-deficit/hyperactivity disorder. Alcoholism Clin Exp Res. 2012;36(8):1431–41. Epub 2012/05/17. https://doi.org/10.1111/j.1530-0277.2011.01718.x.
Crocker N, Vaurio L, Riley EP, Mattson SN. Comparison of verbal learning and memory in children with heavy prenatal alcohol exposure or attention-deficit/hyperactivity disorder. Alcoholism Clin Exp Res. 2011;35(6):1114–21. Epub 2011/03/18. https://doi.org/10.1111/j.1530-0277.2011.01444.x.
Vaurio L, Riley EP, Mattson SN. Differences in executive functioning in children with heavy prenatal alcohol exposure or attention-deficit/hyperactivity disorder. J Int Neuropsychol Soc. 2008;14(1):119–29. Epub 2007/12/15. https://doi.org/10.1017/S1355617708080144.
Jacobson JL, Dodge NC, Burden MJ, Klorman R, Jacobson SW. Number processing in adolescents with prenatal alcohol exposure and ADHD: differences in the neurobehavioral phenotype. Alcoholism Clin Exp Res. 2011;35(3):431–42. Epub 2010/12/17. https://doi.org/10.1111/j.1530-0277.2010.01360.x.
Ware AL, O’Brien JW, Crocker N, Deweese BN, Roesch SC, Coles CD, et al. The effects of prenatal alcohol exposure and attention-deficit/hyperactivity disorder on psychopathology and behavior. Alcoholism Clin Exp Res. 2013;37(3):507–16. Epub 2012/09/15. https://doi.org/10.1111/j.1530-0277.2012.01953.x.
Kodali VN, Jacobson JL, Lindinger NM, Dodge NC, Molteno CD, Meintjes EM, et al. Differential Recruitment of Brain Regions During Response Inhibition in Children Prenatally Exposed to Alcohol. Alcoholism Clin Exp Res. 2017;41(2):334–44. Epub 2017/01/12. https://doi.org/10.1111/acer.13307.
Moore EM, Migliorini R, Infante MA, Riley EP. Fetal alcohol spectrum disorders: recent neuroimaging findings. Curr Dev Disord Rep. 2014;1(3):161–72. Epub 2014/10/28. https://doi.org/10.1007/s40474-014-0020-8.
Treit S, Zhou D, Chudley AE, Andrew G, Rasmussen C, Nikkel SM, et al. Relationships between head circumference, brain volume and cognition in children with prenatal alcohol exposure. PLoS One. 2016;11(2):e0150370. Epub 2016/03/02. https://doi.org/10.1371/journal.pone.0150370.
Spadoni AD, McGee CL, Fryer SL, Riley EP. Neuroimaging and fetal alcohol spectrum disorders. Neurosci Biobehav Rev. 2007;31(2):239–45. Epub 2006/11/14. https://doi.org/10.1016/j.neubiorev.2006.09.006.
Jirikowic T, Gelo J, Astley S. Children and youth with fetal alcohol spectrum disorders: summary of intervention recommendations after clinical diagnosis. Intellect Dev Disabil. 2010;48(5):330–44. Epub 2010/10/27. https://doi.org/10.1352/1934-9556-48.5.330.
Hanlon-Dearman A, Malik S, Wellwood J, Johnston K, Gammon H, N Andrew K, Maxwell B, Longstaffe S. A descriptive study of a community-based home-visiting program with preschool children prenatally exposed to alcohol. J Popul Ther Clin Pharmacol. 2017;24(2):e61–e71. https://doi.org/10.22374/1710-6222.24.2.3. PMID: 28632983.
Zarnegar Z, Hambrick EP, Perry BD, Azen SP, Peterson C. Clinical improvements in adopted children with fetal alcohol spectrum disorders through neurodevelopmentally informed clinical intervention: a pilot study. Clin Child Psychol Psychiatry. 2016;21(4):551–67. Epub 2016/11/04. https://doi.org/10.1177/1359104516636438.
Schoeps A, Peterson ER, Mia Y, Waldie KE, Underwood L, D'Souza S, et al. Prenatal alcohol consumption and infant and child behavior: evidence from the growing up in New Zealand cohort. Early Hum Dev. 2018;123:22–9. Epub 2018/07/24. https://doi.org/10.1016/j.earlhumdev.2018.06.011.
