Abstract
Patient autonomy is the foundational moral principle of healthcare. In this chapter, I review how autonomy has been conceptualized in the medical field and compare that with understandings of autonomy discussed in design. I argue that patient autonomy in healthcare has mainly been understood as negative freedom—independence from the interference of others, especially medical paternalism. Therefore, patient autonomy has been conceptualized as decision-making and has been applied to practice as a procedural means to cure rather than an end in itself. In contrast, user autonomy in design highlights positive freedom—the elevated state of one’s ability to govern one’s own life according to an internal will. Therefore, autonomy in design has been construed more broadly as a concept that encompasses thoughts, decisions, and actions, and has been seen as an end in itself. The collaboration of healthcare professionals and designers allows for productive opportunities to holistically support patients and their caregivers, as this collaboration brings together autonomy as means and autonomy as ends. I conclude the chapter by proposing that the study of autonomy as a guiding principle is essential in expanding healthcare service design to consider diverse agents.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
1 Introduction
Plato’s Phaedrus begins with a symbolic setting: Socrates and Phaedrus walk outside the Athenian Wall into the wilderness to search for a suitable place for their conversation. They choose a holy place known as the location where Boreas, the God of the North Wind, carried the Athenian girl Orithyia away. Plato explains that in reality, Orithyia must have fallen from a cliff, pushed by a strong wind. Here, Plato is retelling the myth in order to reposition it as an allegory to foreshadow his later discussion about the flight and fall of the soul. In order to do this, he also adds a divine character, Pharmacia, as the playmate of Orithyia. Pharmacia is a nymph who is known to have the power to transform well water into poison or medicine, as her name, “pharmacy,” indicates.
In other words, Plato is introducing the problem of a soul (Orithyia) that was experiencing a transformation, potentially related to health, as indicated by the allegory of Pharmacia, but ended up “falling” due to a conflict between inner will and external force. The significance of this story is that it introduces the most fundamental principle in medical ethics—autonomy. The rest of the Phaedrus is a discussion about the soul, a rather antique yet holistic interpretation of what constitutes a person’s humanity. When the “horse” of action and the “horse” of passion are balanced via the driving factor of human reason, the “chariot” of the soul is liberated from the external necessity of the material world, represented by gravity, and gains autonomy.
Almost 2500 years have passed since Plato presumably composed the Phaedrus and described autonomy as the flight of free will toward the ethical ideal. Many more interpretations of autonomy have since been proposed, such as Rousseau’s citizen self-governance (1762/2018, n.d.), Kant’s self-imposed universal moral law (1785/1998, n.d.), and Nietzsche (1883/2008, n.d.)’s mastery, which balances self-love and self-respect. Psychological studies, such as self-determination theory (Deci & Ryan, 2008, pp. 182–185) and locus of control (Rotter, 1966, pp. 1–28), reveal that autonomy is essential for well-being, providing the utilitarian foundation for the importance of autonomy in healthcare. Today, healthcare is one of the areas in which research on the concept of autonomy is most active. Autonomy is one of the four pillars of medical ethics (Beauchamp & Childress, 1979, pp. 60–62) and is broadly accepted as a central value in Western medicine (Varelius, 2006, p. 377). Scholars like Jennings (2016, p. 11) even argue that autonomy is the sole foundational concept in the contemporary development of bioethics.
As the collaborative opportunities among designers and healthcare professionals increase, designers need to understand autonomy as a key moral principle of medical ethics and embed it in the services they create. Medicine is transformative, as previously indicated in the allegory of Pharmacia, and so too is service design (Karpen et al., 2017, p. 391; Kim, 2021, pp. 89–90; Sangiorgi, 2011, pp. 29–40). Patients and users shape and are shaped by the practices and processes that constitute these respective fields. Therefore, nurturing autonomy is important for enhancing patient experience in healthcare service design; furthermore, exploring a human-centered perspective in design can enhance a patient-centered approach in healthcare. However, there is a dearth of research that reviews the definitions and dimensions of patient autonomy for designers.
In this chapter, I aim to examine the concept of autonomy in healthcare and design, highlighting the importance of autonomy as a grounding principle that can integrate multidisciplinary collaboration in healthcare service design. I present autonomy’s central role in medical ethics, the broadly accepted principle of patient autonomy to respect patient’s rights to make independent decisions, and the recent discussions on relational autonomy. I then introduce concepts of autonomy represented in design. Designers have emphasized the need to design products and services in a way that controls technology to properly nurture the autonomy of users.
