Abstract
The quality of pharmaceutical preparations is the result of the planning and implementation of the manufacturing process. The Good Manufacturing Practice (GMP) principles and guidelines are about incorporating quality into all aspects of the manufacturing process. This chapter covers the planning, implementation, monitoring and validation of the process, as well as product quality control and release.
Preparations differ in size and complexity. The scale can range from a tailor-made preparation for one patient to production for many thousands of patients. The complexity can range from reconstitution to complex preparations from active pharmaceutical ingredients (API) and excipients. For all kind of preparations it is essential to minimise the risk of mix-up or cross-contamination by applying technical measures and an appropriate working discipline. All preparation steps must be controlled and traceable. A validated procedure for quarantine, final quality control and release has to be in place. Furthermore, to guarantee the quality and safety of a product the preparation and cleaning processes have to be validated, including the qualification of premises and equipment. These validation activities have to be planned and executed in accordance with quality risk management principles.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Production
- In-process controls
- Line clearance
- Reconciliation
- Quality control
- Quarantine
- Release
- Cleaning
- Qualification
- Validation
The text on parametric release has been rewritten, in accordance with the new version of GMP Annex 17, and is now included as a separate section. New concepts, such as Process Analytical Technology, Quality by Design and Real Time Release Testing have been introduced.
In the sections on qualification of equipment and installations and on process validation, retrospective qualification and retrospective validation have been removed, in line with the latest version of GMP Annex 15.
A new figure has been added to illustrate the relationship between process validation and qualification of equipment, computerised systems and personnel, driven by product quality requirements. The V-diagram showing the different phases of qualification and validation has been redesigned.
The section on good cleaning practice and cleaning validation has been improved.
Minor improvements have been made throughout the chapter.
The reference list has been updated.
FormalPara Learning Objectives-
The reader understands the principles of Good Manufacturing Practice.
-
The reader learns about production and quality control of different kinds of products – from tailor-made production for one patient to large scale production for many patients.
-
The reader is aware of the main elements to be included in risk assessment and planning, when a new or a well-known product has to be prepared.
-
The reader understands the importance of adequate material handling and keeping good batch documentation, so that all operations are traceable.
-
The reader learns about the different methods used for quality assurance, like the execution of in process controls, physical and microbiological monitoring, qualification and validation.
-
The reader is aware of the importance of technical and organisational measures to prevent (cross-)contamination and mix-ups, line clearance and yield and label reconciliation.
-
The reader understands the need of a watertight quarantine and release policy.
-
The reader knows the principles of parametric release.
32.1 Introduction
This chapter is about preparation and quality control of medicines. The text is mainly based on Chaps. 5, 6 and Annex 15 of the GMP [1,2,3]. We have chosen to clarify a selected number of subjects from these GMP chapters and to give some practical examples. The main topics discussed are briefly introduced below.
Preparations can be divided into stock preparations and extemporaneous preparations. The principles described in this chapter are applicable to both stock preparations and extemporaneous preparations. However, the amount of quality control and validation may be reduced in extemporaneous preparations due to the small number of affected patients and the need to deliver urgently.
Product quality is the result of the design quality, documentation and execution of the preparation or manufacturing process. Production activities must follow clearly defined procedures and must comply with the principles of GMP in order to obtain products that meet the quality requirements. GMP means incorporating quality into all aspects of the process (see Chap. 35).
First of all, measures to prevent (cross-)contamination and mix-ups must be in place. These measures can be technical or organisational. Other methods to guarantee a safe process include adequate documentation, in-process controls, line clearance, yield and label reconciliation. All processes should be validated, controlled and supervised.
Quality Control is concerned with sampling, specifications and testing as well as organisation, documentation and release procedures. These processes ensure that materials and products are not released for use until their quality has been judged satisfactory. Quality Control must be involved in all decisions that may concern the quality of the product. The independence of Quality Control from Production is fundamental.
Batch documentation review and analytical testing are decisive for the release of the products. To ensure a safe release process a watertight quarantine procedure must be used.
An important part of this chapter is dedicated to validation and qualification. It is a GMP requirement that critical aspects of production activities are controlled through qualification and validation. This should occur during the lifecycle of the premises, equipment, processes and products. Any planned changes to the facilities, equipment and processes should be formally documented and the impact on the validated status or control strategy assessed. Decisions on the scope and extent of validation and qualification should be based on a justified and documented risk assessment.
Personnel issues, premises and equipment, which may affect the described processes, are discussed elsewhere (Chaps. 25, 27 and 28 respectively), as well as the product design (Chap. 4) and the documentation of the preparation process (Chap. 37).
32.2 Quality of Production
Preparations differ in size and complexity. The scale may range from a tailor-made preparation for one patient to (semi-)industrial production for thousands of patients. The complexity may range from the reconstitution of an authorised medicine to complex preparations from active ingredients and excipients. In this chapter we focus mainly on stock preparations. The principles described are equally applicable to simpler preparations (such as extemporaneous preparations) or reconstitution [4]. However, the extent of quality control and validation should be based on risk assessment [5, 6 and Chap. 36].
The main elements to guarantee the quality of the preparation process are:
-
The use of qualified and validated premises, systems and equipment
-
The use of active ingredients, excipients and primary packaging materials of suitable quality
-
The application of a validated preparation process
-
A validated program for cleaning of premises, equipment, utensils and clothing
-
Minimisation of the risk of mix-up or cross-contamination
-
A clear description of all operations in preparation instructions, operating instructions and procedures (see Chap. 37)
-
Continuous education and training of employees (see Chap. 25)
-
A clear indication of identity and/or status of materials, premises and equipment in all phases of the production process
-
The control and recording of all essential preparation steps, so they are traceable
-
The use of deviations, errors, complaints, changes, audit results and periodic evaluation or revalidation of preparation processes for continuous optimisation of the production process and the necessary conditions (see also Chap. 35)
-
A comprehensive procedure for quarantine, final inspection and release
These essential elements are elaborated in the following sections or are cross-referred.
Products that are prescribed sporadically, with a variable composition and a limited shelf life are often prepared extemporaneously. Preferably a standardised preparation instruction is used, because this is the best guarantee for a reproducible preparation process. Often only the batch size is varied, because the required amount may differ for each patient. For example, the amount of a cutaneous preparation required depends on the body area to be treated, the nature of the preparation and the duration of treatment.
If a standardised preparation instruction is not available, a non-standardised preparation instruction has to be drafted ad hoc. This increases the risk of errors. Therefore, it is preferable to make a template for each type of preparation where only the active substances and the amount have to be added. For instance, templates of preparation instructions for capsules or suppositories could be developed (see Chap. 37). The appropriateness of the templates has to be demonstrated, including the preparation method.
Many preparations for individual patients concern reconstitution of licensed products. Examples are dissolving and diluting a powder for injection or creating an antibiotic suspension. Again, quality is incorporated by standardising the instructions and in-process controls applied.
The quality of preparation and manufacturing processes is based on a combination of technical and organisational measures, instructions, in-process controls, reconciliation, quality control (QC) and documentation. An automated system is recommended for the process support.
