Abstract
Cardiac rhythm disorders (arrhythmias) are one of the leading causes of death worldwide. Therefore, the detection and classification of arrhythmias are essential for diagnosing patients with cardiac abnormalities. With new technologies, we can see the opening of medical institutions toward health information technology systems. To give researchers an overview of existing works about health monitoring systems for heart patients, we have established a comparative study between recent and well-known methods based on their results. The focus is in this comparison on the features used, the signal length, the datasets used, features extraction methods, features selection methods, classification methods, and the performances of each method. Furthermore, we classified these works by disease types (Paroxysmal Atrial Fibrillation PAF, Atrial Fibrillation AF, Ventricular Tachyarrhythmia VTA such as Ventricular Tachycardia (VT) and Ventricular Fibrillation (VF), Sudden Cardiac Death SCD, Obstructive Sleep Apnea OSA).
According to this comparative study, it has been found that many studies got exciting results. However, the classification rate achieved remains moderate. Moreover, heart rate monitoring devices are not within reach of the average citizen in terms of price and prediction time, and more studies are needed using more extensive databases. This study gives a comprehensive view of what is currently being done to monitor heart patients’ health. After discussing the achievements and limitations of existing approaches to monitoring the status of cardiac patients, we conclude by providing several potential research directions for the future.
Access provided by Autonomous University of Puebla. Download conference paper PDF
Similar content being viewed by others
Keywords
1 Introduction
According to the World Health Organization (WHO) [25], cardiovascular diseases occupy first place in the medical field as a leading cause of death worldwide over the past 20 years. Also, obstructive sleep apnea (OSA) is a source of fatigue and also cardiovascular diseases where its incidence increases almost linearly with age in adults [15]. Early detection of cardiac abnormalities is an exciting field, which has become the focus of many researchers because of the seriousness of its consequences, such as sudden death or subsequent physical or psychological sequelae. On the other hand, there are many types of heart diseases, one of them known as arrhythmia or also heart rhythm abnormalities such as Atrial Fibrillation (AF), Ventricular Tachycardia (VT), and Ventricular Fibrillation (VF) ...
Many companies have shown interest in detecting heart diseases such as cardiac arrhythmia via smart devices, namely the Android Wear, Apple Watch, and CRONOVO... Millions of people wear heart rate sensors on their wrists, but these devices do not allow automatic learning to detect people with arrhythmias using this data in terms of results and high price. Furthermore, simple ECG acquisition is insufficient because many heart rhythm abnormalities require continuous recording of this signal. It should be noted that the absence of the patient’s medical history forces the doctor to prescribe maximum treatment to cope with the uncertainty of the diagnosis, which can tire the patient by taking medication with adverse effects or performing exhausting daily tests.
Various methods have been proposed in the studies to monitor the health status of patients with chronic heart disease through ECG monitoring for early detection of cardiac abnormalities as well as to detect untreated sleep apnea associated with cardiovascular disease [38] where several techniques have been proposed to derive respiratory information from ECG signal. To increase predictability, each of these methods uses a combination of features extracted by linear, time-frequency, and nonlinear analysis performed on heart rate variability, which allows researchers to extract new features and compare them with conventional features. In addition, some studies have automatically extracted features using CNN to predict heart disease. Other methods also extract respiratory information from a heart rate variability (HRV) signal, which calculates ECG-derived respiration signal (EDR) and Apnea-hypopnea index (AHI).
The effectiveness of these features varies depending on the period to be predicted and the disease to be discovered. Each disease has its identifiable features that appear on the electrocardiogram ECG. On this basis, a comparison is made between 12 methods from the research of recent years in the detection of heart disease and sleep apnea because there is a relationship between them. We classify the heart diseases in groups according to the type of disease and compare them in terms of learning methods, the features used, and the results obtained while mentioning the shortcomings of each method. In contrast, we compare the methods developed in the investigations of cardio-respiratory monitoring.
This paper is composed of three sections in addition to this introduction, and it is organized as follows: Sect. 2: Classification of ECG-based studies by disease types, Sect. 3: conclusion.