2 Autonomy in Healthcare and Design
The Dictionary of Public Health defines autonomy as “free will; self-governing, ability of a person or a group to choose a course of action. Autonomy is a basic human right and is one of the principles of bioethics (Last, 2007, n.d.).” As indicated in this definition, many scholars agree that autonomy is closely related to the concept of freedom. In this respect, Berlin’s (1969, pp. 118–72) conception of negative liberty/freedom and positive liberty/freedom provides a useful framework for this study, which aims to compare autonomy in healthcare and design. According to Berlin (1969, p. 121), negative freedom refers to an external state without “the source of control or interference that can determine someone to do, or be.” This conception of negative freedom often serves as a basis for an understanding of autonomy as the right to make independent, uncoerced decisions as one wishes.
However, other scholars argue that not all freedom is autonomy; many philosophers suggest that autonomy includes the responsibility to use reason to self-control one’s freedom in a way that aligns with universal moral law (Rousseau, 1762/2018, n.d.; Kant, 1785/1998, n.d.; Nietzsche, 1883/2008, n.d.) In other words, respect for other agents’ autonomy is the precondition for one’s own autonomy. For example, Kant (1785/1998) theorizes that autonomy necessarily requires treating other humans as ends, not as means. Berlin’s (1969, pp. 118–72) conception of positive freedom refers to this internal autonomy—the moral ability to effectively direct one’s own life according to self-imposed rules that align with community values. Therefore, autonomy as positive freedom involves not only making independent decisions but also making good decisions, leading to the capacity to carry out actions according to one’s thoughts.
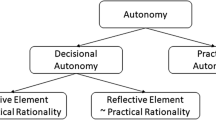
I propose that patient autonomy tends to result from negative freedom, as it provides a minimal condition for freedom from external coercion, while user autonomy is an outgrowth of positive freedom, as it seeks holistic support for actions, thoughts, and decision-making. Additionally, I present two perspectives on how autonomy is discussed in practice in the two fields of healthcare and design: autonomy as means and autonomy as ends. Generally speaking, patient autonomy in healthcare approaches autonomy as a procedural means to ensure a cure as the ends. In contrast, user autonomy in design assumes autonomy as the ends of services and products/services that provide care as the means.
2.1 Patient Autonomy in Healthcare
Today, patient autonomy, or personal autonomy, is broadly accepted as a fundamental principle in healthcare. The bioethical principle of respect for autonomy generally refers to healthcare professionals’ obligation to provide a condition for autonomy regarding the medical intervention or treatment that they will receive (Pugh, 2020, p. 298). Specifically, autonomy generally refers to respect for or protection of individuals’ self-determination (Schermer, 2002, p. 1) that is “shaped by personal preferences and choices” (Beauchamp & Childress, 1979, p. 58), as in the definition of patient autonomy as “allowing or enabling patients to make their own decisions about which healthcare interventions they will or will not receive” (Entwistle et al., 2010, p. 41). In medical practice, patient autonomy manifests itself as minimal yet concrete procedures, such as an explanation of potential risk and the magnitude of harm in regard to certain inspections, treatments, or surgeries, as well as signing forms to ensure informed consent.
Historically, recognizing patient vulnerability has been the antecedent of patients’ autonomy. The Hippocratic oath, one of the first expressions of medical ethics, reveals early concerns about protecting patients’ bodies and private information from abuse (Edelstein, 1943, n.d.). In the twentieth century, respect for autonomy (RFA) evolved as a response to unethical experiments during the Second World War and medical paternalism that can lead to an imbalance of power and information. The Nuremberg Code (1947), known as the foundation of bioethics, emphasized the essentiality of the informed and voluntary consent of human subjects. The Nuremberg Code, in turn, impacted the Declaration of Geneva (1948), the Physician’s Oath (1948), and the Belmont Report (1978), which clarified research-related ethical principles. The first of these principles was respect for persons (RFP), which includes a requirement to protect patient autonomy. Today, autonomy has become one of the most important principles, along with benevolence, nonmaleficence, and justice, in the foundational Principles of Biomedical Ethics published in 1979 (Beauchamp & Childress, 1979, n.d.).
Shaped by this historical background, contemporary medical ethics places a strong liberal emphasis on individual rights, such as protecting privacy and self-determined choices (Tauber, 2001, pp. 299–319). Beauchamp and Childress observe that “to respect autonomous agents is to acknowledge their right to hold views, make choices, and to take actions based on their values and beliefs” (Beauchamp & Childress, 1979, p. 106). Therefore, truth-telling, informed consent, and conditions that ensure uncoerced decision-making are emphasized. Beauchamp and Childress further assert that the following four points are integral to personal autonomy: (a) being free from the controlling influence of others, (b) being free from limitations that prevent meaningful choice, (c) being free from inadequate understanding, and (d) being able to freely act in accordance with a self-chosen plan. Burkhardt and Nathaniel (2002, pp. 205–32) also assert that underpinning personal autonomy is an environment that encourages independence and freedom of choice. In light of the points raised by scholars of medical ethics, there appear to be two essential conditions for personal autonomy: those of liberty (independence from controlling influences) and those of agency (capacity for intentional action).