32.3 Prevention of Contamination and Cross-Contamination
32.3.1 Technical Measures
Contamination is the pollution of raw materials (active ingredients, excipients and primary packaging materials), product or equipment with dust or microorganisms. Cross-contamination is pollution with substances from other preparations. Measures to prevent (cross-)contamination include the use of dedicated and well-designed facilities and equipment (e.g. closed systems), maintaining adequate ventilation in rooms and pressure differences between rooms, as well as the partitioning of areas where different activities take place. The partitioning of rooms, with walls or partitions on workbenches, reduces the risk of mix-ups and (cross-)contamination. Other technical measures, such as the installation of barriers, the use of different floors colours support the maintenance of a proper work discipline. Performing a valid cleaning process of rooms, equipment and utensils (see Chap. 33) will prevent cross-contamination. Furthermore, the use of single-use materials (disposables) or dedicated equipment can be considered to reduce the risk of cross-contamination.
32.3.2 Organisational Measures
It cannot be stressed enough that people are a key risk factor for contamination and cross-contamination. The work discipline should aim to avoid mix-up of materials at each stage of the preparation process. The golden rule is: never work on different products in the same room simultaneously or subsequently, unless any risk of confusion is excluded. An example of achieving this is the practice of performing only one preparation per workplace and that this workplace is released before starting a new preparation: the so-called line clearance. It is recommended to organise the work in such a way that once started, preparations can be completed undisturbed and uninterrupted.
A logical method is needed to avoid mix-ups. An example is the weighing process of different ingredients, where all steps (identification, opening container, weighing and replacing of the container) always take place in the same logical order. The weighed ingredients must preferably be processed immediately. If this is not possible, encode them and keep them together so that it is clear for which preparation they are intended.
Another example is the implementation of line clearance. At the end of the process all printed labels not attached to the product and packaging materials, must carefully be removed and destroyed before a new product is labelled. Correct performance of the line clearance must be verified.
A good working discipline is essential to prevent cross-contamination. This requires careful planning and a system for identification. The identity of the product in preparation must be indicated on doors or walls of rooms, equipment and vessels. For this purpose labels can be used, or a form that is part of the batch preparation record. Logbooks play an important role in recording the history of use of rooms and equipment (see Chap. 37). If a room or equipment has been cleaned according to the applicable procedure, the status indication “clean” has to be applied.
In extemporaneous preparations, the identification of premises, equipment and vessels is not necessary because of the very short processing time. A clean workspace, clean materials and line clearance are sufficient.
Working procedures need to be controlled. During weighing and processing of ingredients, the generation of dust has to be prevented. Manufacturing processes and cleaning operations must be carried out in such a way that remnants of preparations cannot end up elsewhere. If this does happen, for example in a calamity, a proper cleaning procedure has to be followed before the room or equipment can be released for the next preparation process.
32.3.2.1 Supervision
Despite the presence of well-trained staff and clear documents, unplanned deviations from the procedures and agreements may occur. This requires supervision of working behaviour by for example the immediate superior, or team leader. A stepwise supervision system can be considered, in which experienced pharmacy technicians, the team leader and pharmacists play a role. In all cases it is helpful to make checklists to record all control operations that are part of the supervision carried out. Examples of items on such a checklist are the control of completing logbooks and cleaning verification.
32.4 Material Handling
It is important to have clear procedures about routing and encoding, to ensure traceability of materials. These procedures specify that all materials are put into quarantine upon arrival. They are then sampled, tested and finally released. In all these steps, the status of the article must be clear. Until release the status is “in quarantine”. Upon sampling of raw materials it is recommended to indicate containers with a label “sampled” and to note the date of sampling for ingredients with a short shelf life after opening. Upon release a label is attached on the container with identifying names, a code referring to quality control and the expiry date. The quality control code or number may be printed in the form of a barcode. This facilitates identification when weighing or measuring the ingredients, as this code includes the identity, status and expiry date of the material. Only released ingredients may be used for preparation. Packaging materials and labels are processed the same way as pharmaceutical ingredients.
During the preparation process, it is also important that materials have been identified and that the status of the process phase is unambiguous. If ingredients are not immediately processed after weighing or volume measurement, their container has to be unambiguously labelled with the name and batch number of the target preparation.
The storage conditions and allowed storage period of bulk and intermediate product should be mentioned in the product dossier and, if applicable, the product should be stored securely. At relevant points in the process the quarantine status is indicated and monitored. An example is an intermediate or bulk product that is not directly processed further. Unambiguous procedures for dealing with surplus and discarded materials must be in place. Excess materials may only be returned to stock if these procedures are met. For example, how to deal with sterile materials when the overpouch is removed has to be defined.
If it is not yet clear whether materials can be used in the future, the material has to be marked clearly with “quarantine” and stored separately.
The way rejected materials and products should be removed safely has to be described in a procedure. In addition, a procedure on the conditions for reprocessing (when an intermediate or bulk product does not meet the requirements) has to be in place. Reprocessing should be minimised performed only in close collaboration with the quality control laboratory and documented carefully. The reprocessing of previously delivered and returned products must not be performed.
32.5 Batch Documentation
The function of the batch documentation or the batch record, is to document the entire process (from weighing of ingredients to the release) and provide traceability of materials, premises and equipment (see Chap. 37). This enables easy reference to processes and procedures. For the purposes of quality control, all deviations from the intended process must be recorded. As part of continuous quality improvement, it is useful to record suggested improvements to the preparation instructions on the batch record.
The weight and/or volume measurement of ingredients must be verified independently. Both the weighing/measurement and the verification need to be recorded. If an automated system is used for these recordings, it should be validated.
32.6 In-Process Controls
In-process controls, also called IPC’s, are important parts of the batch documentation. These are checks incorporated into the preparation process, in order to ensure that critical process steps have been performed correctly. There are quantitative or numerical IPC’s, where results are logged (e.g. pH value) as well as qualitative or alphanumeric IPC’s, where an observation is described (e.g. colour) or ticked off and initialed (e.g. if a solution is clear). Some IPC’s relate to the product (e.g. homogeneity) and some to the process (e.g. a mixing time) – but all IPC’s should be related to the initial risk assessment and process and/or product design.
Unnecessary IPC’s may reduce the awareness and discipline of the personnel, so it is important to consider carefully whether IPC’s are really needed to control product quality. An example is the preparation of an all-in-one parenteral nutrition admixture of which the aqueous part has to be checked for clarity, because precipitates or particulate matter cannot be detected after the fat emulsion is added. In this case, an IPC is necessary before adding the fat emulsion. IPC’s are also used to control critical process steps when verification is not possible during the final quality control of the product. An example of this is the control of the application of nitrogen to remove oxygen from ampoules following the filling process. The quality control laboratory is unable to measure the oxygen content in each ampoule. This IPC is based upon the validation of the oxygen replacement process.
The results of the IPC’s are useful for trend analysis and the validation of preparation and manufacturing processes.
32.7 Label and Yield Reconciliation
Labelling and packaging operations are an essential part of the production process. These operations can be recorded in a separate packaging record. However, in pharmacies, given the limited batch sizes and the relatively short process time, it is common to include these operations in the batch preparation record.