2 Classification of ECG-Based Studies by Disease Types
This paper will cover three main classifications of the most common and dangerous areas of heart disease by categorizing studies that have used deep and machine learning techniques to predict these diseases and the impact of extracted features on prediction results in recent years. In addition, it will cover one of the diseases related to cardiovascular diseases in the fourth classification. The following are four main classifications: (1) Paroxysmal atrial fibrillation (PAF) and Atrial Fibrillation (AF), (2) Ventricular Tachyarrhythmia (VTA) such as Ventricular Tachycardia (VT) and Ventricular Fibrillation (VF), (3) Sudden Cardiac Death (SCD), (4) Obstructive Sleep Apnea OSA.
2.1 Paroxysmal Atrial Fibrillation (PAF) and Atrial Fibrillation (AF)
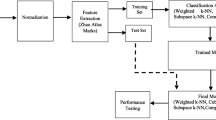
One of the most widely used applications of machine learning in cardiology is the prediction of cardiac arrhythmias. Paroxysmal atrial fibrillation (PAF) and atrial fibrillation (AF) are the most common significant cardiac arrhythmias. Doctors emphasize that if PAF is not treated promptly, it may progress to persistent Atrial Fibrillation (AF), resulting in a high risk of morbidity and mortality. As a result, more focus is being paid to the prediction of PAF to enable early detection and halt the disease’s progression. A validated approach to forecast PAF has not yet been developed despite the availability of pharmacological and electrical therapies. Numerous studies have focused on predictive models using predictive machine learning (ML) systems composed of different sub-processes such as signal preprocessing, significant feature extraction, feature selection, and classification algorithms.
Ebrahimzadeh et al. [6] extracted the HRV signal from the electrocardiogram ECG and segmented it into 5-min intervals, they used a variety of features retrieved from heart rate variability (HRV) by linear, and Wigner Ville transforms to extract Time-Frequency, and thereupon, nonlinear features. Then the best features combination are selected based on their capacity to differentiate the two classes, and Local Feature Subset Selection is used to accomplish the selection of features. Furthermore, to distinguish between signals before and after PAF, they utilized four classifiers: the K-nearest neighbor (KNN), support vector machine (SVM), Multilayer Perceptron (MLP), and Mixture of Expert (ME). A ten-fold cross-validation approach is used to assess the performance of the classifiers. Moreover, They employed the standard database named the Atrial Fibrillation Prediction Database (AFPDB) [10], which contains 53 patients (106 regular and abnormal recordings), resulting in 100% sensitivity, 95.55% specificity, and 98.21% accuracy.
Although implantable defibrillators have limited computational capacities, they can detect and treat PAF early. To help lower the computational overhead of initiating PAF detection, Parsi et al. [27] propose seven novel features for predicting the existence of PAF with high accuracy. They extracted features from a Poincar’e representation of R-R interval signals recovered from patient ECG data in 5-min segments and prioritized them based on feature rankings. The method is evaluated using the same standard database (AFPDB) [10] that [6] worked with. Their paper [27] uses the features with four standard classification techniques for PAF prediction: SVM, MLP, KNN, and Random Forest (RF) to compare the classic and proposed feature sets. Furthermore, the performance of the classifiers is evaluated using a ten-fold cross-validation technique with different feature sets. Their findings confirm that the results are further improved when the proposed features are combined with several classic features, reaching 98.8% sensitivity, 96.7% specificity, and 97.7% accuracy.
Atrial fibrillation (AF) can develop from PAF. Some patients with AF have no apparent clinical symptoms, exposing them to the risk of several severe illnesses while they are unaware of it. As a result, early detection and prediction of AF and appropriate treatment to reduce its occurrence are clinically and socially significant. Therefore, Shen et al. [33] study aim to discover AF by proposing a method that combines manual and neural network extraction features. First, They processed the ECG signals into 4-s data, then manually extracted 180-dimensional time-frequency-domain features and combined them with the improved 128-dimensional features extracted by the neural network, they also employed an integrated model to enhance machine learning results, including Decision Tree, RF, GBDT, XGBoost, LightGBM as sub-models, and the stacking model in the final experiment, this is to discriminate between signals that indicate AF and those that do not indicate AF. They used a five-fold cross-validation approach for the initial training set to assess the performance of the stacking model. Furthermore, they performed their experiments using the standard database called the MIT-BIH Atrial Fibrillation Database [22], which contains 25 records (50 signals), each record is about ten-hour with the frequency equaling 250 HZ. They achieved an accuracy of 99.1%.