Chen JH. Maternal alcohol use during pregnancy, birth weight and early behavioral outcomes. Alcohol Alcohol. 2012;47(6):649–56. Epub 2012/08/16. https://doi.org/10.1093/alcalc/ags089.
Sirvinskiene G, Zemaitiene N, Zaborskis A, Markuniene E, Jusiene R. Infant difficult behaviors in the context of perinatal biomedical conditions and early child environment. BMC Pediatr. 2012;12:44. Epub 2012/04/13. https://doi.org/10.1186/1471-2431-12-44.
Oberlander TF, Jacobson SW, Weinberg J, Grunau RE, Molteno CD, Jacobson JL. Prenatal alcohol exposure alters biobehavioral reactivity to pain in newborns. Alcoholism Clin Exp Res. 2010;34(4):681–92. Epub 2010/02/04. https://doi.org/10.1111/j.1530-0277.2009.01137.x.
Carter RC, Jacobson SW, Molteno CD, Chiodo LM, Viljoen D, Jacobson JL. Effects of prenatal alcohol exposure on infant visual acuity. J Pediatr. 2005;147(4):473–9. Epub 2005/10/18. https://doi.org/10.1016/j.jpeds.2005.04.063.
de Beer M, Kritzinger A, Zsilavecz U. Young children with fetal alcohol spectrum disorder--communication profiles. S Afr J Commun Disord. 2010;57:33–42. Epub 2011/02/19. https://doi.org/10.4102/sajcd.v57i1.47.
Sujay NK, Jones M, Whittle E, Murphy H, Auth MK. Severe gastrooesophageal reflux disease associated with foetal alcohol syndrome. Case Rep Pediatr. 2012;2012:509253. Epub 2012/09/08. https://doi.org/10.1155/2012/509253.
Jacobson SW, Jacobson JL, Molteno CD, Warton CMR, Wintermark P, Hoyme HE, et al. Heavy prenatal alcohol exposure is related to smaller corpus callosum in newborn MRI scans. Alcoholism Clin Exp Res. 2017;41(5):965–75. Epub 2017/03/02. https://doi.org/10.1111/acer.13363.
Molteno CD, Jacobson JL, Carter RC, Jacobson SW. Infant symbolic play as an early indicator of fetal alcohol-related deficit. Infancy. 2010;15(6):586–607. Epub 2010/10/19. https://doi.org/10.1111/j.1532-7078.2010.00031.x.
Chudley AE, Kilgour AR, Cranston M, Edwards M. Challenges of diagnosis in fetal alcohol syndrome and fetal alcohol spectrum disorder in the adult. Am J Med Genet C Semin Med Genet. 2007;145C(3):261–72. https://doi.org/10.1002/ajmg.c.30140.
Allen GC, Farnell YZ, Maeng JU, West JR, Chen WJ, Earnest DJ. Long-term effects of neonatal alcohol exposure on photic reentrainment and phase-shifting responses of the activity rhythm in adult rats. Alcohol. 2005;37(2):79–88. Epub 2006/04/06. https://doi.org/10.1016/j.alcohol.2005.11.003.
Volgin DV, Kubin L. Reduced sleep and impaired sleep initiation in adult male rats exposed to alcohol during early postnatal period. Behav Brain Res. 2012;234(1):38–42. Epub 2012/06/16. https://doi.org/10.1016/j.bbr.2012.06.002.
Church MW, Hotra JW, Holmes PA, Anumba JI, Jackson DA, Adams BR. Auditory brainstem response (ABR) abnormalities across the life span of rats prenatally exposed to alcohol. Alcoholism Clin Exp Res. 2012;36(1):83–96. Epub 2011/08/06. https://doi.org/10.1111/j.1530-0277.2011.01594.x.
Kelly SJ, Goodlett CR, Hannigan JH. Animal models of fetal alcohol spectrum disorders: impact of the social environment. Dev Disabil Res Rev. 2009;15(3):200–8. Epub 2009/09/05. https://doi.org/10.1002/ddrr.69.
Morley R, Dwyer T, Hynes KL, Cochrane J, Ponsonby AL, Parkington HC, et al. Maternal alcohol intake and offspring pulse wave velocity. Neonatology. 2010;97(3):204–11. Epub 2009/10/30. https://doi.org/10.1159/000252973.