In general, roll-feed labels are preferable to cut-labels in order to prevent mix-ups. When reconciling the printed labels, unused and discarded labels should be included. The reconciliation has to include all labels utilised for primary and secondary packaging, for labelling the quality control samples and for documentation in the batch record and logbook, if applicable. The number of rejected labels (for example, due to poor printing quality) should also be recorded.
The production yield must be recorded in an unambiguous manner, detailing both units produced and rejected (e. g. due to breakage) at various stages of the process. Any deviation from expected yield should be explained. See example in Table 32.1.
Table 32.1 shows that ampoules are packed in boxes of 12. At first glance the reconciliation seems accurate. Upon closer inspection, there are some deviations. Ten ampoules are not labeled and two boxes have been over-labeled (4116 ampoules correspond to 343 boxes). It should be verified if line clearance has been performed correctly. Also the batch has to be inspected (are all boxes filled?) and the ampoules and boxes have to be recounted. An inconclusive reconciliation may be a result of counting and/or writing errors. The relatively low yield is explained satisfactorily. However, verification of sufficient inspection of ampoules (glass particles present?) is needed. Also additional particle counts may be considered because of the reported problems when closing ampoules.
32.8 Quarantine Management
To prevent the delivery of unapproved products, a watertight quarantine policy is very important. Materials with a quarantine status must be suitably separated from released materials.
The following items must have quarantine status:
-
Unreleased starting materials
-
Intermediate and bulk products which are not directly processed further
-
Filled units that have not yet been labelled
-
End products not yet analysed or released or both
-
Starting materials or products where quality doubt has arisen after release of the batch in question
It is preferable that these items are placed in a lockable quarantine room. An alternative is storing in lockable cabinets or quarantine-carts. Access to quarantine locations should be limited to a small number of people.
If storage in a closed quarantine location is not possible, for example a bulk product in a production vessel that is not directly processed further, quarantine status is indicated with a prominent, well-attached label.
Quarantine status is indicated on the batch documentation, to include the number of items placed in quarantine and the number of samples for quality control, reference and retention [7].
32.9 Quality Control and Release
32.9.1 Batch Documentation Review
Final inspection is an essential element in controlling the quality of pharmaceutical preparations. In the first place, final control comprises the review of the batch documentation. In a larger organisation, such as a hospital, this is often the task of the production pharmacist.
The final inspection of batch documentation should comprise the following checks:
-
Have all ingredients and packaging materials been identified properly and has the correct amount of each substance been processed?
-
Have all items of the batch record been completed correctly?
-
Have all initials been set?
-
Are all IPC’s within limits and have any discrepancies been handled correctly?
-
Has the necessary documentary evidence, such as print-out of pH meter, label of used filter, print-out of filter testing device, sterilisation indicator and sterilisation report, been attached?
-
Are raw data for critical processes within specifications?
-
Have the correct labels been used and are the printed data correct and complete?
-
Has the label and yield reconciliation, including line clearance, been performed correctly?
-
Have deviations, if any, been documented and concluded adequately?
If deviations have occurred this must be noted on the batch record. For example, if sterilization has been carried out over too long a timeframe, special attention must be paid during analysis to the potential presence of degradation products.
32.9.2 Quality Control
The Quality Control (QC) department has to operate according to Good Quality Control Laboratory Practice (GQCLP) standards [2]. All QC methods have to be validated and verified before application. The instruments used for QC are qualified and calibrated before QC testing is performed. There is a procedure in place for the investigation of Out Of Specification (OOS) and Out Of Trend (OOT) results. The reference standards used should be certified, qualified and verified. Documentation and traceability are important, just like in production. All raw data should be retained.
During quality control the laboratory checks whether the product meets all specifications. The control of the end product includes a number of non-destructive tests, such as checking the yield, determining the weight distribution (e.g. capsules) and a visual control of packaging and labelling. Subsequently, the required analytical and microbiological tests are carried out. The assessment of the finished product includes production conditions, results of IPC’s, batch documentation review and conformity of the final product with the specifications.
An important part of quality control is the sampling policy (number of samples, method of sampling, select or random samples or both; see Chap. 38). The samples must be taken when and where the risk of deviation is greatest (for example of worst case procedure, see 11.5 for sampling suspension-type suppositories after serial filling). In addition, samples are taken for stability testing (reference and retention samples) and validation [7].
QC is not restricted to laboratory operations, but should be involved in all decisions related to product quality (see Chap. 35). As an example, QC participates in the investigation of complaints about product quality. QC is involved in the assessment and monitoring of product stability as well. The QC department should approve the IPC methods used in production. In all situations, the independence of QC from the production department is fundamental.
When the pharmacy doesn’t have its own facilities for conducting pharmaceutical analysis, QC activities may be outsourced [11].
32.9.3 Release Policy
The final release of products is a major responsibility, which must be carried out by someone independent of production. In the pharmaceutical industry, release is performed by a qualified person (QP) and in pharmacies usually by a pharmacist. Investigational medicinal products (IMPs) always have to be released by a registered QP (see Chap. 25).
The extent of the final inspection and release policy depends on the type of preparation. Thus, for extemporaneous preparations an independent control of the preparation record and a few non-destructive inspections of the product are sufficient. If no abnormalities are observed, an authorised pharmacist can perform the product release. In some countries an authorised employee (e.g. an analyst) may release the extemporaneous prepared product conditionally. Later, within a defined time-frame, the authorised pharmacist releases the product formally.
In some situations, for example with very short-lived radiopharmaceuticals, conditional release is needed before all QC tests have been performed (see Sect. 23.6.8). As a consequence, process validation is important. A recall procedure must be carried out immediately when product quality is found to be insufficient.
Stock preparations usually undergo extensive analytical control (see Sect. 32.9.2) and remain in quarantine until the QC is fully completed (see Sect. 32.9). The release is based on the batch documentation review in combination with the analytical quality controls. During release, final reconciliation takes place. For certain preparations (e.g. aseptic preparations) the results of environmental monitoring are included.
32.9.4 Parametric Release and Real Time Release Testing
Parametric release is a system of release that provides assurance that the product meets the intended quality requirements based on information collected during the preparation process. This procedure has to comply with specific GMP requirements related to parametric release [8]. This release principle is based on the recognition that a comprehensive set of in-process tests and controls may provide greater assurance that the product meets the specifications, rather than final product testing. Parametric release may be applicable for the routine release of finished products without carrying out a sterility test and may be authorised if the batch documentation provides sufficient assurance, on its own, that the process designed and validated to ensure the sterility of the product has been performed correctly. By application of process analytical technology (PAT), the quality by design (QbD)-principle and quality risk management (QRM) it is possible to extend the concept of parametric release to real time release testing. In this case, the finished product testing is replaced by the control of relevant process parameters and material attributes.
Real time product testing and parametric release of products with a market authorisation has to be authorised by the competent authorities. Authorisation is based on a strict set of requirements described in annex 17 of the EU GMP [8]. The principle of parametric release is also used in the release of terminally sterilised products in hospital pharmacies (see Chap. 30). The requirements mentioned in GMP annex 17 have to be described in a procedure. One of the requirements is a risk assessment of the complete production process (see box in Sect. 32.14.1).