Marinucci et al. [21] aim to offer a novel artificial neural network (ANN) for reliably detecting AF in ECGs recorded via portable devices. To achieve this goal, they created a supervised fully connected artificial neural network (RSL_ANN) using repeated structuring and learning procedures [30]. Then, the two most common symptoms of Atrial Fibrillation on an ECG are interval irregularity and the disappearance of the P wave, which is replaced by a continuous f wave [33]. Their research [21] uses 19 features represented in 11 morphological, four on F waves, and four on HRV features in the input to a supervised fully connected artificial neural network (RSL_ANN) to distinguish between AF and non-AF classes. RSL_ANN was developed and evaluated based on the “AF Classification from a Short Single Lead ECG Recording” database [4], and acquired by AliveCor with the portable KARDIA device [4]. It contains 8244 a short Single ECG, duration ranging from 9 s to 61 s (average: 33 s), and the sampling rate = 300 Hz. For the scope of their paper, they used 8028, a short Single ECG (training: 4493; validation: 1125; testing: 2410). They achieved an area under the curve (AUC) of 91.1% (CI: 89.1–93.0%) for the training, 90.2% (CI: 86.2–94.3%) for the validation, and 90.8% (CI: 88.1–93.5%) for the testing datasets.
The comparison between methods based on PAF and AF are summarized in Table 1.
Discussion of the Comparison Between Method Based on ‘PAF and AF’
We found that the researchers applied SVM, KNN, MLP, RF, and CNN methods to detect AF and PAF, with the accuracy varying between 73.8% and 99.1%, using features ranging from 12 to 308 features. They used datasets for atrial fibrillation from Physionet [11] represented in AFPDB [10], the MIT-BIH Atrial Fibrillation Database [22], and AF Classification from a Short Single Lead ECG Recording Database [4]. The signal length of their ECG records ranges between 4 s and 5 min.
The researchers in [6, 27] extracted HRV relative features on the AFPDB [10] database as an input to the model. They found a remarkable performance. However, the number of subjects in their training and testing set was not nearly enough. Ebrahimzadeh et al. [6] have found the best results with 100% sensitivity and 95.5% specificity. Although their sensitivity cannot be improved, they are based on a mixture of expert (ME) classifiers, a more complex approach than the individual model.
In [33], deep learning methods are effective for classification accuracy but not so much for comprehensive analysis of HRV signals. At the same time, in [21], the authors chose the Features based on the changes that occur in the recording of the ECG during AF, which is the disappearance of the p wave and its replacement by the continuous f wave and possible HRV increment. This was confirmed by the statistical analysis of feature distributions of known clinical observations performed. However, the irregularity of the RR interval can also be seen in other types of arrhythmias. The P wave or f wave is a weak signal, and it has a difficult time detecting feature points and grasping form features.
2.2 Ventricular Tachyarrhythmia (VTA)
Since the ventricles are fundamental to the heart’s capacity to pump blood, any disturbance in their regular rhythm may be devastating. Where doctors confirm that among life-threatening ventricular abnormalities is ventricular tachyarrhythmia (VTA), which includes ventricular tachycardia (VT) and ventricular fibrillation (VF). Because of this, Some studies have shown encouraging results in predicting the occurrence of VT and VF using classic HRV features and machine learning algorithms.
The goal of Taye et al. [36] in their studies was to see if QRS complex features might be used to predict VF as compared to classic HRV measures, and to achieve this goal, they extracted two features from 120 s ECG signals represented in QRS complex singed area and R-peak amplitude, as well as traditional HRV features for comparison, to predict the beginning of VF 30 s before its occurrence. They tested and trained two ANN classifiers based on 10-fold cross-validation with two different input parameters. The first, with 11 features extracted from HRV, they get an accuracy of 72%, and the second one with 4 QRS complex shape features obtained a high accuracy of 98.6%. Taye et al. [36] have worked on three datasets from PhysioNet [11] such as CU Ventricular Tachyarrhythmia Database (CUVTDB) [9], (AFPDB) [10], MIT-BIH Normal Sinus Rhythm Database (NSRDB) [11].