However, there are also downsides to this strong focus on patients’ independent choice and the provision of minimal conditions to protect patients’ decisions from medical paternalism. The underlying assumption is that a generally capable individual can make autonomous decisions as long as interference is removed (Mackenzie & Stoljar, 2000, n.d.). It is often presupposed that patients are rational and are well aware of what decisions are best for their well-being. This liberal, procedural, and rather narrow interpretation of autonomy based on negative freedom becomes problematic because it can miss other complicated aspects of autonomy that often pose challenges to less-represented populations and require more active interventions (Entwistle et al., 2010, pp. 741–745).
As for an alternative, recent studies highlight the importance of relational autonomy proposed by feminist theorists. Individuals are products of their social relationships, which often limit or enhance their autonomy (Friedman, 1986, pp. 26–29). Many studies in healthcare, especially nursing and gerontology literature, argue for the need to expand the concept of patient autonomy beyond atomism and decisional autonomy regarding a specific medical situation (Perkins et al., 2012, pp. 214–215; Walker, 2000, 97–111; Lindberg et al., 2014, pp. 2208–2221). A relational view of patient autonomy provides a critical examination of conditions that can reduce autonomy and sheds light on how autonomy can be shared and assisted (Mackenzie & Stoljar, 2000, n.d.), as individuals who were traditionally seen as less capable of independence can still have the capacity for autonomy with proper support (Sherwin & Winsby, 2011, pp. 182–190). This emphasis on relational autonomy calls for the need to expand and diversify these minimal, individualistic conceptions of autonomy to a more holistic ecology of care (Lindberg et al., 2014, pp. 2208–2221). Here, design can play a key role in actively mediating not only patients and healthcare professionals but also the family and personal relationships of patients, with the help of products and services.
2.2 User Autonomy in Design
The term “patient autonomy” is seldom referenced in the field of design, but there are a few recent studies that show that this topic is an emerging theme in healthcare design. Zhu et al. (2020, pp. 230–244) propose using bioethical conditions for promoting patient autonomy as principles for designing a healthcare environment that respects the autonomy of patients. Kim et al. (2022, pp. 143–164) discuss the importance of relational autonomy in older adults’ healthcare and later-life transitions and propose utilizing autonomy as a key principle in service design. Another area in which autonomy in a healthcare context has been actively studied is assistive technology. Güldenpfennig et al.’s (2019, pp. 1–14) study on people with multiple sclerosis using assistive devices shows that design plays a central role in promoting or restricting autonomy by helping users manage factors that are closely related to their sense of autonomy, such as digital technology. The mission statement of the Active and Assisted Living (AAL) program of the European Union is to extend “the time people can live in their preferred environment by increasing their autonomy, self-confidence, and mobility.”
There are further studies that have researched the autonomy of users in the context of their relationship with technology. Friedman (1998, pp. 26–29) discusses the significance of users’ control over technology and how technology should be designed to enhance users’ lives. Littlewood (1996, pp. 427–435) proposes that the “ability (knowledge about the choices available)” and “willingness (motivation and beliefs about one’s own capabilities)” of users are important factors that promote their autonomous use of technologies. Calvo et al. (2014, pp. 37–40) propose the importance of environments and tools that promote autonomy in users’ everyday activities through personalized design that supports the psychological development of users. While these studies focus on human agents’ use of technology as tools, recent discussions on autonomy highlight the interaction between two agents—human agents and artificial intelligence (AI). Here, the focus is on the difference between automation and autonomy of technology, and how AI can support and benefit human autonomy (De Visser et al., 2018, pp. 1409–1427; Rozenblit, 1992, pp. 1–18), which is often related to ethics for responsible AI. As healthcare is a sector where new technologies are constantly adopted and adapted, these studies on human autonomy in relation to technology acquire newfound importance in healthcare service design.