32.10 Validation: General Principles and Terminology
32.10.1 Validation and Qualification
GMP (Annex 15) requires that the manufacturer controls the critical properties of the product and the critical steps in the process [3]. This means that the quality of the design of the product, the preparation or manufacturing process, the equipment and automated systems used all have to be assured. The organisation must demonstrate that processes, equipment, systems, installations and analysis perform reliably and reproducibly under all possible conditions. This is usually called validation.
According to GMP, validation means providing evidence that any procedure, process, equipment, material, activity or system actually leads to the expected results. Qualification is proving that any equipment is operating correctly and meets the requirements of the validated process. The definition of validation is sometimes widened to incorporate the concept of qualification.
Because of their somewhat vague and overlapping definitions, the terms validation and qualification are often used interchangeably. In this chapter the term qualification is used for equipment and personnel and the term validation when assessing processes or methods.
32.10.2 Prospective and Concurrent Validation
As a rule, qualification of equipment and building-related installations takes place before putting them into operation; this is called prospective qualification. Validation of preparation and manufacturing processes is preferably carried out prospectively as well, when designing a new process. However, in some situations qualification or validation has to be performed simultaneously with the application of the equipment or process; this is called concurrent qualification or validation. Concurrent qualification or validation should only be applied to simple equipment or processes, where there is little chance that the outcome would be negative and products would have to be rejected.
In the past, retrospective validation (evaluating and assessing data from the past) was also performed. In the latest version of GMP annex 15 this is no longer allowed.
When process changes occur, it has to be ascertained that the product still meets the specifications and it must be decided whether revalidation is necessary to prove this. Therefore, an effective change control procedure has to be in place.
32.10.3 Revalidation and Requalification
A one-time validation or qualification is not sufficient. The minimum requirement is that the status of validation and qualification has to be evaluated on a regular basis. The evaluation frequency has to be pre-defined in accordance with a risk-based approach. The evaluation has to include a systematic review of any changes, deviations or trends in performance, e.g. as indicated by test results. If the evaluation leads to the conclusion that the “validated state” is changed a targeted revalidation has to be carried out. If there is no indication or need for revalidation the evaluation is documented in a report, which has to be approved by the same persons as for the initial validation or qualification. For sterilisation processes re-validation is mandatory every year. Beyond the planned revalidation a critical change in the equipment, the process or the product range is a major reason for intermediate revalidation.
All proposed changes must be handled according to the change control procedure (see Chap. 35) to determine their impact on all related equipment, systems and processes. A standardised risk assessment procedure may be helpful to determine the extent of revalidation activities. It is usually not necessary to entirely repeat the initial validation. Guided by the quality requirements of the product and the nature of the changes, it is decided which parts of the initial validation have to be repeated.
32.10.4 Organisation
In general, the head of the production department and the head of the QC department have management responsibility for the validation program. Quality staff may play a significant supporting role in supporting validation activities. The final responsibility for validation is described in the validation master plan (see Sect. 32.11). Validation activities should only be performed by suitably trained personnel who follow approved validation procedures.
Despite its complexity, validation provides benefits. Besides the increased control of processes, validation provides more insight into the critical factors, which can result in increased patient safety, fewer errors and less rejections. The PIC/S has published a recommendation regarding validation, which may be used as reference material [9]. However, the latest version is from 2007 and recent developments are not included.
In the following sections the principles and different types of validation and qualification are elaborated.
32.11 Validation Master Plan
Validation has to be planned, implemented and maintained in the total life cycle of products, premises, equipment and systems. A systematic approach targeted at local conditions is mandatory and it is recommended to document this approach in a so-called validation master plan (VMP) [3, 9]. According to Annex 15 of the GMP a validation master plan contains the following topics:
-
Validation policy
-
Organisational structure of validation activities
-
Summary of facilities, systems, equipment and processes to be validated
-
Documentation format: templates for instructions and reports
-
Planning and scheduling
-
Change control
-
Reference to existing documents
The validation policy indicates the necessity of the validation activities and the responsibility of the management, so that the preconditions for implementation can be met.
In the VMP the organisation of the validation activities and the tasks of the members of the validation team (see below) are laid down. What to validate and to what extent is decided after the execution of a risk assessment. Frequently used methods for risk assessment are described in ICH Q9 [10] (see also Chap. 36).
Through prioritisation, the sequence of the qualification and validation activities is formulated. For all equipment and processes acceptance criteria have to be set based on a risk assessment including critical aspects for the respective product range. Tests in relation to acceptance criteria are described in test plans. Tests have to be reported and the approved report may be the base for future change control. Ideally, instructions and reports with a fixed layout are used.
Qualification and validation may be outsourced. However, the responsibility remains in-house so the contract-taker has to be approved according to current GMP requirements for outsourced activities [11]. For example, the following qualification and validation items may be outsourced: LAF cabinets, safety cabinets, HVAC-systems, sterilisers, rinsing machines and filter integrity testing devices. When qualification and validation are outsourced, approval of instructions, raw data and reports have to take place according to internal procedures.
Activities should be planned in a logical way to complete the validation efficiently. After listing and prioritising the activities a validation plan (including costs and need for resources) and a timetable are formulated and presented to the management. A logical plan begins with the validation of the analytical methods because they support the conclusions of the process validation. Furthermore, before initiation of process validation of production processes the qualification of the relevant equipment has to be finalised. For example, before validating aseptic processes, qualification of the HVAC-installation and the LAF cabinets has to be finished.
32.12 Validation Documentation
Documentation is an important part of validation. Prior to the execution, validation instructions need to be set up. The persons responsible for the validation check and authorise these instructions.
Validation instructions and reports may include the following sections:
-
Introduction
-
Responsibilities and tasks (for executing activities, for evaluation the results and for release)
-
Validation test plans
-
Acceptance criteria
-
Results
-
Conclusion
-
Recommendations for revalidation
The results of the validation are archived in a validation file. A validation file of equipment may consist of the following chapters: URS, functional/technical specification, DQ, IQ, OQ, PQ, revalidation (see Sect. 32.15).
32.13 Validation Team
For successful validation a multidisciplinary approach, involving production, quality control, quality assurance and technical support, is mandatory. The GMP designates the head of production and the head of quality control as the responsible persons for validation.
Extensive and complex validations can be addressed by establishing a validation team. The validation team may consist of the responsible pharmacists for production, quality control and quality management, and a pharmacy technician, an analyst, a quality manager and a technical expert. If necessary, a person with additional expertise may be added to the team. In larger projects, the validation team can act more decisively by working with a steering committee (e.g. pharmacists and quality manager) and dedicated working groups for each validation topic. In the formation of a validation team it is important to incorporate thorough knowledge of the process to ensure the best possible assessment of quality risks and to set the right priorities.
32.14 Process Validation
32.14.1 General Aspects
Process validation aims to show that the producer controls (the critical steps of) the process so the preparation method consistently leads to the intended result [12, 13]. The structure and the critical steps of the process have to be determined using process analysis and risk assessment (see Chap. 36). The effects of deviations in the preparation process have to be determined in order to define the limits for critical parameters during routine production, the so-called design space (see Chap. 4).