The primary purpose of another study by Taye et al. [35] was to validate the CNN algorithm’s efficacy in feature extraction and VTA prediction. According to this basis and to predict the onset of VT and VF within 1 min, they used a one-dimensional CNN to extract features from 5 min HRV signals. They used a 10-fold cross-validation approach to assess the accuracy of the prediction and achieved an accuracy of 84.6%. In addition, the spontaneous ventricular tachyarrhythmia database (MVTDB) [12] in PhysioNet [11] was used to evaluate the method, which contains 135 pairs of RR intervals recorded by implantable cardioverter defibrillators (ICD) with Sampling rate equal 10000 HZ.
Because ICD devices have limited computing capabilities, it is essential to classify VTA events leading to SCD and reducing the number of features helps reduce the load on the device. So to predict VT and VF for devices with limited computational capabilities, such as ICDs, with a reduced set of features, Parsi et al. [26] ranked HRV features by applying feature selection techniques based on a Minimal redundancy-maximal relevance (mRMR) method by combining mRMR classifiers with statistical machine learning such as SVM, kNN, and RF. They obtained 91.5% accuracy with a kNN classifier while processing a 5 min window of R-R interval signals and 90.1% accuracy with an SVM classifier while processing a 1 min window of R-R interval signals utilizing only 6 HRV features. The authors used leave-one-out cross-validation method in the assessment database, which is (MVTDB) [12] which [35] have also worked on.
Since of the enormous differences in ECG morphology, clinicians find that it is challenging to diagnose a patient’s heart state from an ECG signal because manual interpretation is an error-prone task [18, 20, 31]. Therefore, a computer-aided diagnostic (CAD) system for classifying cardiac anomalies might help identify the severity of the disease [20]. The objective of Mandal et al. [20] is to create a CAD system that can classify ECG signals from patients with VT and VF. They used thirty feature extraction methods to calculate the features of HRV signals and ECG pulse images. In order to reduce the number of features, they employed the Cardiac-score selection algorithm. Furthermore, to distinguish between healthy and VA persons, they utilized an ensemble classifier such as KNN, SVM, RF and Probabilistic Neural Network (PNN). They achieved an accuracy of 99.99%, and evaluated the performance of the classifiers using a five-fold cross-validation technique, worked on three datasets as (CUVTDB) [9], (NSRDB) [11], The MIT-BIH Malignant Ventricular Arrhythmia Database (VFDB) [32].
The comparison between methods based on ventricular tachycardia and ventricular fibrillation are summarized in Table 2.
Discussion of the Comparison Between Method Based on ‘VT and VF’
The presented works use KNN, CNN, and SVM methods to detect VTA, including ventricular tachycardia (VT) and ventricular fibrillation (VF), giving an accuracy between 84,6% and 99,99% by using 4 to 7 features. They used datasets from Physionet [11], such as CUDB [9], AFPDB [10], NSRDB [11], MVTDB [12], VFDB [32] and MVTDB [12], with a signal length between 1 min and 30 min.
Although Taye et al.’s result in [36] show that the performance of ANN was excellent using QRS shape features compared to traditional HRV features, the datasets used were small. Therefore, to confirm the clinical feasibility of this approach, more research with a more significant number of datasets is needed. Moreover, the duration of prediction of the appearance of VF 30 s before it occurs is minimal, and the same may be said for the other paper by Taye et al. [35] implying that clinical applicability will require more research with a more significant number of datasets and an increase in the forecast time.
To improve the findings of [26], future research should focus on determining the ideal duration of signal length (which could be dynamic) based on clinical knowledge about heart problems.
The system’s detection accuracy is limited to samples. Although the study of [20] performed well, the database employed was insufficient, and future research should concentrate on developing a VTA detection system with a vast number of datasets.