Design principles and theories are other important areas in discussions on autonomy in design. For example, Friedman (1996, n.d.) proposes user autonomy as one of the key principles in her theory of value-sensitive design. She posits that designers should perceive users as autonomous agents who can best promote their own values. Davy (2015, pp. 132–148) discusses the autonomy of vulnerable individuals as an important concept in inclusive design, in which there is a need to expand the concept of autonomy to include diverse people who deviate from the standardized images of users. Millar (2015, pp. 47–55) argues that a designed thing serves as a moral proxy in a designer–technology–user trio, as it acts on behalf of a person. He proposes that designers should pay attention to avoiding paternalism and respecting user autonomy, drawing upon the conception of human moral proxies in healthcare. Scholars in the 2014 Conference on Human Factors in Computing Systems (Calvo et al., 2014, 37–40) workshop collectively organized different conceptions of autonomy as principles in design as follows: (a) enhancing users’ sense of control over technology; (b) supporting independence in users’ daily lives; (c) empowering users to create their own technology, which makes them more autonomous; and (d) fostering autonomy as an overarching characteristic of psychological development.
Overall, the conceptions of user autonomy in design are different from the conceptions of patient autonomy in several aspects. User autonomy in design illuminates broader, general senses of positive freedom that coordinate one’s action to align with one’s belief, preferred situation, or moral value. Therefore, I argue that the conception of autonomy in design is broader than patient autonomy—it encompasses contexts such as socio-cultural situations and human connections, thought, identity, and autonomous action, which expands the relatively narrow interpretation of patient autonomy simply as decision-making. Therefore, autonomy in design is considered an end in itself—designers create products and services that are geared toward solving specific problems, but this is, in the end, to enhance the autonomy of those who use it. This self-justifying nature of user autonomy is in contrast to the procedural nature of patient autonomy.
However, I argue that patient autonomy and user autonomy are not necessarily diametrically opposed. Rather, these concepts complement each other by connecting two different opportunities of healthcare for the patient-user: the point of cure in a hospital setting, and the points of care throughout patients’ lives where the patient and their family and diverse service experts manage their health. Procedural autonomy as means is more practical in the former case, while the latter case should aim for a broader sense of self-justifying autonomy as ends to position the patient’s life at the center of care. By providing practical, objective, and efficient guidelines in the form of informed consent, medical professionals can ensure that they provide minimal, but concrete and essential, conditions that allow for the decisional autonomy of patients. From the patient’s perspective, they have to manage their own health in their everyday lives, and medical treatment is just one aspect of living autonomously. Designers can intervene with products and services to support patient-users’ autonomy in a holistic way and enhance their relational autonomy by actively connecting them with other agents of care.
3 Case Study: Designing for the Health Autonomy of Older Adults
Managing one’s own health is an important aspect of autonomy and requires design intervention, as this activity needs holistic support, such as access to health information, health literacy, and proper communication among people who are important to a patient’s life. To demonstrate how different conceptions of autonomy can be applied to healthcare design, I introduce a service design project titled “Designing for the Health Autonomy of Older Adults” as a case study. In this academic project, our research team interviewed 15 adults aged 65 years and older and 5 caregivers at three local senior homes (The Hearth at Olmsted Green, the Grove at Olmsted Green, and St. Helena’s House in Boston) and one senior community center (Boston Centers for Youth and Families Grove Hall Senior Center) in Greater Boston Area, Massachusetts, USA, to learn about the factors that nurture or thwart seniors’ health autonomy. The participants included 17 females and 3 males; 10 were African American, 3 were Caucasian, 2 were Asian, and 5 were of other races, including those who identified as mixed race. All the participants suffered from at least one chronic disease and were in need of home-based self-care.
The outcome of this research reveals that there is a need to support autonomy both as means and ends to comprehensively support older patients as they navigate their everyday lives. Our participants expressed that they wanted information to enhance their decisions in healthcare not only when they found themselves in medical treatment situations but also in other situations in which they are advocating for their health. These could include conversations about disease prevention, health insurance negotiations, and other encounters with healthcare professionals, such as making appointments (see Fig. 1). At the same time, they wanted this information personalized so that it was relevant to their everyday needs, rather than in a form of abstract knowledge that is less applicable to their specific needs and action goals. Said information could help them carry out practical tasks, which would enhance their sense of autonomy in their lives. The participants also strongly preferred plans that privilege relational autonomy by involving their family members, friends, senior-home caregivers, public service workers, and healthcare professionals, such as primary-care physicians, nurses, and pharmacists whom they trust.
According to these findings, the team initially generated a service concept that utilizes storytelling and games to move the foci of health information from topic-based nouns (e.g., broken hipbone) to scenario-based actions (e.g., what do I do if I fall and cannot stand up?) that are contextualized in seniors’ everyday lives and tasks. These games included themes such as action (making appointments and visiting hospitals using mobile apps), decision (creating protocols for emergency situations), and thought (deliberating in advance on end-of-life care). However, the COVID-19 pandemic mandated that people quarantine and practice social distancing, which forced our team to shift the focus of our research to prioritizing the urgent needs of the isolated residents in local senior homes. Therefore, as the next phase of the health autonomy project, we collaborated with Middlesex Community College’s nursing students to provide basic health checkups and disseminate health information to isolated older adults in our partnering organization, the Peter Sanborn Center for Senior Living in Reading, Massachusetts (see Fig. 2).