In most cases, a preparation process is not designed from scratch. Typically, the process, whether or not after acquisition from the literature or from a colleague, is optimized continuously and recorded in procedures and instructions. A useful tool in the development and validation of the preparation process is process analysis. To this end, the entire process is divided into small steps (unit operations), which are performed after each other. It must be clear how each step has to be carried out and which conditions have to be met (see example in Table 32.2). The correctness of each process step has to be checked, for example by performing in-process controls. Also, the influence of external circumstances or factors on the different process steps has to be verified.
A useful tool in the further development of a process is risk assessment ([10], see also Chap. 36). Based on the severity of possible errors in the process steps, the probability of occurrence and the timely detectability of a mistake, the preparation process can be provided with appropriate instructions and in-process controls (see example below).
A detailed evaluation of a process is not only necessary for the optimisation of a preparation process, but also for the validation.
-
A risk assessment is the basis for parametric release of sterilisation processes, replacing the sterility test. One of the requirements of GMP Annex 17 for applying parametric release is the implementation of a risk-analysis of the sterility assurance system [8]. All process steps in which errors may occur are listed. Then the severity of any possible error, the probability of occurrence of these errors and the likelihood of non-detection of the error are assessed. Each of these three factors is scored, for example between 1 and 5, and the product of the outcomes is calculated. The resulting number is called the Risk Priority Number (RPN). The RPN is a relative number. It is a way to identify the principal risks of the process and the main topics of validation.
-
An example of a process step with a relatively low risk is the use of water for injections (WFI). As a possible failure WFI with a too high bioburden is considered. The severity is scored as 2 (bacterial filtration and terminal sterilisation of the finished product), the probability of occurrence as 1 (WFI is continuously kept at a temperature of above 80 °C and circulated), and the risk of non-detection as 3 (continuous monitoring of temperature and conductivity, regular determination of the bioburden), and RPN = 2 × 1 × 3 = 6.
-
An example of a process step with a relatively high risk is the incorrect loading of the steriliser. Here the severity is 5 (insufficient heat penetration in certain units), the probability of occurrence is 2 (a loading instruction is in place) and the risk of non-detection 3 (only one person is responsible for loading and unloading), so, RPN = 2 × 3 × 5 = 30. This process step needs more attention than the other example.
32.14.2 Process Validation in Practice
Process validation is basically a facility-based activity specific for each product or group of products [12, 13]. The basis for validation of a preparation process consists of the qualification or validation of the contributing parts of that process:
-
Building-related installations
-
Equipment
-
Utilities
-
Automated systems
-
Process validation of unit-operations
-
Cleaning methods
-
Analytical methods
-
Last but not least: personnel
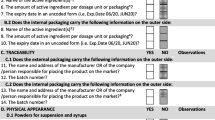
Figure 32.1 shows the relationship between process validation and qualification of equipment, computerized systems and personnel, and the requirements set based on the product specifications.
It is essential that relevant documentation is up to date and accessible. If data from Product Quality Review (PQR, see Chap. 35) and stability testing are available, they should be evaluated in order to identify any critical aspect of the processes. If not available, related quality indicators, such as test results, deviations and complaints should be evaluated.
In process validation, it is important to perform the necessary steps in the correct order (see Sect. 32.11), which can make this a complex activity. Later in this section the validation of the process ‘preparing injectables’ is elaborated.
When all components of a preparation process have been qualified or validated separately, the largest part of the process validation is complete. The prerequisites are described in an instruction including test plans. Usually, process validation includes preparation of three consecutive batches with extended sampling. Acceptance criteria typically include: no OOS, no OOT and all critical IPC’s within specified limits. Samples may be collected from critical control points during the manufacture. However, when unit operations have been validated, often only samples of the finished product (after packaging and labelling) are tested. A conclusion on the preparation process as a whole is reported in a validation report, which has to be approved by the heads of Production, QC and QA and afterwards will be the basis for future change control regarding the process.
Due to the large amount of products in a (hospital) pharmacy, validation of the preparation process for each product is not feasible. Products may be validated in groups if the production process is standardised, for example, when performing media fills to simulate and validate aseptic handling (see Chap. 31). Another example is the validation of a mixing process by using an ingredient with poor mixing properties. This is called a worst-case scenario. For each product, it must be decided whether the general process validation is applicable and this has to be recorded in the product dossier.
The validation master plan specifies which processes have to be validated and which priorities have been set (see Sect. 32.11).
Processes with a high degree of reproducibility, for example filling injection liquids in ampoules with a machine, are generally easier to validate than processes with many manual steps or stages, such as mixing a semisolid dermatological preparation manually in a mortar, or the small-scale preparation of capsules. For processes with many manual steps the knowledge and skills of the technician plays a crucial role, and therefore emphasis should be placed on the qualification of personnel and the execution of in-process controls. These checks give essential information about the accuracy of that step or the process up to that point.
Preferably, process validation is carried out prospectively. The process is carried out an agreed number of times (often three) and is taken into use only after a positive evaluation.
As an example, the process of the preparation of parenteral solutions in ampoules and its validation are elaborated. In Table 32.2, the process from weighing the ingredients to sterilisation of the ampoules is displayed stepwise. During the validation of this process there is a relationship with the following “external” factors that need to be qualified or calibrated:
-
Premises (air control, microbiological monitoring)
-
Water production
-
Balances
-
pH meter
-
Oxygen meter
-
Filter integrity testing equipment
In the past, retrospective validation (evaluating and assessing data from the past) was also performed. In the latest version of GMP annex 15 retrospective validation is no longer considered an acceptable approach. Concurrent validation may be executed, when a risk assessment reveals no major risks (See Sect. 32.10.2).
The conclusion of a process validation is based on the measured quality of all process components studied. Revalidation is indicated if significant changes in the process are introduced. The change control procedure provides for this. The validation report should contain a recommendation on the maximum period for revalidation of the process. This is important, because the impact of small or creeping changes on the quality of the process is only visible in the course of time. An example of a creeping change is a decrease in the working discipline that can occur with changes in personnel. During revalidation it is noted whether there have been changes in (the way of execution of) one of the process steps, for example in response to recommendations in the initial validation report. Also handling of deviations and reported complaints about products have to be addressed.
The design of the revalidation process largely follows that of the initial process validation. However, if no significant changes have occurred and evaluation of data does not indicate the presence of OOT, revalidation may be limited to paperwork.
32.14.3 Extemporaneous Preparations
The preparation instruction of a standardised preparation is validated beforehand. For non-standardised preparations this is not the case, and therefore it is recommended to validate the preparation template of the relevant dosage forms. The validation can be carried out by choosing a model preparation for each combination of dosage form and preparation method. It is not necessary to prepare the model preparation in daily practice. An example is the validation of the manual preparation of suspension suppositories. Suppositories with acetylsalicylic acid 100 mg can serve as a model preparation, because the uniform distribution of the active ingredient in this product is difficult (see Chap. 19). By scheduling the model preparations in a periodic cycle, this validation can be linked to the continuous qualification of personnel.