2.3 Sudden Cardiac Death (SCD)
Sudden Cardiac Death (SCD) is an unexpected death caused by a loss of heart function that claims millions of lives worldwide each year [7]. Sudden Cardiac Death (SCD) happens within an hour of symptoms, and there is currently no reliable approach for early detection [29]. As a result, several researchers have turned their attention to predicting SCD.
To develop a novel approach to local feature subset selection for predicting sudden cardiac death from ECG signals, Ebrahimzadeh et al. [7] used meticulous methodologies developed in their previous studies for extracting features from non-linear, time-frequency, and classical processes. So they can select features that differ from one another in each 1-min interval before the incident. According to this team [7], the SCD can be predicted 12 min before it occurs using their proposed algorithm. After selecting the best combination of features, they used a multilayer perceptron (MLP) to differentiate ECG signals of normal subjects from those susceptible to SCD. They applied a leave-one-out cross-validation method, and they employed the database named the Sudden Cardiac Death Holter Database [32] and (NSRDB) [11], resulting in an accuracy of 88.29%.
Ebrahimzadeh et al. used in another work [5] an innovative and automated strategy to ensure Local Feature Subset Selection with the most rigorous methodology. They utilized time-domain, frequency-domain, time-frequency domain, and nonlinear HRV features. These suggested approaches allow them to find features that vary from one another every minute before an accident by selecting the best features found at each 1 min interval of the signal, allowing them to anticipate SCD 13 min before it occurs. They utilized four classifiers such as KNN, SVM, MLP, and ME, and to assess the performance of the classifiers, they used a leave-one-out cross-validation approach. Moreover, they also employed the same databases [32] [11] that they worked on in their previous work in order to predict sudden cardiac death (SCD), which led to improved accuracy to 90.18% for 13 min instead of 88.29% for 12 min
Rohila et al. [29] obtained one-hour ECG signals before VF onset that were divided into twelve 5 min segments, and these segments were converted into HRV signals. They used nonlinear techniques to extract features from HRV signals and five new S-transform based time-frequency domains in a comparative analysis of HRV for four subject groups: normal sinus rhythm (NSR), coronary artery disease (CAD), congestive heart failure (CHF), and SCD. They used Kruskal-Wallis one-way analysis of variance and multiple comparisons to assess the clinical relevance of the retrieved features. Moreover, they performed the classification using two classifiers represented in SVM and DT classifiers to classify between four classes: NSR, CAD, CHF, and SCD. They employed the database NSRDB [11], Long-Term ST Database (LTSTDB) [16], BIDMC Congestive Heart Failure Database (CHFDB) [3], and (SDDB) [32], which led to 91.67% accuracy, 83.33% sensitivity, 94.64% specificity.
The comparison between methods based on SCD are summarized in Table 3.
Discussion of the Comparison Between Methods Based on SCD
MLP, KNN, SVM, ME, and DT methods were applied to the SDDB [32], NSRDB [11], CHFDB [3], and LTSTDB [16] datasets from Physionet [11] to detect Sudden Cardiac Death (SCD). These presented works give an accuracy of 88.29% and 91.67% by using HRV features ranging from 15 to 23 features. The signal length of their ECG records ranges between 5 min and 13 min.
HRV is less established in predicting SCD risk in patients with coronary heart disease [8, 19], which also cannot be tested in other patients with atrial fibrillation or recurrent arrhythmias [19]. Furthermore, the reported advance prediction time of 5 to 13 min would limit the use of HRV for risk prediction of SCD in a clinical situation [5, 7, 29].
Experimental findings gained via retrospective data analysis are promising. However, to generalize the results, the approaches need to be evaluated on larger datasets [5, 7, 29].
2.4 Obstructive Sleep Apnea (OSA)
Untreated sleep apnea has been linked to a variety of conditions, including high blood pressure, cardiovascular disease, and neurovascular disease [14, 17, 24]. Because of this relation between OSA and cardiovascular disease, people with heart problems should have their breathing monitored. The gold standard for apnea diagnosis is polysomnography (PSG), but it is very expensive and time-consuming [13]. As a result, the researchers in recent years concentrated on creating low-cost, low-complex methodologies as an alternative to PSG in the OSA detection procedure. Authors of [1, 37] employed a variety of methods to detect OSA automatically using the SpO2 signal, and several approaches based on single-lead ECG readings have also been developed to detect OSA [2, 14, 34].