Procedural support (autonomy as means) for decisional autonomy gained key significance in this extreme situation. When conducting the research, we followed the Institutional Review Board (IRB) protocol thoroughly. The IRB approval process to ensure research participants’ informed consent is one of the methods that designers have adopted from biomedical research, which systematically embeds procedural autonomy in the design process. However, the situation senior residents faced, in which they were isolated in their rooms and only a limited number of service workers had access to the senior homes, created additional challenges. A more difficult and particular factor was our participants’ low technology literacy. We were unable to use virtual platforms, such as Zoom, for our research. Therefore, the assistance of senior-home workers was essential for promoting procedural autonomy. Instead of interviewing the participants in person or gathering opinions in focus group sessions, we distributed multiple surveys, newsletters, and flyers via senior-home workers to ensure the participation and informed procedural autonomy of the senior residents.
As the COVID-19 situation improved, we gained permission from the management for nursing students to enter the senior homes and perform basic health checkups on senior residents who wanted the service. Therefore, the senior residents had to make a decision: whether to minimize their exposure to COVID-19 by not participating in this event or to participate in the health checkup event to alleviate the impact of not being able to visit hospitals regularly during the pandemic. In order to create an environment to optimize the residents’ decisional autonomy, the team thoroughly informed them about the face-to-face meeting and health checkup protocols. We also provided the residents with details of the students’ action protocols that they would be following to protect the seniors from potential exposure to the COVID-19 virus. In order to deliver all this information, we also created digital journals, information flyers, and a service blueprint that outlined the face-to-face assessment procedures. Senior-home workers also communicated with the residents to explain the procedures and conducted surveys so that the service design could reflect the opinions and preferences of the senior residents. For example, the surveys showed that the majority of senior residents preferred personalized health checkups in their rooms rather than collective outdoor events in which residents undergo checkups together. Therefore, we designed the service accordingly such that nursing students would visit residents’ rooms wearing personal protective equipment.
During this process, we also intended to utilize and nurture relational autonomy. Studies show that older adults’ autonomy is characterized by its emphasis on connectedness rather than independence, highlighting the importance of relational autonomy (Kim et al., 2022, pp. 143–164). Many design solutions today aim to provide services that individuals can use independently on their personal devices. However, we learned that older adults who are not familiar with technology generally gain a better sense of control when communicating with real people instead of using digital interfaces. Therefore, throughout the pandemic, senior residents’ sense of relational autonomy has been significantly impacted because of their isolation from human interaction and the digitalization of services. Our research provided the conditions for senior residents to communicate frequently with senior-home staff members, as we sought to fortify our participants’ procedural autonomy. Additionally, this project helped the senior residents become more connected to healthcare networks and the local community via interactions with nursing students. As a result of the increased communication, the residents’ relational autonomy has also been improved.
In addition to the health checkup, we created a series of wellness lectures delivered by nursing students. The goal of this lecture series is to nurture the foundational capability for autonomous action—in this case, we interpreted autonomy as an end in itself as the outcome of this project. Each week, two nursing students selected various health-related topics and conducted hour-long lectures for 10–15 participants. These lectures were provided virtually via Zoom in order to allow for social distancing. Therefore, the team first had to increase the technology literacy of older adults. The team helped senior residents to adapt to virtual meetings by designing how-to-join flyers, troubleshooting questionnaires, guidelines for senior home-owned devices that could be rented, and information cards that the participants kept next to their phones. By improving the residents’ technology literacy, we not only wanted to engage the participants in virtual lectures but also encourage them to overcome fears of new technologies and increase their action capacity by teaching them to use digital services. Contemporary healthcare services are increasingly incorporating digital technology; therefore, digital literacy education is fundamental to a patient’s actional autonomy, as they can manage their own well-being and pursue healthier lives.
In addition, we designed the lectures such that senior residents were continually engaged. Thus, we drew upon research we had conducted prior to the COVID-19 pandemic regarding the creation of personalized, thematic games designed to enhance seniors’ health autonomy. These games are personalized in that they account for each resident’s unique needs and the particular everyday situations in which they find themselves. The design ideas that we embedded in the wellness lectures included a hybrid bingo game, conversational objects, and goodie bags with instructions and tools so that our subjects could participate in the game, as well as audio-based prompts for those who did not have a computer but were participating via phone. Our intention was to help the senior residents make direct connections between the systematic knowledge that they gain from the lectures and their resultant improved sense of actional autonomy. This improved sense of autonomy is exemplified in activities such as planning for health scenarios in advance and setting goals, thereby taking actions that contribute positively to their health.