In addition, it is useful to analyse individual preparations from daily practice at a fixed frequency, for example by preparation of an excess.
A practical approach for the validation of non-standardised extemporaneous preparations may be:
-
List all non-standardised extemporaneous preparations that have been carried out in a sufficiently long period.
-
Group them according to their dosage form.
-
Per dosage form: list all applied methods of preparation (such as capsule filling after dry mixing or using the solvent method).
-
Specify all utensils used.
-
Determine important factors for risk assessment: high frequency of preparation, critical preparation method (e.g. dispersing), critical quality requirement (e.g. content uniformity).
-
Based on the combination of dosage form/preparation methods/utensils and on risk assessment, decide on the method and frequency of validation.
-
Decide which validations have to be executed in general and which validations have to be carried out operator-specific.
Parameters to be analysed (this list is intended as a guideline):
-
Capsules: content, uniformity of weight, content uniformity, appearance, disintegration time, dissolution rate.
-
Cutaneous preparations: content, homogeneity, appearance, particle size, chemical purity, microbial purity.
-
Solutions: content, appearance, homogeneity (especially with viscous solvents), chemical purity, microbial purity.
-
Suppositories: content, mean weight, content uniformity, appearance, microbial purity.
-
Suspensions: content, resuspendability, homogeneity, appearance, particle size.
How to choose model preparations:
-
Active ingredient should be rather troublesome to process but does not have to be relevant to daily practice (for instance acetylsalicylic acid in suppositories; hydrocortisone acetate to be dispersed in a cream base; salicylic acid to be dispersed in white soft paraffin).
-
Analysis should be feasible and preferably easy to perform.
How to sample:
-
Define the sample size. Generally 1 sample is sufficient for homogeneous preparations and 6 for divided dosage forms.
-
Define the sampling method, for instance:
-
Capsules: per filled portion 3 from the corners and 3 from the center
-
Cutaneous preparations: 6 spread across the batch
-
Solutions: 1 or 2 random samples
-
Suppositories poured in series: first and last one plus 4 in between
-
Suspensions: take 2–3 samples after shaking, spread across the batch
-
32.15 Qualification of Premises, Installations, Equipment and Automated Systems
See also Chap. 27. Building-related installations (including utilities), manufacturing equipment and automated systems have to be qualified for use according to predetermined specifications. For the qualification of equipment and installations specific guidelines are provided in annex 15 of the GMP. Annex 11 of the GMP states that computerised systems should be validated [14, 15]. Detailed instructions for the validation of computer systems can be found in the Good Automated Manufacturing Practice Guide for Validation of Automated Systems in Pharmaceutical Manufacture (GAMP) [16]. This guidance has been issued by the International Society for Pharmaceutical Engineering.
When, for example, a new machine is purchased, the following order of the qualification process can be used, although other terminology may also be used:
-
Determine user and regulatory requirements for the intended use of the machine (User Requirements Specification, URS).
-
Draft functional and technical requirements (Functional Requirements Specification, FRS and Technical Requirements Specification, TRS).
-
Usually the previous two steps are accompanied by a risk assessment to determine which requirements are mandatory and which are nice to have.
-
Qualify the design (custom-made) or justify the purchase (off the shelf) (Design Qualification, DQ).
-
Carry out a factory acceptance test (FAT) and a site acceptance test (SAT), if applicable.
-
Perform the installation qualification (IQ).
-
Perform the operational qualification (OQ).
-
Perform the performance qualification (PQ).
Depending on the associated risk, some of the above mentioned steps may be skipped, combined or extended.
The user lists the (legislative) requirements and his wishes regarding the equipment in the URS. Then he tries to find a supplier who can deliver a machine or installation that meets the URS. It is wise to include the URS in the agreement with the supplier to avoid discussions after delivery. This also gives the option to defer part of the payment until all requirements have been met.
After the URS the FRS has to be drafted. The FRS results from the translation of the wishes of the user (what should it be able to do?) to the functionality and design of a device or installation (how are the requirements met?). The functional requirements describe what the equipment should be able to do, what the dimensions should be and which materials should be used. Sometimes technical requirements are laid down in a separate document: the TRS. Based on these specifications a vendor may then design the machine or installation. The more carefully the user prepares the URS and FRS, the better the quality of the next steps. Depending on the situation, the TRS and FRS may be prepared in cooperation with the supplier.
The next step is the Design Qualification (DQ). In this document the purchase is justified and the design, including drawings and documentation, of custom-made equipment is reviewed and approved. It is important to prepare the first version of the URS before agreement with the supplier and to finalise it in connection with the DQ.
For very large and expensive projects it is worthwhile including a FAT. If possible, staff from the pharmacy should participate in the FAT in order to become familiar with the equipment and to detect failures as soon as possible, potentially saving a lot of time and money. Usually, after delivery a SAT is performed to check adequate correction of the deviations identified during the FAT and to detect any damage caused during transport. The conclusion of the SAT may have major legal impact as handover of the equipment may be linked to finalisation of this step. The term commissioning is sometimes used for this formal step.
After delivery of the equipment the IQ is performed. This is a check to see whether the equipment is delivered and installed according to the specifications. Also, a check on the completeness of the documentation is performed, including operating, maintenance and cleaning instructions and calibration documents. It should also include technical drawings (‘as-built’ drawings) and diagrams (Piping & Instrumentation Diagrams (P & IDs)).
During the OQ the functioning of the equipment is tested and measured. The aim is to show that the system works according to pre-established specifications and acceptance criteria. The OQ includes tests for the system operation, calibration, operation and handling of alarms and the simulation of emergency situations. Also local operating procedures and a maintenance plan have to be drafted at this stage.
The IQ- and OQ-tests may be performed by, or in cooperation with the supplier; the formal qualification is the responsibility of the user.
The final step in the validation process is the PQ, which is the verification of the suitability of the installation for the intended purpose in the production process. Often quality control of the finished product is part of carrying out the PQ. An example is the measurement of the homogeneity of a mixture that is produced by a mixing machine. The PQ is performed by the user. When all the above-mentioned steps are completed satisfactorily, the equipment is qualified and may be used in the preparation process. Alternatively, the equipment can be provisionally released for use after finishing the OQ. The final release takes place after completing the PQ (concurrent qualification).
The different phases of the qualification or validation process can be shown in a V-model (Fig. 32.2), which shows the mutual relationships. Each step in the validation process (right arm of the diagram) refers to a step prior to delivery (left arm). This model was developed in the context of software validation, but may well be applied to the qualification of equipment, installations and even a cleanroom.
32.16 Cleaning
32.16.1 Good Cleaning Practice and Cleaning Validation
Proper cleaning of premises, equipment and utensils is essential to prevent microbiological and cross-contamination (see Sect. 32.3). The purpose of cleaning validation is to demonstrate that the correct cleaning processes are applied, that the cleaning frequency is adequate and that cleaning leads to the desired result, namely the prevention of (cross-)contamination during preparation [9, 17]. In general, cleaning validation is necessary before use of new or changed facilities or equipment, in the context of corrective and preventive actions (CAPA, see Chap. 35) after non-conformities or monitoring trends and when cleaning procedures or materials are changed.