Zarei et al. [39] have proposed a new approach to extract features based on the spectral autocorrelation function and autoregressive (AR) models using single-lead ECG signals for automated sleep apnea detection. They used the sequential forward feature selection (SFFS) technique to choose the most effective features. Moreover, they performed the classification using RF classifiers to classify between the apnea and normal events based on a 10-fold cross-validation. They get an accuracy of 93.90%, a sensitivity of 92.26%, a specificity of 94.92% in per-segment classification, and 97.14% in pre-recording classifications. In addition, the Physionet Apnea-ECG [28] dataset from PhysioNet [11] was used to evaluate the method.
In another work by Zarei et al. [38], single-lead ECG recordings are used to detect OSA. The authors extracted the ECG-derived respiration (EDR) signal from a single-lead ECG using six distinct techniques. Furthermore, they extracted features from ECG-derived respiration (EDR) and HRV signals. To choose the most effective features, they used a sequential feature selection approach. Their method for detecting OSA is divided into two steps (per-segment classification and pre-recording classification). To determine the best classifier for per-segment, six different classifiers were used to detect apnea: KNN, RUSBoost, GentleBoost, Sub-spaceKNN, ANN, and SVM, which led to 93.26% accuracy, 91.52% sensitivity, 94.36% specificity which GentleBoost and 100% accuracy in pre-recording classifications. Furthermore, to assess the performance of the classifiers, they used A ten-fold cross-validation approach. Moreover, they utilized the Physionet Apnea-ECG [28] and Fantasia datasets [23] to evaluate the OSA detection technique and EDR extraction methods suggeste.
The comparison between methods based on OSA are summarized in Table 4.
Discussion of the Comparison Between Methods Based on OSA
Current HRV research focuses on determining how sympathovagal balance varies throughout sleep and in response to OSA disease. Future studies might evaluate the relative contributions of hypoxia, arousal, and intrathoracic pressure on changed HRV indices in individuals with OSA and cardiovascular disease using experimental designs.
3 Conclusion
Early diagnosis of cardiovascular disease such as cardiac arrhythmia can save human lives and help provide prompt treatment to avoid serious physical, psychological, and financial sequelae. The ECG is the primary tool for diagnosing the electrical activity of the heart because any abnormalities in cardiac activity are reflected in the ECG signals. However, the visual assessment of ECG signals is a difficult and time-consuming task. Therefore, the implementation of a system that continuously monitors the patient will ensure an objective and rapid diagnosis of cardiac arrhythmia. To provide researchers with a comprehensive view of the current works, we have established a comparative study between several existing works in this study. We classify ECG-based studies by disease types into four classes represented in Paroxysmal Atrial Fibrillation (PAF) and Atrial Fibrillation (AF), Ventricular Tachyarrhythmia (VTA) such as Ventricular Tachycardia (VT) and Ventricular Fibrillation (VF), Sudden Cardiac Death (SCD), Obstructive Sleep Apnea (OSA). Going forward, we will rely on increasing the anomaly prediction period, as well as using a larger, unified data set to make a more accurate comparison.