After the partnering organization finished giving vaccines to senior residents, the management center developed the wellness education sessions into an official program offered as an ongoing series by the organization’s regional wellness nurses, using our tools to facilitate conversations and activities (see Fig. 3). Additionally, we are in the process of exploring procedural autonomy by utilizing a deliberate forum (Fishkin & Luskin, 2005, n.d.) for enhancing the senior residents’ autonomy as thoughts when deciding the topics and ideas of these wellness lectures. Deliberate forum is a grassroots, democratic process that enables citizens to deliberate about local issues with the support of structural processes. We will assess how collective decision-making about the topics, forms, and games comprising the lectures can serve as a self-sustainable system that supports the autonomous co-design of the lecture series by senior residents and staff members.
4 Discussion
I have reviewed how autonomy has been conceptualized by healthcare and design scholars. Broadly speaking, healthcare scholars have focused on procedures that protect decisional autonomy in medical interventions, while design scholars extend the conception of autonomy to include relational and actional autonomy in broader contexts. I argue that the study of autonomy is essential in developing human-centered principles of healthcare service design, as services are coproduced by diverse people, and there is a need to consider the different aspects of these multiple agents. Multidimensional concepts of autonomy will help expand the concept of healthcare services and create opportunities for design interventions, hence broadening the horizon of possibilities that healthcare services can strive to achieve and offer. I will discuss the autonomy of multiple agents who are involved in the system of cure and care and highlight a few questions that can nurture discussions of autonomy in healthcare service design and the development of methods, tools, and projects.
4.1 Autonomy of Patients
Patients are not a single entity, as discussed in the scholarly literature about relational autonomy, and providing support to better connect people is one way that designers can provide their expertise. Scholars of healthcare service design need to include relational identity in their discussions of autonomy in addition to discussing individual identity. Moreover, they should extend their concept of an autonomous unit from an individual to their family and caregivers. Such a shift opens up the possibility of expanding the service system so that it is more inclusive and thus considers the autonomy of patients who do not express themselves in the same way that so-called standard patients would. These patients would include children, people with mental issues, or patients with other severe conditions, such as dementia or terminal cancer. The discussions of people with disabilities and chronic disease reveal that their autonomy is intensely situational. I argue that the dependency that arises due to these conditions does not necessarily diminish a patient’s autonomy. Rather, dependency can supplement one’s autonomy from the perspective of seeing the patient as a holistic person. How can we design a system that considers the unique needs of less-represented populations and, in so doing, arrive at a more comprehensive understanding of autonomy? How can we design systems that provide holistic support in the ecology of care as ongoing processes that benefit patients and their families throughout their lives? How can designers gradually nurture the autonomy of patients during their transition from cure (e.g., surgery) to care (e.g., continued self-care) phase so that the patient recovers their life in a holistic sense? How can designers create services to provide personalized support for the different autonomy needs of patients, which could include autonomy of thought, autonomy of action, and autonomy of decision-making?
4.2 Autonomy of Healthcare Workers
The principle of respecting patient autonomy in medical ethics has evolved to protect the decisional rights of patients, but at the same time, it is also a procedure created to protect healthcare workers from potential conflict with patients and their families. Doctors are only a small part of the diverse community of experts and laborers who support healthcare systems, and issues associated with a lack of protocols and burnout of healthcare workers have surfaced during the pandemic. How can we create a system that can better support the autonomy of these workers and also protect their decisional rights? How can services and products help these workers so that they can carry out actions that reflect the decisions of patients and their families? Additionally, in practice, there are continued efforts by healthcare workers to support patients so that they can make “correct” decisions. How can services and products nudge patients and their family members so that they can make the best decisions while keeping the efficiency of autonomy grounded in the concept of negative freedom?
4.3 Autonomy of Designers
One thing that differentiates the field of design from fine art may be that designers must consider the unique needs of various agents when designing, especially those of users. However, there have been more discussions that suggest designers do have authority over the design process and about how the autonomy of designers influences the value manifested in products and services. Designers can learn from the history of medical ethics, as the relationship between the autonomy of designers and the autonomy of users recalls discussions about medical paternalism and the autonomy of patients. For example, when considering medical paternalism and patient’s rights, designers can examine the array of healthcare design products and services on a spectrum. At one end, there are products and services that strongly reflect the intention of the designer and limit the autonomy of users. At the other end, there are products and services that ask so much of users that users become confused. How can we balance the autonomy of designers, users, and clients when making design decisions and determining the intended usage of healthcare products and services? How can we create more concrete methods, models, and tools that can help designers to consider the autonomy needs of multiple agents when designing and thus strive for balanced autonomy in healthcare design research and processes? What can design learn from healthcare in terms of respect for autonomy? For example, as there is already an emphasis on autonomy as ends in the field of design, designers should learn from healthcare experts’ concept of autonomy as means. In so doing, designers can more concretely develop systematized procedures in the creation, usage, and evaluation of healthcare services and products from the perspective of autonomy.