Cleaning validation starts with describing all cleaning activities and to standardise these when possible. The influence of the human factor in cleaning processes cannot be overestimated. Cleaning activities can be divided into cleaning of premises, equipment and utensils. Cleaning may be performed manually (e.g. by using a brush) or mechanically (e.g. in a washing machine). Objects may be cleaned in another place (e.g. in a sink in another room) or in place (e.g. a large production vessel). The risks differ per method and the cleaning validation should take this into account.
32.16.2 Premises, Workbenches and Worktops
Own staff may clean the premises, workbenches and worktops, but the cleaning may be outsourced as well. In both cases, it is important to agree on what has to be cleaned and how often, and which tools and products have to be used. Supervision, control forms and logbooks are useful to determine whether these activities are performed according to the agreements. In case of outsourcing, it is necessary to agree on a service level agreement (see Chap. 35). It is also important that only people with proven knowledge of hygiene are allowed to perform cleaning activities.
Cleaning and disinfection of qualified areas, such as clean rooms, require intensive training, an appropriate attitude and a thoughtful system. This is necessary to ensure that the persons carrying out the cleaning do not cause more harm than good.
Wet cleaning may constitute a problem with the moisture regulation. As the walls, floors and ceilings of clean rooms are basically airtight, introduced moisture has to be removed through condensation in the Heating Ventilation Air Conditioning (HVAC) system (see Chap. 27). This not only takes a lot of energy, but also lasts too long. This poses a risk, because a room that is too humid promotes the growth of microorganisms.
Cleaning with a clean room vacuum cleaner (vacuum cleaner fitted with a HEPA filter) is preferred to remove dust. Dust from prior activities that is not removed through the HVAC system will accumulate, mainly on the floor. For removing non-dusty dirt (e.g. spilled and dried liquids) damp cleaning is suitable, preferably with disposable mops on wipers. The required frequency of cleaning may be different for floors, walls, counter tops and ceilings. Affected places such as door handles, push buttons and switches must be given explicit attention. For the cleaning of small surfaces disposable low-dust wipes may be used. Microfibre towels are suitable as well; they can be reused after washing at a minimum of 70 °C and centrifuging at 1000 rpm. The advantage of these towels is cleaning without moisture and detergents. The disadvantage is that washing and reuse poses a risk of contamination.
Cleaning materials should not be moved from a less clean environment to a cleaner room. The use of dedicated cleaning materials for each manufacturing area is preferred.
There is an important difference between cleaning and disinfection. Cleaning is removing dirt and other unwanted substances. Disinfection is aimed at reducing germs on surfaces (e.g. worktops) and is effective only when the surfaces are clean, since the effect of disinfectants can be reduced by dirt (see also Chap. 31). In practice, the right order is: first cleaning and then, where required (for example, the worktop of a laminar flow cabinet), disinfection.
Monitoring of the cleaning is performed by visual inspection (recorded in the logbook), but also by microbiological monitoring and wipe tests. Microbiological monitoring provides insight into the microbiological contamination of critical points in rooms. Since microorganisms are usually attached to dust particles, microbiological monitoring also gives an indication of the particle contamination. By sampling before and after cleaning the quality of the cleaning can be established. In high risk processes, e.g. preparation of chemotherapy or radiopharmaceuticals, periodic surface sampling (wipe tests) is performed to check the cleaning and to ensure personnel safety.
The validation of the cleaning of rooms is required for surfaces that may influence the quality of the product. It may be executed by checking whether all scheduled cleaning activities have been performed in accordance with the agreements and whether correct actions have been taken in response to any deviations. Furthermore, the results of the microbiological monitoring, wipe testing and validation of air quality provide quantitative information on the quality of the cleaning processes. By setting limits, conclusions can be drawn about the effectiveness of cleaning activities.
32.16.3 Equipment
The operating instructions of equipment provide information about the correct way of cleaning. After cleaning, every machine or device must be visually checked for residues of the product or detergent (if applicable). The spots of the equipment to be visually checked must be well defined, based upon experiments with, for instance, contamination with a model substance (see below). However, visual inspection is not sufficient, because not all residues are visible and some equipment cannot be inspected entirely.
Cleaning validation is required only for surfaces of reusable equipment that come into direct contact with different products. When using dedicated equipment only verification of the cleaning process is necessary. Attention should be paid to so-called hot spots: difficult-to-clean locations, which would lead to (cross-)contamination if improperly cleaned.
Sampling should be carried out through wipe tests and by collecting flushing liquid. Hot spots can be detected by UV light when a model substance (e.g. riboflavin) is used in the test procedure. The suitability of the sampling procedure has to be proven. In the analysis of rinse water, it is important that the cleaning has been carried out in the correct manner. When cleaning a production vessel, rinsing the inside of the lid could be forgotten. If the rinse water is clean nothing can be concluded about the cleanliness of the entire production vessel. In comparison: in a kitchen one will not judge the cleanliness of a pan solely based on the clarity of the dishwater. Because a wipe test is conclusive about local cleaning, both methods should be carried out [9, 18].
For some equipment microbiological purity is of importance for product quality. This equipment must be designed and constructed ‘sanitary’. This means that all parts that may come into contact with the product must be cleanable and that no moisture remains after cleaning. Chemical cleaning (often an alkaline detergent, followed by an acid agent for neutralising) combined with rinsing leads to a strong bacterial reduction. Microbiological controls, including the determination of total bacterial count in a subsequent preparation, provide information about the cleaning procedure.
For the validation of the cleaning of equipment existing products or model substances may be used. When validation with a model substance is performed, its solubility should be similar to the least soluble substance processed with this equipment, since this is the most difficult to remove (worst-case approach). The nature of the model substance(s) (organic, inorganic, or both) is substantiated for all equipment and preparation methods. Because the pH may affect the solubility of active ingredients and excipients this must be taken into account in the design of the flushing procedure and the choice of the model substance.
Furthermore, the analytical methods to assess the rinse and wipe samples have to be validated. Also, the recovery of the test substance during sampling has to be established.
The amount of an active ingredient that may be present in the next product must meet established criteria, such as the strictest of the following three conditions [9]:
-
Up to 0.1% of the normal dose of each product may be detectable in the maximum dose of the next product.
-
Up to 10 ppm of each product may be detectable in the next product.
-
No residual should be visually detectable.
To assess acceptance criteria for cleaning validation, limits for the maximum allowable carryover of product residues must be calculated, based on the pharmacological or toxicological properties of the substances studied and their permitted daily exposure (see Chap. 26). A risk assessment may be useful to support choices and decisions.
If allergens, steroids or cytotoxic drugs are prepared, these substances must not be detectable above the detection limit of the analytical method used [9].
The detection limit of model substances should be low enough to meet the established requirements.
Finally, the dirty hold time and the clean hold time have to be established [18]. When a vessel is not cleaned immediately after use, the remaining fluid may dry out so the vessel may not be cleanable using the normal procedure. The dirty hold time is the time for the cleaning to be completed to be sure that the validated cleaning procedure is still effective. The clean hold time is the period during which the equipment may be considered clean after carrying out cleaning and sanitisation (if applicable) and may be safely used for the next production process.