References
Al-Angari, H.M., Sahakian, A.V.: Automated recognition of obstructive sleep apnea syndrome using support vector machine classifier. IEEE Trans. Inf Technol. Biomed. 16(3), 463–468 (2012)
Atri, R., Mohebbi, M.: Obstructive sleep apnea detection using spectrum and bispectrum analysis of single-lead ECG signal. Physiol. Meas. 36(9), 1963 (2015)
Baim, D.S., et al.: Survival of patients with severe congestive heart failure treated with oral milrinone. J. Am. Coll. Cardiol. 7(3), 661–670 (1986). https://doi.org/10.1016/S0735-1097(86)80478-8
Clifford, G., et al.: AF classification from a short single lead ECG recording - the PhysioNet computing in cardiology challenge 2017 (2017). https://physionet.org/content/challenge-2017/1.0.0/
Ebrahimzadeh, E., et al.: An optimal strategy for prediction of sudden cardiac death through a pioneering feature-selection approach from HRV signal. Comput. Methods Programs Biomed. 169, 19–36 (2019)
Ebrahimzadeh, E., Kalantari, M., Joulani, M., Shahraki, R.S., Fayaz, F., Ahmadi, F.: Prediction of paroxysmal atrial fibrillation: a machine learning based approach using combined feature vector and mixture of expert classification on HRV signal. Comput. Methods Programs Biomed. 165, 53–67 (2018)
Ebrahimzadeh, E., Manuchehri, M.S., Amoozegar, S., Araabi, B.N., Soltanian-Zadeh, H.: A time local subset feature selection for prediction of sudden cardiac death from ECG signal. Med. Biol. Eng. Comput. 56(7), 1253–1270 (2018)
Evrengul, H., et al.: The relationship between heart rate recovery and heart rate variability in coronary artery disease. Ann. Noninvasive Electrocardiol. 11(2), 154–162 (2006)
Nolle, F.M., Badura, F.K., Catlett, J.M., Bowser, R.W., Sketch, M.H.: CREI-GARD, a new concept in computerized arrhythmia monitoring systems (1986)
Moody, G., Goldberger, A., McClennen, S., Swiryn, S.: Predicting the onset of paroxysmal atrial fibrillation: the computers in cardiology challenge 2001 (2001). https://physionet.org/content/afpdb/1.0.0/
Goldberger, A., et al.: PhysioBank, PhysioToolkit, and PhysioNet: Components of a new research resource for complex physiologic signals. Circulation 101(23), e215–e220 (2000)
Goldberger, A., et al.: Spontaneous ventricular tachyarrhythmia database (2007). https://physionet.org/content/mvtdb/1.0/
Gutiérrez-Tobal, G.C., Álvarez, D., Del Campo, F., Hornero, R.: Utility of AdaBoost to detect sleep apnea-hypopnea syndrome from single-channel airflow. IEEE Trans. Biomed. Eng. 63(3), 636–646 (2015)
Hwang, S.H., Lee, Y.J., Jeong, D.U., Park, K.S., et al.: Apnea-hypopnea index prediction using electrocardiogram acquired during the sleep-onset period. IEEE Trans. Biomed. Eng. 64(2), 295–301 (2016)
Inserm: Apnèe du sommeil. une source de fatigue, mais aussi de maladies cardiovasculaires. Website page (2017). https://www.inserm.fr/dossier/apnee-sommeil
Jager, F., et al.: Long-term ST database: a reference for the development and evaluation of automated ischaemia detectors and for the study of the dynamics of myocardial ischaemia. Med. Biol. Eng. Comput. 41(2), 172–183 (2003)
Khandoker, A.H., Gubbi, J., Palaniswami, M.: Automated scoring of obstructive sleep apnea and hypopnea events using short-term electrocardiogram recordings. IEEE Trans. Inf Technol. Biomed. 13(6), 1057–1067 (2009)
Krasteva, V., Jekova, I.: Assessment of ECG frequency and morphology parameters for automatic classification of life-threatening cardiac arrhythmias. Physiol. Meas. 26(5), 707 (2005)
Liew, R.: Electrocardiogram-based predictors of sudden cardiac death in patients with coronary artery disease. Clin. Cardiol. 34(8), 466–473 (2011)
Mandal, S., Mondal, P., Roy, A.H.: Detection of ventricular arrhythmia by using heart rate variability signal and ECG beat image. Biomed. Signal Process. Control 68, 102692 (2021)
Marinucci, D., Sbrollini, A., Marcantoni, I., Morettini, M., Swenne, C.A., Burattini, L.: Artificial neural network for atrial fibrillation identification in portable devices. Sensors 20(12), 3570 (2020)