4.4 Autonomy of Technology
Technology is a new agent in healthcare ecology, which is one reason why design is gaining critical importance in healthcare. Many people share the expectation that fast-evolving technology will soon obtain its own autonomy. In the near future, highly autonomous machines and intelligences will manage social systems, even without the intervention of human agents. Although these technologies may not entirely usurp human agents, this situation begs the question: What is the role of designers in a society where technology will gain autonomy when there is no proper support for people’s autonomy? This question is especially applicable to healthcare where patient autonomy is crucial. In this respect, it is essential to develop the ethics and guidelines of healthcare design, especially in relation to evolving technology. I would argue that the concept of autonomy based on positive freedom is synonymous with the philosophical tradition of moral autonomy (autonomy of thought), which is closely tied not only to individual identity but also to the moral value of certain societies. Design materializes these thoughts and helps users to reflect them in their decisions and actions in a way that can be justifiable to all stakeholders. In this sense, design is a moral process, especially when designers create healthcare-related products and services that directly impact people’s lives and well-being. Therefore, designers need to pay ethical attention to the design of healthcare services and products when incorporating technology, which will be another key agent.
5 Conclusion
In this chapter, I have introduced the diverse conceptions of autonomy discussed in both healthcare and design. This study contributes to these two fields by providing a grounding principle of autonomy for the collaboration between healthcare and design. I propose that there is a need to expand the burgeoning discussion of autonomy in healthcare design and provide a more comprehensive understanding of autonomy that considers autonomy as both means and ends. The discussion on autonomy provides a framework for healthcare service designers to develop methods and tools that highlight the importance of autonomy in design processes. The study of autonomy as a human-centered principle of healthcare design provides a new lens for scholars who study medical and design ethics. I hope this chapter will provide the opportunity for the design community to discuss autonomy beyond the control of interface to a broader service-level consideration and a self-justifying value of design that supports people’s everyday lives.
References
Beauchamp, T. L., & Childress, J. F. (1979). Principles of biomedical ethics. New York, Oxford: Oxford University Press.
Berlin, I. (1969). Two concepts of liberty. In I. Berlin (Eds.), Four essays on liberty (pp. 118–172). London, UK: Oxford University Press.
Burkhardt, M. A., & Nathaniel, A. K. (2002). Practice issues related to patient self-determination. In N. Y. Albany (Ed.), Ethics & issues in contemporary nursing (pp. 205–232). Albany, NY: Delmar Thomson Learning Inc.
Calvo, R. A., Peters, D., Johnson, D. & Rogers, Y. (2014). Autonomy in technology design, In ACM CHI 2014 extended abstracts on human factors in computing systems (pp. 37–40).
Davy, L. (2015). Philosophical inclusive design: Intellectual disability and the limits of individual autonomy in moral and political theory. Hypatia, 30(1), 132–148.
Deci, E. L., & Ryan, R. M. (2008). Self-determination theory: A macrotheory of human motivation, development, and health. Canadian Psychology/psychologie Canadienne, 49(3), 182–185.
De Visser, E. J., Pak, R., & Shaw, T. H. (2018). From automation to autonomy: The importance of trust repair in human–machine interaction. Ergonomics, 61(10), 1409–1427.
Edelstein, L. (1943). The hippocratic oath: Text, translation and interpretation. Baltimore, MD: The Johns Hopkins Press.
Entwistle, V. A., Carter, S. M., Cribb, A., & McCaffery, K. (2010). Supporting patient autonomy: The importance of clinician-patient relationships. Journal of General Internal Medicine, 25(7), 741–745.
Fishkin, J. S., & Luskin, R. C. (2005). Experimenting with a democratic ideal: Deliberative polling and public opinion. Acta Politica, 40(3), 284–298.
Friedman, B. (1996). Value-sensitive design, Interactions, 3(6), 16–23.
Friedman, B. (1998). User autonomy: Who should control what and when? A CHI 96 workshop. ACM SIGCHI Bulletin, 30(1), 26–29.