32.16.4 Utensils and Clothing
Tools or utensils used for manufacturing include glassware, mortars and spoons. Because the cleanliness of these items and that of clothing and clogs directly or indirectly may influence the quality of the product, the cleaning of utensils and clothing has to be validated.
Utensils and clogs can be cleaned and disinfected manually or mechanically. A manual cleaning process is difficult to validate. Only the final result can be assessed by visual inspection and by analysis of random wipe and rinse samples. To avoid unnecessary validation activities, the use of disposables should be considered.
Mechanical cleaning processes are more reproducible and therefore easier to validate. A disinfection step may be introduced by increasing the temperature to above 80 °C by the end of the cleaning phase, so the cleaned articles are germ-free after the procedure. The process can be monitored by measuring the temperature, the consumption of detergents and the conductivity of the process water. In addition, tools are available that can demonstrate the cleaning effectiveness of the process (e.g. Tosi® test).
The Tosi® test is a validated cleaning indicator, which is made up of a grooved stainless steel plate on which a strong adhesive red colored substance has been applied. This plate is mounted at a very narrow angle in a transparent plastic container. At the end of the cleaning process, the plate must be fully free of the red test substance. If not, the cleaning process has been insufficient.
Random visual inspection and analytical and microbiological checks of the final result may yield additional substantiation of the quality of the cleaning and disinfection process. Separate attention must be paid to the drying and storage of utensils, in order to prevent recontamination.
Garments can be thrown away after use (disposable clean room overalls), or reused after cleaning. If clothes are used that are cleaned in house, validation of this process will not be easy. Therefore, the use of clothing cleaned and packaged by specialised and certified companies applying validated processes is preferred.
Questions
-
1.
Mention measures to lower the probability of (cross-)contamination and mix-ups.
-
2.
Which types of ipc’s do you know and what are the goals of their execution?
-
3.
What is the purpose of yield and label reconciliation?
-
4.
Mention checks to include in batch documentation review.
-
5.
Explain when parametric release may be performed.
-
6.
Mention elements of a validation master plan.
-
7.
Explain the difference between qualification and validation and their relationship.
-
8.
Describe the different phases of qualification and validation during a V-diagram.
-
9.
Describe which aspects are important in cleaning validation.
References
European Commission (2014) Eudralex volume 4 EU guidelines to good manufacturing practice medicinal products for human and veterinary use – Chapter 5: Production. pp 1–12. https://ec.europa.eu/health/sites/default/files/files/eudralex/vol-4/chapter_5.pdf
European Commission (2014) Eudralex volume 4 EU guidelines to good manufacturing practice medicinal products for human and veterinary use – Chapter 6: Quality control. pp 1–8. https://ec.europa.eu/health/sites/default/files/files/eudralex/vol-4/2014-11_vol4_chapter_6.pdf
European Commission (2015) Eudralex volume 4 EU guidelines to good manufacturing practice medicinal products for human and veterinary use – Annex 15: Qualification and validation. pp 1–16. https://ec.europa.eu/health/sites/default/files/files/eudralex/vol-4/2015-10_annex15.pdf
Pharmaceutical Inspection Convention Pharmaceutical Inspection Co-operation Scheme (2014) PIC/S Guide to good practices for the preparation of medicinal products in healthcare establishments. PE 010-4. pp 1–56. https://picscheme.org/docview/3443
Council of Europe (2011) Resolution CM/ResAP(2011)1 on quality and safety requirements for medicinal products prepared in pharmacies for the special needs of patients. https://www.edqm.eu/sites/default/files/resolution_cm_resap_2011_1.pdf
Bouwman Y, Andersen LM (2012) GMP and preparation in hospital pharmacies. Eur J Hosp Pharm Sci Pract 19(5):469–473
European Commission (2005) Eudralex volume 4 EU guidelines to good manufacturing practice medicinal products for human and veterinary use - Annex 19: Reference and Retention Samples. pp 1–5. https://ec.europa.eu/health/sites/default/files/files/eudralex/vol-4/pdfs-en/2005_12_14_annex19_en.pdf
European Commission (2018) Eudralex volume 4 EU guidelines to good manufacturing practice medicinal products for human and veterinary use – Annex 17: Real Time Release Testing and Parametric Release. pp 1–5. https://ec.europa.eu/health/sites/default/files/files/eudralex/vol-4/pdfs-en/2018_annex17_en.pdf
Pharmaceutical Inspection Convention Pharmaceutical Inspection Co-operation Scheme (2007) Recommendations on validation master plan – installation and operational qualification – non-sterile process validation – cleaning validation. PI 006-3. pp 1–26. https://picscheme.org/docview/3447
European Medicines Agency (2015) ICH Guideline on Quality Risk Management, pp 1–20. https://www.ema.europa.eu/en/documents/scientific-guideline/international-conference-harmonisation-technical-requirements-registration-pharmaceuticals-human-use_en-3.pdf
European Commission (2012) Eudralex volume 4 EU guidelines to good manufacturing practice medicinal products for human and veterinary use – Chapter 7: Outsourced Activities. pp 1–4. https://ec.europa.eu/health/sites/default/files/files/eudralex/vol-4/vol4-chap7_2012-06_en.pdf
US Food and Drug Administration (2011) Process validation: general principles and practices. pp 1–22. https://www.fda.gov/files/drugs/published/Process-Validation%2D%2DGeneral-Principles-and-Practices.pdf
European Medicines Agency (2016) Guideline on process validation for finished products. pp 1–15. https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-process-validation-finished-products-information-data-be-provided-regulatory-submissions_en.pdf
European Commission (2011) Eudralex volume 4 EU guidelines to good manufacturing practice medicinal products for human and veterinary use – Annex 11: Computerised systems. pp 1–5. https://ec.europa.eu/health/sites/default/files/files/eudralex/vol-4/annex11_01-2011_en.pdf
Pharmaceutical Inspection Convention Pharmaceutical Inspection Co-operation Scheme (2007) Good practices for computerised systems in regulated “GxP” environments. PI 011-3. pp. 1–54. https://picscheme.org/docview/3444
International Society for Pharmaceutical Engineering. Good Automated Manufacturing Practice (GAMP) 5 Guide. 2008
European Medicines Agency (2014) Guideline on setting health based exposure limits for use in risk identification in the manufacture of different medicinal products in sherad facilities. pp 1–11. https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-setting-health-based-exposure-limits-use-risk-identification-manufacture-different_en.pdf
International Society for Pharmaceutical Engineering. Cleaning Validation Lifecycle – Application, Methods, & Controls 2020, pp 1-236.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Lange, R., Schnor, T. (2023). Product Quality, Quality Control and Validation. In: Le Brun, P., Crauste-Manciet, S., Krämer, I., Smith, J., Woerdenbag, H. (eds) Practical Pharmaceutics. Springer, Cham. https://doi.org/10.1007/978-3-031-20298-8_32
Download citation
DOI: https://doi.org/10.1007/978-3-031-20298-8_32
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-20297-1
Online ISBN: 978-3-031-20298-8
eBook Packages: MedicineMedicine (R0)