Akison LK, Moritz KM, Reid N. Adverse reproductive outcomes associated with fetal alcohol exposure: a systematic review. Reproduction. 2019;157(4):329–43. Epub 2019/01/18. https://doi.org/10.1530/REP-18-0607.
Ramlau-Hansen CH, Toft G, Jensen MS, Strandberg-Larsen K, Hansen ML, Olsen J. Maternal alcohol consumption during pregnancy and semen quality in the male offspring: two decades of follow-up. Hum Reprod. 2010;25(9):2340–5. Epub 2010/07/01. https://doi.org/10.1093/humrep/deq140.
Ma X, Coles CD, Lynch ME, Laconte SM, Zurkiya O, Wang D, et al. Evaluation of corpus callosum anisotropy in young adults with fetal alcohol syndrome according to diffusion tensor imaging. Alcohol Clin Exp Res. 2005;29(7):1214–22. Epub 2005/07/28. https://doi.org/10.1097/01.alc.0000171934.22755.6d.
Fagerlund A, Heikkinen S, Autti-Ramo I, Korkman M, Timonen M, Kuusi T, et al. Brain metabolic alterations in adolescents and young adults with fetal alcohol spectrum disorders. Alcohol Clin Exp Res. 2006;30(12):2097–104. Epub 2006/11/23. https://doi.org/10.1111/j.1530-0277.2006.00257.x.
Chen X, Coles CD, Lynch ME, Hu X. Understanding specific effects of prenatal alcohol exposure on brain structure in young adults. Hum Brain Mapp. 2012;33(7):1663–76. Epub 2011/06/22. https://doi.org/10.1002/hbm.21313.
Spohr HL, Steinhausen HC. Fetal alcohol spectrum disorders and their persisting sequelae in adult life. Dtsch Arztebl Int. 2008;105(41):693–8. Epub 2009/07/23. https://doi.org/10.3238/arztebl.2008.0693.
Kully-Martens K, Denys K, Treit S, Tamana S, Rasmussen C. A review of social skills deficits in individuals with fetal alcohol spectrum disorders and prenatal alcohol exposure: profiles, mechanisms, and interventions. Alcohol Clin Exp Res. 2012;36(4):568–76.
Freunscht I, Feldmann R. Young adults with fetal alcohol syndrome (FAS): social, emotional and occupational development. Klin Padiatr. 2011;223(1):33–7. Epub 2010/08/03. https://doi.org/10.1055/s-0030-1261927.
Acknowledgments
The authors would like to acknowledge the authors of the 2016 Fetal alcohol spectrum disorder: a guideline for diagnosis across the lifespan for their work reviewing some of this background material during the guideline development process.
Multiple Choice Questions
-
1.
Which of the following nomenclature for FASD is not a diagnosis?
-
a.
FASD with Sentinel Facial Features
-
b.
FASD without Sentinel Facial Features
-
c.
At Risk for Neurodevelopmental Disorder and FASD, Associated with Prenatal Alcohol Exposure
-
d.
Alcohol-Related Neurodevelopmental Disorder
-
a.
-
2.
Which of the following diagnostic criteria is no longer needed for diagnosis?
-
a.
Growth
-
b.
Facial dysmorphology
-
c.
Brain dysfunction
-
d.
Congenital abnormalities
-
a.
-
3.
How is neurodevelopmental impairment calculated?
-
a.
< 1 standard deviation below the mean
-
b.
< 1.5 standard deviations below the mean
-
c.
< 2 standard deviations below the mean
-
d.
< 3 standard deviations below the mean
-
a.
-
4.
What is the minimum number of domains of impairment required to confirm neurodevelopmental deficits for a FASD diagnosis?
-
a.
1 domain
-
b.
2 domains
-
c.
3 domains
-
d.
5 domains
-
a.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Cook, J.L., Green, C.R. (2023). Fetal Alcohol Spectrum Disorder: Diagnosis. In: Eisenstat, D.D., Goldowitz, D., Oberlander, T.F., Yager, J.Y. (eds) Neurodevelopmental Pediatrics. Springer, Cham. https://doi.org/10.1007/978-3-031-20792-1_24
Download citation
DOI: https://doi.org/10.1007/978-3-031-20792-1_24
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-20791-4
Online ISBN: 978-3-031-20792-1
eBook Packages: MedicineMedicine (R0)