Friedman, M. A. (1986). Autonomy and the split-level self. The Southern Journal of Philosophy, 24(1), 19–35.
Güldenpfennig, F., Mayer, P., Panek, P. & Fitzpatrick, G. (2019). An autonomy-perspective on the design of assistive technology experiences of people with multiple sclerosis. In The ACM CHI conference on human factors in computing systems, Glasgow, UK (pp. 1–14), 4–9 May.
Jennings, B. (2016). Reconceptualizing autonomy: A relational turn in bioethics. Hastings Center Report, 46(3), 11–16.
Kant, I. (1785/1998). Groundwork for the metaphysics of morals (M. Gregor, Trans.). Cambridge, UK: Cambridge University Press.
Karpen, I. O., Gemser, G., & Calabretta, G. (2017). A multilevel consideration of service design conditions: Towards a portfolio of organisational capabilities, interactive practices and individual abilities. Journal of Service Theory and Practice, 27(2), 384–407.
Kim, M. (2021). A study of dignity as a principle of service design. International Journal of Design, 15(3), 87–100.
Kim, M., Ramdin, V., Pozzar, R., Fombelle, P., Zhou, X., Zhang, Y., & Jiang, M. (2022). Healthy aging adviser: Designing a service to support the life transitions and autonomy of older adults. The Design Journal, 25(2), 143–164.
Last, J. M. (2007). A dictionary of public health. Oxford, UK: Oxford University Press.
Nietzsche, F. (1883/2008). Thus spoke Zarathustra: A book for everyone and nobody. Oxford, UK: Oxford University Press.
Lindberg, C., Fagerström, C., Sivberg, B., & Willman, A. (2014). Concept analysis: Patient autonomy in a caring context. Journal of Advanced Nursing, 70(10), 2208–2221.
Littlewood, W. (1996). Autonomy: An anatomy and a framework. System, 24(4), 427–435.
Mackenzie, C., & Stoljar, N. (Eds.). (2000). Relational autonomy: Feminist perspectives on autonomy, agency, and the social self. Oxford, UK: Oxford University Press.
Millar, J. (2015). Technology as moral proxy: Autonomy and paternalism by design. IEEE Technology and Society Magazine, 34(2), 47–55.
Perkins, M. M., Ball, M. M., Whittington, F. J., & Hollingsworth, C. (2012). Relational autonomy in assisted living: A focus on diverse care settings for older adults. Journal of Aging Studies, 26(2), 214–225.
Plato, P. (1995). Translated by A. Nehamas and P. Woodruff. Indianapolis, IN: Hackett.
Pugh, J. (2020). Autonomy, rationality, and contemporary bioethics. Oxford, UK: Oxford University Press.
Rotter, J. B. (1966). Generalized expectancies for internal versus external control of reinforcement. Psychological Monographs: General and Applied, 80(1), 1–28.
Rousseau, J. J. (1762/2018). The social contract and other later political writings. Cambridge, UK: Cambridge University Press.
Rozenblit, J. W. (1992). Design for autonomy: An overview, Applied Artificial Intelligence an International Journal. 6(1), 1–18.
Sangiorgi, D. (2011). Transformative services and transformation design. International Journal of Design, 5(2), 29–40.
Schermer, M. (2002). The different faces of autonomy: Patient autonomy in ethical theory and hospital practice (Vol. 13). Berlin, Germany: Springer Science & Business Media.
Sherwin, S., & Winsby, M. (2011). A relational perspective on autonomy for older adults residing in nursing homes. Health Expectations, 14(2), 182–190.
Tauber, A. I. (2001). Historical and philosophical reflections on patient autonomy. Health Care Analysis, 9(3), 299–319.
Varelius, J. (2006). The value of autonomy in medical ethics. Medicine, Health Care and Philosophy, 9(3), 377–388.
Walker, M. U. (2000). Getting out of line: Alternatives to life as, Mother time: Women, aging, and ethics (pp. 97–111).
Zhu, L., Zhang, S. & Lu, Z. (2020). Respect for autonomy: Seeking the roles of healthcare design from the principle of biomedical ethics, HERD: Health Environments Research & Design Journal, 13(3), 230–244.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this chapter
Cite this chapter
Kim, M. (2023). Patient Autonomy and User Autonomy in the Ecology of Care. In: Pfannstiel, M.A. (eds) Human-Centered Service Design for Healthcare Transformation. Springer, Cham. https://doi.org/10.1007/978-3-031-20168-4_9
Download citation
DOI: https://doi.org/10.1007/978-3-031-20168-4_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-20167-7
Online ISBN: 978-3-031-20168-4
eBook Packages: Business and ManagementBusiness and Management (R0)