Moody, G., Mark, R.: A new method for detecting atrial fibrillation using R-R intervals. Comput. Cardiol. 10, 227–230 (1983)
Iyengar, N., Peng, C.K., Morin, R., Goldberger, A.L., Lipsitz, L.A.: Age-related alterations in the fractal scaling of cardiac interbeat interval dynamics. Am. J. Physiol. 271, 1078–1084 (1996)
Nguyen, H.D., Wilkins, B.A., Cheng, Q., Benjamin, B.A.: An online sleep apnea detection method based on recurrence quantification analysis. IEEE J. Biomed. Health Inform. 18(4), 1285–1293 (2013)
World Health Organization: L’oms lève le voile sur les principales causes de mortalité et d’incapacité dans le monde: 2000–2019. Website page (2020). https://www.who.int/fr/news/item/09-12-2020-who-reveals-leading -causes-of-death-and-disability-worldwide-2000-2019
Parsi, A., Byrne, D., Glavin, M., Jones, E.: Heart rate variability feature selection method for automated prediction of sudden cardiac death. Biomed. Signal Process. Control 65, 102310 (2021)
Parsi, A., Glavin, M., Jones, E., Byrne, D.: Prediction of paroxysmal atrial fibrillation using new heart rate variability features. Comput. Biol. Med. 133, 104367 (2021)
Penzel, T., Moody, G., Mark, R., Goldberger, A., Peter, J.: The apnea-ECG database. In: Computers in Cardiology 2000 (Cat. 00CH37163), vol. 27, pp. 255–258. IEEE (2000). https://doi.org/10.1109/CIC.2000.898505
Rohila, A., Sharma, A.: Detection of sudden cardiac death by a comparative study of heart rate variability in normal and abnormal heart conditions. Biocybern. Biomed. Eng. 40(3), 1140–1154 (2020)
Sbrollini, A., et al.: Serial electrocardiography to detect newly emerging or aggravating cardiac pathology: a deep-learning approach. Biomed. Eng. Online 18(1), 1–17 (2019)
Schuch, S., Tipper, S.P.: On observing another person’s actions: influences of observed inhibition and errors. Percept. Psychophys. 69(5), 828–837 (2007)
Greenwald, S.D.: Development and analysis of a ventricular fibrillation detector. Master’s thesis, MIT Dept. of Electrical Engineering and Computer Science, Cambridge (1986)
Shen, M., Zhang, L., Luo, X., Xu, J.: Atrial fibrillation detection algorithm based on manual extraction features and automatic extraction features. In: IOP Conference Series: Earth and Environmental Science. vol. 428, p. 012050. IOP Publishing (2020)
Smruthy, A., Suchetha, M.: Real-time classification of healthy and apnea subjects using ECG signals with variational mode decomposition. IEEE Sens. J. 17(10), 3092–3099 (2017)
Taye, G.T., Hwang, H.J., Lim, K.M.: Application of a convolutional neural network for predicting the occurrence of ventricular tachyarrhythmia using heart rate variability features. Sci. Rep. 10(1), 1–7 (2020)
Taye, G.T., Shim, E.B., Hwang, H.J., Lim, K.M.: Machine learning approach to predict ventricular fibrillation based on QRS complex shape. Front. Physiol. 10, 1193 (2019)
Xie, B., Minn, H.: Real-time sleep apnea detection by classifier combination. IEEE Trans. Inf Technol. Biomed. 16(3), 469–477 (2012)
Zarei, A., Asl, B.M.: Automatic classification of apnea and normal subjects using new features extracted from HRV and ECG-derived respiration signals. Biomed. Signal Process. Control 59, 101927 (2020)
Zarei, A., Asl, B.M.: Performance evaluation of the spectral autocorrelation function and autoregressive models for automated sleep apnea detection using single-lead ECG signal. Comput. Methods Programs Biomed. 195, 105626 (2020)
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Switzerland AG
About this paper
Cite this paper
Kerdoudi, S., Guezouli, L., Dilekh, T. (2023). An Overview of Health Monitoring Systems for Arrhythmia Patients. In: Chikhi, S., Diaz-Descalzo, G., Amine, A., Chaoui, A., Saidouni, D.E., Kholladi, M.K. (eds) Modelling and Implementation of Complex Systems. MISC 2022. Lecture Notes in Networks and Systems, vol 593. Springer, Cham. https://doi.org/10.1007/978-3-031-18516-8_1
Download citation
DOI: https://doi.org/10.1007/978-3-031-18516-8_1
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-18515-1
Online ISBN: 978-3-031-18516-8
eBook Packages: EngineeringEngineering (R0)